Chitosan Microparticles Loaded with New Non-Cytotoxic Isoniazid Derivatives for the Treatment of Tuberculosis: In Vitro and In Vivo Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Structural Confirmation of Isoniazid Derivatives
2.2.2. Preparation of Chitosan Microparticles Loaded with Isoniazid Derivatives
2.2.3. Microscopic Characterization of the Obtained Microparticles
2.2.4. Loading Efficiency (LE)
2.2.5. Assessment of In Vitro Biodegradation Capacity
2.2.6. Evaluation of In Vitro Biocompatibility Using MTT Cell Viability Analysis
2.2.7. Biological Evaluation
In Vivo Toxicological Screening: The Determination of Chronic Toxicity
- 17.52 mg/kg body weight for isoniazid (INH) in Group 1;
- 35.234 mg/kg body weight for INH-a in Group 2;
- 177.88 mg/kg body weight for INH-b in Group 3;
- 125.15 mg/kg body weight for INH-c in Group 4.
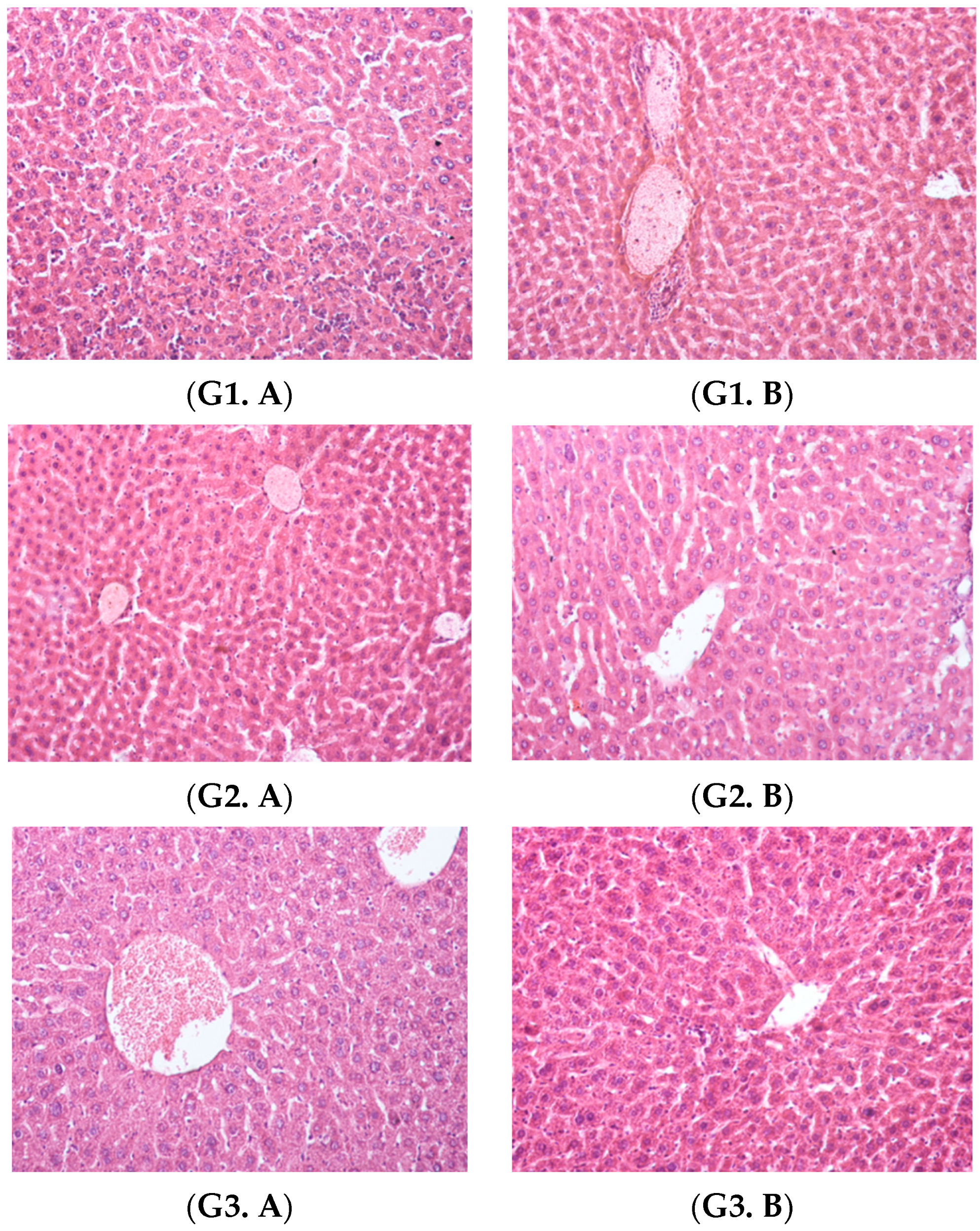
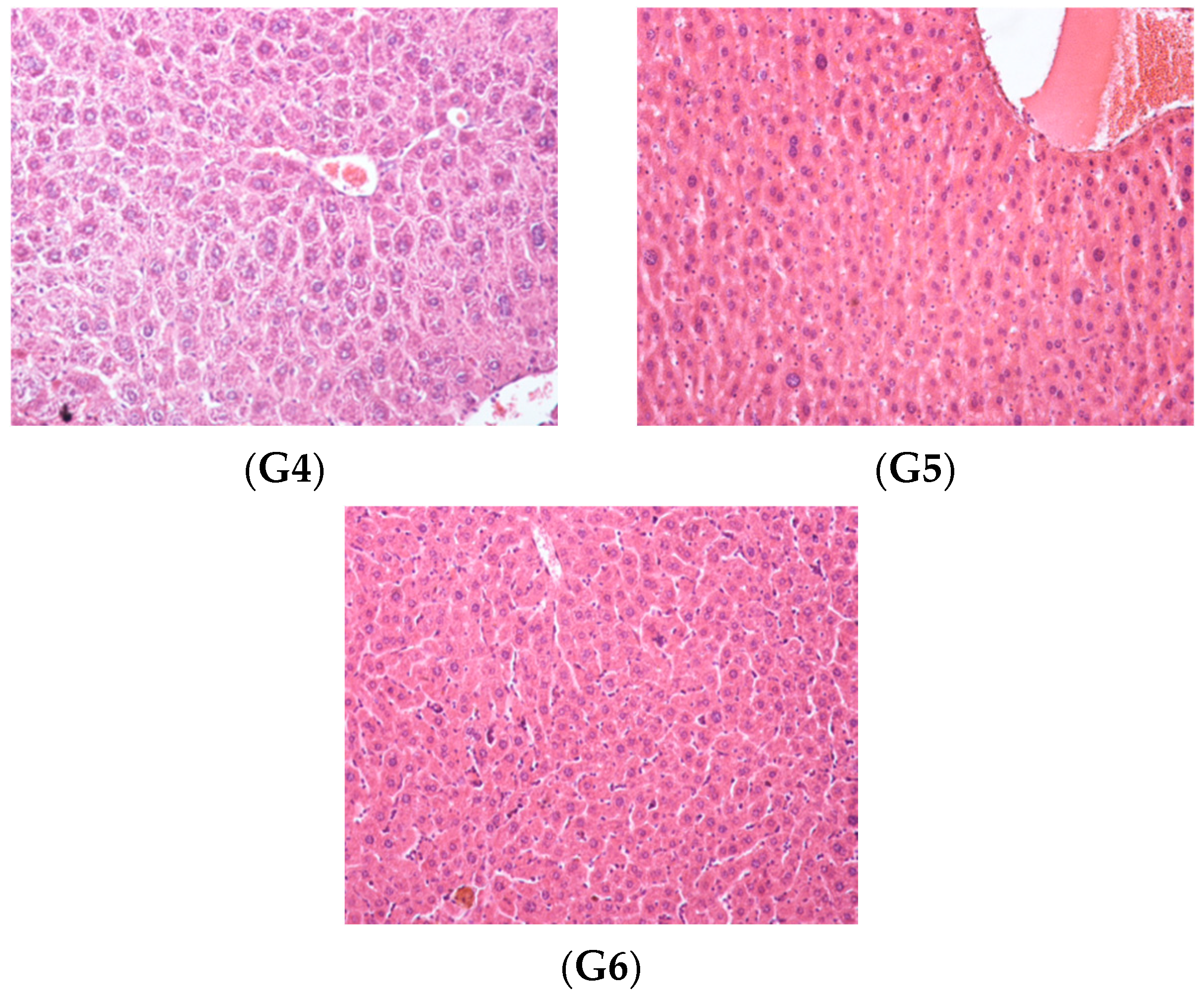
Histopathological Examination
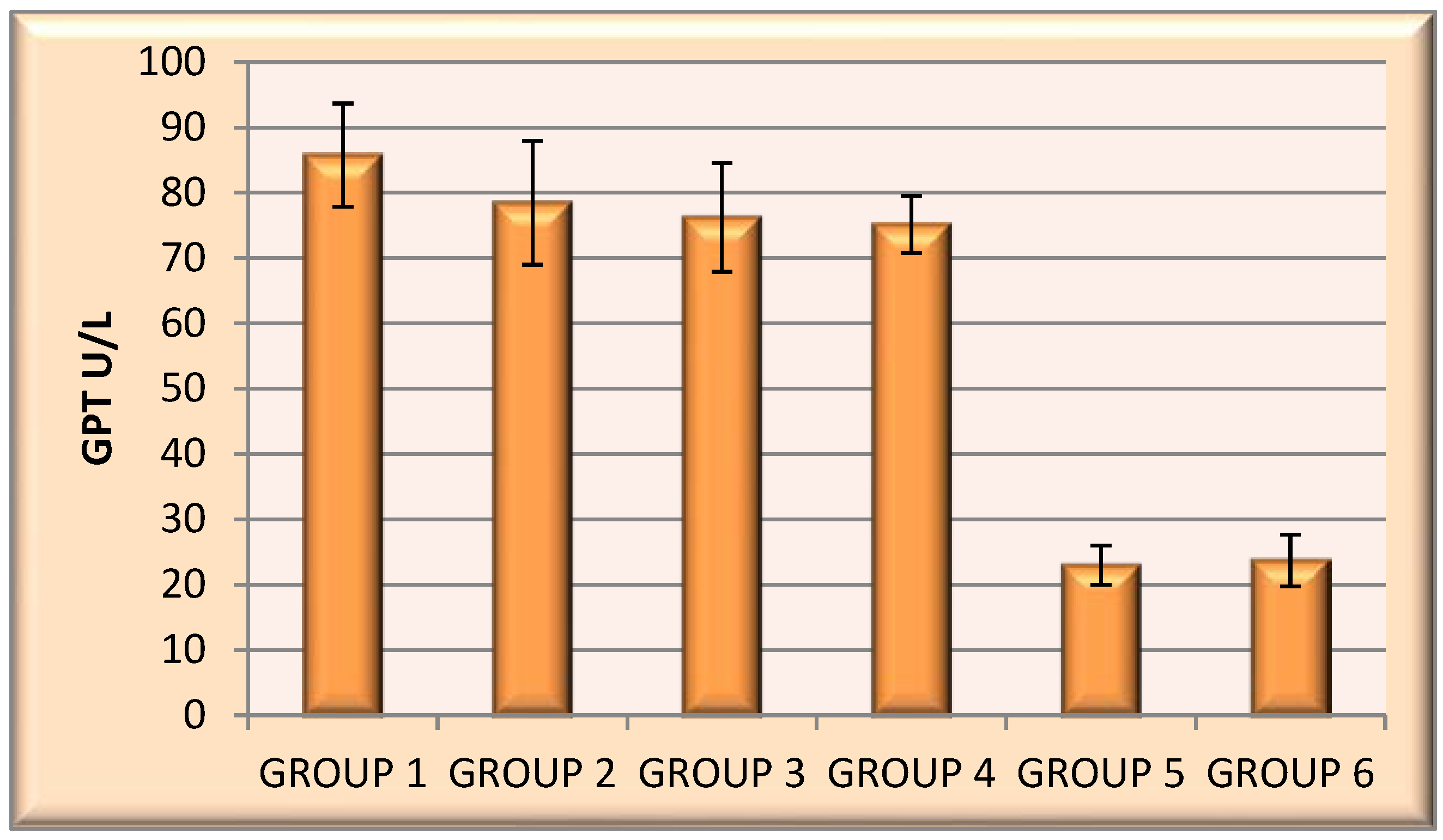
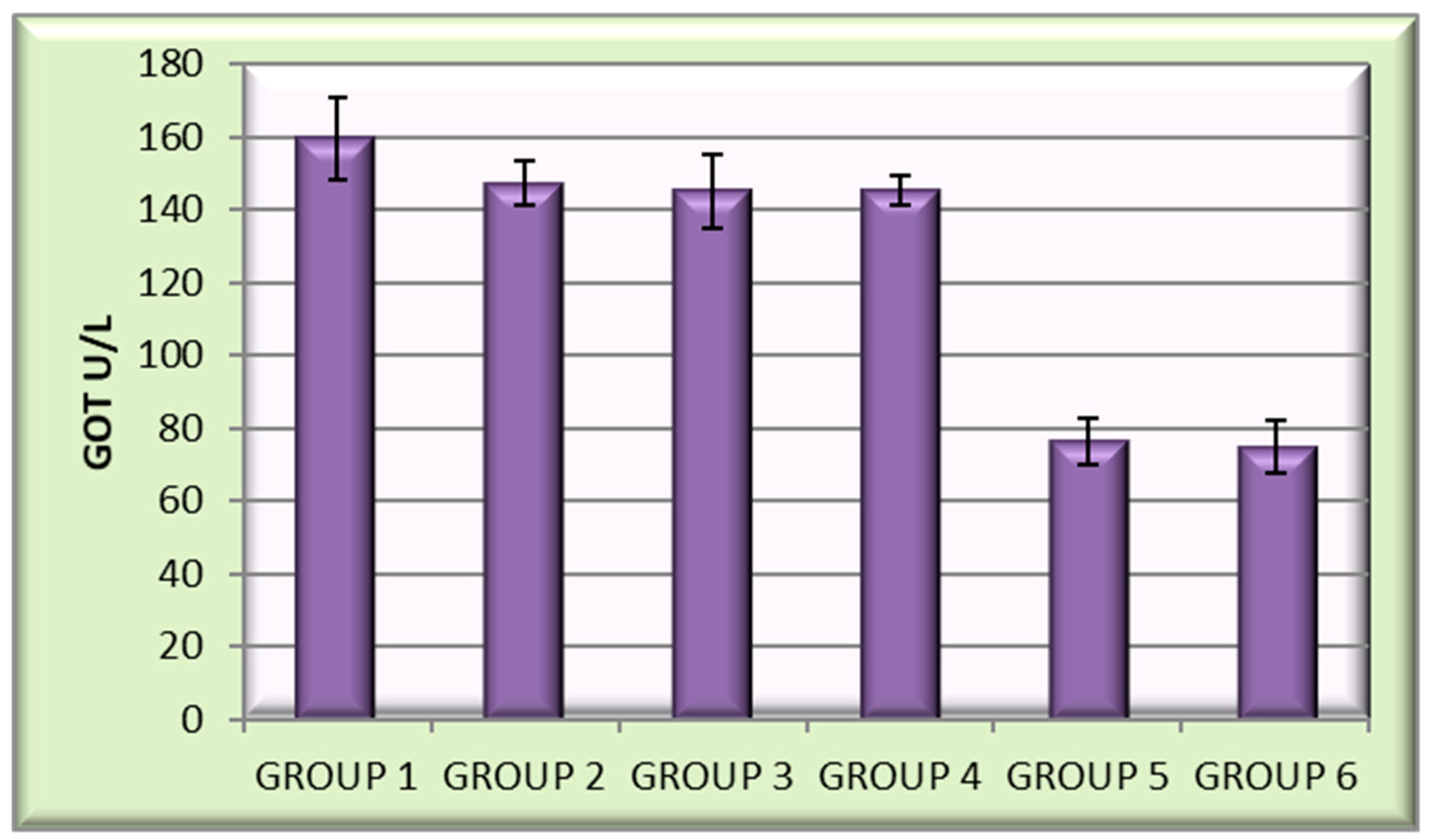
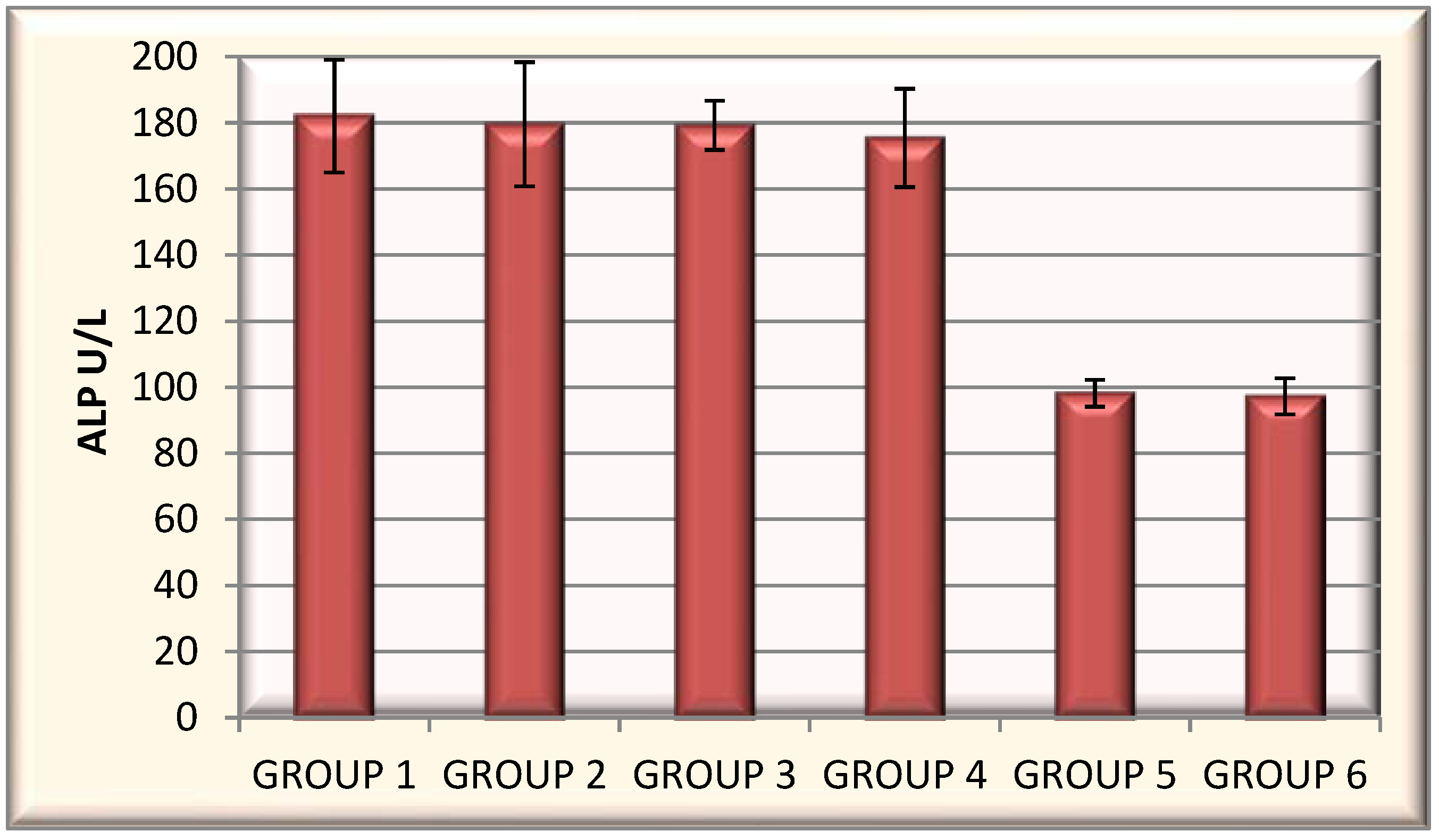
Evaluation of Biochemical Parameters
2.2.8. Statistical Analysis
3. Results
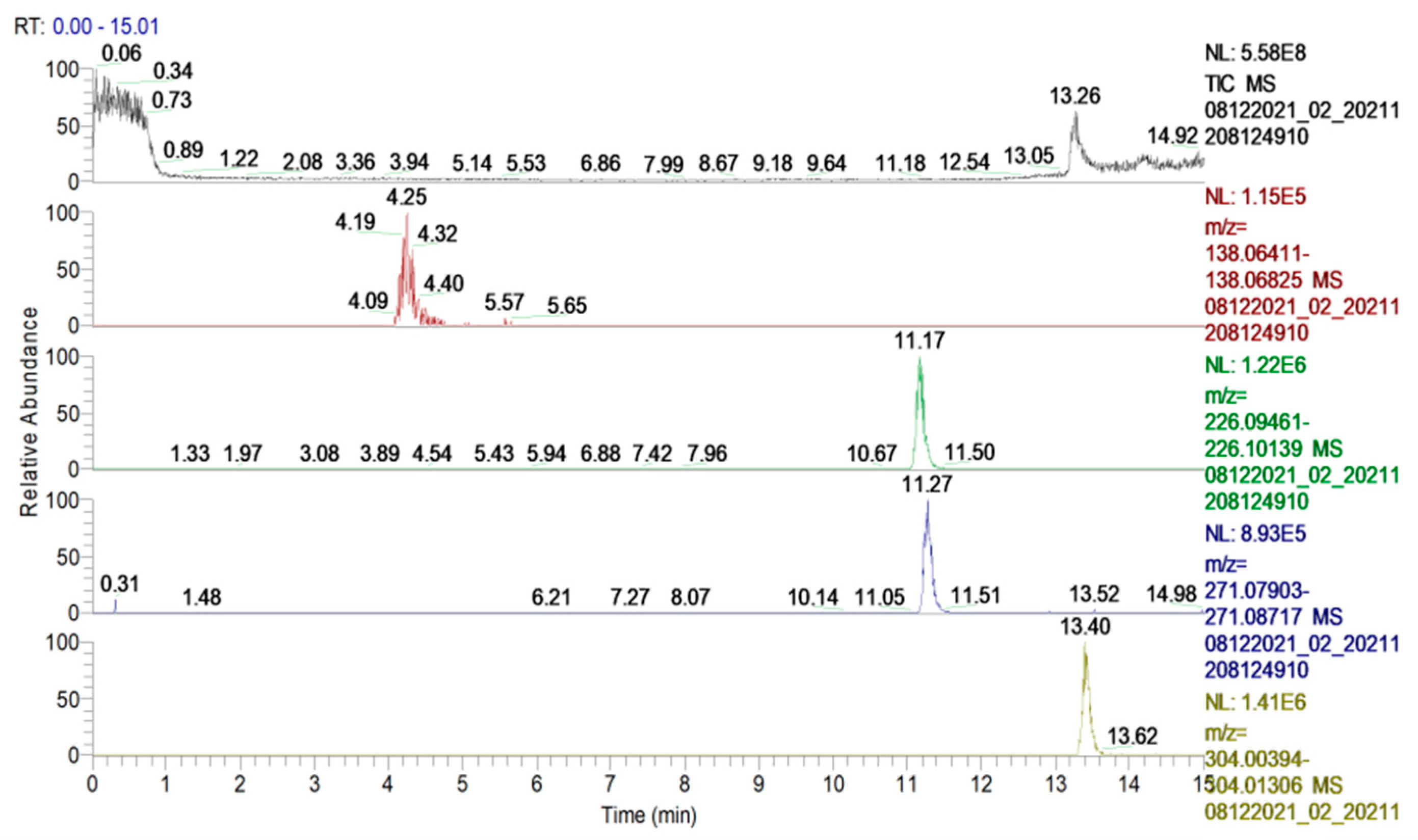
3.1. Mass Spectrometric Structural Confirmation of the Active Compounds
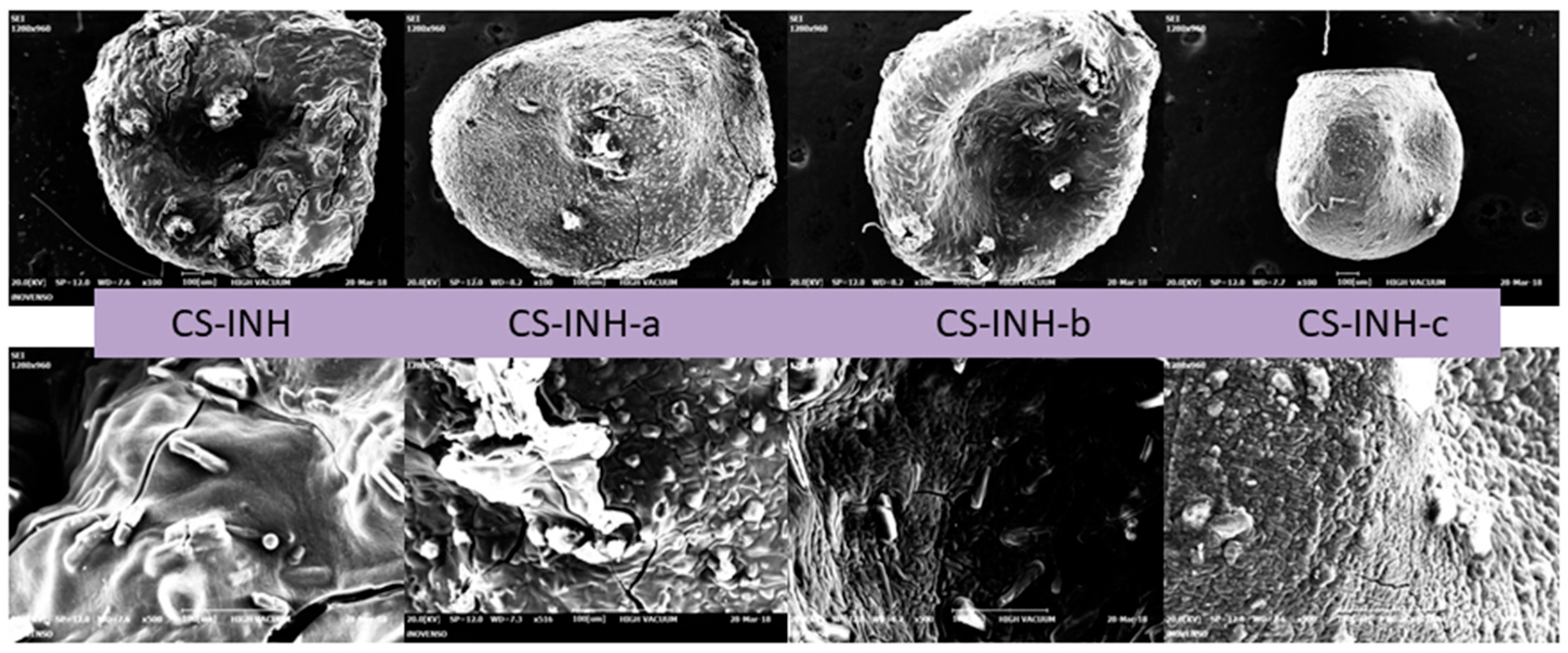
3.2. Macroscopic and Microscopic Characterization of the Obtained Microparticles
3.3. Loading Efficiency (LE)
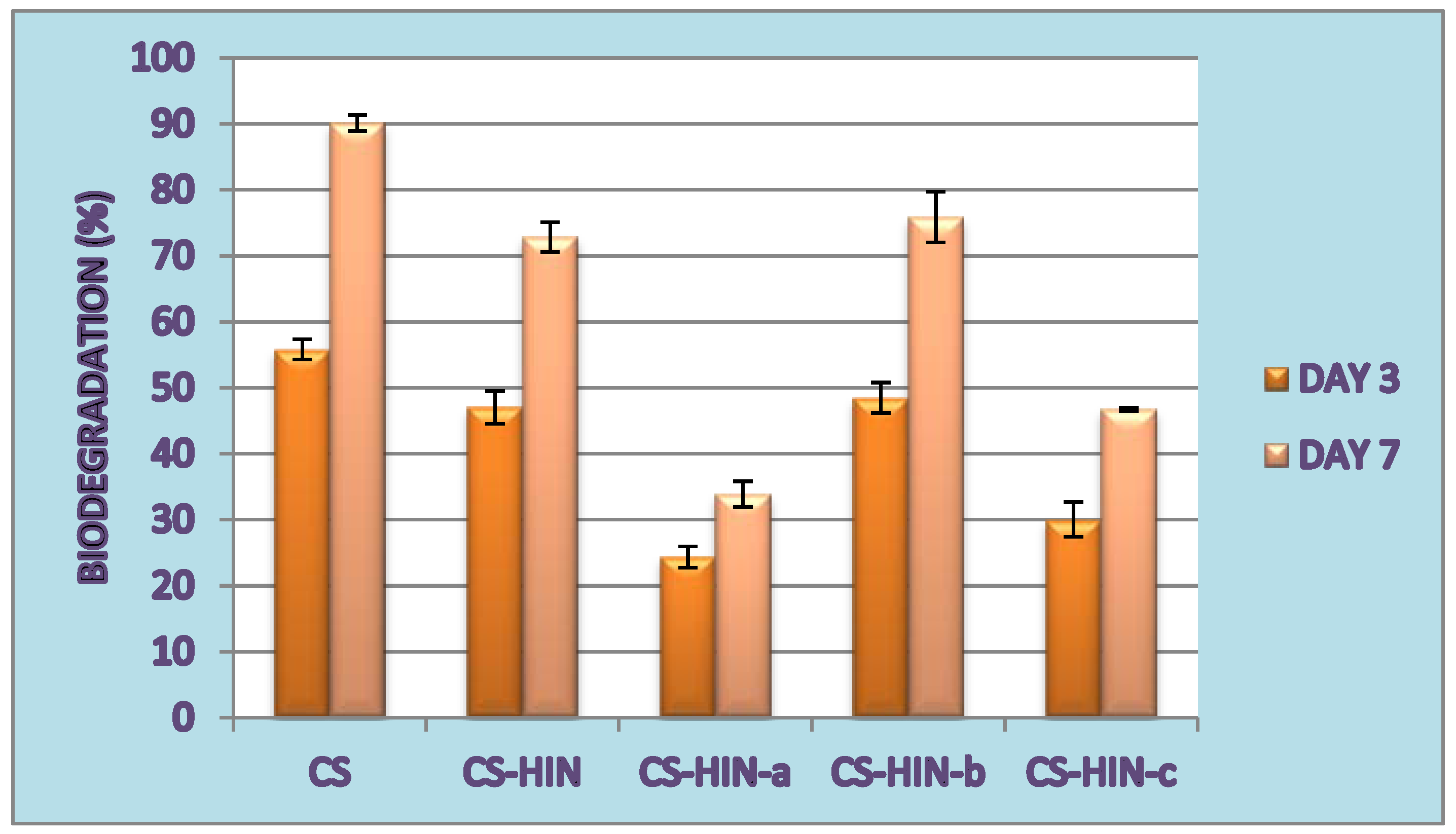
3.4. In Vitro Biodegradation Capacity
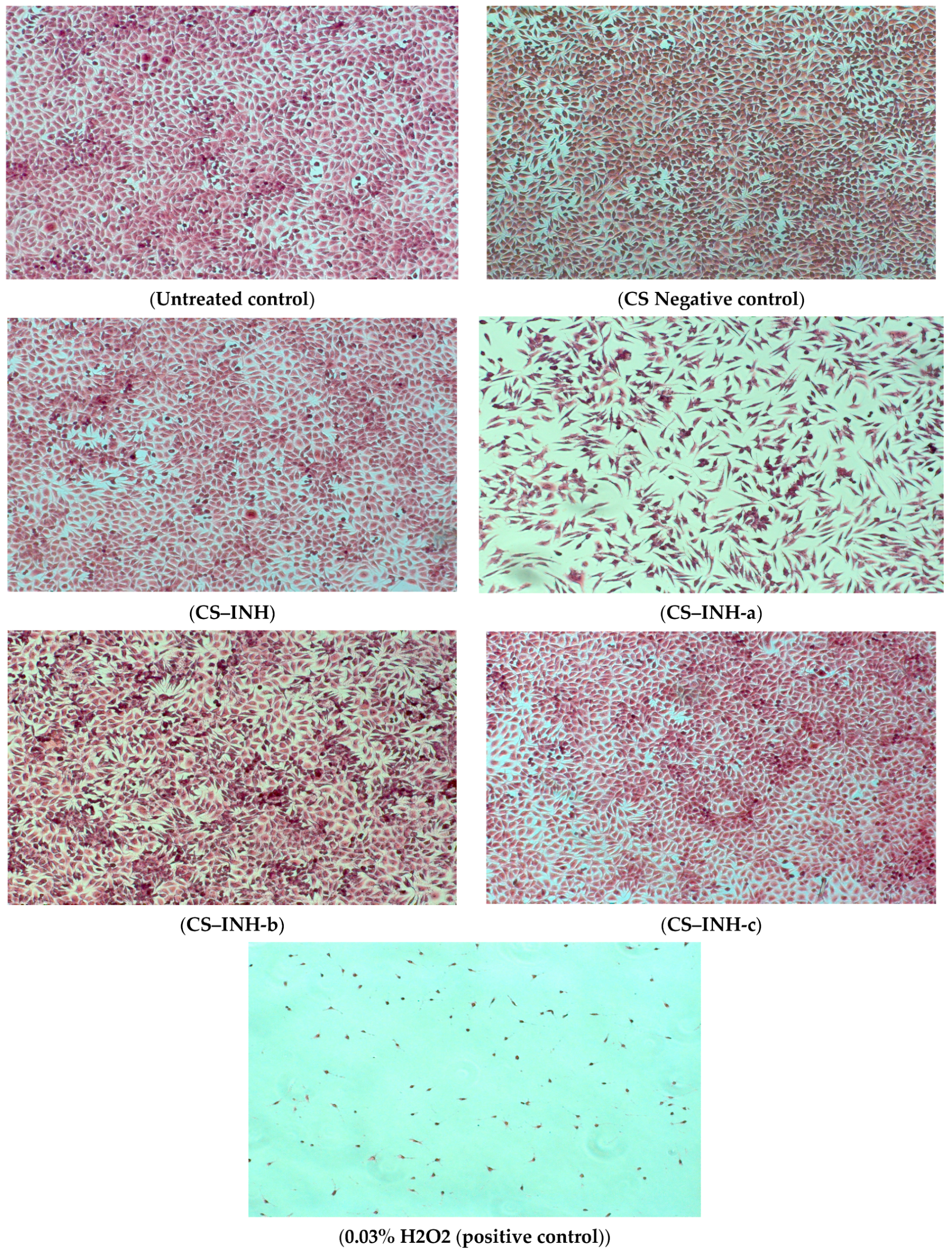
3.5. In Vitro Biocompatibility Using MTT Cell Viability Analysis
3.6. Biological Evaluation
3.6.1. In Vivo Toxicological Screening: The Determination of Chronic Toxicity
3.6.2. Evaluation of Biochemical Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dragostin, I.; Dragostin, O.M.; Samal, S.K.; Dash, S.; Tatia, R.; Dragan, M.; Confederat, L.; Ghiciuc, C.M.; Diculencu, D.; Lupușoru, C.E.; et al. New isoniazid derivatives with improved pharmaco-toxicological profile: Obtaining, characterization and biological evaluation. Eur. J. Pharm. Sci. 2019, 137, 104974. [Google Scholar] [CrossRef] [PubMed]
- Dragostin, I.; Dragostin, O.; Pelin, A.-M.; Grigore, C.; Zamfir, C.L. The importance of polymers for encapsulation process and for enhanced cellular functions. J. Macromol. Sci.—Pure Appl. Chem. 2017, 54, 489–493. [Google Scholar] [CrossRef]
- Baltrusch, K.L.; Torres, M.D.; Domínguez, H.; Florez-Fernandez, N. Spray-drying microencapsulation of tea extracts using green starch, alginate or carrageenan as carrier materials. Int. J. Biol. Macromol. 2022, 203, 417–429. [Google Scholar] [CrossRef]
- Thuekeaw, S.; Angkanaporn, K.; Chirachanchai, S.; Nuengjamnong, C. Dual pH responsive via double—Layered microencapsulation for controlled release of active ingredients in simulated gastrointestinal tract: A model case of chitosan-alginate microcapsules containing basil oil (Ocimum basilicum Linn.). Polym. Degrad. Stab. 2021, 191, 109660. [Google Scholar] [CrossRef]
- Annunziata, G.; Jiménez-García, M.; Capó, X.; Moranta, D.; Arnone, A.; Tenore, G.C.; Sureda, A.; Tejada, S. Microencapsulation as a tool to counteract the typical low bioavailability of polyphenols in the management of diabetes. Food Chem. Toxicol. 2020, 139, 111248. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Xia, W. Preparation, characterization and antibacterial activity of water-soluble O-fumaryl-chitosan. Carbohydr. Polym. 2011, 83, 1169–1173. [Google Scholar] [CrossRef]
- Kong, M.; Chen, X.G.; Xing, K.; Park, H.J. Antimicrobial properties of chitosan and mode of action: A state of the art review. Int. J. Food Microbiol. 2010, 144, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Dragostin, O.M.; Samal, S.K.; Lupascu, F.; Pânzariu, A.; Dubruel, P.; Lupascu, D.; Tuchilus, C.; Vasile, C.; Profire, L. Development and Characterization of Novel Films Based on Sulfonamide-Chitosan Derivatives for Potential Wound Dressing. Int. J. Mol. Sci. 2015, 16, 29843–29855. [Google Scholar] [CrossRef]
- Lupascu, F.G.; Dash, M.; Samal, S.K.; Dubruel, P.; Lupusoru, C.E.; Lupusoru, R.V.; Dragostin, O.; Profire, L. Development, optimization and biological evaluation of chitosan scaffold formulations of new xanthine derivatives for treatment of type-2 diabetes mellitus. Eur. J. Pharm. Sci. 2015, 77, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Garcia, L.G.S.; da Rocha, M.G.; Lima, L.R.; Cunha, A.P.; de Oliveira, J.S.; de Andrade, A.R.C.; Ricardo, N.M.P.S.; Pereira-Neto, W.A.; Sidrim, J.J.C.; Rocha, M.F.G.; et al. Essential oils encapsulated in chitosan microparticles against Candida albicans biofilms. Int. J. Biol. Macromol. 2021, 166, 621–632. [Google Scholar] [CrossRef]
- Punarvasu, T.P.; Prashanth, K.V.H. Self-assembled chitosan derived microparticles inhibit tumor angiogenesis and induce apoptosis in Ehrlich-ascites-tumor bearing mice. Carbohydr. Polym. 2022, 278, 118941. [Google Scholar] [CrossRef]
- Dragostin, O.M.; Tatia, R.; Samal, S.K.; Oancea, A.; Zamfir, A.S.; Dragostin, I.; Lisa, E.-L.; Apetrei, C.; Zamfir, C.L. Designing of Chitosan Derivatives Nanoparticles with Antiangiogenic Efect for Cancer Therapy. Nanomaterials 2020, 10, 698. [Google Scholar] [CrossRef]
- Bai, J.; Zhanga, Y.; Chen, L.; Yan, H.; Zhang, C.; Liu, L.; Xu, X. Synthesis and characterization of paclitaxel-imprinted microparticles for controlled release of an anticancer drug. Mater. Sci. Eng. C 2018, 92, 338–348. [Google Scholar] [CrossRef]
- Dragostin, O.M.; Samal, S.K.; Dash, M.; Lupascu, F.; Pânzariu, A.; Tuchilus, C.; Ghetu, N.; Danciu, M.; Dubruel, P.; Pieptu, D.; et al. New antimicrobial chitosan derivatives for wound dressing applications. Carbohydr. Polym. 2016, 141, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Batir-Marin, D.; Mircea, C.; Boev, M.; Burlec, A.F.; Corciova, A.; Fifere, A.; Iacobescu, A.; Cioanca, O.; Verestiuc, L.; Hancianu, M. In Vitro Antioxidant, Antitumor and Photocatalytic Activities of Silver Nanoparticles Synthesized Using Equisetum Species: A Green Approach. Molecules 2021, 26, 7325. [Google Scholar] [CrossRef]
- Avwioro, G. Histochemical Uses of Haematoxylin—A Review Godwin Avwioro. J. Phys. Conf. Ser. 2011, 1, 24–34. [Google Scholar]
- Mogoanta, L. Ghid de Tehnici de Histologie si Imunohistochimie; Medicala Universitara: Craiova, Romania, 2007. [Google Scholar]
- Géhin, C.; Holman, S.W. Advances in high-resolution mass spectrometry applied to pharmaceuticals in 2020: A whole new age of information. Anal. Sci. Adv. 2021, 2, 142–156. [Google Scholar] [CrossRef]
- Morariu, D.I.; Avasilcăi, L.; Vieriu, M.; Lungu, I.I.; Morariu, B.; Robu, S.; Tiutunaru, D.; Cioancă, O.; Hăncianu, M. Estimation of Quinolones, Ceftiofur and Thiamphenicol Residues Levels In Honey. Farmacia 2021, 69, 3. [Google Scholar] [CrossRef]
- Floros, D.J.; Petras, D.; Kapono, C.A.; Melnik, A.V.; Ling, T.J.; Knight, R. Mass spectrometry based molecular 3D-cartography of plant metabolites. Front. Plant Sci. 2017, 8, 429. [Google Scholar] [CrossRef]
- Carrano, L.; Naggi, A.; Urso, E. High Resolution Mass Spectrometry for the Recognition and Structural Characterization of a New Antimicrobial Compound. Pharmacol. Pharm. 2018, 9, 135. [Google Scholar] [CrossRef][Green Version]
- Daly, A.K.; Day, C.P. Genetic association studies in drug-induced liver injury. Drug Metab. Rev. 2012, 44, 116–126. [Google Scholar] [CrossRef]
- Matei, L.; Bleotu, C.; Baciu, I.; Draghici, C.; Ionita, P.; Paun, A.; Chifiriuc, M.C.; Sbarcea, A.; Zarafu, I. Synthesis and bioevaluation of some new isoniazid derivatives. Bioorg. Med. Chem. 2013, 21, 5355–5361. [Google Scholar] [CrossRef]
- Hu, Y.-Q.; Zhang, S.; Zhao, F.; Gao, C.; Feng, L.-S.; Lv, Z.-S.; Xu, Z.; Wu, X. Isoniazid derivatives and their anti-tubercular activity. Eur. J. Med. Chem. 2017, 133, 255–267. [Google Scholar] [CrossRef]
- Jahromi, H.K.; Pourahmad, M.; Abedi, H.A.; Karimi, M.; Jahromi, Z.K. Protective effects of salep against isoniazid liver toxicity in wistar rats. J. Tradit. Complement Med. 2017, 8, 239–240. [Google Scholar] [CrossRef]
- Panchal, R.; Patel, H.; Patel, V.; Joshi, P.; Parikh, A. Formulation and evalution of montelukast sodium—Chitosan based spray dried microspheres for pulmonary drug delivery. J. Pharm. Bioallied Sci. 2012, 4, S110–S111. [Google Scholar] [CrossRef] [PubMed]
- Pham, D.-D.; Fattal, E.; Tsapis, N. Pulmonary drug delivery systems for tuberculosis treatment. Int. J. Pharm. 2015, 478, 517–529. [Google Scholar] [CrossRef]
- Ranganathan, P.; Mutharani, B.; Chen, S.-M.; Sireesha, P. Biocompatible chitosan-pectin polyelectrolyte complex for simultaneous electrochemical determination of metronidazole and metribuzin. Carbohydr. Polym. 2019, 214, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Muttil, P.; Yadav, A.B.; Rath, S.K.; Bajpai, V.K.; Mani, U.; Misra, A. Uptake of inhalable microparticles affects defence responses of macrophages infected with Mycobacterium tuberculosis H37Ra. J. Antimicrob. Chemother. 2007, 59, 499–506. [Google Scholar] [CrossRef]
- Liu, S.; Qin, S.; He, M.; Zhou, D.; Qin, Q.; Wang, H. Current applications of poly (lactic acid) composites in tissue engineering and drug delivery. Compos. Part B 2020, 199, 108238. [Google Scholar] [CrossRef]
- O’Connora, G.; Krishnane, N.; Fagan-Murphy, A.; Cassidy, J.; O’Learyd, S.; Robertsone, B.D.; Keaned, J.; O’Sullivand, M.P.; Cryan, S.-A. Inhalable poly (lactic-co-glycolic acid) (PLGA) microparticles encapsulating all-trans-Retinoic acid (ATRA) as a host-directed, adjunctive treatment for Mycobacterium tuberculosis infection. Eur. J. Pharm. Biopharm. 2019, 134, 153–165. [Google Scholar] [CrossRef]
- Mukhtar, M.; Szakonyi, Z.; ´Farkas, A.; Burian, K.; Kokai, D.; Ambrus, R. Freeze-dried vs spray-dried nanoplex DPIs based on chitosan and its derivatives conjugated with hyaluronic acid for tuberculosis: In vitro aerodynamic and in silico deposition profiles. Eur. Polym. J. 2021, 160, 110775. [Google Scholar] [CrossRef]
- Pandey, R.P.; Kumar, S.; Ahmad, S.; Vibhuti, A.; Raj, V.S.; Verma, A.K.; Sharma, P.; Leal, E. Use Chou’s 5-steps rule to evaluate protective efficacy induced by antigenic proteins of Mycobacterium tuberculosis encapsulated in chitosan nanoparticles. Life Sci. 2020, 256, 117961. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Aziz, M.M.; Abu Elella, M.H.; Mohamed, R.R. Green synthesis of quaternized chitosan/silver nanocomposites for targeting Mycobacterium tuberculosis and lung carcinoma cells (A-549). Int. J. Biol. Macromol. 2020, 142, 244–253. [Google Scholar] [CrossRef]
- Bhat, A.R.; Wani, F.A.; Behera, K.; Khan, A.B.; Patel, R. Formulation of biocompatible microemulsions for encapsulation of anti-TB drug rifampicin: A physicochemical and spectroscopic study. Colloids Surf. A Physicochem. Eng. Asp. 2022, 645, 128846. [Google Scholar] [CrossRef]
- Manning, T.; Mikula, R.; Lee, H.; Calvin, A.; Darrah, J.; Wylie, G.; Phillips, D.; Bythell, B.J. The copper (II) ion as a carrier for the antibiotic capreomycin against Mycobacterium tuberculosis. Bioorg. Med. Chem. Lett. 2014, 24, 976–982. [Google Scholar] [CrossRef]
- Abdelghany, S.; Parumasivam, T.; Pang, A.; Roediger, B.; Tang, P.; Jahn, K.; Britton, W.J.; Chan, H.-K. Alginate modified-PLGA nanoparticles entrapping amikacin and moxifloxacin as a novel host-directed therapy for multidrug-resistant tuberculosis. J. Drug Deliv. Sci. Technol. 2019, 52, 642–651. [Google Scholar] [CrossRef]
- Suarez, S.; O’Hara, P.; Kazantseva, M.; Newcomer, C.E.; Hopfer, R.; McMurray, D.N.; Hickey, A.J. Airways delivery of rifampicin microparticles for the treatment of tuberculosis. J. Antimicrob. Chemother. 2001, 48, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Kundawala, A.J. Treating tuberculosis with chitosan microparticles loaded with rifampicin as respirable powder for pulmonary delivery. Indian J. Nov. Drug Deliv. 2012, 4, 57–65. [Google Scholar]
- Zhao, X.-H.; Qian, L.; Yin, D.-L.; Zhou, Y. Hypolipidemic effect of the polysaccharides extracted from pumpkin by cellulase-assisted method on mice. Int. J. Biol. Macromol. 2014, 64, 137–138. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.; Zhang, J.; Mi, Y.; Dong, F.; Li, Q.; Guo, Z. Synthesis, characterization, and evaluation of antifungal and antioxidant properties of cationic chitosan derivative via azide-alkyne click reaction. Int. J. Biol. Macromol. 2018, 120, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Afonso, C.R.; Hirano, R.S.; Gaspar, A.L.; Chagas, E.G.L.; Carvalho, R.A.; Silva, F.V.; Leonardi, G.R.; Lopes, P.S.; Silva, C.F.; Yoshida, C.M.P. Biodegradable antioxidant chitosan films useful as an anti-aging skin mask. Int. J. Biol. Macromol. 2019, 132, 1262–1273. [Google Scholar] [CrossRef] [PubMed]
- Yingjun, J.; Jianghao, H.; Xueqing, X. Maintenance of the antioxidant capacity of fresh-cut pineapple by procyanidin-grafted chitosan. Postharvest Biol. Technol. 2019, 154, 79–86. [Google Scholar]
- Savic, I.M.; Savic Gajic, I.M.; Milovanovic, M.G.; Zerajic, S.; Gajic, D.G. Optimization of Ultrasound-Assisted Extraction and Encapsulation of Antioxidants from Orange Peels in Alginate-Chitosan Microparticles. Antioxidants 2022, 11, 297. [Google Scholar] [CrossRef]
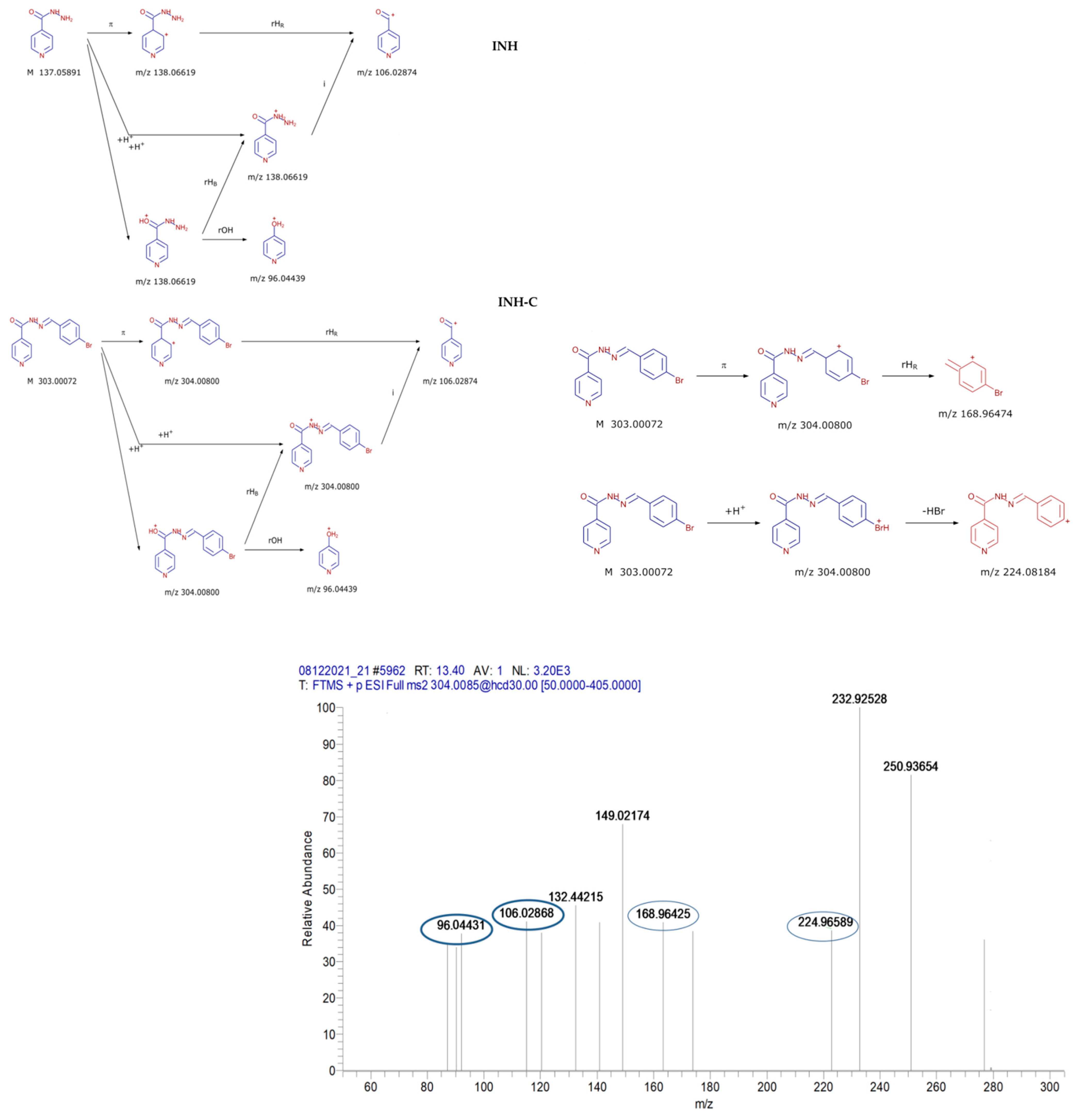


| Compound | R.T. (min) | Formula | Exact Mass | Error (ppm) | Adduct Ion (m/z) | MS2 Fragments (m/z) |
|---|---|---|---|---|---|---|
| INH | 4.25 | C6H7N3O | 137.0589 | 1.47 | 138.0667 | 122.0712; 120.0556; 108.04429; 106.0287; 96.0443; 59.0239 |
| INH-a | 11.17 | C13H11N3O | 225.0902 | 1.25 | 226.0980 | 208.08692; 148.0505; 147.05527; 106.0287; 96.0443 |
| INH-b | 11.27 | C13H10N4O3 | 270.0753 | 0.86 | 271.0831 | 255.0876; 253.0720; 224.0818; 192.0430; 148.0505; 136.0393; 106.0287; 96.0443 |
| INH-c | 13.40 | C13H10N3OBr | 303.0007 | 0.5 | 304.0085 | 288.0130; 285.9974;224.9658; 224.0818; 168.9647; 148.0505; 106.0287; 96.0443 |
| Compound | C0 (mg/mL) | C1 (mg/mL) | LE (%), n = 3 |
|---|---|---|---|
| CS–INH | 5 | 0.282 | 94.36 ± 0.7 |
| CS–INH-a | 5 | 0.52 | 89.60 ± 0.9 |
| CS–INH-b | 5 | 0.39 | 92.17 ± 0.8 |
| CS–INH-c | 5 | 0.45 | 90.89 ± 0.7 |
| Samples | Cell Viability 24 h | (%) 48 h | 72 h |
|---|---|---|---|
| CS–INH-a | 83.92 ± 0.7 | 71.08 ± 0.9 | 63.99 ± 0.6 |
| CS–INH-b | 106.54 ± 0.9 | 99.09 ± 1.2 | 89.64 ± 0.8 |
| CS–INH-c | 94.96 ± 0.5 | 80.22 ± 0.9 | 94.14 ± 0.7 |
| CS–INH | 100.27 ± 1.1 | 98.37 ± 0.7 | 95.53 ± 0.9 |
| CS (Negative Control) | 98.23 ± 0.8 | 90.92 ± 0.4 | 97.10 ± 0.6 |
| H2O2 0.03% (Positive Control) | 11.99 ± 0.8 | 5.02 ± 0.5 | 2.90 ± 1.4 |
| Untreated Control | 100.00 | 100.00 | 100.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dragostin, I.; Dragostin, O.-M.; Iacob, A.T.; Dragan, M.; Chitescu, C.L.; Confederat, L.; Zamfir, A.-S.; Tatia, R.; Stan, C.D.; Zamfir, C.L. Chitosan Microparticles Loaded with New Non-Cytotoxic Isoniazid Derivatives for the Treatment of Tuberculosis: In Vitro and In Vivo Studies. Polymers 2022, 14, 2310. https://doi.org/10.3390/polym14122310
Dragostin I, Dragostin O-M, Iacob AT, Dragan M, Chitescu CL, Confederat L, Zamfir A-S, Tatia R, Stan CD, Zamfir CL. Chitosan Microparticles Loaded with New Non-Cytotoxic Isoniazid Derivatives for the Treatment of Tuberculosis: In Vitro and In Vivo Studies. Polymers. 2022; 14(12):2310. https://doi.org/10.3390/polym14122310
Chicago/Turabian StyleDragostin, Ionut, Oana-Maria Dragostin, Andreea Teodora Iacob, Maria Dragan, Carmen Lidia Chitescu, Luminita Confederat, Alexandra-Simona Zamfir, Rodica Tatia, Catalina Daniela Stan, and Carmen Lacramioara Zamfir. 2022. "Chitosan Microparticles Loaded with New Non-Cytotoxic Isoniazid Derivatives for the Treatment of Tuberculosis: In Vitro and In Vivo Studies" Polymers 14, no. 12: 2310. https://doi.org/10.3390/polym14122310
APA StyleDragostin, I., Dragostin, O.-M., Iacob, A. T., Dragan, M., Chitescu, C. L., Confederat, L., Zamfir, A.-S., Tatia, R., Stan, C. D., & Zamfir, C. L. (2022). Chitosan Microparticles Loaded with New Non-Cytotoxic Isoniazid Derivatives for the Treatment of Tuberculosis: In Vitro and In Vivo Studies. Polymers, 14(12), 2310. https://doi.org/10.3390/polym14122310







