Development and Characterization of Oral Raft Forming In Situ Gelling System of Neratinib Anticancer Drug Using 32 Factorial Design
Abstract
1. Introduction
2. Resources and Methods
2.1. Materials
2.2. Methods
2.2.1. PEG—Neratinib Solid Dispersion Preparations
2.2.2. Determination of Saturation Solubility
2.2.3. Analytical Method Development
Determination of Absorption Maxima of NTB
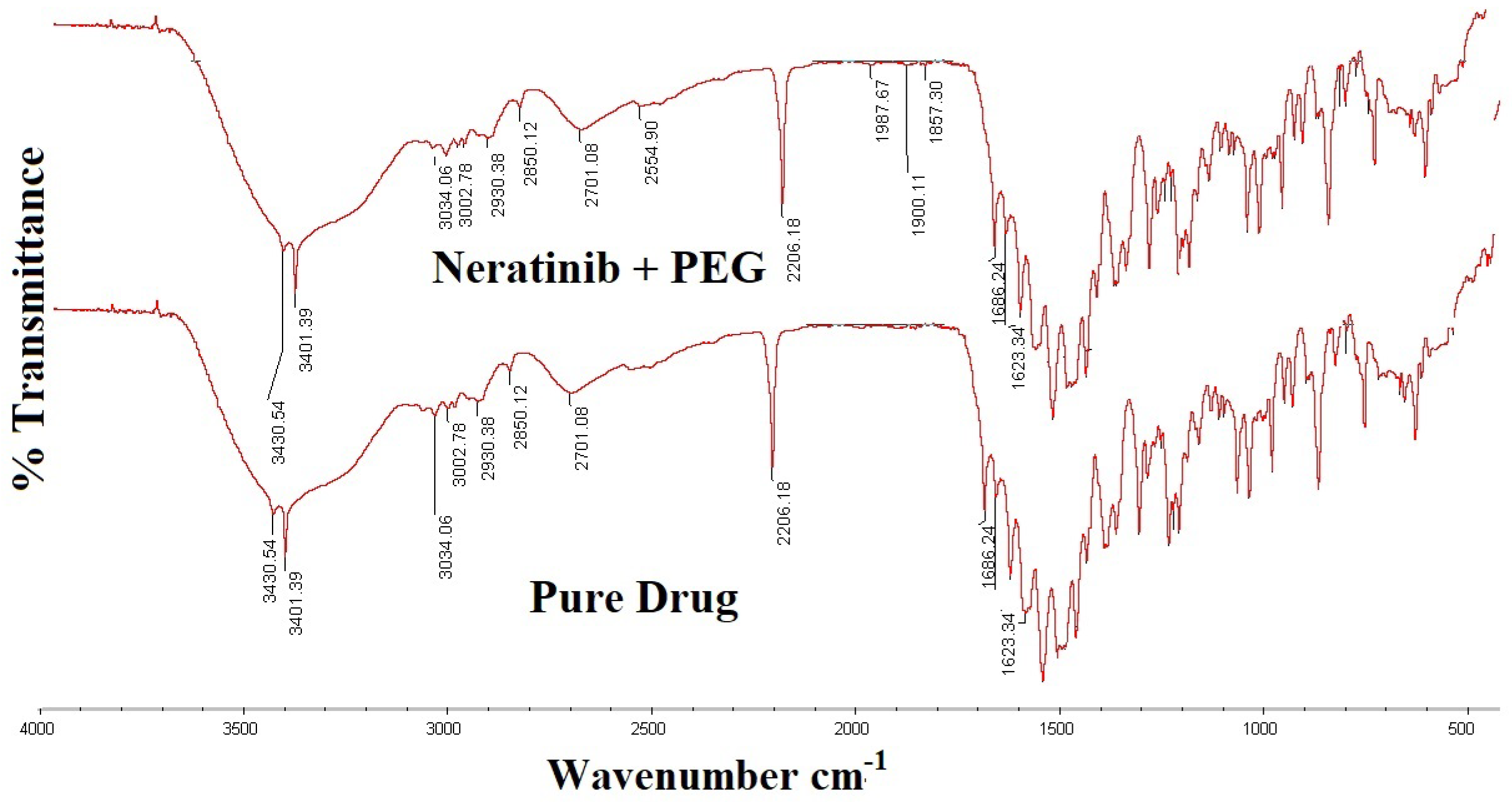
2.2.4. Fourier Transform Infrared Spectroscopy (FT-IR) Studies
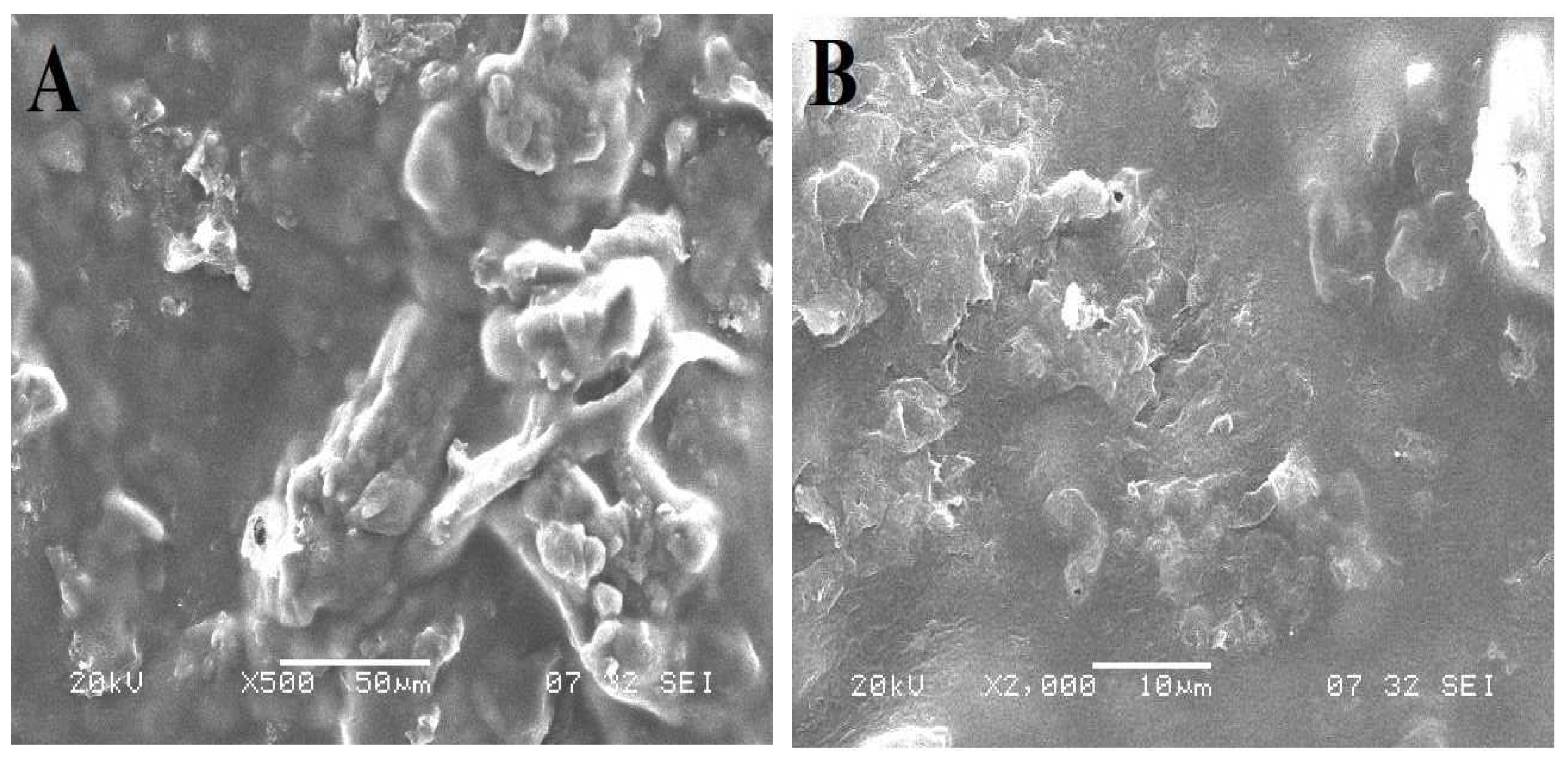
2.2.5. Scanning Electron Microscopy
2.2.6. NTB Floating In Situ Gel Preparation
2.2.7. Experimental Design
2.3. Evaluation
2.3.1. Physicochemical Properties
2.3.2. Drug Content Determination
2.3.3. pH Determination
2.3.4. In Vitro Gelling Capacity
2.3.5. In Vitro Floating Study
2.3.6. Water Uptake Study
2.3.7. In Vitro Drug Release Study
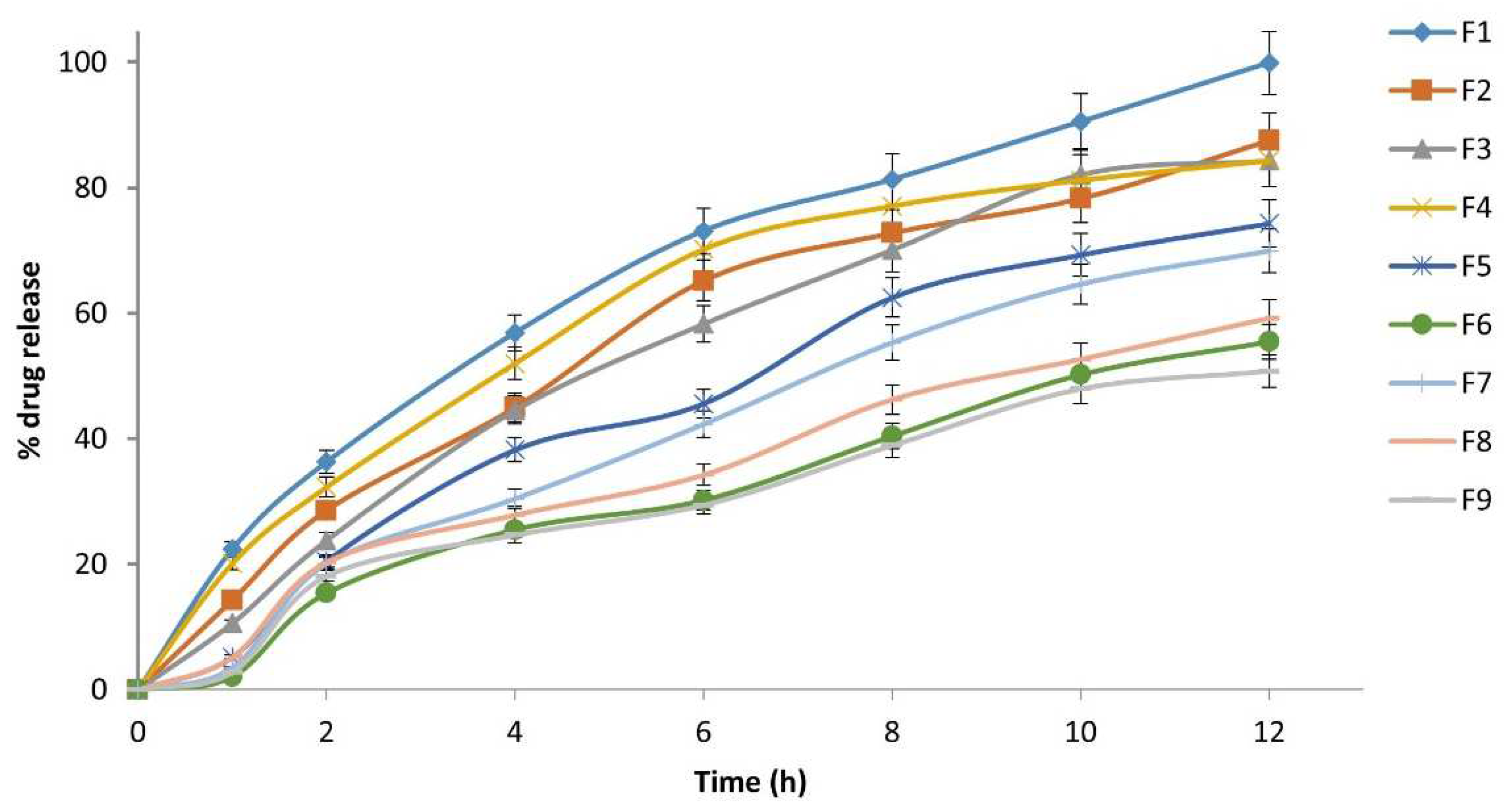
2.3.8. Kinetics of Drug Release Studies
3. Results and Discussion
3.1. Saturation Solubility Studies of NTB PEG Solid Dispersions
3.2. FT-IR Spectra
3.3. Scanning Electron Microscopy
3.4. Drug Content
3.5. Physicochemical Properties
3.6. pH Determination
3.7. In Vitro Gelling Capacity
3.8. In Vitro Floating Study
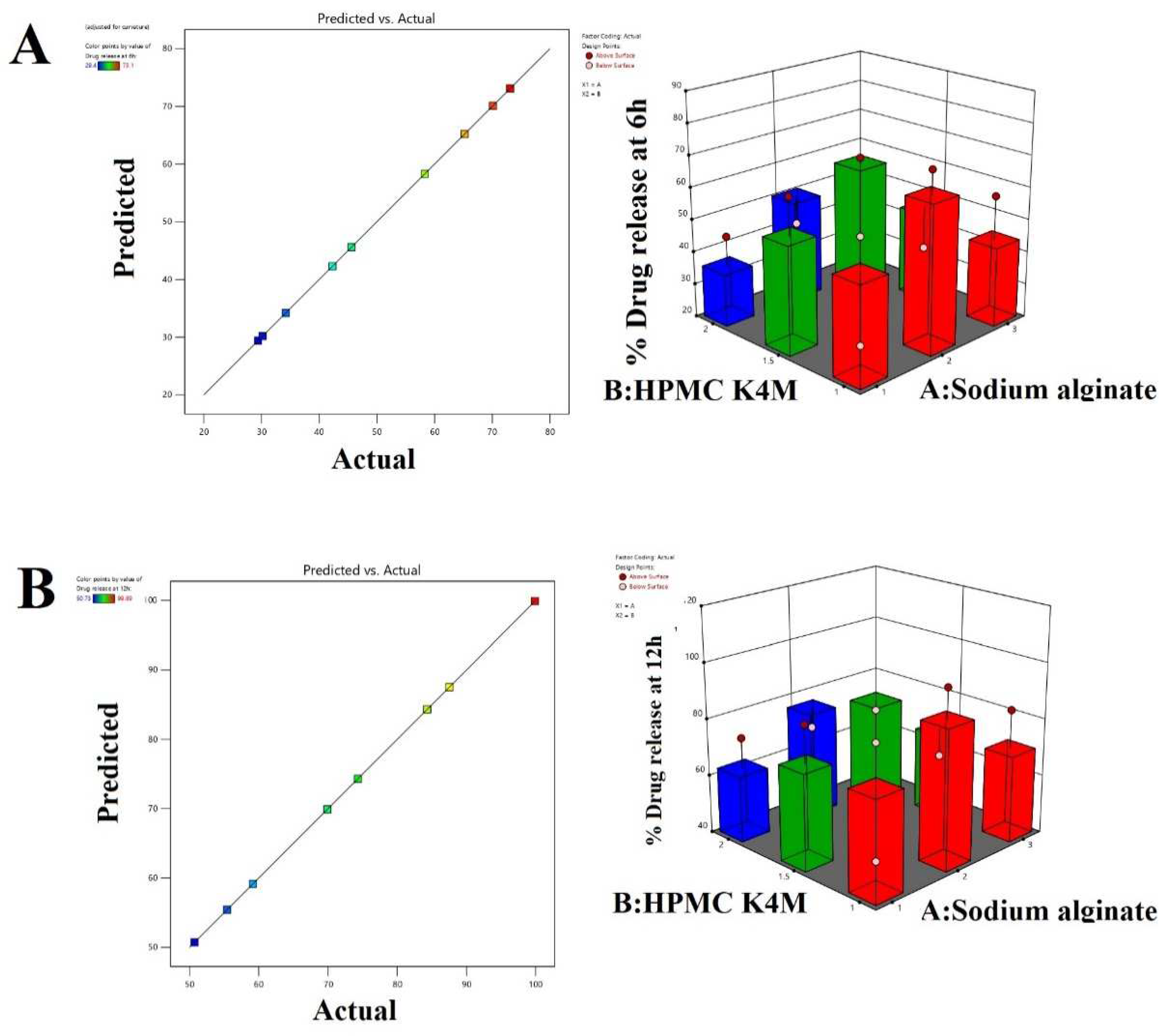
3.9. In Vitro Drug Release
3.10. Kinetics of Drug Release Studies
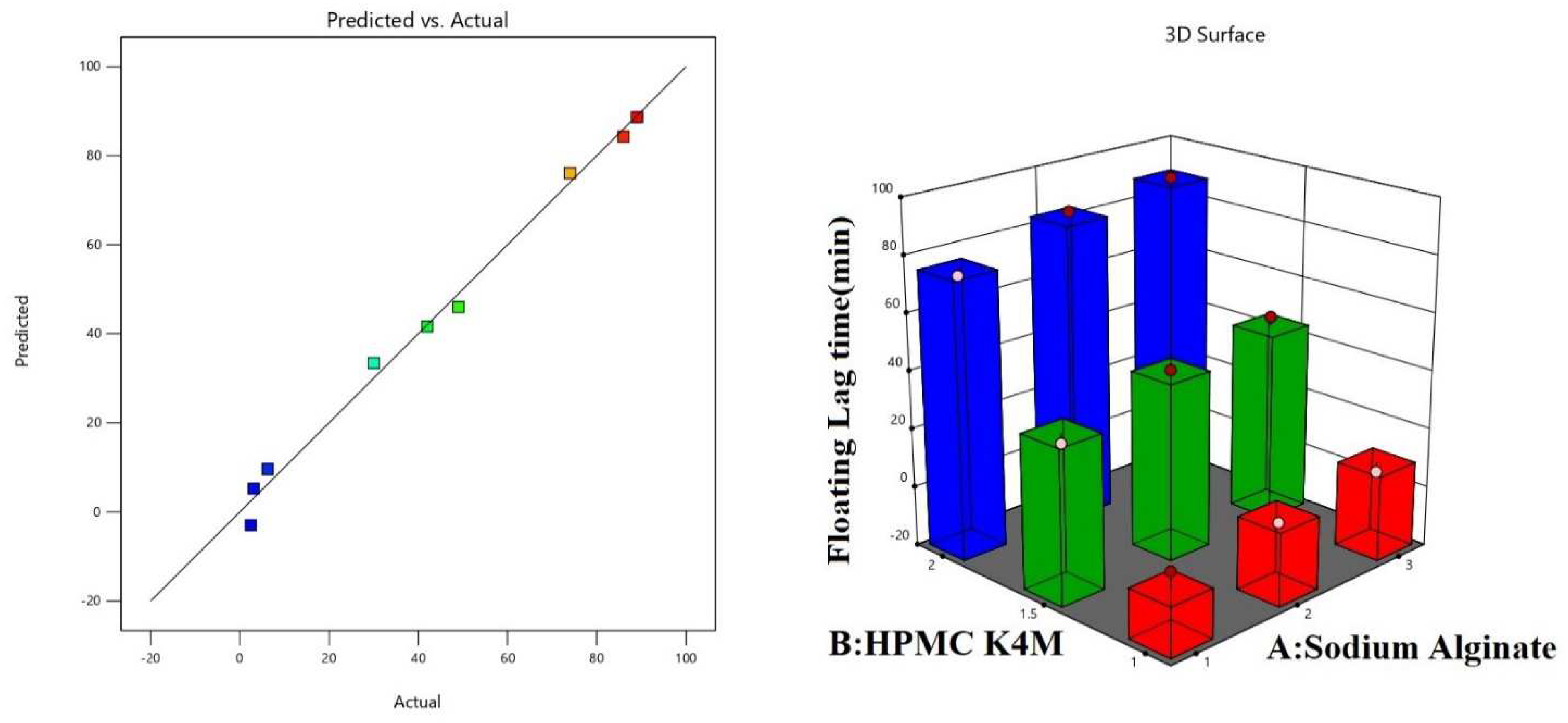
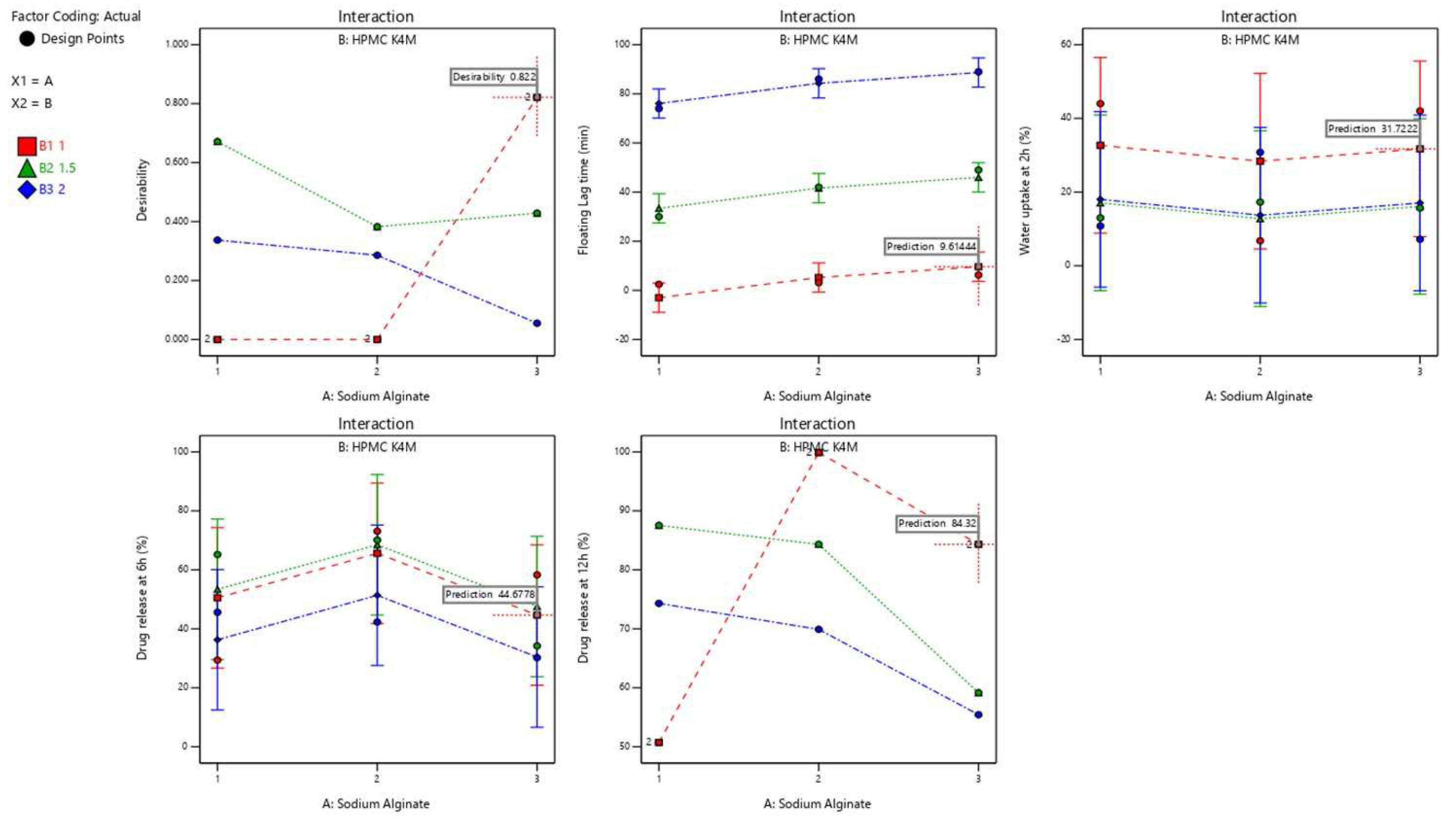
4. Data Analysis and Optimization
4.1. Impact of Independent Variables on Floating Lag Time Response
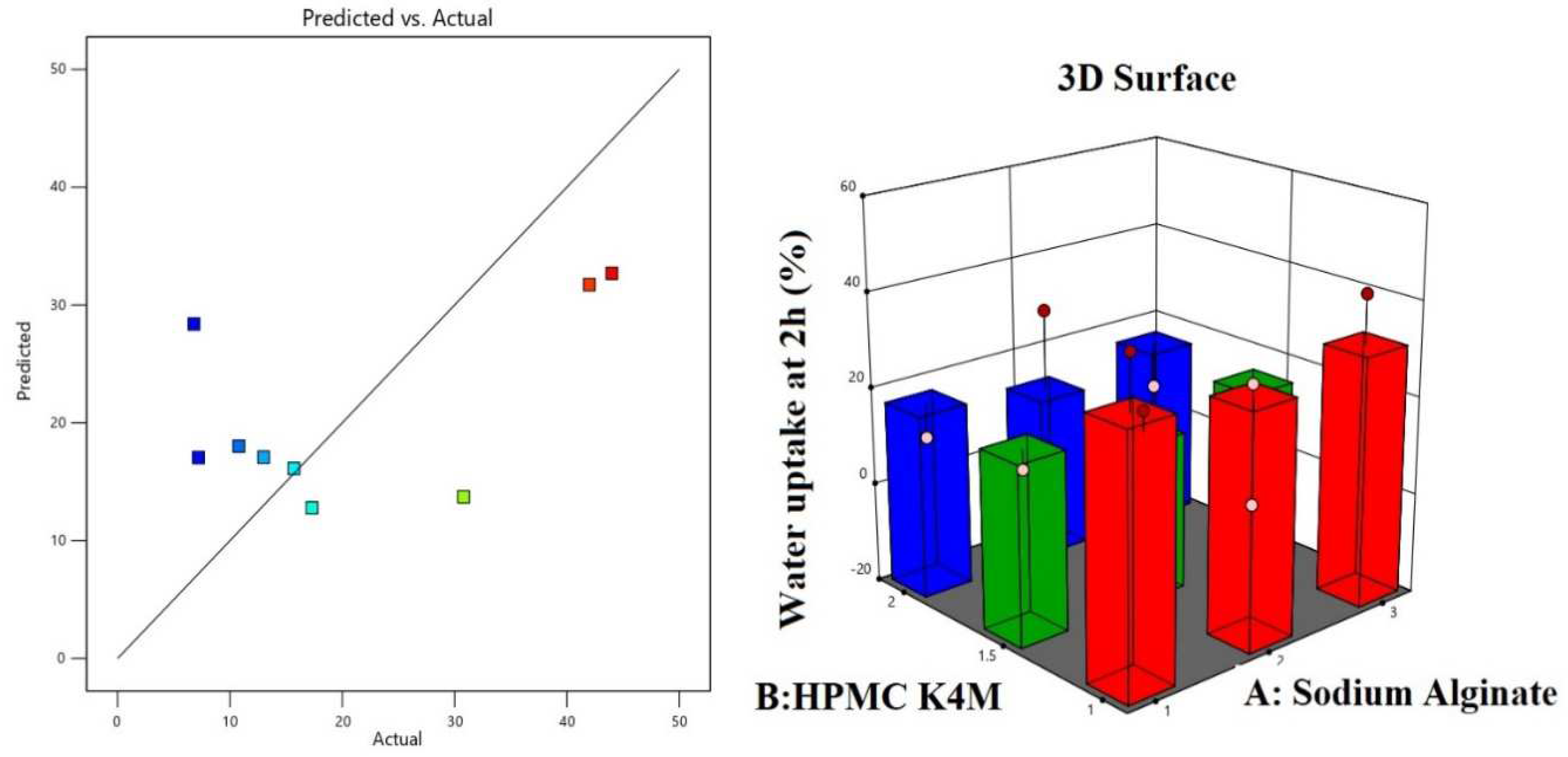
4.2. Impact of Independent Variables on Percentage Water Uptake Response
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HER-2 | Pan-human epidermal growth factor (HER-2) |
| HCL | Hydrochloric acid |
| GIT | Gastrointestinal tract (GIT) |
| KP | Korsemeyer Peppas |
| PEG | Polyethylene glycol |
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Hani, U.; Begum, M.Y.; Wahab, S.; Siddiqua, A.; Osmani, R.A.M.; Rahamathulla, M. Correction to: A Comprehensive Review of Current Perspectives on Novel Drug Delivery Systems and Approaches for Lung Cancer Management. J. Pharm. Innov. 2021. [Google Scholar] [CrossRef]
- Kolak, A.; Kamińska, M.; Sygit, K.; Budny, A.; Surdyka, D.; Kukiełka-Budny, B.; Burdan, F. Primary and secondary prevention of breast cancer. Ann. Agric. Environ. Med. 2017, 24, 549–553. [Google Scholar] [CrossRef]
- Kenchegowda, M.; Rahamathulla, M.; Hani, U.; Begum, M.Y.; Guruswamy, S.; Osmani, R.A.M.; Gowrav, M.P.; Alshehri, S.; Ghoneim, M.M.; Alshlowi, A.; et al. Smart Nanocarriers as an Emerging Platform for Cancer Therapy: A Review. Molecules 2021, 27, 146. [Google Scholar] [CrossRef]
- Hani, U.; Rahamathulla, M.; Osmani, R.A.M.; Urolagin, D.; Urolagin, D.; Ansari, M.Y.; Pandey, K.; Devi, K.; Yasmin, S. Recent advances in novel drug delivery systems and approaches for management of breast cancer: A comprehensive review. J. Drug Deliv. Sci. Technol. 2020, 56, 101505. [Google Scholar] [CrossRef]
- Rahamathulla, M.; Hani, U.; Alqahtani, A.; Gangadharappa, H.V.; Begum, M.Y.; Jafar, M.; Osmani, R.A.M.; Chidambaram, K.; Moin, A.; Shankar, S.J. 23 Factorial Design and Optimization of Effervescent Floating Matrix Tablet of Neratinib. J. Pharm. Innov. 2021. [Google Scholar] [CrossRef]
- Jackisch, C.; Barcenas, C.H.; Bartsch, R.; Di Palma, J.; Glück, S.; Harbeck, N.; Macedo, G.; O’Shaughnessy, J.; Pistilli, B.; Ruiz-Borrego, M.; et al. Optimal Strategies for Successful Initiation of Neratinib in Patients with HER2-Positive Breast Cancer. Clin. Breast Cancer 2021, 21, e575–e583. [Google Scholar] [CrossRef]
- Rahamathulla, M.; Alam, N.; Hani, U.; Ibrahim, Q.; Alhamhoom, Y. Development and in vitro evaluation of effervescent floating matrix tablet of neritinib: An anticancer drug. Pak. J. Pharm. Sci. 2021, 34, 1297–1303. [Google Scholar]
- Rahamathulla, M.; Alsahhrani, S.M.; Al Saqr, A.; Alshetaili, A.; Shakeel, F. Effervescent floating matrix tablets of a novel anti-cancer drug neratinib for breast cancer treatment. J. Drug Deliv. Sci. Technol. 2021, 66, 102788. [Google Scholar] [CrossRef]
- Hani, U.; Krishna, G.; Shivakumar, H.G. Design and optimization of clotrimazole–hydroxypropyl-β-cyclodextrin bioadhesive vaginal tablets using Anacardium occidentale gum by 32 factorial design. RSC Adv. 2015, 5, 35391–35404. [Google Scholar] [CrossRef]
- Saisivam, S.; Rahamathulla, M.; Shakeel, F. Development of floating matrix tablets of losartan potassium: In vitro and in vivo evaluation. J. Drug Deliv. Sci. Technol. 2013, 6, 611–617. [Google Scholar] [PubMed]
- Rahamathulla, M.; HV, G.; Veerapu, G.; Hani, U.; Alhamhoom, Y.; Alqahtani, A.; Moin, A. Characterization, Optimization, In Vitro and In Vivo Evaluation of Simvastatin Proliposomes, as a Drug Delivery. AAPS PharmSciTech 2020, 13, 129. [Google Scholar] [CrossRef] [PubMed]
- Prajapati, V.D.; Jani, G.K.; Khutliwala, T.A.; Zala, B.S. Raft forming system-an upcoming approach of gastroretentive drug delivery system. J. Control. Release 2013, 10, 151–165. [Google Scholar] [CrossRef] [PubMed]
- Jauhari, S.; Dash, A.K. A mucoadhesive in situ gel delivery system for paclitaxel. AAPS PharmSciTech 2006, 7, E154–E159. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Geng, J.; Su, S.; Zhang, L.; Xu, Q.; Zhang, L.; Xie, Y.; Wu, S.; Sun, Y.; Gao, Z. Doxorubicin-Loaded Zein in Situ Gel for Interstitial Chemotherapy. Chem. Pharm. Bull. 2012, 60, 1227–1233. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hani, U.; Osmani, R.A.M.; Alqahtani, A.; Ghazwani, M.; Rahamathulla, M.; Almordy, S.A.; Alsaleh, H.A. 23 Full Factorial Design for Formulation and Evaluation of Floating Oral In Situ Gelling System of Piroxicam. J. Pharm. Innov. 2020, 16, 528–536. [Google Scholar] [CrossRef]
- Rahamathulla, M.; Hv, G.; Rathod, N. Solubility and dissolution improvement of Rofecoxib using solid dispersion technique. Pak. J. Pharm. Sci. 2008, 21, 350–355. [Google Scholar]
- Sakure, K.; Kumari, L.; Badwaik, H. Development and evaluation of solid dispersion based rapid disintegrating tablets of poorly water-soluble anti-diabetic drug. J. Drug Deliv. Sci. Technol. 2020, 60, 101942. [Google Scholar] [CrossRef]
- Alshehri, S.; Imam, S.S.; Hussain, A.; Altamimi, M.A.; Alruwaili, N.K.; Alotaibi, F.; Alanazi, A.; Shakeel, F. Potential of solid dispersions to enhance solubility, bioavailability, and therapeutic efficacy of poorly water-soluble drugs: Newer formulation techniques, current marketed scenario and patents. Drug Deliv. 2020, 27, 1625–1643. [Google Scholar] [CrossRef]
- Costa, B.L.A.; Sauceau, M.; Confetto, S.D.; Sescousse, R.; Ré, M.I. Determination of drug-polymer solubility from supersaturated spray-dried amorphous solid dispersions: A case study with Efavirenz and Soluplus. Eur. J. Pharm. Biopharm. 2019, 142, 300–306. [Google Scholar] [CrossRef]
- Obiedallah, M.M.; Abdel-Mageed, A.M.; Elfaham, T.H. Ocular administration of acetazolamide microsponges in-situ gel formulations. Saudi Pharm. J. 2018, 26, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Dadhani, B.; Ladani, R.; Baria, A.; Patel, J. Formulation, evaluation and optimization of stomach specific in situ gel of clarithromycin and metronidazole benzoate. Int. J. Drug Deliv. 2010, 2, 141–153. [Google Scholar] [CrossRef]
- Chen, N.; Niu, J.; Li, Q.; Li, J.; Chen, X.; Ren, Y.; Wu, G.; Liu, Y.; Shi, Y. Development and evaluation of a new gastroretentive drug delivery system: Nanomicelles-loaded floating mucoadhesive beads. J. Drug Deliv. Sci. Technol. 2019, 51, 485–492. [Google Scholar] [CrossRef]
- Paradkar, M.U.; Parmar, M. Formulation development and evaluation of Natamycin niosomal in-situ gel for ophthalmic drug delivery. J. Drug Deliv. Sci. Technol. 2017, 39, 113–122. [Google Scholar] [CrossRef]
- Osmani, R.A.M.; Aloorkar, N.H.; Ingale, D.J.; Kulkarni, P.K.; Hani, U.; Bhosale, R.R.; Dev, D.J. Microsponges based novel drug delivery system for augmented arthritis therapy. Saudi Pharm. J. 2015, 23, 562–572. [Google Scholar] [CrossRef] [PubMed]
- Osmani, R.A.M.; Aloorkar, N.H.; Thaware, B.U.; Kulkarni, P.K.; Moin, A.; Hani, U.; Srivastava, A.; Bhosale, R.R. Microsponge based drug delivery system for augmented gastroparesis therapy: Formulation development and evaluation. Asian J. Pharm. Sci. 2015, 10, 442–451. [Google Scholar] [CrossRef]
- Jahangir, M.A.; Saleem, M.; Shahab, M.S.; Muheem, A.; Saleem, S. Formulation and evaluation of novel floating in situ gelling system of macrolide antibiotic using different gelling polymers. J. Drug Deliv. Ther. 2015, 5, 48–55. [Google Scholar] [CrossRef]
- Suraj, S.; Gunjan, S.; Bhupendra, S. In-situ fast gelling formulation for oral sustained drug delivery of paracetamol to dysphagic patients. Int. J. Biol. Macromol. 2019, 134, 864–868. [Google Scholar]
- Singh, E.; Osmani, R.A.M.; Banerjee, R.; Abu Lila, A.S.; Moin, A.; Almansour, K.; Arab, H.H.; Alotaibi, H.F.; Khafagy, E.-S. Poly ε-Caprolactone Nanoparticles for Sustained Intra-Articular Immune Modulation in Adjuvant-Induced Arthritis Rodent Model. Pharmaceutics 2022, 14, 519. [Google Scholar] [CrossRef]
- Rani, K.R.V.; Rajan, S.; Bhupathyraaj, M.; Priya, R.K.; Halligudi, N.; Al-Ghazali, M.A.; Sridhar, S.B.; Shareef, J.; Thomas, S.; Desai, S.M.; et al. The Effect of Polymers on Drug Release Kinetics in Nanoemulsion In Situ Gel Formulation. Polymers 2022, 14, 427. [Google Scholar] [CrossRef]
- Osmani, R.A.M.; Aloorkar, N.H.; Kulkarni, A.S.; Kulkarni, P.K.; Hani, U.; Thirumaleshwar, S.; Bhosale, R.R. Novel cream containing microsponges of anti-acne agent: Formulation development and evaluation. Curr. Drug Deliv. 2015, 12, 504–516. [Google Scholar] [CrossRef] [PubMed]
- Osmani, R.A.M.; Moin, A.; Deb, T.K.; Bhosale, R.R.; Hani, U. Fabrication, characterization, and evaluation of microsponge delivery system for facilitated fungal therapy. J. Basic Clin. Pharm. 2016, 7, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Osmani, R.A.M.; Kulkarni, P.K.; Shanmuganathan, S.; Hani, U.; Srivastava, A.; Prerana, M.; Shinde, C.G.; Bhosale, R.R. A 32 full factorial design for development and characterization of a nanosponge-based intravaginal in-situ gelling system for vulvovaginal candidiasis. RSC Adv. 2016, 6, 18737–18750. [Google Scholar] [CrossRef]

| Ingredients | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 |
|---|---|---|---|---|---|---|---|---|---|
| Neratinib (mg) | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Sodium alginate (g) | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 |
| HPMC K4M (g) | 1 | 1 | 1 | 1.5 | 1.5 | 1.5 | 2 | 2 | 2 |
| Sodium bicarbonate (%) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Sodium citrate (%) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Methyl paraben (%) | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 | 0.8 |
| Variables | Actual Value (g) | Coded Value | ||||
|---|---|---|---|---|---|---|
| Low | Medium | High | Low | Medium | High | |
| A: sodium alginate | 1 | 2 | 3 | −1 | 0 | +1 |
| B: HPMC K4M | 1 | 1.5 | 2 | −1 | 0 | +1 |
| Formulation | Drug: PEG Ratio | Percentage Drug Content NTB Solid Dispersion (%) * | Saturation Solubility of Solid Dispersion (μg/mL) * |
|---|---|---|---|
| Neratinib | - | - | 58.3 ± 1.82 |
| A1 | 1:1 | 96.22 ± 1.67 | 96.37 ± 1.67 |
| A2 | 1:2 | 97.70 ± 1.89 | 92.81 ± 1.53 |
| A3 | 1:3 | 96.90 ± 2.14 | 132.11 ± 2.14 |
| Formulations | pH | Drug Content * (%) | In Vitro Gelation | Floating Lag Time * (min) | Total Floating Time (h) | % Drug Release * (6 h) | % Drug Release * (12 h) |
|---|---|---|---|---|---|---|---|
| F1 | 7.2 ± 0.44 | 98.7 ± 0.52 | +++ | 2.47 ± 0.4 | >24 | 73.1 ± 0.42 | 99.89 ± 0.27 |
| F2 | 7.8 ± 0.24 | 99.3 ± 0.32 | +++ | 3.12 ± 0.2 | >12 | 65.2 ± 0.53 | 87.54 ± 0.65 |
| F3 | 7.8 ± 0.32 | 97.8 ± 0.41 | +++ | 6.27 ± 0.2 | >12 | 58.3 ± 0.21 | 84.32 ± 0.14 |
| F4 | 7.1 ± 0.21 | 97.4 ± 0.22 | +++ | 30 ± 0.8 | 1.0 | 70.2 ± 0.02 | 84.33 ± 0.17 |
| F5 | 7.4 ± 0.52 | 98.8 ± 0.16 | +++ | 42 ± 0.5 | >12 | 45.6 ± 0.62 | 74.31 ± 0.02 |
| F6 | 7.3 ± 0.12 | 99.2 ± 0.51 | +++ | 49 ± 0.4 | >12 | 30.2 ± 0.76 | 55.44 ± 0.87 |
| F7 | 7.1 ± 0.52 | 97.8 ± 0.46 | +++ | 74 ± 0.6 | <3 | 42.3 ± 0.29 | 69.91 ± 0.54 |
| F8 | 7.2 ± 0.52 | 98.4 ± 0.31 | +++ | 86 ± 0.2 | <3 | 34.2 ± 0.71 | 59.16 ± 0.22 |
| F9 | 7.2 ± 0.52 | 97.7 ± 0.61 | +++ | 89 ± 0.7 | <3 | 29.4 ± 0.63 | 50.73 ± 0.87 |
| Formulation | Zero Order | Hix Crow | Higuchi Matrix | 1st Order | Korsmeyer–Peppas | Mechanism of Drug Release | Release Kinetic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 | K | R2 | K | R2 | K | R2 | K | R2 | K | n | |||
| F1 | 0.994 | 10.845 | 0.968 | 25.480 | 0.979 | 13.179 | 0.971 | 11.194 | 0.982 | 10.052 | 0.385 | fickian | Zero order |
| F2 | 0.918 | 10.539 | 0.973 | 15.678 | 0.871 | 12.802 | 0.945 | 11.986 | 0.996 | 12.983 | 0.417 | fickian | Peppas release |
| F3 | 0.974 | 6.132 | 0.835 | 10.605 | 0.997 | 19.769 | 0.994 | 16.897 | 0.987 | 18.529 | 0.564 | Nonfickian | Higuchi matrix |
| F4 | 0.942 | 12.195 | 0.899 | 11.481 | 0.934 | 11.983 | 0.992 | 10.631 | 0.995 | 14.777 | 0.399 | fickian | Peppas release |
| F5 | 0.891 | 10.523 | 0.971 | 10.771 | 0.909 | 16.911 | 0.919 | 12.752 | 0.979 | 11.650 | 0.672 | Nonfickian | Peppas release |
| F6 | 0.917 | 15.225 | 0.993 | 17.232 | 0.781 | 17.668 | 0.984 | 11.981 | 0.843 | 21.811 | 0.685 | Nonfickian | Hix Crow |
| F7 | 0.932 | 13.809 | 0.789 | 10.765 | 0.927 | 21.286 | 0.912 | 10.098 | 0.998 | 16.659 | 0.391 | fickian | Peppas release |
| F8 | 0.874 | 17.220 | 0.985 | 13.723 | 0.801 | 10.096 | 0.951 | 13.231 | 0.992 | 10.526 | 0.772 | Nonfickian | Peppas release |
| F9 | 0.909 | 10.448 | 0.987 | 11.791 | 0.923 | 11.776 | 0.926 | 11.875 | 0.975 | 15.433 | 0.566 | Nonfickian | Hix Crow |
| Formulations | Variables | Responses | ||||
|---|---|---|---|---|---|---|
| A (Sodium Alginate) g | B (HPMC K4M) g | Floating Lag Time * (min) | Water Uptake at 2 h *(%) | % Drug Release * (6 h) | % Drug Release * (12 h) | |
| F1 | 1 | 1 | 2.47 ± 0.4 | 44 ± 0.76 | 73.1 ± 0.42 | 99.89 ± 0.27 |
| F2 | 2 | 1 | 3.12 ± 0.2 | 6.8 ± 0.42 | 65.2 ± 0.53 | 87.54 ± 0.65 |
| F3 | 3 | 1 | 6.27 ± 0.2 | 42 ± 0.71 | 58.3 ± 0.21 | 84.32 ± 0.14 |
| F4 | 1 | 1.5 | 30 ± 0.8 | 13 ± 0.18 | 70.2 ± 0.02 | 84.33 ± 0.17 |
| F5 | 2 | 1.5 | 42 ± 0.5 | 17.3 ± 0.22 | 45.6 ± 0.62 | 74.31 ± 0.02 |
| F6 | 3 | 1.5 | 49 ± 0.4 | 15.7 ± 0.32 | 30.2 ± 0.76 | 55.44 ± 0.87 |
| F7 | 1 | 2 | 74 ± 0.6 | 10.82 ± 0.43 | 42.3 ± 0.29 | 69.91 ± 0.54 |
| F8 | 2 | 2 | 86 ± 0.2 | 30.87 ± 0.21 | 34.2 ± 0.71 | 59.16 ± 0.22 |
| F9 | 3 | 2 | 89 ± 0.7 | 7.2 ± 0.11 | 29.4 ± 0.63 | 50.73 ± 0.87 |
| Intercept | A[1] | A[2] | B[1] | B[2] | R2 | |
|---|---|---|---|---|---|---|
| Floating lag time | +42.4289 | −6.93889 | 1.27778 | −38.4756 | −2.09556 | 0.9924 |
| p−value | 0.0530 | 0.0530 | <0.0001 | <00001 | ||
| % Water uptake at 2 h | +20.8444 | 1.75556 | −2.5444 | 10.0889 | −5.511 | 0.9111 |
| p−value | 0.059 | 0.059 | 0.0517 | 0.0517 | ||
| % Drug release at 6 h | +49.82 | −3.09 | +12.01 | +3.78 | +6.68 | 0.8977 |
| p−value | 0.0748 | 0.0748 | 0.0197 | 0.0197 | ||
| % Drug release at 12 h | +73.96 | −3.10 | +10.75 | +4.35 | +3.05 | 0.9312 |
| p−value | 0.0523 | 0.0523 | 0.0528 | 0.0528 |
| Source | b-Coefficient | Sum of Sqaure | d.f. | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|---|
| Floating Lag Time (min) | ||||||
| Model | +42.43 | 9637.8 | 4 | 2409.45 | 131.23 | 0.0002 |
| A[1] | −6.94 | 245.49 | 2 | 122.74 | 6.69 | 0.0530 |
| B[1] | −38.48 | 9392.32 | 2 | 4696.16 | 255.78 | <0.0001 |
| Residual | 73.44 | 4 | 18.36 | |||
| 9711.25 | 8 | |||||
| % Water Uptake | ||||||
| Model | +20.84 | 489.88 | 4 | 122.47 | 41.59 | 0.059 |
| A[1] | +1.76 | 30.54 | 2 | 15.27 | 5.18 | 0.095 |
| B[1] | +10.09 | 459.34 | 2 | 229.67 | 7.8 | 0.051 |
| Residual | 1177.84 | 4 | 294.46 | |||
| 1667.72 | 8 | |||||
| % Drug Release at 6 h | ||||||
| Model | +49.82 | 2058.12 | 4 | 514.53 | 8.78 | 0.0292 |
| A[1] | −3.09 | 622.67 | 2 | 311.33 | 5.31 | 0.748 |
| B[1] | +3.78 | 1435.45 | 2 | 717.72 | 12.25 | 0.0197 |
| Residual | 234.41 | 4 | 58.6 | |||
| 2292.53 | 8 | |||||
| % Drug Release at 12 h | ||||||
| Model | +73.96 | 800.58 | 4 | 200.53 | 8.78 | 0.0571 |
| A[1] | −3.10 | 551.24 | 2 | 275.33 | 5.31 | 0.852 |
| B[1] | +4.35 | 249.45 | 2 | 124.72 | 12.25 | 0.0432 |
| Residual | 1389.41 | 4 | 347 | |||
| 2189.53 | 8 | |||||
| Formulations | % Water Uptake * | ||
|---|---|---|---|
| At 30 min | At 60 min | At 120 min | |
| F1 | 7.5 ± 0.61 | 33 ± 0.49 | 44 ± 0.76 |
| F2 | 15.6 ± 0.31 | 23.5 ± 0.28 | 6.8 ± 0.42 |
| F3 | 16 ± 0.22 | 16 ± 0.12 | 42 ± 0.71 |
| F4 | 7.4 ± 0.34 | 7.5 ± 0.18 | 13 ± 0.18 |
| F5 | 0 ± 0.76 | 15.3 ± 0.08 | 17.3 ± 0.22 |
| F6 | 4.5 ± 0.28 | 14.79 ± 0.32 | 15.7 ± 0.32 |
| F7 | 0.57 ± 0.11 | 2.2 ± 0.63 | 10.82 ± 0.43 |
| F8 | 5.26 ± 0.37 | 12.5 ± 0.42 | 30.87 ± 0.21 |
| F9 | 13 ± 0.28 | 5.6 ± 0.28 | 7.2 ± 0.11 |
| Factor A | Factor B | Optimized Formulation Independent Variables | Predicted Value | Observed Value | Desirability |
|---|---|---|---|---|---|
| 3 g | 1 g | Floating lag time (min) | 9.61 | 8.91 | 0.822 |
| % Water uptake at 2 h | 31.72 | 30.96 | |||
| % Drug release at 6 h | 44.67 | 43.21 | |||
| % Drug release at 12 h | 84.32 | 86.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hani, U.; Rahamathulla, M.; Osmani, R.A.M.; Begum, M.Y.; Wahab, S.; Ghazwani, M.; Fatease, A.A.; Alamri, A.H.; Gowda, D.V.; Alqahtani, A. Development and Characterization of Oral Raft Forming In Situ Gelling System of Neratinib Anticancer Drug Using 32 Factorial Design. Polymers 2022, 14, 2520. https://doi.org/10.3390/polym14132520
Hani U, Rahamathulla M, Osmani RAM, Begum MY, Wahab S, Ghazwani M, Fatease AA, Alamri AH, Gowda DV, Alqahtani A. Development and Characterization of Oral Raft Forming In Situ Gelling System of Neratinib Anticancer Drug Using 32 Factorial Design. Polymers. 2022; 14(13):2520. https://doi.org/10.3390/polym14132520
Chicago/Turabian StyleHani, Umme, Mohamed Rahamathulla, Riyaz Ali M. Osmani, M.Yasmin Begum, Shadma Wahab, Mohammed Ghazwani, Adel Al Fatease, Ali H. Alamri, Devegowda V. Gowda, and Ali Alqahtani. 2022. "Development and Characterization of Oral Raft Forming In Situ Gelling System of Neratinib Anticancer Drug Using 32 Factorial Design" Polymers 14, no. 13: 2520. https://doi.org/10.3390/polym14132520
APA StyleHani, U., Rahamathulla, M., Osmani, R. A. M., Begum, M. Y., Wahab, S., Ghazwani, M., Fatease, A. A., Alamri, A. H., Gowda, D. V., & Alqahtani, A. (2022). Development and Characterization of Oral Raft Forming In Situ Gelling System of Neratinib Anticancer Drug Using 32 Factorial Design. Polymers, 14(13), 2520. https://doi.org/10.3390/polym14132520







