Shear Bond Strength of Composite Diluted with Composite-Handling Agents on Dentin and Enamel
Abstract
:1. Introduction
2. Materials and Methods
2.1. Teeth Preparation
2.2. Bonding Agent and Composite Resin Application
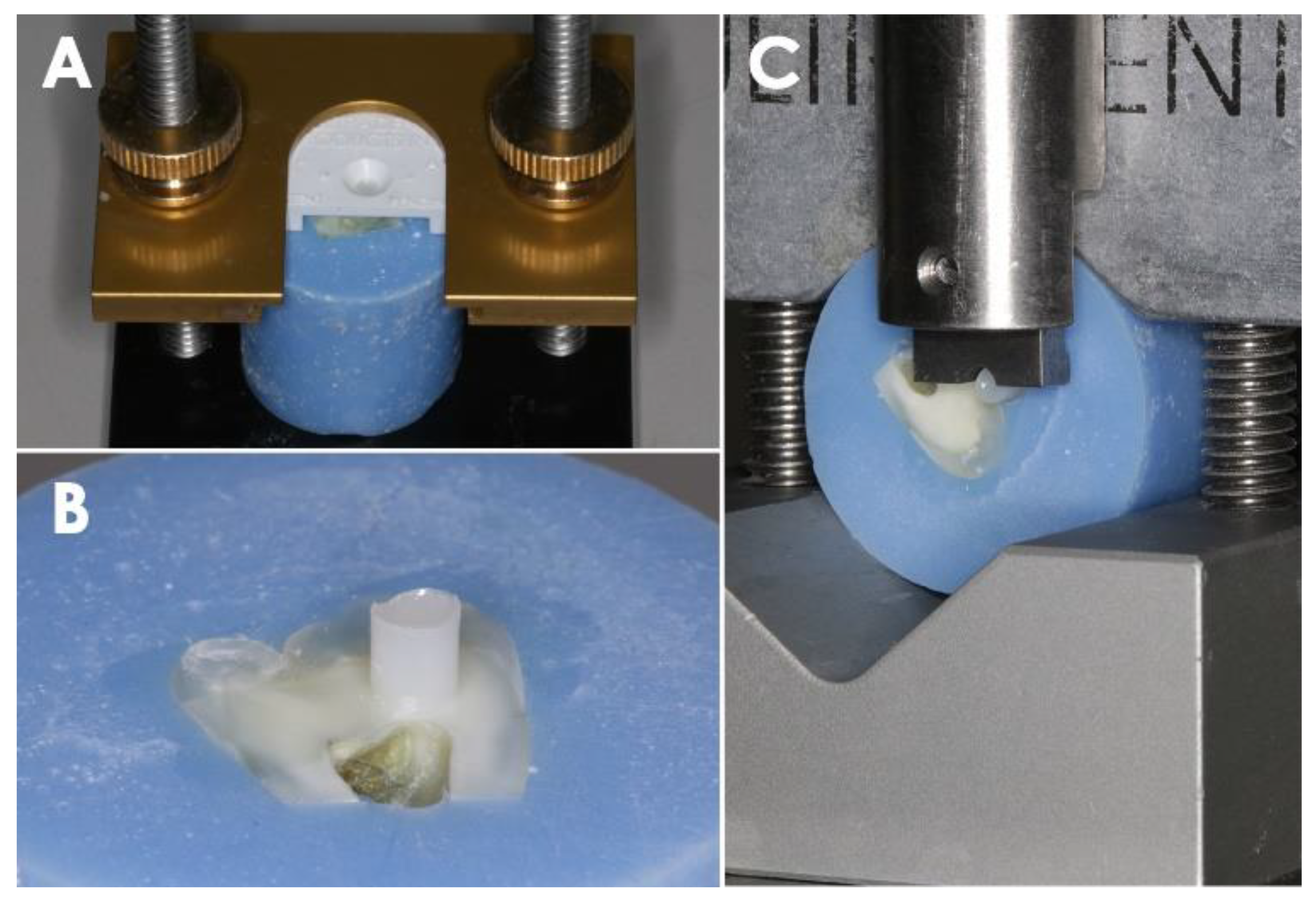
2.3. Shear Bond Strength Test
2.4. Cohesive and Adhesive Failure Evaluation
2.5. Statistical Analysis
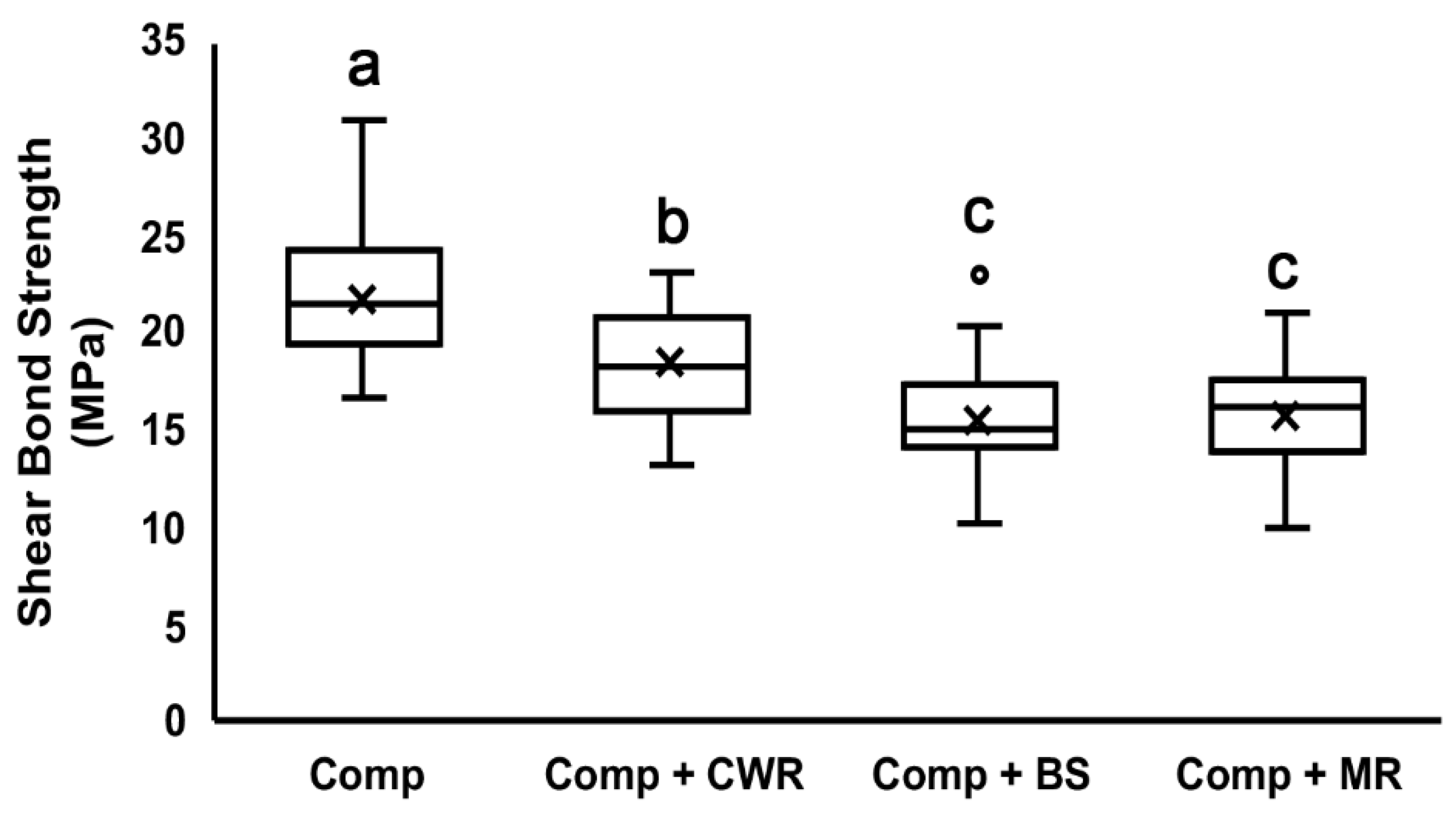
3. Results
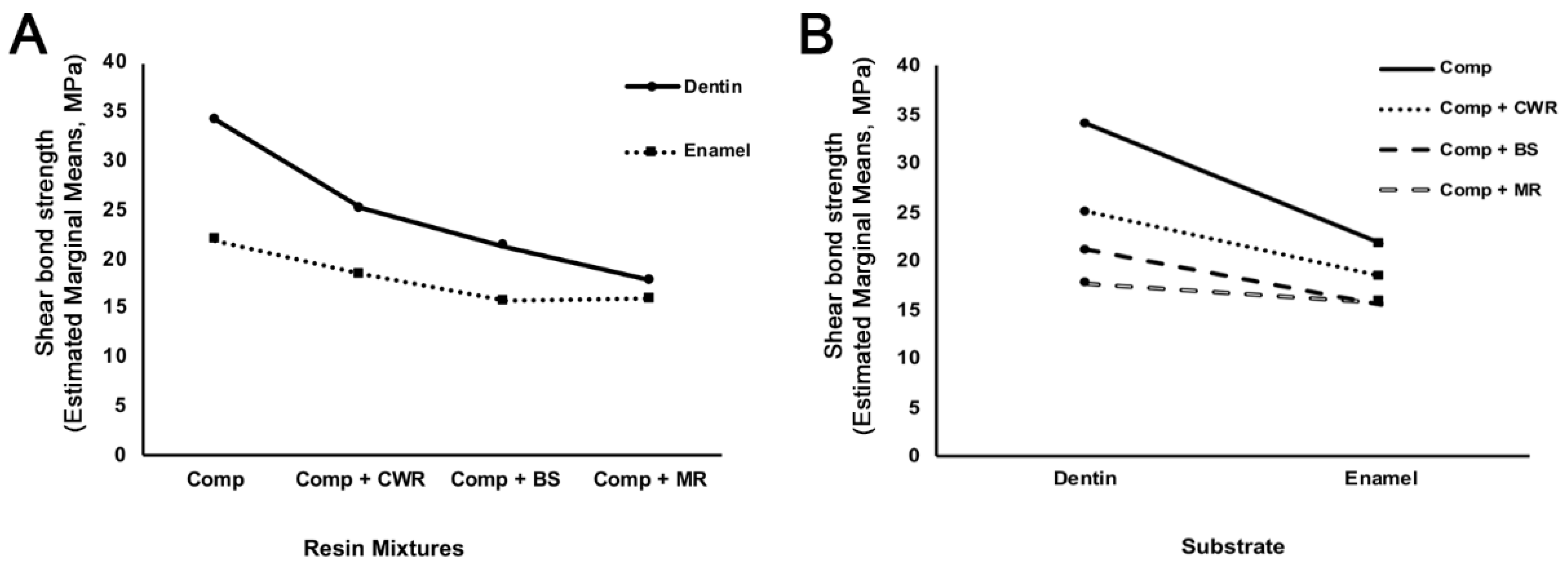
3.1. Shear Bond Test to the Dentin Surface
3.2. Shear Bond Test to the Enamel Surface
3.3. Effects of Resin Mixtures and Substrates on Shear Bond Strength
3.4. The Mode of Bonding Failure
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Villarroel, M.; Fahl, N.; De Sousa, A.M.; De Oliveira, O.B., Jr. Direct esthetic restorations based on translucency and opacity of composite resins. J. Esthet. Restor. Dent. 2011, 23, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Alzraikat, H.; Burrow, M.F.; Maghaireh, G.A.; Taha, N.A. Nanofilled Resin Composite Properties and Clinical Performance: A Review. Oper. Dent. 2018, 43, E173–E190. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.D. Successful Posterior Composites; Quintessence Publishing Company Limited: Surrey, UK, 2019; Volume 32. [Google Scholar]
- Demarco, F.F.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.; van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef]
- Demarco, F.F.; Collares, K.; Coelho-de-Souza, F.H.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Anterior composite restorations: A systematic review on long-term survival and reasons for failure. Dent. Mater. 2015, 31, 1214–1224. [Google Scholar] [CrossRef]
- Velo, M.M.D.A.C.; Coelho, L.V.B.F.; Basting, R.T.; Amaral, F.L.B.D.; França, F.M.G. Longevity of restorations in direct composite resin: Literature review. RGO-Rev. Gaúcha Odontol. 2016, 64, 320–326. [Google Scholar] [CrossRef] [Green Version]
- da Veiga, A.M.; Cunha, A.C.; Ferreira, D.M.; da Silva Fidalgo, T.K.; Chianca, T.K.; Reis, K.R.; Maia, L.C. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: A systematic review and meta-analysis. J. Dent. 2016, 54, 1–12. [Google Scholar] [CrossRef]
- Eiriksson, S.O.; Pereira, P.N.; Swift Jr, E.J.; Heymann, H.O.; Sigurdsson, A. Effects of saliva contamination on resin–resin bond strength. Dent. Mater. 2004, 20, 37–44. [Google Scholar] [CrossRef]
- de Carvalho Mendonça, E.C.; Vieira, S.N.; Kawaguchi, F.A.; Powers, J.; Matos, A.B. Influence of blood contamination on bond strength of a self-etching system. Eur. J. Dent. 2010, 4, 280–286. [Google Scholar] [CrossRef] [Green Version]
- Gaviolli, E.; Vieira, E.O.; da Silva, F.D.; Valandro, L.F.; dos Santos, S.S.; van de Sande, F.H.; Bacchi, A.; Pereira, G.K.R.; de Carvalho, R.V. Influence of different contaminants and cleansing agents on bond strength and in situ degree of conversion of composite-adhesive interface. Int. J. Adhes. Adhes. 2021, 110, 102932. [Google Scholar] [CrossRef]
- Takamizawa, T.; Ishii, R.; Tamura, T.; Yokoyama, M.; Hirokane, E.; Tsujimoto, A.; Miyazaki, M.; Kitahara, N. Handling properties and surface characteristics of universal resin composites. Dent. Mater. 2021, 37, 1390–1401. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Granger, C.; Parker, S.; Patel, M. The effect of instrument lubricant on the diametral tensile strength and water uptake of posterior composite restorative material. J. Dent. 2017, 56, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, E.T.; Atali, P.Y.; Korkut, B.; Kesimli, E.G.; Tarcin, B.; Turkmen, C. Effect of Modeling Resins on Microhardness of Resin Composites. Eur. J. Dent. 2021, 15, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Muenchow, E.A.; Sedrez-Porto, J.A.; Piva, E.; Pereira-Cenci, T.; Cenci, M.S. Use of dental adhesives as modeler liquid of resin composites. Dent. Mater. 2016, 32, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liu, W.; Sun, L.; Aifantis, K.E.; Yu, B.; Fan, Y.; Feng, Q.; Cui, F.; Watari, F. Resin composites reinforced by nanoscaled fibers or tubes for dental regeneration. BioMed Res. Int. 2014, 2014, 542958. [Google Scholar] [CrossRef] [PubMed]
- Cangul, S.; Erpacal, B.; Adiguzel, O.; Unal, M.; Gunay, A. Effect of Surface Wetting Resin on the Color Stability and Microhardness of Esthetic Composites. Odovtos Int. J. Dent. Sci. 2021, 23, 82–89. [Google Scholar] [CrossRef]
- Krajangta, N.; Ninbanjong, S.; Khosook, S.; Chaitontuak, K.; Klaisiri, A. Effects of Immediate Coating on Unset Composite with Different Bonding Agents to Surface Hardness. Eur. J. Dent. 2022. [Google Scholar] [CrossRef]
- Kutuk, Z.B.; Erden, E.; Aksahin, D.L.; Durak, Z.E.; Dulda, A.C. Influence of modeling agents on the surface properties of an esthetic nano-hybrid composite. Restor. Dent. Endod. 2020, 45, e13. [Google Scholar] [CrossRef] [Green Version]
- Sarmiento, G.; Ayala, G.; Watanabe, R.; Salcedo-Moncada, D.; Alvítez-Temoche, D.; Mayta-Tovalino, F. Microleakage in premolar class I restorations between nanohybrid and microhybrid composites: A comparative in vitro study. J. Int. Oral Health 2021, 13, 288. [Google Scholar]
- Tuncer, S.; Demirci, M.; Tiryaki, M.; Ünlü, N.; Uysal, Ö. The effect of a modeling resin and thermocycling on the surface hardness, roughness, and color of different resin composites. J. Esthet. Restor. Dent. 2013, 25, 404–419. [Google Scholar] [CrossRef]
- De Munck, J.; Van Landuyt, K.; Peumans, M.; Poitevin, A.; Lambrechts, P.; Braem, M.; Van Meerbeek, B. A critical review of the durability of adhesion to tooth tissue: Methods and results. J. Dent. Res. 2005, 84, 118–132. [Google Scholar] [CrossRef] [PubMed]
- Nujella, B.P.; Choudary, M.T.; Reddy, S.P.; Kumar, M.K.; Gopal, T. Comparison of shear bond strength of aesthetic restorative materials. Contemp. Clin. Dent. 2012, 3, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Holderegger, C.; Sailer, I.; Schuhmacher, C.; Schlapfer, R.; Hammerle, C.; Fischer, J. Shear bond strength of resin cements to human dentin. Dent. Mater. 2008, 24, 944–950. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perdigao, J.; Gomes, G. Effect of instrument lubricant on the cohesive strength of a hybrid resin composite. Quintessence Int. 2006, 37, 621–625. [Google Scholar]
- Dunn, W.J.; Strong, T.C. Effect of alcohol and unfilled resin in the incremental buildup of resin composite. Quintessence Int. 2007, 38, e20–e26. [Google Scholar]
- Barcellos, D.C.; Pucci, C.R.; Torres, C.R.G.; Goto, E.H.; Inocencio, A.C. Effects of resinous monomers used in restorative dental modeling on the cohesive strength of composite resin. J. Adhes. Dent. 2008, 10, 351–354. [Google Scholar]
- Al-Towairqi, W.; Hamouda, I. Effect of instrument lubricant on water sorption and solubility of incrementally applied nanofilled resin composite. J. Nanotechnol. Nanomed. Nanobiotechnol. 2017, 4, 019. [Google Scholar]
- Najafi-Abrandabadi, A.; Najafi-Abrandabadi, S.; Ghasemi, A.; Kotick, P.G. Microshear bond strength of composite resins to enamel and porcelain substrates utilizing unfilled versus filled resins. Dent. Res. J. 2014, 11, 636–644. [Google Scholar]
- Mortazavi, V.; Fathi, M.; Ataei, E.; Khodaeian, N.; Askari, N. Shear bond strengths and morphological evaluation of filled and unfilled adhesive interfaces to enamel and dentine. Int. J. Dent. 2012, 2012, 858459. [Google Scholar] [CrossRef] [Green Version]
- Pashley, D.H.; Swift, E.J., Jr. Dentin bonding. J. Esthet. Restor. Dent. 2008, 20, 153–154. [Google Scholar] [CrossRef]
- Leirskar, J.; Øilo, G.; Nordbø, H. In vitro shear bond strength of two resin composites to dentin with five different dentin adhesives. Quintessence Int. 1998, 29, 787–792. [Google Scholar] [PubMed]
- Meharry, M.R.; Moazzami, S.M.; Li, Y. Comparison of enamel and dentin shear bond strengths of current dental bonding adhesives from three bond generations. Oper. Dent. 2013, 38, E237–E245. [Google Scholar] [CrossRef] [PubMed]
- Shimada, Y.; Tagami, J. Effects of regional enamel and prism orientation on resin bonding. Oper. Dent. 2003, 28, 20–27. [Google Scholar] [PubMed]
- Guo, J.; Wang, L.P.; Zhu, J.; Yang, J.; Zhu, H.S. Impact of Dentinal Tubule Orientation on Dentin Bond Strength. Curr. Med. Sci. 2018, 38, 721–726. [Google Scholar] [CrossRef]
- Frankenberger, R.; Lohbauer, U.; Roggendorf, M.J.; Naumann, M.; Taschner, M. Selective enamel etching reconsidered: Better than etch-and-rinse and self-etch? J. Adhes. Dent. 2008, 10, 339–344. [Google Scholar]


| Products | Manufacturer | Filler (%) | Filler Material | Organic Matrix |
|---|---|---|---|---|
| Composite Wetting Resin (CWR) | Ultradent | 45% | Undisclosed | DUDMA, BHT, TEGDMA |
| Brush and Sculpt (BS) | Cosmedent | 36% | 0.04 µm silicon dioxide | UDMA, Bis-GMA, 1,4-Butanediol dimethacrylate |
| Modeling Resin (MR) | BISCO | 20–40% | Amorphous silica | UDMA, Bis-GMA, TEGDMA, ethoxylated Bis A dimethacrylate |
| Group | Dentin (Mean ± STD) | Enamel (Mean ± STD) |
|---|---|---|
| Comp | 34.16 ± 3.65 a | 21.84 ± 3.49 a |
| Comp + CWR | 25.09 ± 3.10 b | 18.45 ± 2.98 b |
| Comp + BS | 21.24 ± 3.37 c | 15.66 ± 3.19 c |
| Comp + MR | 17.73 ± 3.26 d | 15.84 ± 2.75 c |
| Source | Type III Sum of Squares | Df | Mean Square | F | p |
|---|---|---|---|---|---|
| Corrected Model | 5251.171 a | 7 | 750.167 | 71.685 | <0.001 |
| Intercept | 72,284.004 | 1 | 72,284.004 | 6907.367 | <0.001 |
| Resin Mixtures | 2943.575 | 3 | 981.192 | 93.761 | <0.001 |
| Substrate | 1747.684 | 1 | 1747.684 | 167.006 | <0.001 |
| Resin Mixtures * Substrates | 559.912 | 3 | 186.637 | 17.835 | <0.001 |
| Error | 1590.645 | 152 | 10.465 | ||
| Total | 79,125.820 | 160 | |||
| Corrected Total | 6841.816 | 159 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Jo, D.-W.; Khalifah, S.A.; Yu, B.; Hayashi, M.; Kim, R.H. Shear Bond Strength of Composite Diluted with Composite-Handling Agents on Dentin and Enamel. Polymers 2022, 14, 2665. https://doi.org/10.3390/polym14132665
Kim M, Jo D-W, Khalifah SA, Yu B, Hayashi M, Kim RH. Shear Bond Strength of Composite Diluted with Composite-Handling Agents on Dentin and Enamel. Polymers. 2022; 14(13):2665. https://doi.org/10.3390/polym14132665
Chicago/Turabian StyleKim, Mijoo, Deuk-Won Jo, Shahed Al Khalifah, Bo Yu, Marc Hayashi, and Reuben H. Kim. 2022. "Shear Bond Strength of Composite Diluted with Composite-Handling Agents on Dentin and Enamel" Polymers 14, no. 13: 2665. https://doi.org/10.3390/polym14132665
APA StyleKim, M., Jo, D.-W., Khalifah, S. A., Yu, B., Hayashi, M., & Kim, R. H. (2022). Shear Bond Strength of Composite Diluted with Composite-Handling Agents on Dentin and Enamel. Polymers, 14(13), 2665. https://doi.org/10.3390/polym14132665






