Microstructural and Tribological Properties of a Dopamine Hydrochloride and Graphene Oxide Coating Applied to Multifilament Surgical Sutures
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
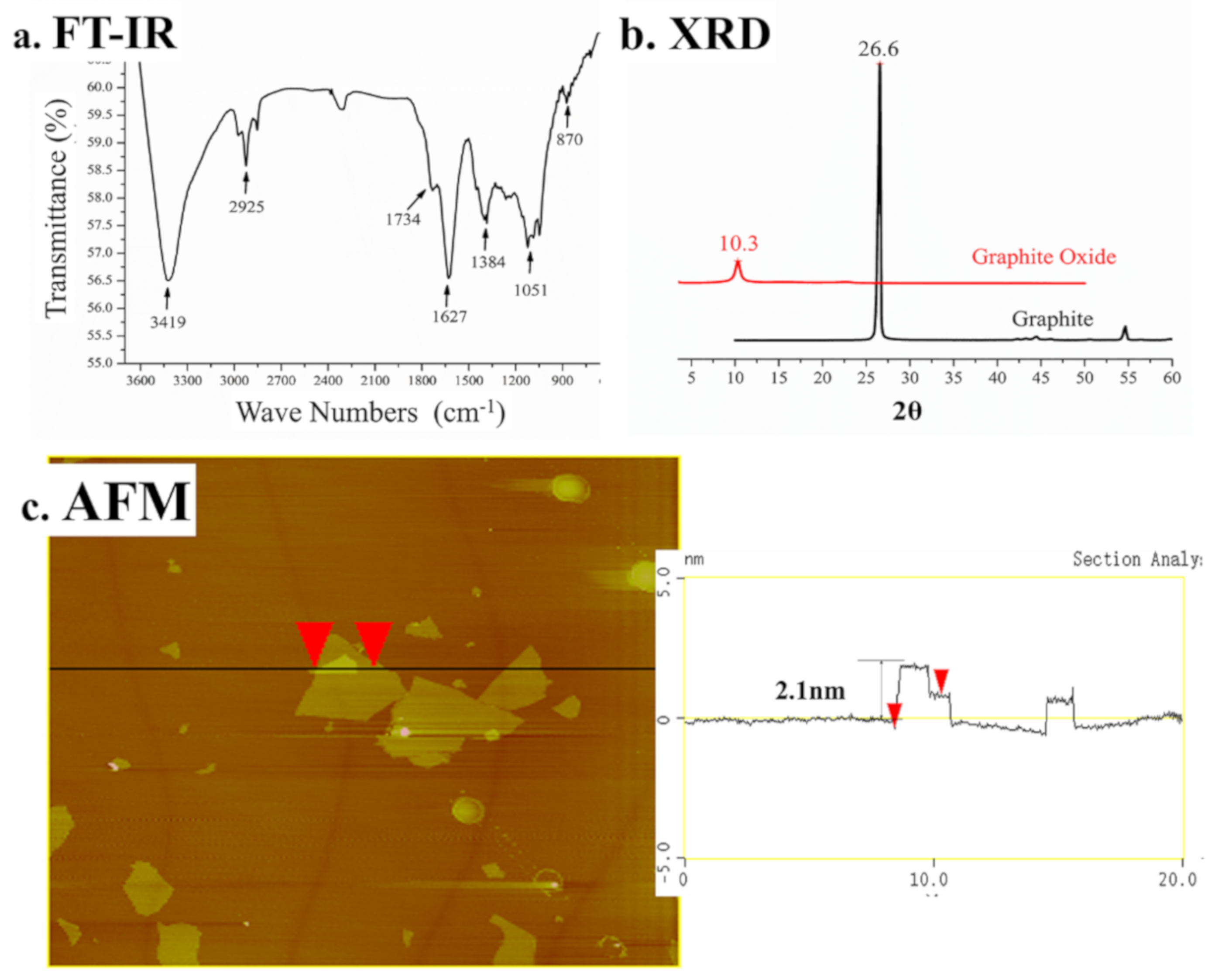
2.2. Synthesis and Characterization of Graphene Oxide
2.3. Coating of the Multifilament Surgical Sutures
2.3.1. The Coating Treatment
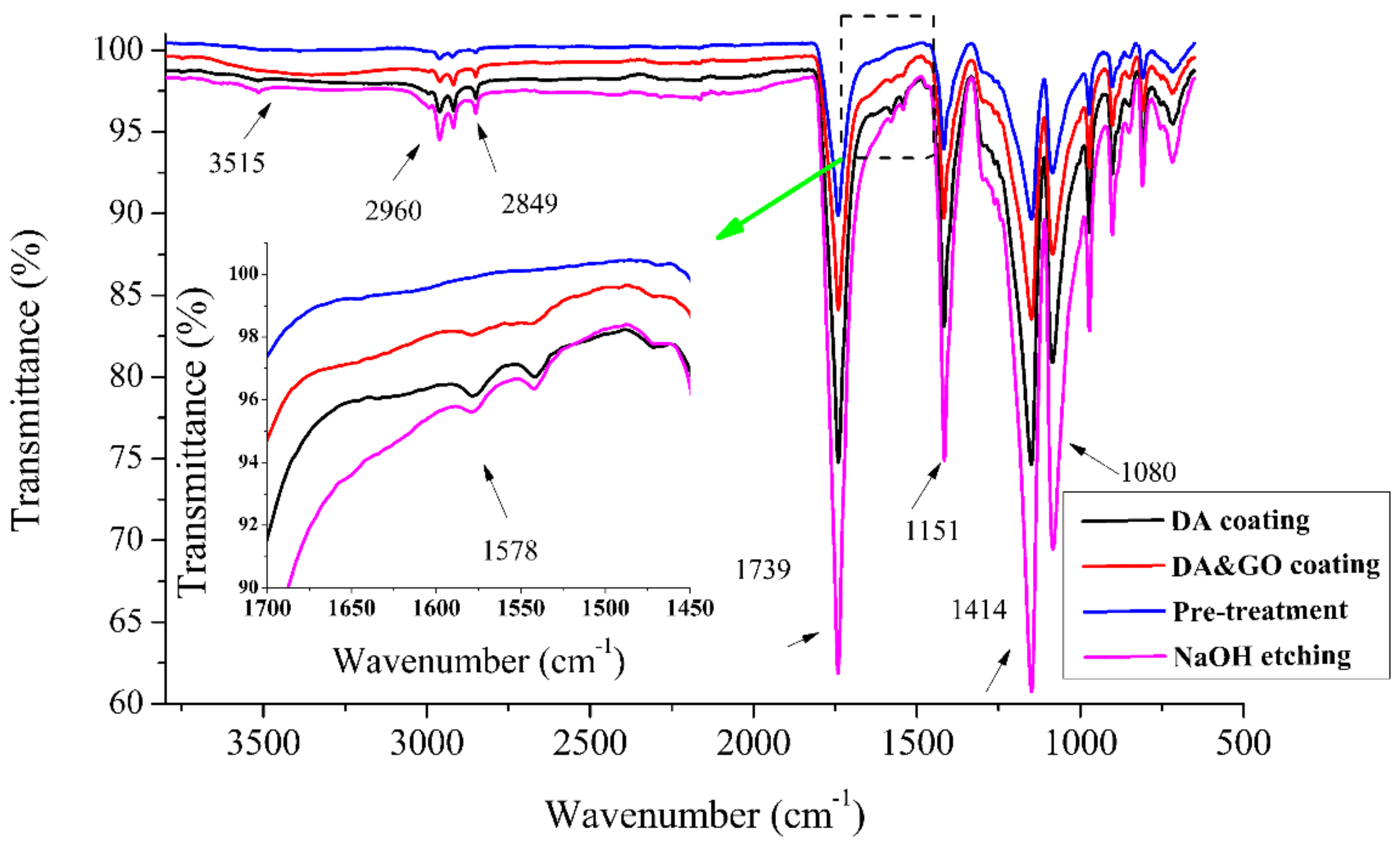
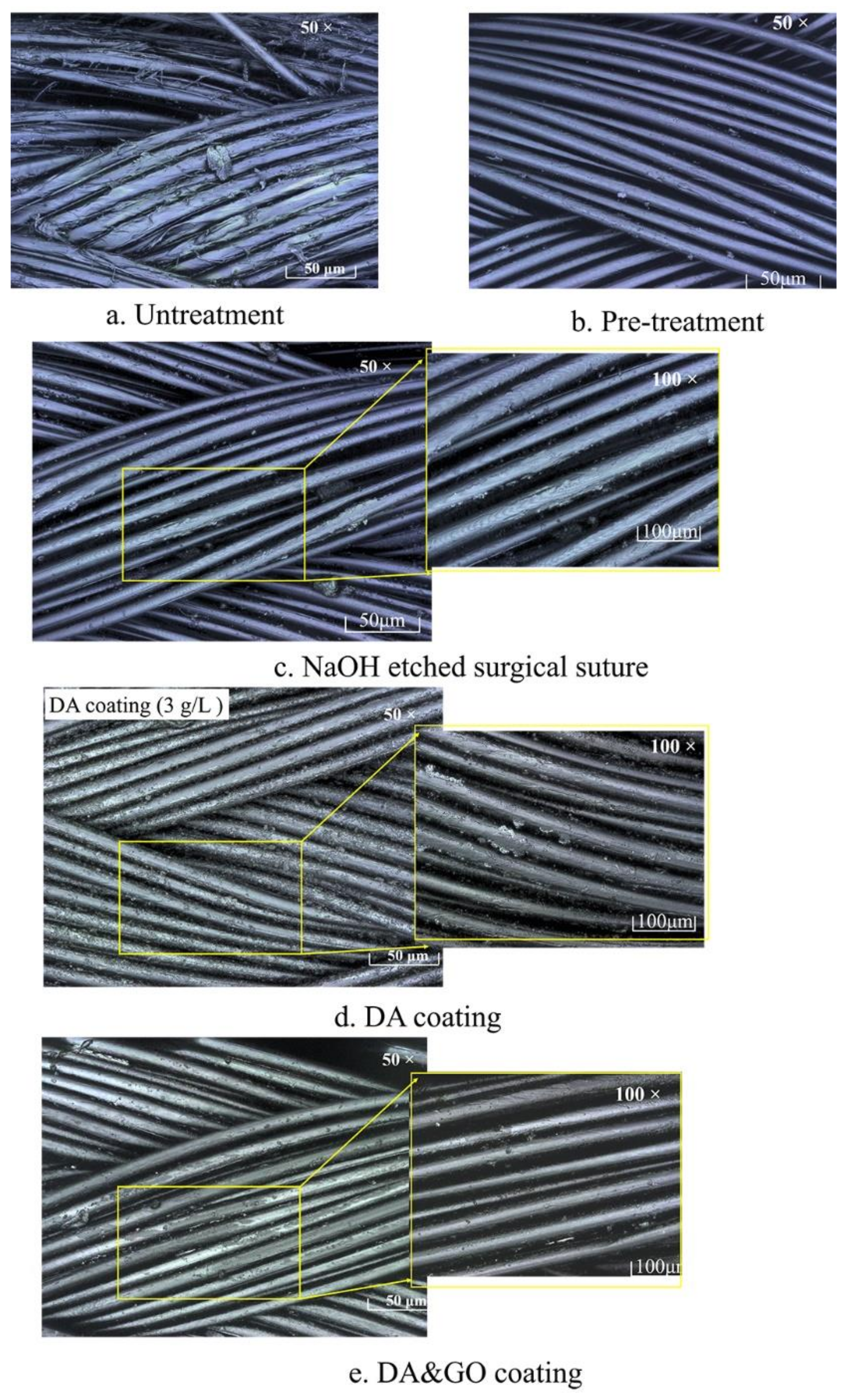
2.3.2. Surface Analysis
2.3.3. Mechanical Properties
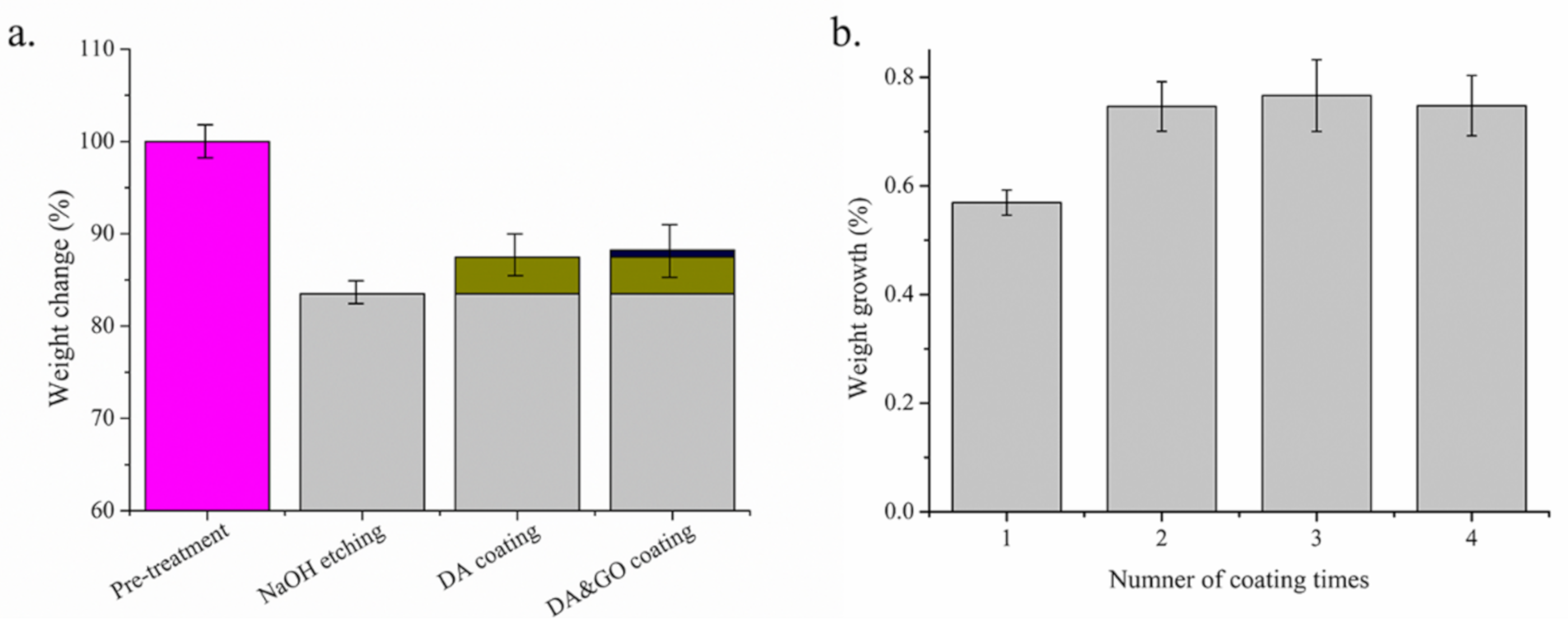
Weight Change
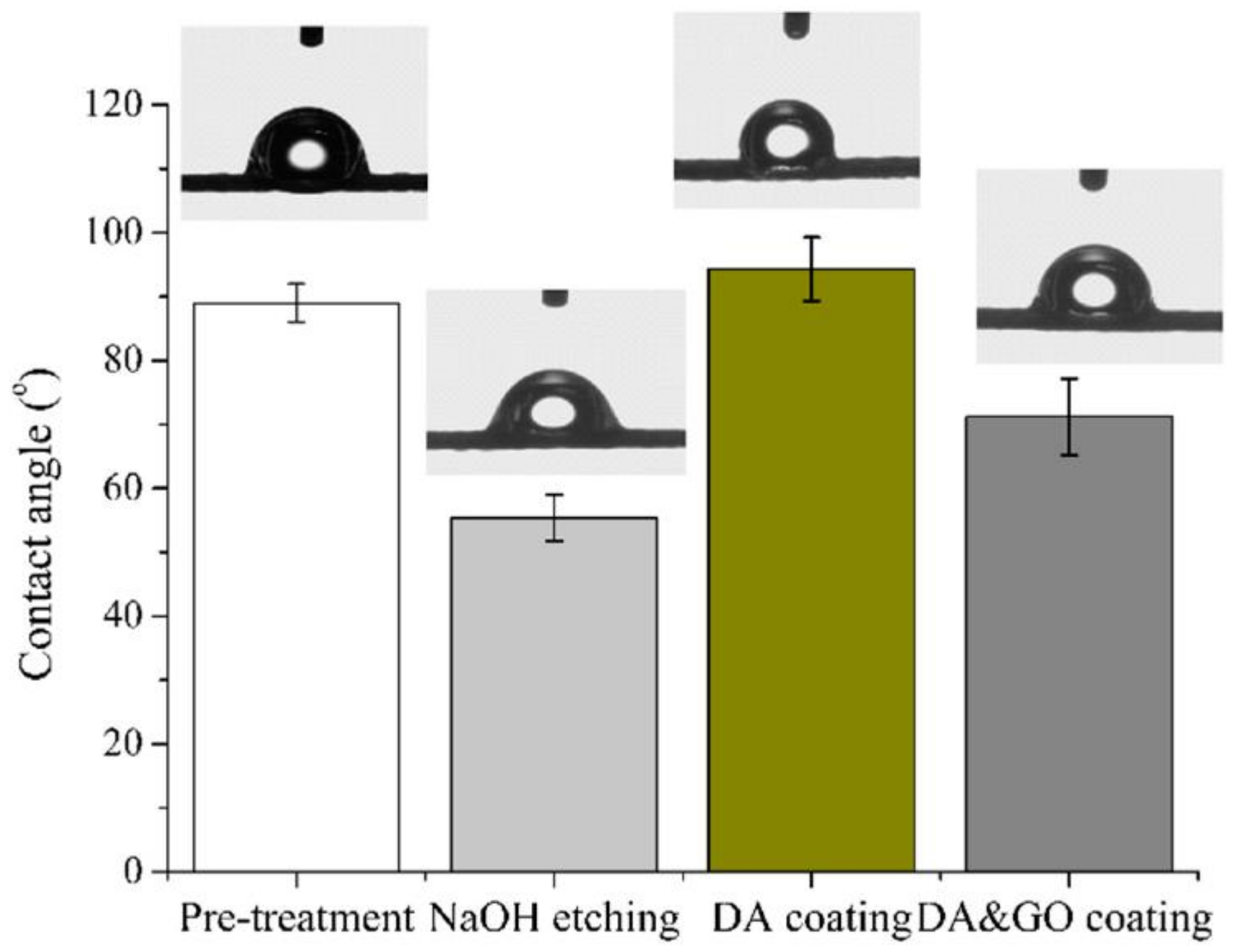
Contact Angle
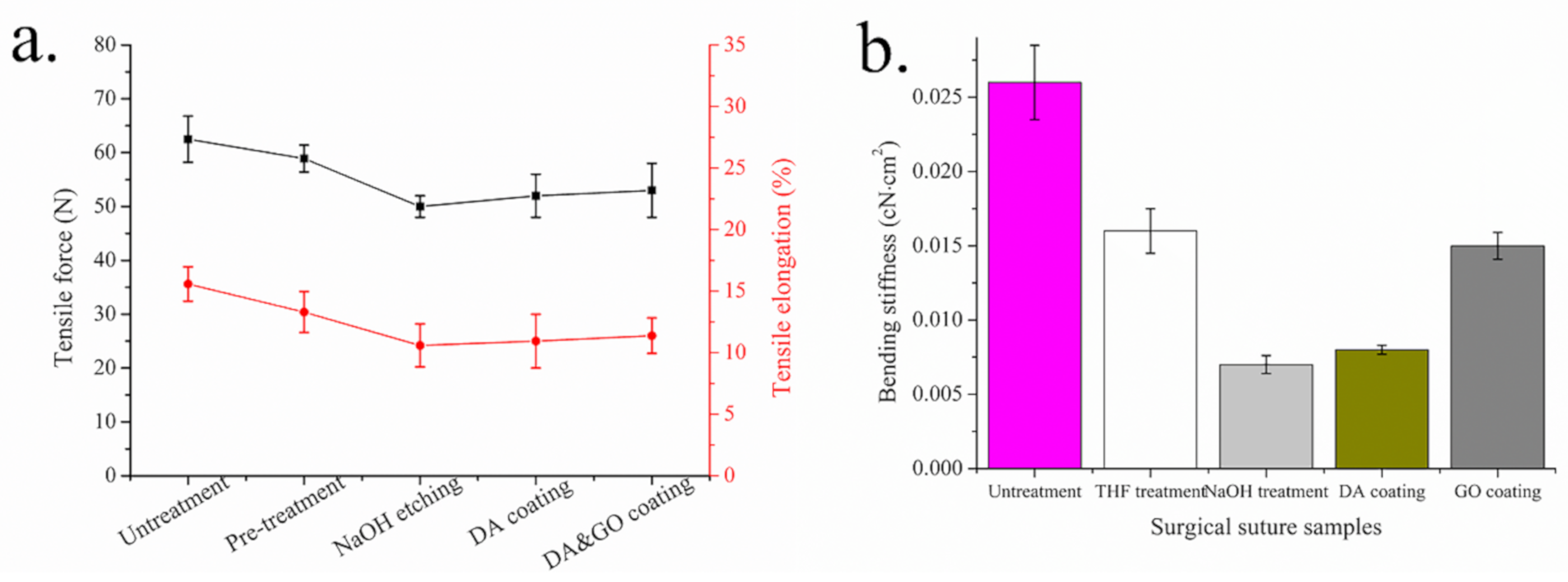
Tensile Strength Test
Bending Stiffness
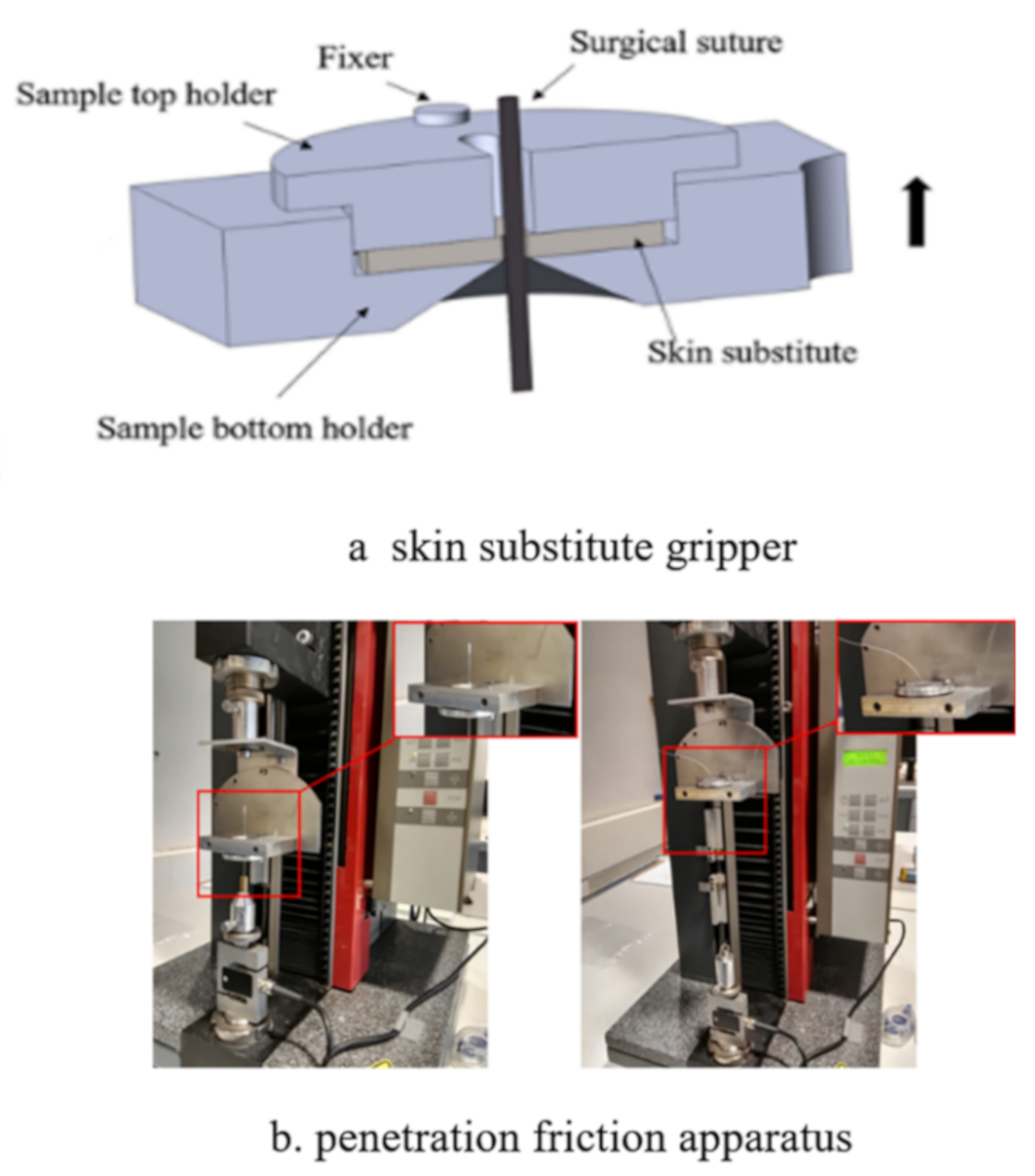
2.4. Tribological Measurement
3. Results and Discussion
3.1. Characterization of Graphene Oxide
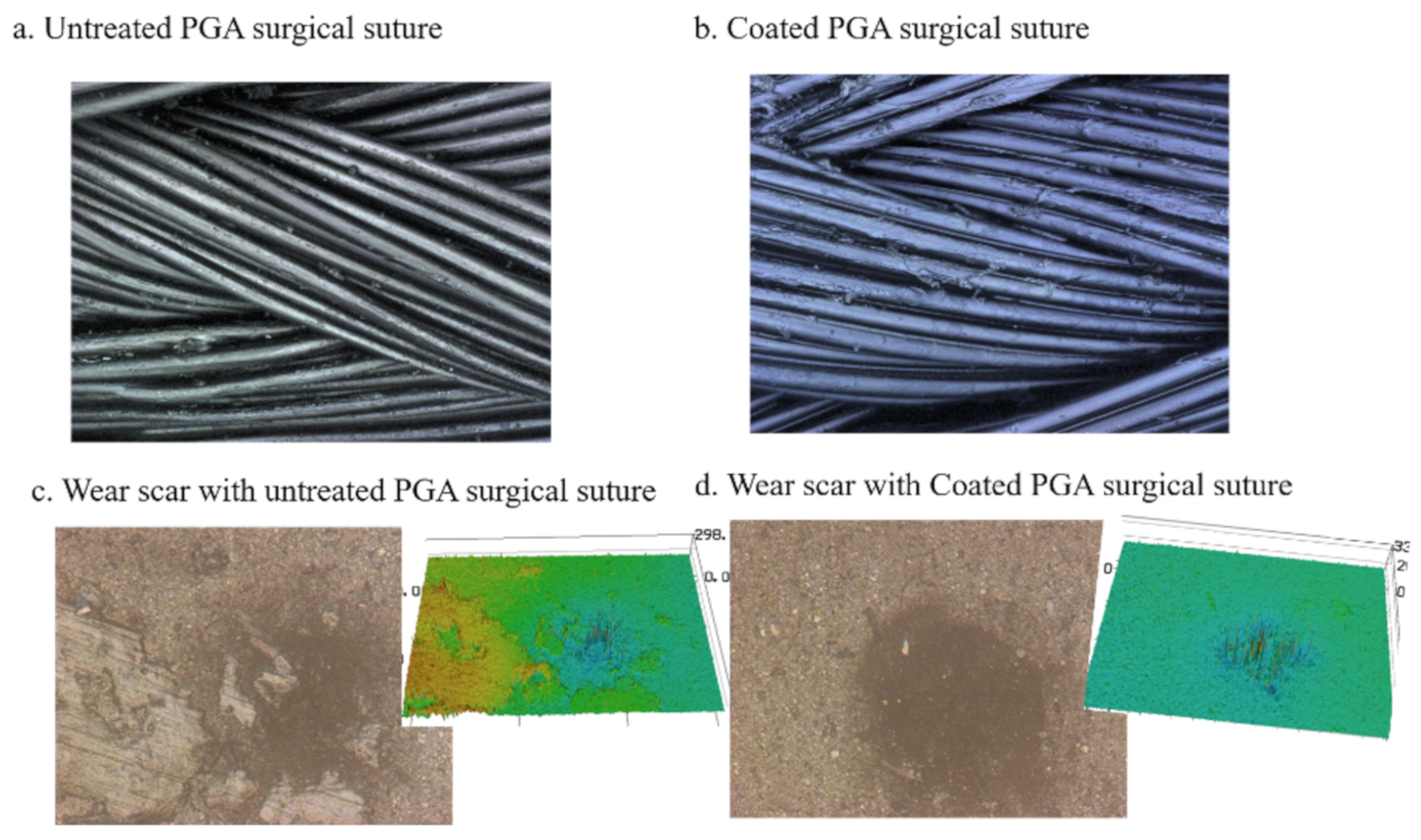
3.2. Surface Chemical Composite and Morphology
3.3. Mechanical Properties
3.4. Wettability Properties
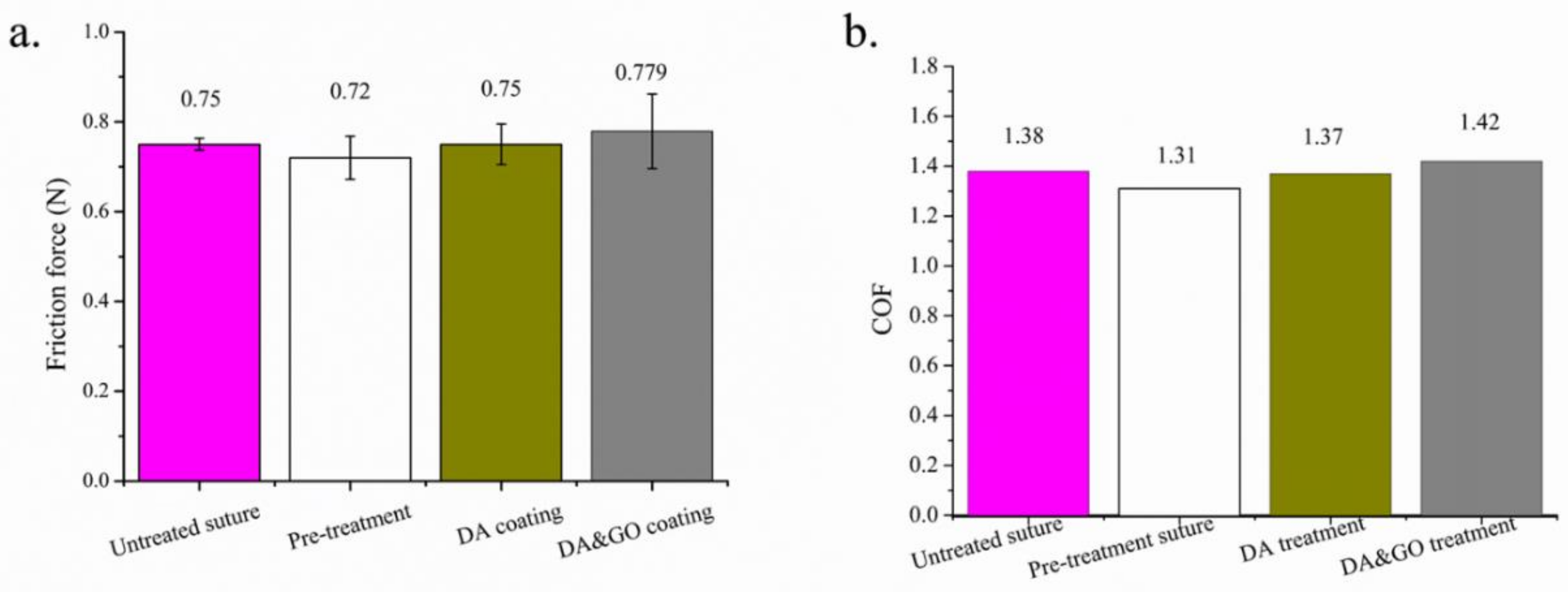
3.5. Tribological Properties
3.5.1. Frictional Properties
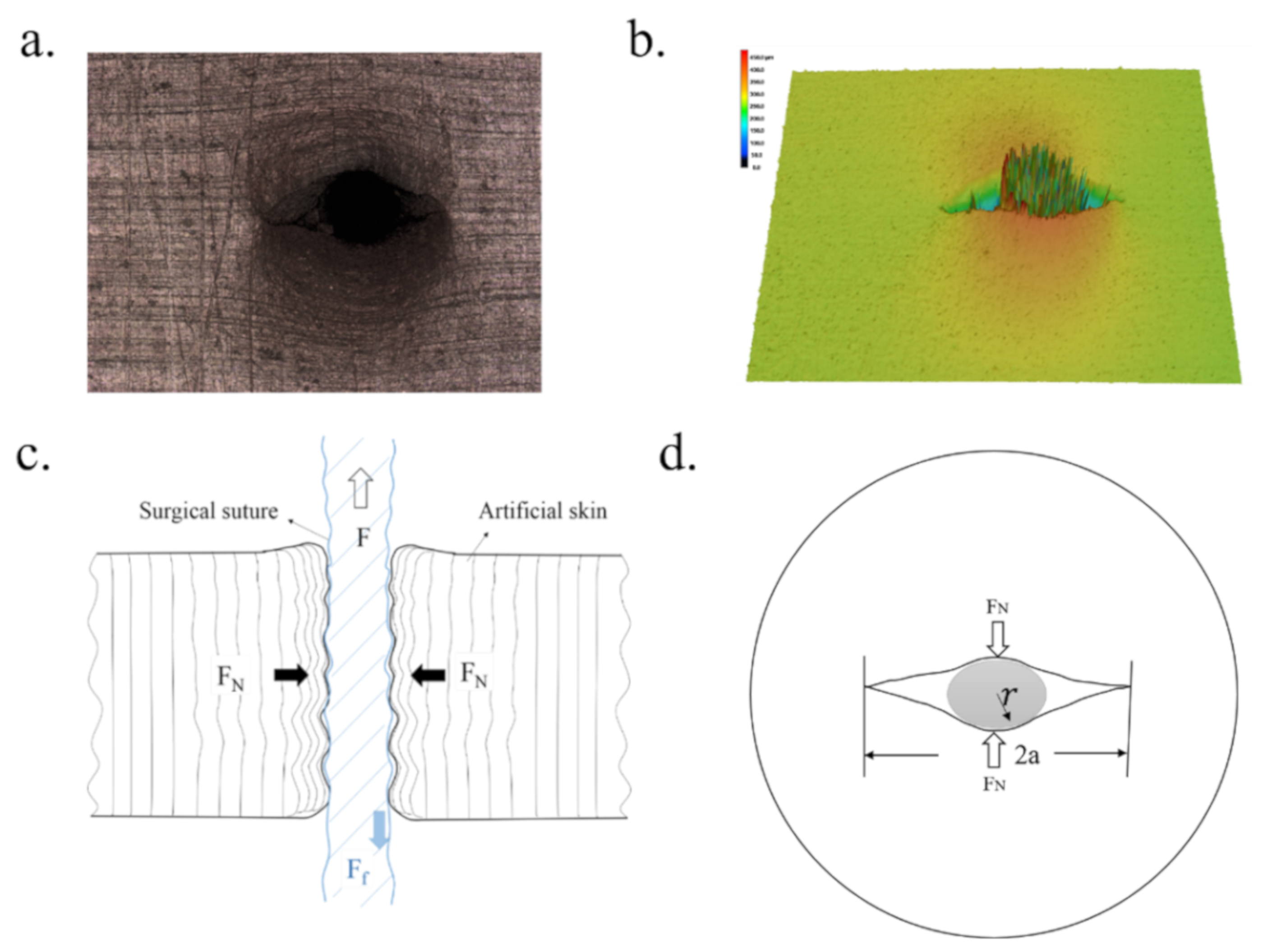
3.5.2. Wear Properties
3.5.3. Mechanism
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Misra, S.; Ramesh, K.; Okamura, A. Modeling of tool-tissue interactions for computer-based surgical simulation: A literature review. Presence 2008, 17, 463–491. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, J.L. Wound closure biomaterials and devices. Shock 1999, 11, 226. [Google Scholar] [CrossRef]
- Moy, R.L.; Waldman, B.; Hein, D.W. A review of sutures and suturing techniques. J. Dermatol. Surg. Oncol. 1992, 18, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Rao, Y.; Farris, R.J. A modeling and experimental study of the influence of twist on the mechanical properties of high-performance fiber yarns. J. Appl. Polym. Sci. 2000, 77, 1938–1949. [Google Scholar] [CrossRef]
- Apt, L.; Henrick, A. “Tissue-drag” with polyglycolic acid (dexon) and polyglactin 910 (vicryl) sutures in strabismus surgery. J. Pediatr. Ophthalmol. 1976, 13, 360–364. [Google Scholar] [CrossRef]
- Ajmeri, J.R.; Ajmeri, C.J. Surgical sutures: The largest textile implant material. In Medical Textiles and Biomaterials for Healthcare; Woodhead Publishing: Gujarat, India, 2006; pp. 432–440. [Google Scholar]
- Zhang, G.; Zheng, G.; Ren, T.; Zeng, X.; Der Heide, E.V. Dopamine hydrochloride and carboxymethyl chitosan coatings for multifilament surgical suture and their influence on friction during sliding contact with skin substitute. Friction 2020, 8, 58–69. [Google Scholar] [CrossRef]
- Li, M.; Liu, Q.; Jia, Z.; Xu, X.; Cheng, Y.; Zheng, Y.; Xi, T.; Wei, S. Graphene oxide/hydroxyapatite composite coatings fabricated by electrophoretic nanotechnology for biological applications. Carbon 2014, 67, 185–197. [Google Scholar] [CrossRef]
- Tong, L.; Zhang, J.; Xu, C.; Wang, X.; Song, S.; Jiang, Z.H.; Kamado, S.; Cheng, L.; Zhang, H. Enhanced corrosion and wear resistances by graphene oxide coating on the surface of mg-zn-ca alloy. Carbon 2016, 109, 340–351. [Google Scholar] [CrossRef]
- Li, P.; Zhou, H.; Cheng, X. Nano/micro tribological behaviors of a self-assembled graphene oxide nanolayer on ti/titanium alloy substrates. Appl. Surf. Sci. 2013, 285, 937–944. [Google Scholar] [CrossRef]
- Cai, G.; Xu, Z.; Yang, M.; Tang, B.; Wang, X. Functionalization of cotton fabrics through thermal reduction of graphene oxide. Appl. Surf. Sci. 2017, 393, 441–448. [Google Scholar] [CrossRef]
- Chen, L.; Wei, F.; Liu, L.; Cheng, W.; Hu, Z.; Wu, G.; Du, Y.; Zhang, C.; Huang, Y. Grafting of silane and graphene oxide onto pbo fibers: Multifunctional interphase for fiber/polymer matrix composites with simultaneously improved interfacial and atomic oxygen resistant properties. Compos. Sci. Technol. 2015, 106, 32–38. [Google Scholar] [CrossRef]
- Hu, X.; Tian, M.; Qu, L.; Zhu, S.; Han, G. Multifunctional cotton fabrics with graphene/polyurethane coatings with far-infrared emission, electrical conductivity, and ultraviolet-blocking properties. Carbon 2015, 95, 625–633. [Google Scholar] [CrossRef]
- Yan, J.; Yang, L.; Lin, M.F.; Ma, J.; Lu, X.; Lee, P.S. Polydopamine spheres as active templates for convenient synthesis of various nanostructures. Small 2013, 9, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Ku, S.H.; Ryu, J.; Hong, S.K.; Lee, H.; Park, C.B. General functionalization route for cell adhesion on non-wetting surfaces. Biomaterials 2010, 31, 2535–2541. [Google Scholar] [CrossRef]
- Barras, A.; Lyskawa, J.; Szunerits, S.; Woisel, P.; Boukherroub, R. Direct functionalization of nanodiamond particles using dopamine derivatives. Langmuir 2011, 27, 12451–12457. [Google Scholar] [CrossRef]
- Lee, H.; Dellatore, S.M.; Miller, W.M.; Messersmith, P.B. Mussel-inspired surface chemistry for multifunctional coatings. Science 2007, 318, 426–430. [Google Scholar] [CrossRef]
- Zhang, G.; Ren, T.; Zhang, S.; Zeng, X.; van der Heide, E. Study on the tribological behavior of surgical suture interacting with a skin substitute by using a penetration friction apparatus. Colloids Surf. B Biointerfaces 2018, 162, 228–235. [Google Scholar] [CrossRef]
- Zhang, G.; Zeng, X.; Su, Y.; Borras, F.X.; de Rooij, M.B.; Ren, T.; van der Heide, E. Influence of suture size on the frictional performance of surgical suture evaluated by a penetration friction measurement approach. J. Mech. Behav. Biomed. Mater. 2018, 80, 171–179. [Google Scholar] [CrossRef]
- Zhang, G.; Ren, T.; Lette, W.; Zeng, X.; van der Heide, E. Development of a penetration friction apparatus (pfa) to measure the frictional performance of surgical suture. J. Mech. Behav. Biomed. Mater. 2017, 74, 392–399. [Google Scholar] [CrossRef]
- Shergold, O.A.; Fleck, N.A. Experimental investigation into the deep penetration of soft solids by sharp and blunt punches, with application to the piercing of skin. J. Biomech. Eng. 2005, 127, 838–848. [Google Scholar] [CrossRef]
- Azar, T.; Hayward, V. Estimation of the Fracture Toughness of Soft Tissue from Needle Insertion. In International Symposium on Biomedical Simulation; Springer: Berlin/Heidelberg, Germany, 2008; pp. 166–175. [Google Scholar]
- Shergold, O.A.; Fleck, N.A.; Radford, D. The uniaxial stress versus strain response of pig skin and silicone rubber at low and high strain rates. Int. J. Impact Eng. 2006, 32, 1384–1402. [Google Scholar] [CrossRef]
- Marcano, D.C.; Kosynkin, D.V.; Berlin, J.M.; Sinitskii, A.; Sun, Z.; Slesarev, A.; Alemany, L.B.; Lu, W.; Tour, J.M. Improved synthesis of graphene oxide. ACS Nano 2010, 4, 4806–4814. [Google Scholar] [CrossRef] [PubMed]
- Peng, F.; Olson, J.R.; Shaw, M.T.; Wei, M. Influence of pretreatment on the surface characteristics of plla fibers and subsequent hydroxyapatite coating. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 220–229. [Google Scholar] [CrossRef]
- De Simone, S.; Gallo, A.; Paladini, F.; Sannino, A.; Pollini, M. Development of silver nano-coatings on silk sutures as a novel approach against surgical infections. J. Mater. Sci. Mater. Med. 2014, 25, 2205–2214. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Hou, D.; Tang, X.; Wang, L. Quantitative physical and handling characteristics of novel antibacterial braided silk suture materials. J. Mech. Behav. Biomed. Mater. 2015, 50, 160–170. [Google Scholar] [CrossRef]
- Rodeheaver, G.T. Knotting and handling characteristics of coated synthetic absorbable sutures. J. Surg. Res. 1983, 35, 525–530. [Google Scholar] [CrossRef]
- Singh, V.K.; Elomaa, O.; Johansson, L.-S.; Hannula, S.-P.; Koskinen, J. Lubricating properties of silica/graphene oxide composite powders. Carbon 2014, 79, 227–235. [Google Scholar] [CrossRef]
- Some, S.; Kim, Y.; Yoon, Y.; Yoo, H.; Lee, S.; Park, Y.; Lee, H. High-quality reduced graphene oxide by a dual-function chemical reduction and healing process. Sci. Rep. 2013, 3, 1929. [Google Scholar] [CrossRef] [PubMed]
- Stankovich, S.; Dikin, D.A.; Dommett, G.H.; Kohlhaas, K.M.; Zimney, E.J.; Stach, E.A.; Piner, R.D.; Nguyen, S.T.; Ruoff, R.S. Graphene-based composite materials. Nature 2006, 442, 282–286. [Google Scholar] [CrossRef]
- Brugnerotto, J.; Lizardi, J.; Goycoolea, F.M.; Argüelles-Monal, W.; Desbrières, J.; Rinaudo, M. An infrared investigation in relation with chitin and chitosan characterization. Polymer 2001, 42, 3569–3580. [Google Scholar] [CrossRef]
- Chen, X.-G.; Park, H.-J. Chemical characteristics of o-carboxymethyl chitosans related to the preparation conditions. Carbohydr. Polym. 2003, 53, 355–359. [Google Scholar] [CrossRef]
- Zheng, M.; Han, B.; Yang, Y.; Liu, W. Synthesis, characterization and biological safety of o-carboxymethyl chitosan used to treat sarcoma 180 tumor. Carbohydr. Polym. 2011, 86, 231–238. [Google Scholar] [CrossRef]
- Zhang, G.; Ren, T.; Zeng, X.; Van Der Heide, E. Influence of surgical suture properties on the tribological interactions with artificial skin by a capstan experiment approach. Friction 2017, 5, 87–98. [Google Scholar] [CrossRef]
- Roselman, I.; Tabor, D. The friction of carbon fibres. J. Phys. D Appl. Phys. 1976, 9, 2517. [Google Scholar] [CrossRef]
- Roselman, I.C.; Tabor, D. The friction and wear of individual carbon fibres. J. Phys. D Appl. Phys. 1977, 10, 1181. [Google Scholar] [CrossRef]

| Test-Related Factors | Instructions |
|---|---|
| Equipment | Penetration friction apparatus |
| The diameter of the space of gripper | 25 ± 0.5 mm |
| Puncture angle | 90° |
| Puncture velocity of the needle | 60 mm/min |
| Puncture distance of the needle | 10 mm |
| Penetration velocity of the suture | 100 mm/min |
| Penetration distance of the suture | 100 mm |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, G.; Hu, J.; Ren, T.; Zhu, P. Microstructural and Tribological Properties of a Dopamine Hydrochloride and Graphene Oxide Coating Applied to Multifilament Surgical Sutures. Polymers 2020, 12, 1630. https://doi.org/10.3390/polym12081630
Zhang G, Hu J, Ren T, Zhu P. Microstructural and Tribological Properties of a Dopamine Hydrochloride and Graphene Oxide Coating Applied to Multifilament Surgical Sutures. Polymers. 2020; 12(8):1630. https://doi.org/10.3390/polym12081630
Chicago/Turabian StyleZhang, Gangqiang, Jiewen Hu, Tianhui Ren, and Ping Zhu. 2020. "Microstructural and Tribological Properties of a Dopamine Hydrochloride and Graphene Oxide Coating Applied to Multifilament Surgical Sutures" Polymers 12, no. 8: 1630. https://doi.org/10.3390/polym12081630
APA StyleZhang, G., Hu, J., Ren, T., & Zhu, P. (2020). Microstructural and Tribological Properties of a Dopamine Hydrochloride and Graphene Oxide Coating Applied to Multifilament Surgical Sutures. Polymers, 12(8), 1630. https://doi.org/10.3390/polym12081630





