Feasibility and Acceptability of the Cancer-Specific PRONTO Protocol for Nutritional Risk Screening in Outpatient Oncology Cancer Care: A Pilot Study
Simple Summary
Abstract
1. Introduction
- •
- Body Weight Loss: Have you unintentionally lost weight (5% to 10% or more) in the last 3–6 months/since our last consultation?
- •
- Appetite and Food Intake: Have you been eating less than usual in the last week/since our last consultation?
- •
- Strength and Mobility: Have you lost strength, or do you feel weaker than usual/since our last consultation?
2. Materials and Methods
2.1. Study Design
2.2. Healthcare Professionals (HCPs)
2.3. Patients
2.4. Sample Size
2.5. Ethical Review
2.6. Statistical Analyses
3. Results
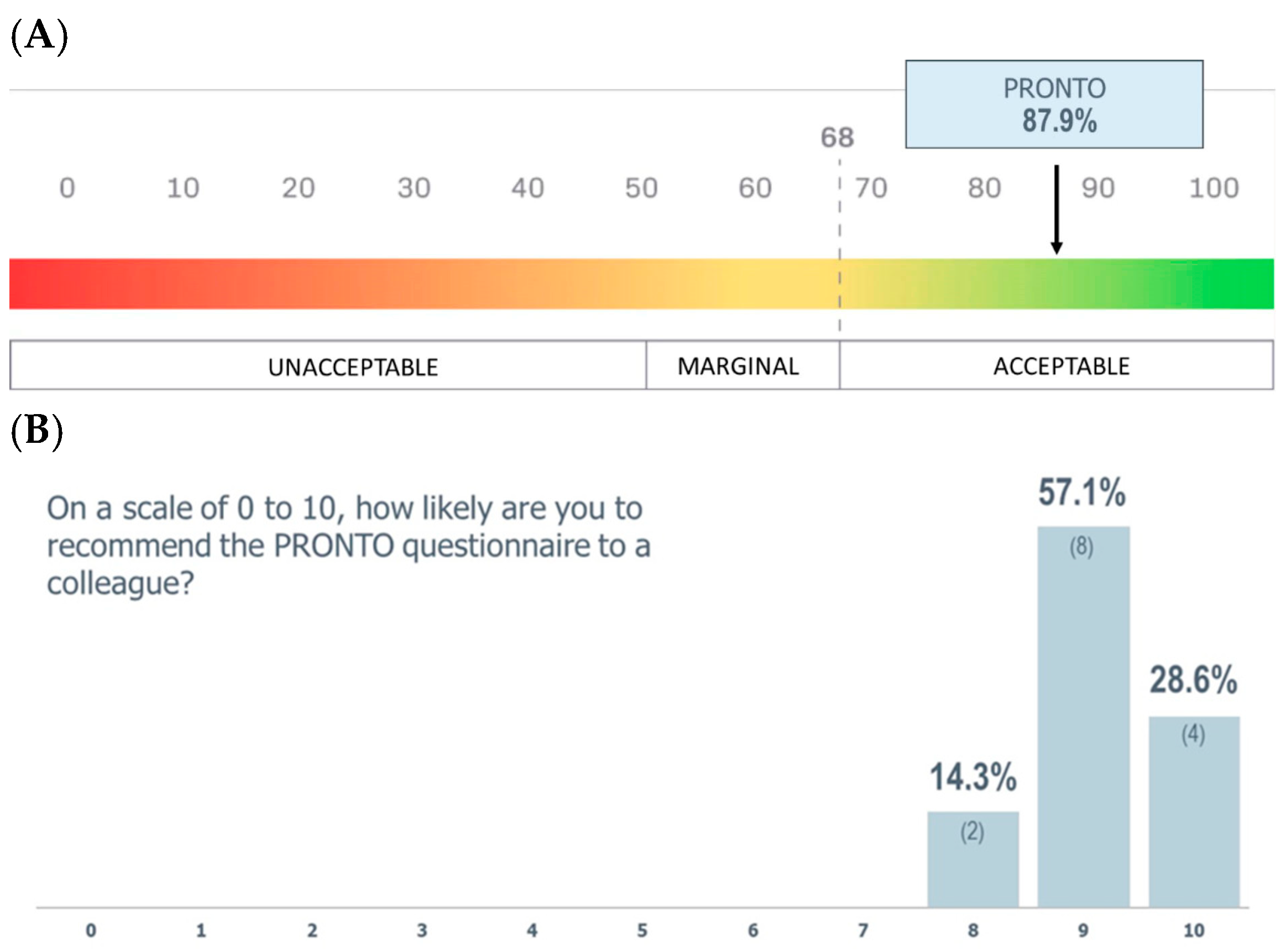
3.1. PRONTO Feasibility
3.2. Patient Results
4. Discussion
4.1. Malnutrition Is Present Among Oncology Outpatients at Initial Consultation Visits
4.2. PRONTO Is Simple to Screen for Malnutrition and Streamline Nutrition Care
4.3. Incorporating Nutritional Risk Screening as Part of Nutrition-Focused Quality Improvement Programs
4.4. Strengths
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Q.; Zhang, K.-P.; Zhang, X.; Tang, M.; Song, C.-H.; Cong, M.-H.; Guo, Z.-Q.; Ding, J.-S.; Braga, M.; Cederholm, T.; et al. Scored-GLIM as an effective tool to assess nutrition status and predict survival in patients with cancer. Clin. Nutr. 2021, 40, 4225–4233. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, E.S.; López-Aliaga, I.; Alferez, M. Cribado nutricional en pacientes oncológicos: Análisis de tres métodos [Analysis of three methods of nutritional screening in oncologic patients]. Nutr. Hosp. 2018, 3, 35. [Google Scholar] [CrossRef] [PubMed]
- de Las Peñas, R.; Majem, M.; Perez-Altozano, J.; Virizuela, J.A.; Cancer, E.; Diz, P.; Donnay, O.; Hurtado, A.; Jimenez-Fonseca, P.; Ocon, M.J. SEOM clinical guidelines on nutrition in cancer patients (2018). Clin. Transl. Oncol. 2019, 21, 87–93. [Google Scholar] [CrossRef]
- Planas, M.; Álvarez-Hernández, J.; León-Sanz, M.; Celaya-Pérez, S.; Araujo, K.; García de Lorenzo, A. Prevalence of hospital malnutrition in cancer patients: A sub-analysis of the PREDyCES® study. Support. Care Cancer 2016, 24, 429–435. [Google Scholar] [CrossRef]
- Hébuterne, X.; Lemarié, E.; Michallet, M.; de Montreuil, C.B.; Schneider, S.M.; Goldwasser, F. Prevalence of Malnutrition and Current Use of Nutrition Support in Patients With Cancer. J. Parenter. Enter. Nutr. 2014, 38, 196–204. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Lucia, S.; Farcomeni, A.; Lorusso, V.; Saracino, V.; Barone, C.; Plastino, F.; Gori, S.; Magarotto, R.; Carteni, G.; et al. Prevalence of malnutrition in patients at first medical oncology visit: The PreMiO study. Oncotarget 2017, 8, 79884–79896. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.; Muscaritoli, M.; Bourdel-Marchasson, I.; Kubrak, C.; Laird, B.; Gagnon, B.; Chasen, M.; Gioulbasanis, I.; Wallengren, O.; Voss, A.C.; et al. Diagnostic criteria for cancer cachexia: Reduced food intake and inflammation predict weight loss and survival in an international, multi-cohort analysis. J. Cachexia Sarcopenia Muscle 2021, 12, 1189–1202. [Google Scholar] [CrossRef]
- Marceca, G.P.; Londhe, P.; Calore, F. Management of Cancer Cachexia: Attempting to Develop New Pharmacological Agents for New Effective Therapeutic Options. Front. Oncol. 2020, 10, 298. [Google Scholar] [CrossRef]
- Ryan, A.M.; Prado, C.M.; Sullivan, E.S.; Power, D.G.; Daly, L.E. Effects of weight loss and sarcopenia on response to chemotherapy, quality of life, and survival. Nutrition 2019, 67–68, 110539. [Google Scholar] [CrossRef]
- Ryan, A.M.; Power, D.G.; Daly, L.; Cushen, S.J.; Ní Bhuachalla, E.; Prado, C.M. Cancer-associated malnutrition, cachexia and sarcopenia: The skeleton in the hospital closet 40 years later. Proc. Nutr. Soc. 2016, 75, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Imbimbo, G.; Jager-Wittenaar, H.; Cederholm, T.; Rothenberg, E.; di Girolamo, F.G.; Amabile, M.I.; Sealy, M.; Schneider, S.; Barazzoni, R.; et al. Disease-related malnutrition with inflammation and cachexia. Clin. Nutr. 2023, 42, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Muscaritoli, M.; Bar-Sela, G.; Battisti, N.M.L.; Belev, B.; Contreras-Martínez, J.; Cortesi, E.; de Brito-Ashurst, I.; Prado, C.M.; Ravasco, P.; Yalcin, S. Oncology-Led Early Identification of Nutritional Risk: A Pragmatic, Evidence-Based Protocol (PRONTO). Cancers 2023, 15, 380. [Google Scholar] [CrossRef] [PubMed]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Corsaro, E.; Molfino, A. Awareness of Cancer-Related Malnutrition and Its Management: Analysis of the Results From a Survey Conducted Among Medical Oncologists. Front. Oncol. 2021, 11, 682999. [Google Scholar] [CrossRef]
- Suárez-Llanos, J.P.; Vera-García, R.; Contreras-Martinez, J. The Determination of a Consensus Nutritional Approach for Cancer Patients in Spain Using the Delphi Methodology. Nutrient 2022, 14, 1404. [Google Scholar] [CrossRef] [PubMed]
- Segura, A.; Pardo, J.; Jara, C.; Zugazabeitia, L.; Carulla, J.; Peñas, R.d.L.; García-Cabrera, E.; Azuara, M.L.; Casadó, J.; Gómez-Candela, C. An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin. Nutr. 2005, 24, 801–814. [Google Scholar] [CrossRef]
- Stratton, R.J.; Hackston, A.; Longmore, D.; Dixon, R.; Price, S.; Stroud, M.; King, C.; Elia, M. Malnutrition in hospital outpatients and inpatients: Prevalence, concurrent validity and ease of use of the “malnutrition universal screening tool” (‘MUST’) for adults. Br. J. Nutr. 2004, 92, 799–808. [Google Scholar] [CrossRef]
- Kondrup, J.; Ramussen, H.H.; Hamberg, O.; Stanga, Z.; Camilo, M.; Richardson, R. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Ferguson, M.; Capra, S.; Bauer, J.; Banks, M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999, 15, 458–464. [Google Scholar] [CrossRef]
- Zhang, X.; Tang, M.; Zhang, Q.; Zhang, K.P.; Guo, Z.Q.; Xu, H.X.; Yuan, K.T.; Yu, M.; Braga, M.; Cederholm, T.; et al. The GLIM criteria as an effective tool for nutrition assessment and survival prediction in older adult cancer patients. Clin. Nutr. 2021, 40, 1224–1232. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 10, 207–217. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.R.; Kaplan, C.P.; Squiers, L.B.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Sevilla-Gonzalez, M.D.R.; Loaeza, L.M.; Lazaro-Carrera, L.S.; Ramirez, B.B.; Rodríguez, A.V.; Peralta-Pedrero, M.L.; Almeda-Valdes, P. Spanish Version of the System Usability Scale for the Assessment of Electronic Tools: Development and Validation. JMIR Hum. Factors 2020, 7, e21161. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A “Quick and Dirty” Usability Scale. In Usability Evaluation in Industry; CRC Press: Boca Raton, FL, USA, 1996; Volume 189, pp. 4–7. [Google Scholar]
- ECOG Performance Status Scale—ECOG-ACRIN Cancer Research Group. Available online: https://ecog-acrin.org/resources/ecog-performance-status/ (accessed on 1 April 2024).
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicology and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. Cancer Clin. Trials 1982, 5, 649–655. [Google Scholar]
- Muscaritoli, M.; Modena, A.; Valerio, M.; Marchetti, P.; Magarotto, R.; Quadrini, S.; Narducci, F.; Tonini, G.; Grassani, T.; Cavanna, L.; et al. The Impact of NUTRItional Status at First Medical Oncology Visit on Clinical Outcomes: The NUTRIONCO Study. Cancers 2023, 15, 3206. [Google Scholar] [CrossRef]
- Gellrich, N.-C.; Handschel, J.; Holtmann, H.; Krüskemper, G. Oral cancer malnutrition impacts weight and quality of life. Nutrients 2015, 7, 2145–2160. [Google Scholar] [CrossRef] [PubMed]
- Bolte, F.J.; McTavish, S.; Wakefield, N.; Shantzer, L.; Hubbard, C.; Krishnaraj, A.; Novicoff, W.; Gentzler, R.D.; Hall, R.D. Association of sarcopenia with survival in advanced NSCLC patients receiving concurrent immunotherapy and chemotherapy. Front. Oncol. 2022, 12, 986236. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Hu, X.; Xie, L.; Zhang, L.; Zhou, J.; Lin, J.; Wang, Y.; Li, Y.; Han, Z.; Zhang, D.; et al. Screening Sarcopenia in Community-Dwelling Older Adults: SARC-F vs. SARC-F Combined With Calf Circumference (SARC-CalF). J. Am. Med. Dir. Assoc. 2018, 19, 277.e1–277.e8. [Google Scholar] [CrossRef]
- Chen, L.; Qi, Y.; Kong, X.; Su, Z.; Wang, Z.; Wang, X.; Du, Y.; Fang, Y.; Li, X.; Wang, J. Nutritional Risk Index Predicts Survival in Patients With Breast Cancer Treated With Neoadjuvant Chemotherapy. Front. Nutr. 2022, 8, 786742. [Google Scholar] [CrossRef]
- Bossi, P.; Delrio, P.; Mascheroni, A.; Zanetti, M. The Spectrum of Malnutrition/Cachexia/Sarcopenia in Oncology According to Different Cancer Types and Settings: A Narrative Review. Nutrients 2021, 13, 1980. [Google Scholar] [CrossRef]
- Zhang, Z.; Wan, Z.; Zhu, Y.; Zhang, L.; Zhang, L.; Wan, H. Prevalence of malnutrition comparing NRS2002, MUST, and PG-SGA with the GLIM criteria in adults with cancer: A multi-center study. Nutrition 2021, 83, 111072. [Google Scholar] [CrossRef] [PubMed]
- Steer, B.; Loeliger, J.; Edbrooke, L.; Deftereos, I.; Laing, E.; Kiss, N. Malnutrition Prevalence according to the GLIM Criteria in Head and Neck Cancer Patients Undergoing Cancer Treatment. Nutrients 2020, 12, 3493. [Google Scholar] [CrossRef] [PubMed]
- Matsui, R.; Rifu, K.; Watanabe, J.; Inaki, N.; Fukunaga, T. Meta-analyses Impact of malnutrition as defined by the GLIM criteria on treatment outcomes in patients with cancer: A systematic review and meta-analysis. Clin. Nutr. 2023, 42, 615–624. [Google Scholar] [CrossRef]
- Xu, J.; Jie, Y.; Sun, Y.; Gong, D.; Fan, Y. Association of Global Leadership Initiative on Malnutrition with survival outcomes in patients with cancer: A systematic review and meta-analysis. Clin. Nutr. 2022, 41, 1874–1880. [Google Scholar] [CrossRef] [PubMed]
- Gersely, G.D.; Klein, R.C.M.; Rocha, G.D.G.V.d.; Bruzaca, W.F.d.S.; Ribeiro, L.M.K.; Santos, B.C.; de Almeida, M.M.F.A.; Junior, J.M.S.; Correia, M.I.T.D.; Waitzberg, D.L.; et al. GLIM criteria validation and reliability in critically ill patients with cancer: A prospective study. JPEN J. Parenter. Enter. Nutr. 2024, 48, 726–734. [Google Scholar] [CrossRef]
- Rasschaert, M.; Vandecandelaere, P.; Marechal, S.; D’hOndt, R.; Vulsteke, C.; Mailleux, M.; De Roock, W.; Van Erps, J.; Himpe, U.; De Man, M.; et al. Malnutrition prevalence in cancer patients in Belgium: The ONCOCARE study. Support. Care Cancer 2024, 32, 135. [Google Scholar] [CrossRef]
- Bian, W.; Li, Y.; Wang, Y.; Chang, L.; Deng, L.; Li, Y.; Jiang, H.; Zhou, P. Prevalence of malnutrition based on global leadership initiative in malnutrition criteria for completeness of diagnosis and future risk of malnutrition based on current malnutrition diagnosis: Systematic review and meta-analysis. Front. Nutr. 2023, 10, 1174945. [Google Scholar] [CrossRef]
- Huo, Z.; Chong, F.; Yin, L.; Li, N.; Liu, J.; Zhang, M.; Guo, J.; Fan, Y.; Zhang, L.; Lin, X.; et al. Comparison of the performance of the GLIM criteria, PG-SGA and mPG-SGA in diagnosing malnutrition and predicting survival among lung cancer patients: A multicenter study. Clin. Nutr. 2023, 42, 1048–1058. [Google Scholar] [CrossRef]
- Gascón-Ruiz, M.; Casas-Deza, D.; Torres-Ramón, I.; Zapata-García, M.; Alonso, N.; Sesma, A.; Lambea, J.; Álvarez-Alejandro, M.; Quílez, E.; Isla, D.; et al. Comparation of different malnutrition screening tools according to GLIM criteria in cancer outpatients. Eur. J. Clin. Nutr. 2022, 76, 698–702. [Google Scholar] [CrossRef]
- de Miranda, B.L.G.; Silva, F.M.; de Sousa, I.M.; Bertuleza, L.N.; Xavier, J.G.; Rüegg, R.A.B.; Gonzalez, M.C.; Fayh, A.P.T. Complementarity of nutrition risk screening tools with malnutrition diagnosis in patients with cancer: A 12-month follow-up study assessing accuracy metrics and mortality. Nutr. Clin. Pract. 2025, 40, 1166–1177. [Google Scholar] [CrossRef]
- Arensberg, M.B.; Sulo, S.; Drawert, S. Addressing Malnutrition in Cancer Care with Nutrition-Focused Quality Improvement Programs (QIPs) that Support Value-based Payment in the United States. J. Clin. Nutr. Food Sci. 2020, 3, 48–55. [Google Scholar]
- Arensberg, M.B.; Richards, J.; Benjamin, J.; Kerr, K.; Hegazi, R. Opportunities for quality improvement programs (QIPs) in the nutrition support of patients with cancer. Healthcare 2020, 8, 227. [Google Scholar] [CrossRef]
- Hong, K.; Sulo, S.; Wang, W.; Kim, S.; Huettner, L.; Taroyan, R.; Kerr, K.W.; Kaloostian, C. Nutrition Care for Poorly Nourished Outpatients Reduces Resource Use and Lowers Costs. J. Prim. Care Community Health 2021, 12, 21501327211017014. [Google Scholar] [CrossRef] [PubMed]
- Sriram, K.; Sulo, S.; VanDerBosch, G.; Partridge, J.; Feldstein, J.; Hegazi, R.A.; Summerfelt, W.T. A comprehensive nutrition-focused quality improvement program reduces 30-day readmissions and length of stay in hospitalized patients. J. Parenter. Enter. Nutr. 2017, 41, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Gomez, G.; Botero-Rodríguez, F.; Misas, J.D.; Garcia-Cifuentes, E.; Sulo, S.; Brunton, C.; Venegas-Sanabria, L.C.; Gracia, D.A.; Gutierrez, C.A.C. A nutritionally focused program for community-living older adults resulted in improved health and well-being. Clin. Nutr. 2022, 41, 1549–1556. [Google Scholar] [CrossRef] [PubMed]
- Chavarro-Carvajal, D.A.; Ayala, A.M.; Venegas-Sanabria, L.C.; Gomez, G.; Sulo, S.; Misas, J.D.; Cano-Gutiérrez, C. Use of a nutrition-focused quality improvement program for community-living older adults at malnutrition risk is associated with better nutritional outcomes. Clin. Nutr. ESPEN 2022, 48, 291–297. [Google Scholar] [CrossRef]
| Age, Mean ± SD | 65.3 ± 12.8 |
|---|---|
| Sex, % (n) | |
| Male | 49.5 (99/200) |
| Female | 50.5 (101/200) |
| Cancer Type, % (n) | |
| Lung | 34.5 (69/200) |
| Colon and Rectal | 22.5 (45/200) |
| Breast | 7.5 (15/200) |
| Head and Neck | 7.0 (14/200) |
| Gastric | 4.5 (9/200) |
| Bladder | 4.0 (8/200) |
| Kidney | 3.5 (7/200) |
| Other Cancers | 16.5 (33/200) |
| Cancer Stage, % (n) | |
| 0 | 3.0 (6/200) |
| I | 11.0 (22/200) |
| II | 17.0 (34/200) |
| III | 24.5 (49/200) |
| IV | 44.5 (89/200) |
| ECOG Performance Status, % (n) | |
| 0 | 59.5 (119/200) |
| 1 | 30.0 (60/200) |
| 2 | 6.5 (13/200) |
| 3 | 3.5 (7/200) |
| 4 | 0.5 (1/200) |
| Lung | Colon and Rectum | Breast | Head and Neck | Gastric | Bladder | kidney | Others | |
|---|---|---|---|---|---|---|---|---|
| Cancer Stage n = 200 | ||||||||
| 0 n = 6 | 0 (0/69) | 2.2 (1/45) | 20 (3/15) | 7.1 (1/14) | 11.1 (1/9) | 0 (0/8) | 0 (0/4) | 0 (0/33) |
| I n = 22 | 8.7 (6/69) | 4.4 (2/45) | 33.3 (5/15) | 14.3 (2/14) | 0 (0/9) | 0 (0/8) | 14.3 (1/4) | 18.2 (6/33) |
| II n = 34 | 7.2 (5/69) | 28.9 (13/45) | 13.3 (2/15) | 28.6 (4/14) | 22.2 (2/9) | 37.5 (3/8) | 14.3 (1/4) | 12.1 (4/33) |
| III n = 49 | 15.9 (11/69) | 42.2 (19/45) | 13.3 (2/15) | 28.6 (4/14) | 44.4 (4/9) | 25 (2/8) | 14.3 (1/4) | 18.2 (6/33) |
| IV n = 89 | 68.1 (47/69) | 22.2 (10/45) | 20 (3/15) | 21.4 (3/14) | 22.2 (2/9) | 37.5 (3/8) | 57.1 (4/4) | 51.5 (17/33) |
| 1 Body Weight Loss | 2 Appetite and Food Intake | 3 Strength and Mobility | |
|---|---|---|---|
| Overall n = 200 | 48.0 (96/200) | 42.0 (84/200) | 42.5 (85/200) |
| Cancer Type n = 200 | |||
| Lung n = 69 | 32.3 (31/96) | 35.7 (30/84) | 38.8 (33/85) |
| Colon and Rectal n = 45 | 27.1 (26/96) | 19.0 (16/84) | 17.6 (15/85) |
| Breast n = 15 | 3.1 (3/96) | 1.2 (1/84) | 3.5 (3/85) |
| Head and Neck n = 14 | 5.2 (5/96) | 8.3 (7/84) | 4.7 (4/85) |
| Gastric n = 9 | 9.4 (9/96) | 9.5 (8/84) | 7.1 (6/85) |
| Bladder n = 8 | 2.1 (2/96) | 3.6 (3/84) | 3.5 (3/85) |
| Kidney n = 7 | 5.2 (5/96) | 4.8 (4/84) | 4.7 (4/85) |
| Other Cancers n = 33 | 15.6 (15/96) | 17.9 (15/84) | 20.0 (17/85) |
| Cancer Stage n = 200 | |||
| 0 n = 6 | 1.0 (1/96) | 1.2 (1/84) | 0.0 (0/85) |
| I n = 22 | 8.3 (8/96) | 8.3 (7/84) | 8.2 (7/85) |
| II n = 34 | 18.8 (18/96) | 19.0 (16/84) | 14.1 (12/85) |
| III n = 49 | 19.8 (19/96) | 17.9 (15/84) | 15.3 (13/85) |
| IV n = 89 | 52.1 (50/96) | 53.6 (45/84) | 62.4 (53/85) |
| ECOG Performance Status n = 200 | |||
| 0 n = 119 | 52.1 (50/96) | 45.2 (38/84) | 37.6 (32/85) |
| 1 n = 60 | 36.5 (35/96) | 39.3 (33/84) | 43.5 (37/85) |
| 2 n = 13 | 7.3 (7/96) | 9.5 (8/84) | 12.9 (11/85) |
| 3 n = 7 | 4.2 (4/96) | 4.8 (4/84) | 5.9 (5/85) |
| 4 n = 1 | 0.0 (0/96) | 1.2 (1/84) | 0.0 (0/85) |
| Malnutrition | Moderate Malnutrition | Severe Malnutrition | |
|---|---|---|---|
| Overall n = 200 | 57.0 (114/200) | 76.3 (87/114) | 23.7 (27/114) |
| Cancer Type n = 200 | |||
| Lung n = 69 | 58.0 (40/69) | 72.5 (29/40) | 27.5 (11/40) |
| Colon and Rectal n = 45 | 62.2. (28/45) | 89.3 (25/28) | 10.7 (3/28) |
| Breast n = 15 | 26.7 (4/15) | 100.0 (4/4) | 0.0 (0/4) |
| Head and Neck n = 14 | 42.9 (6/14) | 83.3 (5/6) | 16.7 (1/6) |
| Gastric n = 9 | 100.0 (9/9) | 77.8 (7/9) | 22.2 (2/9) |
| Bladder n = 8 | 50 (4/8) | 75.0 (3/4) | 25.0 (1/4) |
| Kidney n = 7 | 85.7 (6/7) | 100.0 (6/6) | 0 (0/6) |
| Other Cancers n = 33 | 51.5 (17/33) | 47.1 (8/17) | 52.9 (9/17) |
| Cancer Stage n = 200 | |||
| 0 n = 6 | 16.7 (1/6) | 100.0 (1/1) | 0.0 (0/1) |
| I n = 22 | 36.4 (8/22) | 75.0 (6/8) | 25.0 (2/8) |
| II n = 34 | 52.9 (18/34) | 77.8 (14/18) | 22.2 (4/18) |
| III n = 49 | 46.9 (23/49) | 95.7 (22/23) | 4.3 (1/23) |
| IV n = 89 | 71.9 (64/89) | 68.8 (44/64) | 31.3 (20/64) |
| ECOG Performance Status n = 200 | |||
| 0 n = 119 | 47.1 (56/119) | 82.1 (46/56) | 17.9 (10/56) |
| 1 n = 60 | 70.0 (42/60) | 73.8 (31/42) | 26.2 (11/42) |
| 2 n = 13 | 76.9 (10/13) | 60.0 (6/10) | 40.0 (4/10) |
| 3 n = 7 | 71.4 (5/7) | 60.0 (3/5) | 40.0 (2/5) |
| 4 n = 1 | 100.0 (1/1) | 100.0 (1) | 0.0 (0/1) |
| Body Weight Loss (BWL) | Appetite and Food Intake (AFI) | Strength and Mobility (SM) | GLIM Diagnosis, % (n) | No GLIM Diagnosis, % (n) | ||
|---|---|---|---|---|---|---|
| All 3 | 24.5 (49/200) | YES | YES | YES | 42.1 (48/114) | 1.2 (1/86) |
| BWL + AFI | 9.5 (19/200) | YES | YES | NO | 16.7 (19/114) | 0.0 (0/86) |
| BWL + SM | 7.5 (15/200) | YES | NO | YES | 13.2 (15/114) | 0.0 (0/86) |
| BWL Only | 6.5 (13/200) | YES | NO | NO | 7.0 (8/114) | 5.8 (5/86) |
| AFI Only | 3.5 (7/200) | NO | YES | NO | 1.8 (2/114) | 5.8 (5/86) |
| SM Only | 6.0 (12/200 | NO | NO | YES | 6.1 (7/114) | 5.8 (5/86) |
| AFI + SM | 4.5 (9/200) | NO | YES | YES | 3.5 (4/114) | 5.8 (5/86) |
| None | 38.0 (76/200) | NO | NO | NO | 9.6 (11/114) | 75.6 (65/86) |
| Totals | 100.0 (200/200) | 48.0 (96/200) | 42.0 (84/200) | 42.5 (85/200) | 57.0 (114/200) | 43.0 (86/200) |
| All Malnutrition n = 114 | Moderate Malnutrition n = 87 | Severe Malnutrition n = 27 | |
|---|---|---|---|
| Clinical Nutrition Consultation Only | 2.6 (3/114) | 2.3 (2/87) | 3.7 (1/27) |
| ONS Only | 51.8 (59/114) | 55.2 (48/87) | 40.7 (11/27) |
| Clinical Nutrition Consultation + ONS | 18.4 (21/114) | 14.9 (13/87) | 29.6 (8/27) |
| No Nutritional Intervention | 27.2 (31/114) | 27.6 (24/87) | 25.9 (7/27) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Cabrero, D.; Rubio, J.; Durá Esteve, J.; Guzmán-Gómez, L.; Guzmán-Rolo, G.; Grande, C.; Martín Aguilar, A.; Pérez-Wert, P.; Pertejo, A.; Sulo, S.; et al. Feasibility and Acceptability of the Cancer-Specific PRONTO Protocol for Nutritional Risk Screening in Outpatient Oncology Cancer Care: A Pilot Study. Cancers 2025, 17, 3697. https://doi.org/10.3390/cancers17223697
Sánchez-Cabrero D, Rubio J, Durá Esteve J, Guzmán-Gómez L, Guzmán-Rolo G, Grande C, Martín Aguilar A, Pérez-Wert P, Pertejo A, Sulo S, et al. Feasibility and Acceptability of the Cancer-Specific PRONTO Protocol for Nutritional Risk Screening in Outpatient Oncology Cancer Care: A Pilot Study. Cancers. 2025; 17(22):3697. https://doi.org/10.3390/cancers17223697
Chicago/Turabian StyleSánchez-Cabrero, Darío, Jaime Rubio, Jorge Durá Esteve, Laura Guzmán-Gómez, Germán Guzmán-Rolo, Cristina Grande, Andrea Martín Aguilar, Pablo Pérez-Wert, Ana Pertejo, Suela Sulo, and et al. 2025. "Feasibility and Acceptability of the Cancer-Specific PRONTO Protocol for Nutritional Risk Screening in Outpatient Oncology Cancer Care: A Pilot Study" Cancers 17, no. 22: 3697. https://doi.org/10.3390/cancers17223697
APA StyleSánchez-Cabrero, D., Rubio, J., Durá Esteve, J., Guzmán-Gómez, L., Guzmán-Rolo, G., Grande, C., Martín Aguilar, A., Pérez-Wert, P., Pertejo, A., Sulo, S., Sharn, A. R., Palma Milla, S., Dassen, C., & Muscaritoli, M. (2025). Feasibility and Acceptability of the Cancer-Specific PRONTO Protocol for Nutritional Risk Screening in Outpatient Oncology Cancer Care: A Pilot Study. Cancers, 17(22), 3697. https://doi.org/10.3390/cancers17223697






