Novel 3-Substituted 8-Methoxycoumarin Derivatives as Anti-Breast Cancer Drugs
Abstract
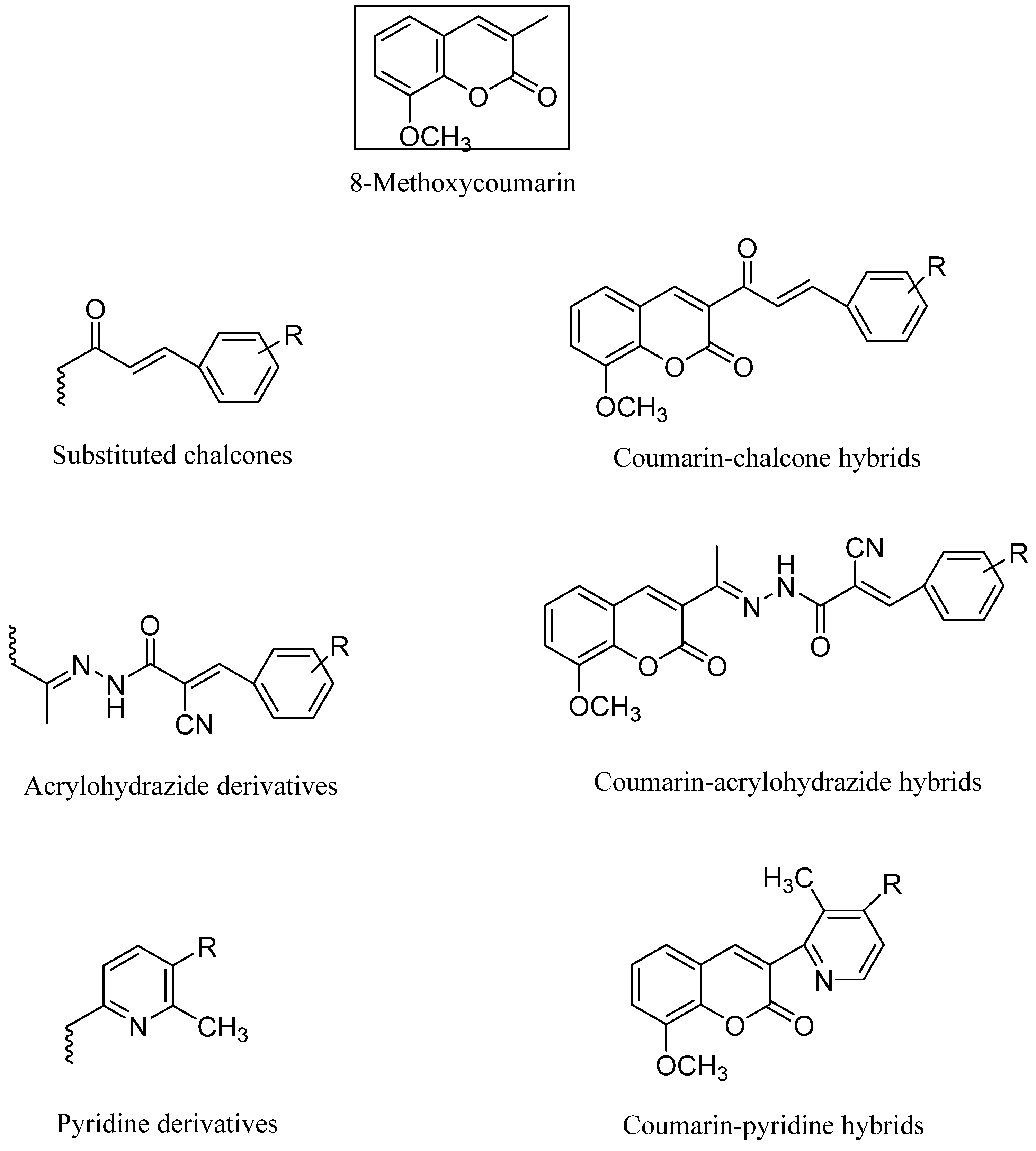
1. Introduction
2. Results and Discussion
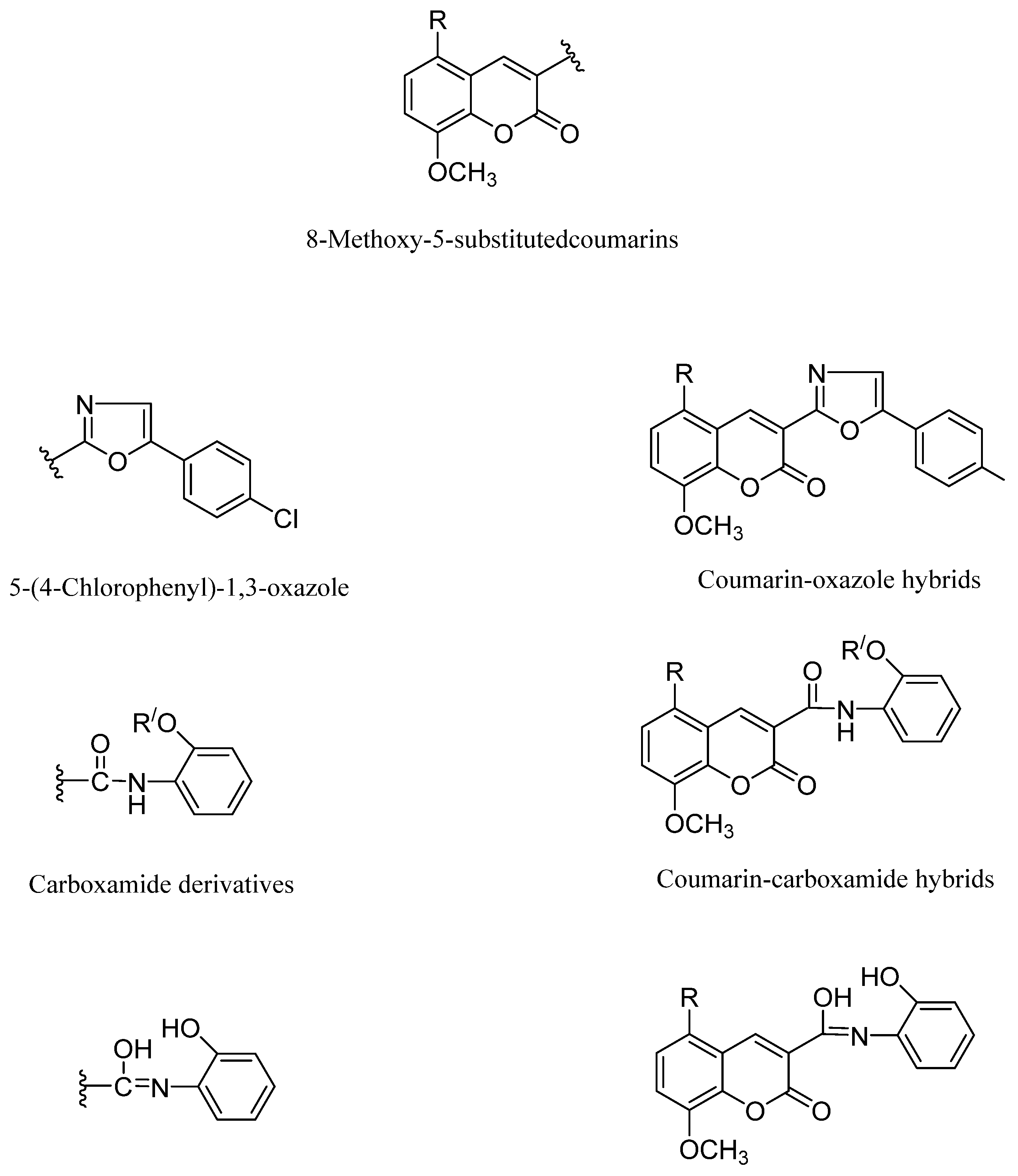
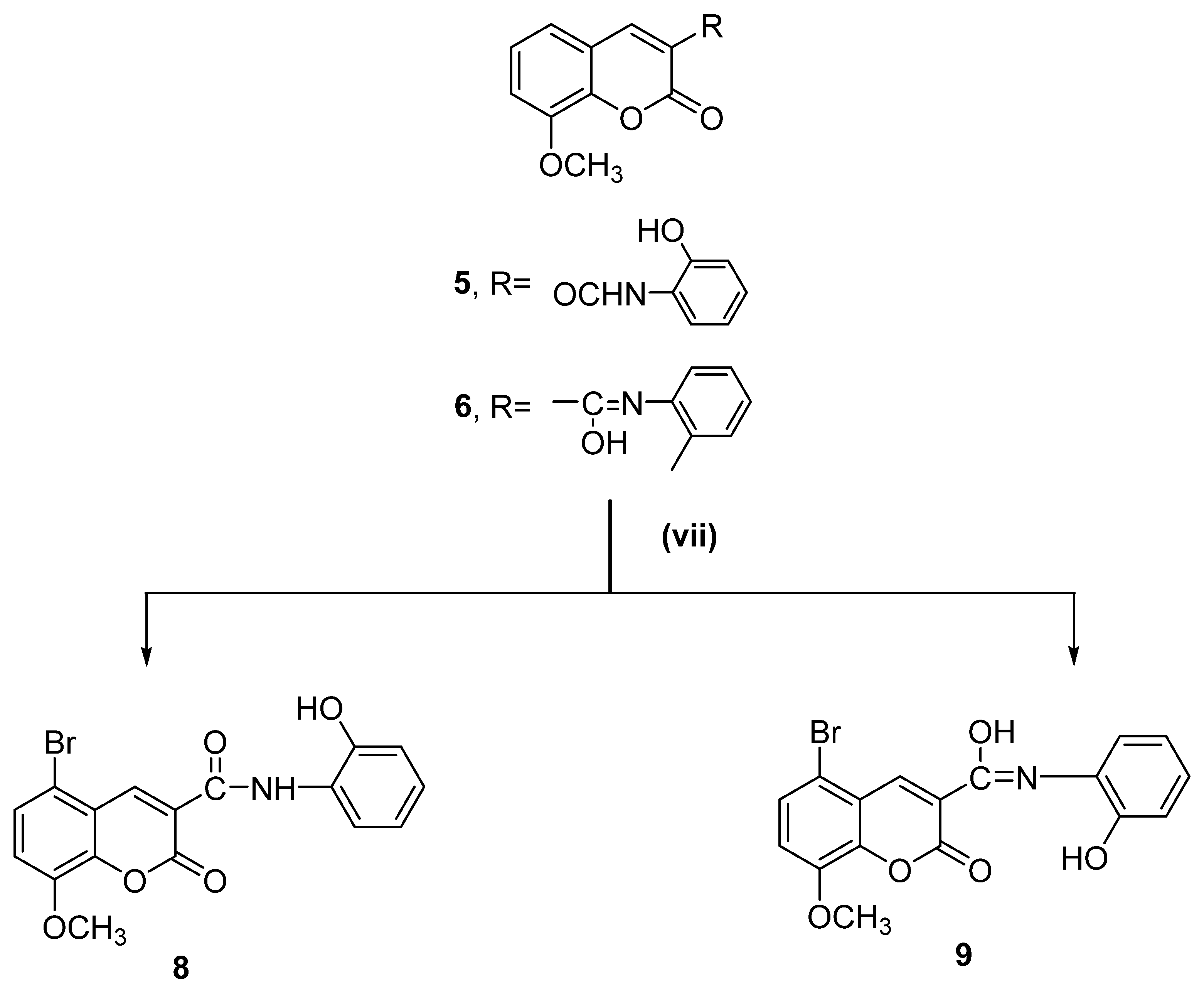
2.1. Chemistry
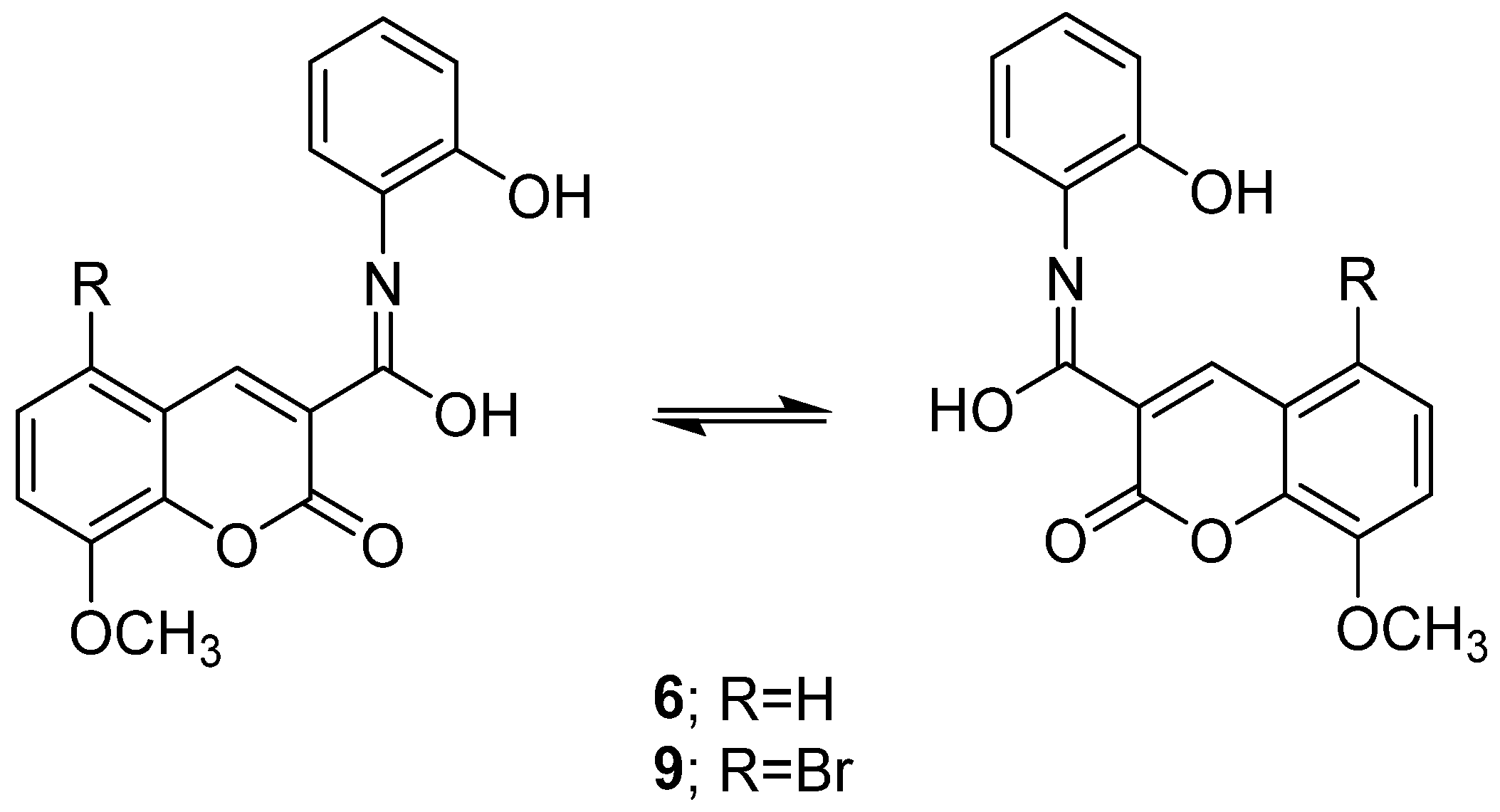
2.2. NMR Spectra Investigation of 8-Methoxycoumarin-3-Carboxamide Derivatives (Compounds 3–9)
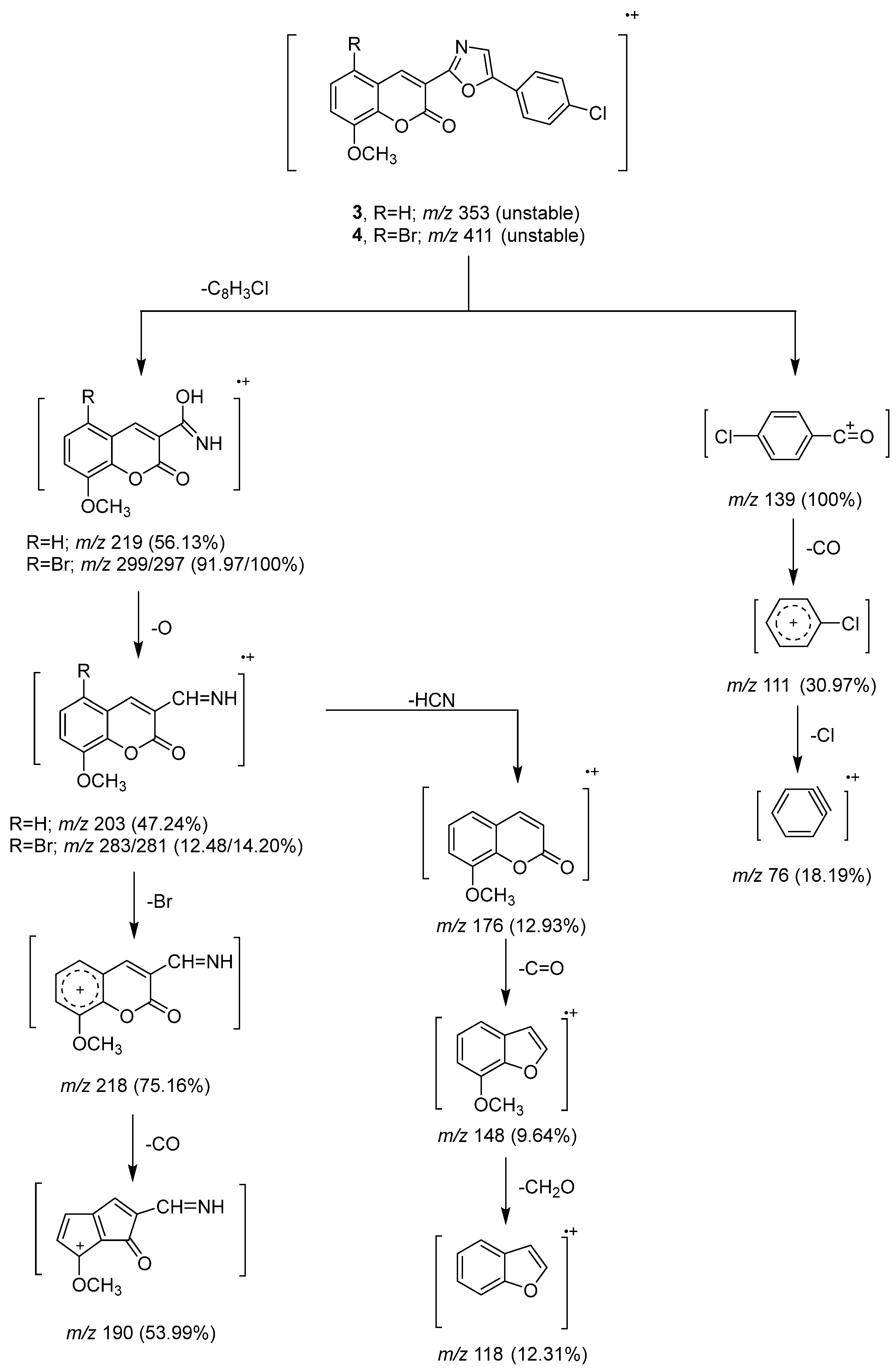
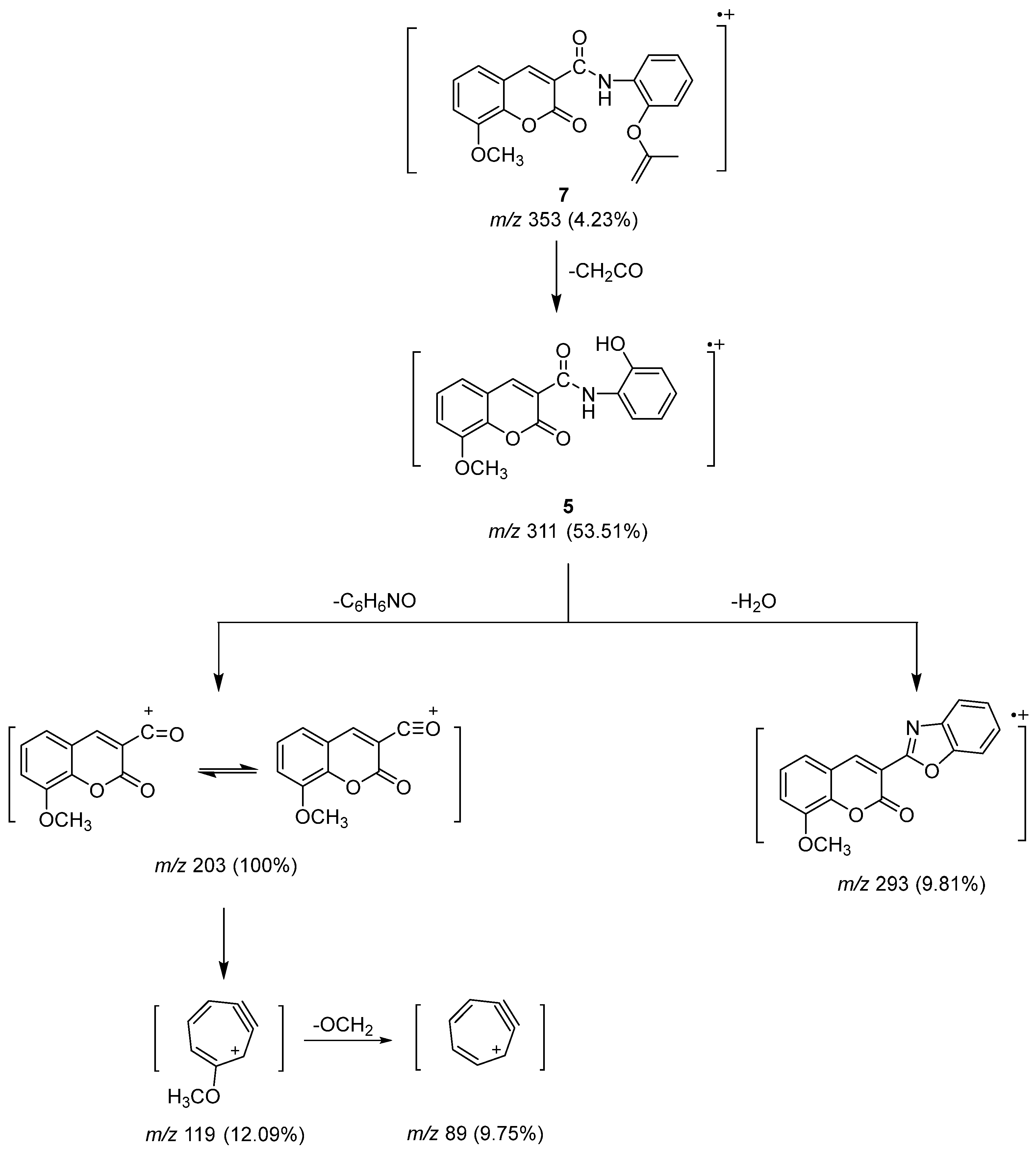
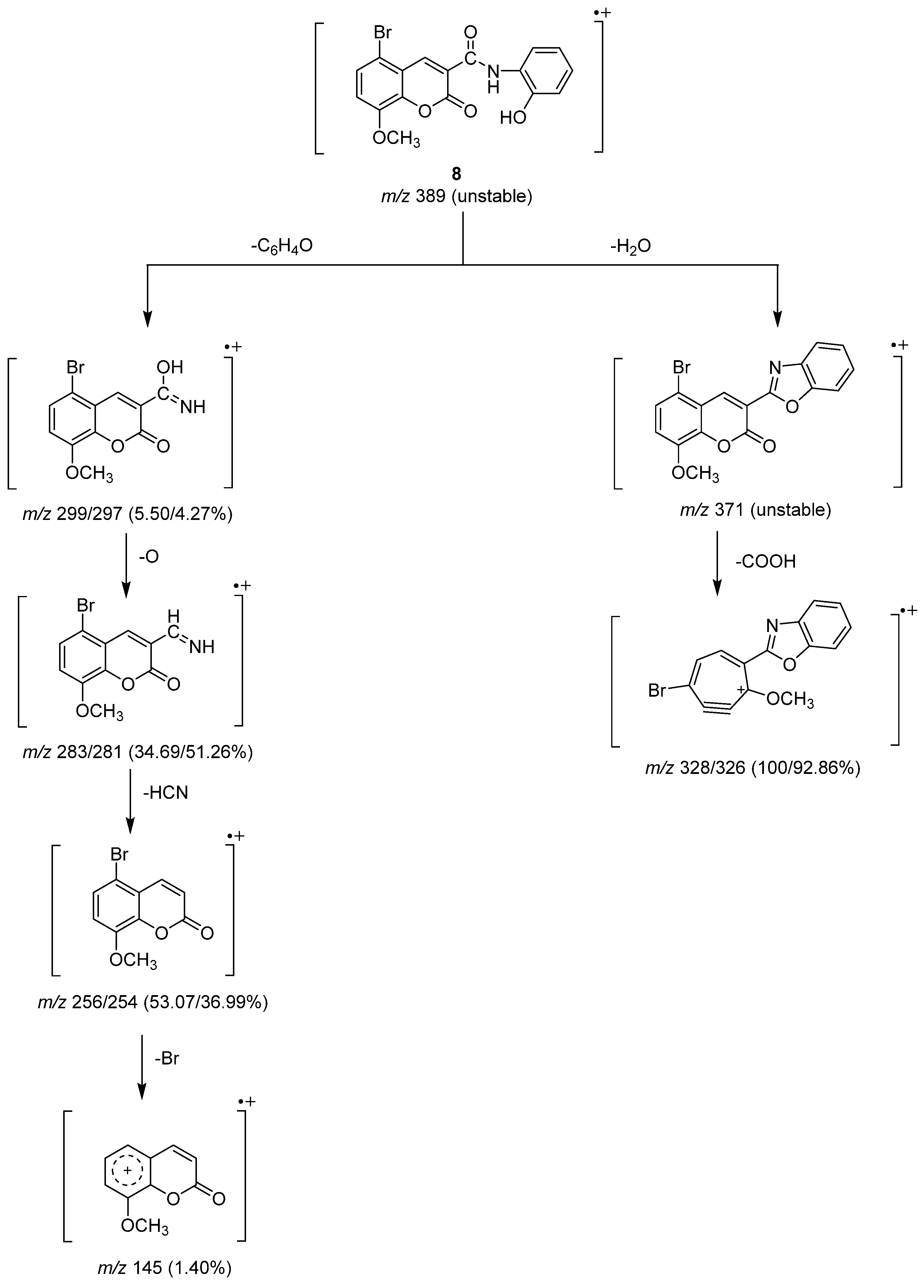
2.3. Mass Spectrometry Investigation
2.4. In Vitro Antitumor Activity
2.4.1. In Vitro Cytotoxic Effects against Breast Cancer Cell Lines
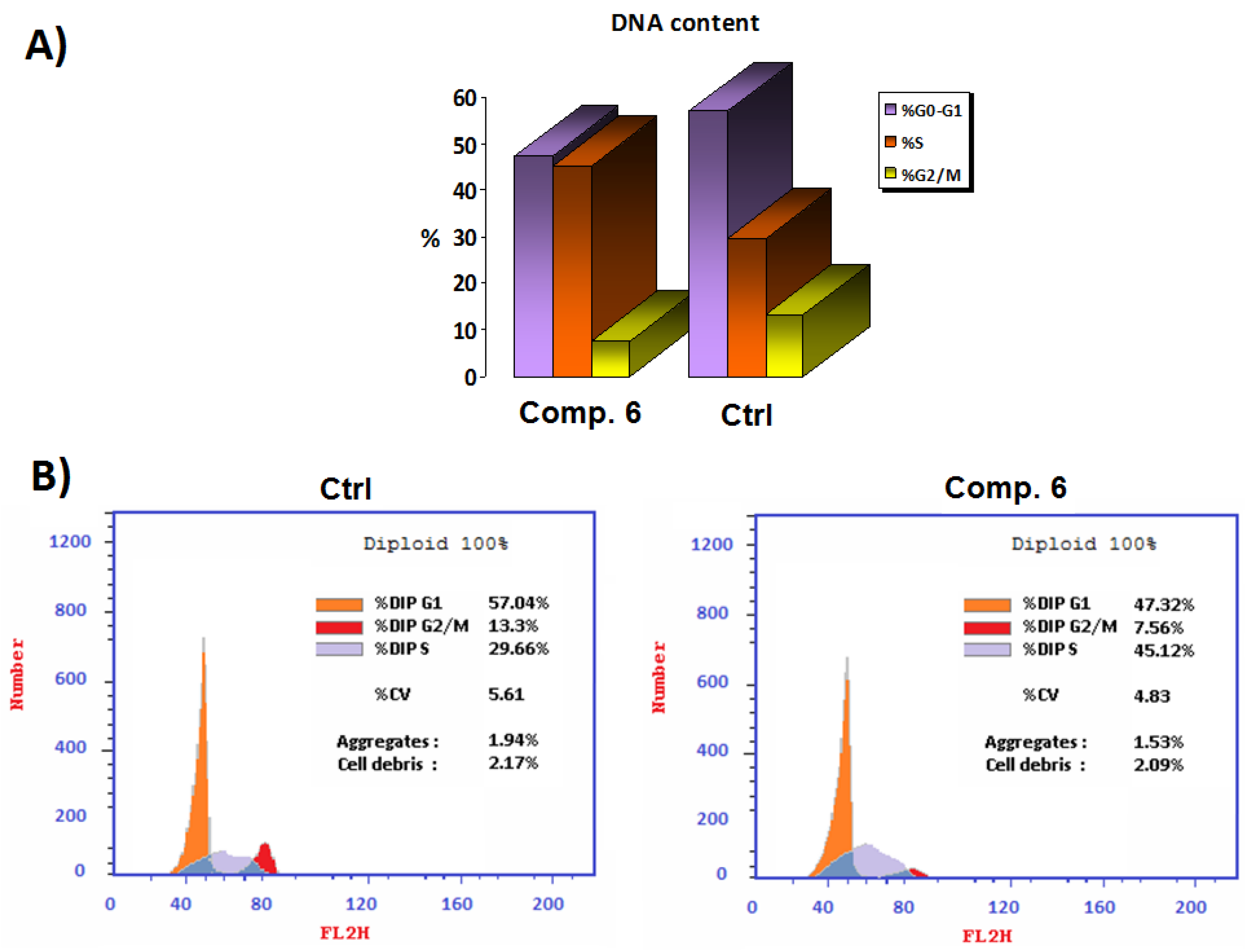
2.4.2. Cell Cycle Analysis
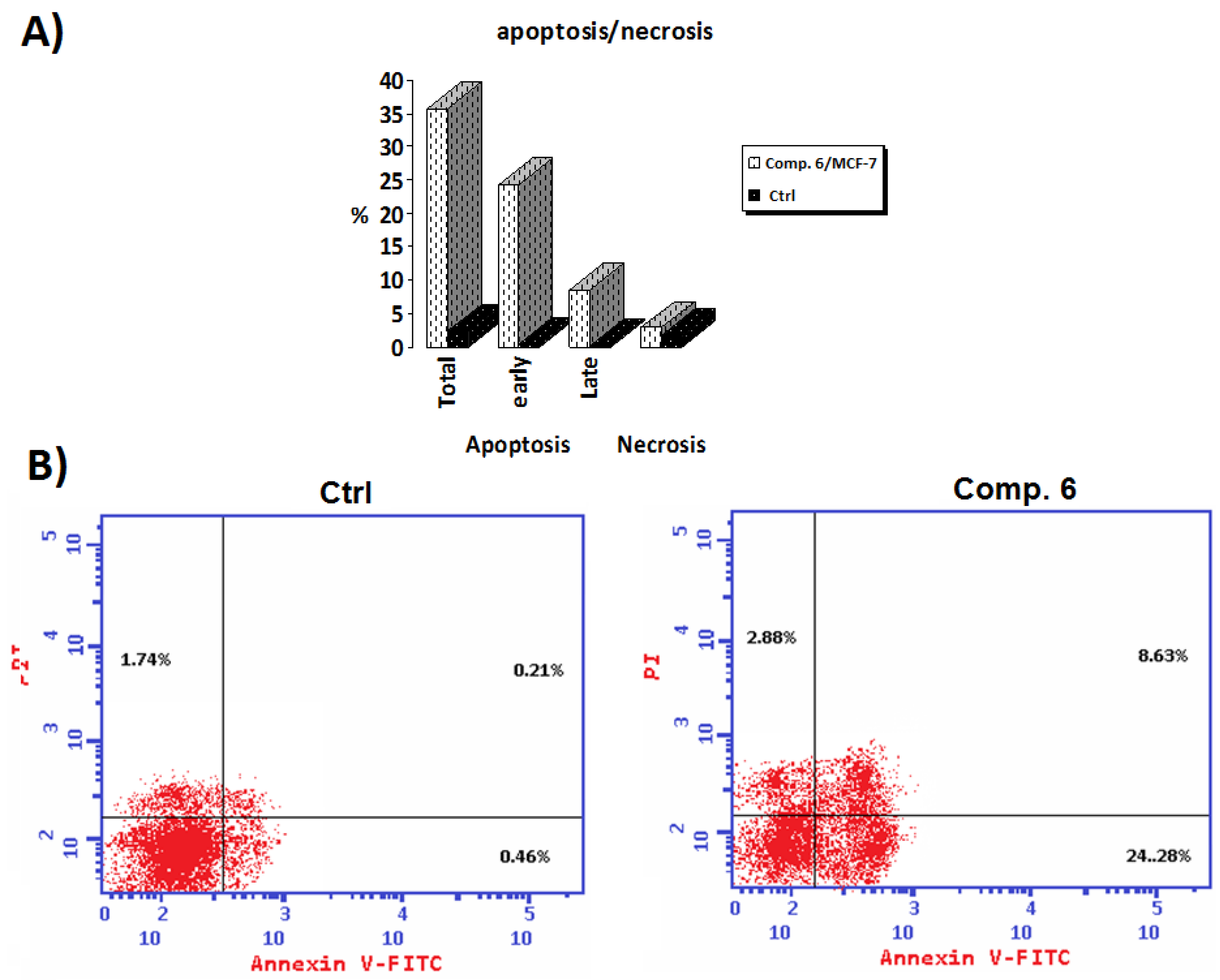
2.4.3. Annexin V-FITC/PI Screening
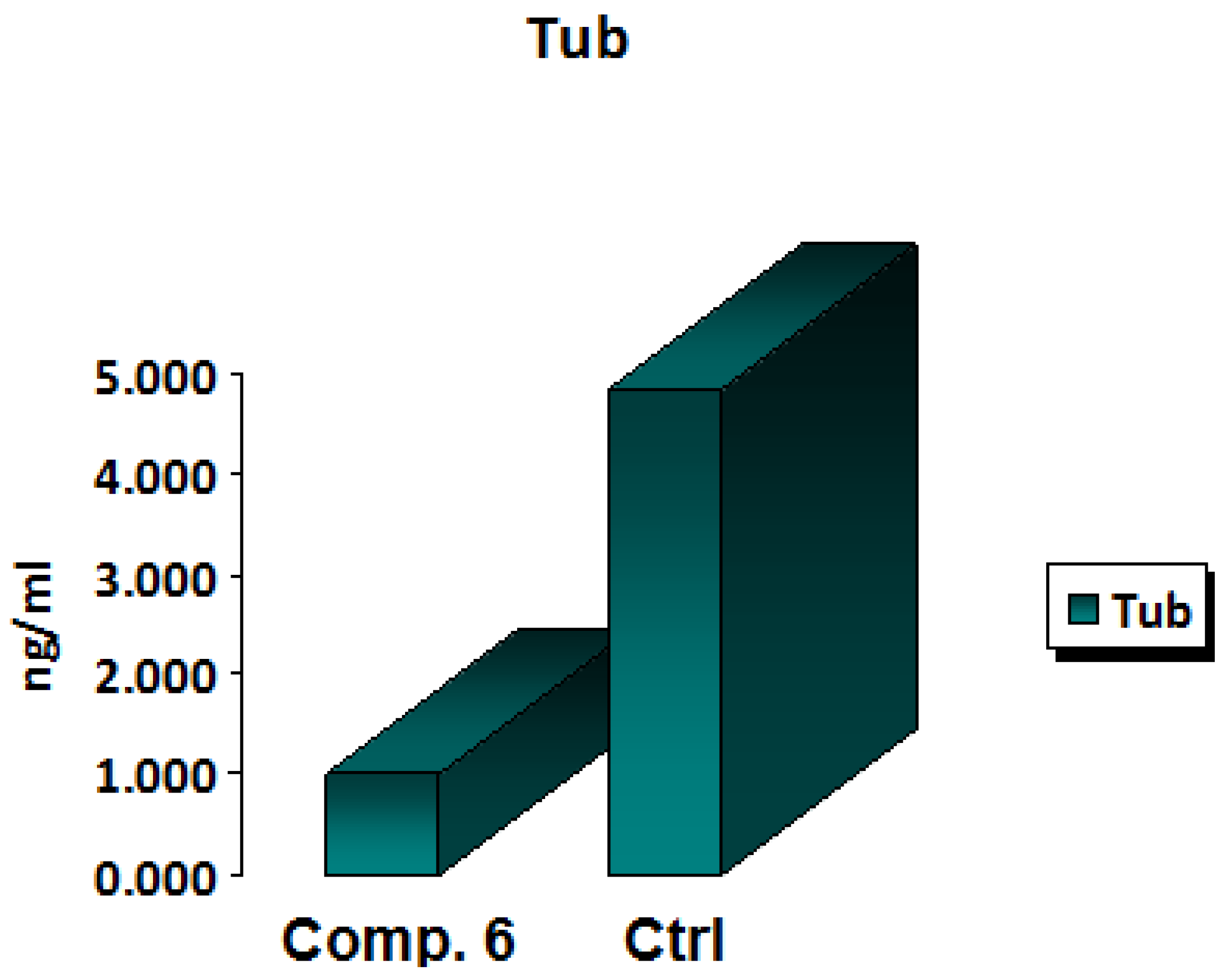
2.4.4. Tubulin Polymerization Inhibition Assay
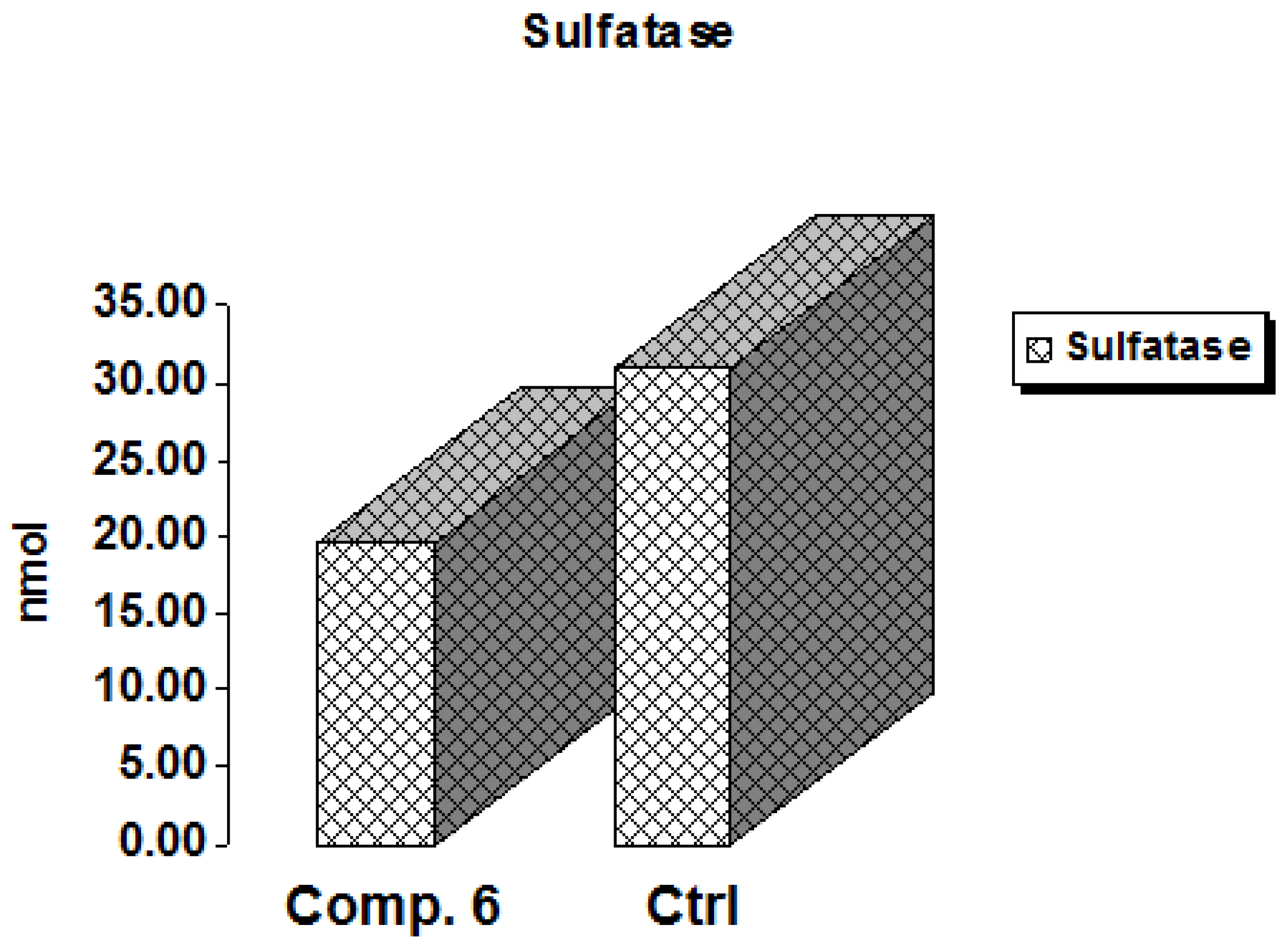
2.4.5. In Vitro Sulfatase Polymerization Inhibition Assay
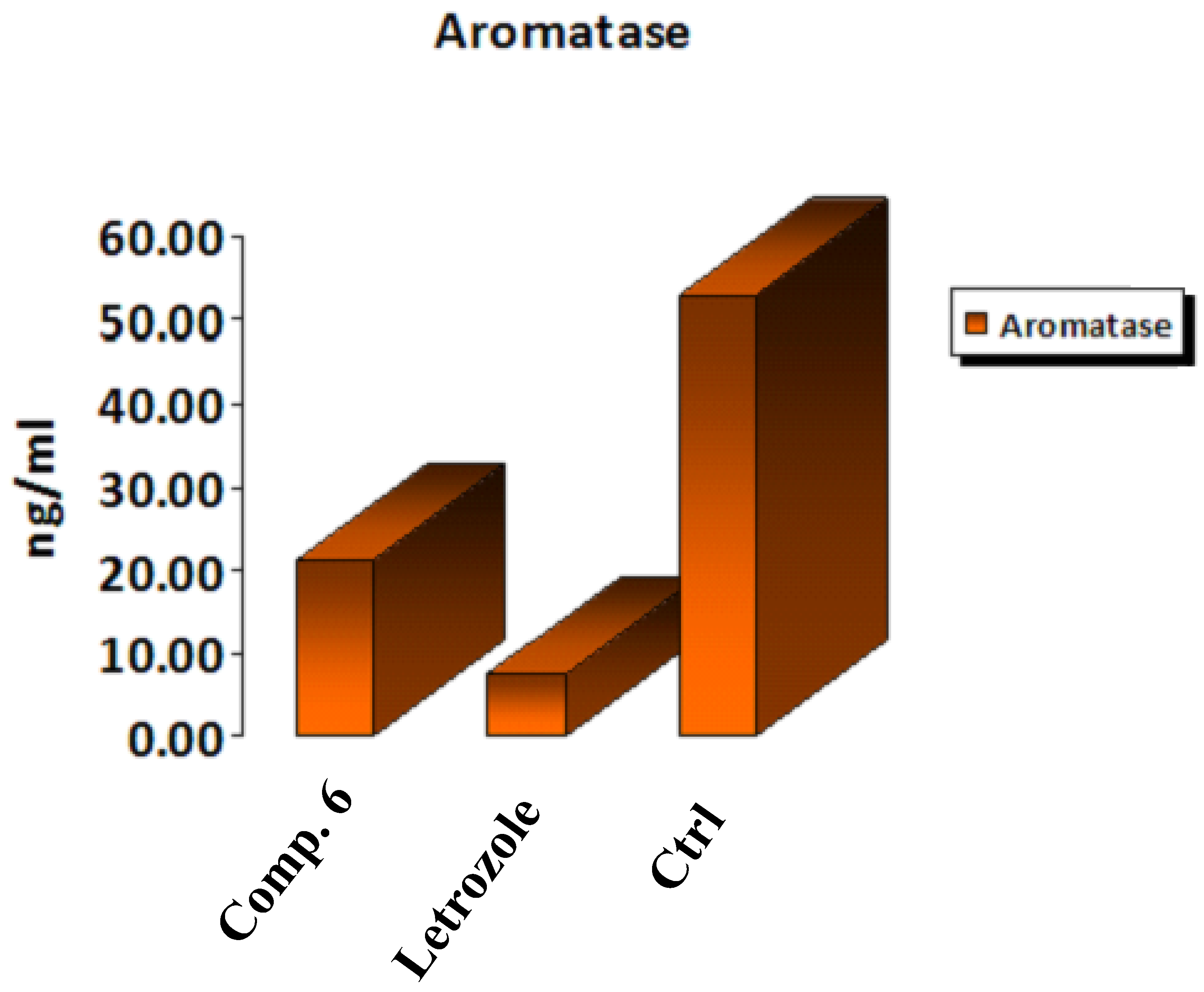
2.4.6. Aromatase Enzyme Assay of Compound 6
2.4.7. Molecular Docking
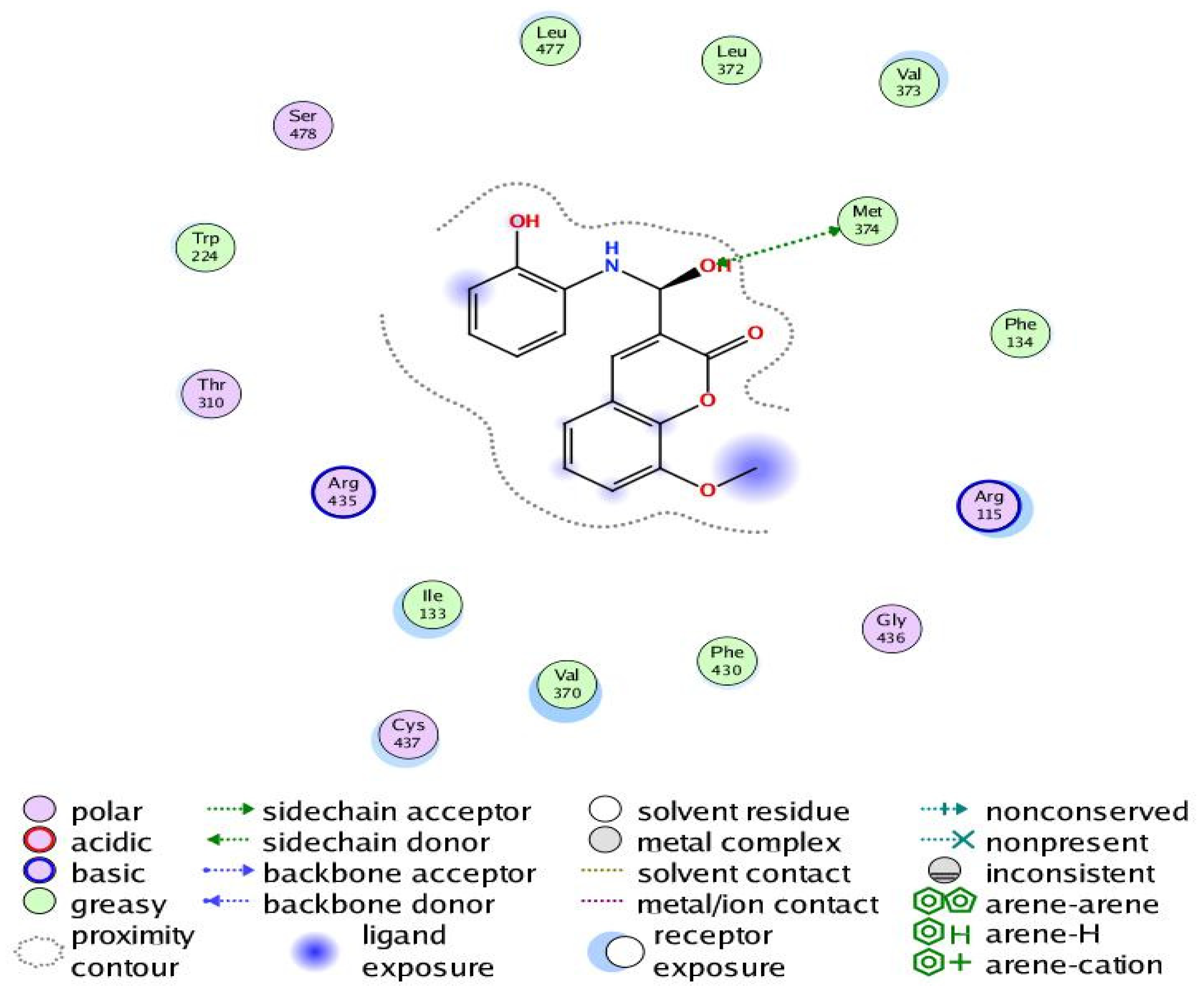
The Human Progesterone Receptor
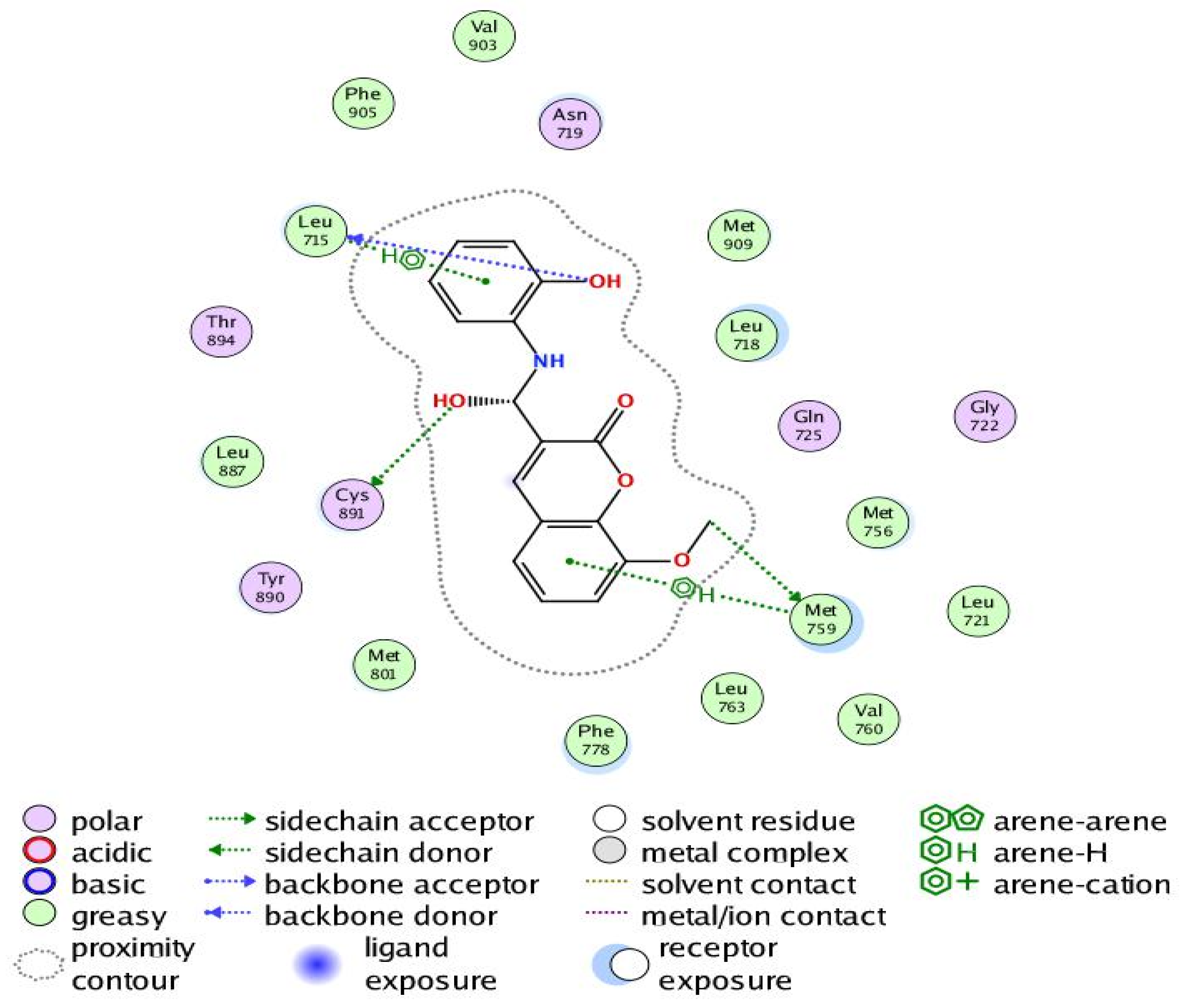
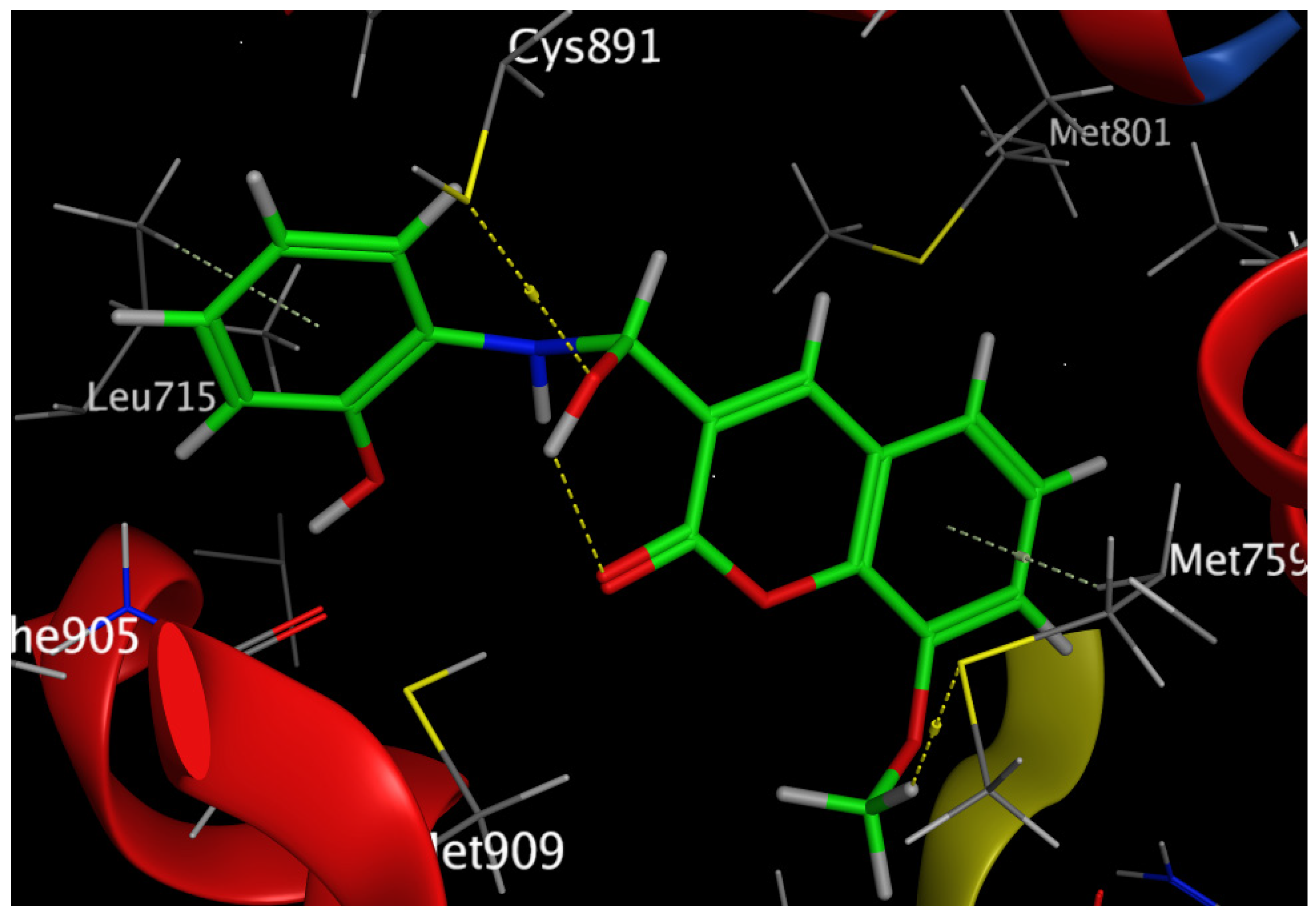
The Human Aromatase Cytochrome P450 (CYP19A1)
3. Materials and Methods
3.1. Chemistry
3.1.1. Ethyl 8-Methoxycoumarin-3-Carboxylate (Compound 1)
3.1.2. Synthesis of 8-Methoxycoumarin-3-Carboxamide (Compound 2)
3.1.3. Synthesis of 3-(5-(4-Chlorophenyl)oxazol-2-yl)-8-Methoxycoumarin (Compound 3)
3.1.4. Condensation of Ester Coumarin (Compound 1) with 2-Aminophenol: Formation of Compounds 5 and 6
3.1.5. Synthesis of 2-(8-Methoxycoumarin-3-Carboxamido)phenyl Acetate (Compound 7)
3.1.6. General Procedure for the Bromination Reactions of Compounds 3, 5, and 6: Formation of Bromo Derivatives Compounds 4, 8, and 9
3.2. Biological Assay
3.2.1. In Vitro Cytotoxicity Assay against (MCF-7) and (MDA-MB-231) Cell Lines
3.2.2. Cell Cycle Analysis
3.2.3. Annexin V-FITC/PI Assay of Compound 6
3.2.4. In Vitro Evaluation of β-Tubulin Inhibition Assay
3.2.5. Sulfatase Enzyme Inhibitory Assay
3.2.6. In Vitro Aromatase Enzyme Inhibitory Assay
3.2.7. Preparation of Protein and Molecular Docking
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sharma, S.; Singh, J.; Ojha, R.; Singh, H.; Kaur, M.; Bedi, P.M.S.; Nepali, K. Design Strategies, Structure Activity Relationship and Mechanistic Insights for Purine as Kinase Inhibitors. Eur. J. Med. Chem. 2016, 112, 298–346. [Google Scholar] [CrossRef] [PubMed]
- Nepali, K.; Sharn, S.; Sharma, M.; Bedi, P.M.S.; Dhar, K.I. Rational Approaches, Design Strategies, Structure Activity Relationship and Mechanistic Insights for Anticancer Hybrids. Eur. J. Med. Chem. 2014, 77, 422–487. [Google Scholar] [CrossRef]
- Nepali, K.; Ojha, R.; Sharma, S.; Bedi, P.M.S.; Dahr, K.I. Tubulin Inhibitors: A Patent Survey. Recent Pat. Anticancer Drug Discov. 2014, 9, 303–339. [Google Scholar] [CrossRef] [PubMed]
- Marco-Contelles, J.; Soriano, E. The Medicinal Chemistry of Hybrid-based Drugs Targeting Multiple Sites of Action. Curr. Med. Chem. 2011, 11, 2714–2715. [Google Scholar] [CrossRef] [PubMed]
- Bansal, Y.; Silakari, O. Multifunctional compounds: Smart molecules for multifactorial diseases. Eur. J. Med. Chem. 2014, 76, 31. [Google Scholar] [CrossRef] [PubMed]
- Geldenhys, W.J.; Youdim, M.R.H.; Carroll, R.T.; Van der Schyf, C. The emergence of designed multiple ligands for neurodegenerative disorders. J. Prog. Neurobiol. 2011, 94, 347. [Google Scholar] [CrossRef]
- Zhang, H.Y. One-compound-multiple-targets strategy to combat Alzheimer’s disease. FEBS Lett. 2005, 579, 5260. [Google Scholar] [CrossRef]
- Geldenhys, W.J.; Van der Schyf, C. Multimodal drugs and their future for Alzheimer’s and Parkinson’s disease. J. Int. Rev. Neurobiol. 2011, 100, 107. [Google Scholar]
- Flores-Morales, V.; Villasana-Ruíz, A.P.; Garza-Veloz, I.; González-Delgado, S.; Martinez-Fierro, M.L. Therapeutic Effects of Coumarins with Different Substitution Patterns. Molecules 2023, 28, 2413. [Google Scholar] [CrossRef]
- Vilar, S.; Quezada, E.; Santana, L.; Uriarte, E.; Yanez, M.; Fraiz, N.; Alcaide, C.; Cano, E.; Orallo, F. Design, synthesis, and vasorelaxant and platelet antiaggregatory activities of coumarin–resveratrol hybrids. Bioorg. Med. Chem. Lett. 2006, 16, 257. [Google Scholar] [CrossRef]
- Song, H.Y.; Ngai, M.H.; Song, Z.Y.; MacAry, P.A.; Hobley, J.; Lear, M. Practical synthesis of maleimides and coumarin-linked probes for protein and antibodylabellingviareduction of native disulfides. J. Biomol. Chem. 2009, 7, 3400. [Google Scholar] [CrossRef]
- Melagraki, G.; Afantitis, A.; Igglesst, M.O.; Detsi, A.; Koufaki, M.; Kontogiorgis, C.; Hadjipavlou, L.D. Synthesis and evaluation of the antioxidant and anti-inflammatory activity of novel coumarin-3-aminoamides and their alpha-lipoic acid adducts. Eur. J. Med. Chem. 2009, 44, 3020. [Google Scholar] [CrossRef]
- Kamath, P.R.; Sunil, D.; Josheph, M.M.; Salam, A.A.A.; Sreelekha, T.T. Indole-coumarin-thiadiazole hybrid: An appraisal of their MCF-7 cell growth inhibition, apoptic, antimetastatic and computational BCL-2 binding potential. Eur. J. Med. Chem. 2017, 136, 442–451. [Google Scholar] [CrossRef]
- Mokale, S.N.; Begum, A.; Sakle, N.S.; Shelke, V.R.; Bhavale, S.A. Design, synthesis and anticancer screening of 3-(3-(substitutedphenyl)acryloyl)-2H-chromen-2-ones as selective anti-brast cancer agent. Biomed. Pharmacother. 2017, 89, 966–972. [Google Scholar] [CrossRef]
- Falcon, I.H.; Amesty, A.; Afonso, L.A.; Castrillejo, I.L.; Machin, F.; Estevez Braun, A. Synthesis and biological evaluation of naphthoquinpne-coumarin conjugates as topoisomerase II inhibitors. Bioorg. Med. Chem. Lett. 2017, 27, 484–489. [Google Scholar] [CrossRef]
- Elshemy, H.A.H.; Zaki, M.A. Design and synthesis of new coumarin hybrids and insight into their mode of antiproliferative action. Bioorg. Med. Chem. 2017, 25, 1066–1075. [Google Scholar] [CrossRef]
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global Cancer Statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef]
- Kim, S.-K. Handbook of Anticancer Drugs from Marine Origin; Springer International Publishing: Cham, Switzerland, 2015. [Google Scholar]
- WHO. Cancer Fact Sheet No. 297; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Radwan, E.M.; Elsayed, E.H.; El-Moniem, M.A.; Moustafa, A.M.Y. Design, Synthesis, and Anti-Breast Cancer Activity of Some Hybrid Molecules Containing Coumarin Moiety. Russ. J. Bioorg. Chem. 2021, 47, 149–157. [Google Scholar] [CrossRef]
- Radwan, E.M.; Elsayed, E.H.; El-Moniem, M.A.; Moustafa, A.M.Y. Synthesis and Biological Evaluation of Some New 3,4-Disubstituted Coumarin Derivatives as Anticancer Agents. Indian J. Heterocycl. Chem. 2021, 31, 101–111. [Google Scholar]
- Zaki, I.; Elsayed, E.H.; Radwan, E.M. Synthesis and Antiproliferative Activity of Some New Coumarin Derivatives Derived from 8-Hydroxycoumarin. Russ. J. Bioorg. Chem. 2021, 47, 514–523. [Google Scholar] [CrossRef]
- Salem, M.G.; Abu-El Maaty, D.M.; El-Deen, Y.I.M.; Elesawy, B.H.; El Askary, A.; Saleh, A.; Saied, E.M.; El Behery, M. Novel 1,3-Thiazole Analogues with Potent Activity against Breast Cancer: A Design, Synthesis, In Vitro, and In Silico Study. Molecules 2022, 27, 4898. [Google Scholar] [CrossRef] [PubMed]
- Barreca, M.; Spanò, V.; Rocca, R.; Bivacqua, R.; Abel, A.-C.; Maruca, A.; Montalbano, A.; Raimondi, M.V.; Tarantelli, C.; Gaudio, E.; et al. Development of [1,2]oxazoloisoindoles tubulin polymerization inhibitors: Further chemical modifications and potential therapeutic effects against lymphomas. Eur. J. Med. Chem. 2022, 243, 114744. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, S.; Kaku, K.; Robles, A.J.; Hamel, E.; Mooberry, S.L.; Gangjee, A. Simple monocyclic pyrimidine analogs as microtubule targeting agents binding to the colchicine site. Bioorg. Med. Chem. 2023, 82, 117217. [Google Scholar] [CrossRef] [PubMed]
- Barreca, M.; Spano, V.; Raimondi, M.V.; Tarantelli, C.; Spriano, F.; Bertoni, F.; Barraja, P.; Montalbano, A. Recurrence of the oxazole motif in tubulin colchicine site inhibitors with anti-tumor activity. Eur. J. Med. Chem. 2021, 1, 100004. [Google Scholar] [CrossRef]
- Chen, Z.-H.; Xu, R.-M.; Zheng, G.-H.; Jin, Y.-Z.; Li, Y.; Chen, X.-Y.; Tian, Y.-S. Development of Combretastatin A-4 Analogues as Potential Anticancer Agents with Improved Aqueous Solubility. Molecules 2023, 28, 1717. [Google Scholar] [CrossRef]
- Jain, S.; Chandra, V.; Jain, P.K.; Pathak, K.; Pathak, D.; Vaidya, A. Comprehensive review on current developments of quinoline-based anticancer agents. Arab. J. Chem. 2019, 12, 4920–4946. [Google Scholar] [CrossRef]
- Hettle, A.G.; Vickers, C.J.; Boraston, A.B. Sulfatases: Critical Enzymes for Algal Polysaccharide Processing. Front. Plant Sci. 2022, 13, 837636. [Google Scholar] [CrossRef]
- Lenne, P.F.; Trivedi, V. Sculpting tissues by phase transitions. Nat. Commun. 2022, 13, 664. [Google Scholar] [CrossRef]
- Huang, L.; Huang, J.; Nie, H.; Li, Y.; Song, L.; Wu, F. Design, synthesis and biological evaluation of combretastatin A-4 sulfamate derivatives as potential anti-cancer agents. RSC Med. Chem. 2021, 12, 1374–1380. [Google Scholar] [CrossRef]
- Kozak, W.; Daśko, M.; Masłyk, M.; Pieczykolan, J.S.; Gielniewski, B.; Rachon, J.; Demkowicz, S. Phosphate tricyclic coumarin analogs as steroid sulfatase inhibitors: Synthesis and biological activity. RSC Adv. 2014, 4, 44350–44358. [Google Scholar] [CrossRef]
- Brueggemeier, R.W. Aromatase inhibitors in breast cancer therapy. Expert. Rev. Anticancer Ther. 2002, 2, 181–191. [Google Scholar] [CrossRef]
- Brueggemeier, R.W.; Richards, J.A.; Joomprabutra, S.; Bhat, A.S.; Whetstone, J.L. Molecular pharmacology of aromatase and its regulation by endogenous and exogenous agents. J. Steroid Biochem. Mol. Biol. 2001, 79, 75–84. [Google Scholar] [CrossRef]
- Miller, W.R. Aromatase inhibitors in the treatment of advanced breast cancer. Cancer Treat. Rev. 1989, 16, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Banting, L.; Nicholls, P.J.; Shaw, M.A.; Smith, H.J. Recent developments in aromatase inhibition as a potential treatment for oestrogen-dependent breast cancer. Prog. Med. Chem. 1989, 26, 253–298. [Google Scholar] [PubMed]
- Park, W.C.; Jordan, V.C. Selective estrogen receptor modulators (SERMs) and their roles in breast cancer prevention. Trends Mol. Med. 2002, 8, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R. Biological rationale for endocrine therapy in breast cancer. Best Pract. Res. Clin. Endocrinol. Metab. 2004, 18, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; James, K.; Owen, C.P. Inhibition of estrone sulfatase (ES) by derivatives of 4-[(aminosulfonyl)oxy] benzoic acid. Biorg. Med. Chem. Lett. 2002, 12, 2391–2394. [Google Scholar] [CrossRef]
- Ratre, P.; Kulkarni, S.; Das, S.; Liang, C.; Mishra, P.K.; Thareja, S. Medicinal chemistry aspects and synthetic strategies of coumarin as aromatase inhibitors: An overview. Med. Oncol. 2022, 40, 41. [Google Scholar] [CrossRef]
- Brandão, M.; Aftimos, P.; Azim, H.A.; Sotiriou, C. Chapter 26-Molecular Biology of Breast Cancer, 2nd ed.; Coleman, W.B., Tsongalis, E., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 449–461. [Google Scholar]
- Li, Z.; Wei, H.; Li, S.; Wu, P.; Mao, X. The Role of Progesterone Receptors in Breast Cancer. Drug Des. Dev. Ther. 2022, 16, 305–314. [Google Scholar] [CrossRef]
- Barros-Oliveira, M.d.C.; Costa-Silva, D.R.; dos Santos, A.R.; Pereira, R.O.; Soares-Júnior, J.M.; da Silva, B.B. Influence of CYP19A1 gene expression levels in women with breast cancer: A systematic review of the literature. Clinics 2021, 76, e2846. [Google Scholar] [CrossRef]
- Testa, U.; Castelli, G.; Pelosi, E. Breast Cancer: A Molecularly Heterogenous Disease Needing Subtype-Specific Treatments. Med. Sci. 2020, 8, 18. [Google Scholar] [CrossRef]
- Blackburn, H.L.; Ellsworth, D.L.; Shriver, C.D.; Ellsworth, R.E. Role of cytochrome P450 genes in breast cancer etiology and treatment: Effects on estrogen biosynthesis, metabolism, and response to endocrine therapy. Cancer Causes Control 2015, 26, 319–332. [Google Scholar] [CrossRef] [PubMed]
- Long, J.; Kataoka, N.; Shu, X.; Wen, W.; Gao, Y.; Cai, Q.; Zheng, W. Genetic Polymorphisms of the CYP19A1 Gene and Breast Cancer Survival. Cancer Epidemiol. Biomark. Prev. 2006, 15, 2115–2122. [Google Scholar] [CrossRef] [PubMed]
- Han, J.; Talorete, T.P.N.; Yamada, P.; Isoda, H. Anti-proliferative and apoptotic effects of oleuropein and hydroxytyrosol on human breast cancer MCF-7 cells. Cytotechnology 2009, 59, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Zaki, I.; Abdelhameid, M.K.; El-Deen, I.M.; Wahab, H.A.A.; Ashmawy, A.M.; Mohamed, K.O. Design, synthesis and screening of 1, 2, 4-triazinone derivatives as potential antitumor agents with apoptosis inducing activity on MCF-7 breast cancer cell line. Eur. J. Med. Chem. 2018, 156, 563–579. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-S.; Chen, Y.-J.; Chen, J.J.; Shieh, J.-J.; Huang, C.-H.; Lin, P.-S.; Chang, G.-C.; Chang, J.-T.; Lin, C.-C. Terpinen-4-ol induces apoptosis in human nonsmall cell lung cancer in vitro and in vivo. Evid. Based Complement. Altern. Med. 2012, 2012, 121–134. [Google Scholar]
- Mourad, A.A.E.; Rizzk, Y.W.; Zaki, I.; Mohammed, F.Z.; El Behery, M. Synthesis and cytotoxicity screening of some synthesized hybrid nitrogen molecules as anticancer agents. J. Mol. Struct. 2021, 1242, 130722. [Google Scholar] [CrossRef]
- AboulWafa, O.M.; Daabees, H.M.G.; Badawi, W.A. 2-Anilinopyrimidine derivatives: Design, synthesis, in vitro anti-proliferative activity, EGFR and ARO inhibitory activity, cell cycle analysis and molecular docking study. Bioorg. Chem. 2020, 99, 103798. [Google Scholar] [CrossRef]
- Matias, P.M.; Donner, P.; Coelho, R.; Thomaz, M.; Peixoto, C.; Macedo, S.; Otto, N.; Joschko, S.; Scholz, P.; Wegg, A.; et al. Structural evidence for ligand specificity in the binding domain of the human androgen receptor: Implications for pathogenic gene mutations. J. Biol. Chem. 2000, 275, 26164–26171. [Google Scholar] [CrossRef]
- Ghosh, D.; Egbuta, C.; Lo, J. Testosterone complex and non-steroidal ligands of human aromatase. J. Steroid Biochem. Mol. Biol. 2018, 181, 11–19. [Google Scholar] [CrossRef]
- Thomsen, R.; Christensen, M.H. MolDock: A new technique for high-accuracy molecular docking. J. Med. Chem. 2006, 49, 3315–3321. [Google Scholar] [CrossRef] [PubMed]

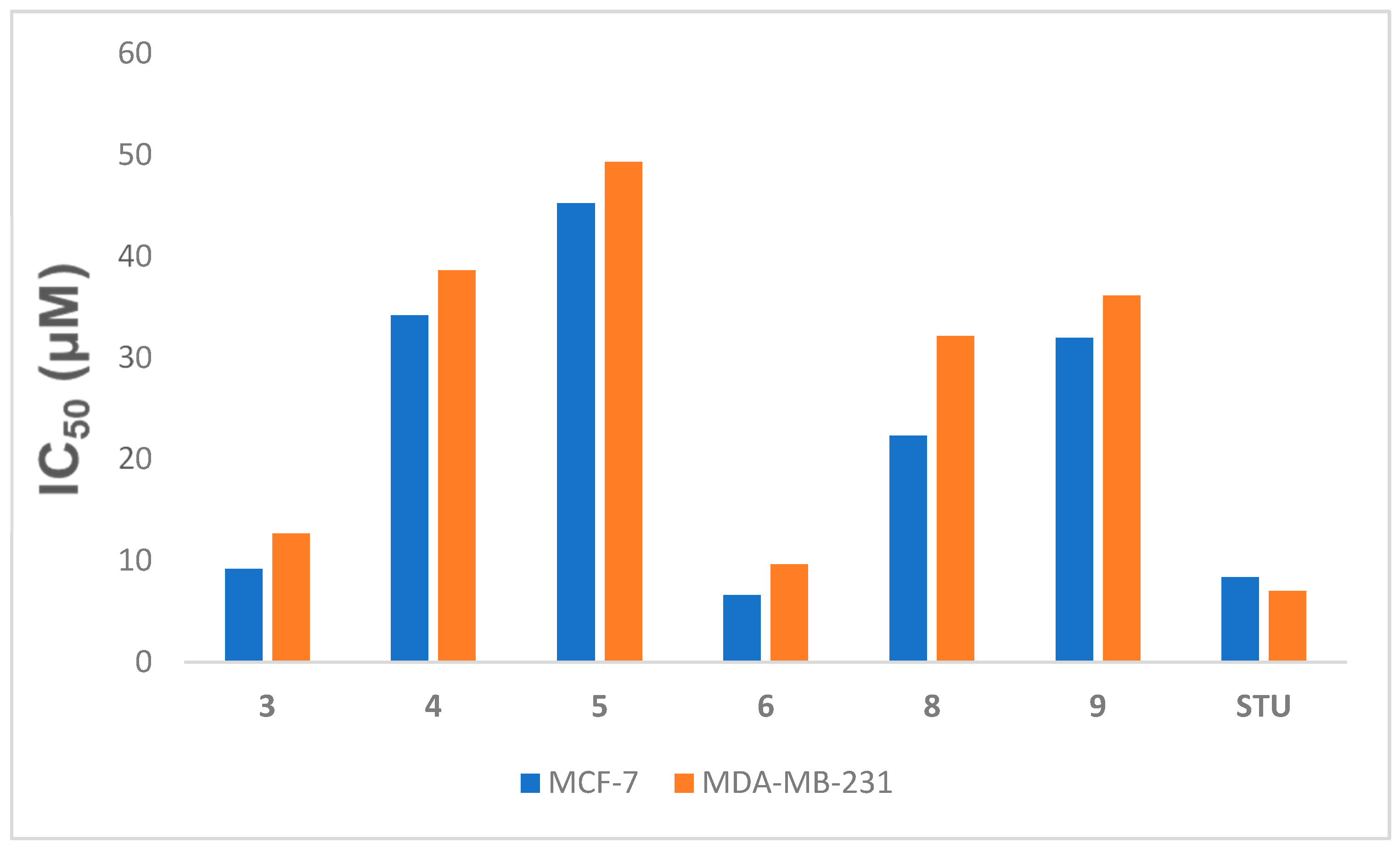

| Comp No. | IC50 Values (µM) | ||
|---|---|---|---|
| MCF-7 | MDA-MB-231 | MCF-10A | |
| 3 | 9.165 ± 0.36 | 12.65 ± 1.32 | NT |
| 4 | 34.19 ± 1.35 | 38.61 ± 2.93 | NT |
| 5 | 45.23 ± 1.79 | 49.32 ± 2.93 | NT |
| 6 | 6.621 ± 0.26 | 9.62 ± 1.46 | 35.83 ± 1.93 |
| 8 | 22.300 ± 1.27 | 32.15 ± 2.13 | NT |
| 9 | 31.98 ± 0.88 | 36.16 ± 2.41 | NT |
| STU | 4.086 ± 0.16 | 7.03 ± 0.19 | 26.72 ± 1.26 |
| Receptors (PDB) | S (kcal/mol) | Distance (A) | Hydrophilic Interactions | Hydrophobic Interactions | |
|---|---|---|---|---|---|
| Compound 6 | 1E3K | −7.63 | 1.87 | Leu715 Cys891 Met759 | Val903, Phe905, Leu887, Met801, Phe778, Leu763, Val 760, Leu721, Met756, Leu718, Met909 |
| 5JKV | −7 | 1.73 | Met374 | Leu477, Leu372, Val373, Phe134, Phe430, Val370, Ile133, Trp224 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Warhi, T.; Abu Ali, O.A.; Alqahtani, L.S.; Abo-Elabass, E.; El Behery, M.; El-Baky, A.E.A.; Samir A. Zaki, M.; Fayad, E.; Radwan, E.M. Novel 3-Substituted 8-Methoxycoumarin Derivatives as Anti-Breast Cancer Drugs. Crystals 2023, 13, 1037. https://doi.org/10.3390/cryst13071037
Al-Warhi T, Abu Ali OA, Alqahtani LS, Abo-Elabass E, El Behery M, El-Baky AEA, Samir A. Zaki M, Fayad E, Radwan EM. Novel 3-Substituted 8-Methoxycoumarin Derivatives as Anti-Breast Cancer Drugs. Crystals. 2023; 13(7):1037. https://doi.org/10.3390/cryst13071037
Chicago/Turabian StyleAl-Warhi, Tarfah, Ola A. Abu Ali, Leena S. Alqahtani, Eman Abo-Elabass, Mohammed El Behery, Atef E. Abd El-Baky, Mohamed Samir A. Zaki, Eman Fayad, and Eman M. Radwan. 2023. "Novel 3-Substituted 8-Methoxycoumarin Derivatives as Anti-Breast Cancer Drugs" Crystals 13, no. 7: 1037. https://doi.org/10.3390/cryst13071037
APA StyleAl-Warhi, T., Abu Ali, O. A., Alqahtani, L. S., Abo-Elabass, E., El Behery, M., El-Baky, A. E. A., Samir A. Zaki, M., Fayad, E., & Radwan, E. M. (2023). Novel 3-Substituted 8-Methoxycoumarin Derivatives as Anti-Breast Cancer Drugs. Crystals, 13(7), 1037. https://doi.org/10.3390/cryst13071037







