Effects of Litsea cubeba Essential Oil Incorporated into Denture Soft Lining Materials
Abstract
1. Introduction
2. Materials and Methods
2.1. Antimicrobial Additives
2.2. Soft Lining Material
2.3. Microbial Culture
2.4. Antimicrobial Activity of LCEO
2.5. Antimicrobial Activity of LCEO Incorporated into Soft Lining Materials
2.6. Cytotoxicity Test
2.7. Shore AO Hardness Testing
2.8. Statistical Analysis
3. Results
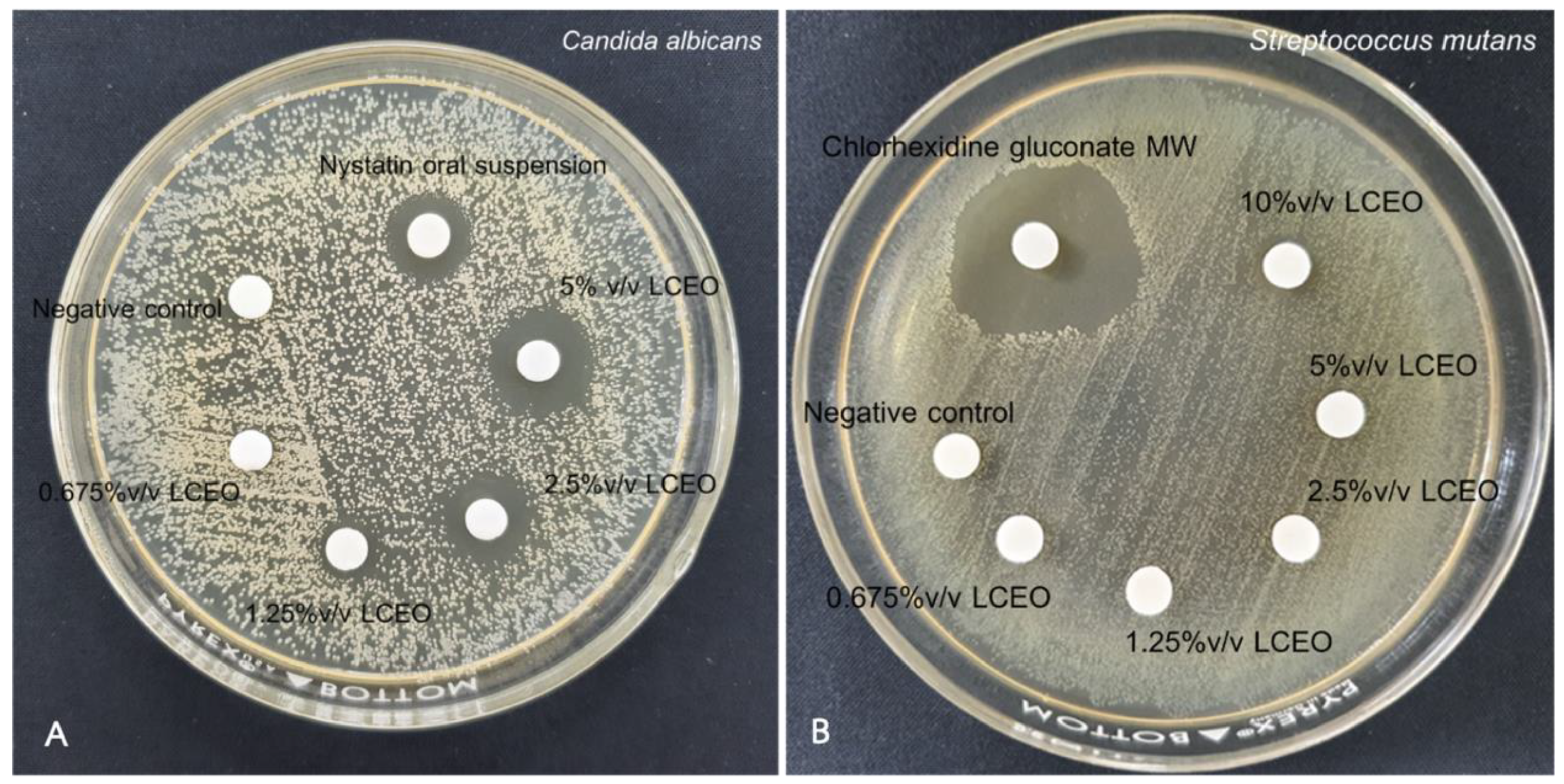
3.1. Antimicrobial Activity of LCEO towards C. albicans and S. mutans
3.2. Antimicrobial Activity of LCEO Incorporated into Different Soft Lining Materials against C. albicans and S. mutans
3.3. Cell Viability of HGF Cell Line
3.4. Surface Hardness of Soft Lining Materials
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Garcia, L.T.; Jones, J.D. Soft liners. Dent. Clin. N. Am. 2004, 48, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Budtz-Jörgensen, E. Clinical aspects of Candida infection in denture wearers. J. Am. Dent. Assoc. 1978, 96, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Baena-Monroy, T.; Moreno-Maldonado, V.; Franco-Martínez, F.; Aldape-Barrios, B.; Quindós, G.; Sánchez-Vargas, L.O. Candida albicans, Staphylococcus aureus and Streptococcus mutans colonization in patients wearing dental prosthesis. Med. Oral Patol. Oral Cir. Bucal 2005, 10 (Suppl. S1), E27–E39. [Google Scholar] [PubMed]
- Iqbal, Z.; Zafar, M.S. Role of antifungal medicaments added to tissue conditioners: A systematic review. J. Prosthodont. Res. 2016, 60, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.-M.; Hwang, J.-K. Effects of methanolic extract and fractions from Litsea cubeba bark on the production of inflammatory mediators in RAW264.7 cells. Fitoterapia 2004, 75, 141–148. [Google Scholar] [CrossRef]
- Ho, C.-L.; Jie-Ping, O.; Liu, Y.-C.; Hung, C.-P.; Tsai, M.-C.; Liao, P.-C.; Wang, E.I.-C.; Chen, Y.-L.; Su, Y.-C. Compositions and in vitro Anticancer activities of the Leaf and Fruit Oils of Litsea cubeba from Taiwan. Nat. Prod. Commun. 2010, 5, 1934578X1000500425. [Google Scholar] [CrossRef]
- Wang, H.; Liu, Y. Chemical composition and antibacterial activity of essential oils from different parts of Litsea cubeba. Chem. Biodivers. 2010, 7, 229–235. [Google Scholar] [CrossRef]
- Hammid, S.A.; Ahmad, F. Chemotype of Litsea cubeba Essential Oil and Its Bioactivity. Nat. Prod. Commun. 2015, 10, 1301–1304. [Google Scholar] [CrossRef]
- Thielmann, J.; Muranyi, P. Review on the chemical composition of Litsea cubeba essential oils and the bioactivity of its major constituents citral and limonene. J. Essent. Oil Res. 2019, 31, 361–378. [Google Scholar] [CrossRef]
- Al-Nemi, R.; Makki, A.A.; Sawalha, K.; Hajjar, D.; Jaremko, M. Untargeted Metabolomic Profiling and Antioxidant Capacities of Different Solvent Crude Extracts of Ephedra foeminea. Metabolites 2022, 12, 451. [Google Scholar] [CrossRef]
- Khan, A.A.; Atiya, A.; Akhtar, S.; Yadav, Y.; Qureshi, K.A.; Jaremko, M.; Mahmood, S. Optimization of a Cefuroxime Axetil-Loaded Liquid Self-Nanoemulsifying Drug Delivery System: Enhanced Solubility, Dissolution and Caco2 Cell Uptake. Pharmaceutics 2022, 14, 772. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.A.; Henttu, P.; Parker, M.G.; Sumpter, J.P. The estrogenic activity of phthalate esters in vitro. Environ. Health Perspect. 1997, 105, 802–811. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.W.; Sutow, E.J.; Hall, G.C.; Tobin, W.M.; Graham, B.S. Dental soft polymers: Plasticizer composition and leachability. Dent. Mater. 1988, 4, 1–7. [Google Scholar] [CrossRef]
- ISO 10993-5; Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity. International Organization for Standardization: Geneva, Switzerland, 2009.
- ISO 10993-12; Biological Evaluation of Medical Devices—Part 12: Sample Preparation and Reference Materials. International Organization for Standardization: Geneva, Switzerland, 2021.
- ISO 10139-1; Dentistry–Soft Lining Materials for Removable Dentures–Part 1: Materials for Short-Term Use. International Organization for Standardization: Geneva, Switzerland, 2018.
- Kumpanich, J.; Eiampongpaiboon, T.; Kanchanavasita, W.; Chitmongkolsuk, S.; Puripattanavong, J. Effect of Piper betle extract on anti-candidal activity, gelation time, and surface hardness of a short-term soft lining material. Dent. Mater. J. 2020, 39, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Onawunmi, G.O. Evaluation of the antimicrobial activity of citral. Lett. Appl. Microbiol. 1989, 9, 105–108. [Google Scholar] [CrossRef]
- Leite, M.C.A.; de Brito Bezerra, A.P.; de Sousa, J.P.; Guerra, F.Q.S.; de Oliveira Lima, E. Evaluation of Antifungal Activity and Mechanism of Action of Citral against Candida albicans. Evid.-Based Complement. Altern. Med. 2014, 2014, 378280. [Google Scholar] [CrossRef]
- Saikia, A.K.; Chetia, D.; D’Arrigo, M.; Smeriglio, A.; Strano, T.; Ruberto, G. Screening of fruit and leaf essential oils of Litsea cubeba Pers. from north-east India–chemical composition and antimicrobial activity. J. Essent. Oil Res. 2013, 25, 330–338. [Google Scholar] [CrossRef]
- Yang, T.-S.; Liou, M.-L.; Hu, T.-F.; Peng, C.-W.; Liu, T.-T. Antimicrobial activity of the essential oil of Litsea cubeba on cariogenic bacteria. J. Essent. Oil Res. 2013, 25, 120–128. [Google Scholar] [CrossRef]
- Catalán, A.; Pacheco, J.G.; Martínez, A.; Mondaca, M.A. In vitro and in vivo activity of melaleuca alternifolia mixed with tissue conditioner on Candida albicans. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 105, 327–332. [Google Scholar] [CrossRef]
- Chow, C.K.; Matear, D.W.; Lawrence, H.P. Efficacy of antifungal agents in tissue conditioners in treating candidiasis. Gerodontology 2008, 16, 110–118. [Google Scholar] [CrossRef]
- Luo, M.; Jiang, L.-K.; Zou, G.-L. Acute and Genetic Toxicity of Essential Oil Extracted from Litsea cubeba (Lour.) Pers. J. Food Prot. 2005, 68, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.X.; Werner, J.; Kirsch, T.; Zuckerman, J.; Virk, M.S. Cytotoxicity evaluation of chlorhexidine gluconate on human fibroblasts, myoblasts, and osteoblasts. J. Bone Jt. Infect. 2018, 3, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Audus, K.L. Cytotoxic effects of chlorhexidine and nystatin on cultured hamster buccal epithelial cells. Int. J. Pharm. 1994, 101, 121–126. [Google Scholar] [CrossRef]
- Seal, S.; Chatterjee, P.; Bhattacharya, S.; Pal, D.; Dasgupta, S.; Kundu, R.; Mukherjee, S.; Bhattacharya, S.; Bhuyan, M.; Bhattacharyya, P.R.; et al. Vapor of Volatile Oils from Litsea cubeba Seed Induces Apoptosis and Causes Cell Cycle Arrest in Lung Cancer Cells. PLoS ONE 2012, 7, e47014. [Google Scholar] [CrossRef]
- Senichev, V.Y.; Tereshatov, V.V. Theories of Compatibility. In Handbook of Plasticizers, 3rd ed.; Wypych, G., Ed.; ChemTec Publishing: Toronto, ON, Canada, 2017; pp. 121–148. [Google Scholar]
- Hansen, C.M. Hansen Solubility Parameters: A User’s Handbook, 2nd ed.; CRC Press Inc.: Boca Raton, FL, USA, 2007. [Google Scholar]
- Parker, S.; Braden, M. Formulation of tissue conditioners. Biomaterials 1990, 11, 579–584. [Google Scholar] [CrossRef]
- Boersma, A. Mobility and solubility of antioxidants and oxygen in glassy polymers. I. Concentration and temperature dependence of antioxidant sorption. J. Appl. Polym. Sci. 2003, 89, 2163–2178. [Google Scholar] [CrossRef]
- Leelaphiwat, P.; Auras, R.A.; Burgess, G.J.; Harte, J.B.; Chonhenchob, V. Preliminary quantification of the permeability, solubility and diffusion coefficients of major aroma compounds present in herbs through various plastic packaging materials. J. Sci. Food Agric. 2018, 98, 1545–1553. [Google Scholar] [CrossRef]
- Hong, G.; Maeda, T.; Li, Y.; Sadamori, S.; Hamada, T.; Murata, H. Effect of PMMA polymer on the dynamic viscoelasticity and plasticizer leachability of PEMA-based tissue conditioners. Dent. Mater. J. 2010, 29, 374–380. [Google Scholar] [CrossRef][Green Version]



| Product | Powder Compositions | Liquid Compositions | P/L |
|---|---|---|---|
| GC Soft liner (GC DENTAL PRODUCTS CORP., Japan) | Poly(ethyl methacrylate), PEMA (100%) | Butyl phthalyl butyl glycolate, BPBG (80.9%) Dibutyl phthalate, DBP (4.3%) Ethanol, EtOH (14.8%) | 2.2 g/1.8 g |
| Coe comfort (GC DENTAL PRODUCTS CORP, Japan) | Poly(ethyl methacrylate), PEMA (100%) | Benzyl Benzoate, (50–70%) Ethanol (5–10%) Peppermint oil (menthol) (<1%) Butylated hydroxytoluene (<0.5%) | 6 g/5 mL |
| Viscogel (DENTSPLY SIRONA INC., Germany) | Poly(ethyl methacrylate), PEMA (86.2%) Poly(methyl methacrylate), PMMA (13.8%) | Butyl phthalyl butyl glycolate, BPBG (86.9%) Dibutyl phthalate, DBP (8.2%) Ethanol, EtOH (4.9%) | 3 g/2 mL |
| Condition | Candida albicans Mean Inhibition Zone ± SD (mm) |
|---|---|
| Negative control (DMSO) | ND |
| Nystatin oral suspension | 12.74 ± 0.27 |
| 0.675% v/v LCEO | ND |
| 1.25% v/v LCEO | 8.33 ± 0.20 |
| 2.5% v/v LCEO | 10.74 ± 0.70 |
| 5% v/v LCEO | 14.33 ± 0.52 |
| Condition | Streptococcus mutans Mean Inhibition Zone ± SD (mm) |
|---|---|
| Negative control (DMSO) | ND |
| 5% v/v of 2% Chlorhexidine gluconate | 21.15 ± 0.35 |
| 0.675% v/v LCEO | ND |
| 1.25% v/v LCEO | ND |
| 2.5% v/v LCEO | ND |
| 5% v/v LCEO | ND |
| 10% v/v LCEO | 9.56 ± 0.52 |
| Condition | Mean Inhibition Zone (Mean ± SD) | |||||
|---|---|---|---|---|---|---|
| No Additive | 5% v/v LCEO | 10% v/v LCEO | 20% v/v LCEO | 30% v/v LCEO | 30% Nystatin Oral Suspension | |
| GC soft liner | ND | ND | 7.61 ± 0.24 A | 13.19 ± 0.66 B | 22.42 ± 0.97 C | 12.14 ± 0.25 B |
| Viscogel | ND | ND | 12.09 ± 0.57 D | 16.56 ± 0.88 E | 24.68 ± 1.07 F | 11.33 ± 0.31 D |
| Coe comfort | ND | ND | 10.22 ± 0.81 G | 14.07 ± 0.60 H | 22.61 ± 0.52 I | 11.75± 0.37 G,H |
| Condition | Mean Inhibition Zone (Mean ± SD) | |||||
|---|---|---|---|---|---|---|
| No Additive | 5% v/v LCEO | 10% v/v LCEO | 20% v/v LCEO | 30% v/v LCEO | CHX | |
| GC Soft liner | ND | ND | ND | ND | 7.89 ± 0.40 A | 22.90 ± 0.75 B |
| Viscogel | ND | ND | ND | ND | 7.96 ± 0.45 C | 20.06 ± 0.20 D |
| Coe comfort | ND | ND | ND | ND | 8.15 ± 0.25 E | 20.08± 1.67 F |
| Soft Lining Material/ Additives | GC Soft Liner | |
|---|---|---|
| 2 h | 7 days | |
| No additive | 21.72 ± 0.92 A,a | 25.56 ± 1.39 G,b |
| NYS | 16.88 ± 1.38 B,a | 22.44 ± 0.82 G,b |
| CHX | 16.80 ± 0.65 B,a | 24.80 ± 2.08 G,b |
| 5% v/v LCEO | 14.72 ± 1.12 B,a | 22.36 ± 1.79 G,b |
| 10% v/v LCEO | 11.24 ± 1.16 C,a | 18.52 ± 1.89 H,b |
| 20% v/v LCEO | 6.88 ± 0.88 D,a | 13.64 ± 0.75 I,b |
| 30% v/v LCEO | 4.08 ± 0.88 E,a | 8.84 ± 1.81 J,b |
| Soft Lining Material/ Additives | Viscogel | |
|---|---|---|
| 2 h | 7 days | |
| No additive | 37.13 ± 0.81 A,a | 40.20 ± 0.53 G,b |
| NYS | 35.27 ± 0.61 AB,a | 38.67 ± 0.95 GH,b |
| CHX | 35.33 ± 1.10 AB,a | 39.33 ± 1.40 G,b |
| 5% v/v LCEO | 34.67 ± 0.99 AB,a | 37.93 ± 0.83 GH,b |
| 10% v/v LCEO | 32.73 ± 0.64 B,a | 35.87 ± 1.17 H,b |
| 20% v/v LCEO | 29.07 ± 1.33 C,a | 32.53 ± 1.45 I,b |
| 30% v/v LCEO | 22.27 ± 0.99 D,a | 27.93 ± 0.90 J,b |
| Soft lining Material/ Additives | Coe Comfort | |
|---|---|---|
| 2 h | 7 days | |
| No additive | 16.32 ± 0.67 A,a | 22.20 ± 2.32 G,b |
| NYS | 13.88 ± 0.67 B,a | 17.36 ± 0.59 I,b |
| CHX | 16.12 ± 1.74 AB,a | 20.76 ± 0.52 GH,b |
| 5%v/v LCEO | 13.96 ± 1.34 B,a | 19.88 ± 1.15 H,b |
| 10%v/v LCEO | 10.00 ± 0.87 C,a | 15.16 ± 0.38 I,b |
| 20%v/v LCEO | 5.20 ± 1.31 D,a | 9.76 ± 0.62 J,b |
| 30%v/v LCEO | 2.12 ± 0.58 E,a | 5.20 ± 0.71 K,b |
| Materials | Main Composition | Hansen’s Solubility Parameter (δ, MPa1/2) |
|---|---|---|
| GC soft liner powder Coe comfort powder | Poly (ethyl methacrylate) | 20.5 |
| GC soft liner liquid | Butyl phthalyl butyl glycolate (80.9%) | 20.7 |
| Dibutyl phthalate (4.3%) | 19.0, 20.1 | |
| Ethanol (14.8%) | 26.0, 26.5 | |
| Coe comfort liquid | Benzyl Benzoate, (50–70%) | 21.3 |
| Ethanol (5–10%) | 26.0, 26.5 | |
| Peppermint oil (menthol) (<1%) | 20.2 | |
| Butylated hydroxytoluene (<0.5%) | 16.7 | |
| Viscogel powder | Poly (ethyl methacrylate) (86.2%) | 20.5 |
| Poly (methyl methacrylate) (13.8%) | 20.2, 21.5 | |
| Viscogel liquid | Butyl benzyl phthalate (87.3%) | 22.4, 22.3 |
| Dibutyl phthalate (4.5%) | 19.0, 20.1 | |
| Ethanol (4.9%) | 26.0, 26.5 | |
| LCEO | Citral | 18.6 |
| Nystatin oral suspension | Nystatin | ND |
| Water | 47.8 | |
| Sucrose | 36.3 | |
| Chlorhexidine gluconate | Chlorhexidine gluconate salt | ND |
| Water | 47.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Songsang, N.; Anunmana, C.; Pudla, M.; Eiampongpaiboon, T. Effects of Litsea cubeba Essential Oil Incorporated into Denture Soft Lining Materials. Polymers 2022, 14, 3261. https://doi.org/10.3390/polym14163261
Songsang N, Anunmana C, Pudla M, Eiampongpaiboon T. Effects of Litsea cubeba Essential Oil Incorporated into Denture Soft Lining Materials. Polymers. 2022; 14(16):3261. https://doi.org/10.3390/polym14163261
Chicago/Turabian StyleSongsang, Nichakorn, Chuchai Anunmana, Matsayapan Pudla, and Trinuch Eiampongpaiboon. 2022. "Effects of Litsea cubeba Essential Oil Incorporated into Denture Soft Lining Materials" Polymers 14, no. 16: 3261. https://doi.org/10.3390/polym14163261
APA StyleSongsang, N., Anunmana, C., Pudla, M., & Eiampongpaiboon, T. (2022). Effects of Litsea cubeba Essential Oil Incorporated into Denture Soft Lining Materials. Polymers, 14(16), 3261. https://doi.org/10.3390/polym14163261







