Gastric Cancer: Current Status of Diagnosis and Treatment
Abstract
:1. Introduction
2. Diagnosis
2.1. Upper Gastrointestinal Endoscopy
2.2. 18F-Fluorodeoxyglucose (FDG)-Positron Emission Tomography (PET)
2.3. Staging Laparoscopy (SL)
3. Treatment
3.1. Endoscopic Resection
3.2. Laparoscopic Surgery
| Reference | Eligibility | n | Endpoints |
|---|---|---|---|
| Kitano, et al. (2002) [28] | T1 | 28 | Operative findings, postoperative course and pulmonary function |
| Huscher, et al. (2005) [29] | TanyNanyM0 | 59 | Operative findings, postoperative course, pathologic findings and overall survival |
| Lee, et al. (2005) [30] | T1 | 47 | Operative findings, postoperative course, pathologic findings |
| Hayashi, et al. (2005) [31] | T1 | 28 | Operative findings, postoperative course and enzyme immunoassays |
| Kim, et al. (2008) [32] | T1 | 164 | Operative findings, postoperative course and QOL questionnaires |
3.3. Lymphadenectomy
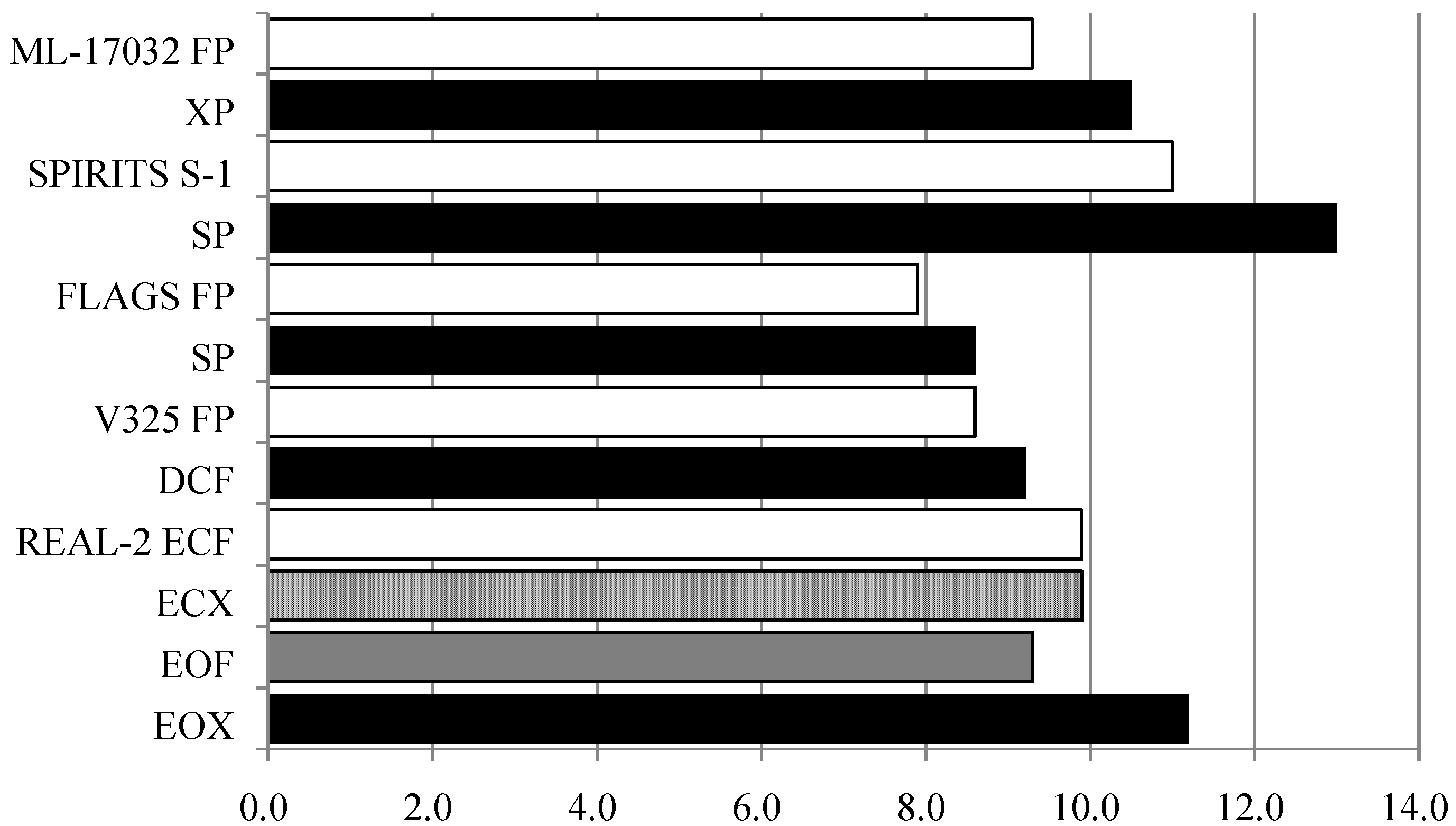
3.4. Chemotherapy
3.5. Adjuvant Therapy
3.6. Radiation Therapy
3.7. Molecular Targeted Agents
| Study | Line | Molecular targeted agent | Control arm | Primary endpoint |
|---|---|---|---|---|
| LOGiC | 1st | Lapatinib | Capecitabine/Oxaliplatin | Overall survival |
| TYTAN | 2nd | Lapatinib | Paclitaxel | Overall survival |
| RAINBOW | 2nd | Ramuciruab | Paclitaxel | Overall survival |
| GRANITE-1 | 2nd/3rd | Everolimus | Placebo | Overall survival |
| GRANITE-2 | 2nd | Everolimus | Paclitaxel | Overall survival |
4. Conclusions
Conflict of Interest
Reference
- Ferlay, J.; Shin, H.R.; Bray, F.; Forman, D.; Mathers, C.; Parkin, D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int. J. Cancer 2010, 127, 2893–2917. [Google Scholar]
- Ezoe, Y.; Muto, M.; Uedo, N.; Doyama, H.; Yao, K.; Oda, I.; Kaneko, K.; Kawahara, Y.; Yokoi, C.; Sugiura, Y.; et al. Magnifying narrowband imaging is more accurate than conventional white-lite imaging in diagnosis of gastric mucosal cancer. Gastroenterology 2011, 141, 2017–2025. [Google Scholar]
- Nagahama, T.; Yao, K.; Maki, S.; Yasaka, M.; Takaki, Y.; Matsui, T.; Tanabe, H.; Iwashita, A.; Ota, A. Usefulness of magnifying endoscopy with narrow-band imaging for determining the horizontal extent of early gastric cancer when there is an unclear margin by chrmoendoscopy (with video). Gastrointest. Endosc. 2011, 74, 1259–1267. [Google Scholar] [CrossRef]
- Inoue, H.; Sasajima, K.; Kaga, M.; Sugaya, S.; Sato, Y.; Wada, Y.; Inui, M.; Satodate, H.; Kudo, S.E.; Kimura, S.; et al. Endoscopic in vivo evaluation of tissue atypia in the esophagus using a newly designed integrated endocytoscope: A pilot trial. Endoscopy 2006, 38, 891–895. [Google Scholar] [CrossRef]
- Kumagai, Y.; Kawada, K.; Yamazaki, S.; Iida, M.; Momma, K.; Odajima, H.; Kawachi, H.; Nemoto, T.; Kawano, T.; Takubo, K. Endocytoscopic observation for esophageal squamous cell carcinoma: Can biopsy histology be omitted? Dis. Esophagus 2009, 22, 505–512. [Google Scholar] [CrossRef]
- Inamoto, K.; Kouzai, K.; Ueeda, T.; Marukawa, T. CT virtual endoscopy of the stomach: Comparison study with gastric fiberscopy. Abdom. Imaging 2005, 30, 473–479. [Google Scholar] [CrossRef]
- Kole, A.C.; Plukker, J.T.; Nieweg, O.E.; Vaalburg, W. Positron emission tomography for staging of oesophageal and gastroesophageal malignancy. Br. J. Cancer 1998, 78, 521–527. [Google Scholar] [CrossRef]
- McAteer, D.; Wallis, F.; Couper, G.; Norton, M.; Welch, A.; Bruce, D.; Park, K.; Nicolson, M.; Gilbert, F.J.; Sharp, P. Evaluation of 18F-FDG positron emission tomography in gastric and oesophageal carcinoma. Br. J. Radiol. 1999, 72, 525–529. [Google Scholar]
- Yoshikawa, K.; Kitaoka, H. Bone metastasis of gastric cancer. Jpn. J. Surg. 1983, 13, 173–176. [Google Scholar] [CrossRef]
- Smyth, E.; Scölder, H.; Strong, V.E.; Capanu, M.; Kelsen, D.P.; Coit, D.G.; Shah, M.A. A prospective evaluation of the utility of 2-deoxy-2-[(18) F] fluoro-D-glucose positron emission tomography and computed tomography in staging locally advanced gastric cancer. Cancer 2012, 118, 5481–5488. [Google Scholar] [CrossRef]
- Suittie, S.A.; Welch, A.E.; Park, K.G. Positron emission tomography for monitoring response to neoadjuvant therapy in patients with oesophageal and gastro-oesophageal junction carcinoma. Eur. J. Surg. Oncol. 2009, 35, 1019–1029. [Google Scholar] [CrossRef]
- Burke, E.C.; Karpeh, M.S.; Conlon, K.C.; Brennan, M.F. Laparoscopy in the management of gastric adenocarcinoma. Ann. Surg. 1997, 225, 262–267. [Google Scholar] [CrossRef]
- Lowy, A.M.; Mansfield, P.F.; Leach, S.D.; Ajani, J. Laparoscopic staging for gastric cancer. Surgery 1996, 119, 611–614. [Google Scholar] [CrossRef]
- Edge, S.B.; Byrd, D.R.; Compton, C.C.; Fritz, A.G.; Greene, F.L.; Trotti, A. AJCC Cancer Staging Manual, 7th ed; Springer-Verlag: New York, NY, USA, 2009; pp. 117–126. [Google Scholar]
- Bentrem, D.; Wilton, A.; Mazumdar, M.; Brennan, M.; Coit, D. The value of peritoneal cytology as a preoperative predictor in patients with gastric carcinoma undergoing a curative resection. Ann. Surg. Oncol. 2005, 12, 347–353. [Google Scholar] [CrossRef]
- Kodera, Y.; Yamamura, Y.; Shimizu, Y.; Torii, A.; Hirai, T.; Yasui, K.; Morimoto, T.; Kato, T. Peritoneal washing cytology: Prognostic value of positive findings in patients with gastric carcinoma undergoing a potentially curative resection. J. Surg. Oncol. 1999, 72, 60–65. [Google Scholar] [CrossRef]
- Ono, H.; Kondo, H.; Gotoda, T.; Shirao, K.; Yamaguchi, H.; Saito, D.; Hosokawa, K.; Shimoda, T.; Yoshida, S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut 2001, 48, 225–229. [Google Scholar] [CrossRef]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011, 14, 113–123. [CrossRef]
- Ono, H. Endoscopic submucosal dissection for early gastric cancer. Chin. J. Dig. Dis. 2005, 6, 119–121. [Google Scholar] [CrossRef]
- Kodashima, S.; Fujishiro, M.; Yahagi, N.; Kakushima, N.; Ichinose, M.; Omata, M. Endoscopic submucosal dissection for gastric neoplasia: Experience with the flex-knife. Acta Gastroenterol. Belg. 2006, 69, 224–229. [Google Scholar]
- Phillips, E.; Daykhovsky, L.; Carroll, B.; Gershman, A.; Grundfest, W.S. Laparoscopic cholecystectomy: Instrumentation and technique. J. Laparoendosc. Surg. 1990, 1, 3–15. [Google Scholar] [CrossRef]
- Jacobs, M.; Verdeja, J.C.; Goldstein, H.S. Minimally invasive colon resection (laparoscopic colectomy). Surg. Laparosc. Endosc. 1991, 1, 144–150. [Google Scholar]
- Hüscher, C.G.; Lirici, M.M.; Chiodini, S. Laparoscopic liver resections. Semin. Laparosc. Surg. 1998, 5, 204–210. [Google Scholar]
- Kitano, S.; Iso, Y.; Moriyama, M.; Sugimachi, K. Laparoscopy-assisted Billroth-I gasrtrectomy. Surg. Laparosc. Endosc. 1994, 4, 146–148. [Google Scholar]
- Kanaya, S.; Haruta, S.; Kawamura, Y.; Yoshimura, F.; Inaba, K.; Hiramatsu, Y.; Ishida, Y.; Taniguchi, K.; Isogaki, J.; Uyama, I. Video: Laparosopy distinctive technique for suprapancreatic lymph node dissection: Medial approach for laparoscopic gastric cancer surgery. Surg. Endosc. 2011, 25, 3928–3929. [Google Scholar] [CrossRef]
- Ikeda, O.; Sakaguchi, Y.; Aoki, Y.; Harimoto, N.; Taomoto, J.; Masuda, T.; Ohga, T.; Adachi, E.; Toh, Y.; Okamura, T.; et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg. Endosc. 2009, 23, 2374–2379. [Google Scholar] [CrossRef]
- Hirahara, N.; Tanaka, T.; Yano, S.; Yamanoi, A.; Minari, Y.; Kawabata, Y.; Ueda, S.; Hira, E.; Yamamoto, T.; Nishi, T.; et al. Reconstruction of the gastrointestinal tract by hemi-double stapling method for the esophagus and jejunum using EEA OrVill in laparoscopic total gasrtectomy and proximal gastrectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2011, 21, e11–e15. [Google Scholar] [CrossRef]
- Kitano, S.; Shiraishi, N.; Uyama, I.; Sugihara, K.; Tanigawa, N. Japanese Laparoscopic Surgery Study Group. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann. Surg. 2007, 245, 68–72. [Google Scholar] [CrossRef]
- Kitano, S.; Shiraishi, N.; Fujii, K.; Yasuda, K.; Inomata, M.; Adachi, Y. A randomized controlled trial comparing open vs. laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: An interim report. Surgery 2002, 131, S306–S311. [Google Scholar] [CrossRef]
- Huscher, C.G.; Mingoli, A.; Sgarzini, G.; Sansonetti, A.; di Paola, M.; Recher, A.; Ponzano, C. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: Five-year results of a randomized prospective trial. Ann. Surg. 2005, 241, 232–237. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, H.S.; Lee, J.H. A prospective randomized study comparing open vs. laparoscopy-assisted distal gastrectiomy in early gastric cancer: Early result. Surg. Endosc. 2005, 19, 168–173. [Google Scholar] [CrossRef]
- Hayashi, H.; Ochiai, T.; Shimada, H.; Gunji, Y. Prospective randomized study of open versus laparoscopy-assisted distal gastrectiomy with extrperigastric lymph node dissection for early gastric cancer. Surg. Endosc. 2005, 19, 1172–1176. [Google Scholar] [CrossRef]
- Kim, Y.W.; Baik, Y.H.; Yun, Y.H.; Nam, B.H.; Kim, D.H.; Choi, I.J.; Bae, J.M. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: Results of a prospective randomized clinical trial. Ann. Surg. 2008, 248, 721–727. [Google Scholar] [CrossRef]
- Katai, H.; Sasako, M.; Fukuda, H.; Nakamura, K.; Hiki, N.; Saka, M.; Yamaue, H.; Yoshikawa, T.; Kojima, K. JCOG Gastric Cancer Surgical Study Group. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: A multicenter phase II trial (JCOG0703). Gastric Cancer 2010, 13, 238–244. [Google Scholar] [CrossRef]
- Kim, H.H.; Hyung, W.J.; Cho, G.S.; Kim, M.C.; Han, S.U.; Kim, W.; Ryu, S.W.; Lee, H.J.; Song, K.Y. Morbidity and motality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: An interim report-a phase III multicenter, prospective, randomized trial (KLASS Trial). Ann. Surg. 2010, 251, 417–420. [Google Scholar] [CrossRef]
- Pietrabissa, A.; Sbrana, F.; Morelli, L.; Badessi, F.; Pugliese, L.; Vinci, A.; Klersy, C.; Spinoglio, G. Overcoming the challenges of single-incision cholecystectomy with robotic single-site technology. Arch. Surg. 2012, 147, 709–714. [Google Scholar] [CrossRef]
- Woo, R.; Le, D.; Krummel, T.M.; Albanese, C. Robot-assisted pediatric surgery. Am. J. Surg. 2004, 188, 27S–37S. [Google Scholar]
- Lowery, W.J.; Leath, C.A., 3rd; Robinson, R.D. Robotic surgery applications in tne management of gynecologic malignancies. J. Surg. Oncol. 2012, 105, 481–487. [Google Scholar] [CrossRef]
- Nix, J.; Smith, A.; Kurpad, R.; Nielsen, M.E.; Wallen, E.M.; Pruthi, R.S. Prospective randomized controlled trial of robotic versus open radical cystectomy of bladder cancer: Perioperative and pathologic results. Eur. Urol. 2010, 57, 196–201. [Google Scholar] [CrossRef]
- Cuschieri, A.; Weeden, S.; Fielding, J.; Bancewicz, J.; Craven, J.; Joypaul, V.; Sydes, M.; Fayers, P. Patient survival after D1 and D2 resection for gastric cancer: Long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br. J. Cancer 1999, 79, 1522–1530. [Google Scholar] [CrossRef]
- Hartgrink, H.H.; van de Velde, C.J.; Putter, H.; Bonenkamp, J.J.; Klein Kranenbarg, E.; Songun, I.; Welvaart, K.; van Krieken, J.H.; Meijer, S.; Plukker, J.T.; et al. Extended lymph node dissection for gastric cancer: Who may benefit? Final results of the randomized Dutch Gastric Cancer Group Trial. J. Clin. Oncol. 2004, 22, 2069–2077. [Google Scholar]
- Sano, T.; Sasako, M.; Yamamoto, S.; Nashimoto, A.; Kurita, A.; Hiratsuka, M.; Tsujinaka, T.; Kinoshita, T.; Arai, K.; Yamamura, Y.; et al. Gastric cancer surgery: Morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy—Japan Clinical Oncology Study Group Study 9501. J. Clin. Oncol. 2004, 22, 2767–2773. [Google Scholar] [CrossRef]
- Sasako, M.; Sano, T.; Yamamoto, S.; Kurokawa, Y.; Nashimoto, A.; Kurita, A.; Hiratsuka, M.; Tsujinaka, T.; Kinoshita, T.; Arai, K.; et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N. Engl. J. Med. 2008, 359, 453–462. [Google Scholar] [CrossRef]
- Kang, Y.K.; Kang, W.K.; Shin, D.B.; Chen, J.; Xiong, J.; Wang, J.; Lichinitser, M.; Guan, Z.; Khasanov, R.; Zheng, L.; et al. Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: A randomised phase III noninferiority trial. Ann. Oncol. 2009, 20, 663–673. [Google Scholar]
- Ajani, J.A.; Rodriguez, W.; Bodoky, G.; Moiseyenko, V.; Lichinitser, M.; Gorbunova, V.; Vynnychenko, I.; Garin, A.; Lang, I.; Falcon, S. Multicenter phase III comparison of cisplatin/S-1 with cisplatin/infusional fluorouracil in advanced gastric or gastroesophageal adenocarcinoma study: The FLAGS trial. J. Clin. Oncol. 2010, 28, 1547–1553. [Google Scholar]
- Van Cutsem, E.; Moiseyenko, V.M.; Tjulandin, S.; Majlis, A.; Constenla, M.; Boni, C.; Rodrigues, A.; Fodor, M.; Chao, Y.; Voznyi, E.; et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line chemotherapy for advanced gastric cancer: A report of the V325 study group. J. Clin. Oncol. 2006, 24, 4991–4997. [Google Scholar]
- Koizumi, W.; Narahara, H.; Hara, T.; Takagane, A.; Akiya, T.; Takagi, M.; Miyashita, K.; Nishizaki, T.; Kobayashi, O.; Takiyama, W.; et al. S-1 plus cisplatin versus S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): A phase III trial. Lancet Oncol. 2008, 9, 215–221. [Google Scholar] [CrossRef]
- Cunningham, D.; Starling, N.; Rao, S.; Iveson, T.; Nicolson, M.; Coxon, F.; Middleton, G.; Daniel, F.; Oates, J.; Norman, A.R.; et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N. Engl. J. Med. 2008, 358, 36–46. [Google Scholar] [CrossRef]
- Macdonald, J.S.; Smalley, S.R.; Benedetti, J.; Hundahl, S.A.; Estes, N.C.; Stemmermann, G.N.; Haller, D.G.; Ajani, J.A.; Gunderson, L.L.; Jessup, J.M.; et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N. Engl. J. Med. 2001, 345, 725–730. [Google Scholar]
- Lee, J.; Lim, D.H.; Kim, S.; Park, S.H.; Park, J.O.; Park, Y.S.; Lim, H.Y.; Choi, M.G.; Sohn, T.S.; Noh, J.H.; et al. Phase III trial comparing capecitabine plus cisplatin vesus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: The ARTIST trial. J. Clin. Oncol. 2012, 30, 268–273. [Google Scholar]
- Cunningham, D.; Allum, W.H.; Stenning, S.P.; Thompson, J.N.; van de Velde, C.J.; Nicolson, M.; Scarffe, J.H.; Lofts, F.J.; Falk, S.J.; Iveson, T.J.; et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N. Engl. J. Med. 2006, 355, 11–20. [Google Scholar] [CrossRef]
- Dikken, J.L.; van Sandick, J.W.; Mauritis Swellengrebel, H.A.; Lind, P.A.; Putter, H.; Jansen, E.P.; Boot, H.; van Grieken, N.C.; van de Velde, C.J.; Verheij, M.; et al. Neo-adjuvant chemotherapy followed by surgery and chemotherapy or by surgery and chemoradiotherapy for patients with resectable gastric cancer (CRITICS). BMC Cancer 2011, 11, 329. [Google Scholar] [CrossRef]
- Sasako, M.; Sakuramoto, S.; Katai, H.; Kinoshita, T.; Furukawa, H.; Yamaguchi, T.; Nashimoto, A.; Fujii, M.; Nakajima, T.; Ohashi, Y. Five-year outcomes of randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J. Clin. Oncol. 2011, 29, 4387–4393. [Google Scholar] [CrossRef]
- Bang, Y.J.; Kim, Y.W.; Yang, H.K.; Chung, H.C.; Park, Y.K.; Lee, K.H.; Lee, K.W.; Kim, Y.H.; Noh, S.I.; Cho, J.Y.; et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): A phase 3 open-label, randomized controlled trial. Lancet 2012, 379, 315–321. [Google Scholar]
- Childs, D.S., Jr.; Moetrel, C.G.; Holbrook, M.A.; Reitemeier, R.J.; Colby, M., Jr. Treatment of unresectable adenocarcinomas of the stomach with a combination of 5-fluorouracil and radiation. Am. J. Roentgenol. Ther. Nucl. Med. 1968, 102, 541–544. [Google Scholar]
- Falkson, G.; Falkson, H.C. Fluorouracil and radiotherapy in gastrointestinal cancer. Lancet 1969, 2, 1252–1253. [Google Scholar]
- Klaassen, D.J.; Maclntyre, J.M.; Catton, G.E.; Engstrom, P.F.; Moertel, C.G. Treatment of locally unresectable cancer of the stomach and pancreas: A randomized comparison of 5-fluorouracil alone with radiation plus concurrent and maintenance 5-fluorouracil—An Eastern Cooperative Oncology Group Study. J. Clin. Oncol. 1985, 3, 373–378. [Google Scholar]
- Saikawa, Y.; Kubota, T.; Kumagai, K.; Nakamura, R.; Kumai, K.; Shigematsu, N.; Kubo, A.; Kitajima, M.; Kitagawa, Y. Phase II study of chemoradiotherapy with S-1 and low-dose cisplatin for inoperable advanced gastric cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 71, 173–179. [Google Scholar]
- Yoshikawa, T.; Tsuburaya, A.; Hirabayashi, N.; Yoshida, K.; Nagata, N.; Kodera, Y.; Takahashi, N.; Oba, K.; Kimura, M.; Ishikura, S.; et al. A phase I study of palliative chemoradiation therapy with paclitaxel and cisplatin for local symptoms due to an unresectable primary advanced or locally recurrent gastric adenocarcinoma. Cancer Chemother. Pharmacol. 2009, 64, 1071–1077. [Google Scholar] [CrossRef]
- Hashimoto, K.; Mayahara, H.; Takashima, A.; Nakajima, T.E.; Kato, K.; Hamaguchi, T.; Ito, Y.; Yamada, Y.; Kagami, Y.; Itami, J.; et al. Palliative radiation therapy for hemorrhage of unresectable gastric cancer: A single institute experience. J. Cancer Res. Clin. Oncol. 2009, 135, 1117–1123. [Google Scholar] [CrossRef]
- Dawood, S.; Broglio, K.; Buzdar, A.U.; Hortobagyi, G.N.; Giordano, S.H. Prognosis of women with metaplastic breast cancer by HER2 status and trastuzumab treatment: An institutional-based review. J. Clin. Oncol. 2010, 28, 92–98. [Google Scholar] [CrossRef]
- Terashima, M.; Kitada, K.; Ochiai, A.; Ichikawa, W.; Kurahashi, I.; Sakuramoto, S.; Katai, H.; Sano, T.; Imamura, H.; Sasako, M.; et al. Impact of expression of human epidermal growth factor receptors EGFR and ERBB2 on survival in Stage II/III gastric cancer. Clin. Cancer Res. 2012, 18, 5992–6000. [Google Scholar]
- Janjigian, Y.Y.; Werner, D.; Pauligk, C.; Steinmetz, K.; Kelsen, D.P.; Jäger, E.; Altmannsberger, H.M.; Robinson, E.; Tafe, L.J.; Tang, L.H.; et al. Prognosis of metastatic gastric and gastroesophageal junction cancer by HER2 status: A European and USA international collaborative analysis. Ann. Oncol. 2012, 23, 2656–2662. [Google Scholar]
- Bang, Y.J.; van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open label, randomised controlled trial. Lancet 2010, 376, 687–697. [Google Scholar]
- Ohtsu, A.; Shah, M.A.; van Cutsem, E.; Rha, S.Y.; Sawaki, A.; Park, S.R.; Lim, H.Y.; Yamada, Y.; Wu, J.; Langer, B.; et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: A randomized, double-blind, placebo-controlled phase III study. J. Clin. Oncol. 2011, 29, 3968–3976. [Google Scholar]
- Chau, I.; Okines, A.F.; Castro, D.G.; Saffery, Y.; Barbachano, A.; Wotherspoon, L.; Puckey, S.; Hulkki Wilson, F.Y.; Coxon, G.W.; Middleton, D.R.; et al. REAL3: A multicenter randomized phase II/III trial of epirubicin, oxaliplatin, and capecitabine (EOC) versus modified (m) EOC plus panitumumab (P) in advanced oesophagogastric (OG) cancer—Response rate (RR), toxicity, and molecular analysis from phase II. J. Clin. Oncol. 2011, 29, Abstract 4131. [Google Scholar]
- Lordick, F.; Bodoky, G.; Chung, H.; Kurteva, G.; Kang, Y.; Oh, S.C.; Salman, P.; Goette, H.; Melezinkova, H.; Moehler, M. Cetuximab in combination with capecitabine and cisplatin as first-line treatment in advanced gastric cancer: Randomized controlled phase III EXPAND study. Ann. Oncol. 2012, 23, BA3. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Takahashi, T.; Saikawa, Y.; Kitagawa, Y. Gastric Cancer: Current Status of Diagnosis and Treatment. Cancers 2013, 5, 48-63. https://doi.org/10.3390/cancers5010048
Takahashi T, Saikawa Y, Kitagawa Y. Gastric Cancer: Current Status of Diagnosis and Treatment. Cancers. 2013; 5(1):48-63. https://doi.org/10.3390/cancers5010048
Chicago/Turabian StyleTakahashi, Tsunehiro, Yoshiro Saikawa, and Yuko Kitagawa. 2013. "Gastric Cancer: Current Status of Diagnosis and Treatment" Cancers 5, no. 1: 48-63. https://doi.org/10.3390/cancers5010048
APA StyleTakahashi, T., Saikawa, Y., & Kitagawa, Y. (2013). Gastric Cancer: Current Status of Diagnosis and Treatment. Cancers, 5(1), 48-63. https://doi.org/10.3390/cancers5010048




