Histological Evaluation of Cassava Starch/Chicken Gelatin Membranes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of the Sample of Chicken Gelatin
2.2.2. Synthesis of Cassava Starch/Gelatin Composite Membranes
2.2.3. Membrane Characterization
Thermal Analysis
Differential Scanning Calorimetry (DSC)
Functional Group Characterization of the Membranes
Morphology Analysis
X-ray Diffraction (XRD)
2.2.4. In Vivo Biocompatibility Tests
3. Results and Discussion
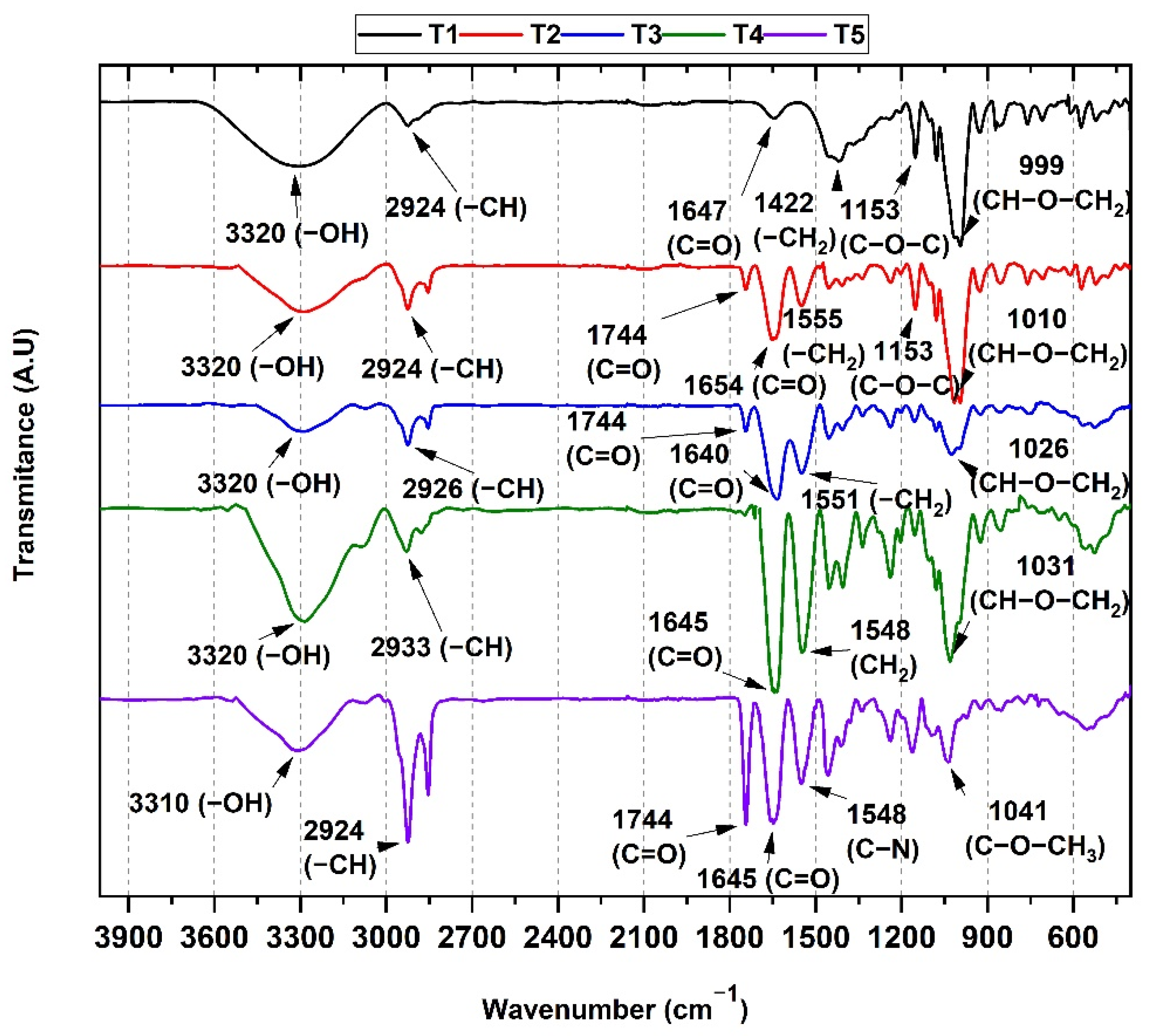
3.1. FT-IR Spectroscopy Analysis of the Cassava Starch/Gelatin Membranes
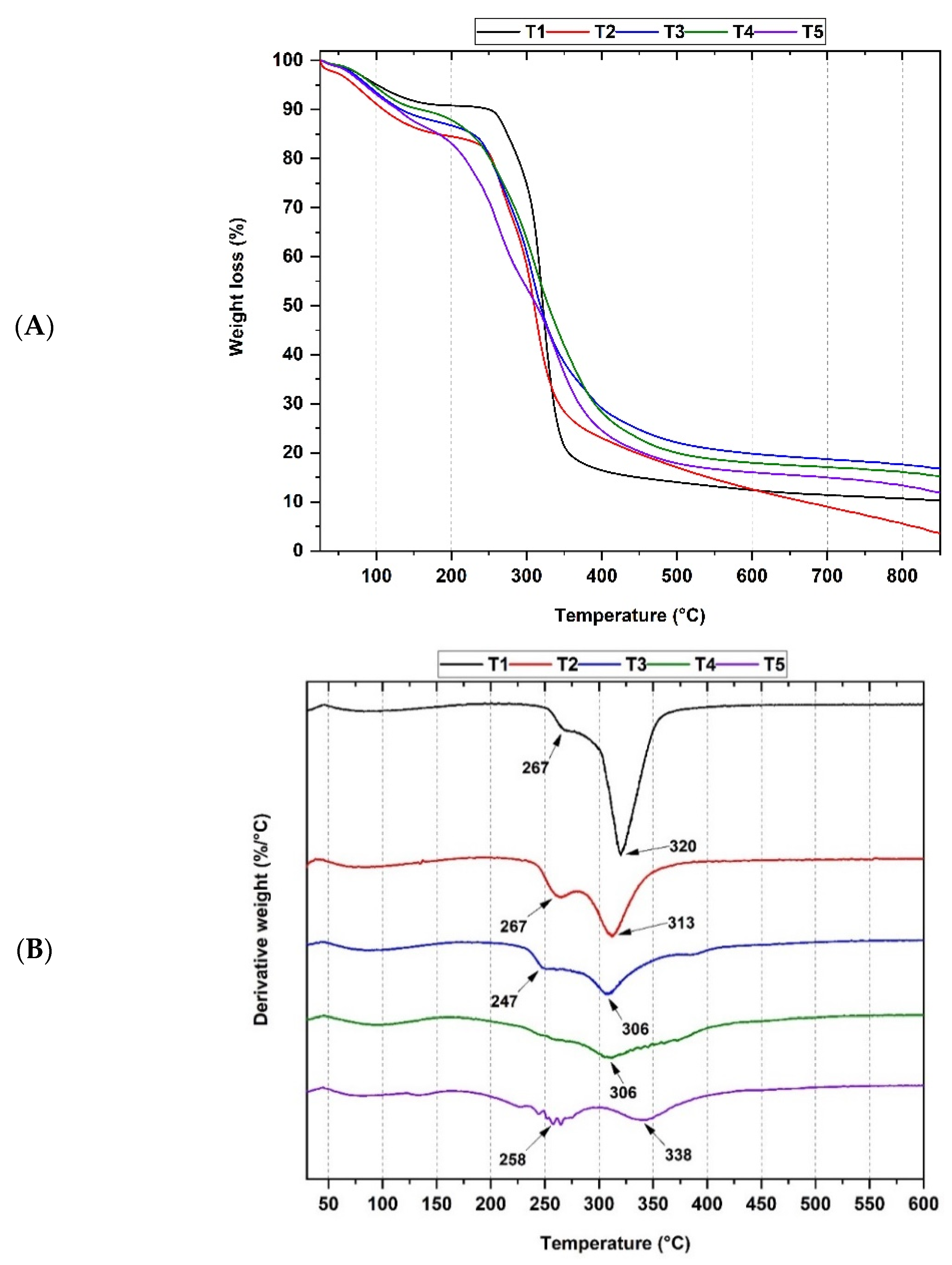
3.2. Thermal Analysis of Cassava Starch/Gelatin Membranes
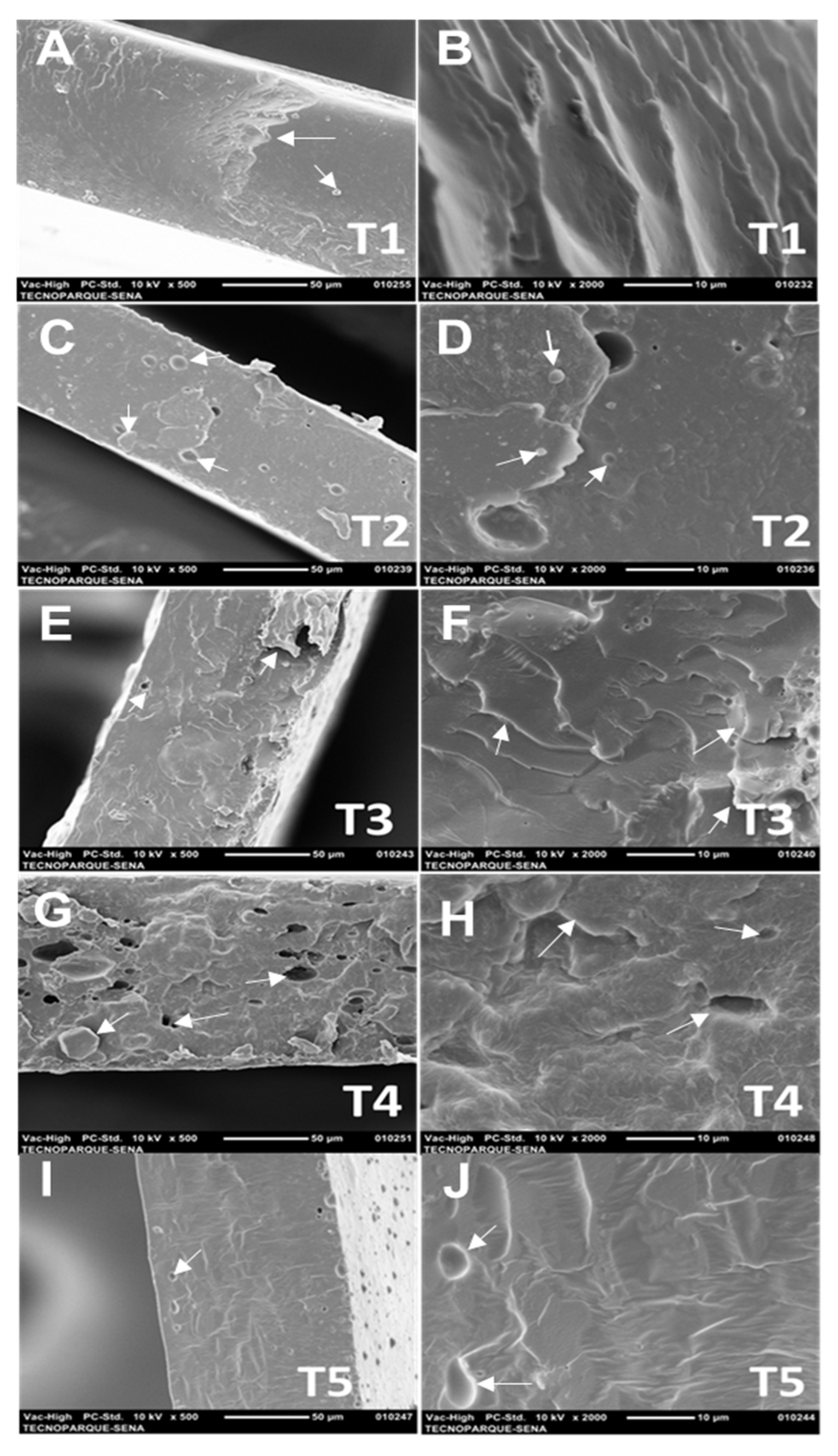
3.3. Scanning Electron Microscopy (SEM) of Cassava Starch/Gelatin Membranes
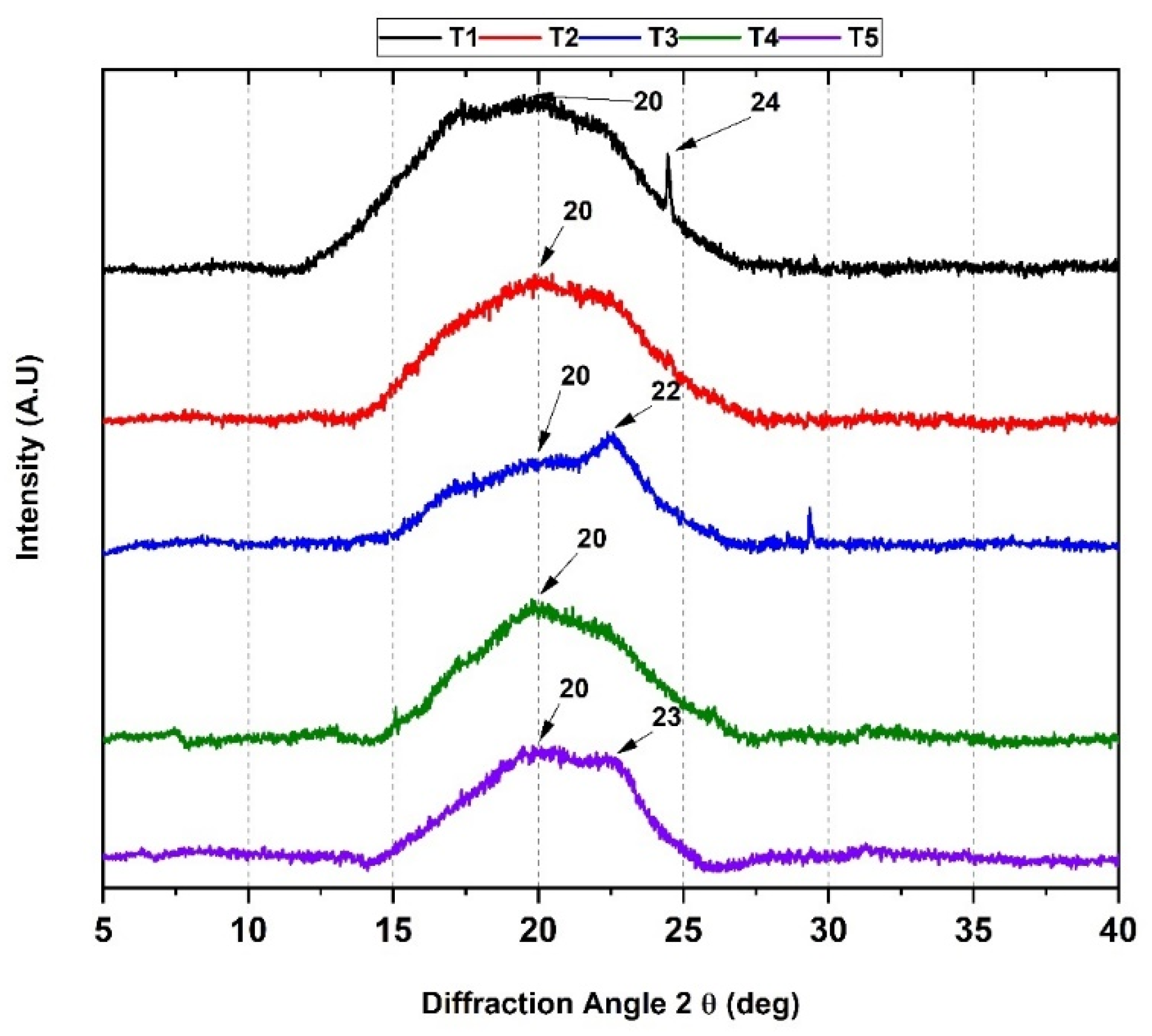
3.4. X-ray Diffraction (XRD)
3.5. Biological Tests
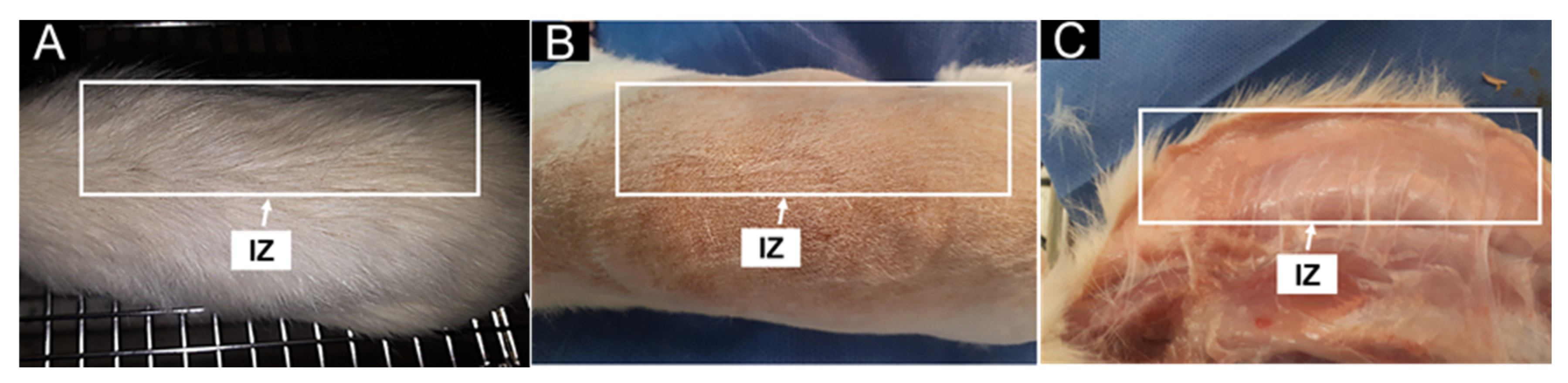
3.5.1. In Vivo Biocompatibility Assessment
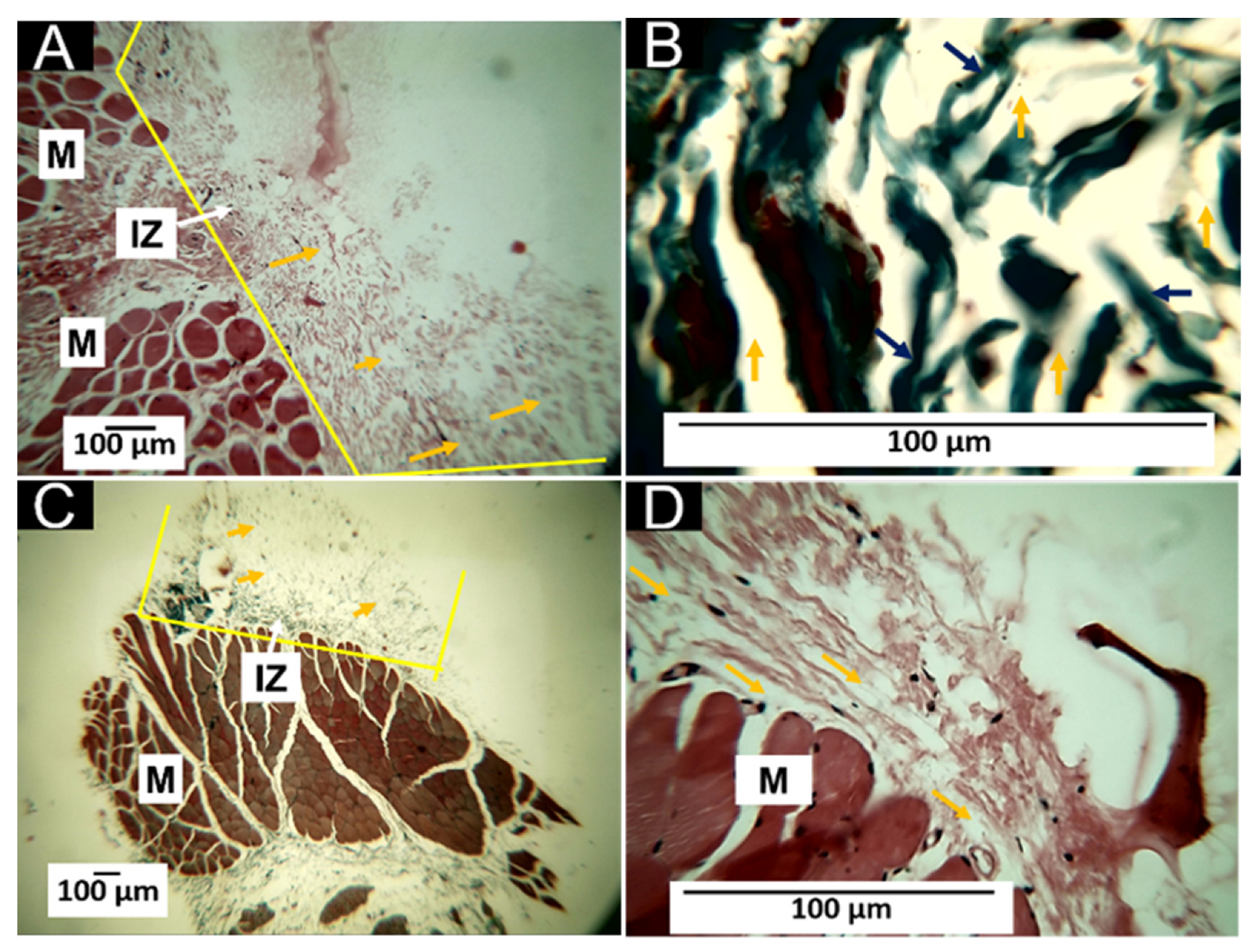
3.5.2. Histology Results of T1 (100%CS)
3.5.3. Histology Results of T2 (25%G/75%CS)
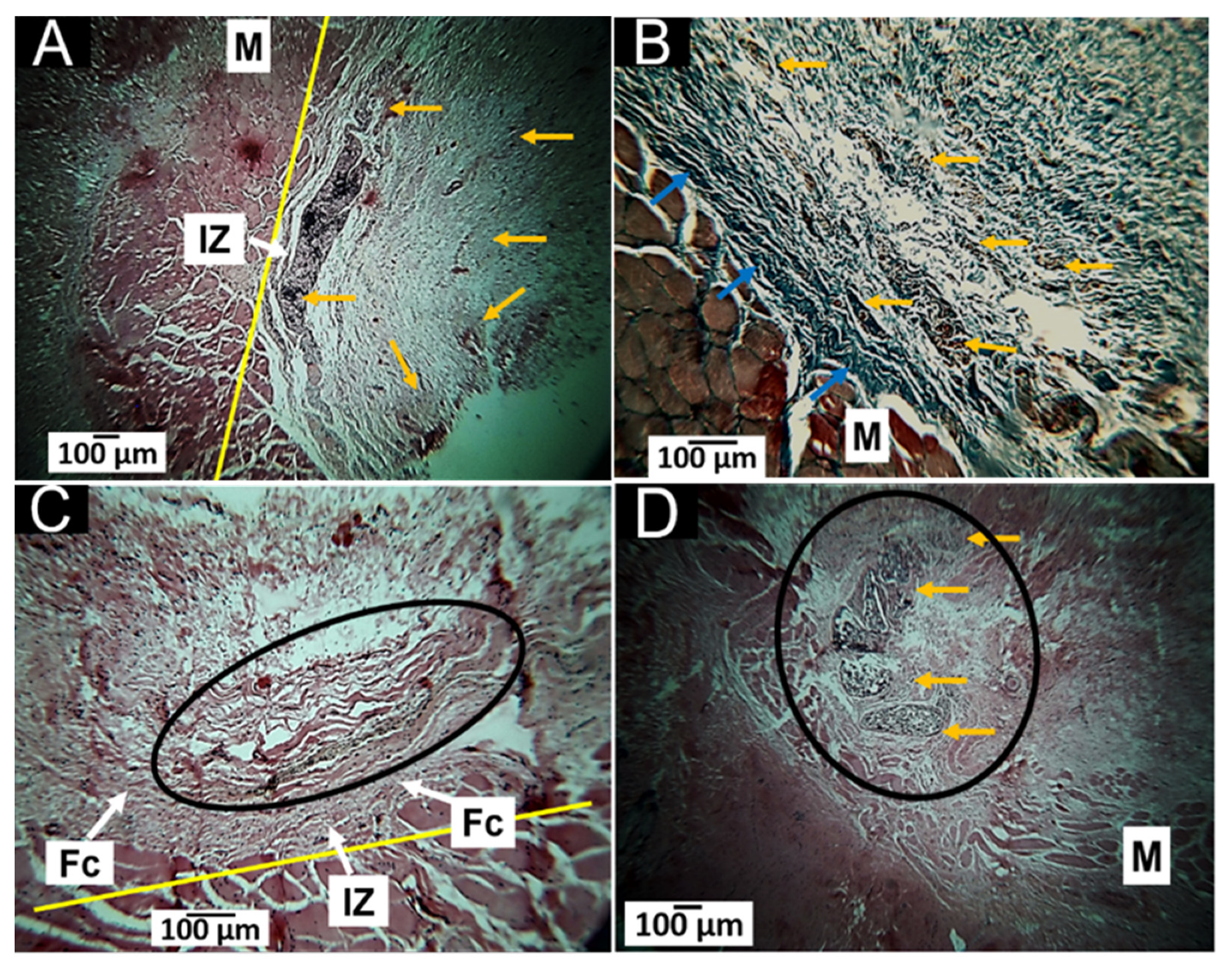
3.5.4. Histology Results of T3 (50%G/50%CS)
3.5.5. Histology Results of T4 (75%G/25%CS)
3.5.6. Histology Results of T5 (100%G)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Umesh, M.; Shanmugam, S.; Kikas, T.; Lan Chi, N.T.; Pugazhendhi, A. Progress in Bio-Based Biodegradable Polymer as the Effective Replacement for the Engineering Applicators. J. Clean. Prod. 2022, 362, 132267. [Google Scholar] [CrossRef]
- Osorio, L.L.; Flórez-López, E.; Grande-Tovar, C.D. The Potential of Selected Agri-Food Loss and Waste to Contribute to a Circular Economy: Applications in the Food, Cosmetic and Pharmaceutical Industries. Molecules 2021, 26, 515. [Google Scholar] [CrossRef] [PubMed]
- Sofi, H.S.; Ashraf, R.; Beigh, M.A.; Sheikh, F.A. Scaffolds Fabricated from Natural Polymers/Composites by Electrospinning for Bone Tissue Regeneration. Adv. Exp. Med. Biol. 2018, 1078, 49–78. [Google Scholar] [PubMed]
- Osmani, R.A.M.; Singh, E.; Jadhav, K.; Jadhav, S.; Banerjee, R. 23—Biopolymers and Biocomposites: Nature’s Tools for Wound Healing and Tissue Engineering. In Applications of Advanced Green Materials; Ahmed, S., Ed.; Woodhead Publishing in Materials; Woodhead Publishing: Duxford, UK, 2021; pp. 573–630. ISBN 978-0-12-820484-9. [Google Scholar]
- Pandit, A.; Kumar, R. A Review on Production, Characterization and Application of Bacterial Cellulose and Its Biocomposites. J. Polym. Environ. 2021, 29, 2738–2755. [Google Scholar] [CrossRef]
- Formela, K.; Hejna, A.; Piszczyk, Ł.; Saeb, M.R.; Colom, X. Processing and Structure–Property Relationships of Natural Rubber/Wheat Bran Biocomposites. Cellulose 2016, 23, 3157–3175. [Google Scholar] [CrossRef]
- Hejna, A.; Sulyman, M.; Przybysz, M.; Saeb, M.R.; Klein, M.; Formela, K. On the Correlation of Lignocellulosic Filler Composition with the Performance Properties of Poly (ε-Caprolactone) Based Biocomposites. Waste Biomass Valoriz. 2020, 11, 1467–1479. [Google Scholar] [CrossRef]
- Bilal, M.; Rasheed, T.; Nabeel, F.; Iqbal, H. Bionanocomposites from Biofibers and Biopolymers. In Biofibers and Biopolymers for Biocomposites; Springer: Cham, Switzerland, 2020; pp. 135–157. [Google Scholar]
- Jouyandeh, M.; Vahabi, H.; Rabiee, N.; Rabiee, M.; Bagherzadeh, M.; Saeb, M.R. Green Composites in Bone Tissue Engineering. Emergent Mater. 2022, 5, 603–620. [Google Scholar] [CrossRef]
- Zarski, A.; Bajer, K.; Kapuśniak, J. Review of the Most Important Methods of Improving the Processing Properties of Starch toward Non-Food Applications. Polymers 2021, 13, 832. [Google Scholar] [CrossRef]
- Hanashiro, I. Fine Structure of Amylose. In Starch; Springer: Tokyo, Japan, 2015; pp. 41–60. [Google Scholar]
- Kong, X. Fine Structure of Amylose and Amylopectin. In Starch Structure, Functionality and Application in Foods; Springer: Singapore, 2020; pp. 29–39. [Google Scholar]
- Vieira, M.G.A.; da Silva, M.A.; dos Santos, L.O.; Beppu, M.M. Natural-Based Plasticizers and Biopolymer Films: A Review. Eur. Polym. J. 2011, 47, 254–263. [Google Scholar] [CrossRef]
- Sarder, R.; Piner, E.; Rios, D.C.; Chacon, L.; Artner, M.A.; Barrios, N.; Argyropoulos, D. Copolymers of Starch, a Sustainable Template for Biomedical Applications: A Review. Carbohydr. Polym. 2022, 278, 118973. [Google Scholar] [CrossRef]
- Quintanilla de Stéfano, J.C.; Abundis-Correa, V.; Herrera-Flores, S.D.; Alvarez, A.J. PH-Sensitive Starch-Based Hydrogels: Synthesis and Effect of Molecular Components on Drug Release Behavior. Polymers 2020, 12, 1974. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Zi, Y.; Lei, J.; Mo, X.; Shao, Z.; Wu, Y.; Tian, Y.; Li, D.; Mu, C. PH-Responsive Nanoparticles Based on Cholesterol/Imidazole Modified Oxidized-Starch for Targeted Anticancer Drug Delivery. Carbohydr. Polym. 2020, 233, 115858. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Liang, Z.; Yang, L.; Du, W.; Yu, T.; Tang, H.; Li, C.; Qiu, H. The Role of Natural Polymers in Bone Tissue Engineering. J. Control. Release 2021, 338, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Ghany, N.A.; Aziz, M.S.A.; Abdel-Aziz, M.M.; Mahmoud, Z. Antimicrobial and Swelling Behaviors of Novel Biodegradable Corn Starch Grafted/Poly (4-Acrylamidobenzoic Acid) Copolymers. Int. J. Biol. Macromol. 2019, 134, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.-F.; Zhang, X.-Q.; Zhang, X.-Y.; Yang, B.; Wang, K.; Wang, S.-Q.; Yuan, J.-Y.; Tao, L.; Wei, Y. Synthesis of Starch-Based Amphiphilic Fluorescent Nanoparticles and Their Application in Biological Imaging. J. Nanosci. Nanotechnol. 2018, 18, 2345–2351. [Google Scholar] [CrossRef]
- Shahriarpanah, S.; Nourmohammadi, J.; Amoabediny, G. Fabrication and Characterization of Carboxylated Starch-Chitosan Bioactive Scaffold for Bone Regeneration. Int. J. Biol. Macromol. 2016, 93, 1069–1078. [Google Scholar] [CrossRef]
- Leonor, I.B.; Rodrigues, M.T.; Gomes, M.E.; Reis, R.L. In Situ Functionalization of Wet-spun Fibre Meshes for Bone Tissue Engineering. J. Tissue Eng. Regen. Med. 2011, 5, 104–111. [Google Scholar] [CrossRef]
- Liu, D.; Nikoo, M.; Boran, G.; Zhou, P.; Regenstein, J.M. Collagen and Gelatin. Annu. Rev. Food Sci. Technol. 2015, 6, 527–557. [Google Scholar] [CrossRef]
- Lv, L.-C.; Huang, Q.-Y.; Ding, W.; Xiao, X.-H.; Zhang, H.-Y.; Xiong, L.-X. Fish Gelatin: The Novel Potential Applications. J. Funct. Foods 2019, 63, 103581. [Google Scholar] [CrossRef]
- Baziwane, D.; He, Q. Gelatin: The Paramount Food Additive. Food Rev. Int. 2003, 19, 423–435. [Google Scholar] [CrossRef]
- Djagny, K.B.; Wang, Z.; Xu, S. Gelatin: A Valuable Protein for Food and Pharmaceutical Industries. Crit. Rev. Food Sci. Nutr. 2001, 41, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Wang, H.; Zhang, L.; Li, Y.; Wei, S. In Situ Synthesis and in Vitro Biocompatibility of Needle-like Nano-Hydroxyapatite in Agar–Gelatin Co-Hydrogel. Mater. Lett. 2013, 104, 8–12. [Google Scholar] [CrossRef]
- Wang, C.-Y.; Kuo, Z.-K.; Hsieh, M.-K.; Ke, L.-Y.; Chen, C.-C.; Cheng, C.-M.; Lai, P.-L. Cell Migration of Preosteoblast Cells on a Clinical Gelatin Sponge for 3D Bone Tissue Engineering. Biomed. Mater. 2019, 15, 15005. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Boerman, O.C.; Sariibrahimoglu, K.; Li, Y.; Jansen, J.A.; Leeuwenburgh, S.C.G. Comparison of Micro-vs. Nanostructured Colloidal Gelatin Gels for Sustained Delivery of Osteogenic Proteins: Bone Morphogenetic Protein-2 and Alkaline Phosphatase. Biomaterials 2012, 33, 8695–8703. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuwenhove, I.; Salamon, A.; Adam, S.; Dubruel, P.; Van Vlierberghe, S.; Peters, K. Gelatin- and Starch-Based Hydrogels. Part B: In Vitro Mesenchymal Stem Cell Behavior on the Hydrogels. Carbohydr. Polym. 2017, 161, 295–305. [Google Scholar] [CrossRef] [PubMed]
- Bombin, A.D.J.; Dunne, N.J.; McCarthy, H.O. Electrospinning of Natural Polymers for the Production of Nanofibres for Wound Healing Applications. Mater. Sci. Eng. C 2020, 114, 110994. [Google Scholar] [CrossRef] [PubMed]
- Ye, S.; Jiang, L.; Su, C.; Zhu, Z.; Wen, Y.; Shao, W. Development of Gelatin/Bacterial Cellulose Composite Sponges as Potential Natural Wound Dressings. Int. J. Biol. Macromol. 2019, 133, 148–155. [Google Scholar] [CrossRef]
- de Paula de Lima Lima, T.; Passos, M.F. Skin Wounds, the Healing Process, and Hydrogel-Based Wound Dressings: A Short Review. J. Biomater. Sci. Polym. Ed. 2021, 32, 1910–1925. [Google Scholar] [CrossRef]
- Sakthiguru, N.; Sithique, M.A. Fabrication of Bioinspired Chitosan/Gelatin/Allantoin Biocomposite Film for Wound Dressing Application. Int. J. Biol. Macromol. 2020, 152, 873–883. [Google Scholar] [CrossRef]
- Adeli, H.; Khorasani, M.T.; Parvazinia, M. Wound Dressing Based on Electrospun PVA/Chitosan/Starch Nanofibrous Mats: Fabrication, Antibacterial and Cytocompatibility Evaluation and in Vitro Healing Assay. Int. J. Biol. Macromol. 2019, 122, 238–254. [Google Scholar] [CrossRef]
- Zoran, L.; Marija, B.; Radomir, M.; Stevo, M.; Marko, M.; Igor, D. Comparison of Resorbable Membranes for Guided Bone Regeneration of Human and Bovine Origin. Acta Vet. Brno. 2014, 64, 477–492. [Google Scholar] [CrossRef]
- Castro, J.I.; Navia-Porras, D.P.; Arbeláez Cortés, J.A.; Mina Hernández, J.H.; Grande-Tovar, C.D. Synthesis, Characterization, and Optimization Studies of Starch/Chicken Gelatin Composites for Food-Packaging Applications. Molecules 2022, 27, 2264. [Google Scholar] [CrossRef] [PubMed]
- Podshivalov, A.; Zakharova, M.; Glazacheva, E.; Uspenskaya, M. Gelatin/Potato Starch Edible Biocomposite Films: Correlation between Morphology and Physical Properties. Carbohydr. Polym. 2017, 157, 1162–1172. [Google Scholar] [CrossRef] [PubMed]
- Biswal, D.R.; Singh, R.P. Characterisation of Carboxymethyl Cellulose and Polyacrylamide Graft Copolymer. Carbohydr. Polym. 2004, 57, 379–387. [Google Scholar] [CrossRef]
- Tongdeesoontorn, W.; Mauer, L.J.; Wongruong, S.; Sriburi, P.; Rachtanapun, P. Effect of Carboxymethyl Cellulose Concentration on Physical Properties of Biodegradable Cassava Starch-Based Films. Chem. Cent. J. 2011, 5, 6. [Google Scholar] [CrossRef]
- Hanani, Z.N.; Roos, Y.; Kerry, J. Fourier Transform Infrared (FTIR) Spectroscopic Analysis of Biodegradable Gelatin Films Immersed in Water. In Proceedings of the 11th International Congress on Engineering and Food, ICEF11, Athens, Greece, 22–26 May 2011. [Google Scholar]
- Ahmadi, A.; Ahmadi, P.; Ehsani, A. Development of an Active Packaging System Containing Zinc Oxide Nanoparticles for the Extension of Chicken Fillet Shelf Life. Food Sci. Nutr. 2020, 8, 5461–5473. [Google Scholar] [CrossRef]
- Bertoft, E. Understanding Starch Structure: Recent Progress. Agronomy 2017, 7, 56. [Google Scholar] [CrossRef]
- Walker, M. Investigating the Colloidal Properties of Drum-Dried Wheat Starches in Low-Fat Oil-In-Water Emulsions. Master’s Thesis, The University of Guelph, Guelph, ON, Canada, 2021. [Google Scholar]
- Schick, C. Differential Scanning Calorimetry (DSC) of Semicrystalline Polymers. Anal. Bioanal. Chem. 2009, 395, 1589–1611. [Google Scholar] [CrossRef]
- Jenkins, P.J.; Donald, A.M. Gelatinisation of Starch: A Combined SAXS/WAXS/DSC and SANS Study. Carbohydr. Res. 1998, 308, 133–147. [Google Scholar] [CrossRef]
- Fuentes, C.; Kang, I.; Lee, J.; Song, D.; Sjöö, M.; Choi, J.; Lee, S.; Nilsson, L. Fractionation and Characterization of Starch Granules Using Field-Flow Fractionation (FFF) and Differential Scanning Calorimetry (DSC). Anal. Bioanal. Chem. 2019, 411, 3665–3674. [Google Scholar] [CrossRef] [Green Version]
- Andrade, M.M.P.; De Oliveira, C.S.; Colman, T.A.D.; Da Costa, F.J.O.G.; Schnitzler, E. Effects of Heat-Moisture Treatment on Organic Cassava Starch: Thermal, Rheological and Structural Study. J. Therm. Anal. Calorim. 2014, 115, 2115–2122. [Google Scholar] [CrossRef]
- Cooke, D.; Gidley, M.J. Loss of Crystalline and Molecular Order during Starch Gelatinisation: Origin of the Enthalpic Transition. Carbohydr. Res. 1992, 227, 103–112. [Google Scholar] [CrossRef]
- Wang, L.Z.; Liu, L.; Holmes, J.; Kerry, J.F.; Kerry, J.P. Assessment of Film-forming Potential and Properties of Protein and Polysaccharide-based Biopolymer Films. Int. J. Food Sci. Technol. 2007, 42, 1128–1138. [Google Scholar] [CrossRef]
- Loo, C.P.Y.; Sarbon, N.M. Chicken Skin Gelatin Films with Tapioca Starch. Food Biosci. 2020, 35, 100589. [Google Scholar] [CrossRef]
- Mendes, J.F.; Paschoalin, R.T.; Carmona, V.B.; Neto, A.R.S.; Marques, A.C.P.; Marconcini, J.M.; Mattoso, L.H.C.; Medeiros, E.S.; Oliveira, J.E. Biodegradable Polymer Blends Based on Corn Starch and Thermoplastic Chitosan Processed by Extrusion. Carbohydr. Polym. 2016, 137, 452–458. [Google Scholar] [CrossRef]
- Moreno, O.; Díaz, R.; Atarés, L.; Chiralt, A. Influence of the Processing Method and Antimicrobial Agents on Properties of Starch-gelatin Biodegradable Films. Polym. Int. 2016, 65, 905–914. [Google Scholar] [CrossRef]
- Tongdeesoontorn, W.; Mauer, L.J.; Wongruong, S.; Sriburi, P.; Rachtanapun, P. Mechanical and Physical Properties of Cassava Starch-Gelatin Composite Films. Int. J. Polym. Mater. 2012, 61, 778–792. [Google Scholar] [CrossRef]
- Lee, J.H.; Yi, G.S.; Lee, J.W.; Kim, D.J. Physicochemical Characterization of Porcine Bone-Derived Grafting Material and Comparison with Bovine Xenografts for Dental Applications. J. Periodontal Implant Sci. 2017, 47, 388–401. [Google Scholar] [CrossRef]
- Naguleswaran, S.; Li, J.; Vasanthan, T.; Bressler, D.; Hoover, R. Amylolysis of Large and Small Granules of Native Triticale, Wheat and Corn Starches Using a Mixture of α-Amylase and Glucoamylase. Carbohydr. Polym. 2012, 88, 864–874. [Google Scholar] [CrossRef]
- Cano, A.; Jiménez, A.; Cháfer, M.; Gónzalez, C.; Chiralt, A. Effect of Amylose: Amylopectin Ratio and Rice Bran Addition on Starch Films Properties. Carbohydr. Polym. 2014, 111, 543–555. [Google Scholar] [CrossRef] [Green Version]
- Becerra, J.; Rodriguez, M.; Leal, D.; Noris-Suarez, K.; Gonzalez, G. Chitosan-Collagen-Hydroxyapatite Membranes for Tissue Engineering. J. Mater. Sci. Mater. Med. 2022, 33, 18. [Google Scholar] [CrossRef] [PubMed]
- Mosleh, Y.; de Zeeuw, W.; Nijemeisland, M.; Bijleveld, J.C.; van Duin, P.; Poulis, J.A. The Structure–Property Correlations in Dry Gelatin Adhesive Films. Adv. Eng. Mater. 2021, 23, 2000716. [Google Scholar] [CrossRef]
- Valencia, G.A.; Luciano, C.G.; Lourenço, R.V.; Bittante, A.M.Q.B.; do Amaral Sobral, P.J. Morphological and Physical Properties of Nano-Biocomposite Films Based on Collagen Loaded with Laponite®. Food Packag. Shelf Life 2019, 19, 24–30. [Google Scholar] [CrossRef]
- Andonegi, M.; Peñalba, M.; de la Caba, K.; Guerrero, P. ZnO Nanoparticle-Incorporated Native Collagen Films with Electro-Conductive Properties. Mater. Sci. Eng. C 2020, 108, 110394. [Google Scholar] [CrossRef]
- Qamruzzaman, M.; Ahmed, F.; Mondal, M.I.H. An Overview on Starch-Based Sustainable Hydrogels: Potential Applications and Aspects. J. Polym. Environ. 2022, 30, 19–50. [Google Scholar] [CrossRef]
- Araújo, M.A.; Cunha, A.M.; Mota, M. Enzymatic Degradation of Starch-Based Thermoplastic Compounds Used in Protheses: Identification of the Degradation Products in Solution. Biomaterials 2004, 25, 2687–2693. [Google Scholar] [CrossRef]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign Body Reaction to Biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef]
- Van Putten, S.M.; Ploeger, D.T.A.; Popa, E.R.; Bank, R.A. Macrophage Phenotypes in the Collagen-Induced Foreign Body Reaction in Rats. Acta Biomater. 2013, 9, 6502–6510. [Google Scholar] [CrossRef]
- Luttikhuizen, D.T.; Harmsen, M.C.; Van Luyn, M.J.A. Cellular and Molecular Dynamics in the Foreign Body Reaction. Tissue Eng. 2006, 12, 1955–1970. [Google Scholar] [CrossRef]
- Du, W.; Zhang, Z.; Gao, W.; Li, Z. Porous Organosilicone Modified Gelatin Hybrids with Controllable and Homogeneous in Vitro Degradation Behaviors for Potential Application as Skin Regeneration Scaffold. Polym. Int. 2019, 68, 1411–1419. [Google Scholar] [CrossRef]
- Ozeki, M.; Tabata, Y. In Vivo Degradability of Hydrogels Prepared from Different Gelatins by Various Cross-Linking Methods. J. Biomater. Sci. Polym. Ed. 2005, 16, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Blaine, G. Absorbable Gelatin Sponge in Experimental Surgery. Lancet 1951, 2, 427–429. [Google Scholar] [CrossRef]
- Cegielski, M.; Izykowska, I.; Podhorska-Okolow, M.; Zabel, M.; Dziegiel, P. Development of Foreign Body Giant Cells in Response to Implantation of Spongostan® as a Scaffold for Cartilage Tissue Engineering. In Vivo 2008, 22, 203–206. [Google Scholar] [PubMed]
- Ye, Q.; Harmsen, M.C.; Ren, Y.; Bank, R.A. The Role of Collagen Receptors Endo180 and DDR-2 in the Foreign Body Reaction against Non-Crosslinked Collagen and Gelatin. Biomaterials 2011, 32, 1339–1350. [Google Scholar] [CrossRef] [PubMed]
- Samperio, G.; Garay, C.; Guitrón, A.; Vega, J. Modelo Para La Valoración Cuantitativa de La Cicatrización. Estudio Piloto Con Miel de Abeja. Cir. Gen. 2015, 27, 114–119. [Google Scholar]
- Valencia-Llano, C.H.; López-Tenorio, D.; Grande-Tovar, C.D. Biocompatibility Assessment of Two Commercial Bone Xenografts by In Vitro and In Vivo Methods. Polymers 2022, 14, 2672. [Google Scholar] [CrossRef]





| Formulation | Gelatin | Cassava Starch |
|---|---|---|
| T1 | 0 | 100 |
| T2 | 25 | 75 |
| T3 | 50 | 50 |
| T4 | 75 | 25 |
| T5 | 100 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valencia-Llano, C.H.; Castro, J.I.; Saavedra, M.; Zapata, P.A.; Navia-Porras, D.P.; Flórez-López, E.; Caicedo, C.; Calambas, H.L.; Grande-Tovar, C.D. Histological Evaluation of Cassava Starch/Chicken Gelatin Membranes. Polymers 2022, 14, 3849. https://doi.org/10.3390/polym14183849
Valencia-Llano CH, Castro JI, Saavedra M, Zapata PA, Navia-Porras DP, Flórez-López E, Caicedo C, Calambas HL, Grande-Tovar CD. Histological Evaluation of Cassava Starch/Chicken Gelatin Membranes. Polymers. 2022; 14(18):3849. https://doi.org/10.3390/polym14183849
Chicago/Turabian StyleValencia-Llano, Carlos Humberto, Jorge Iván Castro, Marcela Saavedra, Paula A. Zapata, Diana Paola Navia-Porras, Edwin Flórez-López, Carolina Caicedo, Heidy Lorena Calambas, and Carlos David Grande-Tovar. 2022. "Histological Evaluation of Cassava Starch/Chicken Gelatin Membranes" Polymers 14, no. 18: 3849. https://doi.org/10.3390/polym14183849
APA StyleValencia-Llano, C. H., Castro, J. I., Saavedra, M., Zapata, P. A., Navia-Porras, D. P., Flórez-López, E., Caicedo, C., Calambas, H. L., & Grande-Tovar, C. D. (2022). Histological Evaluation of Cassava Starch/Chicken Gelatin Membranes. Polymers, 14(18), 3849. https://doi.org/10.3390/polym14183849








