Cell Secretome Strategies for Controlled Drug Delivery and Wound-Healing Applications
Abstract
1. Introduction
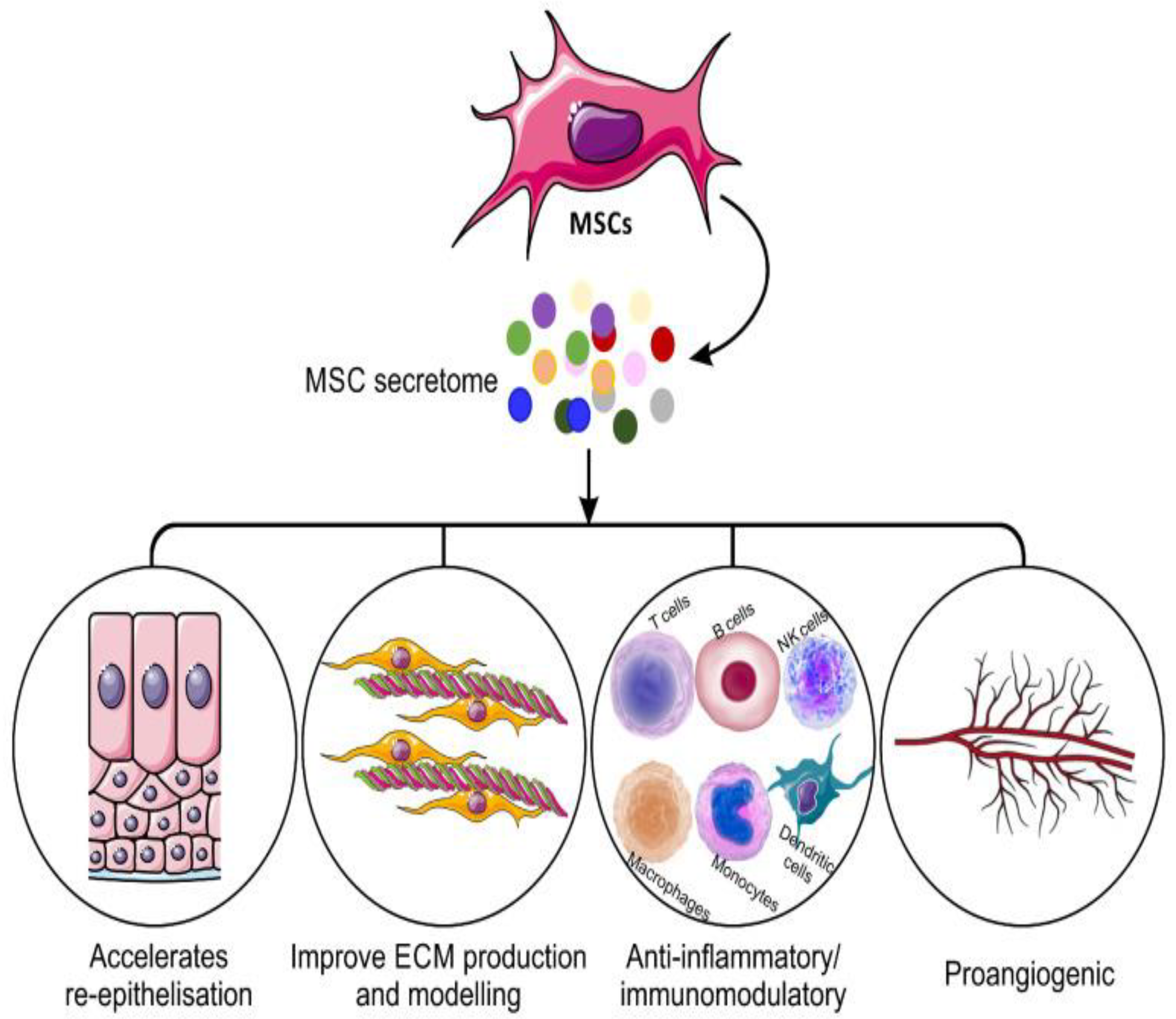
2. Secretome
2.1. Secretome Composition
2.2. Advantage of Secretome over Cell Therapy
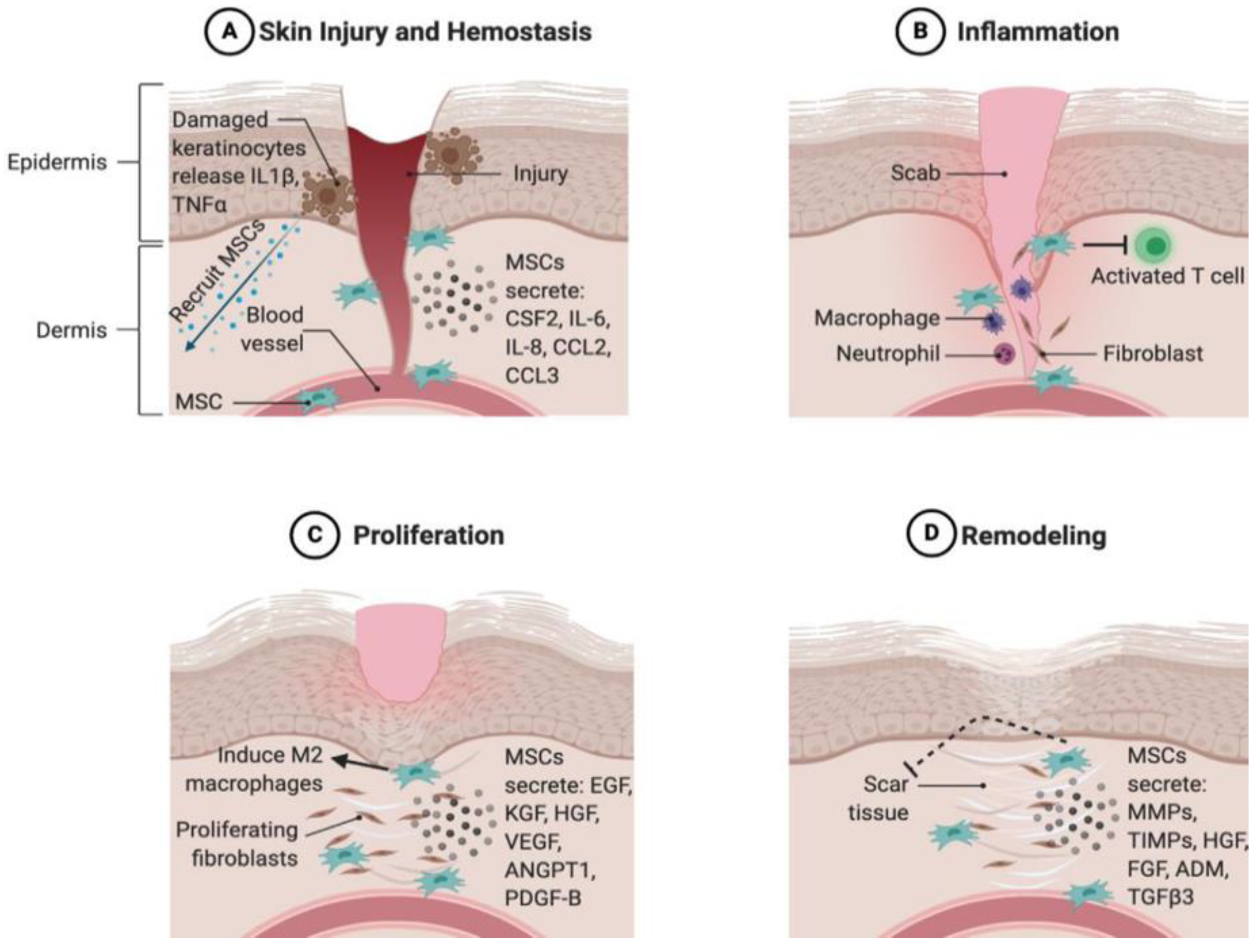
2.3. The Role of the Secretome in Different Stages of Wound Healing
3. Secretome Applications in Wound Healing
4. Secretome Delivery in Wound Healing
5. Structural Formulation Using Biomaterials with Secretome for Wound-Healing Applications
5.1. MSC Soluble Secretions and Their Combination with Biomaterials for Application in Different Wounds
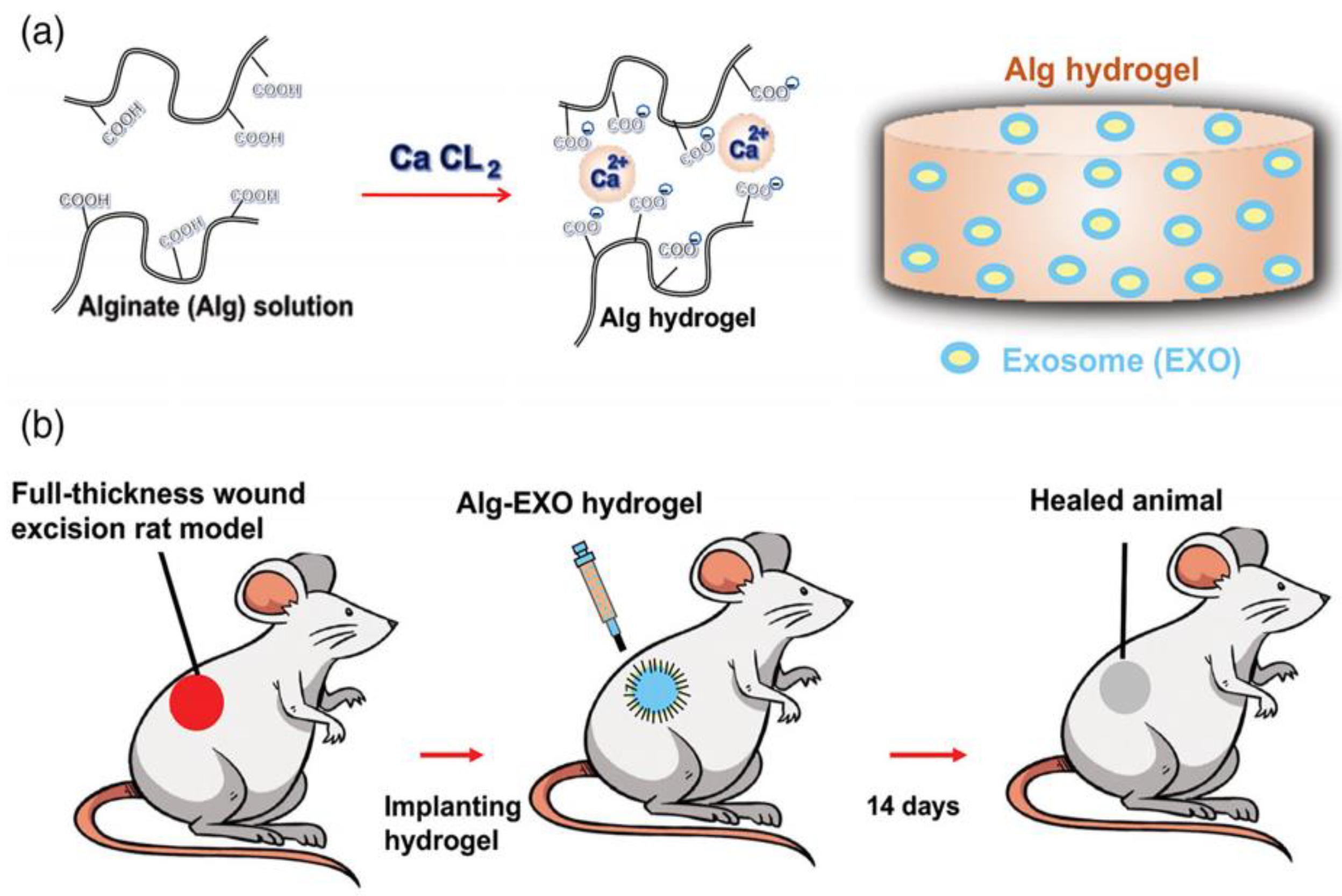
5.2. MSC EVs and Their Combination with Biomaterials for Application in Different Wounds
5.3. Secretome in 3D Bioprinting
6. Conclusions
7. Future Prospective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Activated phosphatidylinositol 3 kinase/Protein kinase | PI3K/Akt |
| Adipose tissue-derived stem cells | ADSCs |
| Alginate hydrogel-incorporated exosome | Alg-EXO |
| Angiopoietin | Ang |
| Basic fibroblast growth factor | bFGF |
| Beta-tricalcium phosphate | β-TCP |
| Bone marrow mesenchymal stem cells | BM-MSCs |
| Chemokine | CXCL5 |
| Conditioned medium from human uterine cervical stem cells | CM-hUCESCs |
| Endothelial growth factor | EGF |
| Extracellular matrix | ECM |
| Extracellular signal regulated kinase 1 | ERK1 |
| Extracellular vesicles | EV |
| Focal adhesion kinase | FAK |
| Gelatin methacrylate | GelMA |
| Good manufacturing practice | GMP |
| Granulocyte-colony stimulating factor | G-CSF |
| Hepatocyte growth factor | HGF |
| Human adipose tissue mesenchymal stem cell | |
| HATMSC | |
| Human bone marrow mesenchymal stem cell | BMSC |
| Human microvascular endothelial cells | HMEC |
| Human umbilical cord perivascular cells | HUCPVCs |
| Human umbilical vascular endothelial cells | HUVECs |
| Human uterine cervical stem cells | hUCESCs |
| Hyaluronic acid | HA |
| Hyperbaric oxygen therapy | HBO2 |
| Interleukins | IL |
| Keratinocyte growth factor | KGF |
| Leukemia inhibitory factor | LIF |
| Matrix metalloproteinase | MMP |
| Mesenchymal stem-cell-conditioned media | MSC-CM |
| Mesenchymal stem cells | MSC |
| Mesenchymal stromal cell secretome-chitosan hydrogel | MSC-Ch |
| Monocyte chemoattractant protein | MCP |
| Multipotent adult progenitor cell-conditioned medium | MAPC-CM |
| Multipotent mesenchymal stromal cell | MMSC |
| Platelet-derived growth factor | PDGF |
| Polyisocyanate | PIC |
| Polylactide-co-glycolide | PLGA |
| Poly-L-lactic acid | PLLA |
| Sickle cell disease | SCD |
| Smooth muscle actin | SMA |
| Synovium mesenchymal stromal cell | SMSC |
| Tissue inhibitors of metalloproteinases | TIMP |
| Transforming growth factor | TGF |
| Tumour necrosis factor-alpha | TNF |
| Umbilical cord mesenchymal stem cells C-derived exosomes | UMSC-Exos |
| Vascular endothelial growth factor | VEGF |
| Wharton’s jelly mesenchymal stem cells | WJ-MSCs |
| Polyethylene glycol | PEG |
References
- Proksch, E.; Brandner, J.M.; Jensen, J.M. The skin: An indispensable barrier. Exp. Dermatol. 2008, 17, 1063–1072. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Dao, H. Physiology, Integument; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Xu, X.; Zhang, H.; Yan, Y.; Wang, J.; Guo, L. Effects of electrical stimulation on skin surface. Acta Mech. Sin. 2021, 37, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Raziyeva, K.; Kim, Y.; Zharkinbekov, Z.; Kassymbek, K.; Jimi, S.; Saparov, A. Immunology of acute and chronic wound healing. Biomolecules 2021, 11, 700. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.; Kosaric, N.; Bonham, C.A.; Gurtner, G.C. Wound healing: A cellular perspective. Physiol. Rev. 2019, 99, 665–706. [Google Scholar] [CrossRef]
- Uzun, M. A review of wound management materials. J. Text. Eng. Fash. Technol. 2018, 4, 00121. [Google Scholar] [CrossRef]
- Okur, M.E.; Karantas, I.D.; Şenyiğit, Z.; Okur, N.Ü.; Siafaka, P.I. Recent trends on wound management: New therapeutic choices based on polymeric carriers. Asian J. Pharm. Sci. 2020, 15, 661–684. [Google Scholar] [CrossRef]
- Ma, H.; Lam, P.K.; Siu, W.S.; Tong, C.S.W.; Lo, K.K.Y.; Koon, C.M.; Wu, X.X.; Li, X.; Cheng, W.; Shum, W.T. Adipose Tissue-Derived Mesenchymal Stem Cells (ADMSCs) and ADMSC-Derived Secretome Expedited Wound Healing in a Rodent Model—A Preliminary Study. Clin. Cosmet. Investig. Dermatol. 2021, 14, 753. [Google Scholar] [CrossRef]
- Wang, P.H.; Huang, B.-S.; Horng, H.-C.; Yeh, C.-C.; Chen, Y.-J. Wound healing. J. Chin. Med. Assoc. 2018, 2, 94–101. [Google Scholar] [CrossRef]
- Rezvani Ghomi, E.; Khalili, S.; Nouri Khorasani, S.; Esmaeely Neisiany, R.; Ramakrishna, S. Wound dressings: Current advances and future directions. J. Appl. Polym. Sci. 2019, 136, 47738. [Google Scholar] [CrossRef]
- Rittié, L. Cellular mechanisms of skin repair in humans and other mammals. J. Cell Commun. Signal. 2016, 10, 103–120. [Google Scholar] [CrossRef]
- Han, G.; Ceilley, R. Chronic wound healing: A review of current management and treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef]
- Xu, Z.; Han, S.; Gu, Z.; Wu, J. Advances and impact of antioxidant hydrogel in chronic wound healing. Adv. Healthc. Mater. 2020, 9, 1901502. [Google Scholar] [CrossRef] [PubMed]
- Berwin Singh, S.; Park, H.; Khang, G.; Lee, D. Hydrogen peroxide-responsive engineered polyoxalate nanoparticles for enhanced wound healing. Macromol. Res. 2018, 26, 40–47. [Google Scholar] [CrossRef]
- Kucharzewski, M.; Rojczyk, E.; Wilemska-Kucharzewska, K.; Wilk, R.; Hudecki, J.; Los, M.J. Novel trends in application of stem cells in skin wound healing. Eur. J. Pharmacol. 2019, 843, 307–315. [Google Scholar] [CrossRef] [PubMed]
- González-González, A.; García-Sánchez, D.; Dotta, M.; Rodríguez-Rey, J.C.; Pérez-Campo, F.M. Mesenchymal stem cells secretome: The cornerstone of cell-free regenerative medicine. World J. Stem Cells 2020, 12, 1529. [Google Scholar] [CrossRef]
- Nourian Dehkordi, A.; Mirahmadi Babaheydari, F.; Chehelgerdi, M.; Raeisi Dehkordi, S. Skin tissue engineering: Wound healing based on stem-cell-based therapeutic strategies. Stem Cell Res. Ther. 2019, 10, 1–20. [Google Scholar] [CrossRef]
- Gruca, D.; Zając, M.; Wróblewski, W.; Borowiecka, M.; Buksak, D. The relation between adipose-derived stem cells and wound healing process-the review. J. Educ. Health Sport 2022, 12, 87–93. [Google Scholar] [CrossRef]
- Vizoso, F.J.; Eiro, N.; Cid, S.; Schneider, J.; Perez-Fernandez, R. Mesenchymal stem cell secretome: Toward cell-free therapeutic strategies in regenerative medicine. Int. J. Mol. Sci. 2017, 18, 1852. [Google Scholar] [CrossRef]
- Mendes-Pinheiro, B.; Marote, A.; Marques, C.R.; Teixeira, F.G.; Ribeiro, J.C.; Salgado, A.J. Applications of the stem cell secretome in regenerative medicine. In Mesenchymal Stem Cells in Human Health and Diseases; Elsevier: Amsterdam, The Netherlands, 2020; pp. 79–114. [Google Scholar]
- Brembilla, N.; Modarressi, A.; Levigne, D.A.; Brioudes, E.; Lanza, F.; Vuagnat, H.; Durual, S.; Marger, L.; Boehncke, W.-H.; Krause, K.-H. Efficacy and safety of a patch containing adipose-derived stem cells for skin wound healing. Results form a comprehensive pre-clinical evaluation program. bioRxiv 2022. [Google Scholar] [CrossRef]
- Ahangar, P.; Mills, S.J.; Cowin, A.J. Mesenchymal stem cell secretome as an emerging cell-free alternative for improving wound repair. Int. J. Mol. Sci. 2020, 21, 7038. [Google Scholar] [CrossRef]
- Pinho, A.G.; Cibrão, J.R.; Silva, N.A.; Monteiro, S.; Salgado, A.J. Cell secretome: Basic insights and therapeutic opportunities for CNS disorders. Pharmaceuticals 2020, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Pokrovskaya, L.A.; Zubareva, E.V.; Nadezhdin, S.V.; Lysenko, A.S.; Litovkina, T.L. Biological activity of mesenchymal stem cells secretome as a basis for cell-free therapeutic approach. Res. Results Pharmacol. 2020, 6, 57–68. [Google Scholar] [CrossRef]
- Mitchell, R.; Mellows, B.; Sheard, J.; Antonioli, M.; Kretz, O.; Chambers, D.; Zeuner, M.-T.; Tomkins, J.E.; Denecke, B.; Musante, L. Secretome of adipose-derived mesenchymal stem cells promotes skeletal muscle regeneration through synergistic action of extracellular vesicle cargo and soluble proteins. Stem Cell Res. Ther. 2019, 10, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Casado-Díaz, A.; Quesada-Gómez, J.M.; Dorado, G. Extracellular vesicles derived from mesenchymal stem cells (MSC) in regenerative medicine: Applications in skin wound healing. Front. Bioeng. Biotechnol. 2020, 8, 146. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Schaudinn, C.; Blume-Peytavi, U.; Vogt, A.; Rancan, F. Effects of Adipose-Derived Stem Cells and Their Conditioned Medium in a Human Ex Vivo Wound Model. Cells 2022, 11, 1198. [Google Scholar] [CrossRef]
- Bartaula-Brevik, S.; Bolstad, A.; Mustafa, K.; Pedersen, T. Secretome of mesenchymal stem cells grown in hypoxia accelerates wound healing and vessel formation in vitro. Int. J. Stem Cell Res. Ther. 2017, 4, 1–9. [Google Scholar] [CrossRef]
- Li, F.; Zhang, J.; Yi, K.; Wang, H.; Wei, H.; Chan, H.F.; Tao, Y.; Li, M. Delivery of Stem Cell Secretome for Therapeutic Applications. ACS Appl. Bio Mater. 2022, 5, 2009–2030. [Google Scholar] [CrossRef]
- Spicer, C.D. Hydrogel scaffolds for tissue engineering: The importance of polymer choice. Polym. Chem. 2020, 11, 184–219. [Google Scholar] [CrossRef]
- Robert, A.W.; Azevedo Gomes, F.; Rode, M.P.; Marques da Silva, M.; Veleirinho, M.B.d.R.; Maraschin, M.; Hayashi, L.; Wosgrau Calloni, G.; Stimamiglio, M.A. The skin regeneration potential of a pro-angiogenic secretome from human skin-derived multipotent stromal cells. J. Tissue Eng. 2019, 10, 2041731419833391. [Google Scholar] [CrossRef]
- Lukomskyj, A.O.; Rao, N.; Yan, L.; Pye, J.S.; Li, H.; Wang, B.; Li, J.J. Stem cell-based tissue engineering for the treatment of burn wounds: A systematic review of preclinical studies. Stem Cell Rev. Rep. 2022, in press. [Google Scholar] [CrossRef]
- Martins, A.; Ferreira, H.; Reis, R.L.; Neves, N.M. Delivery Systems Made of Natural-Origin Polymers for Tissue Engineering and Regenerative Medicine Applications; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
- Miranda, J.P.; Camões, S.P.; Gaspar, M.M.; Rodrigues, J.S.; Carvalheiro, M.; Bárcia, R.N.; Cruz, P.; Cruz, H.; Simões, S.; Santos, J.M. The secretome derived from 3D-cultured umbilical cord tissue MSCs counteracts manifestations typifying rheumatoid arthritis. Front. Immunol. 2019, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Mendes-Pinheiro, B.; Anjo, S.I.; Manadas, B.; Da Silva, J.D.; Marote, A.; Behie, L.A.; Teixeira, F.G.; Salgado, A.J. Bone marrow mesenchymal stem cells’ secretome exerts neuroprotective effects in a Parkinson’s disease rat model. Front. Bioeng. Biotechnol. 2019, 7, 294. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Lee, J.; Kwon, Y.; Park, K.-S.; Jeong, J.-H.; Choi, S.-J.; Bang, S.I.; Chang, J.W.; Lee, C. Comparative proteomic analysis of the mesenchymal stem cells secretome from adipose, bone marrow, placenta and wharton’s jelly. Int. J. Mol. Sci. 2021, 22, 845. [Google Scholar] [CrossRef] [PubMed]
- Beer, L.; Mildner, M.; Gyöngyösi, M.; Ankersmit, H.J. Peripheral blood mononuclear cell secretome for tissue repair. Apoptosis 2016, 21, 1336–1353. [Google Scholar] [CrossRef]
- Pires, A.O.; Mendes-Pinheiro, B.; Teixeira, F.G.; Anjo, S.I.; Ribeiro-Samy, S.; Gomes, E.D.; Serra, S.C.; Silva, N.A.; Manadas, B.; Sousa, N. Unveiling the differences of secretome of human bone marrow mesenchymal stem cells, adipose tissue-derived stem cells, and human umbilical cord perivascular cells: A proteomic analysis. Stem Cells Dev. 2016, 25, 1073–1083. [Google Scholar] [CrossRef]
- Airuddin, S.S.; Halim, A.S.; Wan Sulaiman, W.A.; Kadir, R.; Nasir, N.A.M. Adipose-Derived Stem Cell: “Treat or Trick”. Biomedicines 2021, 9, 1624. [Google Scholar] [CrossRef]
- Foo, J.B.; Looi, Q.H.; Chong, P.P.; Hassan, N.H.; Yeo, G.E.C.; Ng, C.Y.; Koh, B.; How, C.W.; Lee, S.H.; Law, J.X. Comparing the Therapeutic Potential of Stem Cells and their Secretory Products in Regenerative Medicine. Stem Cells Int. 2021, 2021, 2616807. [Google Scholar] [CrossRef]
- Trzyna, A.; Banaś-Ząbczyk, A. Adipose-derived stem cells secretome and its potential application in “stem cell-free therapy”. Biomolecules 2021, 11, 878. [Google Scholar] [CrossRef]
- Park, S.-R.; Kim, J.-W.; Jun, H.-S.; Roh, J.Y.; Lee, H.-Y.; Hong, I.-S. Stem cell secretome and its effect on cellular mechanisms relevant to wound healing. Mol. Ther. 2018, 26, 606–617. [Google Scholar] [CrossRef]
- Ahangar, P.; Mills, S.J.; Smith, L.E.; Gronthos, S.; Cowin, A.J. Human gingival fibroblast secretome accelerates wound healing through anti-inflammatory and pro-angiogenic mechanisms. NPJ Regen. Med. 2020, 5, 1–10. [Google Scholar] [CrossRef]
- Riedl, J.; Popp, C.; Eide, C.; Ebens, C.; Tolar, J. Mesenchymal stromal cells in wound healing applications: Role of the secretome, targeted delivery and impact on recessive dystrophic epidermolysis bullosa treatment. Cytotherapy 2021, 23, 961–973. [Google Scholar] [CrossRef] [PubMed]
- Motamed, S.; Taghiabadi, E.; Molaei, H.; Sodeifi, N.; Hassanpour, S.E.; Shafieyan, S.; Azargashb, E.; Farajzadeh-Vajari, F.; Aghdami, N.; Bajouri, A. Cell-based skin substitutes accelerate regeneration of extensive burn wounds in rats. Am. J. Surg. 2017, 214, 762–769. [Google Scholar] [CrossRef]
- Li, X.; Wang, Y.; Shi, L.; Li, B.; Li, J.; Wei, Z.; Lv, H.; Wu, L.; Zhang, H.; Yang, B. Magnetic targeting enhances the cutaneous wound healing effects of human mesenchymal stem cell-derived iron oxide exosomes. J. Nanobiotechnol. 2020, 18, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Daneshmandi, L.; Shah, S.; Jafari, T.; Bhattacharjee, M.; Momah, D.; Saveh-Shemshaki, N.; Lo, K.W.; Laurencin, C.T. Emergence of the stem cell secretome in regenerative engineering. Trends Biotechnol. 2020, 38, 1373–1384. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, M.A.; Sendon-Lago, J.; Eiro, N.; Trevino, M.; Gonzalez, F.; Yebra-Pimentel, E.; Giraldez, M.J.; Macia, M.; Lamelas, M.L.; Saa, J. Corneal epithelial wound healing and bactericidal effect of conditioned medium from human uterine cervical stem cells. Investig. Ophthalmol. Vis. Sci. 2015, 56, 983–992. [Google Scholar] [CrossRef]
- Osugi, M.; Katagiri, W.; Yoshimi, R.; Inukai, T.; Hibi, H.; Ueda, M. Conditioned media from mesenchymal stem cells enhanced bone regeneration in rat calvarial bone defects. Tissue Eng. Part A 2012, 18, 1479–1489. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, Y.; Shu, F.; Zhou, R.; Bao, B.; Xiao, S.; Li, K.; Lin, Q.; Zhu, L.; Xia, Z. In situ-formed adhesive hyaluronic acid hydrogel with prolonged amnion-derived conditioned medium release for diabetic wound repair. Carbohydr. Polym. 2022, 276, 118752. [Google Scholar] [CrossRef]
- Driscoll, J.; Yan, I.K.; Patel, T. Development of a Lyophilized Off-the-Shelf Mesenchymal Stem Cell-Derived Acellular Therapeutic. Pharmaceutics 2022, 14, 849. [Google Scholar] [CrossRef]
- Gonzalez, A.C.d.O.; Costa, T.F.; Andrade, Z.d.A.; Medrado, A.R.A.P. Wound healing-A literature review. An. Bras. Dermatol. 2016, 91, 614–620. [Google Scholar] [CrossRef]
- Lotfinia, M.; Lak, S.; Ghahhari, N.M.; Johari, B.; Maghsood, F.; Parsania, S.; Tabrizi, B.S.; Kadivar, M. Hypoxia pre-conditioned embryonic mesenchymal stem cell secretome reduces IL-10 production by peripheral blood mononuclear cells. Iran. Biomed. J. 2017, 21, 24. [Google Scholar] [CrossRef]
- Ahangar, P.; Mills, S.J.; Smith, L.E.; Strudwick, X.L.; Ting, A.E.; Vaes, B.; Cowin, A.J. Human multipotent adult progenitor cell-conditioned medium improves wound healing through modulating inflammation and angiogenesis in mice. Stem Cell Res. Ther. 2020, 11, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Marfia, G.; Navone, S.E.; Di Vito, C.; Ughi, N.; Tabano, S.; Miozzo, M.; Tremolada, C.; Bolla, G.; Crotti, C.; Ingegnoli, F. Mesenchymal stem cells: Potential for therapy and treatment of chronic non-healing skin wounds. Organogenesis 2015, 11, 183–206. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, T.O.; Silveira, B.M.; Meira, M.C.; Carreira, A.C.; Sogayar, M.C.; Meyer, R.; Fortuna, V. Investigating the potential of the secretome of mesenchymal stem cells derived from sickle cell disease patients. PLoS ONE 2019, 14, e0222093. [Google Scholar] [CrossRef]
- Waters, R.; Subham, S.; Pacelli, S.; Modaresi, S.; Chakravarti, A.R.; Paul, A. Development of MicroRNA-146a-enriched stem cell secretome for wound-healing applications. Mol. Pharm. 2019, 16, 4302–4312. [Google Scholar] [CrossRef] [PubMed]
- Fukutake, M.; Ochiai, D.; Masuda, H.; Abe, Y.; Sato, Y.; Otani, T.; Sakai, S.; Aramaki-Hattori, N.; Shimoda, M.; Matsumoto, T. Human amniotic fluid stem cells have a unique potential to accelerate cutaneous wound healing with reduced fibrotic scarring like a fetus. Hum. Cell 2019, 32, 51–63. [Google Scholar] [CrossRef]
- Saheli, M.; Bayat, M.; Ganji, R.; Hendudari, F.; Kheirjou, R.; Pakzad, M.; Najar, B.; Piryaei, A. Human mesenchymal stem cells-conditioned medium improves diabetic wound healing mainly through modulating fibroblast behaviors. Arch. Dermatol. Res. 2020, 312, 325–336. [Google Scholar] [CrossRef]
- Sun, J.; Zhang, Y.; Song, X.; Zhu, J.; Zhu, Q. The healing effects of conditioned medium derived from mesenchymal stem cells on radiation-induced skin wounds in rats. Cell Transplant. 2019, 28, 105–115. [Google Scholar] [CrossRef]
- Hacker, S.; Mittermayr, R.; Nickl, S.; Haider, T.; Lebherz-Eichinger, D.; Beer, L.; Mitterbauer, A.; Leiss, H.; Zimmermann, M.; Schweiger, T. Paracrine factors from irradiated peripheral blood mononuclear cells improve skin regeneration and angiogenesis in a porcine burn model. Sci. Rep. 2016, 6, 1–13. [Google Scholar]
- Padeta, I.; Nugroho, W.S.; Kusindarta, D.L.; Fibrianto, Y.H.; Budipitojo, T. Mesenchymal stem cell-conditioned medium promote the recovery of skin burn wound. Asian J. Anim. Vet. Adv. 2017, 12, 132–141. [Google Scholar] [CrossRef][Green Version]
- Tan, S.T.; Firmansyah, Y.; Elizabeth, J. New approach to skin burn treatment: Potential of secretome from wharton’s jelly mesenchymal stem cell therapy. Biochem J. 2020, 4, 11–16. [Google Scholar]
- Fang, S.; Xu, C.; Zhang, Y.; Xue, C.; Yang, C.; Bi, H.; Qian, X.; Wu, M.; Ji, K.; Zhao, Y. Umbilical cord-derived mesenchymal stem cell-derived exosomal microRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-β/SMAD2 pathway during wound healing. Stem Cells Transl. Med. 2016, 5, 1425–1439. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.Á.; Layrolle, P.; Mooney, D.J. Biomaterials functionalized with MSC secreted extracellular vesicles and soluble factors for tissue regeneration. Adv. Funct. Mater. 2020, 30, 1909125. [Google Scholar] [CrossRef] [PubMed]
- Arifka, M.; Wilar, G.; Elamin, K.M.; Wathoni, N. Polymeric Hydrogels as Mesenchymal Stem Cell Secretome Delivery System in Biomedical Applications. Polymers 2022, 14, 1218. [Google Scholar] [CrossRef] [PubMed]
- Attasgah, R.B.; Velasco-Rodríguez, B.; Pardo, A.; Fernández-Vega, J.; Arellano-Galindo, L.; Rosales-Rivera, L.C.; Prieto, G.; Barbosa, S.; Soltero, J.F.A.; Mahmoudi, M. Development of functional hybrid scaffolds for wound healing applications. Iscience 2022, 25, 104019. [Google Scholar] [CrossRef]
- Murray, R.Z.; West, Z.E.; Cowin, A.J.; Farrugia, B.L. Development and use of biomaterials as wound healing therapies. Burn. Trauma 2019, 7, s41038–018–0139–7. [Google Scholar] [CrossRef]
- Deshpande, R.; Kanitkar, M.; Kadam, S.; Dixit, K.; Chhabra, H.; Bellare, J.; Datar, S.; Kale, V.P. Matrix-entrapped cellular secretome rescues diabetes-induced EPC dysfunction and accelerates wound healing in diabetic mice. PLoS ONE 2018, 13, e0202510. [Google Scholar] [CrossRef]
- Wang, C.; Wang, M.; Xu, T.; Zhang, X.; Lin, C.; Gao, W.; Xu, H.; Lei, B.; Mao, C. Engineering bioactive self-healing antibacterial exosomes hydrogel for promoting chronic diabetic wound healing and complete skin regeneration. Theranostics 2019, 9, 65. [Google Scholar] [CrossRef]
- Liu, K.; Veenendaal, T.; Wiendels, M.; Ruiz-Zapata, A.M.; van Laar, J.; Kyranas, R.; Enting, H.; van Cranenbroek, B.; Koenen, H.J.; Mihaila, S.M. Synthetic extracellular matrices as a toolbox to tune stem cell secretome. ACS Appl. Mater. Interfaces 2020, 12, 56723–56730. [Google Scholar] [CrossRef]
- Rogers, G.F.C.; Putra, I.; Lee, H.J.; Cheng, Y.-C.; Eslani, M.; Djalilian, A.R.; Myung, D. Synergistic corneal wound healing effects of human mesenchymal stem cell secreted factors and hyaluronic acid-based viscoelastic gel. Investig. Ophthalmol. Vis. Sci. 2018, 59, 2989. [Google Scholar]
- Zhou, P.; Li, X.; Zhang, B.; Shi, Q.; Li, D.; Ju, X. A human umbilical cord mesenchymal stem cell-conditioned medium/chitosan/collagen/β-glycerophosphate thermosensitive hydrogel promotes burn injury healing in mice. BioMed Res. Int. 2019, 2019, 5768285. [Google Scholar] [CrossRef]
- Yang, J.; Chen, Z.; Pan, D.; Li, H.; Shen, J. Umbilical cord-derived mesenchymal stem cell-derived exosomes combined pluronic F127 hydrogel promote chronic diabetic wound healing and complete skin regeneration. Int. J. Nanomed. 2020, 15, 5911. [Google Scholar] [CrossRef] [PubMed]
- Myung, D.; Fernandes-Cunha, G.; Lee, H.J.; Djalilian, A.R. Enhanced wound healing effects of secretome derived from human mesenchymal stem cells cultured on electrospun fibers. Investig. Ophthalmol. Vis. Sci. 2019, 60, 4830. [Google Scholar]
- Nooshabadi, V.T.; Khanmohamadi, M.; Valipour, E.; Mahdipour, S.; Salati, A.; Malekshahi, Z.V.; Shafei, S.; Amini, E.; Farzamfar, S.; Ai, J. Impact of exosome-loaded chitosan hydrogel in wound repair and layered dermal reconstitution in mice animal model. J. Biomed. Mater. Res. Part A 2020, 108, 2138–2149. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Gong, S.; Yao, W.; Yang, Z.; Wang, R.; Yu, Z.; Wei, M. Exosome loaded genipin crosslinked hydrogel facilitates full thickness cutaneous wound healing in rat animal model. Drug Deliv. 2021, 28, 884–893. [Google Scholar] [CrossRef]
- Schmitt, A.; Rödel, P.; Anamur, C.; Seeliger, C.; Imhoff, A.B.; Herbst, E.; Vogt, S.; Van Griensven, M.; Winter, G.; Engert, J. Calcium alginate gels as stem cell matrix–making paracrine stem cell activity available for enhanced healing after surgery. PLoS ONE 2015, 10, e0118937. [Google Scholar] [CrossRef]
- Shi, Q.; Qian, Z.; Liu, D.; Sun, J.; Wang, X.; Liu, H.; Xu, J.; Guo, X. GMSC-derived exosomes combined with a chitosan/silk hydrogel sponge accelerates wound healing in a diabetic rat skin defect model. Front. Physiol. 2017, 8, 904. [Google Scholar] [CrossRef]
- Khayambashi, P.; Iyer, J.; Pillai, S.; Upadhyay, A.; Zhang, Y.; Tran, S.D. Hydrogel encapsulation of mesenchymal stem cells and their derived exosomes for tissue engineering. Int. J. Mol. Sci. 2021, 22, 684. [Google Scholar] [CrossRef]
- Xie, Y.; Guan, Q.; Guo, J.; Chen, Y.; Yin, Y.; Han, X. Hydrogels for Exosome Delivery in Biomedical Applications. Gels 2022, 8, 328. [Google Scholar] [CrossRef]
- Driscoll, J.; Patel, T. The mesenchymal stem cell secretome as an acellular regenerative therapy for liver disease. J. Gastroenterol. 2019, 54, 763–773. [Google Scholar] [CrossRef]
- Eleuteri, S.; Fierabracci, A. Insights into the secretome of mesenchymal stem cells and its potential applications. Int. J. Mol. Sci. 2019, 20, 4597. [Google Scholar] [CrossRef]
- Chen, J.; Li, Y.; Hao, H.; Li, C.; Du, Y.; Hu, Y.; Li, J.; Liang, Z.; Li, C.; Liu, J. Mesenchymal stem cell conditioned medium promotes proliferation and migration of alveolar epithelial cells under septic conditions in vitro via the JNK-P38 signaling pathway. Cell. Physiol. Biochem. 2015, 37, 1830–1846. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Lie, P.; Miao, T.; Yu, M.; Lu, Q.; Feng, T.; Li, J.; Zu, T.; Liu, X.; Li, H. Conditioned medium from umbilical cord mesenchymal stem cells induces migration and angiogenesis. Mol. Med. Rep. 2015, 12, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Yang, C.; Huang, J.; Liu, L.; Zhang, Y.; Li, S.; Zhang, L.; Sun, Q.; Yang, P. Conditioned medium derived from FGF-2-modified GMSCs enhances migration and angiogenesis of human umbilical vein endothelial cells. Stem Cell Res. Ther. 2020, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.; Ki, S.M.; Park, S.E.; Kim, M.-J.; Hyung, B.; Lee, N.K.; Shim, S.; Choi, B.-O.; Na, D.L.; Lee, J.E. Anti-apoptotic effects of human Wharton’s jelly-derived mesenchymal stem cells on skeletal muscle cells mediated via secretion of XCL1. Mol. Ther. 2016, 24, 1550–1560. [Google Scholar] [CrossRef] [PubMed]
- Kay, A.G.; Long, G.; Tyler, G.; Stefan, A.; Broadfoot, S.J.; Piccinini, A.M.; Middleton, J.; Kehoe, O. Mesenchymal stem cell-conditioned medium reduces disease severity and immune responses in inflammatory arthritis. Sci. Rep. 2017, 7, 1–11. [Google Scholar]
- Li, M.; Luan, F.; Zhao, Y.; Hao, H.; Liu, J.; Dong, L.; Fu, X.; Han, W. Mesenchymal stem cell-conditioned medium accelerates wound healing with fewer scars. Int. Wound J. 2017, 14, 64–73. [Google Scholar] [CrossRef]
- Kudinov, V.A.; Artyushev, R.I.; Zurina, I.M.; Lapshin, R.D.; Snopova, L.B.; Mukhina, I.V.; Grinakovskaya, O.S.; Saburina, I.N. Antimicrobial and Regenerative Effects of Placental Multipotent Mesenchymal Stromal Cell Secretome-Based Chitosan Gel on Infected Burns in Rats. Pharmaceuticals 2021, 14, 1263. [Google Scholar] [CrossRef]
- Kraskiewicz, H.; Hinc, P.; Krawczenko, A.; Bielawska-Pohl, A.; Paprocka, M.; Witkowska, D.; Mohd Isa, I.L.; Pandit, A.; Klimczak, A. HATMSC Secreted Factors in the Hydrogel as a Potential Treatment for Chronic Wounds—In Vitro Study. Int. J. Mol. Sci. 2021, 22, 12241. [Google Scholar] [CrossRef]
- Sears, V.; Danaoui, Y.; Ghosh, G. Impact of mesenchymal stem cell-secretome-loaded hydrogel on proliferative and migratory activities of hyperglycemic fibroblasts. Mater. Today Commun. 2021, 27, 102285. [Google Scholar] [CrossRef]
- Fernandes-Cunha, G.M.; Na, K.-S.; Putra, I.; Lee, H.J.; Hull, S.; Cheng, Y.-C.; Blanco, I.J.; Eslani, M.; Djalilian, A.R.; Myung, D. Corneal wound healing effects of mesenchymal stem cell secretome delivered within a viscoelastic gel carrier. Stem Cells Transl. Med. 2019, 8, 478–489. [Google Scholar] [CrossRef]
- Wang, B.; Pang, M.; Song, Y.; Wang, H.; Qi, P.; Bai, S.; Lei, X.; Wei, S.; Zong, Z.; Lin, S. Human fetal mesenchymal stem cells secretome promotes scarless diabetic wound healing through heat-shock protein family. Bioeng. Transl. Med. 2022, in press. [Google Scholar] [CrossRef]
- Chen, L.; Cheng, L.; Wang, Z.; Zhang, J.; Mao, X.; Liu, Z.; Zhang, Y.; Cui, W.; Sun, X. Conditioned medium-electrospun fiber biomaterials for skin regeneration. Bioact. Mater. 2021, 6, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.-C.; Guo, S.-C.; Li, M.; Ke, Q.-F.; Guo, Y.-P.; Zhang, C.-Q. Chitosan wound dressings incorporating exosomes derived from microRNA-126-overexpressing synovium mesenchymal stem cells provide sustained release of exosomes and heal full-thickness skin defects in a diabetic rat model. Stem Cells Transl. Med. 2017, 6, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Racchetti, G.; Meldolesi, J. Extracellular vesicles of mesenchymal stem cells: Therapeutic properties discovered with extraordinary success. Biomedicines 2021, 9, 667. [Google Scholar] [CrossRef] [PubMed]
- Shafei, S.; Khanmohammadi, M.; Heidari, R.; Ghanbari, H.; Taghdiri Nooshabadi, V.; Farzamfar, S.; Akbariqomi, M.; Sanikhani, N.S.; Absalan, M.; Tavoosidana, G. Exosome loaded alginate hydrogel promotes tissue regeneration in full-thickness skin wounds: An in vivo study. J. Biomed. Mater. Res. Part A 2020, 108, 545–556. [Google Scholar] [CrossRef]
- Wang, C.; Liang, C.; Wang, R.; Yao, X.; Guo, P.; Yuan, W.; Liu, Y.; Song, Y.; Li, Z.; Xie, X. The fabrication of a highly efficient self-healing hydrogel from natural biopolymers loaded with exosomes for the synergistic promotion of severe wound healing. Biomater. Sci. 2020, 8, 313–324. [Google Scholar] [CrossRef]
- Liu, K.; Chen, C.; Zhang, H.; Chen, Y.; Zhou, S. Adipose stem cell-derived exosomes in combination with hyaluronic acid accelerate wound healing through enhancing re-epithelialization and vascularization. Br. J. Dermatol. 2019, 181, 854–856. [Google Scholar] [CrossRef]
- Antezana, P.E.; Municoy, S.; Álvarez-Echazú, M.I.; Santo-Orihuela, P.L.; Catalano, P.N.; Al-Tel, T.H.; Kadumudi, F.B.; Dolatshahi-Pirouz, A.; Orive, G.; Desimone, M.F. The 3D bioprinted scaffolds for wound healing. Pharmaceutics 2022, 14, 464. [Google Scholar] [CrossRef]
- Do, A.V.; Khorsand, B.; Geary, S.M.; Salem, A.K. 3D printing of scaffolds for tissue regeneration applications. Adv. Healthc. Mater. 2015, 4, 1742–1762. [Google Scholar] [CrossRef]
- Roshangar, L.; Rad, J.S.; Kheirjou, R.; Khosroshahi, A.F. Using 3D-bioprinting scaffold loaded with adipose-derived stem cells to burns wound healing. J. Tissue Eng. Regen. Med. 2021, 15, 546–555. [Google Scholar] [CrossRef]
- Bari, E.; Scocozza, F.; Perteghella, S.; Segale, L.; Sorlini, M.; Auricchio, F.; Conti, M.; Torre, M.L. Three-Dimensional Bioprinted Controlled Release Scaffold Containing Mesenchymal Stem/Stromal Lyosecretome for Bone Regeneration: Sterile Manufacturing and In Vitro Biological Efficacy. Biomedicines 2022, 10, 1063. [Google Scholar] [CrossRef] [PubMed]
- Carter, K.; Lee, H.J.; Na, K.-S.; Fernandes-Cunha, G.M.; Blanco, I.J.; Djalilian, A.; Myung, D. Characterizing the impact of 2D and 3D culture conditions on the therapeutic effects of human mesenchymal stem cell secretome on corneal wound healing in vitro and ex vivo. Acta Biomater. 2019, 99, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Gu, C.; Feng, J.; Waqas, A.; Deng, Y.; Zhang, Y.; Chen, W.; Long, J.; Huang, S.; Chen, L. Technological advances of 3D scaffold-based stem cell/exosome therapy in tissues and organs. Front. Cell Dev. Biol. 2021, 9, 709204. [Google Scholar] [CrossRef] [PubMed]

| Stem Cell Type | Type of Wound and Model | Secretome Component | In Vitro Outcome | In Vivo Outcome | Ref. |
|---|---|---|---|---|---|
| Human (BMSC) from SCD patients | Murine excisional wound/endothelial cells in a mouse model | VEGF, IL8, MCP-1, and ANG | Using HUVECs in a 3-dimensional in vitro model demonstrates proliferation and migration in the presence of hypoxic CM that supports angiogenesis. | BMSC condition media exerts high trophic factors that promote angiogenesis and skin regeneration with accelerated wound healing. | [56] |
| ADMSC | Full-thickness skin excision on SD rats | VEGF | Rat dermal fibroblast cell line was treated with secretome revealed viability, proliferation ability, and higher migration capability, which represent better-wound healing. Macrophages were treated with secretome exert reduction of pro-inflammatory cytokines, including IL-6, TNF-α, and MCP-1. | Rapid wound closure enhanced fibroblast proliferation and migration. Moreover, the higher expression of VEGF promotes angiogenesis, which accelerates wound healing potential. | [8] |
| hUCESCs | Corneal epithelial cells/corneal ulcer on SD rats | TIMP-1, TIMP-2, FGF, and HGF | Enhanced epithelial wound healing, rapid regeneration, and the constitution of the corneal surface. | Bactericidal effect on corneal contact lenses (CLs) infected with Escherichia coli and Staphylococcus epidermidis. | [48] |
| hASC transfected with miR-146a | In vitro model using HUVECs | miR-146a UPA, (DPP IV), HGF, FGF-1, and FGF 2 | the secretome146a promotes proliferation, migration, and tube formation of endothelial cells, reflected in enhanced proangiogenic properties. Additionally, the secretome miR-146a has immunomodulation effect that can potentially promote wound healing. | In vivo outcome was not studied. | [57] |
| ADSCs | 6-mm diameter biopsy punch piercing in mice dorsal skin of male balb/c-nude mice | TGF-b1 and VEGF | Increased transdermal delivery of secretome proteins was expressed in an ex vivo porcine skin using iontophoresis as a permeation enhancer. | Acceleration of wound closure with reduced scars, represented by rapid re-epithelization, proliferation, increased tissue remodeling rate, and high vascularization. | [40] |
| HAFS | The full-thickness cutaneous excisional wound created on the dorsal skin of BALB/c mice | VEGF | In vitro effect was not tested in this study. | Speeding up of wound closure due to a decrease in myofibroblasts’ positive expression of α-SMA-rather than contraction enhanced re-epithelialization after 14 days of treatment, and overall fetal-like wound healing without scarring as a result of high expression of type III collagen accomplished by transformation of dermal fibroblasts into fetal-like fibroblasts rather than myelo fibroblasts. | [58] |
| HGFs | Dorsal excisional wounds of female BALB/c mice | IL-6, arginase, MCP-1, and IL-8 are examples of cytokines. Growth factors and ECM proteins such as HGF, FGF-2, VEGF, Ang-1, Ang-2, MMP-2, MMP-9, and TIMP-1 are also present. | Human keratinocytes and foreskin fibroblasts cells were used in vitro to evaluate a higher proliferation and migration rate. There was also an increase in capillary density, indicating enhanced angiogenesis. Additionally, increased collagen deposition is reflected in higher wound contraction without reducing fibrosis. | Wound closure acceleration with reduced inflammation, promotion of angiogenesis, and higher collagen deposition. Higher re epithelization. | [43] |
| Human bone marrow MSC | Full-skin thickness incision wound on the dorsal part of diabetic Wistar male rats (chronic diabetic wound) | bFGF and EGF expression | Human dermal fibroblasts cultured in a high glucose concentration medium resulted in an in vitro advanced wound closure due to rapid fibroblast migration, higher proliferation, and increased bFGF gene expression. | Acceleration of wound healing in terms of reduction of inflammation, increased vascularization, granulation tissue formation and enhanced, collagen deposition, and some trophic factor genes expression. | [59] |
| (WJ-MSCs) | Radiation-induced skin injury on Female Sprague–Dawley (SD) rats | ------------ | (HUVECs) growth rate and proliferation rate are increased. Enhanced number of blood vessels due to increased a-SMA expression. | Acceleration of wound closure enhances the quality of wound healing by promoting cell proliferation, sebaceous gland cell-like regeneration, and angiogenesis. | [60] |
| Gamma irradiation to induce apoptosis PBMCs | Burn wounds of 40 cm2 were created on the dorsum of the female Dan Bred pigs | IL-8 and VEGF | Histology studies carried out by using wound biopsies. | Improved epidermal regeneration and differentiation, a better wound quality without scarring, and increased numbers of CD31+ and ASMA+ cells as markers for angiogenesis. | [61] |
| MSC from fetal umbilical cord | Burn wound on the dorsal area of the Wister rat (Rattus Norvegicus) | bFGF | Histological analysis of skin tissues using M and H stains | Acceleration of wound closure, a more significant number of fibroblasts, high density of collagen fiber, and significant number of blood vessels. | [62] |
| Warton Jelly MSC | Burns on a 47-year-old woman’s left hand due to hot water exposure. | ________ | ________ | Three weeks of treatment with 10% secretome gel acceleration wound healing without scarring t | [63] |
| UMSC-Exos | Full-thickness skin wound on ICR mice and nude mice. | Exosome enriched microRNA represented as (miR-21, -23a, -125b and -145) | fibroblasts cells treated with recombinant TGF-b protein upon exposure to CM, leading to α-SMA suppression. | Wound healing promotion due to suppression of myofibroblast and scar formation through inhibition of transforming growth factor-b2/SMAD2 pathway. | [64] |
| Polymer | Secretome Source | Bioactive Molecules | Type of Hydrogel | Biomedical Apps | References |
|---|---|---|---|---|---|
| Polyisocyanate (PIC) | Human adipose-derived stem cells (hASCs) | IL-10 | Gel | Fibroblast wound healing assay or artificial wound | [71] |
| Carrageenan/poly(vinyl alcohol | SD-MSCs | VEGF | Hydrogel | full-thickness excisional wounds | [31] |
| Polycaprolactone/gelatin | Bone marrow-derived mononuclear cells | ---------------- | Electrospun scaffold | Diabetic wounds | [69] |
| Hyaluronic acid (HA) and chondroitin sulfate (CS) | Bone-marrow-derived human mesenchymal stem cells (hMSC) | Viscoelastic gel | Corneal wound | [72] | |
| Methacrylate anhydride, Hyaluronic acid, N-(2-aminoethyl)-4-[4-(hydroxymethyl)-2-methoxy-5-nitrophenoxy]-butanamide (NB) | Amnion-derived conditioned medium (AM-CM) | VEGF and TGF-β1 | In situ gel | In vivo diabetic wound | [50] |
| chitosan/collagen/β-glycerophosphate | Human umbilical cord mesenchymal stem cell | Thermosensitive hydrogel | In vivo burn wound | [50,73] | |
| Pluronic F-127 | human umbilical cord-derived MSC(hUCMSC)-derived exosomes | VEGF/(TGFβ-1) | A thermosensitive hydrogel | In vivo diabetic wound | [74] |
| Pluronic F127 /oxidative hyaluronic acid/(ε-poly-L-lysine, EPL) | Adipose mesenchymal stem cells (AMSCs)-derived exosomes | ------------- | Hydrogel | Diabetic full-thickness cutaneous wounds | [70] |
| Polycaprolactone/gelatin | Bone-marrow-derived human mesenchymal stem cells | ------------- | Electrospun fiber | In vitro corneal fibroblast cells and rabbit corneal organ culture system | [75] |
| Chitosan | Human endometrial stem cell (hEnSC)-derived exosome | ------------- | Hydrogel | full-thickness cutaneous wounds | [76] |
| Carboxymethyl chitosan/poloxamer 407 | Human umbilical cord-mesenchymal stem cells (hUCSCs)-derived exosomes | ------------- | Thermo and pH-sensitive hydrogel | Rat cutaneous wound | [77] |
| Sodium Alginate/Sodium hyalurinate/PEG | Human BM-MSCs | VEGF and FGF | Hybrid gel | Tissue regeneration after surgry | [78] |
| Sodium alginate | Peripheral blood mononuclear cells (PBMCs) | CD31+ cells | NU-GEL™ Hydrogel | Burn wound | [61] |
| Chitosan/silk fibroin | Gingival mesenchymal stem cells (GMSCs) derived exosomes | Exosomal markers CD9 and CD81 | Sponge | Diabetic rat cutaneous wound | [79] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, R.; Mndlovu, H.; Kumar, P.; Adeyemi, S.A.; Choonara, Y.E. Cell Secretome Strategies for Controlled Drug Delivery and Wound-Healing Applications. Polymers 2022, 14, 2929. https://doi.org/10.3390/polym14142929
Ibrahim R, Mndlovu H, Kumar P, Adeyemi SA, Choonara YE. Cell Secretome Strategies for Controlled Drug Delivery and Wound-Healing Applications. Polymers. 2022; 14(14):2929. https://doi.org/10.3390/polym14142929
Chicago/Turabian StyleIbrahim, Ranya, Hillary Mndlovu, Pradeep Kumar, Samson A. Adeyemi, and Yahya E. Choonara. 2022. "Cell Secretome Strategies for Controlled Drug Delivery and Wound-Healing Applications" Polymers 14, no. 14: 2929. https://doi.org/10.3390/polym14142929
APA StyleIbrahim, R., Mndlovu, H., Kumar, P., Adeyemi, S. A., & Choonara, Y. E. (2022). Cell Secretome Strategies for Controlled Drug Delivery and Wound-Healing Applications. Polymers, 14(14), 2929. https://doi.org/10.3390/polym14142929








