Calcium-Silicate-Incorporated Gellan-Chitosan Induced Osteogenic Differentiation in Mesenchymal Stromal Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis of Calcium Silicate
2.2. Biomaterial Fabrication
2.3. Physicochemical Characterization
2.4. hBMSCs Isolation and Seeding
2.5. Scanning Electron Microscopy Analysis
2.6. Cell Proliferation and Viability Assay
2.7. Alkaline Phosphatase (ALP) Activity
2.8. Mineralization Staining Assay
2.9. Gene Expression
2.10. Immunocytochemistry (ICC)
2.11. Statistics
3. Results
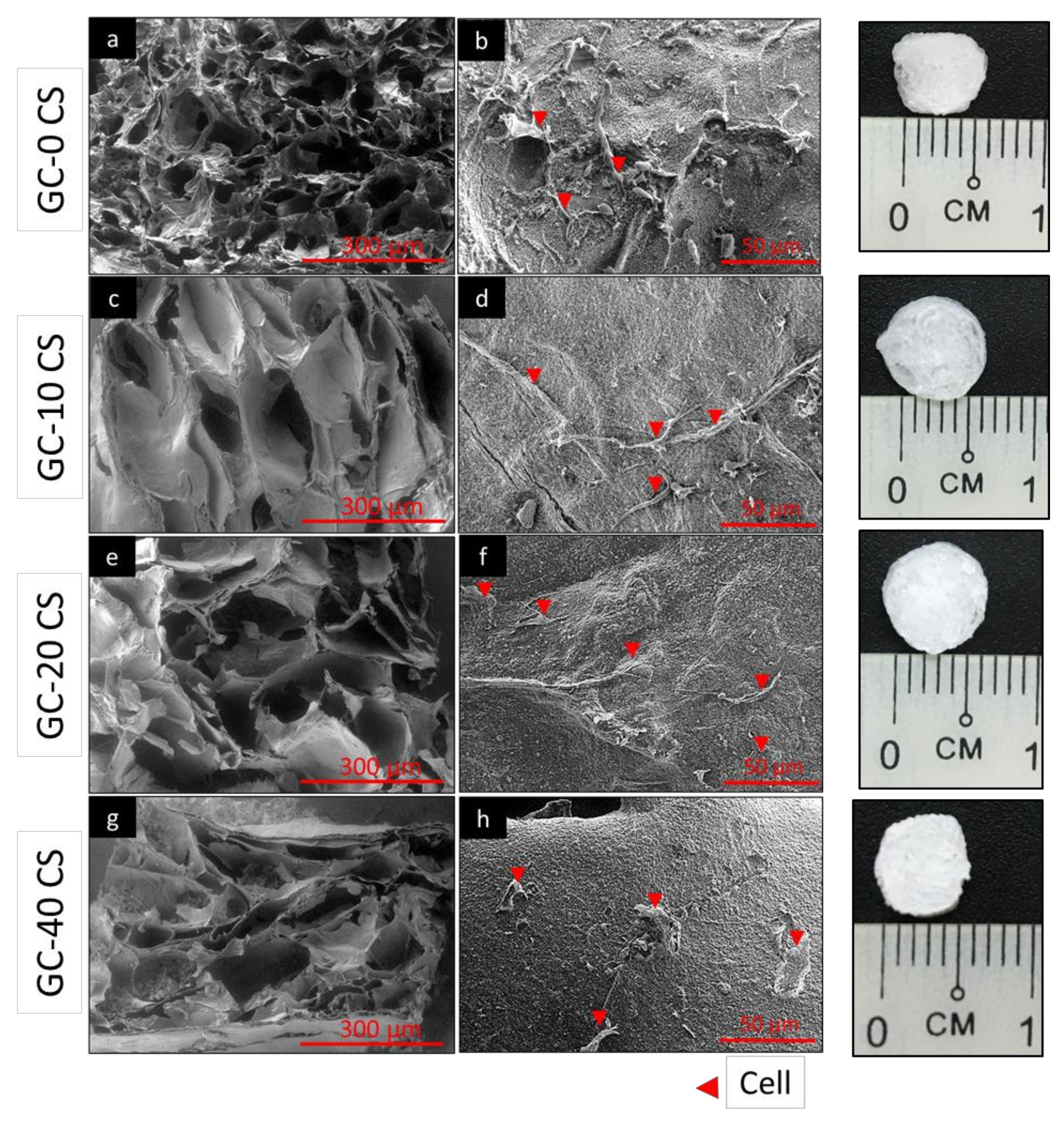
3.1. Cell Attachment Analysis
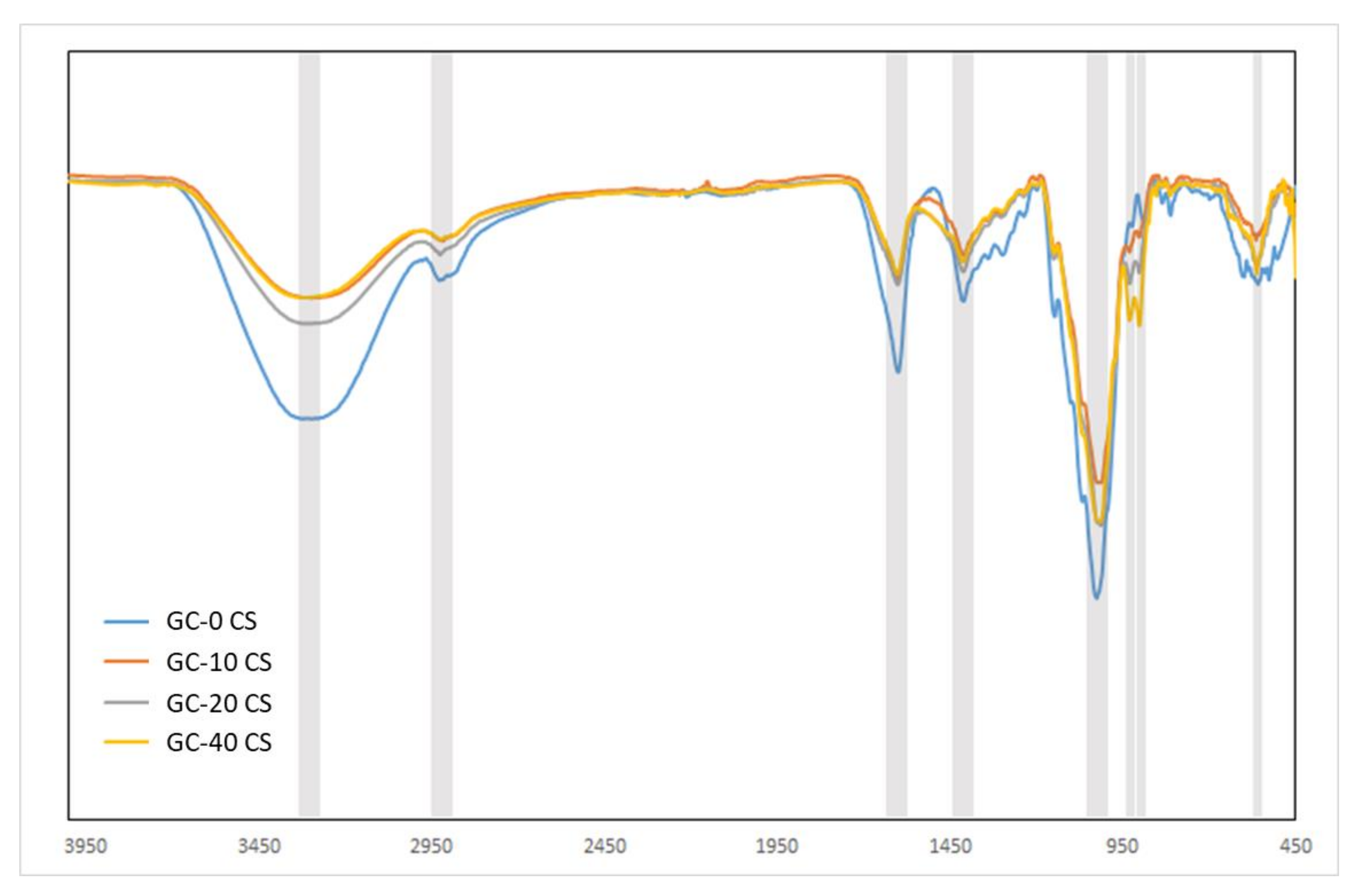
3.2. Chemical Structure
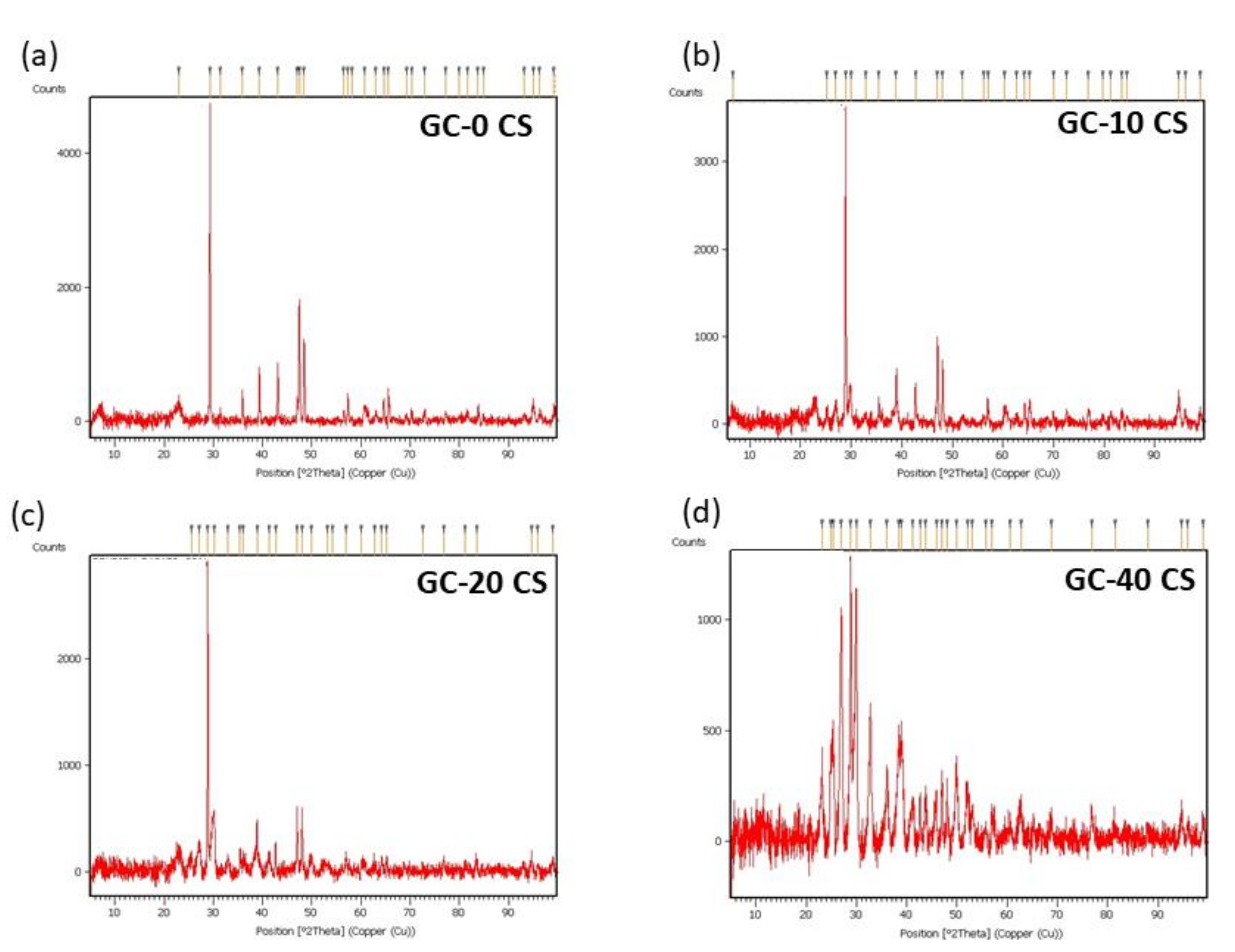
3.3. Phase Identification
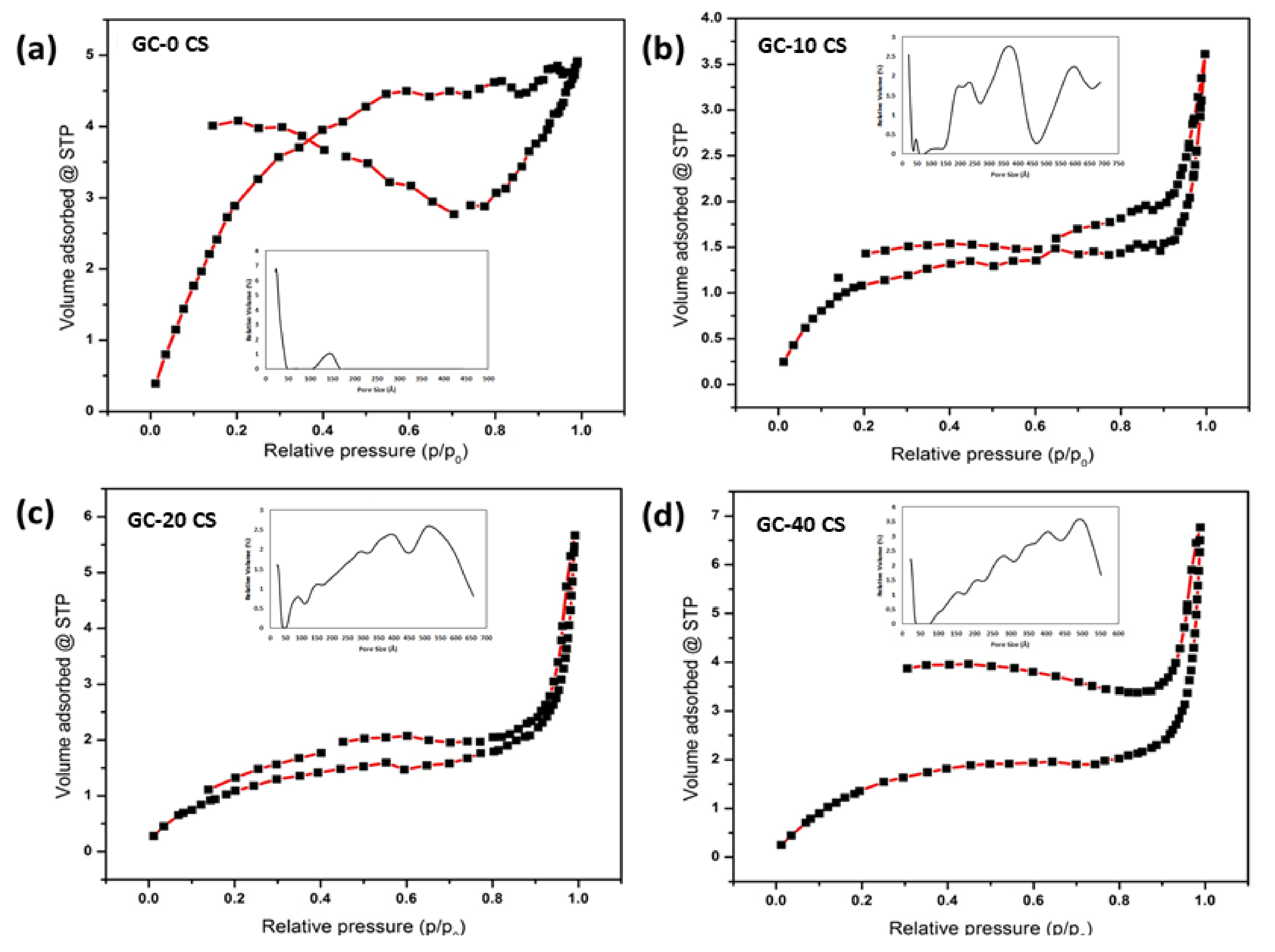
3.4. Specific Surface Area Analysis
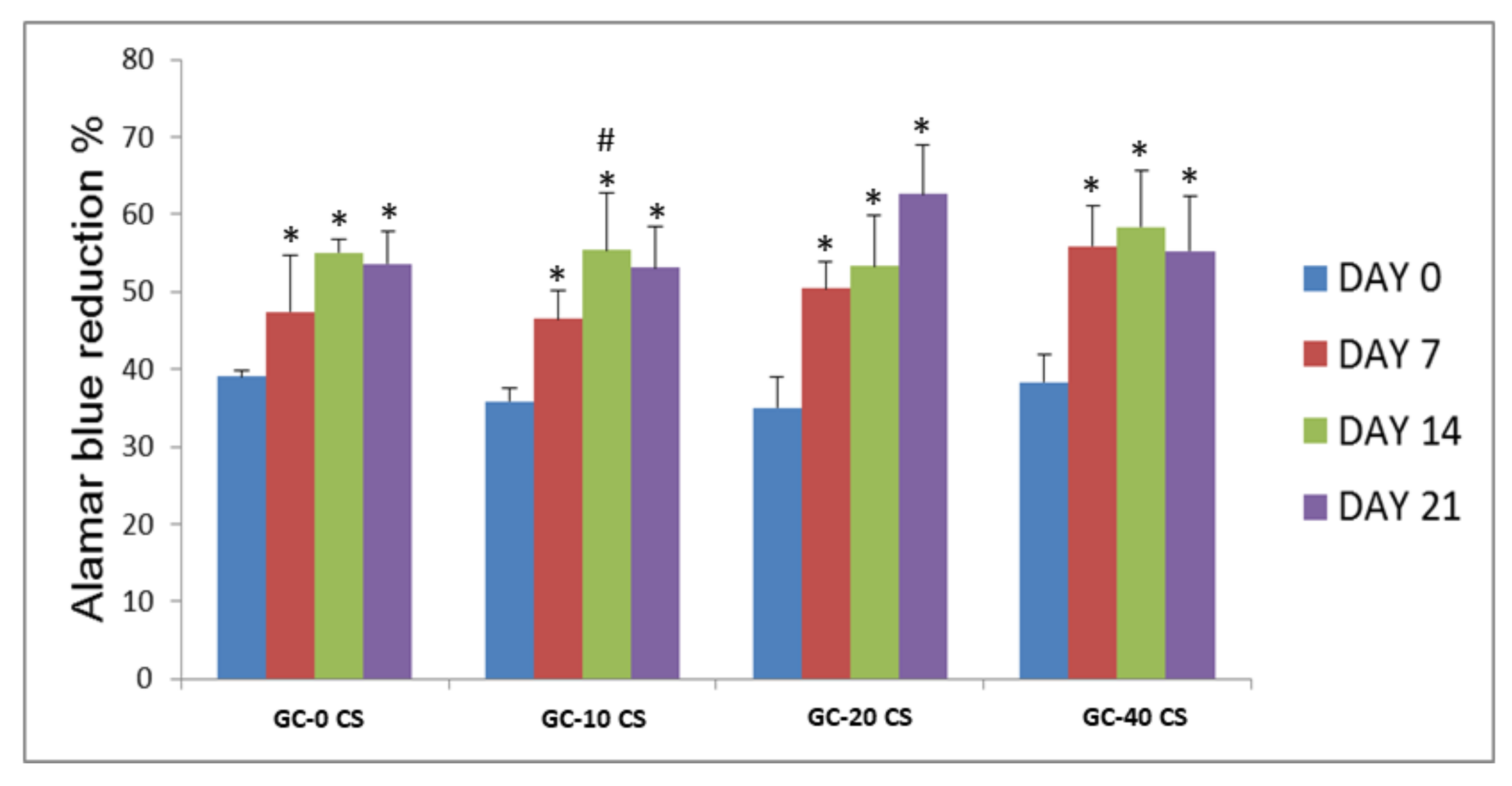
3.5. Cell Proliferation and Viability
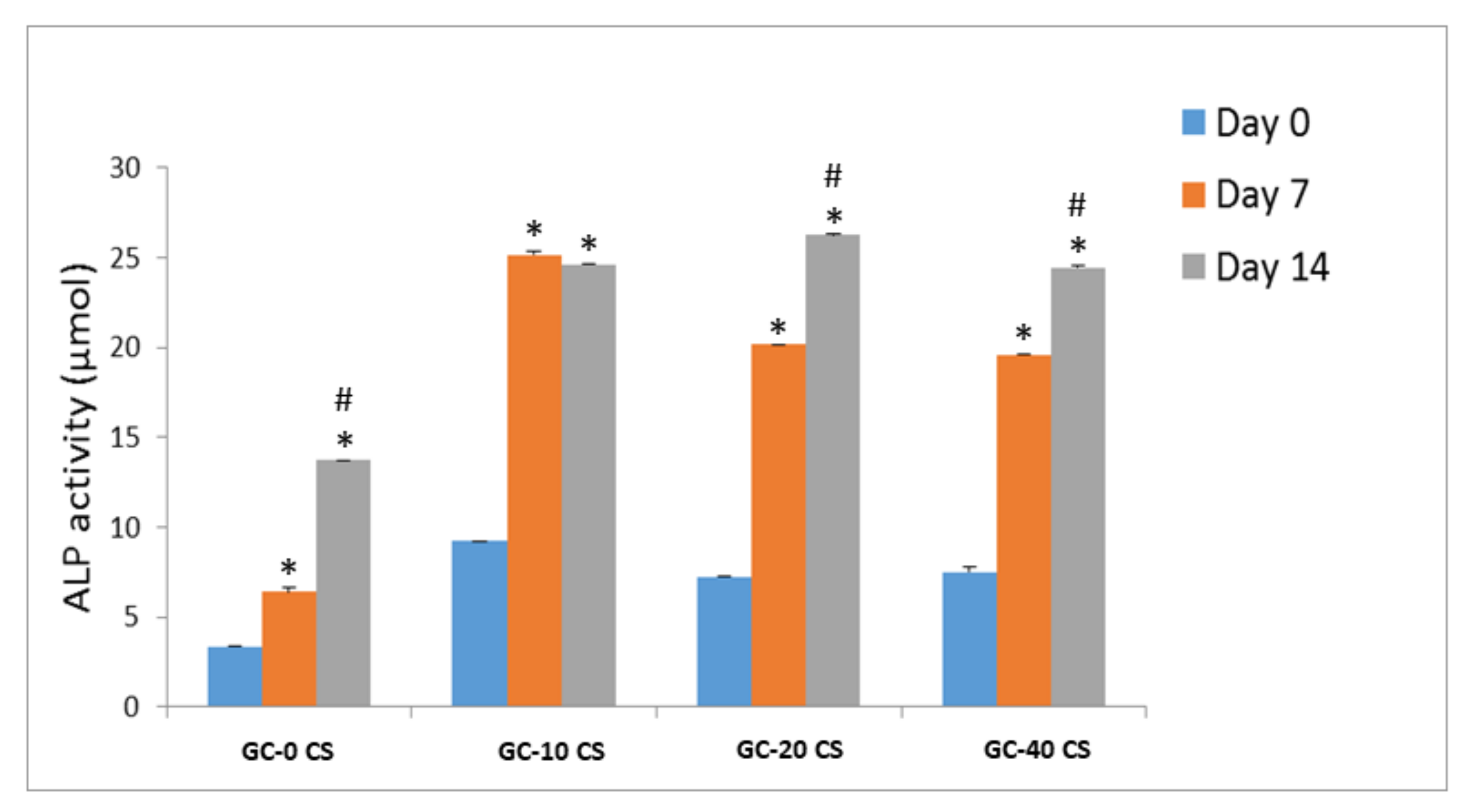
3.6. Bone Early Marker (ALP)
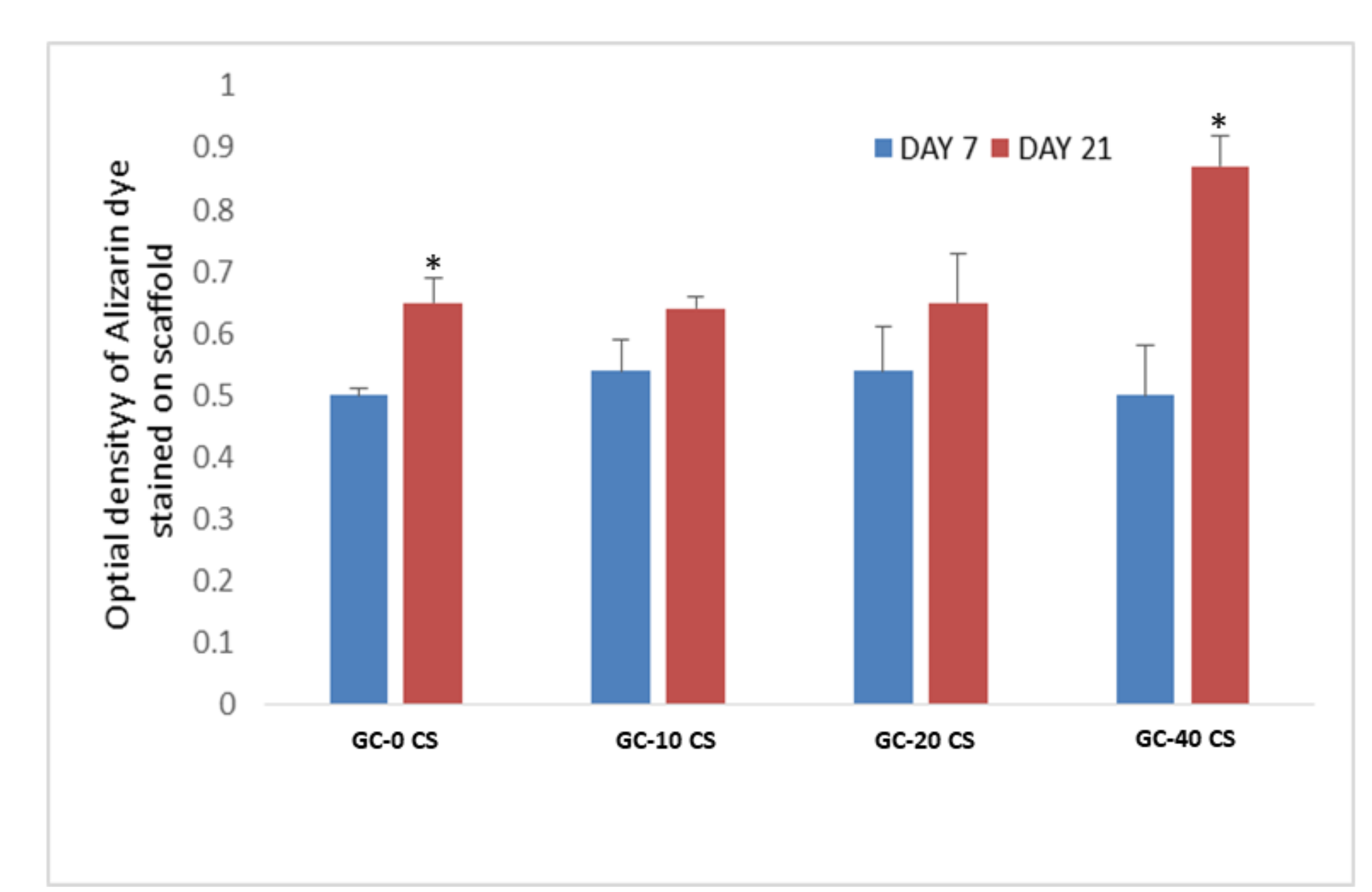
3.7. Detection of Calcium Deposits (Alizarin-Red Staining)
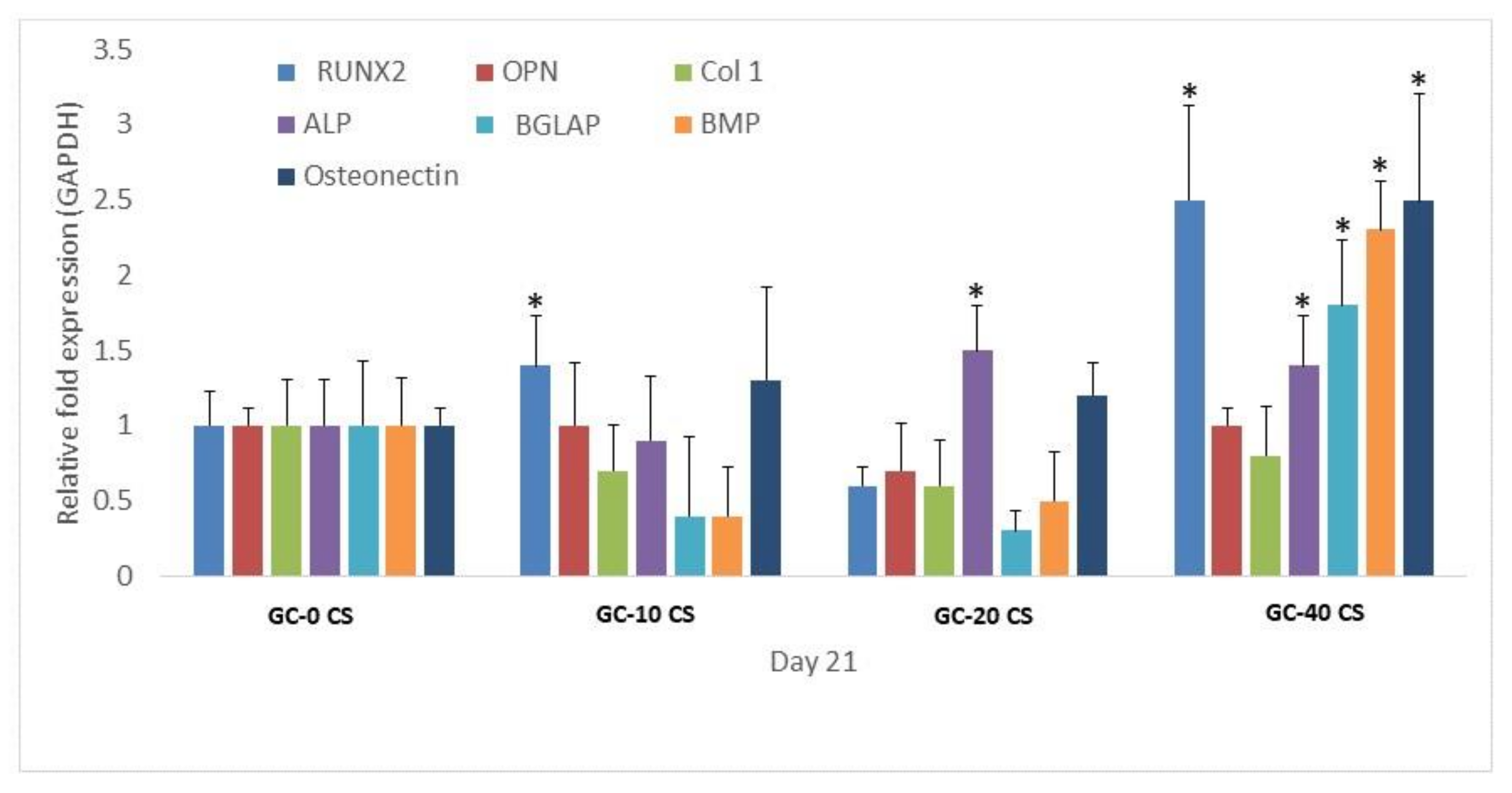
3.8. Osteogenic Gene Expression
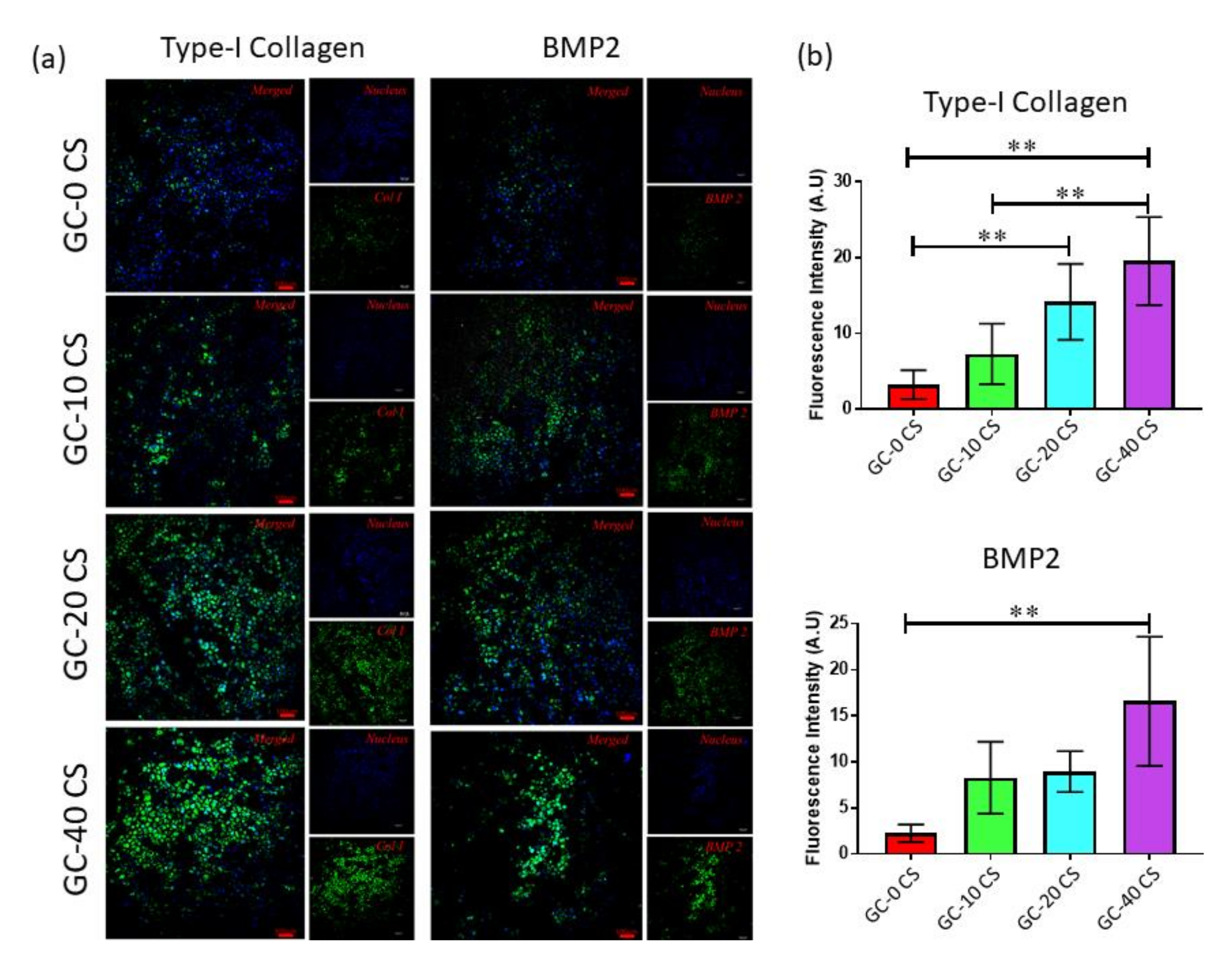
3.9. Osteogenic Protein Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dinoro, J.; Maher, M.; Talebian, S.; Jafarkhani, M.; Mehrali, M.; Orive, G.; Foroughi, J.; Lord, M.S.; Dolatshahi-Pirouz, A. Sulfated polysaccharide-based scaffolds for orthopaedic tissue engineering. Biomaterials 2019, 214, 119214. [Google Scholar] [CrossRef]
- Mohan, S.; Raghavendran, H.B.; Karunanithi, P.; Murali, M.R.; Naveen, S.V.; Talebian, S.; Mehrali, M.; Mehrali, M.; Natarajan, E.; Chan, C.K.; et al. Incorporation of Human-Platelet-Derived Growth Factor-BB Encapsulated Poly(lactic-co-glycolic acid) Microspheres into 3D CORAGRAF Enhances Osteogenic Differentiation of Mesenchymal Stromal Cells. ACS Appl. Mater. Interfaces 2017, 9, 9291–9303. [Google Scholar] [CrossRef]
- Araújo, L.K.; Antunes, G.S.; Melo, M.M.; Castro, S., II. Brazilian dentists’ perceptions of using bone grafts: An inland survey. Acta Odontol. Latinoam. AOL 2020, 33, 165–173. [Google Scholar]
- Zion Market Research. Global Dental Bone Graft Substitutes Market Worth Reach USD 931 Million by 2025. Available online: http://menafn.com/1098701890/Global-Dental-BoneGraft-Substitutes-Market-Worth-Reach-USD-931-MillionBy-2025 (accessed on 31 August 2021).
- Mehrali, M.; Thakur, A.; Pennisi, C.P.; Talebian, S.; Arpanaei, A.; Nikkhah, M.; Dolatshahi-Pirouz, A. Nanoreinforced Hydrogels for Tissue Engineering: Biomaterials that are Compatible with Load-Bearing and Electroactive Tissues. Adv. Mater. 2017, 29, 1603612. [Google Scholar] [CrossRef]
- Mehrali, M.; Thakur, A.; Kadumudi, F.B.; Pierchala, M.K.; Cordova, J.A.V.; Shahbazi, M.A.; Mehrali, M.; Pennisi, C.P.; Orive, G.; Gaharwar, A.K.; et al. Pectin Methacrylate (PEMA) and Gelatin-Based Hydrogels for Cell Delivery: Converting Waste Materials into Biomaterials. ACS Appl. Mater. Interfaces 2019, 11, 12283–12297. [Google Scholar] [CrossRef] [PubMed]
- Saravanan, S.; Leena, R.S.; Selvamurugan, N. Chitosan based biocomposite scaffolds for bone tissue engineering. Int. J. Biol. Macromol. 2016, 93, 1354–1365. [Google Scholar] [CrossRef] [PubMed]
- Ahsan, S.M.; Thomas, M.; Reddy, K.K.; Sooraparaju, S.G.; Asthana, A.; Bhatnagar, I. Chitosan as biomaterial in drug delivery and tissue engineering. Int. J. Biol. Macromol. 2018, 110, 97–109. [Google Scholar] [CrossRef]
- LogithKumar, R.; KeshavNarayan, A.; Dhivya, S.; Chawla, A.; Saravanan, S.; Selvamurugan, N. A review of chitosan and its derivatives in bone tissue engineering. Carbohydr. Polym. 2016, 151, 172–188. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.R.; Gilmore, K.J.; Wallace, G.G.; In Het Panhuis, M. Tissue engineering with gellan gum. Biomater. Sci. 2016, 4, 1276–1290. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, A.C.; Sabino, R.M.; Souza, P.R.; Muniz, E.C.; Popat, K.C.; Kipper, M.J.; Zola, R.S.; Martins, A.F. Chitosan/gellan gum ratio content into blends modulates the scaffolding capacity of hydrogels on bone mesenchymal stem cells. Mater. Sci. Eng. C 2020, 106, 110258. [Google Scholar] [CrossRef]
- Sant, S.; Coutinho, D.F.; Gaharwar, A.K.; Neves, N.M.; Reis, R.L.; Gomes, M.E.; Khademhosseini, A. Self-assembled Hydrogel Fiber Bundles from Oppositely Charged Polyelectrolytes Mimic Micro-/nanoscale Hierarchy of Collagen. Adv. Funct. Mater. 2017, 27, 1606273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dahiya, S.; Rani, R.; Kumar, S.; Dhingra, D.; Dilbaghi, N. Chitosan-Gellan Gum Bipolymeric Nanohydrogels—a Potential Nanocarrier for the Delivery of Epigallocatechin Gallate. BioNanoScience 2017, 7, 508–520. [Google Scholar] [CrossRef]
- Sonje, A.G.; Mahajan, H.S. Nasal inserts containing ondansetron hydrochloride based on Chitosan-gellan gum polyelectrolyte complex: In vitro-in vivo studies. Mater. Sci. Eng. C 2016, 64, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Pina, S.; Ribeiro, V.P.; Marques, C.F.; Maia, F.R.; Silva, T.H.; Reis, R.L.; Oliveira, J.M. Scaffolding Strategies for Tissue Engineering and Regenerative Medicine Applications. Materials 2019, 12, 1824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehrali, M.; Akhiani, A.R.; Talebian, S.; Mehrali, M.; Latibari, S.T.; Dolatshahi-Pirouz, A.; Metselaar, H.S.C. Electrophoretic deposition of calcium silicate–reduced graphene oxide composites on titanium substrate. J. Eur. Ceram. Soc. 2016, 36, 319–332. [Google Scholar] [CrossRef] [Green Version]
- Mehrali, M.; Moghaddam, E.; Shirazi, S.F.; Baradaran, S.; Mehrali, M.; Latibari, S.T.; Metselaar, H.S.; Kadri, N.A.; Zandi, K.; Osman, N.A. Synthesis, mechanical properties, and in vitro biocompatibility with osteoblasts of calcium silicate-reduced graphene oxide composites. ACS Appl. Mater. Interfaces 2014, 6, 3947–3962. [Google Scholar] [CrossRef]
- Peng, X.Y.; Hu, M.; Liao, F.; Yang, F.; Ke, Q.F.; Guo, Y.P.; Zhu, Z.H. La-Doped mesoporous calcium silicate/chitosan scaffolds for bone tissue engineering. Biomater. Sci. 2019, 7, 1565–1573. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Wang, B.; Gao, Y.; Bai, T.C. Chitosan fibers enhanced gellan gum hydrogels with superior mechanical properties and water-holding capacity. Carbohydr. Polym. 2013, 97, 152–158. [Google Scholar] [CrossRef]
- Iaquinta, M.R.; Mazzoni, E.; Bononi, I.; Rotondo, J.C.; Mazziotta, C.; Montesi, M.; Sprio, S.; Tampieri, A.; Tognon, M.; Martini, F. Adult Stem Cells for Bone Regeneration and Repair. Front. Cell Dev. Biol. 2019, 7, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puvaneswary, S.; Raghavendran, H.B.; Talebian, S.; Murali, M.R.; Mahmod, S.A.; Singh, S.; Kamarul, T. Incorporation of Fucoidan in β-Tricalcium phosphate-Chitosan scaffold prompts the differentiation of human bone marrow stromal cells into osteogenic lineage. Sci. Rep. 2016, 6, 24202. [Google Scholar] [CrossRef] [Green Version]
- Mehrali, M.; Moghaddam, E.; Seyed Shirazi, S.F.; Baradaran, S.; Mehrali, M.; Latibari, S.T.; Metselaar, H.S.; Kadri, N.A.; Zandi, K.; Osman, N.A. Mechanical and in vitro biological performance of graphene nanoplatelets reinforced calcium silicate composite. PLoS ONE 2014, 9, e106802. [Google Scholar] [CrossRef] [Green Version]
- Krishnamurithy, G.; Yahya, N.A.; Mehrali, M.; Mehrali, M.; Mohan, S.; Murali, M.R.; Raghavendran, H.R.B.; Kamarul, T. Effects of carbon doping on the microstructural, micro/nano-mechanical, and mesenchymal stromal cells biocompatibility and osteogenic differentiation properties of alumina. Ceram. Int. 2016, 42, 18247–18256. [Google Scholar] [CrossRef]
- Rizwan, M.; Genasan, K.; Murali, M.R.; Balaji Raghavendran, H.R.; Alias, R.; Cheok, Y.Y.; Wong, W.F.; Mansor, A.; Hamdi, M.; Basirun, W.J.; et al. In vitro evaluation of novel low-pressure spark plasma sintered HA–BG composite scaffolds for bone tissue engineering. Rsc. Adv. 2020, 10, 23813–23828. [Google Scholar] [CrossRef]
- Krishnamurithy, G.; Mohan, S.; Yahya, N.A.; Mansor, A.; Murali, M.R.; Raghavendran, H.R.B.; Choudhary, R.; Sasikumar, S.; Kamarul, T. The physicochemical and biomechanical profile of forsterite and its osteogenic potential of mesenchymal stromal cells. PLoS ONE 2019, 14, e0214212. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Lee, D.; Song, D.; Kim, H.-M.; Kim, S.-Y. Biocompatibility and Bioactivity of Set Direct Pulp Capping Materials on Human Dental Pulp Stem Cells. Materials 2020, 13, 3925. [Google Scholar] [CrossRef] [PubMed]
- Krishnamurithy, G.; Murali, M.R.; Hamdi, M.; Abbas, A.A.; Raghavendran, H.B.; Kamarul, T. Proliferation and osteogenic differentiation of mesenchymal stromal cells in a novel porous hydroxyapatite scaffold. Regen. Med. 2015, 10, 579–590. [Google Scholar] [CrossRef]
- Lee, S.; Choi, J.H.; Park, A.; Rim, M.; Youn, J.; Lee, W.; Song, J.E.; Khang, G. Advanced gellan gum-based glycol chitosan hydrogel for cartilage tissue engineering biomaterial. Int. J. Biol. Macromol. 2020, 158, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Diez-Garcia, M.; Gaitero, J.J.; Dolado, J.S.; Aymonier, C. Ultra-Fast Supercritical Hydrothermal Synthesis of Tobermorite under Thermodynamically Metastable Conditions. Angew. Chem. 2017, 56, 3162–3167. [Google Scholar] [CrossRef]
- Mukhopadhyay, P.; Maity, S.; Chakraborty, S.; Rudra, R.; Ghodadara, H.; Solanki, M.; Chakraborti, A.S.; Prajapati, A.K.; Kundu, P.P. Oral delivery of quercetin to diabetic animals using novel pH responsive carboxypropionylated chitosan/alginate microparticles. RSC Adv. 2016, 6, 73210–73221. [Google Scholar] [CrossRef]
- Castro-Silva, I.I.; Zambuzzi, W.F.; de Oliveira Castro, L.; Granjeiro, J.M. Periosteal-derived cells for bone bioengineering: A promising candidate. Clin. Oral. Implant. Res. 2012, 23, 1238–1242. [Google Scholar] [CrossRef] [PubMed]
- Babatunde, E.; Ighalo, J.O.; Akolo, S.; Adeniyi, A.; Adepoju, L. Investigation of Biomaterial Characteristics of Chitosan Produced from Crab Shells. Mater. Int. 2020, 2, 303–310. [Google Scholar] [CrossRef]
- Ikeda, K.; Sugawara, S.; Taira, M.; Sato, H.; Hatakeyama, W.; Kihara, H.; Kondo, H. Ectopic Bone Formation in Muscles Using Injectable Bone-forming Material Consisting of Cross-linked Hyaluronic Acid, Bone Morphogenetic Protein, and Nano-hydroxyapatite. Nano Biomed. 2019, 11, 11–20. [Google Scholar] [CrossRef]
- Islam, M.M.; Shahruzzaman, M.; Biswas, S.; Nurus Sakib, M.; Rashid, T.U. Chitosan based bioactive materials in tissue engineering applications-A review. Bioact. Mater. 2020, 5, 164–183. [Google Scholar] [CrossRef] [PubMed]
- Potaś, J.; Szymańska, E.; Winnicka, K. Challenges in developing of chitosan–Based polyelectrolyte complexes as a platform for mucosal and skin drug delivery. Eur. Polym. J. 2020, 140, 110020. [Google Scholar] [CrossRef]
- De Oliveira, A.C.; Vilsinski, B.H.; Bonafé, E.G.; Monteiro, J.P.; Kipper, M.J.; Martins, A.F. Chitosan content modulates durability and structural homogeneity of chitosan-gellan gum assemblies. Int. J. Biol. Macromol. 2019, 128, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Yadav, L.R.; Chandran, S.V.; Lavanya, K.; Selvamurugan, N. Chitosan-based 3D-printed scaffolds for bone tissue engineering. Int. J. Biol. Macromol. 2021, 183, 1925–1938. [Google Scholar] [CrossRef] [PubMed]
- Gao, C.; Peng, S.; Feng, P.; Shuai, C. Bone biomaterials and interactions with stem cells. Bone Res. 2017, 5, 17059. [Google Scholar] [CrossRef]
- Krishnamurithy, G.; Murali, M.R.; Hamdi, M.; Abbas, A.A.; Raghavendran, H.B.; Kamarul, T. Characterization of bovine-derived porous hydroxyapatite scaffold and its potential to support osteogenic differentiation of human bone marrow derived mesenchymal stem cells. Ceram. Int. 2014, 40, 771–777. [Google Scholar] [CrossRef]
- De Oliveira Lomelino, R.; Castro-Silva, I.I.; Linhares, A.B.R.; Alves, G.G.; de Albuquerque Santos, S.R.; Gameiro, V.S.; Rossi, A.M.; Granjeiro, J.M. The association of human primary bone cells with biphasic calcium phosphate (βTCP/HA 70: 30) granules increases bone repair. J. Mater. Sci. Mater. Med. 2012, 23, 781–788. [Google Scholar] [CrossRef]
- Komori, T. Regulation of Proliferation, Differentiation and Functions of Osteoblasts by Runx2. Int. J. Mol. Sci. 2019, 20, 1694. [Google Scholar] [CrossRef] [Green Version]
- Braga, V.; Gatti, D.; Rossini, M.; Colapietro, F.; Battaglia, E.; Viapiana, O.; Adami, S. Bone turnover markers in patients with osteogenesis imperfecta. Bone 2004, 34, 1013–1016. [Google Scholar] [CrossRef]
- De Godoy, R.F.; Hutchens, S.; Campion, C.; Blunn, G. Silicate-substituted calcium phosphate with enhanced strut porosity stimulates osteogenic differentiation of human mesenchymal stem cells. J. Mater. Sci. Mater. Med. 2015, 26, 54. [Google Scholar] [CrossRef]
- Mathews, S.; Bhonde, R.; Gupta, P.K.; Totey, S. Extracellular matrix protein mediated regulation of the osteoblast differentiation of bone marrow derived human mesenchymal stem cells. Differentiation 2012, 84, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Venkatraman, S.K.; Swamiappan, S. Review on calcium- and magnesium-based silicates for bone tissue engineering applications. J. Biomed. Mater. Research. Part. A 2020, 108, 1546–1562. [Google Scholar] [CrossRef] [PubMed]
- Tannoury, C.A.; An, H.S. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J. Off. J. N. Am. Spine Soc. 2014, 14, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Borgiani, E.; Duda, G.N.; Willie, B.M.; Checa, S. Bone morphogenetic protein 2-induced cellular chemotaxis drives tissue patterning during critical-sized bone defect healing: An in silico study. Biomech. Modeling Mechanobiol. 2021, 20, 1627–1644. [Google Scholar] [CrossRef] [PubMed]
- Zhai, D.; Xu, M.; Liu, L.; Chang, J.; Wu, C. Silicate-based bioceramics regulating osteoblast differentiation through a BMP2 signalling pathway. J. Mater. Chem. B 2017, 5, 7297–7306. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, K.; Karsdal, M.A. Chapter 1-Type I Collagen. In Biochemistry of Collagens, Laminins and Elastin; Karsdal, M.A., Ed.; Academic Press: Cambridge, MA, USA, 2016; pp. 1–11. [Google Scholar] [CrossRef]
| Name | Sequence |
|---|---|
| Col1 Forward | CCCGCAGGCTCCTCCCAG |
| Col1Reverse | AAGCCCGGATCTGCCCTATTTAT |
| OPN Forward | CAGCCAGGACTCCATTGACTCGA |
| OPN Reverse | CCACACTATCACCTCGGCCATCA |
| BGLAP Forward | GGAGGGCAGCGAGGTAGTGAAGA |
| BGLAP Reverse | GCCTCCTGAAAGCCGATGTGGT |
| RUNX2 Forward | CCGCCATGCACCACCACCT |
| RUNX2 Reverse | CTGGGCCACTGCTGAGGAATTT |
| BMP2 Forward | TGGCCCACTTGGAGGAGAAACA |
| BMP2 Reverse | CGCTGTTTGTGTTTGGCTTGACG |
| ALP Forward | GATGTGGAGTATGAGAGTGACG |
| ALP Reverse | GGTCAAGGGTCAGGAGTTC |
| Osteonectin Forward | TTGCAATGGGCCACATACCT |
| Osteonectin Reverse | GGGCCAATCTCTCCTACTGC |
| S. No. | Sample Name | BET Surface Area m2/g | Pore Volume cc/g | Pore Size nm |
|---|---|---|---|---|
| 1 | GC-0 CS | 16.72 | 0.0040 | 19.03 |
| 2 | GC-10 CS | 4.80 | 0.0052 | 5.79 |
| 3 | GC-20 CS | 4.63 | 0.0093 | 6.99 |
| 4 | GC-40 CS | 6.72 | 0.0057 | 41.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genasan, K.; Mehrali, M.; Veerappan, T.; Talebian, S.; Malliga Raman, M.; Singh, S.; Swamiappan, S.; Mehrali, M.; Kamarul, T.; Balaji Raghavendran, H.R. Calcium-Silicate-Incorporated Gellan-Chitosan Induced Osteogenic Differentiation in Mesenchymal Stromal Cells. Polymers 2021, 13, 3211. https://doi.org/10.3390/polym13193211
Genasan K, Mehrali M, Veerappan T, Talebian S, Malliga Raman M, Singh S, Swamiappan S, Mehrali M, Kamarul T, Balaji Raghavendran HR. Calcium-Silicate-Incorporated Gellan-Chitosan Induced Osteogenic Differentiation in Mesenchymal Stromal Cells. Polymers. 2021; 13(19):3211. https://doi.org/10.3390/polym13193211
Chicago/Turabian StyleGenasan, Krishnamurithy, Mohammad Mehrali, Tarini Veerappan, Sepehr Talebian, Murali Malliga Raman, Simmrat Singh, Sasikumar Swamiappan, Mehdi Mehrali, Tunku Kamarul, and Hanumantha Rao Balaji Raghavendran. 2021. "Calcium-Silicate-Incorporated Gellan-Chitosan Induced Osteogenic Differentiation in Mesenchymal Stromal Cells" Polymers 13, no. 19: 3211. https://doi.org/10.3390/polym13193211
APA StyleGenasan, K., Mehrali, M., Veerappan, T., Talebian, S., Malliga Raman, M., Singh, S., Swamiappan, S., Mehrali, M., Kamarul, T., & Balaji Raghavendran, H. R. (2021). Calcium-Silicate-Incorporated Gellan-Chitosan Induced Osteogenic Differentiation in Mesenchymal Stromal Cells. Polymers, 13(19), 3211. https://doi.org/10.3390/polym13193211







