A Bird’s Eye View: A Close Look into Avian CAM Models for Translational Blood Cancer Research
Simple Summary
Abstract
1. Introduction
| Cancer Type | Main Cell Type Affected | Symptoms | Diagnostic Methods | Median Age at Diagnosis | Common Treatment Regime | 5-Year Survival Rate | |
|---|---|---|---|---|---|---|---|
| Leukaemia | Acute Lymphocytic Leukaemia (ALL) | Immature B lymphocytes (lymphoblasts) | Fatigue, frequent infection, bruising, bone pain, swollen lymph nodes | Blood tests (CBC), BM biopsy, cytogenetic analysis | Younger patients, (17 years) [21] | Antimetabolites/Chemotherapy, Steroids, Asparaginase-Specific Enzyme Therapies, Targeted therapy (CAR-T, Bispecifics), Anthracyclines, SCT | ~90% (children), ~60% young adolescent, ~20–40% (adults) [21] |
| Chronic Lymphocytic Leukaemia (CLL) | Mature B lymphocytes | Fatigue, swollen lymph nodes, night sweats, weight loss, frequent infections | Blood tests (lymphocytosis), BM biopsy, biomarker testing | Older adults (~70 years) [22] | Targeted therapy (Bruton Tyrosine/Phosphatidylinositol 3- Kinase/B-cell lymphoma 2- Inhibitors). Monoclonal Abs, Chemo(immuno-)therapy | ~90% [23], (advanced/cytogenetic dependent reduced survival) [22,24] | |
| Acute Myeloid Leukaemia (AML) | Myeloid precursors (myeloblasts) | Fatigue, fever, infections, anaemia, easy bruising, bleeding | Blood tests, BM biopsy, cytogenetic/biomarker analysis | Older adults (~69 years) [25] | Induction chemo (cytarabine + anthracycline) (7 + 3 regimen), targeted therapies (e.g., FLT3 inhibitors), SCT | ~33% [25] | |
| Chronic Myeloid Leukaemia (CML) | Myeloid cells (granulocytes) | Fatigue, weakness, bone pain, enlarged spleen, unexplained weight-loss | Blood tests, BM biopsy, cytogenetic/biomarker analysis | Older patients (~66 years) [26] | Targeted therapy (tyrosine kinase inhibitors), Immunotherapies, ASCT | ~71% [26] | |
| Lymphoma | Hodgkin’s Lymphoma | Mature B lymphocytes (Reed-Sternberg cells present) | Rapidly enlarging lymph nodes, night sweats, fever, weight loss, persistent cough | Biopsy of affected lymph node, PET/CT scan, biomarker analysis | Younger adults (~39 years) [27] | Chemotherapy, radiation, immunotherapy, SCT | ~90% [27] |
| Non-Hodgkin’s Lymphoma | Mature B lymphocytes (Reed-Sternberg cells absent) | Painless swollen lymph nodes, fatigue, fever, night sweats, cough, abdominal pain | Lymph node biopsy, biomarker analysis, imaging | Middle-aged to older adults (~68 years) [28] | Chemoimmunotherapy (e.g., R-CHOP), radiation, SCT | ~74% [28] | |
| Myeloma | Multiple Myeloma (Plasma Cell Myeloma) | Plasma cells | Bone pain, fractures, fatigue, anaemia, kidney dysfunction (CRAB symptoms) | Blood tests (M-protein, free light chain), BM biopsy, skeletal survey | Older adults (median ~70 years) [29] | Proteasome inhibitors, immunomodulators, Steroids, monoclonal Ab therapy, ASCT | ~62% [29] |
2. Laboratory Models for Research in Haematological Cancers
2.1. Mouse Models for Haematological Research
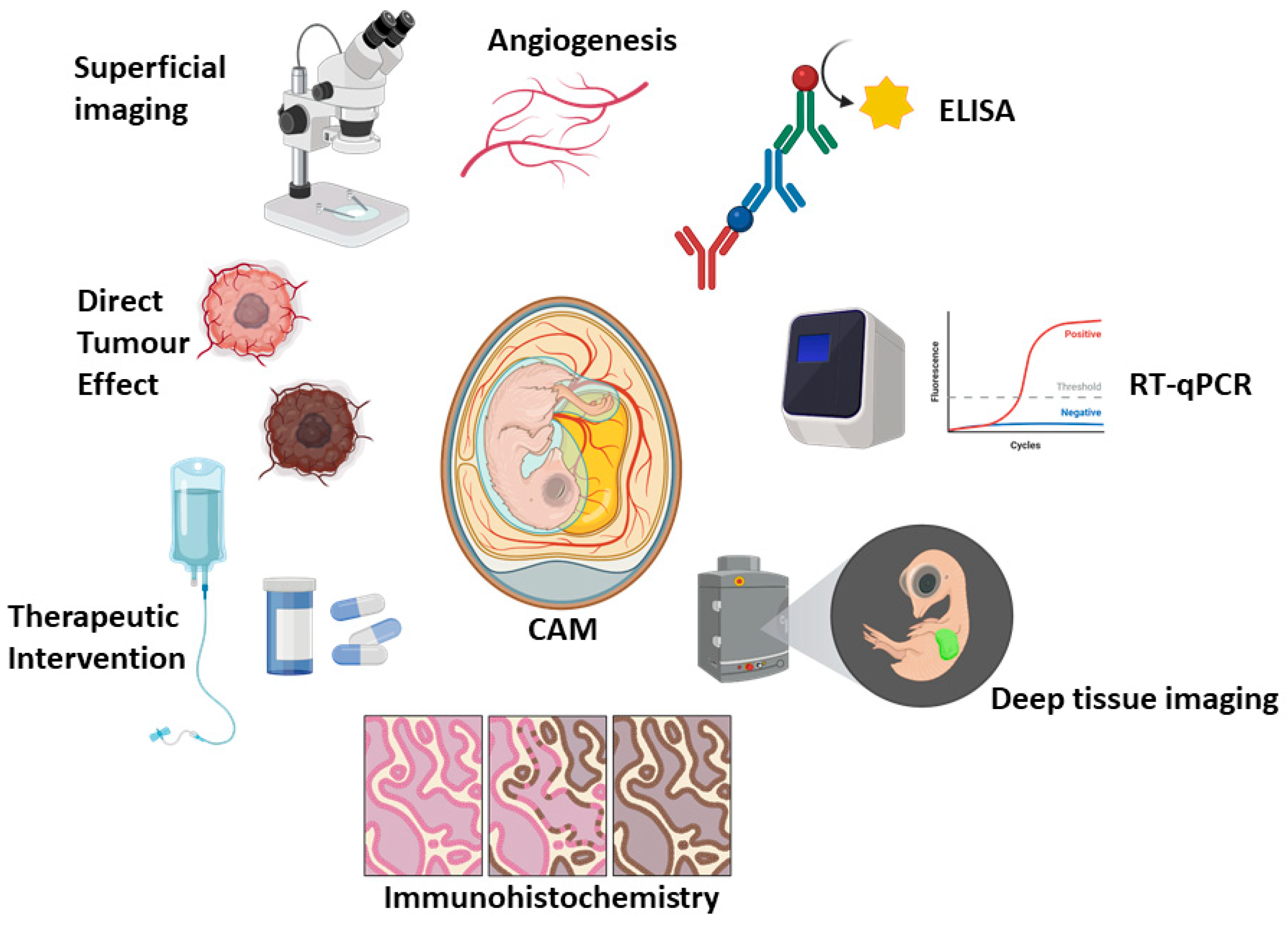
2.2. The CAM Model as a Gateway to Living Systems
2.3. Histopathological Concordance Between Murine and CAM Xenografts
2.4. Evolutionary Distance and Functional Relevance (Or Model Relevance): Avians and Humans Compared
2.5. Species-Specific Considerations in CAM Models of Haematologic Malignancy
| Chick | Turkey | Quail | Ostrich/Emu | |
|---|---|---|---|---|
| Leukaemia | ✓ [109,110,111,112] | ✓ [108] | ✗ [113] † | ✗ |
| Lymphoma | ✓ [114,115,116,117] | ✓ [108] | ✗ | ✗ |
| Myeloma | ✓ [40,118,119,120,121] | ✓ [108] | ✗ | ✗ |
3. Modelling Blood Cancers in the CAM Model
3.1. Leukaemia
3.2. Lymphoma
3.2.1. Hodgkin’s Lymphoma (HL)
3.2.2. Non-Hodgkin’s Lymphoma (NHL)
3.2.3. B-Cell Lymphoma
3.3. Multiple Myeloma
3.3.1. Modelling MM Angiogenesis on the CAM
3.3.2. MM Solid Mass Growth on CAM
3.3.3. MM Drug Testing on the CAM
3.3.4. Repurposing Drugs for MM
| Cancer Type | CAM Model | Cell Line/Patient | Cell Number | Method of Delivery | EDD Inoculation | Therapy | Study | Ref. |
|---|---|---|---|---|---|---|---|---|
| Leukaemia | Chicken | Cell Line (K562 and DAMI) | 5 × 105–5 × 106 K562 or DAMI | 1. Cells atop CAM, 2. YS inj., 3. Amn inj., 4. IV CAM inj., | 1.EDD9–11, 2. EDD3, 3. EDD3, 4. EDD11 | Chemotherapy | Intervention | [109] |
| Leukaemia/lymphoma/multiple myeloma | Turkey | K562, DAMI, Jurkat, HL-60, G2, CCRF, CAG, U266, Raji, HCL-2 and Primary material | 1–10 × 106 | IV inj | EDD11–13 | Chemotherapy | Intervention | [108] |
| Leukaemia | Chicken | MNC or CD34+ cells, Primary material | 2–5 × 104 | IV inj | EDD11 | N/A | Engraftment in organs | [110] |
| Leukaemia | Chicken | Friend erythroleukemia | CM | Soaked GS | EDD8 | N/A | Angiogenesis | [111] |
| Leukaemia | Chicken | N/A | Therapeutic | Soaked GS | EDD8 | d-Limonene | Angiogenesis | [112] |
| Lymphoma (HL) | Chicken | HL L428 cells ± CD14+ PBMCs or macrophages | 2 × 106 | Matrigel | EDD10 | N/A | Tumour growth | [114] |
| Cut. T-cell Lymphoma | Chicken | MyLa or SeAx | (1) 1 × 106 (2) 5 × 104 | IV | (1) EDD10 (2) EDD12 | Ruxolitinib and Resminostat | (1) tumour proliferation (2) Metastasis | [115] |
| Burkitt Lymphoma | Chicken | BL2B95 and BL2-GFP | 106 | Matrigel | EDD10 | N/A | Metastasis | [116] |
| Burkitt Lymphoma | Chicken | BL2B95 | 106 | Matrigel | EDD10 | Imipramine-blue | Tumour effect + lymphogenic dissemination + angiogenesis | [117] |
| Multiple Myeloma | Chicken | CM from patient material | N/A | GS | EDD8 | N/A | Angiogenesis | [119] |
| Multiple Myeloma | Chicken | Patient material | 1.8 × 104 | GS | EDD8–12 | N/A | Angiogenesis | [120] |
| Multiple Myeloma | Chicken | OPM-2eGFP or RPMI-8226eGFP | 2.5 × 105 (MM cells) + 0.5 × 105 (HMSCs) | Collagen Type I | EDD9 | Plitidepsin and bortezomib | Angiogenesis, GFP expression/quantification | [40] |
| Multiple Myeloma | Chicken | OPM-2eGFP or RPMI-8226eGFP GS: CM | 2.5 × 105 (MM cells) + 0.5 × 105 (HMECs) | Collagen Type I and GS | Collagen: EDD7, GS: EDD8 | Marine compounds | Angiogenesis, GFP expression/quantification | [118] |
| Multiple Myeloma | Chicken | OPM-2 eGFP | 3 × 105 | Collagen Type I | EDD9 | Pixatrone | GFP expression/quantification | [135] |
4. Conclusions and Considerations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosmarin, A. Leukemia, Lymphoma, and Myeloma. In Cancer; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2019; pp. 299–316. ISBN 978-1-119-64521-4. [Google Scholar]
- Fardin, F.; Akter, M. Review on Blood Cancer and Their Types. J. Mol. Pharm. Regul. Aff. 2021, 3, 18–26. [Google Scholar]
- Leukaemia Foundation. Blood Cancer Information. Available online: https://www.leukaemia.org.au/blood-cancer/ (accessed on 8 January 2025).
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer Statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Yale Medicine. Blood Cancers. Available online: https://www.yalemedicine.org/conditions/blood-cancers (accessed on 8 January 2025).
- European Cancer Information System. Estimated Incidence/Mortality. 2024. Available online: https://ecis.jrc.ec.europa.eu/data-explorer#/estimates (accessed on 8 January 2025).
- LaCasce, A.S. What Are the Most Common Blood Cancers in Adults? Available online: https://blog.dana-farber.org/insight/2019/11/what-are-the-most-common-blood-cancers-in-adults/ (accessed on 8 January 2025).
- Mattioda, C.; Voena, C.; Ciardelli, G.; Mattu, C. In Vitro 3D Models of Haematological Malignancies: Current Trends and the Road Ahead? Cells 2025, 14, 38. [Google Scholar] [CrossRef]
- Hanahan, D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022, 12, 31–46. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef]
- Haloupek, N. The Landscape of Blood Cancer Research Today—And Where the Field Is Headed. Blood Cancer Discov. 2020, 1, 1–4. [Google Scholar] [CrossRef]
- Zhou, J.; Chng, W.-J. Biological Hallmarks and Emerging Strategies to Target STAT3 Signaling in Multiple Myeloma. Cells 2022, 11, 941. [Google Scholar] [CrossRef]
- Hussain, Y.; Abdullah; Alsharif, K.F.; Aschner, M.; Theyab, A.; Khan, F.; Saso, L.; Khan, H. Therapeutic Role of Carotenoids in Blood Cancer: Mechanistic Insights and Therapeutic Potential. Nutrients 2022, 14, 1949. [Google Scholar] [CrossRef]
- Cao, H.; Wu, T.; Zhou, X.; Xie, S.; Sun, H.; Sun, Y.; Li, Y. Progress of Research on PD-1/PD-L1 in Leukemia. Front. Immunol. 2023, 14, 1265299. [Google Scholar] [CrossRef]
- Bosseboeuf, A.; Allain-Maillet, S.; Mennesson, N.; Tallet, A.; Rossi, C.; Garderet, L.; Caillot, D.; Moreau, P.; Piver, E.; Girodon, F.; et al. Pro-Inflammatory State in Monoclonal Gammopathy of Undetermined Significance and in Multiple Myeloma Is Characterized by Low Sialylation of Pathogen-Specific and Other Monoclonal Immunoglobulins. Front. Immunol. 2017, 8, 1347. [Google Scholar] [CrossRef]
- Chu, M.P.; Kriangkum, J.; Venner, C.P.; Sandhu, I.; Hewitt, J.; Belch, A.R.; Pilarski, L.M. Addressing Heterogeneity of Individual Blood Cancers: The Need for Single Cell Analysis. Cell Biol. Toxicol. 2017, 33, 83–97. [Google Scholar] [CrossRef]
- Stork, M.; Sevcikova, S.; Jelinek, T.; Minarik, J.; Radocha, J.; Pika, T.; Pospisilova, L.; Spicka, I.; Straub, J.; Pavlicek, P.; et al. Unexpected Heterogeneity of Newly Diagnosed Multiple Myeloma Patients with Plasmacytomas. Biomedicines 2022, 10, 2535. [Google Scholar] [CrossRef]
- Capelletti, M.M.; Montini, O.; Ruini, E.; Tettamanti, S.; Savino, A.M.; Sarno, J. Unlocking the Heterogeneity in Acute Leukaemia: Dissection of Clonal Architecture and Metabolic Properties for Clinical Interventions. Int. J. Mol. Sci. 2025, 26, 45. [Google Scholar] [CrossRef]
- Jacquemin, V.; Antoine, M.; Dom, G.; Detours, V.; Maenhaut, C.; Dumont, J.E. Dynamic Cancer Cell Heterogeneity: Diagnostic and Therapeutic Implications. Cancers 2022, 14, 280. [Google Scholar] [CrossRef]
- Brown, P.A.; Shah, B.; Advani, A.; Aoun, P.; Boyer, M.W.; Burke, P.W.; DeAngelo, D.J.; Dinner, S.; Fathi, A.T.; Gauthier, J.; et al. Acute Lymphoblastic Leukemia, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 1079–1109. [Google Scholar] [CrossRef]
- Wainman, L.M.; Khan, W.A.; Kaur, P. Chronic Lymphocytic Leukemia: Current Knowledge and Future Advances in Cytogenomic Testing. In Advancements in Cancer Research; Sergi, C.M., Ed.; Exon Publications: Brisbane, Australia, 2023; ISBN 978-0-6453320-9-4. [Google Scholar]
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Chronic Lymphocytic Leukemia—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/clyl.html (accessed on 5 November 2025).
- Pektaş, G.; Gönül, E.; Öncü, Ş.; Becit Kızılkaya, M.; Sadi, G.; Pektaş, M.B. Chronic Lymphocytic Leukemia: Investigation of Survival and Prognostic Factors with Drug-Related Remission. Diagnostics 2025, 15, 728. [Google Scholar] [CrossRef]
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Acute Myeloid Leukemia—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/amyl.html (accessed on 5 November 2025).
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Chronic Myeloid Leukemia—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/cmyl.html (accessed on 5 November 2025).
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Hodgkin Lymphoma—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/hodg.html (accessed on 5 November 2025).
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Non-Hodgkin Lymphoma—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/nhl.html (accessed on 5 November 2025).
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Myeloma—Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/mulmy.html (accessed on 5 November 2025).
- Sanchez-Herrero, A.; Calvo, I.A.; Flandes-Iparraguirre, M.; Landgraf, M.; Lahr, C.A.; Shafiee, A.; Granero-Molto, F.; Saez, B.; Mazo, M.M.; Paiva, B.; et al. Engineering a Humanised Niche to Support Human Haematopoiesis in Mice: Novel Opportunities in Modelling Cancer. Cancers 2020, 12, 2205. [Google Scholar] [CrossRef]
- Mian, S.A.; Anjos-Afonso, F.; Bonnet, D. Advances in Human Immune System Mouse Models for Studying Human Hematopoiesis and Cancer Immunotherapy. Front. Immunol. 2021, 11, 619236. [Google Scholar] [CrossRef]
- Tian, H.; Lyu, Y.; Yang, Y.-G.; Hu, Z. Humanized Rodent Models for Cancer Research. Front. Oncol. 2020, 10, 1696. [Google Scholar] [CrossRef]
- Walrath, J.C.; Hawes, J.J.; Van Dyke, T.; Reilly, K.M. Genetically Engineered Mouse Models in Cancer Research. Adv. Cancer Res. 2010, 106, 113–164. [Google Scholar] [CrossRef] [PubMed]
- Kohnken, R.; Porcu, P.; Mishra, A. Overview of the Use of Murine Models in Leukemia and Lymphoma Research. Front. Oncol. 2017, 7, 22. [Google Scholar] [CrossRef]
- Van Norman, G.A. Limitations of Animal Studies for Predicting Toxicity in Clinical Trials. JACC Basic Transl. Sci. 2020, 5, 387–397. [Google Scholar] [CrossRef]
- National Research Council. Guide for the Care and Use of Laboratory Animals: Eighth Edition; National Academies Press: Washington, DC, USA, 2011; ISBN 978-0-309-15400-0.
- Hartung, T. The (Misleading) Role of Animal Models in Drug Development. Front. Drug Discov. 2024, 4, 1355044. [Google Scholar] [CrossRef]
- Lang, Y.; Lyu, Y.; Tan, Y.; Hu, Z. Progress in Construction of Mouse Models to Investigate the Pathogenesis and Immune Therapy of Human Hematological Malignancy. Front. Immunol. 2023, 14, 1195194. [Google Scholar] [CrossRef]
- Fischer, D.; Fluegen, G.; Garcia, P.; Ghaffari-Tabrizi-Wizsy, N.; Gribaldo, L.; Huang, R.Y.-J.; Rasche, V.; Ribatti, D.; Rousset, X.; Pinto, M.T.; et al. The CAM Model—Q&A with Experts. Cancers 2022, 15, 191. [Google Scholar] [CrossRef]
- Martowicz, A.; Kern, J.; Gunsilius, E.; Untergasser, G. Establishment of a Human Multiple Myeloma Xenograft Model in the Chicken to Study Tumor Growth, Invasion and Angiogenesis. J. Vis. Exp. 2015, 1, e52665. [Google Scholar] [CrossRef] [PubMed]
- Maastricht University. Will the Netherlands Ever Be Free of Animal Testing?—Will The Netherlands Ever Be Free of Animal Testing?—Maastricht University. Available online: https://www.maastrichtuniversity.nl/will-netherlands-ever-be-free-animal-testing (accessed on 2 December 2025).
- Sanou, H. No Let up for Animals as Testing Increases Despite Projected Ban. Available online: https://www.dutchnews.nl/2024/11/no-let-up-for-animals-as-testing-increases-despite-projected-ban/ (accessed on 29 March 2025).
- Tolliday, B. Biomedical Sector in the Netherlands Welcomes 2022 EU Report on the Number of Animals Used in Research and Testing. Available online: https://www.eara.eu/post/biomedical-sector-in-the-netherlands-welcomes-2022-eu-report-on-the-number-of-animals-used-in-resear (accessed on 31 March 2025).
- Interpharma, Animal Welfare. Dutch Ban on Animal Experiments. Available online: https://animalwelfare.interpharma.ch/en/topics/3r-dutch-ban-on-animal-experiments/ (accessed on 30 March 2025).
- McGrew, M.J.; Sherman, A.; Ellard, F.M.; Lillico, S.G.; Gilhooley, H.J.; Kingsman, A.J.; Mitrophanous, K.A.; Sang, H. Efficient Production of Germline Transgenic Chickens Using Lentiviral Vectors. EMBO Rep. 2004, 5, 728–733. [Google Scholar] [CrossRef] [PubMed]
- The Roslin Institute. Roslin Green (Cytoplasmic GFP). Available online: https://vet.ed.ac.uk/roslin/engagement/facilities/national-avian-research-facility/avian-resources/genetically-altered-lines/cytoplasmic-gfp-roslin-green (accessed on 27 December 2025).
- Davey, M.G.; Balic, A.; Rainger, J.; Sang, H.M.; McGrew, M.J. Illuminating the Chicken Model through Genetic Modification. Int. J. Dev. Biol. 2018, 62, 257–264. [Google Scholar] [CrossRef]
- The Roslin Institute. CSF1R Reporter Lines. Available online: https://vet.ed.ac.uk/roslin/engagement/facilities/national-avian-research-facility/avian-resources/genetically-altered-lines/csf1r-reporter-lines (accessed on 27 December 2025).
- Balic, A.; Garcia-Morales, C.; Vervelde, L.; Gilhooley, H.; Sherman, A.; Garceau, V.; Gutowska, M.W.; Burt, D.W.; Kaiser, P.; Hume, D.A.; et al. Visualisation of Chicken Macrophages Using Transgenic Reporter Genes: Insights into the Development of the Avian Macrophage Lineage. Development 2014, 141, 3255–3265. [Google Scholar] [CrossRef]
- Sutton, K.; Costa, T.; Alber, A.; Bryson, K.; Borowska, D.; Balic, A.; Kaiser, P.; Stevens, M.; Vervelde, L. Visualisation and Characterisation of Mononuclear Phagocytes in the Chicken Respiratory Tract Using CSF1R-Transgenic Chickens. Vet. Res. 2018, 49, 104. [Google Scholar] [CrossRef]
- Gbyli, R.; Song, Y.; Halene, S. Humanized Mice as Preclinical Models for Myeloid Malignancies. Biochem. Pharmacol. 2020, 174, 113794. [Google Scholar] [CrossRef] [PubMed]
- Zitvogel, L.; Pitt, J.M.; Daillère, R.; Smyth, M.J.; Kroemer, G. Mouse Models in Oncoimmunology. Nat. Rev. Cancer 2016, 16, 759–773. [Google Scholar] [CrossRef]
- de Jong, M.M.E.; Chen, L.; Raaijmakers, M.H.G.P.; Cupedo, T. Bone Marrow Inflammation in Haematological Malignancies. Nat. Rev. Immunol. 2024, 24, 543–558. [Google Scholar] [CrossRef]
- Bernardi, R.; Grisendi, S.; Pandolfi, P.P. Modelling Haematopoietic Malignancies in the Mouse and Therapeutical Implications. Oncogene 2002, 21, 3445–3458. [Google Scholar] [CrossRef] [PubMed]
- Yanguas-Casás, N.; Pedrosa, L.; Fernández-Miranda, I.; Sánchez-Beato, M. An Overview on Diffuse Large B-Cell Lymphoma Models: Towards a Functional Genomics Approach. Cancers 2021, 13, 2893. [Google Scholar] [CrossRef]
- Hamburger, V.; Hamilton, H.L. A Series of Normal Stages in the Development of the Chick Embryo. Available online: https://anatomypubs.onlinelibrary.wiley.com/doi/10.1002/aja.1001950404 (accessed on 23 December 2025).
- Stern, C.D. Staging tables for avian embryos: a little history. Int. J. Dev. Biol. 2018, 62, 43–48. [Google Scholar] [CrossRef]
- Ainsworth, S.J.; Stanley, R.L.; Evans, D.J.R. Developmental Stages of the Japanese Quail. J. Anat. 2010, 216, 3–15. [Google Scholar] [CrossRef]
- Ruparelia, A.A.; Simkin, J.E.; Salgado, D.; Newgreen, D.F.; Martins, G.G.; Bryson-Richardson, R.J. The Quail Anatomy Portal. Database 2014, 2014, bau028. [Google Scholar] [CrossRef]
- Wilhelm, L.A.; Robertson, E.I. Observations on the Embryonic Development of Turkeys*. Poult. Sci. 1941, 20, 425–427. [Google Scholar] [CrossRef]
- Mun, A.M.; Kosin, I.L. Developmental Stages of the Broad Breasted Bronze Turkey Embryo. Biol. Bull. 1960, 119, 90–97. [Google Scholar] [CrossRef]
- Brand, Z.; Cloete, S.W.P.; Malecki, I.A.; Brown, C.R. Ostrich (Struthio Camelus) Embryonic Development from 7 to 42 Days of Incubation. Br. Poult. Sci. 2017, 58, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Bai, S.; Li, S.; Li, X.; Zhu, S.; Shan, Z.; Zhang, J.; Irwin, D.M.; Zhang, S.; Wang, Z. Comparison of Embryonic Development, from HH21 to HH40, between Ostrich (Struthio Camelus) and Chicken (Gallus Gallus). Dev. Dyn. 2023, 252, 668–681. [Google Scholar] [CrossRef]
- Malecki, I.A.; Horbanczuk, J.O.; Reed, C.E.; Martin, G.B. The Ostrich (Struthio Camelus) Blastoderm and Embryo Development Following Storage of Eggs at Various Temperatures. Br. Poult. Sci. 2005, 46, 652–660. [Google Scholar] [CrossRef]
- Nowak-Sliwinska, P.; Segura, T.; Iruela-Arispe, M.L. The Chicken Chorioallantoic Membrane Model in Biology, Medicine and Bioengineering. Angiogenesis 2014, 17, 779–804. [Google Scholar] [CrossRef]
- Bellairs, R.; Osmond, M. Chapter 13—Extra-Embryonic Membranes. In Atlas of Chick Development, 3rd ed.; Bellairs, R., Osmond, M., Eds.; Academic Press: Boston, MA, USA, 2014; pp. 127–129. ISBN 978-0-12-384951-9. [Google Scholar]
- Ribatti, D.; Nico, B.; Vacca, A.; Roncali, L.; Burri, P.H.; Djonov, V. Chorioallantoic Membrane Capillary Bed: A Useful Target for Studying Angiogenesis and Anti-Angiogenesis in Vivo. Anat. Rec. 2001, 264, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Ribatti, D. The Chick Embryo Chorioallantoic Membrane (CAM) Assay. Reprod. Toxicol. 2017, 70, 97–101. [Google Scholar] [CrossRef]
- Chen, L.; Wang, S.; Feng, Y.; Zhang, J.; Du, Y.; Zhang, J.; Van Ongeval, C.; Ni, Y.; Li, Y. Utilisation of Chick Embryo Chorioallantoic Membrane as a Model Platform for Imaging-Navigated Biomedical Research. Cells 2021, 10, 463. [Google Scholar] [CrossRef] [PubMed]
- Ismagulov, G.; Takahashi, Y.; Ishiyama, E.; Ogasawara, K.; Sakai, K.; Chan, Y.N.; Huang, R.Y.-J.; Fukuda, T.; Sheng, G. Morphogenetic Maturation of Chicken Chorioallantoic Membrane (CAM) and Its Disruption by Tumor Xenografts. Dev. Biol. 2026, 529, 154–166. [Google Scholar] [CrossRef]
- Rous, P. Tumor Implantations in the Developing Embryo. Experiments with a Transmissible Sarcoma of the Fowl. J. Amer. Med. Ass. 1911, 56, 741–742. [Google Scholar] [CrossRef]
- Murphy, J.B.; Rous, P. The Behavior of Chicken Sarcoma Implanted in the Developing Embryo. J. Exp. Med. 1912, 15, 119–132. [Google Scholar] [CrossRef]
- Sarnella, A.; Ferrara, Y.; Terlizzi, C.; Albanese, S.; Monti, S.; Licenziato, L.; Mancini, M. The Chicken Embryo: An Old but Promising Model for In Vivo Preclinical Research. Biomedicines 2024, 12, 2835. [Google Scholar] [CrossRef]
- Ribatti, D.; Annese, T. Chick Embryo in Experimental Embryology and More. Pathol. Res. Pract. 2023, 245, 154478. [Google Scholar] [CrossRef]
- Rashidi, H.; Sottile, V. The Chick Embryo: Hatching a Model for Contemporary Biomedical Research. Bioessays 2009, 31, 459–465. [Google Scholar] [CrossRef]
- Kain, K.H.; Miller, J.W.I.; Jones-Paris, C.R.; Thomason, R.T.; Lewis, J.D.; Bader, D.M.; Barnett, J.V.; Zijlstra, A. The Chick Embryo as an Expanding Experimental Model for Cancer and Cardiovascular Research. Dev. Dyn. 2014, 243, 216–228. [Google Scholar] [CrossRef] [PubMed]
- Eckrich, J.; Kugler, P.; Buhr, C.R.; Ernst, B.P.; Mendler, S.; Baumgart, J.; Brieger, J.; Wiesmann, N. Monitoring of Tumor Growth and Vascularization with Repetitive Ultrasonography in the Chicken Chorioallantoic-Membrane-Assay. Sci. Rep. 2020, 10, 18585. [Google Scholar] [CrossRef] [PubMed]
- Dhayer, M.; Jordao, A.; Dekiouk, S.; Cleret, D.; Germain, N.; Marchetti, P. Implementing Chicken Chorioallantoic Membrane (CAM) Assays for Validating Biomaterials in Tissue Engineering: Rationale and Methods. J. Biomed. Mater. Res. Part B Appl. Biomater. 2024, 112, e35496. [Google Scholar] [CrossRef]
- Pinto, M.T.; Ribeiro, A.S.; Conde, I.; Carvalho, R.; Paredes, J. The Chick Chorioallantoic Membrane Model: A New In Vivo Tool to Evaluate Breast Cancer Stem Cell Activity. Int. J. Mol. Sci. 2020, 22, 334. [Google Scholar] [CrossRef]
- Garcia, P.; Wang, Y.; Viallet, J.; Macek Jilkova, Z. The Chicken Embryo Model: A Novel and Relevant Model for Immune-Based Studies. Front. Immunol. 2021, 12, 791081. [Google Scholar] [CrossRef]
- Glick, B.; Chang, T.S.; Jaap, R.G. The Bursa of Fabricius and Antibody Production. Poult. Sci. 1956, 35, 224–225. [Google Scholar] [CrossRef]
- Schat, K.A. The Importance of the Bursa of Fabricius, B Cells and T Cells for the Pathogenesis of Marek’s Disease: A Review. Viruses 2022, 14. [Google Scholar] [CrossRef]
- Voelkl, B.; Altman, N.S.; Forsman, A.; Forstmeier, W.; Gurevitch, J.; Jaric, I.; Karp, N.A.; Kas, M.J.; Schielzeth, H.; Van de Casteele, T.; et al. Reproducibility of Animal Research in Light of Biological Variation. Nat. Rev. Neurosci. 2020, 21, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Bruggeman, V.; Van As, P.; Decuypere, E. Developmental Endocrinology of the Reproductive Axis in the Chicken Embryo. Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 2002, 131, 839–846. [Google Scholar] [CrossRef]
- Luo, X.; Guo, J.; Zhang, J.; Ma, Z.; Li, H. Overview of Chicken Embryo Genes Related to Sex Differentiation. PeerJ 2024, 12, e17072. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, J.; Chen, S.; Yang, N.; Zheng, J. Overview of Avian Sex Reversal. Int. J. Mol. Sci. 2023, 24, 8284. [Google Scholar] [CrossRef]
- Ranjan, R.A.; Muenzner, J.K.; Kunze, P.; Geppert, C.I.; Ruebner, M.; Huebner, H.; Fasching, P.A.; Beckmann, M.W.; Bäuerle, T.; Hartmann, A.; et al. The Chorioallantoic Membrane Xenograft Assay as a Reliable Model for Investigating the Biology of Breast Cancer. Cancers 2023, 15, 1704. [Google Scholar] [CrossRef]
- Ishihara, M.; Hu, J.; Zhang, X.; Choi, Y.; Wong, A.; Cano-Ruiz, C.; Zhao, R.; Tan, P.; Tso, J.L.; Wu, L. Comparing Metastatic Clear Cell Renal Cell Carcinoma Model Established in Mouse Kidney and on Chicken Chorioallantoic Membrane. J. Vis. Exp. 2020, 8, 156. [Google Scholar] [CrossRef]
- Wong, E.A.; Uni, Z. Centennial Review: The Chicken Yolk Sac Is a Multifunctional Organ. Poult. Sci. 2021, 100, 100821. [Google Scholar] [CrossRef]
- Guedes, P.T.; de Oliveira, B.C.E.P.D.; de Abreu Manso, P.P.; Caputo, L.F.G.; Cotta-Pereira, G.; Pelajo-Machado, M. Histological Analyses Demonstrate the Temporary Contribution of Yolk Sac, Liver, and Bone Marrow to Hematopoiesis during Chicken Development. PLoS ONE 2014, 9, e90975. [Google Scholar] [CrossRef]
- Fellah, J.S.; Jaffredo, T.; Nagy, N.; Dunon, D. Chapter 3—Development of the Avian Immune System. In Avian Immunology, 2nd ed.; Schat, K.A., Kaspers, B., Kaiser, P., Eds.; Academic Press: Cambridge, MA, USA, 2014; pp. 45–63. ISBN 978-0-12-396965-1. [Google Scholar]
- Oláh, I.; Vervelde, L. Chapter 2—Structure of the Avian Lymphoid System. In Avian Immunology; Davison, F., Kaspers, B., Schat, K.A., Eds.; Academic Press: Cambridge, MA, USA, 2008; pp. 13–50. ISBN 978-0-12-370634-8. [Google Scholar]
- Kaiser, P.; Stäheli, P. Chapter 10—Avian Cytokines and Chemokines. In Avian Immunology, 2nd ed.; Schat, K.A., Kaspers, B., Kaiser, P., Eds.; Academic Press: Cambridge, MA, USA, 2014; pp. 189–204. ISBN 978-0-12-396965-1. [Google Scholar]
- Nair, V. Chapter 19—Tumours of the Avian Immune System. In Avian Immunology; Davison, F., Kaspers, B., Schat, K.A., Eds.; Academic Press: London, UK, 2008; pp. 359–372. ISBN 978-0-12-370634-8. [Google Scholar]
- Nair, V.; Gimeno, I.; Dunn, J.; Zavala, G.; Williams, S.M.; Reece, R.L.; Hafner, S. Diseases of Poultry. In Chapter 15—Neoplastic Diseases; Swayne, D.E., Bouilianne, M., Logue, C.M., McDougald, L.R., Nair, V., Suarez, D.L., de Wit, S., Grimes, T., Johnson, D., Kromm, M., et al., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2020; pp. 548–715. ISBN 978-1-119-37119-9. [Google Scholar]
- Jasrotia, S.; Gupta, R.; Sharma, A.; Halder, A.; Kumar, L. Cytokine Profile in Multiple Myeloma. Cytokine 2020, 136, 155271. [Google Scholar] [CrossRef]
- Akhmetzyanova, I.; Aaron, T.; Galbo, P.; Tikhonova, A.; Dolgalev, I.; Tanaka, M.; Aifantis, I.; Zheng, D.; Zang, X.; Fooksman, D. Tissue-Resident Macrophages Promote Early Dissemination of Multiple Myeloma via IL-6 and TNFα. Blood Adv. 2021, 5, 3592–3608. [Google Scholar] [CrossRef] [PubMed]
- Ullah, T.R. The Role of CXCR4 in Multiple Myeloma: Cells’ Journey from Bone Marrow to Beyond. J. Bone Oncol. 2019, 17, 100253. [Google Scholar] [CrossRef]
- Subramaniam, S.; Johnston, J.; Preeyanon, L.; Brown, C.T.; Kung, H.-J.; Cheng, H.H. Integrated Analyses of Genome-Wide DNA Occupancy and Expression Profiling Identify Key Genes and Pathways Involved in Cellular Transformation by a Marek’s Disease Virus Oncoprotein. Meq. J. Virol. 2013, 87, 9016–9029. [Google Scholar] [CrossRef]
- Kundeková, B.; Máčajová, M.; Meta, M.; Čavarga, I.; Bilčík, B. Chorioallantoic Membrane Models of Various Avian Species: Differences and Applications. Biology 2021, 10, 301. [Google Scholar] [CrossRef] [PubMed]
- Miebach, L.; Berner, J.; Bekeschus, S. In Ovo Model in Cancer Research and Tumor Immunology. Front. Immunol. 2022, 13, 1006064. [Google Scholar] [CrossRef]
- Mesas, C.; Chico, M.A.; Doello, K.; Lara, P.; Moreno, J.; Melguizo, C.; Perazzoli, G.; Prados, J. Experimental Tumor Induction and Evaluation of Its Treatment in the Chicken Embryo Chorioallantoic Membrane Model: A Systematic Review. Int. J. Mol. Sci. 2024, 25, 837. [Google Scholar] [CrossRef]
- Rasmussen, S.V.; Berlow, N.E.; Price, L.H.; Mansoor, A.; Cairo, S.; Rugonyi, S.; Keller, C. Preclinical Therapeutics Ex Ovo Quail Eggs as a Biomimetic Automation-Ready Xenograft Platform. Sci. Rep. 2021, 11, 23302. [Google Scholar] [CrossRef] [PubMed]
- Hecht, M.; Schulte, J.H.; Eggert, A.; Wilting, J.; Schweigerer, L. The Neurotrophin Receptor TrkB Cooperates with C-Met in Enhancing Neuroblastoma Invasiveness. Carcinogenesis 2005, 26, 2105–2115. [Google Scholar] [CrossRef]
- Kawahara-Miki, R.; Sano, S.; Nunome, M.; Shimmura, T.; Kuwayama, T.; Takahashi, S.; Kawashima, T.; Matsuda, Y.; Yoshimura, T.; Kono, T. Next-Generation Sequencing Reveals Genomic Features in the Japanese Quail. Genomics 2013, 101, 345–353. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, Y.; Hou, Z.; Fan, G.; Pi, J.; Sun, S.; Chen, J.; Liu, H.; Du, X.; Shen, J.; et al. Population Genomic Data Reveal Genes Related to Important Traits of Quail. Gigascience 2018, 7, giy049. [Google Scholar] [CrossRef]
- National Library of Medicine. Coturnix Japonica Genome Assembly Coturnix Japonica 2.0. Available online: https://www.ncbi.nlm.nih.gov/datasets/genome/GCF_001577835.1/ (accessed on 11 November 2025).
- Grinberg, I.; Reis, A.; Ohana, A.; Taizi, M.; Cipok, M.; Tavor, S.; Rund, D.; Deutsch, V.R.; Goldstein, R.S. Engraftment of Human Blood Malignancies to the Turkey Embryo: A Robust New in Vivo Model. Leuk. Res. 2009, 33, 1417–1426. [Google Scholar] [CrossRef]
- Taizi, M.; Deutsch, V.R.; Leitner, A.; Ohana, A.; Goldstein, R.S. A Novel and Rapid in Vivo System for Testing Therapeutics on Human Leukemias. Exp. Hematol. 2006, 34, 1698–1708. [Google Scholar] [CrossRef] [PubMed]
- Farhat, A.; Ali-Deeb, E.; Sulaiman, A.; Aljamali, M. Reinforcing the Utility of Chick Embryo Model to in Vivo Evaluate Engraftment of Human Leukemic Stem Cells. J. Egypt. Natl. Cancer Inst. 2018, 30, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pacini, S.; Punzi, T.; Gulisano, M.; Ruggiero, M. Friend Erythroleukemia Cells Induce Angiogenesis in Chick Embryo Chorioallantoic Membrane and in Human Umbilical Vein Endothelial Cells. Biol. Res. 2008, 41, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.B.; Baksi, R.; Chaudagar, K.K.; Nivsarkar, M.; Mehta, A.A. Anti-leukemic and Anti-angiogenic Effects of d-Limonene on K562-implanted C57BL/6 Mice and the Chick Chorioallantoic Membrane Model. Anim. Model Exp. Med. 2018, 1, 328–333. [Google Scholar] [CrossRef]
- Kuete, V.; Eichhorn, T.; Wiench, B.; Krusche, B.; Efferth, T. Cytotoxicity, Anti-Angiogenic, Apoptotic Effects and Transcript Profiling of a Naturally Occurring Naphthyl Butenone, Guieranone A. Cell Div. 2012, 7, 16. [Google Scholar] [CrossRef]
- Arlt, A.; von Bonin, F.; Rehberg, T.; Perez-Rubio, P.; Engelmann, J.C.; Limm, K.; Reinke, S.; Dullin, C.; Sun, X.; Specht, R.; et al. High CD206 Levels in Hodgkin Lymphoma-educated Macrophages Are Linked to Matrix-remodeling and Lymphoma Dissemination. Mol. Oncol. 2020, 14, 571–589. [Google Scholar] [CrossRef]
- Karagianni, F.; Piperi, C.; Casar, B.; de la Fuente-Vivas, D.; García-Gómez, R.; Lampadaki, K.; Pappa, V.; Papadavid, E. Combination of Resminostat with Ruxolitinib Exerts Antitumor Effects in the Chick Embryo Chorioallantoic Membrane Model for Cutaneous T Cell Lymphoma. Cancers 2022, 14, 1070. [Google Scholar] [CrossRef]
- Klingenberg, M.; Becker, J.; Eberth, S.; Kube, D.; Wilting, J. The Chick Chorioallantoic Membrane as an in Vivo Xenograft Model for Burkitt Lymphoma. BMC Cancer 2014, 14, 339. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, M.; Becker, J.; Eberth, S.; Kube, D.; Wilting, J. The NADPH Oxidase Inhibitor Imipramine-Blue in the Treatment of Burkitt Lymphoma. Mol. Cancer Ther. 2014, 13, 833–841. [Google Scholar] [CrossRef] [PubMed]
- Steiner, N.; Ribatti, D.; Willenbacher, W.; Jöhrer, K.; Kern, J.; Marinaccio, C.; Aracil, M.; García-Fernández, L.F.; Gastl, G.; Untergasser, G.; et al. Marine Compounds Inhibit Growth of Multiple Myeloma in Vitro and in Vivo. Oncotarget 2015, 6, 8200–8209. [Google Scholar] [CrossRef]
- Vacca, A.; Ribatti, D.; Presta, M.; Minischetti, M.; Iurlaro, M.; Ria, R.; Albini, A.; Bussolino, F.; Dammacco, F. Bone Marrow Neovascularization, Plasma Cell Angiogenic Potential, and Matrix Metalloproteinase-2 Secretion Parallel Progression of Human Multiple Myeloma. Blood 1999, 93, 3064–3073. [Google Scholar] [CrossRef]
- Ribatti, D.; De Falco, G.; Nico, B.; Ria, R.; Crivellato, E.; Vacca, A. In Vivo Time-Course of the Angiogenic Response Induced by Multiple Myeloma Plasma Cells in the Chick Embryo Chorioallantoic Membrane. J. Anat. 2003, 203, 323–328. [Google Scholar] [CrossRef]
- Ribatti, D.; Nico, B.; Vacca, A.; Presta, M. The Gelatin Sponge-Chorioallantoic Membrane Assay. Nat. Protoc. 2006, 1, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Winkens, T.; Schweitzer, P.; Perkas, O.; Kühnel, C.; Ndum, F.; Pomraenke, M.; Greiser, J.; Freesmeyer, M. In-Ovo Imaging Using Ostrich Eggs: Biodistribution of F-18-FDG in Ostrich Embryos. Exp. Biol. Med. 2025, 250, 10560. [Google Scholar] [CrossRef] [PubMed]
- Pomraenke , M.; Bolney , R.; Winkens, T.; Perkas, O.; Pretzel , D.; Theis, B.; Greiser, J.; Freesmeyer, M. A Novel Breast Cancer Xenograft Model Using the Ostrich Chorioallantoic Membrane—A Proof of Concept. Vet Sci. 2023, 10, 349. [Google Scholar] [CrossRef]
- Nemkov, T.; D’Alessandro, A.; Reisz, J.A. Metabolic Underpinnings of Leukemia Pathology and Treatment. Cancer Rep. 2018, 2, e1139. [Google Scholar] [CrossRef]
- Rajkumar, S.V. Multiple Myeloma: 2024 Update on Diagnosis, Risk-Stratification, and Management. Am. J. Hematol. 2024, 99, 1802–1824. [Google Scholar] [CrossRef]
- Silberstein, J.; Tuchman, S.; Grant, S.J. What Is Multiple Myeloma? JAMA 2022, 327, 497. [Google Scholar] [CrossRef]
- Nandra, T.K.; Devi, A.; Jones, J.R. Multiple Myeloma: What a Non-Haematologist Should Know. Clin. Med. 2022, 22, 230. [Google Scholar] [CrossRef]
- Folkman, J.; Hanahan, D. Switch to the Angiogenic Phenotype during Tumorigenesis. Princess Takamatsu Symp. 1991, 22, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Carmeliet, P. Mechanisms of Angiogenesis and Arteriogenesis. Nat. Med. 2000, 6, 389–395. [Google Scholar] [CrossRef]
- Costa, C.; Soares, R.; Schmitt, F. Angiogenesis: Now and Then. APMIS 2004, 112, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Ribatti, D.; Gualandris, A.; Bastaki, M.; Vacca, A.; Iurlaro, M.; Roncali, L.; Presta, M. New Model for the Study of Angiogenesis and Antiangiogenesis in the Chick Embryo Chorioallantoic Membrane: The Gelatin Sponge/Chorioallantoic Membrane Assay. J. Vasc. Res. 1997, 34, 455–463. [Google Scholar] [CrossRef]
- Steinhardt, M.J.; Truger, M.; Bittrich, M.; Zhou, X.; Noderer, J.; Riedhammer, C.; Xiao, X.; Gawlas, S.; Weis, P.; Eisele, F.; et al. Venetoclax Salvage Therapy in Relapsed/Refractory Multiple Myeloma. Haematologica 2023, 109, 979–981. [Google Scholar] [CrossRef] [PubMed]
- Bahlis, N.J.; Quach, H.; Baz, R.; Vangsted, A.J.; Ho, S.-J.; Abildgaard, N.; Laubach, J.; Ribrag, V.; Voorhees, P.M.; Wang, X.; et al. Venetoclax in Combination with Daratumumab and Dexamethasone Elicits Deep, Durable Responses in Patients with t(11;14) Relapsed/Refractory Multiple Myeloma: Updated Analyses of Minimal Residual Disease Negativity in Phase 1/2 Study. Blood 2023, 142, 338. [Google Scholar] [CrossRef]
- Costa, L.J.; Davies, F.E.; Monohan, G.P.; Kovacsovics, T.; Burwick, N.; Jakubowiak, A.; Kaufman, J.L.; Hong, W.-J.; Dail, M.; Salem, A.H.; et al. Phase 2 Study of Venetoclax plus Carfilzomib and Dexamethasone in Patients with Relapsed/Refractory Multiple Myeloma. Blood Adv. 2021, 5, 3748–3759. [Google Scholar] [CrossRef]
- Willenbacher, E.; Jöhrer, K.; Willenbacher, W.; Flögel, B.; Greil, R.; Kircher, B. Pixantrone Demonstrates Significant in Vitro Activity against Multiple Myeloma and Plasma Cell Leukemia. Ann. Hematol. 2019, 98, 2569–2578. [Google Scholar] [CrossRef]
| Parameter | Chick CAM Model. | Mouse Model (e.g., Xenograft, Syngeneic, GEMM, PDX) |
|---|---|---|
| Engraftment efficiency | High engraftment with efficiency dependent on implantation route and matrix support. | High engraftment rate for established cell lines in immunodeficient strains, with variable success for primary PDX (dependent on host strain and conditioning). |
| Time to detectable tumour/disease | Visible or imageable tumours and associated angiogenesis typically observed within 3–7 days post-engraftment. | Most murine models require 1–3 weeks for stable disease phenotypes, but this may extend to months. |
| Experimental turnaround | Completed within a single gestation cycle, yielding a total experimental duration of <18 days. | Weeks to months, accounting for engraftment, expansion, dissemination, treatment scheduling, and endpoint analysis. |
| Throughput and scalability | High throughput is enabled by low per-unit cost, minimal space requirements. | Throughput and scalability are limited by housing capacity, cost, and regulatory burden. |
| Cost per experimental unit | Low | High |
| Implantation modes relevant to blood cancers | Surface grafting enables mass formation and angiogenesis studies. Intravascular injection enables analysis of circulation, vascularization, etc. | Intravenous, subcutaneous, and intraosseous routes enable systemic dissemination, marrow tropism, organ-specific colonisation, etc. |
| Ability to model dissemination | Early dissemination can be detected in end organs. | Full dissemination cascades and long-term colonisation can be modelled over extended timeframes. |
| Bone marrow niche fidelity | Limited marrow-like microenvironment present in smaller avian models, restricting faithful modelling or marrow-dependent malignancies, unless niche-mimicking scaffolds are used. | High niche fidelity is achievable, humanised niches or stromal co-engraftment. |
| Immune context | Transient immune maturity. | Typically immunodeficient, though humanised models are available. |
| Imaging accessibility | Direct optical access, with high-resolution imaging of tumour-vascular interactions, supported with minimal instrumentation. | Deep imaging required with specialised modalities like bioluminescence imaging, magnetic resonance imaging, increasing technical and cost barriers. |
| Angiogenesis and vascular remodelling | Angiogenesis is a core strength of CAM models, with vessel patterning and remodelling directly visualised. | Angiogenesis studies are possible but require technically demanding intravital approaches. |
| Pharmacological relevance | Local delivery and rapid drug screens are straightforward, though technically demanding if intravenous routes are examined. | Systemic dosing, high metabolism, and toxicity modelling are applicable. |
| Best-fit applications | Rapid mechanistic studies, angiogenesis, early dissemination, direct tumour effect, and high-throughput drug screening. | Systemic disease biology, marrow dependence, immune therapies, resistance evolution. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Cymer, I.M.; McAuley, N.; Richards, C.E.; Jahns, H.; Glavey, S.V.; Hopkins, A.M. A Bird’s Eye View: A Close Look into Avian CAM Models for Translational Blood Cancer Research. Cancers 2026, 18, 209. https://doi.org/10.3390/cancers18020209
Cymer IM, McAuley N, Richards CE, Jahns H, Glavey SV, Hopkins AM. A Bird’s Eye View: A Close Look into Avian CAM Models for Translational Blood Cancer Research. Cancers. 2026; 18(2):209. https://doi.org/10.3390/cancers18020209
Chicago/Turabian StyleCymer, Izabela M., Niamh McAuley, Cathy E. Richards, Hanne Jahns, Siobhan V. Glavey, and Ann M. Hopkins. 2026. "A Bird’s Eye View: A Close Look into Avian CAM Models for Translational Blood Cancer Research" Cancers 18, no. 2: 209. https://doi.org/10.3390/cancers18020209
APA StyleCymer, I. M., McAuley, N., Richards, C. E., Jahns, H., Glavey, S. V., & Hopkins, A. M. (2026). A Bird’s Eye View: A Close Look into Avian CAM Models for Translational Blood Cancer Research. Cancers, 18(2), 209. https://doi.org/10.3390/cancers18020209








