Contact Lenses as Ophthalmic Drug Delivery Systems: A Review
Abstract
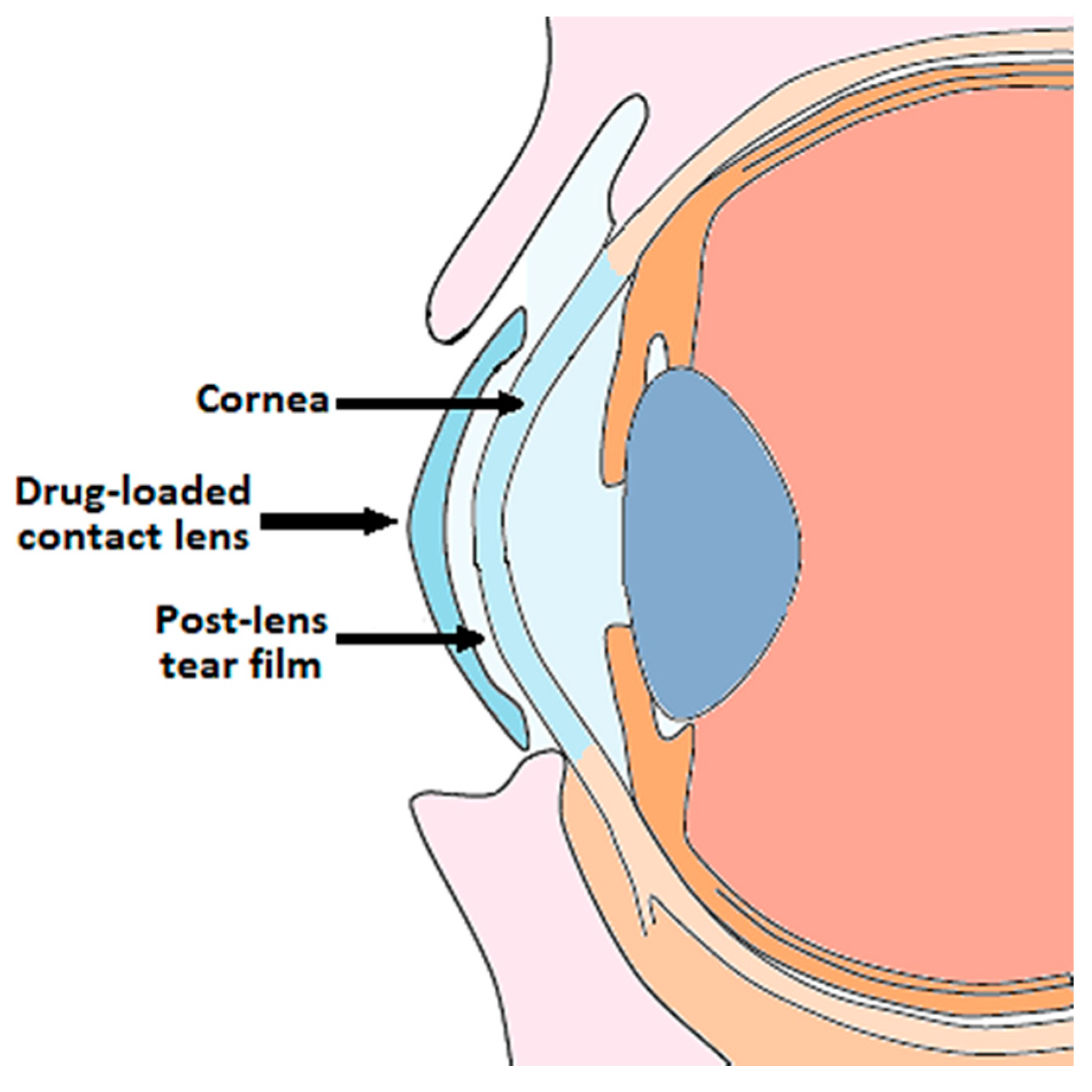
1. Introduction
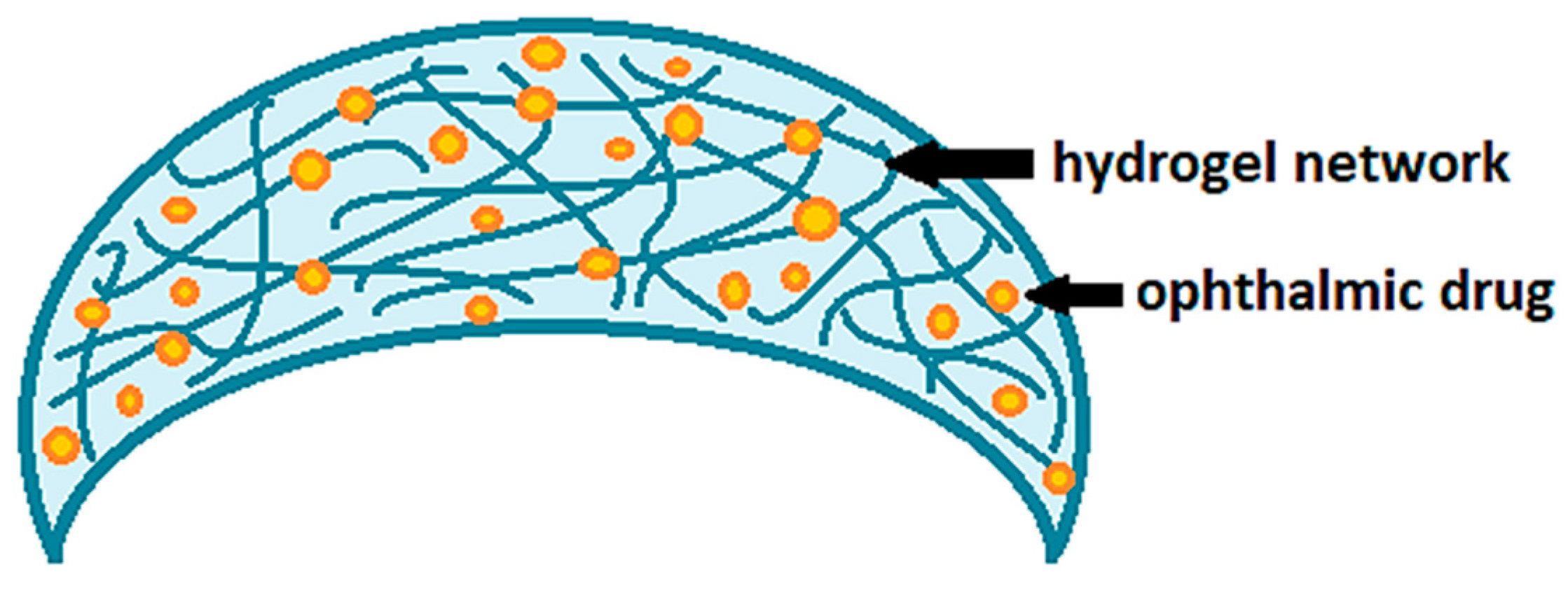
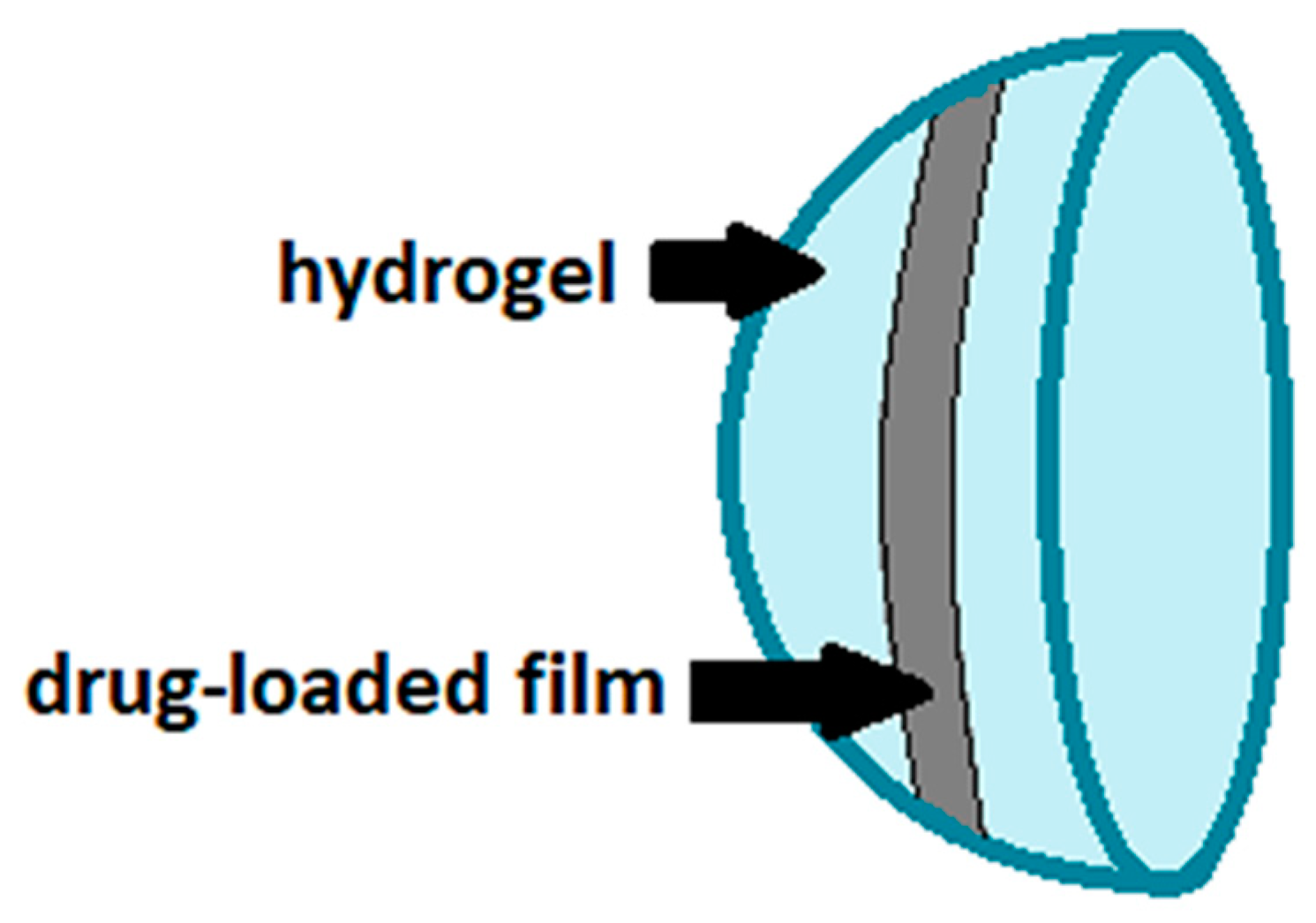
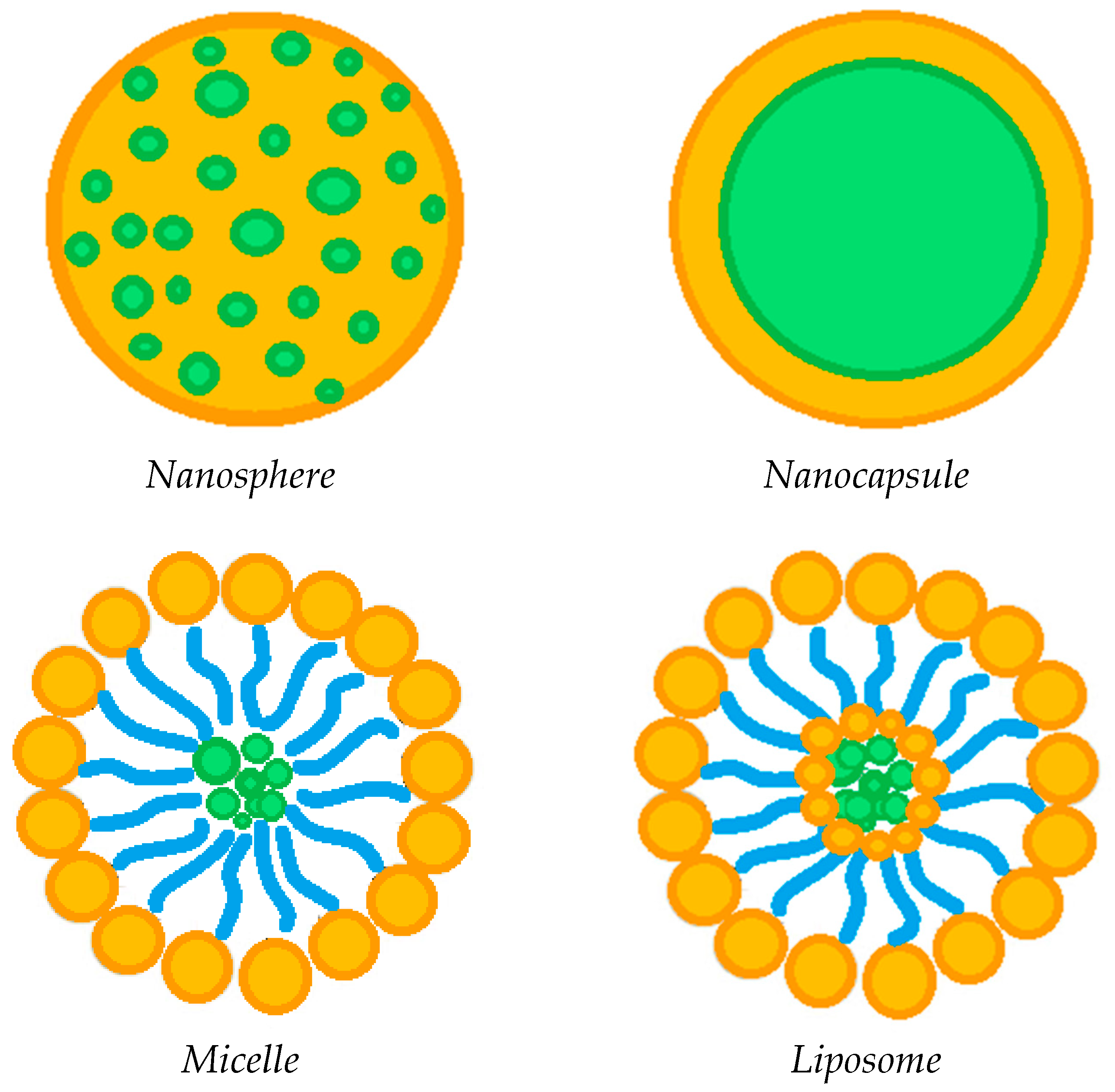
2. Different Supports to Produce Therapeutic Contact Lenses
3. Methods of Loading Active Principles into Contact Lenses
3.1. Soaking Method and Solvent Casting
3.2. Loading of Vitamin E into Therapeutic Contact Lenses
3.3. Incorporation of Drug-Loaded Nanocomposites or Ring Implants into Contact Lenses
3.4. Molecular Imprinting
3.5. Supercritical CO2—Assisted Technologies
3.6. Sterilization Step and Post-Processing Stages
4. Market Outlooks for Therapeutic Contact Lenses
- High oxygen permeability.
- Cost-effectiveness.
- The range of some parameters, mainly the back-optic zone radius (BOZR) and total diameter (TD). In general, soft lenses with standard TDs are used; however, in some cases, lenses with larger size may be necessary, for example to prevent wound bleeding after surgery. Consequently, to assure the desired physical fit, the contact lenses with larger TDs required a flatter BOZR.
- Stability of the contact lens on the eye, guaranteed by the minimal dehydration of the hydrogel that usually occurs after the lens application. However, this aspect is a serious problem, for example, for patients suffering from the dry eye syndrome, among other disorders.
- To minimize the deposition of impurities on the lens surface, which should ideally be resistant to its formation. A practical route could be the use of disposable lenses, but the patient compliance and the efficacy of therapeutic treatment could be reduced.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gorantla, S.; Rapalli, V.K.; Waghule, T.; Singh, P.P.; Dubey, S.K.; Saha, R.N.; Singhvi, G. Nanocarriers for ocular drug delivery: Current status and translational opportunity. RSC Adv. 2020, 10, 27835–27855. [Google Scholar] [CrossRef]
- Wilson, C.G. Topical drug delivery in the eye. Exp. Eye Res. 2004, 78, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Cholkar, K.; Agrahari, V.; Mitra, A.K. Ocular drug delivery systems: An overview. World J. Pharmacol. 2013, 2, 47–64. [Google Scholar] [CrossRef] [PubMed]
- Gulsen, D.; Chauhan, A. Ophthalmic drug delivery through contact lenses. Investig. Ophthalmol. Vis. Sci. 2004, 45, 2342–2347. [Google Scholar] [CrossRef]
- Carvalho, I.; Marques, C.; Oliveira, R.; Coelho, P.; Costa, P.; Ferreira, D. Sustained drug release by contact lenses for glaucoma treatment—A review. J. Control. Release 2015, 202, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Morrison, P.W.; Khutoryanskiy, V.V. Advances in ophthalmic drug delivery. Ther. Deliv. 2014, 5, 1297–1315. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Soni, T.G.; Shah, D.O. A review on therapeutic contact lenses for ocular drug delivery. Drug Deliv. 2016, 23, 3017–3026. [Google Scholar] [CrossRef]
- Zhang, X.; Cao, X.; Qi, P. Therapeutic contact lenses for ophthalmic drug delivery: Major challenges. J. Biomater. Sci. Polym. Ed. 2020, 31, 549–560. [Google Scholar] [CrossRef]
- Alvarez-Lorenzo, C.; Hiratani, H.; Concheiro, A. Contact lenses for drug delivery. Am. J. Adv. Drug Deliv. 2006, 4, 131–151. [Google Scholar] [CrossRef]
- Pillay, R.; Hansraj, R.; Rampersad, N. Historical development, applications and advances in materials used in spectacle lenses and contact lenses. Clin. Optom. 2020, 12, 157–167. [Google Scholar] [CrossRef]
- Tieppo, A.; White, C.; Paine, A.; Voyles, M.; McBride, M.; Byrne, M. Sustained in vivo release from imprinted therapeutic contact lenses. J. Control. Release 2012, 157, 391–397. [Google Scholar] [CrossRef]
- Novack, G. Ophthalmic drug delivery: Development and regulatory considerations. Clin. Pharmacol. Ther. 2009, 85, 539–543. [Google Scholar] [CrossRef]
- Weiner, A.L. Drug delivery systems in ophthalmic applications. In Ocular Therapeutics; Elsevier: Amsterdam, The Netherlands, 2008; pp. 7–43. [Google Scholar]
- Imperiale, J.C.; Acosta, G.B.; Sosnik, A. Polymer-based carriers for ophthalmic drug delivery. J. Control. Release 2018, 285, 106–141. [Google Scholar] [CrossRef] [PubMed]
- Xinming, L.; Yingde, C.; Lloyd, A.W.; Mikhalovsky, S.V.; Sandeman, S.R.; Howel, C.A.; Liewen, L. Polymeric hydrogels for novel contact lens-based ophthalmic drug delivery systems: A review. Cont. Lens Anterior Eye 2008, 31, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lorenzo, C.; Anguiano-Igea, S.; Varela-García, A.; Vivero-Lopez, M.; Concheiro, A. Bioinspired hydrogels for drug-eluting contact lenses. Acta Biomater. 2019, 84, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Torres-Luna, C.; Fan, X.; Domszy, R.; Hu, N.; Wang, N.S.; Yang, A. Hydrogel-based ocular drug delivery systems for hydrophobic drugs. Eur. J. Pharm. Sci. 2020, 154, 105503–105517. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, E.M. Hydrogel: Preparation, characterization, and applications: A review. J. Adv. Res. 2015, 6, 105–121. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Choksi, H.H.; Desai, A.R.; Patel, A.S.; Ranch, K.M.; Vyas, B.A.; Shah, D.O. pH triggered controlled drug delivery from contact lenses: Addressing the challenges of drug leaching during sterilization and storage. Colloids Surf. B 2017, 157, 72–82. [Google Scholar] [CrossRef]
- Xu, W.; Jiao, W.; Li, S.; Tao, X.; Mu, G. Bimatoprost loaded microemulsion laden contact lens to treat glaucoma. J. Drug Deliv. Sci. Tech. 2019, 54, 101330–101336. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Mangukiya, M.A.; Patel, P.A.; Vaidya, R.J.; Koli, A.R.; Ranch, K.M.; Shah, D.O. Extended release of ketotifen from silica shell nanoparticle-laden hydrogel contact lenses: In vitro and in vivo evaluation. J. Mater. Sci. Mater. Med. 2016, 27, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Hiratani, H.; Alvarez-Lorenzo, C. The nature of backbone monomers determines the performance of imprinted soft contact lenses as timolol drug delivery systems. Biomaterials 2004, 25, 1105–1113. [Google Scholar] [CrossRef]
- Lu, C.; Mikhail, A.S.; Wang, X.; Brook, M.A.; Allen, C. Hydrogels containing core cross-linked block co-polymer micelles. J. Biomater. Sci. Polym. Ed. 2012, 23, 1069–1090. [Google Scholar] [CrossRef]
- Desai, A.R.; Maulvi, F.A.; Desai, D.M.; Shukla, M.R.; Ranch, K.M.; Vyas, B.A.; Shah, S.A.; Sandeman, S.; Shah, D.O. Multiple drug delivery from the drug-implants-laden silicone contact lens: Addressing the issue of burst drug release. Mat. Sci. Eng. C 2020, 112, 110885–110899. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Lakdawala, D.H.; Shaikh, A.A.; Desai, A.R.; Choksi, H.H.; Vaidya, R.J.; Ranch, K.M.; Koli, A.R.; Vyas, B.A.; Shah, D.O. In vitro and in vivo evaluation of novel implantation technology in hydrogel contact lenses for controlled drug delivery. J. Control. Release 2016, 226, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Maulvi, F.A.; Singhania, S.S.; Desai, A.R.; Shukla, M.R.; Tannk, A.S.; Ranch, K.M.; Vyas, B.A.; Shah, D.O. Contact lenses with dual drug delivery for the treatment of bacterial conjunctivitis. Int. J. Pharm. 2018, 548, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Ciolino, J.B.; Hoare, T.R.; Iwata, N.G.; Behlau, I.; Dohlman, C.H.; Langer, R.; Kohane, D.S. A drug-eluting contact lens. Invest. Ophthalmol. Vis. Sci. 2009, 50, 3346–3352. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Kim, H.J.; Noh, H. Influence of solution pH on drug release from ionic hydrogel Lens. Macromol. Res. 2019, 27, 191–197. [Google Scholar] [CrossRef]
- Ciolino, J.B.; Hudson, S.P.; Mobbs, A.N.; Hoare, T.R.; Iwata, N.G.; Fink, G.R.; Kohane, D.S. A prototype antifungal contact lens. Invest. Ophthalmol. Vis. Sci. 2011, 52, 6286–6291. [Google Scholar] [CrossRef] [PubMed]
- Ross, A.E.; Bengani, L.C.; Tulsan, R.; Maidana, D.E.; Salvador-Culla, B.; Kobashi, H.; Kolovou, P.E.; Zhai, H.; Taghizadeh, K.; Kuang, L. Topical sustained drug delivery to the retina with a drug-eluting contact lens. Biomaterials 2019, 217, 119285–119297. [Google Scholar] [CrossRef] [PubMed]
- Ciolino, J.B.; Stefanescu, C.F.; Ross, A.E.; Salvador-Culla, B.; Cortez, P.; Ford, E.M.; Wymbs, K.A.; Sprague, S.L.; Mascoop, D.R.; Rudina, S.S. In vivo performance of a drug-eluting contact lens to treat glaucoma for a month. Biomaterials 2014, 35, 432–439. [Google Scholar] [CrossRef]
- Ciolino, J.B.; Ross, A.E.; Tulsan, R.; Watts, A.C.; Wang, R.-F.; Zurakowski, D.; Serle, J.B.; Kohane, D.S. Latanoprost-eluting contact lenses in glaucomatous monkeys. Ophthalmology 2016, 123, 2085–2092. [Google Scholar] [CrossRef]
- Galante, R.; Oliveira, A.S.; Topete, A.; Ghisleni, D.; Braga, M.; Pinto, T.J.; Colaço, R.; Serro, A.P. Drug-eluting silicone hydrogel for therapeutic contact lenses: Impact of sterilization methods on the system performance. Colloids Surf. B 2018, 161, 537–546. [Google Scholar] [CrossRef]
- Lasowski, F.; Rambarran, T.; Rahmani, V.; Brook, M.A.; Sheardown, H. PEG-containing siloxane materials by metal-free click-chemistry for ocular drug delivery applications. J. Biomater. Sci. Polym. Ed. 2020, 32, 1–14. [Google Scholar] [CrossRef]
- Peng, C.-C.; Burke, M.T.; Carbia, B.E.; Plummer, C.; Chauhan, A. Extended drug delivery by contact lenses for glaucoma therapy. J. Control. Release 2012, 162, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.-C.; Kim, J.; Chauhan, A. Extended delivery of hydrophilic drugs from silicone-hydrogel contact lenses containing vitamin E diffusion barriers. Biomaterials 2010, 31, 4032–4047. [Google Scholar] [CrossRef]
- Yu, Y.; Xu, S.; Yu, S.; Li, J.; Tan, G.; Li, S.; Pan, W. A Hybrid Genipin-Cross-Linked Hydrogel/Nanostructured Lipid Carrier for Ocular Drug Delivery: Cellular, ex Vivo, and in Vivo Evaluation. ACS Biomater. Sci. Eng. 2020, 6, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Gandara-Loe, J.; Souza, B.E.; Missyul, A.; Giraldo, G.; Tan, J.-C.; Silvestre-Albero, J. MOF-Based Polymeric Nanocomposite Films as Potential Materials for Drug Delivery Devices in Ocular Therapeutics. ACS Appl. Mater. Interfaces 2020, 12, 30189–30197. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, A.; Das, P.J.; Dey, S.; Nayak, A.K.; Roy, P.K.; Chakrabarti, S.; Marbaniang, D.; Das, S.K.; Ray, S.; Chattopadhyay, P. Development and optimization of besifloxacin hydrochloride loaded liposomal gel prepared by thin film hydration method using 32 full factorial design. Colloids Surf. A Physicochem. Eng. Asp. 2020, 585, 124071–124082. [Google Scholar] [CrossRef]
- Yu, Y.; Macoon, R.; Chauhan, A. Improving wettability and lubricity of commercial contact lenses by polymerizing a thin film of dimethylacryamide. Colloids Surf. A Physicochem. Eng. Asp. 2019, 583, 123974–123983. [Google Scholar] [CrossRef]
- Franco, P.; De Marco, I. The Use of Poly (N-vinyl pyrrolidone) in the Delivery of Drugs: A Review. Polymers 2020, 12, 1114. [Google Scholar] [CrossRef]
- Daza, J.H.U.; Righetto, G.M.; Chaud, M.V.; da Conceição Amaro Martins, V.; Lopes Baratella da Cunha Camargo, I.; Maria de Guzzi Plepis, A. PVA/anionic collagen membranes as drug carriers of ciprofloxacin hydrochloride with sustained antibacterial activity and potential use in the treatment of ulcerative keratitis. J. Biomater. Appl. 2020, 35, 301–312. [Google Scholar] [CrossRef]
- Huang, J.-F.; Zhong, J.; Chen, G.-P.; Lin, Z.-T.; Deng, Y.; Liu, Y.-L.; Cao, P.-Y.; Wang, B.; Wei, Y.; Wu, T. A hydrogel-based hybrid theranostic contact lens for fungal keratitis. ACS Nano 2016, 10, 6464–6473. [Google Scholar] [CrossRef]
- Alvarez-Rivera, F.; Rey-Rico, A.; Venkatesan, J.K.; Diaz-Gomez, L.; Cucchiarini, M.; Concheiro, A.; Alvarez-Lorenzo, C. Controlled release of rAAV vectors from APMA-functionalized contact lenses for corneal gene therapy. Pharmaceutics 2020, 12, 335. [Google Scholar] [CrossRef]
- Li, R.; Guan, X.; Lin, X.; Guan, P.; Zhang, X.; Rao, Z.; Du, L.; Zhao, J.; Rong, J.; Zhao, J. Poly (2-hydroxyethyl methacrylate)/β-cyclodextrin-hyaluronan contact lens with tear protein adsorption resistance and sustained drug delivery for ophthalmic diseases. Acta Biomater. 2020, 110, 105–118. [Google Scholar] [CrossRef] [PubMed]
- Morgan, S.R.; Pilia, N.; Hewitt, M.; Moses, R.L.; Moseley, R.; Lewis, P.N.; Morrison, P.W.; Kelly, S.L.; Parker, J.E.; Whitaker, D. Controlled in vitro delivery of voriconazole and diclofenac to the cornea using contact lenses for the treatment of Acanthamoeba keratitis. Int. J. Pharm. 2020, 579–588, 119102. [Google Scholar] [CrossRef] [PubMed]
- García-Millán, E.; Koprivnik, S.; Otero-Espinar, F.J. Drug loading optimization and extended drug delivery of corticoids from pHEMA based soft contact lenses hydrogels via chemical and microstructural modifications. Int. J. Pharm. 2015, 487, 260–269. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Soni, T.G.; Shah, D.O. Effect of timolol maleate concentration on uptake and release from hydrogel contact lenses using soaking method. J. Pharm. Appl. Sci. 2014, 1, 17–23. [Google Scholar]
- Torres-Luna, C.; Hu, N.; Fan, X.; Domszy, R.; Yang, J.; Briber, R.M.; Yang, A. Extended delivery of cationic drugs from contact lenses loaded with unsaturated fatty acids. Eur. J. Pharm. Biopharm. 2020, 155, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Cho, S.; Park, H.S.; Kwon, I. Ocular drug delivery through pHEMA-Hydrogel contact lenses Co-loaded with lipophilic vitamins. Sci. Rep. 2016, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hsu, K.-H.; Carbia, B.E.; Plummer, C.; Chauhan, A. Dual drug delivery from vitamin E loaded contact lenses for glaucoma therapy. Eur. J. Pharm. Biopharm. 2015, 94, 312–321. [Google Scholar] [CrossRef]
- Kim, J.; Peng, C.-C.; Chauhan, A. Extended release of dexamethasone from silicone-hydrogel contact lenses containing vitamin E. J. Control. Release 2010, 148, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zu, D.; Chen, J.; Peng, J.; Liu, Y.; Zhang, H.; Li, S.; Pan, W. Bovine serum albumin–meloxicam nanoaggregates laden contact lenses for ophthalmic drug delivery in treatment of postcataract endophthalmitis. Int. J. Pharm. 2014, 475, 25–34. [Google Scholar] [CrossRef]
- Lu, C.; Yoganathan, R.B.; Kociolek, M.; Allen, C. Hydrogel containing silica shell cross-linked micelles for ocular drug delivery. J. Pharm. Sci. 2013, 102, 627–637. [Google Scholar] [CrossRef]
- Danion, A.; Arsenault, I.; Vermette, P. Antibacterial activity of contact lenses bearing surface-immobilized layers of intact liposomes loaded with levofloxacin. J. Pharm. Sci. 2007, 96, 2350–2363. [Google Scholar] [CrossRef] [PubMed]
- Gulsen, D.; Li, C.-C.; Chauhan, A. Dispersion of DMPC liposomes in contact lenses for ophthalmic drug delivery. Curr. Eye Res. 2005, 30, 1071–1080. [Google Scholar] [CrossRef]
- Jung, H.J.; Abou-Jaoude, M.; Carbia, B.E.; Plummer, C.; Chauhan, A. Glaucoma therapy by extended release of timolol from nanoparticle loaded silicone-hydrogel contact lenses. J. Control. Release 2013, 165, 82–89. [Google Scholar] [CrossRef]
- Maulvi, F.A.; Patil, R.J.; Desai, A.R.; Shukla, M.R.; Vaidya, R.J.; Ranch, K.M.; Vyas, B.A.; Shah, S.A.; Shah, D.O. Effect of gold nanoparticles on timolol uptake and its release kinetics from contact lenses: In vitro and in vivo evaluation. Acta Biomater. 2019, 86, 350–362. [Google Scholar] [CrossRef]
- Desai, A.R.; Maulvi, F.A.; Pandya, M.M.; Ranch, K.M.; Vyas, B.A.; Shah, S.A.; Shah, D.O. Co-delivery of timolol and hyaluronic acid from semi-circular ring-implanted contact lenses for the treatment of glaucoma: In vitro and in vivo evaluation. Biomater. Sci. 2018, 6, 1580–1591. [Google Scholar] [CrossRef] [PubMed]
- Varela-Garcia, A.; Gomez-Amoza, J.L.; Concheiro, A.; Alvarez-Lorenzo, C. Imprinted contact lenses for ocular administration of antiviral drugs. Polymers 2020, 12, 2026. [Google Scholar] [CrossRef] [PubMed]
- Costa, V.P.; Braga, M.E.; Guerra, J.P.; Duarte, A.R.; Duarte, C.M.; Leite, E.O.; Gil, M.H.; de Sousa, H.C. Development of therapeutic contact lenses using a supercritical solvent impregnation method. J. Supercrit. Fluids 2010, 52, 306–316. [Google Scholar] [CrossRef]
- González-Chomón, C.; Braga, M.E.; de Sousa, H.C.; Concheiro, A.; Alvarez-Lorenzo, C. Antifouling foldable acrylic IOLs loaded with norfloxacin by aqueous soaking and by supercritical carbon dioxide technology. Eur. J. Pharm. Biopharm. 2012, 82, 383–391. [Google Scholar] [CrossRef]
- Yokozaki, Y.; Sakabe, J.; Ng, B.; Shimoyama, Y. Effect of temperature, pressure and depressurization rate on release profile of salicylic acid from contact lenses prepared by supercritical carbon dioxide impregnation. Chem. Eng. Res. Des. 2015, 100, 89–94. [Google Scholar] [CrossRef]
- Masmoudi, Y.; Azzouk, L.B.; Forzano, O.; Andre, J.-M.; Badens, E. Supercritical impregnation of intraocular lenses. J. Supercrit. Fluids 2011, 60, 98–105. [Google Scholar] [CrossRef]
- Costa, V.P.; Braga, M.E.; Duarte, C.M.; Alvarez-Lorenzo, C.; Concheiro, A.; Gil, M.H.; de Sousa, H.C. Anti-glaucoma drug-loaded contact lenses prepared using supercritical solvent impregnation. J. Supercrit. Fluids 2010, 53, 165–173. [Google Scholar] [CrossRef]
- Bouledjouidja, A.; Masmoudi, Y.; Sergent, M.; Trivedi, V.; Meniai, A.; Badens, E. Drug loading of foldable commercial intraocular lenses using supercritical impregnation. Int. J. Pharm. 2016, 500, 85–99. [Google Scholar] [CrossRef]
- Ongkasin, K.; Masmoudi, Y.; Tassaing, T.; Le-Bourdon, G.; Badens, E. Supercritical loading of gatifloxacin into hydrophobic foldable intraocular lenses–Process control and optimization by following in situ CO2 sorption and polymer swelling. Int. J. Pharm. 2020, 581, 119247–119256. [Google Scholar] [CrossRef] [PubMed]
- Duarte, A.R.C.; Simplicio, A.L.; Vega-González, A.; Subra-Paternault, P.; Coimbra, P.; Gil, M.; de Sousa, H.C.; Duarte, C.M. Impregnation of an intraocular lens for ophthalmic drug delivery. Curr. Drug Deliv. 2008, 5, 102–107. [Google Scholar] [CrossRef]
- Ongkasin, K.; Masmoudi, Y.; Wertheimer, C.M.; Hillenmayer, A.; Eibl-Lindner, K.H.; Badens, E. Supercritical fluid technology for the development of innovative ophthalmic medical devices: Drug loaded intraocular lenses to mitigate posterior capsule opacification. Eur. J. Pharm. Biopharm. 2020, 149, 248–256. [Google Scholar] [CrossRef]
- Braga, M.E.; Costa, V.P.; Pereira, M.J.; Fiadeiro, P.T.; Gomes, A.P.A.; Duarte, C.M.; de Sousa, H.C. Effects of operational conditions on the supercritical solvent impregnation of acetazolamide in Balafilcon A commercial contact lenses. Int. J. Pharm. 2011, 420, 231–243. [Google Scholar] [CrossRef] [PubMed]
- Bouledjouidja, A.; Masmoudi, Y.; Sergent, M.; Badens, E. Effect of operational conditions on the supercritical carbon dioxide impregnation of anti-inflammatory and antibiotic drugs in rigid commercial intraocular lenses. J. Supercrit. Fluids 2017, 130, 63–75. [Google Scholar] [CrossRef]
- Yañez, F.; Martikainen, L.; Braga, M.E.; Alvarez-Lorenzo, C.; Concheiro, A.; Duarte, C.M.; Gil, M.H.; De Sousa, H.C. Supercritical fluid-assisted preparation of imprinted contact lenses for drug delivery. Acta Biomater. 2011, 7, 1019–1030. [Google Scholar] [CrossRef]
- Fan, X.; Torres-Luna, C.; Azadi, M.; Domszy, R.; Hu, N.; Yang, A.; David, A.E. Evaluation of commercial soft contact lenses for ocular drug delivery: A review. Acta Biomater. 2020, 115, 60–74. [Google Scholar] [CrossRef] [PubMed]
- Li, C.-C.; Chauhan, A. Modeling ophthalmic drug delivery by soaked contact lenses. Ind. Eng. Chem. Res. 2006, 45, 3718–3734. [Google Scholar] [CrossRef]
- Yılmaz, T.; Aydemir, O.; Özercan, İ.H.; Üstündağ, B. Effects of vitamin e, pentoxifylline and aprotinin on light-induced retinal injury. Ophthalmologica 2007, 221, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Bilgihan, K.; Adiguzel, U.; Sezer, C.; Akyol, G.; Hasanreisoglu, B. Effects of topical vitamin E on keratocyte apoptosis after traditional photorefractive keratectomy. Ophthalmologica 2001, 215, 192–196. [Google Scholar] [CrossRef]
- Ohta, Y. Possibility of clinical application of vitamin E to cataract prevention. J. Clin. Biochem. Nutr. 2004, 35, 35–45. [Google Scholar] [CrossRef][Green Version]
- Nagata, M.; Kojima, M.; Sasaki, K. Effect of vitamin E eye drops on naphthalene-induced cataract in rats. J. Ocul. Pharmacol. Ther. 1999, 15, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Kojima, M.; Shui, Y.B.; Murano, H.; Sasaki, K. Inhibition of steroid-induced cataract in rat eyes by administration of vitamin-E ophthalmic solution. Ophthalmic Res. 1996, 28, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Ohta, Y.; Yamasaki, T.; Niwa, T.; Majima, Y.; Ishiguro, I. Preventive effect of topical vitamin E-containing liposome instillation on the progression of galactose cataract. Comparison between 5-week-and 12-week-old rats fed a 25% galactose diet. Exp. Eye Res. 1999, 68, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Ohta, Y.; Yamasaki, T.; Niwa, T.; Majima, Y. Preventive effect of vitamin E-containing liposome instillation on cataract progression in 12-month-old rats fed a 25% galactose diet. J. Ocul. Pharmacol. Ther. 2000, 16, 323–335. [Google Scholar] [CrossRef]
- Kapoor, Y.; Thomas, J.C.; Tan, G.; John, V.T.; Chauhan, A. Surfactant-laden soft contact lenses for extended delivery of ophthalmic drugs. Biomaterials 2009, 30, 867–878. [Google Scholar] [CrossRef]
- Moustafa, M.A.; Elnaggar, Y.S.; El-Refaie, W.M.; Abdallah, O.Y. Hyalugel-integrated liposomes as a novel ocular nanosized delivery system of fluconazole with promising prolonged effect. Int. J. Pharm. 2017, 534, 14–24. [Google Scholar] [CrossRef]
- Meza-Rios, A.; Navarro-Partida, J.; Armendariz-Borunda, J.; Santos, A. Therapies Based on Nanoparticles for Eye Drug Delivery. Ophthalmol. Ther. 2020, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Campardelli, R.; Trucillo, P.; Reverchon, E. Supercritical assisted process for the efficient production of liposomes containing antibiotics for ocular delivery. J. CO2 Util. 2018, 25, 235–241. [Google Scholar] [CrossRef]
- Abrishami, M.; Abrishami, M.; Mahmoudi, A.; Mosallaei, N.; Vakili Ahrari Roodi, M.; Malaekeh-Nikouei, B. Solid lipid nanoparticles improve the diclofenac availability in vitreous after intraocular injection. J. Drug Deliv. 2016, 2016, 1–5. [Google Scholar] [CrossRef]
- Naseri, N.; Valizadeh, H.; Zakeri-Milani, P. Solid lipid nanoparticles and nanostructured lipid carriers: Structure, preparation and application. Adv. Pharm. Bull. 2015, 5, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Durgun, M.E.; Güngör, S.; Özsoy, Y. Micelles: Promising ocular drug carriers for anterior and posterior segment diseases. J. Ocul. Pharmacol. Ther. 2020, 36, 323–341. [Google Scholar] [CrossRef]
- Gote, V.; Ansong, M.; Pal, D. Prodrugs and nanomicelles to overcome ocular barriers for drug penetration. Expert Opin. Drug Metab. Toxicol. 2020, 16, 885–906. [Google Scholar] [CrossRef]
- Noh, G.; Keum, T.; Seo, J.-E.; Choi, J.; Rakesh, B.; Shrawani, L.; Park, B.; Choi, Y.W.; Lee, S. Development and evaluation of a water soluble fluorometholone eye drop formulation employing polymeric micelle. Pharmaceutics 2018, 10, 208. [Google Scholar] [CrossRef]
- Vadlapudi, A.D.; Mitra, A.K. Nanomicelles: An emerging platform for drug delivery to the eye. Ther. Deliv. 2013, 4, 1–3. [Google Scholar] [CrossRef]
- Singh, A.P.; Biswas, A.; Shukla, A.; Maiti, P. Targeted therapy in chronic diseases using nanomaterial-based drug delivery vehicles. Signal Transduct. Target. Ther. 2019, 4, 1–21. [Google Scholar] [CrossRef]
- Saettone, M.F.; Chetoni, P.; Cerbai, R.; Mazzanti, G.; Braghiroli, L. Evaluation of ocular permeation enhancers: In vitro effects on corneal transport of four β-blockers, and in vitro/in vivo toxic activity. Int. J. Pharm. 1996, 142, 103–113. [Google Scholar] [CrossRef]
- Furrer, P.; Mayer, J.M.; Plazonnet, B.; Gurny, R. Ocular tolerance of absorption enhancers in ophthalmic preparations. Aaps PharmSci. 2002, 4, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Chetoni, P.; Burgalassi, S.; Monti, D.; Saettone, M. Ocular toxicity of some corneal penetration enhancers evaluated by electrophysiology measurements on isolated rabbit corneas. Toxicol. In Vitro 2003, 17, 497–504. [Google Scholar] [CrossRef]
- Chen, L.; Wang, X.; Lu, W.; Wu, X.; Li, J. Molecular imprinting: Perspectives and applications. Chem. Soc. Rev. 2016, 45, 2137–2211. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lorenzo, C.; Concheiro, A. Molecularly imprinted polymers for drug delivery. J. Chromatogr. B 2004, 804, 231–245. [Google Scholar] [CrossRef] [PubMed]
- Cunliffe, D.; Kirby, A.; Alexander, C. Molecularly imprinted drug delivery systems. Adv. Drug Deliv. Rev. 2005, 57, 1836–1853. [Google Scholar] [CrossRef]
- Franco, P.; De Marco, I. Eudragit: A novel carrier for controlled drug delivery in supercritical antisolvent coprecipitation. Polymers 2020, 12, 234. [Google Scholar] [CrossRef]
- Baldino, L.; Cardea, S.; Reverchon, E. Supercritical assisted electrospray: An improved micronization process. Polymers 2019, 11, 244. [Google Scholar] [CrossRef]
- Campardelli, R.; Franco, P.; Reverchon, E.; De Marco, I. Polycaprolactone/nimesulide patches obtained by a one-step supercritical foaming + impregnation process. J. Supercrit. Fluids 2019, 146, 47–54. [Google Scholar] [CrossRef]
- Veys, J.; Meyler, J.; Davies, I. Essential Contact Lens Practice; Elsevier Health Sciences: Philadelphia, PA, USA, 2002. [Google Scholar]
| Polymer | Properties |
|---|---|
| pHEMA |
|
| PMMA |
|
| Silicone/siloxane |
|
| Drug-Loading Method | Polymeric Support | Active Principle | Application | Outcome | Ref. |
|---|---|---|---|---|---|
| Soaking method | Polyurethane film produced by solvent casting | Brimonidine tartrate | Glaucoma | Prolonged drug release up to 14 days | [38] |
| Drug-loaded liposomes by hydration method; soaking method | Lipids-based film | Besifloxacin hydrochloride | Conjunctivitis | Biphasic release: initial burst + sustained (80% released in 10 h) | [39] |
| - | DMA film placed on commercial CLs loaded with AIBN | Loading of vitamin E | - | AIBN release in about 30 min | [40] |
| Solvent casting | PLGA film embedded in methafilcon hydrogel- based CLs | Dexamethasone | Retinal diseases, such as diabetic macular edema | Prolonged drug release up to 160 h | [30] |
| Solvent casting | PLGA film embedded in HEMA hydrogel-based CLs | Ciprofloxacin | Post-operative treatment | Prolonged drug release for 1 month | [27] |
| Solvent casting | PLGA film embedded in HEMA hydrogel-based CLs | Econazole | Fungal keratitis | Extended antifungal activity | [29] |
| Solvent casting | PLGA film embedded in methafilcon hydrogel- based CLs | Latanoprost | Glaucoma | Initial burst + sustained drug release for 1 month. | [31] |
| Solvent casting | PLGA film embedded in methafilcon hydrogel- based CLs | Latanoprost | Ocular hypertension, glaucoma | Sustained drug delivery as effective as eyedrops | [32] |
| Solvent casting | Hydrogel-based CLs | Voriconazole loaded into GO; HTCC and silver nanoparticles as antimicrobial agents | Fungal Keratitis | Good antifungal and antimicrobial activity | [43] |
| Soaking or mixing method | PVA/collagen membrane | Ciprofloxacin hydrochloride, tobramycin | Ulcerative keratitis | Antibacterial activity for 48 h | [42] |
| Soaking method | HEMA hydrogels with/without APMA | rAAV | Corneal gene therapy | Efficacy in transduction/ triggering cell proliferation | [44] |
| Soaking method | Silicone hydrogels | Levofloxacin, chlorhexidine, diclofenac, timolol | - | High burst in the release profiles, optimization of sterilization method | [33] |
| Soaking method | Hydrogels based on HEMA, silicone, NVP and MMA | HPMC | - | pH-sensitivite drug release | [28] |
| Soaking method | PEG-modified silicone hydrogel | Roscovitine | Retinoblastoma | Prolonged drug release | [34] |
| Soaking method | HEMA/β-CD- hyaluronan hydrogels | Diclofenac sodium | Conjunctivitis | Therapeutic effect for conjunctivitis | [45] |
| Soaking method | Commercial hydrogel- based CLs | Voriconazole, diclofenac sodium | Acanthamoeba keratitis | Sustained release, cell proliferation | [46] |
| Soaking method | HEMA hydrogel- based CLs | Triamcinolone acetonide | Allergy | Prolonged drug release | [47] |
| Soaking method | Commercial HEMA hydrogel- based CLs | Timolol maleate | - | High-burst: 95% of drug released in 2 h | [48] |
| Soaking method from a solution or microemulsion | CLs based on siloxane, DMA, EGDMA, HEMA, Irgacure | Bimatoprost | Glaucoma | Microemulsion better than solution to prolong release | [20] |
| Soaking method | Commercial CLs based on silicone or HEMA hydrogels | Tetracaine, bupivacaine, ketotifen, diclofenac, flurbiprofen; loading of fatty acids (i.e., oleic acid, linoleic, α-linolenic acid) | - | Prolonged drug release, with an initial burst in the range 30–90% depending on the drug/CLs system | [49] |
| Soaking method | Commercial silicone hydrogel CLs | Timolol maleate; loading of vitamin E | Ocular hypertension, glaucoma | High drug bioavailability, reduction of hypertension | [35] |
| Soaking method | HEMA-based hydrogels with EGDMA, GMA, NVP, AIBN | Alexa Fluor 488 dye, brimonidine, timolol; loading of vitamin E and A | Glaucoma | Increase in drug loading, drug release in 6 h | [50] |
| Soaking method | Commercial silicone hydrogel CLs | Fluconazole, dexamethasone, timolol maleate; vitamin E loading | Eye inflammation, glaucoma | Prolonged drug release, beneficial effect of blocking UV radiation | [36] |
| Soaking method | Commercial CLs based on senofilcon A | Timolol maleate, dorzolamide hydrochloride; vitamin E loading | Glaucoma | Prolonged drug release | [51] |
| Soaking method | Commercial silicone hydrogel CLs | Dexamethasone; vitamin E loading | Eye inflammation | Prolonged drug release | [52] |
| Drug/BSA NCs by acid-base neutralization reactions; soaking method | NCs based on BSA and loaded into HEMA hydrogels | Meloxicam | Ocular irritation, antophthalmia after cataract surgery | Reduction of eye irritation, extended drug release | [53] |
| Drug-loaded micelles by thin-film hydration method | PEG-b-PCL micelles (with a PCL core and silica shell) loaded into HEMA hydrogels | Dexamethasone | Chronic posterior segment eye diseases | Prolonged drug release up to 30 days | [54] |
| - | PEG-b-PCL micelles into HEMA hydrogels | DDAO dye | - | Extended release for at least 14 days | [23] |
| Drug-loaded liposomes placed on CLs by multilayer immobilization; soaking method | Commercial CLs | Levofloxacin | Bacterial infections, such as keratitis | Antibacterial activity against Staphylococcus aureus | [55] |
| Drug-laden liposomes loaded into hydrogels by free radical solution polymerization | DMPC liposomes loaded into HEMA-hydrogel CLs | Lidocaine | - | Drug release prolonged for about 7 days | [56] |
| Drug-loaded lipid NPs by melt-emulsification and ultrasonication method; soaking | Compritol 888 ATO and triglyceride as lipid carriers for NPs soaked into hydrogels based on CMC and poloxamer 407 | Quercetin | - | Improvement in drug transcorneal penetration and the precorneal retention time | [37] |
| Drug/PGT NPs by thermal polymerization; soaking method | PGT-based NPs loaded into commercial silicone hydrogel CLs | Timolol maleate | Ocular hypertension, glaucoma | Prolonged drug release, reduction in hypertension, optimization of storage conditions | [57] |
| Drug/silica NPs by microemulsion | Drug/silica shell NPs loaded into HEMA-based hydrogels | Lidocaine | Glaucoma | Prolonged drug release kinetics, with a 50% burst effect | [4] |
| Drug/Eudragit NPs by quasi-emulsion solvent diffusion; soaking for direct- drug-loaded CLs | pH-sensitive drug/Eudragit S100 NPs laden into hydrogel CLs | Cyclosporine | Chronic dry eyes syndrome | Prolonged drug release up to 14 h, no leaching after packaging | [19] |
| Drug/silica NPs by microemulsion; direct-drug-loaded CLs by free radical polymerization | Drug/silica shell NPs loaded into hydrogels based on HEMA, MAA, EGDMA | Ketotifen fumarate | Allergy | Reduced loss in transmittance and physical properties of hydrogels with NPs by emultion | [21] |
| Drug-loaded EC NPs by double emulsion | Drug/EC NPs into ring implants based on HEMA, EGDMA and MAA, then incorporated into hydrogel CLs | Timolol maleate | Glaucoma | Sustained drug release and reduction in intraocular pressure (for 170 h /190 h) | [25] |
| Soaking method | CLs based on HEMA, DMA, EGDMA, NVP, siloxane and Irgacure | Timolol maleate, gold NPs | - | Rapid drug release in a few hours, reduction in intraocular pressure | [58] |
| Soaking method | Drug-loaded semi-circular rings based on HEMA, MAA, EGDMA and Irgacure D, then implanted into hydrogel CLs | Moxifloxacin HCl, hyaluronic acid | Conjunctivitis | Improvement in drug residence time, bactericidal activity, optimization of sterilization method | [26] |
| Cast moulding | Drug- loaded semi-circular acrylate rings implanted in CLs | Timolol maleate, hyaluronic acid | Glaucoma | High burst in drug release, optimization of sterilization | [59] |
| Solvent casting for drug-loaded implants; soaking method for direct-drug-loaded CLs | Silicone CLs; implants based on Irgacure, EGDMA, DMA, NVP, siloxane, HEMA, then embedded into silicone CLs | Bimatoprost, hyaluronic acid, timolol | Ocular hypertension, glaucoma | High burst effect in drug release profiles | [24] |
| Molecular imprinting | Hydrogels based on HEMA, DEAA, DMA, SiMA, MMA | Timolol maleate | Glaucoma | Fast release, increase in drug loading by imprinting | [22] |
| Molecular imprinting | Hydrogels based on HEMA, EGDMA, MAA, AIBN | Acyclovir, valacyclovir hydrochloride | Herpes simplex virus ocular keratitis | High drug loadings | [60] |
| Soaking method; supercritical impregnation | Commercial hydrogel CLs based on Methafilcon A, Nelfilcon A, Omafilcon A, Hilafilcon B | Flurbiprofene, timolol maleate | Glaucoma | Higher drug loadings with shorter process times by sup. impregnation | [61] |
| Soaking method; supercritical impregnation | Foldable acrylic hydrogel CLs, based on HEMA and BEM with MAA and acrylamide | Norfloxacin | Cataract | Higher drug loadings by supercritical impregnation | [62] |
| Supercritical impregnation | Commercial silicone CLs based on Hilafilcon B | Salicylic acid | - | Prolonged drug release for 8 h | [63] |
| Supercritical impregnation | Commercial rigid CLs based on PMMA | Cefuroxime sodium | Cataract | Prolonged drug release for 15 days | [64] |
| Supercritical impregnation | Commercial silicone hydrogel CLs, based on Balafilcon A | Acetazolamide, timolol maleate | Glaucoma | Higher drug loadings | [65] |
| Supercritical impregnation | Foldable acrylic CLs, based on HEMA | Dexamethasone, ciprofloxacin | Cataract | Prolonged drug release for 60 days | [66] |
| Supercritical impregnation | Commercial foldable acrylic CLs | Gatifloxacin | Endophthalmitis after cataract surgery | Imrpovement in impregnation yield | [67] |
| Supercritical impregnation | P(MMA-EHA-EGDMA) films | Flurbiprofen | Eye surgery | Prolonged drug released in 3 months | [68] |
| Supercritical impregnation | Commercial foldable acrylic CLs | Methotrexate | Posterior capsule opacification after cataract surgery | Prolonged drug release for more than 100 days, inhibition of fibrosis | [69] |
| Supercritical impregnation | Commercial silicone CLs, based on Balafilcon A | Acetazolamide | Glaucoma | Fast drug release in about 3 h | [70] |
| Supercritical impregnation | Commercial rigid CLs based on PMMA | Dexamethasone, ciprofloxacin | Prevention of short- and mid-term postoperative complications | Prolonged drug release up to about 40 days | [71] |
| Supercritical CO2- assisted molecular imprinting | Commercial silicone CLs | Flurbiprofen | - | Prolonged drug release up to about 8 h | [72] |
| Brand | Material | Company |
|---|---|---|
| PureVision | Balafilcon A | Bausch & Lomb |
| Bioinfinity | Comfilcon A | Cooper Vision |
| Dailies Total | Delefilcon A | Alcon |
| ACUVUE Advance | Galyfilcon A | Johnson & Johnson |
| Night & Day | Lotrafilcon A | CIBA Vision |
| Air Optix Aqua | Lotrafilcon B | CIBA Vision |
| ACUVUE Tru | Eye Narafilcon A | Johnson & Johnson |
| ACUVUE Oasys | Senofilcon A | Johnson & Johnson |
| Clariti 1-day | Somofilcon A | Cooper Vision |
| Method | PROS | CONS |
|---|---|---|
| Soaking method |
|
|
| Solvent casting |
|
|
| Loading of vitamin E |
|
|
| Incorporation of drug-loaded nanostructures or ring implants |
|
|
| Molecular imprinting |
|
|
| Supercritical technologies |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco, P.; De Marco, I. Contact Lenses as Ophthalmic Drug Delivery Systems: A Review. Polymers 2021, 13, 1102. https://doi.org/10.3390/polym13071102
Franco P, De Marco I. Contact Lenses as Ophthalmic Drug Delivery Systems: A Review. Polymers. 2021; 13(7):1102. https://doi.org/10.3390/polym13071102
Chicago/Turabian StyleFranco, Paola, and Iolanda De Marco. 2021. "Contact Lenses as Ophthalmic Drug Delivery Systems: A Review" Polymers 13, no. 7: 1102. https://doi.org/10.3390/polym13071102
APA StyleFranco, P., & De Marco, I. (2021). Contact Lenses as Ophthalmic Drug Delivery Systems: A Review. Polymers, 13(7), 1102. https://doi.org/10.3390/polym13071102







