Patient Positioning and Treatment Techniques in Total Skin Irradiation: A Scoping Review
Simple Summary
Abstract
1. Introduction
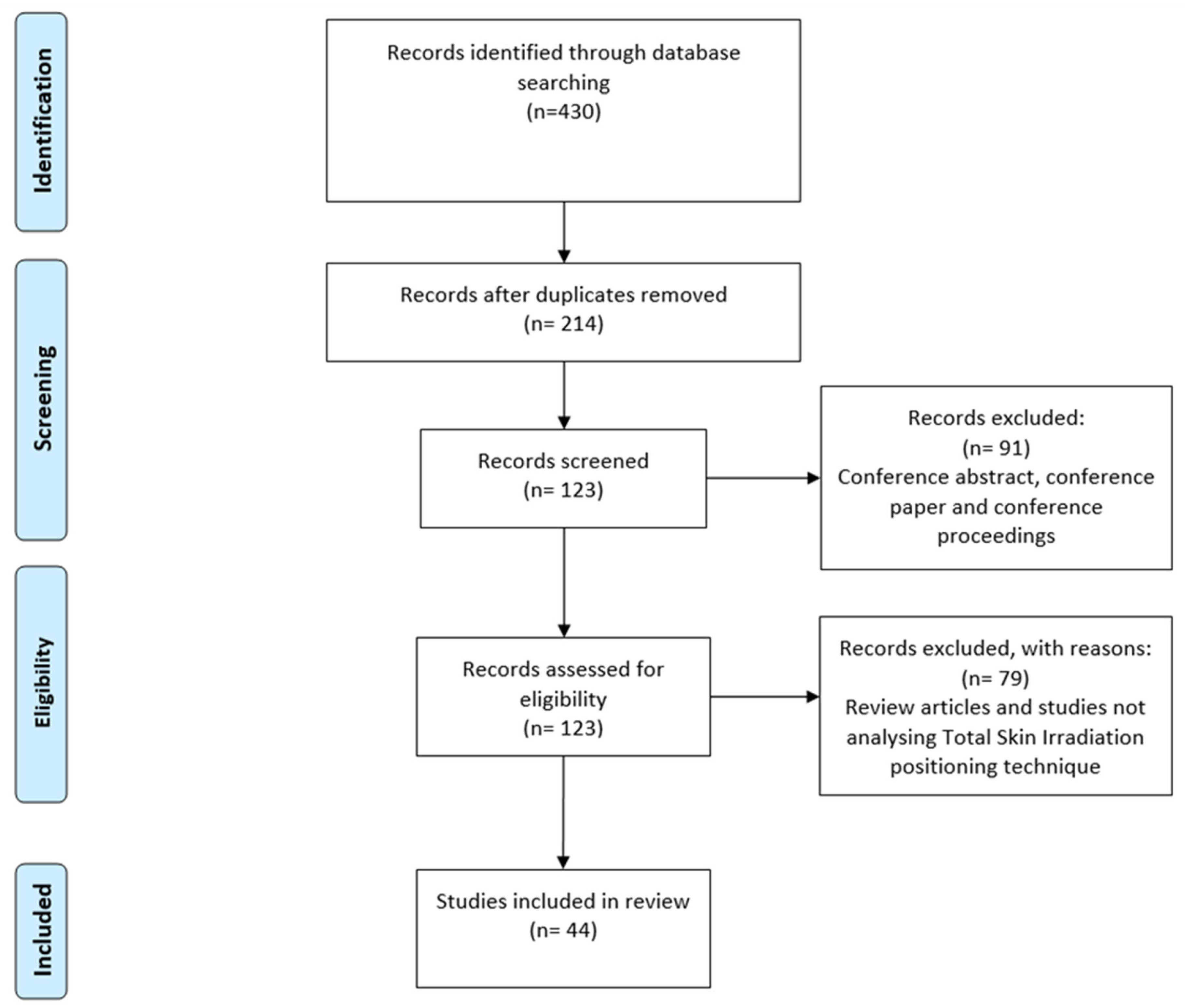
2. Materials and Methods
- Articles were published in English.
- Studies addressed patient positioning techniques implemented in clinical practice during TSI.
- Studies involved human subjects or phantom models.
- Primary research studies were classified under established scientific research frameworks [23].
3. Results
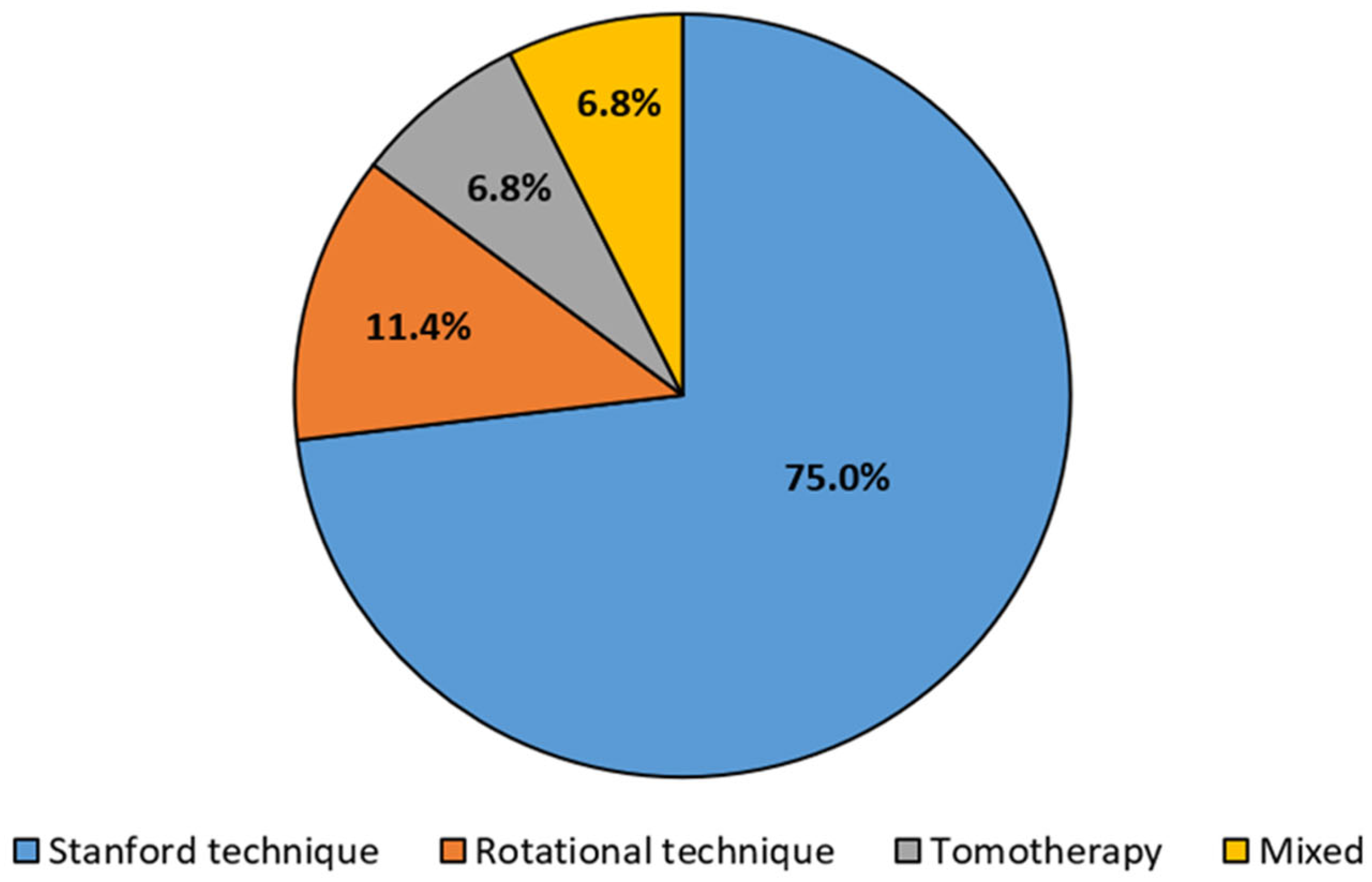
3.1. Study Inclusion and Characteristics
3.2. Stanford Technique
3.3. Rotational Technique
3.4. Tomotherapy
3.5. Mixed Techniques
4. Discussion
4.1. Recommendations for Clinical Practice
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hoppe, R.T.; Fuks, Z.; Bagshaw, M.A. The rationale for curative radiotherapy in mycosis fungoides. Int. J. Radiat. Oncol. Biol. Phys. 1977, 2, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.W.; Hoppe, R.T.; Glatstein, E. Electron Beam Treatment for Cutaneous T-cell Lymphoma. Hematol./Oncol. Clin. N. Am. 1995, 9, 1057–1076. [Google Scholar] [CrossRef]
- Karzmark, C.J.; Anderson, J.; Buffa, A.; Fessenden, P.; Khan, F.; Svensson, G.; Wright, K.; Almond, P.; Fraass, B.; Hogstrom, K.; et al. Total Skin Electron Therapy: Technique and Dosimetry; Report No. 23; American Association of Physicists in Medicine: Alexandria, VA, USA, 1987; ISBN 978-0-883185-49-0. [Google Scholar] [CrossRef]
- Anacak, Y.; Arican, Z.; Bar-Deroma, R.; Tamir, A.; Kuten, A. Total skin electron irradiation: Evaluation of dose uniformity throughout the skin surface. Med. Dosim. 2003, 28, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Schiapparelli, P.; Zefiro, D.; Massone, F.; Taccini, G. Total skin electron therapy (TSET): A reimplementation using radiochromic films and IAEA TRS-398 code of practice. Med. Phys. 2010, 37, 3510–3517. [Google Scholar] [CrossRef]
- Piotrowski, T.; Milecki, P.; Skórska, M.; Fundowicz, D. Total skin electron irradiation techniques: A review. Adv. Dermatol. Allergol. 2013, 1, 50–55. [Google Scholar] [CrossRef]
- Rosenblatt, E.; Kuten, A.; Leviov, M.; Cederbaum, M. Total Skin Electron Irradiation in Mycosis Fungoides Dose and Fractionation Considerations. Leuk. Lymphoma 1998, 30, 143–151. [Google Scholar] [CrossRef]
- Kumar, P.P.; Henschke, U.K.; Nibhanupudy, J.R. Problems and solutions in achieving uniform dose distribution in superficial total body electron therapy. J. Natl. Med. Assoc. 1977, 69, 645–647. [Google Scholar]
- Desai, K.; Pezner, R.; Lipsett, J.; Vora, N.; Luk, K.; Wong, J.; Chan, S.; Findley, D.; Hill, L.; Marin, L.; et al. Total skin electron irradiation for mycosis fungoides: Relationship between acute toxicities and measured dose at different anatomic sites. Int. J. Radiat. Oncol. 1988, 15, 641–645. [Google Scholar] [CrossRef]
- Koken, P.W.; Murrer, L.H. Total Body Irradiation and Total Skin Irradiation Techniques in Belgium and the Netherlands: Current Clinical Practice. Adv. Radiat. Oncol. 2021, 6, 100664. [Google Scholar] [CrossRef]
- Baugh, G.; Al-Alawi, T.; Fletcher, C.L.; A Mills, J.; Grieve, R.J. A preliminary comparison of total skin electron treatment techniques to demonstrate the application of a mid-torso phantom for measurement of dose penetration. Br. J. Radiol. 2011, 84, 1125–1130. [Google Scholar] [CrossRef]
- Karzmark, C.J.; Loevinger, R.; Steele, R.E.; Weissbluth, M. A Technique for Large-Field, Superficial Electron Therapy. Radiology 1960, 74, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Page, V.; Gardner, A.; Karzmark, C.J. Patient Dosimetry in the Electron Treatment of Large Superficial Lesions. Radiology 1970, 94, 635–641. [Google Scholar] [CrossRef]
- Piotrowski, T.; Malicki, J. The rotary dual technique for total skin irradiation in the treatment of mycosis fungoides—A description of the applied method. Rep. Pract. Oncol. Radiother. 2006, 11, 29–37. [Google Scholar] [CrossRef]
- Kumar, P.; Patel, I. Comparison of dose distribution with different techniques of total skin electron beam therapy. Clin. Radiol. 1982, 33, 495–497. [Google Scholar] [CrossRef]
- Wu, J.-M.; Yeh, S.-A.; Hsiao, K.-Y.; Chao, M.M.; Hargrove, I. A conceptual design of rotating board technique for delivering total skin electron therapy. Med. Phys. 2010, 37, 1449–1458. [Google Scholar] [CrossRef]
- Hensley, F.W.; Major, G.; Edel, C.; Hauswald, H.; Bischof, M. Technical and dosimetric aspects of the total skin electron beam technique implemented at Heidelberg University Hospital. Rep. Pract. Oncol. Radiother. 2014, 19, 135–143. [Google Scholar] [CrossRef]
- Ding, G.X.; Osmundson, E.C.; Shinohara, E.; Newman, N.B.; Price, M.; Kirschner, A.N. Monte Carlo study on dose distributions from total skin electron irradiation therapy (TSET). Phys. Med. Biol. 2021, 66, 075010. [Google Scholar] [CrossRef]
- Mackie, T.R. History of tomotherapy. Phys. Med. Biol. 2006, 51, R427–R453. [Google Scholar] [CrossRef]
- Mackie, T.R.; Balog, J.; Ruchala, K.; Shepard, D.; Aldridge, S.; Fitchard, E.; Reckwerdt, P.; Olivera, G.; McNutt, T.; Mehta, M. Tomotherapy. Semin. Radiat. Oncol. 1999, 9, 108–117. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Kapoor, M.C. Types of studies and research design. Indian J. Anaesth. 2016, 60, 626–630. [Google Scholar] [CrossRef]
- Niroomand-Rad, A.; Gillin, M.T.; Komaki, R.; Kline, R.W.; Grimm, D.F. Dose distribution in total skin electron beam irradiation using the six-field technique. Int. J. Radiat. Oncol. 1986, 12, 415–419. [Google Scholar] [CrossRef]
- Gerbi, B.J.; Khan, F.M.; Deibel, F.; Kim, T.H. Total skin electron arc irradiation using a reclined patient position. Int. J. Radiat. Oncol. 1989, 17, 397–404. [Google Scholar] [CrossRef]
- Halberg, F.; Fu, K.; Weaver, K.; Zackheim, H.; Epstein, E.; Wintroub, B. Combined total body X-ray irradiation and total skin electron beam radiotherapy with an improved technique for mycosis fungoides. Int. J. Radiat. Oncol. 1989, 17, 427–432. [Google Scholar] [CrossRef]
- Van Der Merwe, D. Total skin electron therapy: A technique which can be implemented on a conventional electron linear accelerator. Int. J. Radiat. Oncol. 1993, 27, 391–396. [Google Scholar] [CrossRef]
- Peters, V.; Jaywant, S. Implementation of total skin electron therapy using an optional high dose rate mode on a conventional linear accelerator. Med. Dosim. 1995, 20, 99–104. [Google Scholar] [CrossRef]
- Weaver, R.D.; Gerbi, B.J.; Dusenbery, K.E. Evaluation of dose variation during total skin electron irradiation using thermoluminescent dosimeters. Int. J. Radiat. Oncol. 1995, 33, 475–478. [Google Scholar] [CrossRef]
- Earley, L.; Moeller, J.; O’Rear, J.; Leavitt, D.D. A method for total skin electron treatment for infants. Med. Dosim. 1995, 20, 243–248. [Google Scholar] [CrossRef]
- Wu, J.-M.; Leung, S.W.; Wang, C.-J.; Chui, C.-S. Lying-on position of total skin electron therapy. Int. J. Radiat. Oncol. 1997, 39, 521–528. [Google Scholar] [CrossRef]
- Antolak, J.A.; Cundiff, J.H.; Ha, C.S. Utilization of Thermoluminescent Dosimetry in Total Skin Electron Beam Radiotherapy of Mycosis Fungoides. Int. J. Radiat. Oncol. 1998, 40, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Gamble, L.M.; Farrell, T.J.; Jones, G.W.; E Hayward, J. Composite depth dose measurement for total skin electron (TSE) treatments using radiochromic film. Phys. Med. Biol. 2003, 48, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Gamble, L.M.; Farrell, T.J.; Jones, G.W.; Hayward, J.E. Two-dimensional mapping of underdosed areas using radiochromic film for patients undergoing total skin electron beam radiotherapy. Int. J. Radiat. Oncol. 2005, 62, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Bao, Q.; A Hrycushko, B.; Dugas, J.P.; Hager, F.H.; Solberg, T.D. A technique for pediatric total skin electron irradiation. Radiat. Oncol. 2012, 7, 40. [Google Scholar] [CrossRef]
- Platoni, K.; Diamantopoulos, S.; Panayiotakis, G.; Kouloulias, V.; Pantelakos, P.; Kelekis, N.; Efstathopoulos, E. First application of total skin electron beam irradiation in Greece: Setup, measurements and dosimetry. Phys. Med. 2012, 28, 174–182. [Google Scholar] [CrossRef]
- Deufel, C.L.; Antolak, J.A. Total skin electron therapy in the lying-on-the-floor position using a customized flattening filter to accommodate frail patients. J. Appl. Clin. Med. Phys. 2013, 14, 115–126. [Google Scholar] [CrossRef]
- Lučić, F.; Sánchez-Nieto, B.; Caprile, P.; Zelada, G.; Goset, K. Dosimetric characterization and optimization of a customized Stanford Total Skin Electron Irradiation (TSEI) technique. J. Appl. Clin. Med. Phys. 2013, 14, 1–12. [Google Scholar] [CrossRef]
- Sarfehnia, A.; Poon, E.; Davis, S.D.; Fleming, A.; Mitchell, D.; Freeman, C.R. A novel approach to total skin irradiation using helical TomoTherapy. Pract. Radiat. Oncol. 2014, 4, 330–335. [Google Scholar] [CrossRef]
- Fuse, H.; Suzuki, K.; Shida, K.; Mori, Y.; Takahashi, H.; Kobayashi, D.; Seki, M.; Isobe, T.; Okumura, T.; Sakae, T.; et al. Total skin electron beam therapy using an inclinable couch on motorized table and a compensating filter. Rev. Sci. Instrum. 2014, 85, 064301. [Google Scholar] [CrossRef]
- Parida, D.K.; Rath, G.K. Advantages and implications of high dose rate (HDR) total skin electron irradiation (TSEI) for the management of Mycosis Fungoides. Indian experience. Rep. Pract. Oncol. Radiother. 2013, 19, 104–108. [Google Scholar] [CrossRef][Green Version]
- Rivers, C.I.; AlDahlawi, I.; Wang, I.Z.; Singh, A.K.; Podgorsak, M.B. The dose penumbra of a custom-made shield used in hemibody skin electron irradiation. J. Appl. Clin. Med. Phys. 2016, 17, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Andreozzi, J.M.; Zhang, R.; Gladstone, D.J.; Williams, B.B.; Glaser, A.K.; Pogue, B.W.; Jarvis, L.A. Cherenkov imaging method for rapid optimization of clinical treatment geometry in total skin electron beam therapy. Med. Phys. 2016, 43, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Licona, I.; Figueroa-Medina, E.; Gamboa-Debuen, I. Dose distributions and percentage depth dose measurements for a total skin electron therapy. Radiat. Meas. 2017, 106, 365–372. [Google Scholar] [CrossRef]
- Elsayad, K.; Moustakis, C.; Simonsen, M.; Bäcker, D.; Haverkamp, U.; Eich, H.T. In-vivo dosimetric analysis in total skin electron beam therapy. Phys. Imaging Radiat. Oncol. 2018, 6, 61–65. [Google Scholar] [CrossRef]
- Kron, T.; Donahoo, G.; Lonski, P.; Wheeler, G. A technique for total skin electron therapy (TSET) of an anesthetized pediatric patient. J. Appl. Clin. Med. Phys. 2018, 19, 109–116. [Google Scholar] [CrossRef]
- Ansari, M.; Davani, F.A.; Rashti, M.L.; Monadi, S.; Emami, H. Monte Carlo study and design of system for implementation of Rotational Total Skin Electron Irradiation technique. J. Instrum. 2018, 13, P05029. [Google Scholar] [CrossRef]
- Ibanez-Rosello, B.; Bautista, J.A.; Bonaque, J.; Perez-Calatayud, J.; Gonzalez-Sanchis, A.; Lopez-Torrecilla, J.; Brualla-Gonzalez, L.; Garcia-Hernandez, T.; Vicedo-Gonzalez, A.; Granero, D.; et al. Failure modes and effects analysis of total skin electron irradiation technique. Clin. Transl. Oncol. 2018, 20, 330–365. [Google Scholar] [CrossRef]
- Haraldsson, A.; Engleson, J.; Bäck, S.Å.J.; Engelholm, S.; Engström, P.E. A Helical tomotherapy as a robust low-dose treatment alternative for total skin irradiation. J. Appl. Clin. Med. Phys. 2019, 20, 44–54. [Google Scholar] [CrossRef]
- Diamantopoulos, S.; Kagkiouzis, I.; Patatoukas, G.; Kypraiou, E.; Kouloulias, V.; Efstathopoulos, E.; Platoni, K. Three dimensional printed electron beam modifier for total skin electron treatments. Med. Dosim. 2019, 44, 173–178. [Google Scholar] [CrossRef]
- Falahati, L.; Nedaie, H.A.; Esfahani, M.; Banaee, N. Dosimetric evaluation of electron total skin irradiation using gafchromic film and thermoluminescent dosimetry. J. Cancer Res. Ther. 2019, 15, S115–S122. [Google Scholar] [CrossRef]
- Li, R.; Tseng, W.; Wu, Q. Validation of the dosimetry of total skin irradiation techniques by Monte Carlo simulation. J. Appl. Clin. Med. Phys. 2020, 21, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Tseng, W.; Li, R.; Wu, Q. Investigation of effect of filter on the stand-up technique for total skin irradiation by Monte Carlo simulation. J. Appl. Clin. Med. Phys. 2020, 22, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Rahimy, E.; Skinner, L.; Kim, Y.H.; Hoppe, R.T. Technical report: 3D-printed patient-specific scalp shield for hair preservation in total skin electron beam therapy. Tech. Innov. Patient Support Radiat. Oncol. 2021, 18, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Ackerson, B.G.; Wu, Q.; Craciunescu, O.; Oyekunle, T.; Niedzwiecki, D.; Gupton, J.; Laug, P.; Brumfield, K.; Crain, E.; Champ, C.E.; et al. Recumbent Total Skin Electron Beam Therapy. Adv. Radiat. Oncol. 2021, 6, 100698. [Google Scholar] [CrossRef]
- Monzari, S.F.; Geraily, G.; Aghili, M.; Toolee, H. Evaluation of Dose Distribution in Optimized Stanford Total Skin Electron Therapy (TSET) Technique in Rando Anthropomorphic Phantom using EBT3 Gafchromatic Films. J. Biomed. Phys. Eng. 2021, 11, 425–434. [Google Scholar] [CrossRef]
- Zhu, T.C.; Ong, Y.H.; Sun, H.; Zhong, W.; Miao, T.; Dimofte, A.; Bruza, P.; Maity, A.; Plastaras, J.P.; Paydar, I.; et al. Cherenkov imaging for total skin electron therapy: An evaluation of dose uniformity. Proc. SPIE Int. Soc. Opt. Eng. 2021, 11628, 116280R. [Google Scholar]
- Ding, G.X.; Chen, Z.J.; Zhong, W.; Zhu, T.C. Skin dose distributions between Stanford and rotational techniques in total skin electron therapy (TSET). Med. Phys. 2022, 49, 6646–6653. [Google Scholar] [CrossRef]
- Baba, M.H.; Singh, B.K.; Wani, S.Q. In vivo Dosimetry for Dose Verification of Total Skin Electron Beam Therapy Using Gafchromic® EBT3 Film Dosimetry. J. Med. Phys. 2022, 47, 362–366. [Google Scholar] [CrossRef]
- Shariff, M.; Stillkrieg, W.; Lotter, M.; Lohmann, D.; Weissmann, T.; Fietkau, R.; Bert, C. Dosimetry, Optimization and FMEA of Total Skin Electron Irradiation (TSEI). Z. Med. Phys. 2022, 32, 228–239. [Google Scholar] [CrossRef]
- Wang, H.; Pi, Y.; Guo, Y.; Pei, X.; Xu, X.G. Influencing Factors of Total Skin Irradiation With Helical Tomotherapy. Front. Oncol. 2022, 12, 852345. [Google Scholar] [CrossRef]
- Diamantopoulos, S.; Platoni, K.; Dilvoi, M.; Nazos, I.; Geropantas, K.; Maravelis, G.; Tolia, M.; Beli, I.; Efstathopoulos, E.; Pantelakos, P.; et al. Clinical implementation of total skin electron beam (TSEB) therapy: A review of the relevant literature. Phys. Med. 2011, 27, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Miao, T.; Zhang, R.; Jermyn, M.; Bruza, P.; Zhu, T.; Pogue, B.W.; Gladstone, D.J.; Williams, B.B. Computational dose visualization & comparison in total skin electron treatment suggests superior coverage by the rotational versus the Stanford technique. J. Med. Imaging Radiat. Sci. 2022, 53, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Schaff, E.M.; Rosenberg, S.A.; Olson, S.J.; Howard, S.P.; Bradley, K.A. Bone marrow suppression as a complication of total skin helical tomotherapy in the treatment of mycosis fungoides. Radiat. Oncol. 2018, 13, 67. [Google Scholar] [CrossRef]
- Kitaguchi, M.; Yamashita, H.; Takenaka, R.; Okuma, K.; Nawa, K.; Nakagawa, K. Helical Skin Radiation Therapy Including Total Skin Radiation Therapy Using Tomotherapy for Primary Cutaneous Lymphoma With Bone Marrow Suppression as a Related Adverse Event. Pract. Radiat. Oncol. 2021, 11, e308–e321. [Google Scholar] [CrossRef]
| First Author and Year | State | Sample Size | Technique | Delivery Technique | Energy | Prescribed Dose | Filter or Degrader | SSD | Patient Position | Shielding |
|---|---|---|---|---|---|---|---|---|---|---|
| Kumar et al. 1982 [15] | 36 | USA | Rotational | Dual-field technique (gantry angle of ±15° relative to the horizontal axis) | 6 MeV | NA | 1 cm thick polystyrene screen, 20 cm from the patient | NA | Standing on a rotating platform (5 rpm) | NA |
| Niroomand-Rad et al., 1986 [24] | NA | USA | Stanford | Six dual-field technique | NA | NA | Dual scattering foils (stainless steel + Al) | 3.5 m | Standing on a wooden platform | Eye shield (gold-plated lead, 2.0 to 2.5 mm thick). Uninvolved areas of the body were shielded with lead sheets. |
| Gerbi et al. 1989 [25] | NA | USA | Stanford | Two electron arc fields (±48° relative to the vertical axis) for each of the six positions | 6 MeV | NA | NA | 2 m | Reclined on a low couch near the treatment room floor. The oblique fields were achieved by rotating the patient and supporting him using Styrofoam wedges and pillows. | NA |
| Halberg et al. 1989 [26] | 20 | USA | Stanford | Six dual-field technique (beams delivered at gantry angles of 250° and 290°) | 6 MeV | 24 Gy in 6 fractions. Areas not exposed to the beam were boosted with a dose of 12 Gy | NA | 3 m | Standing on an elevated platform with an attached supporting frame | NA |
| Van Der Merwe et al. 1993 [27] | NA | South Africa | Stanford | Six dual-field technique | 6 MeV | NA | NA | 2 m | Supine or prone on a movable wooden trolley on the floor. The oblique fields were treated with the patient resting on a 60-degree Styrofoam wedge. | NA |
| Peters et al. 1995 [28] | NA | Canada | Stanford | Six dual-field technique (gantry angle of ±20° relative to the horizontal axis); HDR TSI mode | 6 MeV | 35 Gy in 20 fractions | An acrylic beam degrader, 6 mm thick, was attached to the front of the stand to reduce electron beam penetration | 3.6 m | Standing on an adjustable treatment stand elevated 20 cm above floor level to prevent underdosage at the feet. The stand featured adjustable pegs to provide optimal arm support and included independent turntables for the foot supports for oblique fields. | NA |
| Weaver et al. 1995 [29] | 22 | USA | Stanford | Six dual-field technique (gantry angle of ±22/28° relative to the horizontal axis); HDR TSI mode | 9 MeV | 35/40 Gy | A 1 cm thick acrylic beam spoiler, placed near the patient, was used to scatter the beam | 4.1 m | Standing | Lead shields were placed over the contact lens and under the eyelid. Lead shields were placed over the toes to shield the toenails after a dose of 10 Gy. |
| Earley et al. 1995 [30] | 1 pediatric patient (14-month-old child) | USA | Stanford | Twelve-beam irradiation technique (the gantry was set at a 60° angle for an oblique position) | 6 MeV | 28 Gy in 14 fractions | NA | 2 m | Supine and prone on an 80 cm long Plexiglas platform (under anesthesia). For oblique positions, the platform was elevated onto a modified cart and adjusted for the correct distance and orientation. | Lead shields were placed over the fingernails. For the toes, lead strips were coated with wax formed to fit over the nails and nail beds. |
| Wu et al. 1997 [31] | NA | USA | Stanford | Dual-field technique for AP/PA positions (gantry angle of ±25° relative to the vertical axis). Four fields rotated 60° toward patients for the oblique position. HDR TSI mode | 6 MeV | NA | For the AP/PA positions, a 0.6 cm thick acrylic board was positioned 15 cm from the patient. For the oblique position, the acrylic board was placed perpendicular to the beam. | 2.13 m for the AP/PA position; 3.3 m for oblique position | Supine and prone positions (laying on the floor). | An eye plaque with a 3 mm lead shield was attached to the surface of the eyeball, functioning as a contact lens. The finger and toenails were covered by a suitable 3 mm lead shielding material. |
| Antolak et al. 1998 [32] | 72 | USA | Stanford | Six dual-field technique (gantry angles were set to 113° and 67°); HDR TSI mode | 4.29/4.41 MeV at the treatment distance | 32 Gy in 16 fractions | A 1.3 cm thick acrylic scatter plate was positioned 25 cm in front of the patient | 1.9/2 m | Standing position | NA |
| Gamble et al. 2003 [33] | NA | Canada | Stanford | Six dual-field technique (gantry angle of ±20° relative to the horizontal axis); HDR TSI mode | 6 MeV (5.2 MeV at treatment distance) | NA | A 6 mm thick acrylic sheet was positioned in front of the patient | 3.6 m | Standing position | NA |
| Gamble et al. 2005 [34] | NA | Canada | Stanford | Six dual-field technique (gantry angle of ±20° relative to the horizontal axis); HDR TSI mode | 6 MeV (5.2 MeV at treatment distance) | 35 Gy in 30 fractions | A 6 mm thick acrylic sheet was positioned in front of the patient | 3.6 m | Standing position | NA |
| Piotrowski et al. 2006 [14] | 15 | Poland | Rotational | Dual-field technique (gantry angle of ±20° relative to the horizontal axis) | 6 MeV | 36 Gy in 24 fractions | A 1 cm thick plexiglass board was placed 20 cm from the skin | 3 m | Standing position on a rotating platform | Eye shields (lead coated in paraffin) nail shields |
| Wu et al. 2010 [16] | NA | Taiwan | Rotational | Dual-beam technique for each patient position (gantry angle of ±15.5° from the horizontal); HDR TSI mode | 9 MeV | 36 Gy in 36 fractions | A 0.6 cm acrylic spoiler was placed 90 cm from the skin to ensure a homogeneous dose | 4.5 m | Supine or prone on a homemade rotating board | NA |
| Bao et al. 2012 [35] | 2 pediatric patients (17 months and 12 months) | USA | Stanford | Six dual-field technique (gantry angle of ±20° relative to the horizontal axis); HDR TSI mode | 6 MeV | 16 Gy in 8 fractions | A 1.2 cm plexiglass scatter plate was placed 25 cm in front of the patient | 3.3 m | Standing position (under anesthesia) in the harness system, attached to a frame used for TBI. This harness covered the patient’s torso and was attached to the rotating plate, with four straps looped through carabiner clips. | NA |
| Platoni et al. 2012 [36] | NA | Greece | Stanford | Six dual-field technique (gantry angle of ±17.5° relative to the horizontal axis); HDR TSI mode | 6 MeV | NA | PMMA sheet (203 × 111 cm) of 0.5 cm thickness was placed in front of the patient | 3.8 m | Standing position using a suitable immobilization system equipped with two support straps | Eye shields (a pair of goggles filled with Pb of 1.5 cm thickness). Toenails and fingernails (lead layer of 0.4 cm thickness). Genital area (covered with a 2 cm water bag, pasted on top of a 0.4 cm Pb layer). Head (0.4 cm thick lead plate). |
| Deufel et al. 2013 [37] | NA | USA | Stanford | Three fields for AP and PA positions (angles: 0°, 60°, and 300°). For the oblique position, the gantry was rotated to 300°; HDR TSI mode | 6 MeV | NA | A 0.4 cm polycarbonate spoiler was placed 5 cm above the patient’s proximal skin surface | 2.31 m for the AP/PA position; 3.12 m for oblique position | In the AP and PA positions, patients were reclined on the floor, oriented head-to-foot perpendicular to the linac waveguide. For the oblique position, the patient was oriented head-to-foot, parallel to the linac waveguide. | Fingernail and eye shields |
| Luĉić et al. 2013 [38] | NA | Chile | Stanford | Dual vertical beams (0° for field) for each patient position with parallel central axes separated by 80 cm, allowing superior and inferior parts of the body | 6 MeV | NA | Custom-made polyester filter and a uniform PMMA degrader plate with a thickness of 8 mm | 2 m | Supine or prone on a translational platform | A strip of lead (3 mm thickness) was used to avoid hot spots in the region where the superior and inferior fields overlapped |
| Sarfehnia et al. 2014 [39] | 1 | Canada | Tomotherapy | FW of 5 cm, pitch of 0.287, and MF of 2.5. Daily full-body megavoltage imaging using MVCT | 6 MV | 14 Gy in 7 fractions | NA | NA | Supine position (under anesthesia); immobilized using a Vac-Lok cushion and a thermoplastic mask | Blocks for the brain, thoracic cavity, and abdomen |
| Fuse et al. 2014 [40] | NA | Japan | Stanford | Six-field technique (comprising four oblique fields and AP and PA gantry orientations) | 6 MeV | NA | Two layers of polystyrene, each 2 mm thick, on a 10 mm thick PMMA sheet | 1.7–1.8 m | Supine and prone positions on a motorized, inclinable table designed with symmetrical asperities to secure suction bags for patient immobilization. The table moved at a constant speed, synchronized with the linac. | Eyes (lead lenses), nails of fingers and toes (lead plate) |
| Hensley et al. 2014 [17] | NA | Germany | Rotational | Dual-field technique (gantry angles of 72° and 108°) | 6 MeV | NA | 6 mm Perspex screen | 3.7 m | Standing position on a rotating turntable, with the patient holding a swivel bar to maintain proper posture, keep their arms extended, and provide support while standing | Fingernail, toe, and eye shields |
| Parida et al. 2013 [41] | 25 (14 treated with older technique and 11 treated with HDTSI mode) | India | Stanford | Six dual-field technique (gantry angle of ±15° relative to the horizontal axis); HDR TSI mode | 4 MeV | 36 Gy in 30 fractions. A boost dose of 10 Gy was delivered to self-shielding regions | Polystyrene screen at a distance of 10 feet. With the implementation of the HDTSI technique, the use of the polystyrene screen was not required. | NA | Standing position on a stationary platform | Eyes and nails shielded with a 3 mm thick lead |
| Rivers et al. 2016 [42] | NA | USA | Stanford | Six dual-field technique (gantry angles of 248° and 292°); HDR TSI mode | 6 MeV | NA | Lucite spoiler accessory | 3.77 m | Standing position on an elevated platform | To treat hemibody, a shield consisting of three rectangular layers of plywood with a total thickness of 4.75 cm was used. The plywood layers were clamped on a stand that was positioned 50 cm away from the patient. |
| Andreozzi et al. 2016 [43] | 3 | USA | Stanford | Six dual-field technique (gantry angles of 284.5° and 255.5°) | 6 MeV | 18 Gy in 18 fractions; 36 Gy in 36 fractions | NA | 4.41 m | Standing position | NA |
| Licona et al. 2017 [44] | NA | Mexico | Stanford | Six dual-field technique; HDR TSI mode | 6 MeV | NA | A large plastic panel with a thickness of 5 mm was located 20 cm in front of the patient | 3 m | Standing position on a wooden platform | NA |
| Elsayad et al. 2018 [45] | 85 (standing, n = 77; reclined, n = 8) | Germany | Stanford | Six dual-field technique; HDR TSI mode | 6–9 MeV | NA | NA | NA | The majority of patients were treated in a standing position, while the remaining 8 patients were treated in a lying position | External eye shields were used during wide-field skin irradiation to protect the cornea and lens, while the nails of the hands and feet were shielded to preserve nail growth |
| Kron et al. 2018 [46] | 1 pediatric patient (2-yr-old patient) | Australia | Stanford | Two sets of six fields (gantry orientations: 0°, 60°, 120°, 180°, 240°, 300°, 360°); HDR TSI mode | 6 MeV | 18 Gy in 12 fractions. Boost doses of 4 and 6 Gy in six areas (respectively, in 2 and 3 fractions) | 1.2 cm thick PMMA block mounted on the gantry | 1.24 m | Supine (under anesthesia) on a customized thin window Mylar top (thickness of 0.3 mm) inserted in the treatment couch. After delivery of the first six fields to the upper part of the body, the patient was rotated and the lower half was treated. | Shields were applied to the eyes. Toenail shields were introduced from the third fraction, while fingernail shields were added after the eighth fraction. |
| Ansari et al. 2018 [47] | NA | Iran | Mixed (Stanford and rotational) | Stanford: six dual-field technique Rotational: dual-field HDR TSI mode | 6 MeV | NA | A 0.8 cm PMMA degrader was placed 20 cm in front of the patient | 3.5 m | Rotational: standing position on a rotating platform at a speed of 3 rpm | NA |
| Ibanez-Rosello et al. 2018 [48] | 80 | Spain | Stanford | Six dual-field technique | 6 MeV | NA | A degradative screen (8 mm methacrylate) placed 20 cm in front of the patient | NA | Standing position | NA |
| Haraldsson et al. 2019 [49] | 2 | Sweden | Tomotherapy | CT simulation acquired with a slice thickness of 5 mm. FW of 5 cm, pitch of 0.2, and MF of 2.3. Daily MVCT performed. | NA | 12 Gy in 6 fractions; 20 Gy in 10 fractions | NA | NA | Supine position with immobilization systems included a large vacuum cushion (VacFix), an individually molded neck rest, and a five-point open-face thermoplastic mask. | Shields for the genitals, eyes, and lips. A hood, gloves, and socks of neoprene. |
| Diamantopoulos et al. 2019 [50] | NA | Greece | Stanford | Six dual-field technique; HDR TSI mode | 6 MeV | NA | A 0.5 cm thick Plexiglas panel | 4 m | Standing position using a custom-made immobilization device equipped with adjustable hand grips | NA |
| Falahati et al. 2019 [51] | NA | Iran | Mixed (Stanford and rotational) | Stanford: six-field technique. Rotational: gantry angle of 90° | 6 MeV | NA | A plexiglass filter with a thickness of 5 mm was placed 20 cm in front of the patient | 4 m | Stanford: standing position; rotational: standing position on a rotating platform. The platform had a 60 cm diameter, with a height of 81 cm, and rotated at a speed of 3 rpm. | NA |
| R. Li et al. 2020 [52] | NA | USA | Stanford | Stanford stand-up: six dual-field technique (gantry angles of 251° and 289°). Stanford lay-down: ten electron beams (AP and PA six beams: gantry orientations of 0°, 300°, 60°—oblique four fields: gantry orientation of 300°) HDR TSI mode | 6 MeV | NA | A customized Cu (0.25 mm copper disk) scattering filter placed on the interface mount | Stand-up: 3 m; lay down—AP/PA: 1.95 m; oblique: 3.05 m | Stand-up: Standing position on a platform that could rotate at steps of 60°. Lay down: Supine and prone on a platform. | NA |
| Koken et al. 2021 [10] | 26 per year (the yearly average number of patients is 11 in Belgium and 15 in the Netherlands) | Netherlands and Belgium | Stanford | Six fields | 4, 6, or 9 MeV | 8 × 1.5 Gy on a daily basis; from 7 to 10 × 3 Gy every other day | Lucite diffuser used for 6 and 9 MeV | NA | Standing position (2 institutions) or lying on a stretcher (2 institutions) in prone and supine positions | In three institutions, eyes were shielded using lead goggles, while one institution did not use any shielding (it used the lowest dose scheme) |
| Tseng et al. 2020 [53] | NA | USA | Stanford | Stanford stand-up: Six dual-field technique (gantry angle of ±15° relative to the horizontal axis). Lay-down: Two vertex fields and four oblique fields (gantry orientation: 60°); HDR TSI mode | 6 MeV | NA | Lay-down: 0.25 mm thick copper disc was placed between two 1 mm polycarbonate layers | Stand-up: 3 m | Stand-up standing position on a specific platform. Lay-down: supine and prone | NA |
| Rahimy et al. 2021 [54] | 20 per year | USA | Stanford | Six dual-field technique; HDR TSI mode | 9 MeV | NA | Two PMMA spoilers, total thickness of 1.4 cm, roughly 600 cm of air | NA | Standing position | 3D-printed scalp shield used to minimize the risk of permanent alopecia |
| Ackerson et al. 2021 [55] | 27 (13 treated in recumbent position and 14 treated in standing position) | USA | Stanford | Lay-down: ten electron beams (AP and PA: six beams with gantry orientations of 0°, 300°, and 60°; oblique: four fields with a gantry orientation of 300°); HDR TSI mode | 6 MeV | From 15 to 36 Gy | Lay-down: A customized scattering filter made of 0.025 cm thick copper was placed in the interface mount of the linac | Lay down: AP/PA: 1.95 m; oblique: 3.05 m | Stand-up: Standing position on an elevated platform. Lay down: Supine and prone (five fields each) on a polycarbonate platform with recessed side wheels (body-to-floor distance of 5 cm) | Hands and feet shielded with the stand-up technique |
| Monzari et al. 2021 [56] | NA | Iran | Stanford | Gantry orientations for AP and PA positions: 0°, 318.5°, 42.5°; Gantry orientation for 4 oblique fields: 291.4° | 6 MeV | NA | A beam spoiler made of Plexiglas with a thickness of 5 mm was placed 6.5 cm (for AP/PA fields) or 5 cm (for oblique fields) in front of the patient | AP and PA positions: 2.06 m /0.95 m. Oblique fields: 2.38 m | Supine or prone position | NA |
| Zhu et al. 2021 [57] | NA | USA | Stanford | Six dual-field technique (gantry angles of 74° and 106°) HDR TSI mode | 6 MeV | NA | NA | 5 m | Standing position | NA |
| Ding et al. 2021 [18] | NA | USA | Rotational | Dual-field technique; HDR TSI mode | 6 MeV | 12 Gy in 12 fractions | An acrylic beam degrader (3 mm or 9 mm thick) was placed 50 cm in front of the patient | 3.16 m | Standing position on a rotating platform, which featured a hand-held bar that freely rotated and was anchored to the ceiling | NA |
| Ding et al. 2022 [58] | NA | USA | Mixed (Stanford and rotational) | Stanford: six-field technique. Stanford and rotational: dual-field technique (for SSD: 3.16 m, 42° difference angle between two beams; for SSD: 5 m, 32° difference angle between two beams); single-field technique (for SSD: 7 m); HDR TSI mode | 6 MeV | NA | A 3 mm acrylic scattering plate used for treatment with SSD, 3.16 m and 5 m. | 3.16 m, 5 m, 7 m | Stanford: standing position. Rotational: standing position on a rotating platform stand | NA |
| Baba et al. 2022 [59] | 6 | India | Stanford | Six dual-field technique | 6 MeV | NA | NA | NA | Standing position | NA |
| Shariff et al. 2022 [60] | NA | Germany | Stanford | Six dual-field technique (289° and 251°); HDR TSI mode | 6 MeV | 30 Gy in 20 fractions | A planar acrylic scatter plate, 5 mm thick, was placed 50 cm in front of the patient | 3.3 m | Standing position | Eye protection, gloves with lead plates to shield fingernails; toenails cover with lead; lead protection for testicles |
| Wang et al. 2022 [61] | 6 | China | Tomotherapy | CT simulation acquired with a slice thickness of 5 mm. FW = 5 cm/2.5 cm, pitch = 0.215/0.287, MF = 3/4 | NA | 24 Gy in 20 fractions | NA | NA | Supine position, immobilized with thermoplastic mask for the head, neck, thorax, and abdomen, and a vacuum cushion for the lower limbs | 5 mm diving suit |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lastrucci, A.; Canzani, E.; Haghighatjou, N.; Marrazzo, L.; Iosca, N.; Wandael, Y.; Giansanti, D.; Ricci, R.; Mangoni, M.; Pallotta, S.; et al. Patient Positioning and Treatment Techniques in Total Skin Irradiation: A Scoping Review. Cancers 2025, 17, 1276. https://doi.org/10.3390/cancers17081276
Lastrucci A, Canzani E, Haghighatjou N, Marrazzo L, Iosca N, Wandael Y, Giansanti D, Ricci R, Mangoni M, Pallotta S, et al. Patient Positioning and Treatment Techniques in Total Skin Irradiation: A Scoping Review. Cancers. 2025; 17(8):1276. https://doi.org/10.3390/cancers17081276
Chicago/Turabian StyleLastrucci, Andrea, Emanuele Canzani, Neda Haghighatjou, Livia Marrazzo, Nicola Iosca, Yannick Wandael, Daniele Giansanti, Renzo Ricci, Monica Mangoni, Stefania Pallotta, and et al. 2025. "Patient Positioning and Treatment Techniques in Total Skin Irradiation: A Scoping Review" Cancers 17, no. 8: 1276. https://doi.org/10.3390/cancers17081276
APA StyleLastrucci, A., Canzani, E., Haghighatjou, N., Marrazzo, L., Iosca, N., Wandael, Y., Giansanti, D., Ricci, R., Mangoni, M., Pallotta, S., Simontacchi, G., & Livi, L. (2025). Patient Positioning and Treatment Techniques in Total Skin Irradiation: A Scoping Review. Cancers, 17(8), 1276. https://doi.org/10.3390/cancers17081276








