Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review
Abstract
1. Introduction
2. Material and Methods
2.1. Focus Questions
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Inclusion and Exclusion Criteria
2.5. Risk of Bias
3. Results
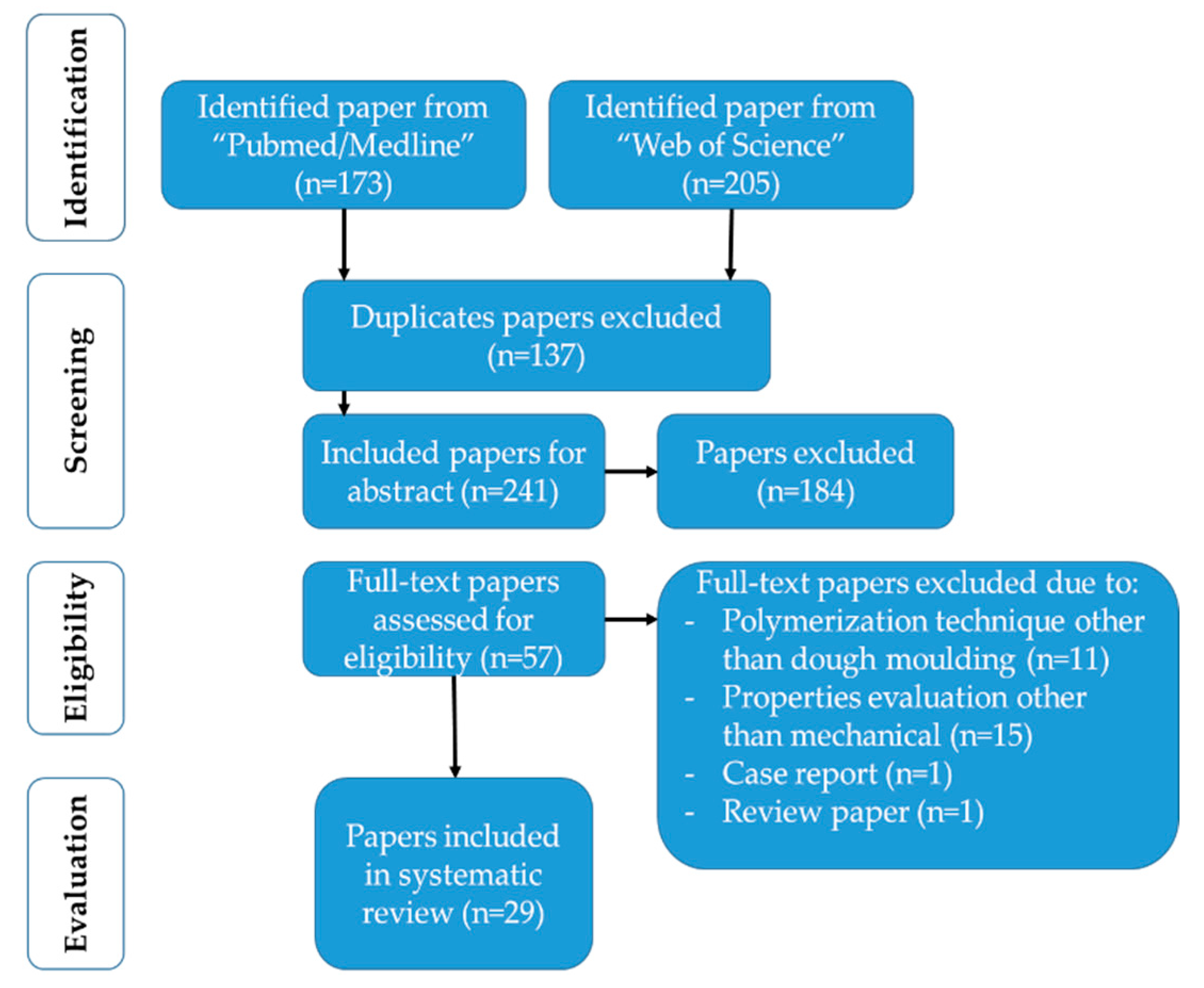
3.1. Data Selection
3.2. Quality Assessment
3.3. Data Analysis
4. Discussion
5. Conclusions
- (1)
- A wide variety of denture base resin reinforcing agents is available, which makes it difficult to compare results;
- (2)
- FS is the most commonly used testing method among investigators for the evaluation of the reinforcing effect on denture base resin;
- (3)
- Up to 5 wt.% of filler loading in denture base resin seems practicable and effective in reinforcing the denture base. At higher filler loadings, the FS of a denture base resin is reduced;
- (4)
- The FT of a denture base resin increases provided that there is an interfacial adhesion between the reinforcing agent and a denture base resin;
- (5)
- The agglomeration of the reinforcing agents increases the SH of a material. Decreased microhardness at elevated loadings might suggest that the denture base resin is not reinforced adequately or the EM of a reinforcing agent is lower than that of the resin itself;
- (6)
- Agglomeration or a loosely attached reinforcing agent in a resin matrix decreases the IS;
- (7)
- The hybridization of fillers in denture base resin seems to be a viable option.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Khindria, S.; Mittal, S.; Sukhija, U. Evolution of denture base materials. J. Indian Prosthodont. Soc. 2009, 9, 64–69. [Google Scholar]
- Kumar, M.V.; Bhagath, S.; Jei, J.B. Historical interest of denture base materials. J. Dent. Sci. 2010, 1, 103–105. [Google Scholar]
- Khan, A.A.; Mirza, E.H.; Syed, J.; Al-Khureif, A.; Mehmood, A.; Vallittu, P.K.; Alfotawi, R. Single and multi-walled carbon nanotube fillers in poly(methyl methacrylate)-based implant material. J. Biomater. Tissue Eng. 2017, 7, 798–806. [Google Scholar] [CrossRef]
- Ayaz, E.A.; Durkan, R.; Bagis, B. The effect of acrylamide incorporation on the thermal and physical properties of denture resins. J. Adv. Prosthodont. 2013, 5, 110–117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef]
- Hassan, M.; Asghar, M.; Din, S.U.; Zafar, M.S. Thermoset polymethacrylate-based materials for dental applications. In Materials for Biomedical Engineering; Grumezescu, V., Grumezescu, A.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 273–308. [Google Scholar]
- Vuorinen, A.-M.; Dyer, S.R.; Lassila, L.V.; Vallittu, P.K. Effect of rigid rod polymer filler on mechanical properties of poly-methyl methacrylate denture base material. Dent. Mater. 2008, 24, 708–713. [Google Scholar] [CrossRef]
- Ali Sabri, B.; Satgunam, M.; Abreeza, N.; Abed, A.N. A review on enhancements of PMMA Denture Base Material with Different Nano-Fillers. Cogent. Eng. 2021, 8, 1875968. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 2017, 3801–3812. [Google Scholar] [CrossRef]
- Prajwala, N.; Kumar, C.R.; Sujesh, M.; Rao, D.C.; Pavani, L. Denture base reinforcing materials-A review. IP. Ann. Prosthodont. Restor. Dent. 2020, 6, 52–59. [Google Scholar] [CrossRef]
- Jagger, D.; Jagger, R.; Allen, S.; Harrison, A. An investigation into the transverse and impact strength ofhigh strength’denture base acrylic resins. J. Oral. Rehabil. 2002, 29, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Franklin, P.; Wood, D.J.; Bubb, N.L. Reinforcement of poly(methyl methacrylate) denture base with glass flake. Dent. Mater. 2005, 21, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Ayaz, E.A.; Durkan, R. Influence of acrylamide monomer addition to the acrylic denture-base resins on mechanical and physical properties. Int. J. Oral. Sci. 2013, 5, 229–235. [Google Scholar] [CrossRef]
- Jagger, D.; Harrison, A.; Jandt, K. The reinforcement of dentures. J. Oral. Rehabil. 1999, 26, 185–194. [Google Scholar] [CrossRef]
- Narva, K.K.; Lassila, L.V.; Vallittu, P.K. Flexural fatigue of denture base polymer with fiber-reinforced composite reinforcement. Compos. A Appl. Sci. Manuf. 2005, 36, 1275–1281. [Google Scholar] [CrossRef]
- Narva, K.K.; Vallittu, P.K.; Helenius, H.; Yli-Urpo, A. Clinical survey of acrylic resin removable denture repairs with glass-fiber reinforcement. Int. J. Prosthodont. 2001, 14, 219–224. [Google Scholar]
- Zafar, M.S.; Ahmed, N. Nanoindentation and surface roughness profilometry of poly methyl methacrylate denture base materials. Technol. Health Care 2014, 22, 573–581. [Google Scholar] [CrossRef]
- Mowade, T.K.; Dange, S.P.; Thakre, M.B.; Kamble, V.D. Effect of fiber reinforcement on impact strength of heat polymerized polymethyl methacrylate denture base resin: In vitro study and SEM analysis. J. Adv. Prosthodont. 2012, 4, 30–36. [Google Scholar] [CrossRef]
- Khosravani, M.R. Mechanical behavior of restorative dental composites under various loading conditions. J. Mech. Behav. Biomed. Mater. 2019, 93, 151–157. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Ebrahim, M.I. Effect of zirconium oxide nano-fillers addition on the flexural strength, fracture toughness, and hardness of heat-polymerized acrylic resin. World. J. Nanosci. Eng. 2014, 2014, 50–57. [Google Scholar] [CrossRef]
- Mallineni, S.K.; Nuvvula, S.; Matinlinna, J.P.; Yiu, C.K.; King, N.M. Biocompatibility of various dental materials in contemporary dentistry: A narrative insight. J. Investig. Clin. Dent. 2013, 4, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Aguirre, B.C.; Chen, J.H.; Kontogiorgos, E.D.; Murchison, D.F.; Nagy, W.W. Flexural strength of denture base acrylic resins processed by conventional and CAD-CAM methods. J. Prosthet. Dent. 2020, 123, 641–646. [Google Scholar] [CrossRef]
- Yadav, R.; Kumar, M. Dental restorative composite materials: A review. J. Oral Biosci. 2019, 61, 78–83. [Google Scholar] [CrossRef]
- Gad, M.M.; Rahoma, A.; Al-Thobity, A.M.; ArRejaie, A.S. Influence of incorporation of ZrO(2) nanoparticles on the repair strength of polymethyl methacrylate denture bases. Int. J. Nanomed. 2016, 11, 5633–5643. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Skupien, J.; Cenci, M.; Moraes, R.; Pereira-Cenci, T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Br. Med. J. 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Shakeri, F.; Nodehi, A.; Atai, M. PMMA/double-modified organoclay nanocomposites as fillers for denture base materials with improved mechanical properties. J. Mech. Behav. Biomed. Mater. 2019, 90, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Kul, E.; Aladağ, L.İ.; Yesildal, R. Evaluation of thermal conductivity and flexural strength properties of poly(methyl methacrylate) denture base material reinforced with different fillers. J. Prosthet. Dent. 2016, 116, 803–810. [Google Scholar] [CrossRef]
- Gad, M.M.; Abualsaud, R.; Al-Thobity, A.M.; Baba, N.Z.; Al-Harbi, F.A. Influence of addition of different nanoparticles on the surface properties of poly(methylmethacrylate) denture base material. J. Prosthodont. 2020, 29, 422–428. [Google Scholar] [CrossRef]
- Ali, A.A.A.R.; John, J.; Mani, S.A.; El-Seedi, H.R. Effect of Thermal Cycling on Flexural Properties of Microcrystalline Cellulose-Reinforced Denture Base Acrylic Resins. J. Prosthodont. 2020, 29, 611–616. [Google Scholar]
- Cevik, P.; Yildirim-Bicer, A.Z. The effect of silica and prepolymer nanoparticles on the mechanical properties of denture base acrylic resin. J. Prosthodont. 2018, 27, 763–770. [Google Scholar] [CrossRef]
- Karci, M.; Demir, N.; Yazman, S. Evaluation of flexural strength of different denture base materials reinforced with different nanoparticles. J. Prosthodont. 2019, 28, 572–579. [Google Scholar] [CrossRef]
- Uyar, T.; Çökeliler, D.; Doğan, M.; Koçum, I.C.; Karatay, O.; Denkbaş, E.B. Electrospun nanofiber reinforcement of dental composites with electromagnetic alignment approach. Mater. Sci. Eng. C 2016, 62, 762–770. [Google Scholar] [CrossRef]
- Al-Bakri, I.; Swain, M.; Naoum, S.; Al-Omari, W.; Martin, E.; Ellakwa, A. Fluoride release, recharge and flexural properties of polymethylmethacrylate containing fluoridated glass fillers. Aus. Dent. J. 2014, 59, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Elshereksi, N.W.; Ghazali, M.J.; Muchtar, A.; Azhari, C.H. Studies on the effects of titanate and silane coupling agents on the performance of poly(methyl methacrylate)/barium titanate denture base nanocomposites. J. Dent. 2017, 56, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.-H.; Ahn, D.-H.; Park, J.-S.; Chung, Y.S.; Han, I.-S.; Lim, J.-S.; Oh, S.; Oda, Y.; Bae, J.-M. Comparison of denture base resin reinforced with polyaromatic polyamide fibers of different orientations. Dent. Mater. J. 2013, 32, 332–340. [Google Scholar] [CrossRef][Green Version]
- Yu, S.-H.; Lee, Y.; Oh, S.; Cho, H.-W.; Oda, Y.; Bae, J.-M. Reinforcing effects of different fibers on denture base resin based on the fiber type, concentration, and combination. Dent. Mater. J. 2012, 31, 1039–1046. [Google Scholar] [CrossRef]
- Kumar, G.V.; Nigam, A.; Naeem, A.; Gaur, A.; Pandey, K.K.; Deora, A. Reinforcing heat-cured poly-methyl-methacrylate resins using fibers of glass, polyaramid, and nylon: An in vitro study. J. Contemp. Dent. 2016, 17, 948–952. [Google Scholar] [CrossRef]
- Gurbuz, O.; Dikbas, I.; Unalan, F. Fatigue resistance of acrylic resin denture base material reinforced with E-glass fibres. Gerodontology 2012, 29, e710–e714. [Google Scholar] [CrossRef]
- Agha, H.; Flinton, R.; Vaidyanathan, T. Optimization of Fracture Resistance and Stiffness of Heat-Polymerized High Impact Acrylic Resin with Localized E-Glass FiBER FORCE® Reinforcement at Different Stress Points. J. Prosthodont. 2016, 25, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Wang, X.; Tang, Q.; Guo, M.; Zhao, J. Reinforcement of denture base PMMA with ZrO2 nanotubes. J. Mech. Behav. Biomed. Mater. 2014, 32, 192–197. [Google Scholar] [CrossRef]
- Mansour, M.M.; Wagner, W.C.; Chu, T.M.G. Effect of mica reinforcement on the flexural strength and microhardness of polymethyl methacrylate denture resin. J. Prosthodont. 2013, 22, 179–183. [Google Scholar] [CrossRef]
- Jiangkongkho, P.; Arksornnukit, M.; Takahashi, H. The synthesis, modification, and application of nanosilica in polymethyl methacrylate denture base. Dent. Mater. J. 2018, 37, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Al-Harbi, F.A.; Abdel-Halim, M.S.; Gad, M.M.; Fouda, S.M.; Baba, N.Z.; AlRumaih, H.S.; Akhtar, S. Effect of nanodiamond addition on flexural strength, impact strength, and surface roughness of PMMA denture base. J. Prosthodont. 2019, 28, e417–e425. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, X.; Zhu, B.; Lin, K.; Chang, J. Mechanical and thermal properties of denture PMMA reinforced with silanized aluminum borate whiskers. Dent. Mater. J. 2012, 31, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Balos, S.; Pilic, B.; Markovic, D.; Pavlicevic, J.; Luzanin, O. Poly(methyl-methacrylate) nanocomposites with low silica addition. J. Prosthet. Dent. 2014, 111, 327–334. [Google Scholar] [CrossRef]
- Asar, N.V.; Albayrak, H.; Korkmaz, T.; Turkyilmaz, I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J. Adv. Prosthodont. 2013, 5, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Chaijareenont, P.; Takahashi, H.; Nishiyama, N.; Arksornnukit, M. Effect of different amounts of 3-methacryloxypropyltrimethoxysilane on the flexural properties and wear resistance of alumina reinforced PMMA. Dent. Mater. J. 2012, 31, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Mittal, R.; Sood, V.K.; Garg, R. Effect of incorporation of silane-treated silver and aluminum microparticles on strength and thermal conductivity of PMMA. J. Prosthodont. 2012, 21, 546–551. [Google Scholar] [CrossRef]
- Galav, A.; Deogade, S.C.; Mantri, S.; Sumathi, K.; Galav, S. Effect of water storage on the flexural strength of heat-cured denture base resin reinforced with stick (s) glass fibers. Contemp. Clin. Dent. 2017, 8, 264–271. [Google Scholar]
- Mathew, M.; Shenoy, K.; Ravishankar, K. Flexural strength of hydrogen plasma-treated polypropylene fiber-reinforced polymethyl methacrylate denture base material. J. Indian Prosthodont. Soc. 2018, 18, 257–262. [Google Scholar] [CrossRef]
- Demir, H.; Özdemİr, A.K.; Doğan, D.Ö.; Tuğut, F.; Hakan, A. Effects of boron on the mechanical properties of polymethylmethacrylate denture base material. Eur. Oral. Res. 2021, 55, 45–53. [Google Scholar]
- Abdallah, R.M. Evaluation of polymethyl methacrylate resin mechanical properties with incorporated halloysite nanotubes. J. Adv. Prosthodont. 2016, 8, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-Y.; Zhang, X.-J.; Huang, Z.-L.; Zhu, B.-S.; Chen, R.-R. Hybrid effects of zirconia nanoparticles with aluminum borate whiskers on mechanical properties of denture base resin PMMA. Dent. Mater. J. 2014, 33, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Naji, S.A.; Behroozibakhsh, M.; Kashi, T.S.J.; Eslami, H.; Masaeli, R.; Mahgoli, H.; Tahriri, M.; Lahiji, M.G.; Rakhshan, V. Effects of incorporation of 2.5 and 5 wt% TiO2 nanotubes on fracture toughness, flexural strength, and microhardness of denture base poly methyl methacrylate (PMMA). J. Adv. Prosthodont. 2018, 10, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. A review of fiber-reinforced denture base resins. J. Prosthodont. 1996, 5, 270–276. [Google Scholar] [CrossRef]
- Gad, M.M.; Abualsaud, R. Behavior of PMMA denture base materials containing titanium dioxide nanoparticles: A literature review. Int. J. Biomater. 2019, 2019, 6190610. [Google Scholar] [CrossRef]
- Elshereksi, N.W.; Ghazali, M.J.; Muchtar, A.; Azhari, C.H. Perspectives for titanium-derived fillers usage on denture base composite construction: A review article. Adv. Mater. Sci. Eng. 2014, 2014, 746252. [Google Scholar] [CrossRef]
- Bangera, M.K.; Kotian, R.; Ravishankar, N. Effect of titanium dioxide nanoparticle reinforcement on flexural strength of denture base resin: A systematic review and meta-analysis. Jpn. Dent. Sci. Rev. 2020, 56, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Al-Kheraif, A.A.; Mohamed, B.A.; Perea-Lowery, L.; Säilynoja, E.; Vallittu, P.K. Influence of primers on the properties of the adhesive interface between resin composite luting cement and fiber-reinforced composite. J. Mech. Behav. Biomed. Mater. 2018, 88, 281–287. [Google Scholar] [CrossRef]
- Khan, A.A.; Mohamed, B.A.; Al-Shamrani, S.S.; Ramakrishnaiah, R.; Perea-Lowery, L.; Säilynoja, E.; Vallittu, P.K. Influence of monomer systems on the bond strength between resin composites and polymerized fiber-reinforced composite upon aging. J. Adhes. Dent. 2019, 21, 509–516. [Google Scholar] [PubMed]
- Khan, A.A.; Al-Khureif, A.A.; Saadaldin, S.A.; Mohamed, B.A.; Musaibah, A.S.; Divakar, D.D.; Eldwakhly, E. Graphene oxide-based experimental silane primers enhance shear bond strength between resin composite and zirconia. Eur. J. Oral. Sci. 2019, 127, 570–576. [Google Scholar] [CrossRef]
- Khan, A.A.; Al Kheraif, A.A.; Syed, J.; Divakar, D.D.; Matinlinna, J.P. Enhanced resin zirconia adhesion with carbon nanotubes-infused silanes: A pilot study. J. Adhes. 2018, 94, 167–180. [Google Scholar] [CrossRef]
- Islam, M.S.; Masoodi, R.; Rostami, H. The effect of nanoparticles percentage on mechanical behavior of silica-epoxy nanocomposites. J. Nanosci. 2013, 2013, 275037. [Google Scholar] [CrossRef]
- Al-Maharma, A.Y.; Sendur, P. Review of the main factors controlling the fracture toughness and impact strength properties of natural composites. Mater. Res. Express. 2018, 6, 022001. [Google Scholar] [CrossRef]
- Korkmaz, T.; Doğan, A.; Usanmaz, A. Dynamic mechanical analysis of provisional resin materials reinforced by metal oxides. Biomed. Mater. Eng. 2005, 15, 179–188. [Google Scholar]
- Mirza, E.H.; Khan, A.A.; Al-Khureif, A.A.; Saadaldin, S.A.; Mohamed, B.A.; Fareedi, F.; Khan, M.M.; Alfayez, M.; Al-Fotawi, R.; Vallittu, P.K. Characterization of osteogenic cells grown over modified graphene-oxide-biostable polymers. Biomed. Mater. 2019, 14, 065004. [Google Scholar] [CrossRef]
- Alhuthali, A.; Low, I.M. Water absorption, mechanical, and thermal properties of halloysite nanotube reinforced vinyl-ester nanocomposites. J. Mater. Sci. 2013, 48, 4260–4273. [Google Scholar] [CrossRef]
| Source | Criteria |
|---|---|
| Database | Medline/Pubmed, Web of Science |
| Date of publication | 1 January 2010–21 April 2021 |
| Keywords | fibers in denture base fillers in denture base reinforcement of denture base |
| Language | English |
| Type of paper | Laboratory research |
| Inclusion criteria | Laboratory studies that evaluated the mechanical properties of PMMA heat polymerized denture base resin |
| Exclusion criteria | Review, meta analysis, case report/series, clinical trial, denture repair, overdenture, denture teeth, implant/finite element analysis/fixed prosthesis, new polymer or polymerization technique |
| Journal category | Dental, medline, materials science |
| Keywords | Database Source | |||
|---|---|---|---|---|
| Pubmed/Medline | Web of Science | |||
| Retrieved | Selected | Retrieved | Selected | |
| Fibers in denture base | 525 | 9 | 97 | 3 |
| Fillers in denture base | 22 | 9 | 29 | 3 |
| Reinforcement of denture base | 99 | 7 | 79 | |
| Ref | Sample Fabrication Technique | Sample Size | Sample Allocation or Concealment | Sample Power Calculation | Materials Testing Standards | Blinding of Operator | Objective/Finding Mentioned | Risk of Bias | |
|---|---|---|---|---|---|---|---|---|---|
| [28] | 1 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [29] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [30] | 1 | 0 | 2 | 2 | 2 | 2 | 0 | High | |
| [31] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [32] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [33] | 0 | 0 | 2 | 0 | 0 | 2 | 0 | Low | |
| [34] | 1 | 1 | 2 | 2 | 2 | 2 | 0 | High | |
| [35] | 1 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [36] | 1 | 0 | 2 | 2 | 2 | 2 | 0 | Moderate | |
| [37] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [38] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [39] | 0 | 0 | 1 | 2 | 2 | 2 | 0 | Moderate | |
| [40] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [41] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [42] | 1 | 2 | 2 | 2 | 2 | 2 | 0 | High | |
| [43] | 0 | 0 | 2 | 0 | 2 | 2 | 0 | Moderate | |
| [44] | 1 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [45] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [46] | 1 | 0 | 0 | 2 | 0 | 2 | 0 | Moderate | |
| [47] | 1 | 1 | 2 | 2 | 2 | 2 | 0 | High | |
| [48] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [49] | 1 | 0 | 2 | 2 | 2 | 2 | 0 | Moderate | |
| [50] | 1 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [51] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [52] | 0 | 0 | 2 | 2 | 2 | 2 | 0 | Moderate | |
| [53] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [54] | 0 | 0 | 2 | 2 | 2 | 2 | 0 | Moderate | |
| [55] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate | |
| [56] | 0 | 0 | 2 | 2 | 0 | 2 | 0 | Moderate |
| Ref. | Testing Method | Reinforcing Agent/s Used | Outcome |
|---|---|---|---|
| [28] | FS, FT | Treated 0.25 and 0.5 wt.% double-modified organoclay nanoparticles | ↑↑ FS and FT in both 0.25 and 0.5 wt.% nanoparticles groups |
| [29] | FS | Ag, TiO2, ZrO2, Al2O3, SiC, SiC-nano, Si3N4, and HA-nano in ratios of 10 wt.% to PMMA | ↔ between the study groups |
| [30] | SH | ZrO2 (14 nm), SiO2 (12 nm), and diamond nanoparticles (19 nm) in concentrations of 0%, 0.5%, 1.0%, 2.5%, and 5.0% by weight of acrylic powder | ↑↑ in SH compared to Control |
| [31] | FS, FM | Microcrystalline cellulose with 2 or 5% by weight | ↑↑ FS, FM in 5 wt.% group |
| [32] | FS | 1 wt.% or 5 wt.% of SiO2 or prepolymer nanoparticles | ↓↓ FS in experimental groups compared to control group |
| [33] | FS | 1, 3, or 5 wt.% of Al2O3 (18 nm), SiO2 (15 nm), or TiO2 (13 nm) nanoparticles | 1 wt.% of nanoparticles ↑↑ FS |
| [34] | FS, EM, FT | Polyvinyl alcohol aligned and non- aligned nanofiber with 0.05% w/w, 0.25% w/w, 1% w/w, or 1.25% w/w. | Aligned nanofiber ↑↑ increased the mechanical properties of denture base resin |
| [35] | FS | Treated glass fillers (1%, 2.5%, 5%, and 10% by weight) 1.5 µm sized | FS ↓ as glass filler uploading ↑ |
| [36] | FT | Silanated nano barium titanate at 5 wt.% | ↑↑ FT in the experimental group |
| [37] | FS, FM | Treated aramid fibers with four orientations (unidirectional, woven, non-woven, and paper-type) | unidirectional and woven aramid fibers ↑↑ FS & FM |
| [38] | FS, FM, FT | GL, aramid, and UHMWPE fibers at volume concentrations of 2.6%, 5.3%, and 7.9%, respectively | Combination of GL/UHMWPE fibers showed ↑↑ FT and FS |
| [39] | FS | GF, aramid, nylon at 4 wt.% (5 mm in length) | ↑↑ FS in GF and aramid reinforced groups |
| [40] | FR | GF (chopped strand mat, continuous or woven) at 2.5, 3, 4, 5 vol.% | ↑ fracture resistance in all forms of GF |
| [41] | FS, FT, FM | E-Glass FiBER FORCE | ↑ mechanical properties were observed |
| [42] | FS | Treated and untreated ZrO2 nanotubes (8 µm in length) | 2.0 wt.% ZrO2 nanotubes ↑ FS |
| [43] | FS, SH | Silane treated fine or coarse mica particles (30 µm and 131 µm) at 10 vol.% or 20 vol.% | ↓ FS, however, ↑ SH with 20 vol.% mica reinforcement |
| [44] | FS, FM | Silanized nano SiO2 (36 nm in size) at 0.25, 0.5, 1, 5, 10, and 15 wt.% | 1 wt.% presented ↑ FS while 10 % 15 wt.% showed ↑ FM |
| [45] | FS, IS | Nanodiamond (30–40 nm in size) at 0.5, 1, and 1.5 wt.% | 0.5 wt.% reinforced PMMA displayed ↑↑ FS. Control group showed ↑↑ IS |
| [46] | FS, SH | 1, 2, 3, 4, 5, 10, 15, or 20 wt.% aluminum borate whiskers (5–30 µm in length) | Silanized ABWs ↑ FS, SH. Optimal loading was 5 wt. % while 15 wt.% for SH |
| [47] | SH, FT | 0.023%, 0.046%, 0.091%, 0.23%, 0.46%, and 0.91% by vol. of SiO2 nanoparticles | 0.023% resulted in ↑ SH and FT |
| [48] | IS, FT | 1% TiO2 and 1% ZrO2, 2% Al2O3, 2% TiO2, and 2% ZrO2 by volume | IS and FT values ↑↑ |
| [49] | FS | Silanized Al2O3 (0.1, 0.2, or 0.4 wt.%) 18–23 µm in size | 0.1 wt.% Al2O3 showed ↑↑ FS |
| [50] | TS, FS, CS | 10%, 20%, and 30% by volume Ag and Al | CS ↑↑ while TS and FS ↓ at 30 vol.% |
| [51] | FS | Treated S-glass fiber, nylon fiber | ↑↑ in S-glass reinforced PMMA |
| [52] | FS | Hydrogen plasma-treated polypropylene fibers (2.5. 5 & 10 wt.%) | ↑↑ FS in tested groups |
| [53] | FS, IS, SH | Borax, boric acid, colemanite | The addition of 1% Colemanite to PMMA ↑ mechanical properties |
| [54] | FS, EM, SH | Halloysite nanotubes at 0.3, 0.6, and 0.9 wt.% | 0.3 wt% halloysite nanotubes ↑ mechanical properties |
| [55] | FS, SH | Silanized nano ZrO₂ and nano aluminum borate whiskers at 1, 2, 3, and 4 wt.% | The mechanical behaviours of silanized ZrO₂-ABW/PMMA composites ↑↑ improved |
| [56] | FS, SH | Treated 2.5 wt%, and 5 wt% of TiO2 nanotubes | ↑↑ FS and SH in experimental groups |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldegheishem, A.; AlDeeb, M.; Al-Ahdal, K.; Helmi, M.; Alsagob, E.I. Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review. Polymers 2021, 13, 3083. https://doi.org/10.3390/polym13183083
Aldegheishem A, AlDeeb M, Al-Ahdal K, Helmi M, Alsagob EI. Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review. Polymers. 2021; 13(18):3083. https://doi.org/10.3390/polym13183083
Chicago/Turabian StyleAldegheishem, Alhanoof, Modhi AlDeeb, Khold Al-Ahdal, Mohammad Helmi, and Eman I. Alsagob. 2021. "Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review" Polymers 13, no. 18: 3083. https://doi.org/10.3390/polym13183083
APA StyleAldegheishem, A., AlDeeb, M., Al-Ahdal, K., Helmi, M., & Alsagob, E. I. (2021). Influence of Reinforcing Agents on the Mechanical Properties of Denture Base Resin: A Systematic Review. Polymers, 13(18), 3083. https://doi.org/10.3390/polym13183083






