Phosphonic Acid Coupling Agent Modification of HAP Nanoparticles: Interfacial Effects in PLLA/HAP Bone Scaffold
Abstract
1. Introduction
2. Materials and Methods
2.1. Material and Scaffold Preparation
2.2. Properties Characterization
2.3. Bioactivity and Biocompatibility Study
2.4. Statistical Analysis
3. Results and Discussion
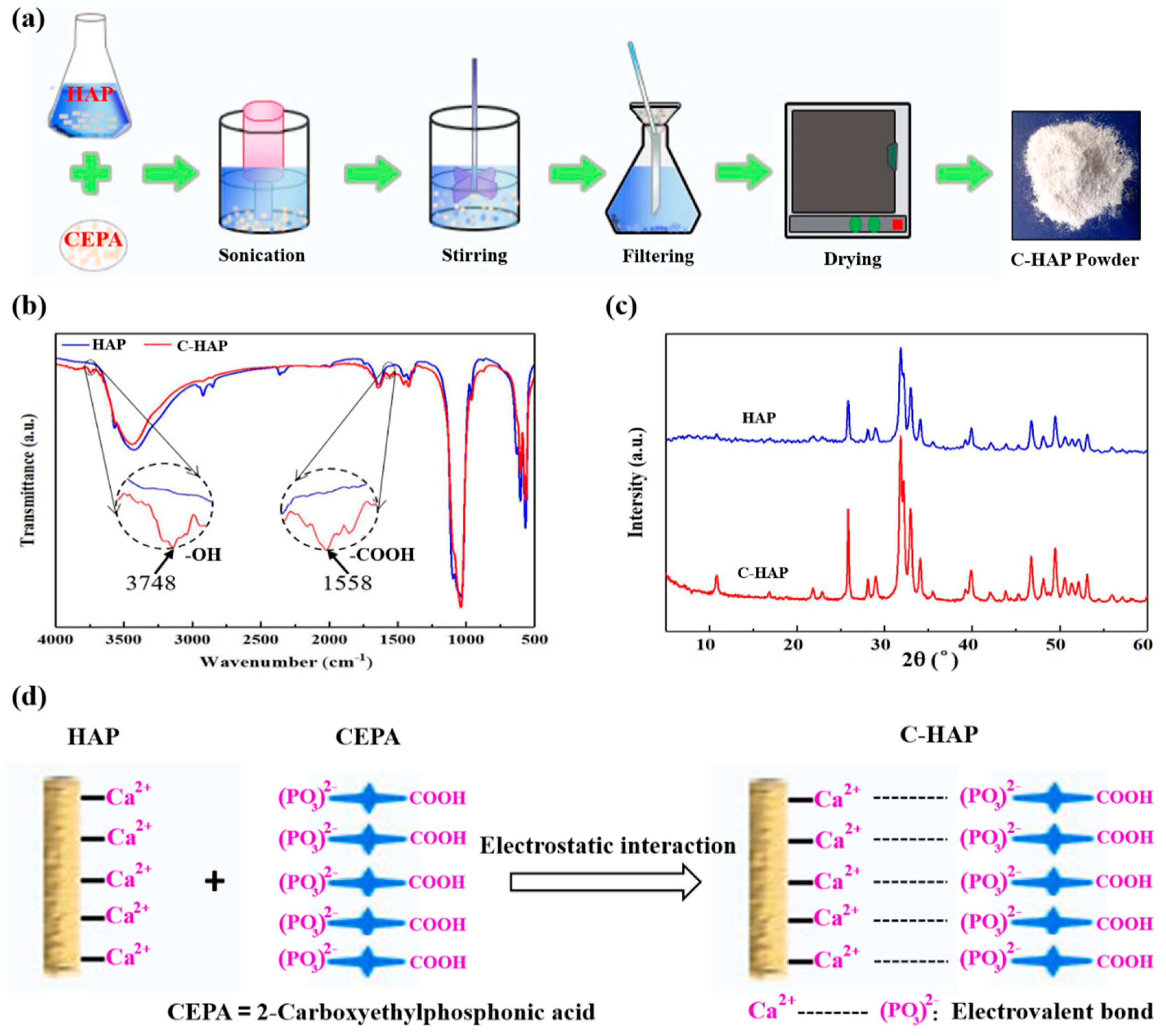
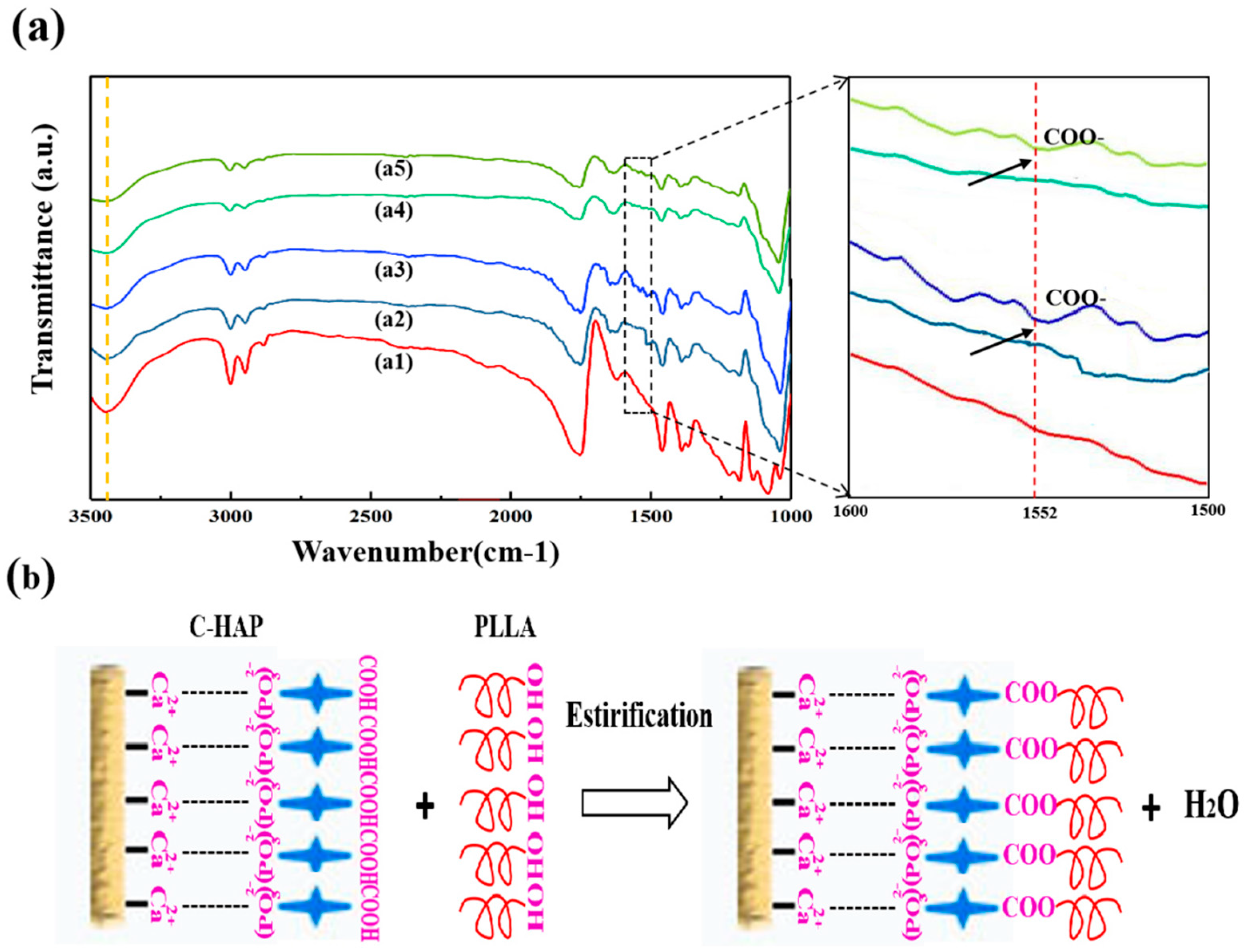
3.1. Surface Modification of HAP with CEPA
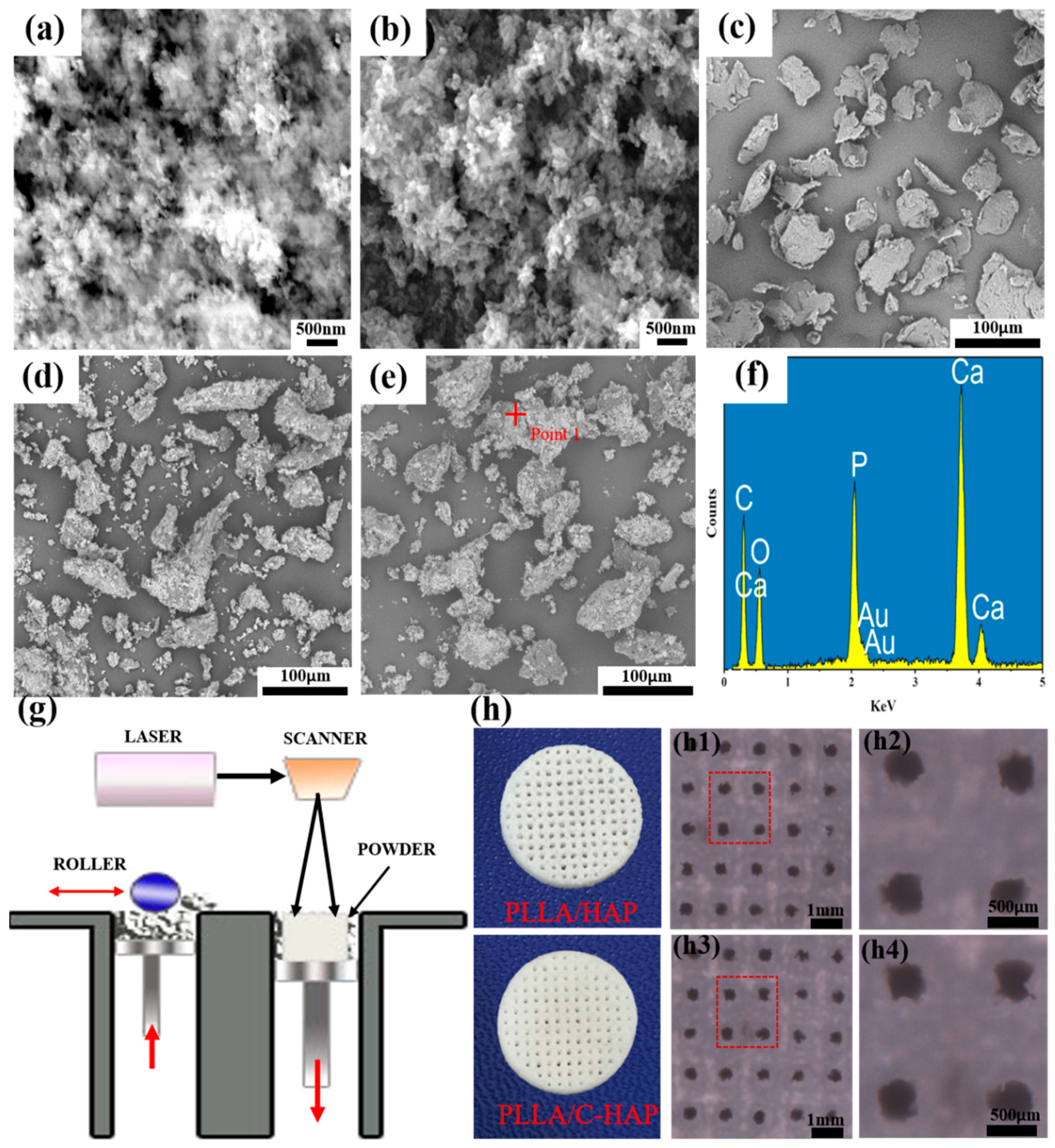
3.2. Fabrication of PLLA/HAP and PLLA/C-HAP Composite Scaffold
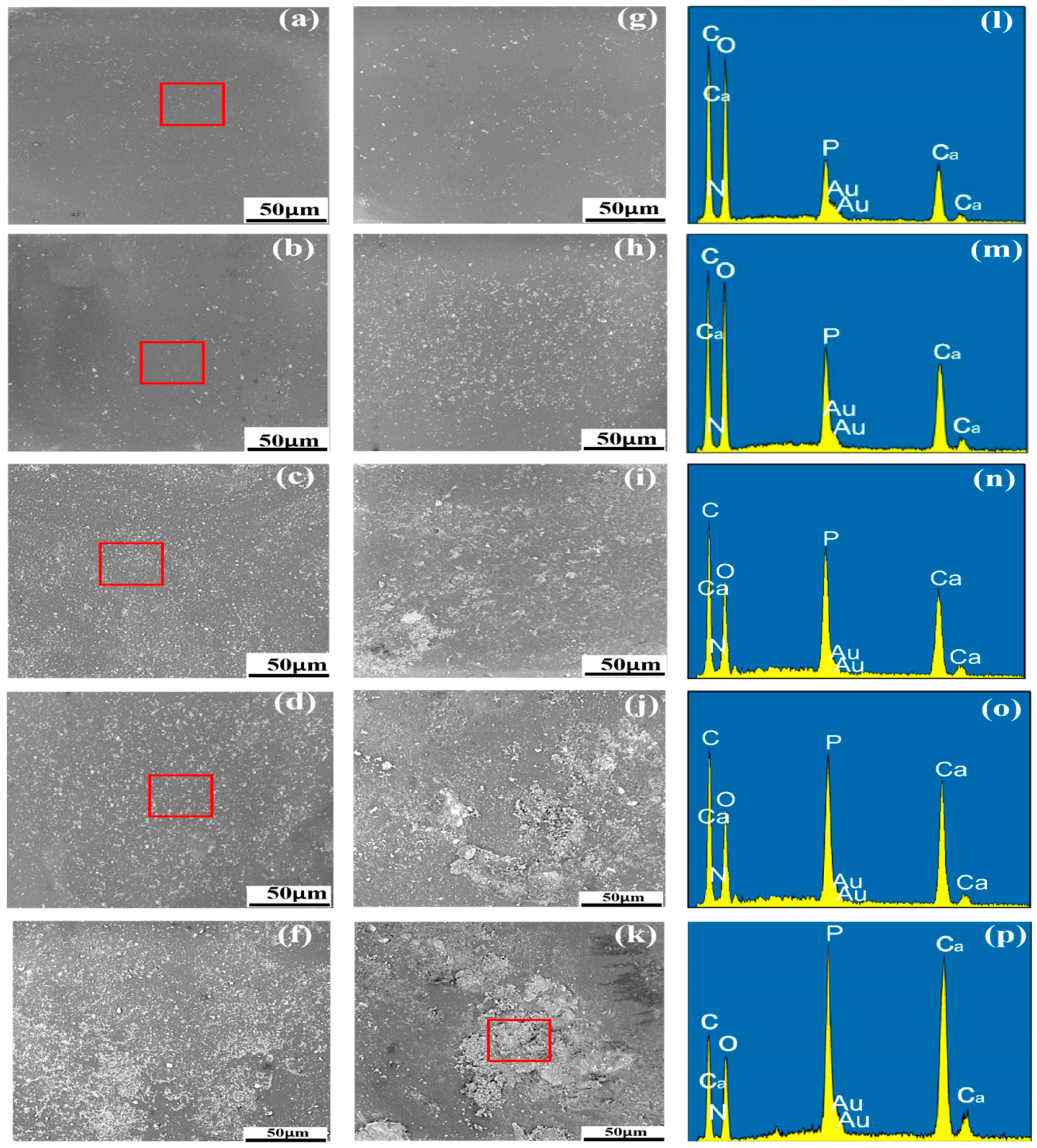
3.3. Distribution of HAP and C-HAP in the PLLA Matrix
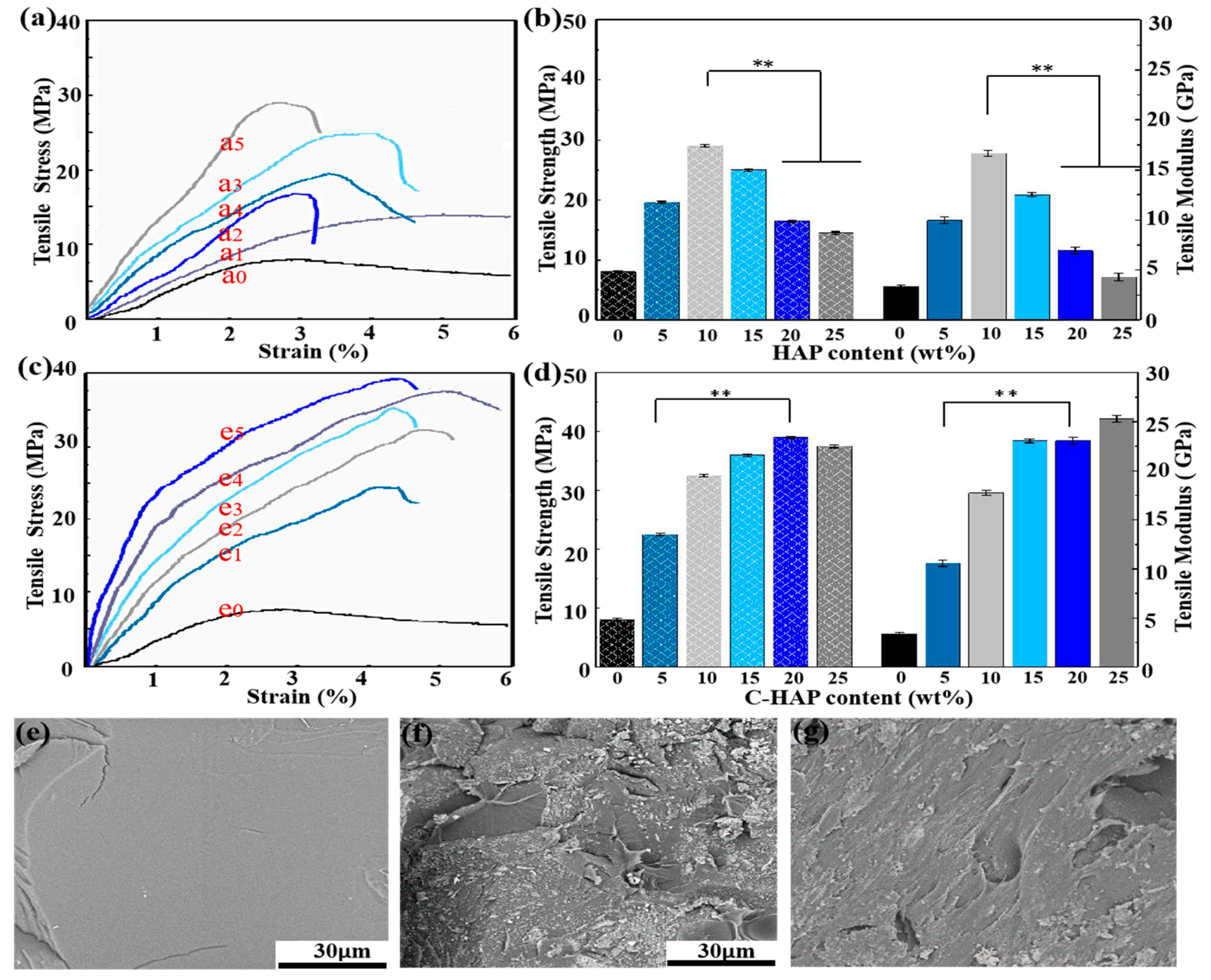
3.4. Mechanical Properties
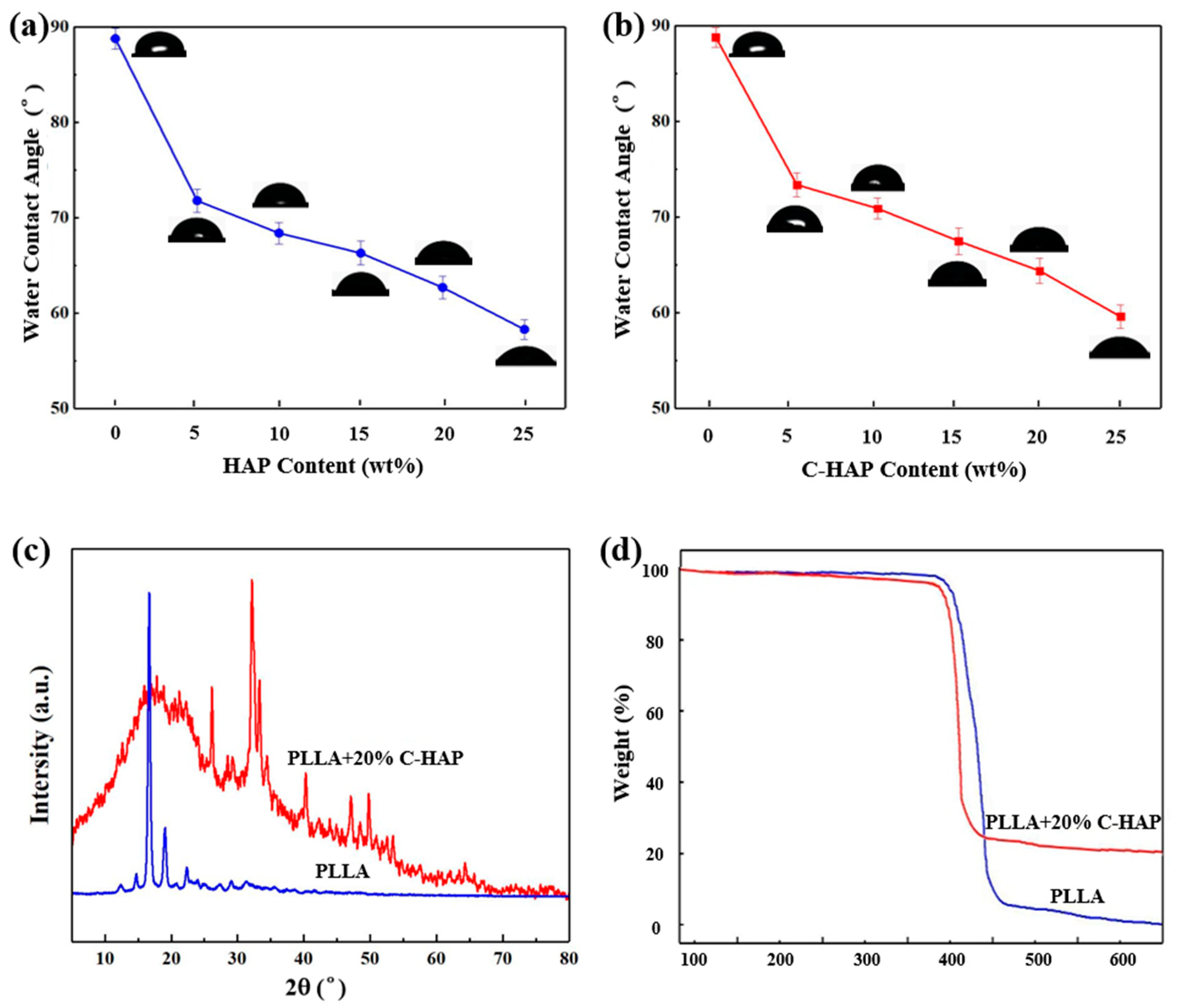
3.5. WCA, XRD and TGA Analyses
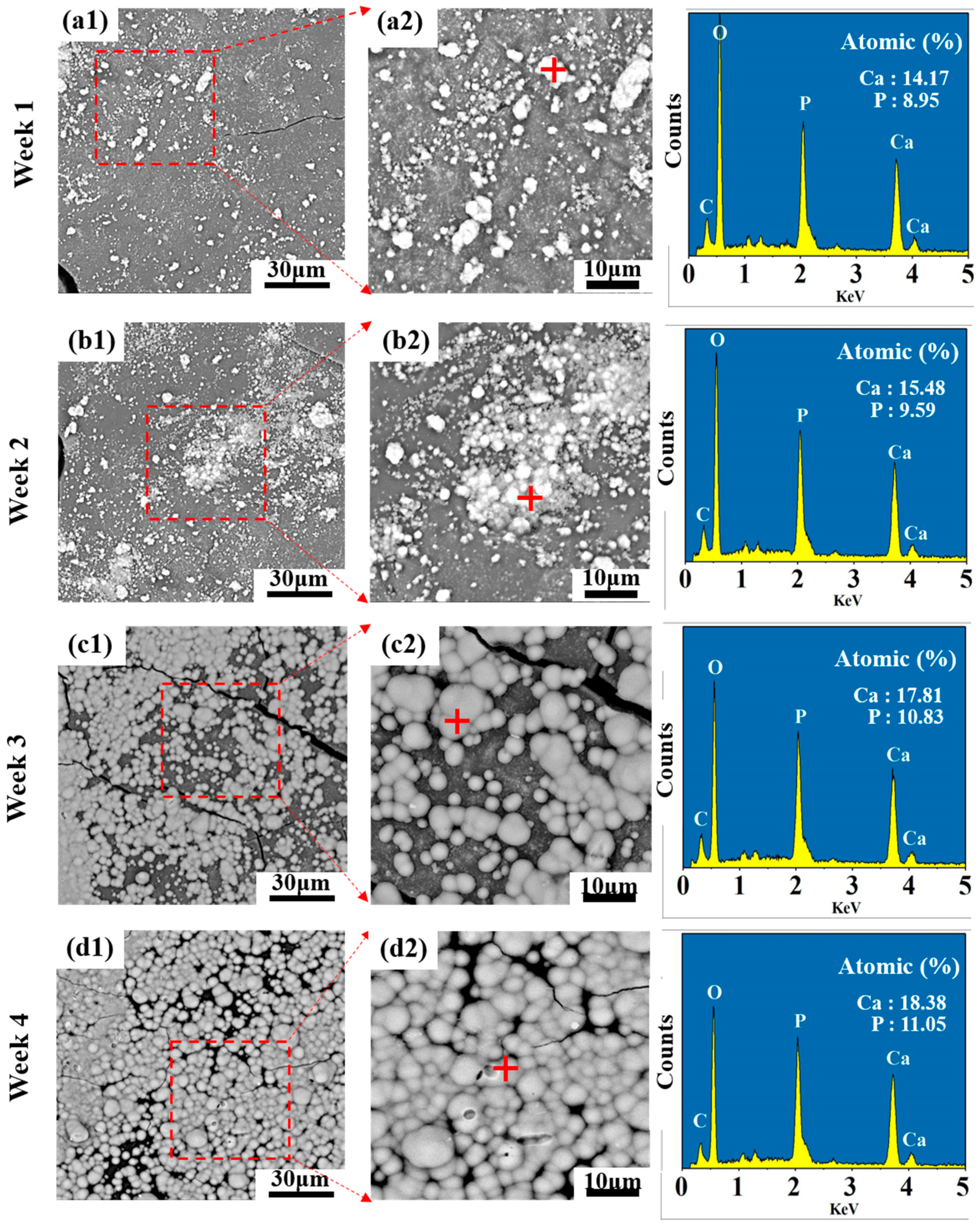
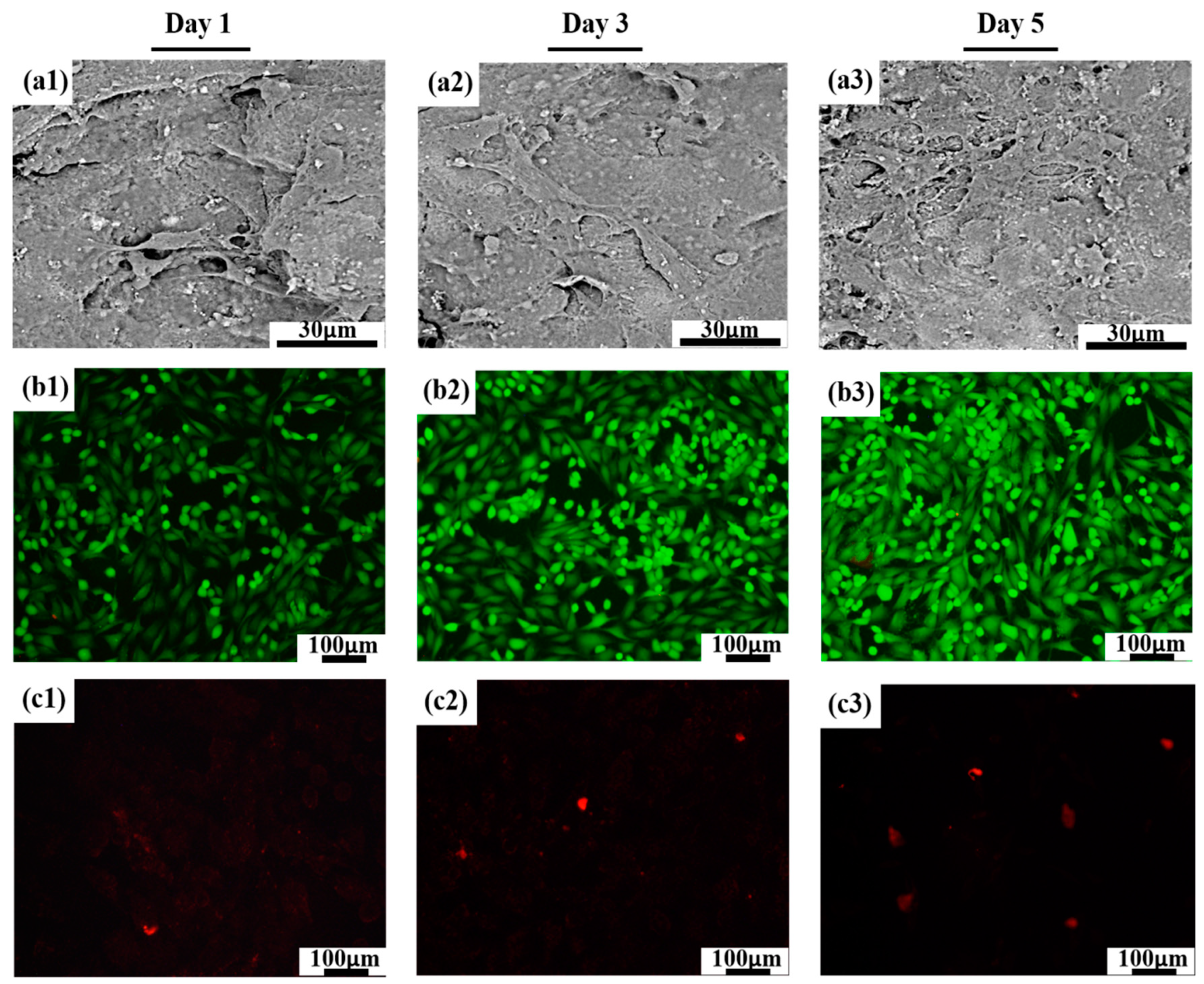
3.6. Bioactivity and Cytocompatibility
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Uskokovic, P.S.; Tang, C.Y.; Tsui, C.P.; Ignjatovic, N.; Uskokovic, D.P. Micromechanical properties of a hydroxyapatite/poly-l-lactide biocomposite using nanoindentation and modulus mapping. J. Eur. Ceram. Soc. 2007, 27, 1559–1564. [Google Scholar] [CrossRef]
- Tham, W.L.; Chow, W.S.; Mohd Ishak, Z.A. Effects of titanate coupling agent on the mechanical, thermal, and morphological properties of poly(methyl methacrylate)/hydroxyapatite denture base composites. J. Compos. Mater. 2011, 45, 2335–2345. [Google Scholar] [CrossRef]
- Szustakiewicz, K.; Stępak, B.; Antończak, A.J.; Maj, M.; Pigłowski, J. Femtosecond laser-induced modification of PLLA/hydroxypatite composite. Polym. Degrad. Stab. 2018, 149, 152–161. [Google Scholar] [CrossRef]
- Li, L.; Song, K.; Chen, Y.; Wang, Y.; Shi, F.; Nie, Y.; Liu, T. Design and Biophysical Characterization of Poly (l-Lactic) Acid Microcarriers with and without Modification of Chitosan and Nanohydroxyapatite. Polymers 2018, 10, 1061. [Google Scholar] [CrossRef]
- Imai, Y.; Nagai, M.; Watanabe, M. Degradation of composite materials composed of tricalcium phosphate and a new type of block polyester containing a poly(L-lactic acid) segment. J. Biomater. Sci. Polym. Ed. 1999, 10, 421–432. [Google Scholar] [CrossRef]
- Hsu, C. Preparation and properties of nano-composite of poly(L-lactide) and surface grafted hydroxyapatite. Appl. Mech. Mater. 2012, 108, 238–243. [Google Scholar]
- Shuai, C.; Zan, J.; Qi, F.; Wang, G.; Liu, Z.; Yang, Y.; Peng, S. NMgO-incorporated PLLA bone scaffolds: Enhanced crystallinity and neutralized acidic products. Mater. Des. 2019, 174, 107801. [Google Scholar] [CrossRef]
- Khosravi, H.; EslamiFarsani, R. Enhanced mechanical properties of unidirectional basalt fiber/epoxy composites using silane-modified Na+-montmorillonite nanoclay. Polym. Test. 2016, 55, 135–142. [Google Scholar] [CrossRef]
- Rooj, S.; Das, A.; Thakur, V.; Mahaling, R.N.; Bhowmick, A.K.; Heinrich, G. Preparation and properties of natural nanocomposites based on natural rubber and naturally occurring halloysite nanotubes. Mater. Des. 2010, 31, 2151–2156. [Google Scholar] [CrossRef]
- Abueva, C.D.G.; Jang, D.-W.; Padalhin, A.; Lee, B.-T. Phosphonate-chitosan functionalization of a multi-channel hydroxyapatite scaffold for interfacial implant-bone tissue integration. J. Mater. Chem. B 2017, 5, 1293–1301. [Google Scholar] [CrossRef]
- Varma, H.K.; Yokogawa, Y.; Espinosa, F.F.; Kawamoto, Y.; Kameyama, T. Porous Calcium Phosphate Coating Over Phosphorylated Chitosan Film by a Biomimetic Method. Biomaterials 1999, 20, 879–884. [Google Scholar] [CrossRef]
- Shinzato, S.; Nakamura, T.; Tamura, J.; Kokubo, T.; Kitamura, Y. Bioactive bone cement: Effects of phosporic ester monomer on mechanical properties and osteoconductivity. J. Biomed. Mater. Res. 2001, 56, 571–577. [Google Scholar] [CrossRef]
- Pramanik, N.; Mohapatra, S.; Bhargava, P.; Pramanik, P. Chemical synthesis and characterization of hydroxyapatite (HAp)-poly (ethylene co vinyl alcohol)(EVA) nanocomposite using a phosphonic acid coupling agent for orthopedic applications. Mater. Sci. Eng. C 2009, 29, 228–236. [Google Scholar] [CrossRef]
- Debeli, D.K.; Zhao, Q.; Guo, J. Study on the Pre-Treatment, Physical and Chemical Properties of Ramie Fibers Reinforced Poly (Lactic Acid) (PLA) Biocomposite. J. Nat. Fibers 2017, 15, 1–15. [Google Scholar] [CrossRef]
- Hao, L.; Savalani, M.M.; Zhang, Y.; Tanner, K.E.; Heath, R.J.; Harris, R.A. Characterization of selective laser-sintered hydroxyapatite-based biocomposite structures for bone replacement. Proc. R. Soc. A 2007, 463, 1857–1869. [Google Scholar] [CrossRef]
- Vo, D.Q.; Kim, E.-J.; Kim, S. Surface modification of hydrophobic nanocrystals using short-chain carboxylic acids. J. Colloid Interface Sci. 2009, 337, 75–80. [Google Scholar] [CrossRef]
- Rath, N.C.; Dimitrijevich, S.; Anbar, M. Effect of polyvinyl phosphonates and ethane hydroxy diphosphonate on mineralization of ectopic bone. Chem. Biol. Interact. 1984, 48, 339–347. [Google Scholar] [CrossRef]
- Shuai, C.; Cheng, Y.; Yang, Y.; Peng, S.; Yang, W.; Qi, F. Laser additive manufacturing of Zn-2Al part for bone repair: Formability, microstructure and properties. J. Alloy. Compd. 2019, 798, 606–615. [Google Scholar] [CrossRef]
- Salmoria, G.V.; Klauss, P.; Paggi, R.A.; Kanis, L.A.; Lago, A. Structure and mechanical properties of cellulose based scaffolds fabricated by selective laser sintering. Polym. Test. 2009, 28, 648–652. [Google Scholar] [CrossRef]
- Park, S.A.; Lee, S.H.; Kim, W.D. Fabrication of porous polycaprolactone/hydroxyapatite (PCL/HA) blend scaffolds using a 3D plotting system for bone tissue engineering. Bioprocess Biosyst. Eng. 2011, 34, 505–513. [Google Scholar] [CrossRef]
- Wang, G.; Qi, F.; Yang, W.; Yang, Y.; He, C.; Peng, S.; Shuai, C. Crystallinity and reinforcement in Poly-l-lactic acid scaffold induced by carbon nanotubes. Adv. Polym. Technol. 2019, 2019, 8625325. [Google Scholar] [CrossRef]
- Roosa, S.M.M.; Kemppainen, J.M.; Moffitt, E.N.; Krebsbach, P.H.; Hollister, S.J. The pore size of polycaprolactone scaffolds has limited influence on bone regeneration in an in vivo model. J. Biomed. Mater. Res. Part A 2010, 92, 359–368. [Google Scholar] [CrossRef]
- Kim, M.; Yun, H.-S.; Kim, G.H. Electric-field assisted 3D-fibrous bioceramic-based scaffolds for bone tissue regeneration: Fabrication, characterization, and in vitro cellular activities. Sci. Rep. 2017, 7, 3166. [Google Scholar] [CrossRef]
- Bareiro, O.F.; dos Santos, L.A. Polydimethylsiloxane/calcium phosphates composites: Effect of the fillers modification on the cross-linking and surface energy. Mater. Sci. Forum 2012, 727–728, 1175–1180. [Google Scholar] [CrossRef]
- Lytkina, D.N.; Shapovalova, Y.G.; Rasskazova, L.A.; Kurzina, I.A.; Filimoshkin, A.G. Obtaining of Biodegradable Polylactide Films and Fibers Filled Hydroxyapatite for Medical Purposes; AIP Publishing: Bandung, Indonesia, 2015; Volume 1688, p. 060004. [Google Scholar]
- Kutikov, A.B.; Song, J. An amphiphilic degradable polymer/hydroxyapatite composite with enhanced handling characteristics promotes osteogenic gene expression in bone marrow stromal cells. Acta Biomater. 2013, 9, 8354–8364. [Google Scholar] [CrossRef]
- Yang, Y.; He, C.; Dianyu, E.; Yang, W.; Qi, F.; Xie, D.; Shen, L.; Peng, S.; Shuai, C. Mg bone implant: Features, developments and perspectives. Mater. Des. 2019, 185, 108259. [Google Scholar] [CrossRef]
- Bobel, A.C.; Lohfeld, S.; Shirazi, R.N.; McHugh, P.E. Experimental mechanical testing of Poly (L-Lactide) (PLLA) to facilitate pre-degradation characteristics for application in cardiovascular stenting. Polym. Test. 2016, 54, 150–158. [Google Scholar] [CrossRef]
- Feng, P.; Kong, Y.; Yu, L.; Li, Y.; Gao, C.; Peng, S.; Pan, H.; Zhao, Z.; Shuai, C. Molybdenum disulfide nanosheets embedded with nanodiamond particles: Co-dispersion nanostructures as reinforcements for polymer scaffolds. Appl. Mater. Today 2019, 17, 216–226. [Google Scholar] [CrossRef]
- Gao, C.; Yao, M.; Shuai, C.; Peng, S.; Deng, Y. Nano-SiC reinforced Zn biocomposites prepared via laser melting: Microstructure, mechanical properties and biodegradability. J. Mater. Sci. Technol. 2019, 35, 2608–2617. [Google Scholar] [CrossRef]
- Chieng, B.; Ibrahim, N.; Yunus, W.; Hussein, M.; Then, Y.; Loo, Y. Effects of graphene nanoplatelets and reduced graphene oxide on poly(lactic acid) and plasticized poly(lactic acid): A comparative study. Polymers 2014, 6, 2232–2246. [Google Scholar] [CrossRef]
- Cao, Y.; Shi, T.; Jiao, C.; Liang, H.; Chen, R.; Tian, Z.; Zou, A.; Yang, Y.; Wei, Z.; Wang, C.; et al. Fabrication and properties of zirconia/hydroxyapatite composite scaffold based on digital light processing. Ceram. Int. 2020, 46, 2300–2308. [Google Scholar] [CrossRef]
- Zare, Y.; Rhee, K.Y. The mechanical behavior of polymer/CNT nanocomposites assuming imperfect interfacial bonding between polymer matrix and nanoparticles and percolation of interphase regions. Compos. Sci. Technol. 2017, 144, 18–25. [Google Scholar] [CrossRef]
- Prasadh, S.; Wong, R.C.W. Unraveling the mechanical strength of biomaterials used as a bone scaffold in oral and maxillofacial defects. Oral Sci. Int. 2018, 15, 48–55. [Google Scholar] [CrossRef]
- Shuai, C.; Liu, G.; Yang, Y.; Yang, W.; He, C.; Wang, G.; Liu, Z.; Qi, F.; Peng, S. Functionalized BaTiO3 enhances piezoelectric effect towards cell response of bone scaffold. Colloids Surf. B Biointerfaces 2020, 185, 110587. [Google Scholar] [CrossRef]
- Cai, Z.; Cong, Z.; Jie, G.; Zhang, Q.; Zhao, K. Electrospun carboxyl multi-walled carbon nanotubes grafted polyhydroxybutyrate composite nanofibers membrane scaffolds: Preparation, characterization and cytocompatibility. Mater. Sci. Eng. C 2017, 82, 29–40. [Google Scholar]
- Dutra, R.C.L.; Lourenço, V.L.; Diniz, M.F.; Azevedo, M.F.P.; Barbosa, R.V.; Soares, B.G. Poly(ethylene-co-vinyl alcohol-co-vinyl mercaptoacetate) (EVALSH)-determination of the vinyl mercaptoacetate content by thermogravimetric analysis and FTIR spectroscopy. Polym. Bull. 1996, 36, 593–600. [Google Scholar] [CrossRef]
- Ji, L.; Shi, H.; Diao, H.; Si, Y.; Zhu, A. Surface modified nano-hydroxyapatite/poly(lactide acid) composite and its osteocyte compatibility. Mater. Sci. Eng. C 2012, 32, 1796–1801. [Google Scholar]
- Liang, H.; Yang, Y.; Xie, D.; Li, L.; Mao, N.; Wang, C.; Tian, Z.; Jiang, Q.; Shen, L. Trabecular-like Ti-6Al-4V scaffolds for orthopedic: Fabrication by selective laser melting and in vitro biocompatibility. J. Mater. Sci. Technol. 2019, 35, 1284–1297. [Google Scholar] [CrossRef]
- Song, X.; Ling, F.; Ma, L.; Yang, C.; Chen, X. Electrospun hydroxyapatite grafted poly(l-lactide)/poly(lactic-co-glycolic acid) nanofibers for guided bone regeneration membrane. Compos. Sci. Technol. 2013, 79, 8–14. [Google Scholar] [CrossRef]
- Akindoyo, J.O.; Beg, M.D.H.; Ghazali, S.; Heim, H.P.; Feldmann, M. Effects of surface modification on dispersion, mechanical, thermal and dynamic mechanical properties of injection molded PLA-hydroxyapatite composites. Compos. Part A Appl. Sci. Manuf. 2017, 103, 96–105. [Google Scholar] [CrossRef]
- Shuai, C.; Zan, J.; Yang, Y.; Peng, S.; Yang, W.; Qi, F.; Shen, L.; Tian, Z. Surface modification enhances interfacial bonding in PLLA/MgO bone scaffold. Mater. Sci. Eng. C 2020, 108, 110486. [Google Scholar] [CrossRef]
- Nejati, E.; Mirzadeh, H.; Zandi, M. Synthesis and characterization of nano-hydroxyapatite rods/poly(l-lactide acid) composite scaffolds for bone tissue engineering. Compos. Part A Appl. Sci. Manuf. 2008, 39, 1589–1596. [Google Scholar] [CrossRef]
- Pluta, M.; Murariu, M.; Dechief, A.-L.; Bonnaud, L.; Galeski, A.; Dubois, P. Impact-modified polylactide–calcium sulfate composites: Structure and properties. J. Appl. Polym. Sci. 2012, 125, 4302–4315. [Google Scholar] [CrossRef]
- Shuai, C.; Yang, W.; He, C.; Peng, S.; Gao, C.; Yang, Y.; Qi, F.; Feng, P. A magnetic micro-environment in scaffolds for stimulating bone regeneration. Mater. Des. 2020, 185, 108275. [Google Scholar] [CrossRef]
- Gelder, J.M.V.; Breuer, E.; Schlossman, A.; Ornoy, A.; Golomb, G. In vitro and in vivo effects of tetrakisphosphonates on bone resorption, tumor osteolysis, ectopic calcification, and macrophages. J. Pharm. Sci. 1997, 86, 283–289. [Google Scholar] [CrossRef]
- Gao, C.; Yao, M.; Li, S.; Feng, P.; Peng, S.; Shuai, C. Highly biodegradable and bioactive Fe-Pd-bredigite biocomposites prepared by selective laser melting. J. Adv. Res. 2019, 20, 91–104. [Google Scholar] [CrossRef]
- Yang, Y.; Guo, X.; He, C.; Gao, C.; Shuai, C. Regulating Degradation Behavior by Incorporating Mesoporous Silica for Mg Bone Implants. ACS Biomater. Sci. Eng. 2018, 4, 1046–1054. [Google Scholar] [CrossRef]
- He, S.; Yang, S.; Zhang, Y.; Li, X.; Gao, D.; Zhong, Y.; Cao, L.; Ma, H.; Liu, Y.; Li, G.; et al. LncRNA ODIR1 Inhibits Osteogenic Differentiation of hUC-MSCs through the FBXO25/H2BK120ub/H3K4me3/OSX Axis. Cell Death Dis. 2019, 10, 1–16. [Google Scholar] [CrossRef]
- Yanagida, H.; Okada, M.; Masuda, M.; Ueki, M.; Narama, I.; Kitao, S.; Koyama, Y.; Furuzono, T.; Takakuda, K. Cell adhesion and tissue response to hydroxyapatite nanocrystal-coated poly(l-lactic acid) fabric. J. Biosci. Bioeng. 2009, 108, 235–243. [Google Scholar] [CrossRef]
- Smieszek, A.; Marycz, K.; Szustakiewicz, K.; Kryszak, B.; Targonska, S.; Zawisza, K.; Watras, A.; Wiglusz, R.J. New approach to modification of poly (l-lactic acid) with nano-hydroxyapatite improving functionality of human adipose-derived stromal cells (hASCs) through increased viability and enhanced mitochondrial activity. Mater. Sci. Eng. C 2019, 98, 213–226. [Google Scholar] [CrossRef]
| Filler Formulations | Material Mass (g) | |||
|---|---|---|---|---|
| PLLA/HAP Composite | PLLA/C-HAP Composite | |||
| PLLA | HAP | PLLA | C-HAP | |
| 0% | 10 | 0 | 10 | 0 |
| 5% | 9.5 | 0.5 | 9.5 | 0.5 |
| 10% | 9 | 1 | 9 | 1 |
| 15% | 8.5 | 1.5 | 8.5 | 1.5 |
| 20% | 8 | 2 | 8 | 2 |
| 25% | 7.5 | 2.5 | 7.5 | 2.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shuai, C.; Yu, L.; Yang, W.; Peng, S.; Zhong, Y.; Feng, P. Phosphonic Acid Coupling Agent Modification of HAP Nanoparticles: Interfacial Effects in PLLA/HAP Bone Scaffold. Polymers 2020, 12, 199. https://doi.org/10.3390/polym12010199
Shuai C, Yu L, Yang W, Peng S, Zhong Y, Feng P. Phosphonic Acid Coupling Agent Modification of HAP Nanoparticles: Interfacial Effects in PLLA/HAP Bone Scaffold. Polymers. 2020; 12(1):199. https://doi.org/10.3390/polym12010199
Chicago/Turabian StyleShuai, Cijun, Li Yu, Wenjing Yang, Shuping Peng, Yancheng Zhong, and Pei Feng. 2020. "Phosphonic Acid Coupling Agent Modification of HAP Nanoparticles: Interfacial Effects in PLLA/HAP Bone Scaffold" Polymers 12, no. 1: 199. https://doi.org/10.3390/polym12010199
APA StyleShuai, C., Yu, L., Yang, W., Peng, S., Zhong, Y., & Feng, P. (2020). Phosphonic Acid Coupling Agent Modification of HAP Nanoparticles: Interfacial Effects in PLLA/HAP Bone Scaffold. Polymers, 12(1), 199. https://doi.org/10.3390/polym12010199






