Expanding Cancer Prevention: Strategies Integrated into Occupational Health Surveillance
Simple Summary
Abstract
1. Introduction
2. The Role of the Occupational Physician on Population Health
3. Avoidable Cancers Prevention
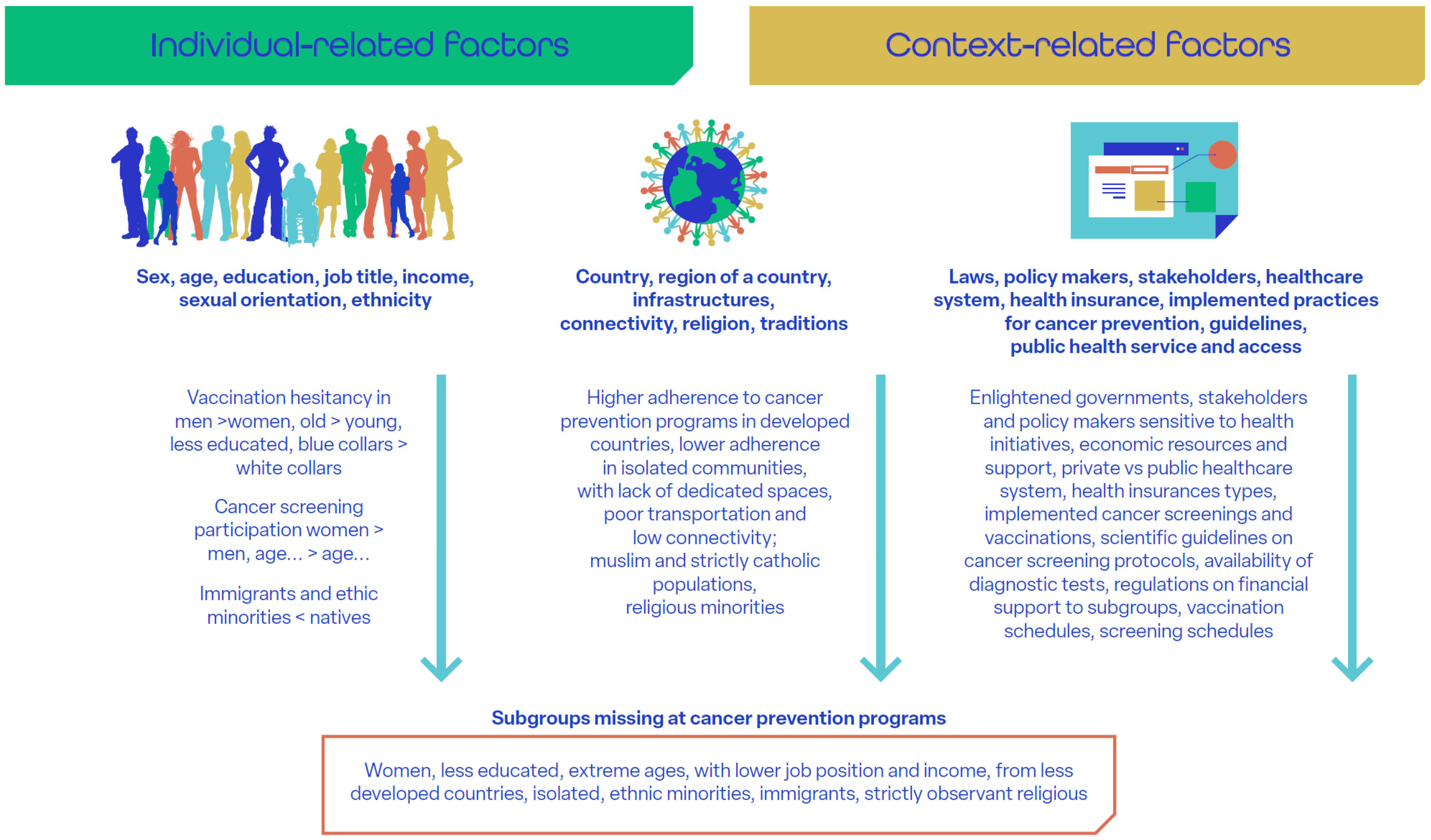
4. Social Determinants of Health and Cancer Prevention Disparities
5. The Workplace as a Setting for Cancer Prevention Programs
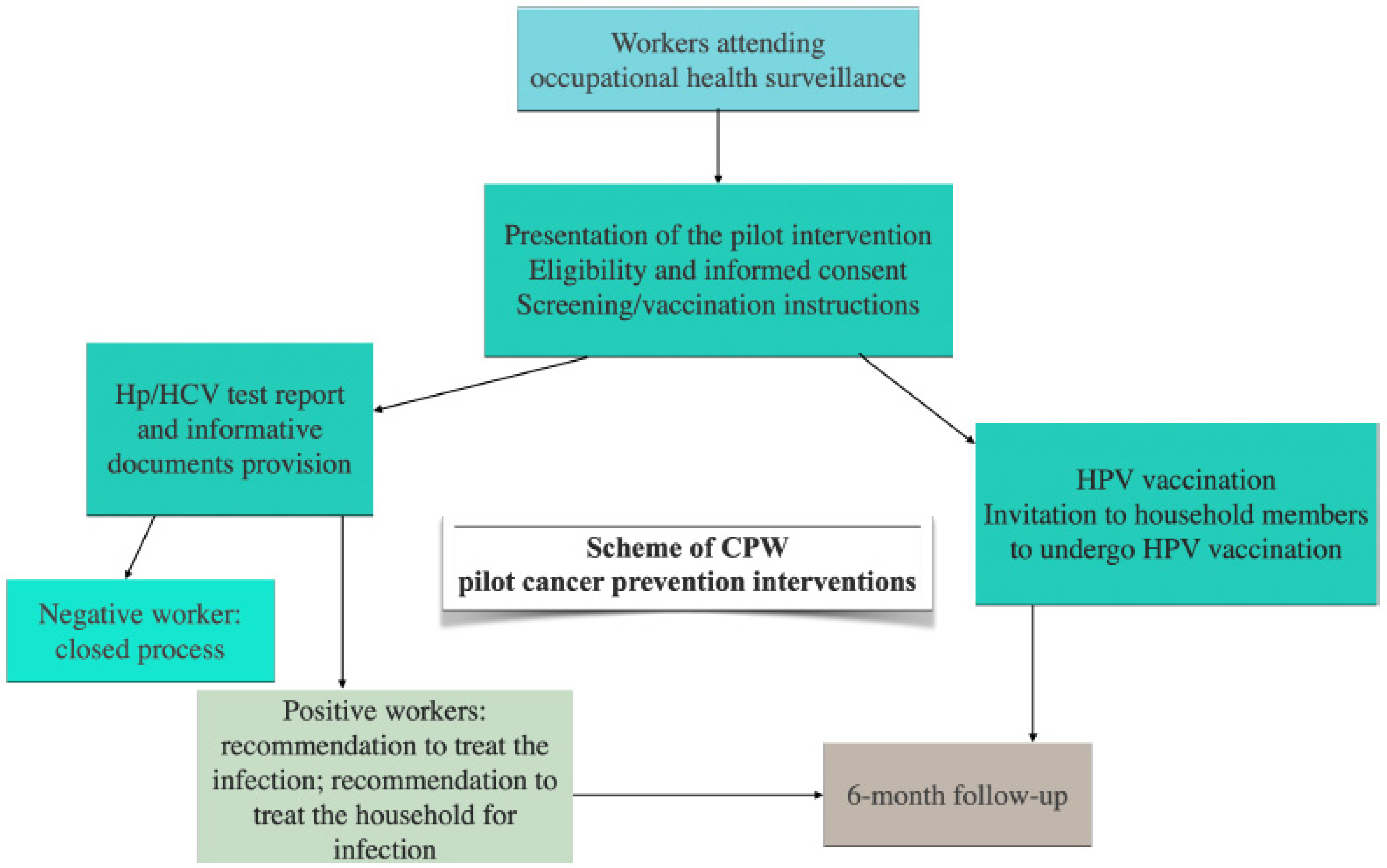
6. Integrating Cancer Prevention in Occupational Health Surveillance
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CPW | Cancer Prevention at Work |
| CSR | Corporate Social Responsibility |
| ECIS | European Cancer Information System |
| ENWHP | European Network for Workplace Health Promotion |
| EU | European Union |
| GP | General Practitioner |
| HBV | Hepatitis B Virus |
| HCV | Hepatitis C Virus |
| HPV | Human Papillomavirus |
| NIOSH | National Institute for Occupational Safety and Health |
| OHS | Occupational Health Surveillance |
| TWH | Total Worker Health |
References
- Lippman, S.M.; Hawk, E.T. Cancer prevention: From 1727 to milestones of the past 100 years. Cancer Res. 2009, 69, 5269–5284. [Google Scholar] [CrossRef]
- Bauer, U.E.; Briss, P.A.; Goodman, R.A.; Bowman, B.A. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Angelini, M.; Collatuzzo, G.; Teglia, F.; Sassano, M.; Siea, A.C.; Boffetta, P. The role of chance in cancer causation. Med. Lav. 2022, 113, e2022056. [Google Scholar] [CrossRef]
- Collatuzzo, G.; Boffetta, P. Cancers Attributable to Modifiable Risk Factors: A Road Map for Prevention. Annu. Rev. Public Health 2023, 44, 279–300. [Google Scholar] [CrossRef]
- GBD 2019 Cancer Risk Factors Collaborators. The global burden of cancer attributable to risk factors, 2010-19: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2022, 400, 563–591. [Google Scholar] [CrossRef]
- Dillner, J. Early detection and prevention. Mol. Oncol. 2019, 13, 591–598. [Google Scholar] [CrossRef]
- Greenwald, P.; Dunn, B.K. Do we make optimal use of the potential of cancer prevention? Recent Results Cancer Res. 2009, 181, 3–17. [Google Scholar]
- Chow, L.W.; Yip, A.Y.; Ng, E.L. Prevention of Oncological Diseases: Primary and Secondary Prevention. Int. J. Biol. Markers 2012, 27, 337–343. [Google Scholar] [CrossRef]
- Bizuayehu, H.M.; Ahmed, K.Y.; Kibret, G.D.; Dadi, A.F.; Belachew, S.A.; Bagade, T.; Tegegne, T.K.; Venchiarutti, R.L.; Kibret, K.T.; Hailegebireal, A.H.; et al. Global Disparities of Cancer and Its Projected Burden in 2050. JAMA Netw. Open 2024, 7, e2443198. [Google Scholar] [CrossRef]
- Hallgren, E.; Yeary, K.H.K.; DelNero, P.; Johnson-Wells, B.; Purvis, R.S.; Moore, R.; Loveless, S.; Shealy, K.; McElfish, P.A. Barriers, facilitators, and priority needs related to cancer prevention, control, and research in rural, persistent poverty areas. Cancer Causes Control 2023, 34, 1145–1155. [Google Scholar] [CrossRef]
- Pinsky, P.F. Principles of Cancer Screening. Surg. Clin. N. Am. 2015, 95, 953–966. [Google Scholar] [CrossRef]
- Lopez, A.M.; Hudson, L.; Vanderford, N.L.; Vanderpool, R.; Griggs, J.; Schonberg, M. Epidemiology and Implementation of Cancer Prevention in Disparate Populations and Settings. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 50–60. [Google Scholar] [CrossRef]
- Kaji, E.; Yoden, A.; Otani, M.; Okuhira, T.; Aomatsu, T.; Tamai, H.; Ashida, A. Helicobacter pylori test-and-treat strategy for second-year junior high school students aimed at the prevention of gastric cancer in Takatsuki City. Helicobacter 2020, 25, e12696. [Google Scholar] [CrossRef]
- Davies, C.; Stoney, T.; Hutton, H.; Parrella, A.; Kang, M.; Macartney, K.; Leask, J.; McCaffery, K.; Zimet, G.; Brotherton, J.M.; et al. School-based HPV vaccination positively impacts parents’ attitudes toward adolescent vaccination. Vaccine 2021, 39, 4190–4198. [Google Scholar] [CrossRef]
- Schoenberg, N.E.; Hatcher, J.; Dignan, M.B.; Shelton, B.; Wright, S.; Dollarhide, K.F. Faith Moves Mountains: An Appalachian cervical cancer prevention program. Am. J. Health Behav. 2009, 33, 627–638. [Google Scholar] [CrossRef]
- Matthews, A.K.; Steffen, A.D.; Kuhns, L.M.; Ruiz, R.A.; Ross, N.A.; Burke, L.A.; Li, C.C.; King, A.C. Evaluation of a Randomized Clinical Trial Comparing the Effectiveness of a Culturally Targeted and Nontargeted Smoking Cessation Intervention for Lesbian, Gay, Bisexual, and Transgender Smokers. Nicotine Tob. Res. 2018, 21, 1506–1516. [Google Scholar] [CrossRef]
- Reiter, P.L.; Katz, M.L.; Bauermeister, J.A.; Shoben, A.B.; Paskett, E.D.; McRee, A.-L. Increasing Human Papillomavirus Vaccination Among Young Gay and Bisexual Men: A Randomized Pilot Trial of the Outsmart HPV Intervention. LGBT Health 2018, 5, 325–329. [Google Scholar] [CrossRef]
- Birnbaum, J.A.; Guttman, D.; Parulekar, M.; Omarufilo, F.; Emeasoba, E.U.; Nguyen, J.; Tokunboh, O.; Coe, J.; Akiyama, M.J.; Sigal, S.H. Eliminating hepatitis B vaccination disparities for West African immigrants. Vaccine 2023, 41, 6255–6260. [Google Scholar] [CrossRef]
- Cox, J.E.; Bogart, L.M.; Elliott, M.N.; Starmer, A.J.; Meleedy-Rey, P.; Goggin, K.; Banerjee, T.; Samuels, R.C.; Hahn, P.D.; Epee-Bounya, A.; et al. Improving HPV Vaccination Rates in a Racially and Eth-nically Diverse Pediatric Population. Pediatrics 2022, 150, e2021054186. [Google Scholar] [CrossRef]
- Nahmias, Z.; Townsend, J.S.; Neri, A.; Stewart, S.L. Worksite Cancer Prevention Activities in the National Comprehensive Cancer Control Program. J. Community Health 2016, 41, 838–844. [Google Scholar] [CrossRef]
- Marshall, H. Workplace cancer screening. Lancet Oncol. 2013, 14, 694. [Google Scholar] [CrossRef]
- Mojica, C.M.; Morales-Campos, D.Y.; Carmona, C.M.; Ouyang, Y.; Liang, Y. Breast, cervical, and colorectal cancer education and navigation: Results of a community health worker intervention. Health Promot. Pract. 2016, 17, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.M.E.; Potter, M.B.; Arora, M.; Gildegorin, G.; Terdiman, J. A workplace colorectal cancer screening program in firefighters: Lessons learned. Occup. Med. 2014, 64, 255–258. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for Europe. Good Practice in Occupational Health Services: A Contribution to Workplace Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2002. [Google Scholar]
- GBD 2016 Occupational Carcinogens Collaborators. Global and regional burden of cancer in 2016 arising from occupational exposure to selected carcinogens: A systematic analysis for the Global Burden of Disease Study 2016. Occup. Environ. Med. 2020, 77, 151–159. [Google Scholar] [CrossRef]
- Technical and Ethical Guidelines for Workers’ Health Surveillance. 1998. Available online: https://eur-lex.europa.eu/legal-content/IT/TXT/?uri=CELEX%3A32004L0037 (accessed on 21 January 2025).
- Schill, A.L.; Chosewood, L.C. The NIOSH Total Worker Health™ program: An overview. J. Occup. Environ. Med. 2013, 55 (Suppl. S12), S8–11. [Google Scholar] [CrossRef]
- Mon, H.M.; Robb, K.A.; Demou, E. Effectiveness of workplace cancer screening interventions: A systematic review. BMC Cancer 2024, 24, 999. [Google Scholar] [CrossRef]
- Cancer Prevention at Work. Available online: https://cancerpreventionatwork.eu/ (accessed on 18 October 2025).
- Available online: https://www.eurofound.europa.eu/en/publications/2023/measures-tackle-labour-shortages-lessons-future-policy (accessed on 1 May 2025).
- Steel, J.S.; Godderis, L.; Luyten, J. Short-term effectiveness of face-to-face periodic occupational health screening versus electronic screening with targeted follow-up: Results from a quasi-randomized controlled trial in four Belgian hospitals. Scand. J. Work. Environ. Health 2022, 48, 220–228. [Google Scholar] [CrossRef]
- Eurostat (Undated): Self-Reported Time Elapsed Since Last Visit to a Medical Professional by Sex, Age and Educational Attainment Level, Online Data Code: Hlth_ehis_am1e. Available online: https://doi.org/10.2908/HLTH_EHIS_AM1E (accessed on 14 April 2025).
- Wyatt, S.; Mohammed, M.A.; de Dumast, L.; Marsall, T. Long-term trends in English general practice consultation rates from 1995 to 2021: A retrospective analysis of two electronic health records databases. BMJ Open 2024, 14, e088845. [Google Scholar] [CrossRef]
- Eurostat. How Often Do You See a Doctor? 2019. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20190225-1 (accessed on 14 April 2025).
- Reho, T.; Atkins, S.; Talola, N.; Sumanen, M.; Viljamaa, M.; Uitti, J. Comparing occasional and persistent frequent attenders in occupational health primary care—A longitudinal study. BMC Public Health 2018, 18, 1291. [Google Scholar] [CrossRef]
- Wolf, A.M.D.; Oeffinger, K.C.; Shih, T.Y.; Walter, L.C.; Church, T.R.; Fontham, E.T.H.; Elkin, E.B.; Etzioni, R.D.; Guerra, C.E.; Perkins, R.B.; et al. Screening for lung cancer: 2023 guideline update from the American Cancer Society. CA A Cancer J. Clin. 2023, 74, 50–81. [Google Scholar] [CrossRef]
- Loomans-Kropp, H.A.; Umar, A. Cancer prevention and screening: The next step in the era of precision medicine. npj Precis. Oncol. 2019, 3, 3. [Google Scholar] [CrossRef]
- de Boer, A.G.; Tamminga, S.J.; Boschman, J.S.; Hoving, J.L. Non-medical interventions to enhance return to work for people with cancer. Cochrane Database Syst. Rev. 2024, 2024, CD007569. [Google Scholar] [CrossRef]
- Farkas, A.H.; Nattinger, A.B. Breast Cancer Screening and Prevention. Ann. Intern. Med. 2023, 176, ITC161–ITC176. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Galiano-Castillo, N.; Cantarero-Villanueva, I.; Fernández-Lao, C.; Ariza-García, A.; Díaz-Rodríguez, L.; Del-Moral-Ávila, R.; Arroyo-Morales, M. Telehealth system: A randomized controlled trial evaluating the impact of an internet-based exercise intervention on quality of life, pain, muscle strength, and fatigue in breast cancer survivors. Cancer 2016, 122, 3166–3174. [Google Scholar] [CrossRef]
- Ladabaum, U.; Dominitz, J.A.; Kahi, C.; Schoen, R.E. Strategies for Colorectal Cancer Screening. Gastroenterology 2020, 158, 418–432. [Google Scholar] [CrossRef]
- Shah, S.C.; Wang, A.Y.; Wallace, M.B.; Hwang, J.H. AGA Clinical Practice Update on Screening and Surveillance in Individuals at Increased Risk for Gastric Cancer in the United States: Expert Review. Gastroenterology 2024, 168, 405–416.e1. [Google Scholar] [CrossRef]
- Simms, K.T.; Steinberg, J.; Caruana, M.; Smith, M.A.; Lew, J.-B.; Soerjomataram, I.; Castle, P.E.; Bray, F.; Canfell, K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–2099: A modelling study. Lancet Oncol. 2019, 20, 394–407. [Google Scholar] [CrossRef]
- Yang, J.D.; Hainaut, P.; Gores, G.J.; Amadou, A.; Plymoth, A.; Roberts, L.R. A global view of hepatocellular carcinoma: Trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 589–604. [Google Scholar] [CrossRef]
- Pinsky, P.F.; Parnes, H. Screening for Prostate Cancer. N. Eng. J. Med. 2023, 388, 1405–1414. [Google Scholar] [CrossRef]
- Schillie, S.; Vellozzi, C.; Reingold, A.; Harris, A.; Haber, P.; Ward, J.W.; Nelson, N.P. Prevention of Hepatitis B Virus Infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recomm. Rep. 2018, 67, 1–31. [Google Scholar] [CrossRef]
- Chang, M.-H.; You, S.-L.; Chen, C.-J.; Liu, C.-J.; Lai, M.-W.; Wu, T.-C.; Wu, S.-F.; Lee, C.-M.; Yang, S.-S.; Chu, H.-C.; et al. Long-term Effects of Hepatitis B Immunization of Infants in Preventing Liver Cancer. Gastroenterology 2016, 151, 472–480.e1. [Google Scholar] [CrossRef]
- Miyagi, E. Human papillomavirus (HPV) vaccination in Japan. J. Obstet. Gynaecol. Res. 2024, 50, 65–71. [Google Scholar] [CrossRef]
- Yagi, A.; Ueda, Y.; Oka, E.; Nakagawa, S.; Kimura, T. Human Papillomavirus Vaccination by Birth Fiscal Year in Japan. JAMA Netw. Open 2024, 7, e2422513. [Google Scholar] [CrossRef]
- IARC List of Classifications by Cancer Sites with Sufficient or Limited Evidence in Humans, IARC Monographs Volumes 1–137. Available online: https://monographs.iarc.who.int/wp-content/uploads/2019/07/Classifications_by_cancer_site.pdf (accessed on 21 January 2025).
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA A Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef]
- Ragelienė, T.; Schneider-Kamp, A.; Askegaard, S.T. Barriers and facilitators of prevention of infections related to cancer: A systematic lit-erature review. Heliyon 2024, 10, e37959. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Wong, L.P.; Wong, P.-F.; Hashim, M.M.A.A.M.; Han, L.; Lin, Y.; Hu, Z.; Zhao, Q.; Zimet, G.D. Multidimensional social and cultural norms influencing HPV vaccine hesitancy in Asia. Hum. Vaccines Immunother. 2020, 16, 1611–1622. [Google Scholar] [CrossRef]
- Sun, J.B.; Perraillon, M.C.; Myerson, R. The Impact of Medicare Health Insurance Coverage on Lung Cancer Screening. Med. Care 2021, 60, 29–36. [Google Scholar] [CrossRef]
- Collatuzzo, G.; Teglia, F.; Boffetta, P. Role of Occupation in Shaping Cancer Disparities. Cancers 2022, 14, 4259. [Google Scholar] [CrossRef]
- Kim, T.V.; Pham, T.N.; Le, D.H.; Dao, D.V.; Phan, L.T.; Le, A.; Trang, A.; Tang, H.K.; Liu, J.J.; Dao, D.Y. Significant gaps in hepatitis B vaccination in adults in Viet Nam: Important targets toward hepatitis B elimination by 2030. Vaccine 2023, 41, 976–988. [Google Scholar] [CrossRef]
- Van Kim, T.; Pham, T.N.D.; Do, B.; Dao, D.V.B.; Nguyen, D.X.; Lee, W.; Gish, R.; Mize, G.; Trang, A.; Le, A.; et al. Low HBV knowledge is associated with low HBV vaccination uptake in general adult population despite incentivization of HBV vaccination. BMC Infect. Dis. 2024, 24, 470. [Google Scholar] [CrossRef]
- Aoki, E.S.; Yin, R.; Li, K.; Bhatla, N.; Singhal, S.; Ocviyanti, D.; Saika, K.; Suh, M.; Kim, M.; Termrungruanglert, W. National screening programs for cervical cancer in Asian countries. J. Gynecol. Oncol. 2020, 31, e55. [Google Scholar] [CrossRef]
- Zhao, S.; Huang, L.; Basu, P.; Domingo, E.J.; Supakarapongkul, W.; Ling, W.Y.; Ocviyanti, D.; Rezhake, R.; Qiao, Y.; Tay, E.H.; et al. Cervical cancer burden, status of implementation and challenges of cervical cancer screening in Association of Southeast Asian Nations (ASEAN) countries. Cancer Lett. 2022, 525, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Jou, K.; Sterling, M.R.; Ramos, R.; Antoine, F.; Nanus, D.M.; Phillips, E. Eliciting the Social Determinants of Cancer Prevention and Control in the Catchment of an Urban Cancer Center. Ethn. Dis. 2021, 31, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Lee, H.Y.; An, S.; Yoon, Y.J.; Oh, J. Predictors of Cervical Cancer Screening Awareness and Literacy Among Korean-American Women. J. Racial Ethn. Health Disparities 2019, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rapkin, B.D.; Weiss, E.; Lounsbury, D.; Michel, T.; Gordon, A.; Erb-Downward, J.; Sabino-Laughlin, E.; Carpenter, A.; Schwartz, C.E.; Bulone, L.; et al. Reducing Disparities in Cancer Screening and Prevention through Community-Based Participatory Research Partnerships with Local Libraries: A Comprehensive Dynamic Trial. Am. J. Community Psychol. 2017, 60, 145–159. [Google Scholar] [CrossRef]
- Prevent Cancer Annual Gala to Celebrate Three Decades Commitment to Cancer Prevention and Early Detection. Available online: https://preventcancer.org/news/prevent-cancer-annual-cancer-prevention-early-detection/ (accessed on 4 December 2024).
- Collatuzzo, G.; Fiorini, G.; Vaira, B.; Violante, F.S.; Farioli, A.; Boffetta, P. The role of the occupational physician in controlling gastric cancer attributable to Helicobacter pylori infection: A review. Prev. Med. Rep. 2021, 24, 101527. [Google Scholar] [CrossRef]
- Fernandez-Tardon, G.; Gan, R.K.; Rodriguez-Suarez, M.-M.; Tardon, A.; Arcos-González, P. Total worker health® based Helicobacter pylori public health prevention strategy. Curr. Opin. Epidemiol. Public Health 2024, 3, 33–39. [Google Scholar] [CrossRef]
- Blacker, A.; Dion, S.; Grossmeier, J.; Hecht, R.; Markle, E.; Meyer, L.; Monley, S.; Sherman, B.; VanderHorst, N.; Wolfe, E. Social Determinants of Health—An Employer Priority. Am. J. Health Promot. 2020, 34, 207–215. [Google Scholar] [CrossRef]
- Song, F.; Bachmann, M.; Howe, A. Factors associated with the consultation of GPs among adults aged ≥16 years: An analysis of data from the Health Survey for England 2019. BJGP Open 2023, 7, BJGPO.2022.0177. [Google Scholar] [CrossRef]
- Baker, P. Missing persons? Men’s use of primary care services. Trends Urol. Men’s Health 2024, 15, 2–5. [Google Scholar] [CrossRef]
- Benavides, F.G.; Serra, C.; Delclos, G.L. What can public health do for the welfare state? Occupational health could be an answer. J. Epidemiol. Community Health 2019, 73, 1141–1144. [Google Scholar] [CrossRef]
- Thorndike, A.N.; McCurley, J.L.; Gelsomin, E.D.; Anderson, E.; Chang, Y.; Porneala, B.; Johnson, C.; Rimm, E.B.; Levy, D.E. Automated Behavioral Workplace Intervention to Prevent Weight Gain and Improve Diet: The ChooseWell 365 Randomized Clinical Trial. JAMA Netw Open. 2021, 4, e2112528. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Lu, E.Y.; Sun, W.; Chang, J.R.; Tsang, H.W.H. Effectiveness of interventions on sedentary behaviors in office workers: A systematic review and meta-analysis. Public Health 2024, 230, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Klein, W.M.P.; O’cOnnell, M.E.; Bloch, M.H.; Czajkowski, S.M.; Green, P.A.; Han, P.K.J.; Moser, R.P.; Nebeling, L.C.; Vanderpool, R.C. Behavioral Research in Cancer Prevention and Control: Emerging Challenges and Opportunities. J. Natl. Cancer Inst. 2021, 114, 179–186. [Google Scholar] [CrossRef]
- Symanzik, C.; John, S.M. Sun protection and occupation: Current developments and perspectives for prevention of occupational skin cancer. Front. Public Health 2022, 10, 1110158. [Google Scholar] [CrossRef]
- Stratil, J.; Rieger, M.A.; Voelter-Mahlknecht, S. Optimizing cooperation between general practitioners, occupational health and rehabilitation physicians in Germany: A qualitative study. Int. Arch. Occup. Environ. Health 2017, 90, 809–821. [Google Scholar] [CrossRef]
- Jiménez, P.; Bregenzer, A.; Kallus, K.W.; Fruhwirth, B.; Wagner-Hartl, V. Enhancing Resources at the Workplace with Health-Promoting Lead-ership. Int. J. Environ. Res. Public Health 2017, 14, 1264. [Google Scholar] [CrossRef]
- Price, W.N., II; Cohen, I.G. Privacy in the age of medical big data. Nat. Med. 2019, 25, 37–43. [Google Scholar] [CrossRef]
- Zusman, E.Z.; Kapanen, A.I.; Klaassen, A.; Reardon, J. Workplace cardiovascular risk reduction by healthcare professionals—A systematic review. Occup. Med. 2021, 71, 270–276. [Google Scholar] [CrossRef]
- Persechino, B.; Fontana, L.; Buresti, G.; Rondinone, B.M.; Laurano, P.; Fortuna, G.; Valenti, A.; Iavicoli, S. Collaboration of occupational physicians with national health system and general practitioners in Italy. Ind. Health 2017, 55, 180–191. [Google Scholar] [CrossRef]
- Steel, J.S.; Godderis, L.; Luyten, J. Disclosure in Online vs.Face-to-Face Occupational Health Screenings: A Cross-Sectional Study in Belgian Hospital Employees. Int. J. Environ. Res. Public Health 2021, 18, 1460. [Google Scholar] [CrossRef]
- Associazione Onconauti. Available online: https://onconauti.it/chi-siamo/ (accessed on 15 September 2025).
- Civilotti, C.; Lucchini, D.; Fogazzi, G.; Palmieri, F.; Benenati, A.; Buffoli, A.; Girardi, V.; Ruzzenenti, N.; Di Betta, A.; Donarelli, E.; et al. The role of integrated psychological support in breast cancer patients: A randomized monocentric prospective study evaluating the Fil-Rouge Integrated Psycho-Oncological Support (FRIPOS) program. Support. Care Cancer 2023, 31, 226. [Google Scholar] [CrossRef]
- Inbaraj, G.; Sathyaprabha, T.N.; Udupa, K.; Ram, A.; Patil, S.; Rajeswaran, J.; Nandakumar, K.K.; Belur, S.; Singh, A.D.; Prathyusha, P.V.; et al. Impact of integrated yoga therapy on cognitive impairment and cardiac dysfunction in relation to quality of life in breast cancer patients undergoing chemotherapy: Study protocol for a two-arm randomized controlled trial. Front. Oncol. 2022, 12, 955184. [Google Scholar] [CrossRef]
- Hanvey, G.A.; Kacel, E.L.; Bacharz, K.C.; Wilborn, A.P.; Mesa, S.; McCracken, H.; Estores, I.M.; Markham, M.-J.; Kaye, F.J.; Jones, D.; et al. Proof-of-Concept of an Integrated Yoga and Psychological Intervention in Mitigating Distress Among Diverse Women With Gynecologic, Gastrointestinal, and Thoracic Cancers. Integr. Cancer Ther. 2024, 23, 15347354241283113. [Google Scholar] [CrossRef] [PubMed]
- European Network for Workplace Health Promotion. Available online: https://www.enwhp.org/?i=portal.en.about (accessed on 18 October 2025).
- Recommendations for Promoting Workplace Health Actions–ENWHP. Available online: https://www.enwhp.org/resources/toolip/doc/2018/05/02/recommendations_for_promoting_wha_01.pdf (accessed on 18 October 2025).
- Sinelnikov, S.; Bixler, E.A.; Kolosh, A. Effectiveness of safety training interventions for supervisors: A systematic review and narrative synthesis. Am. J. Ind. Med. 2020, 63, 878–901. [Google Scholar] [CrossRef]
- Ryan, M.; Erck, L.; McGovern, L.; McCabe, K.; Myers, K.; Nobrega, S.; Li, W.; Lin, W.-C.; Punnett, L. “Working on Wellness:“ protocol for a worksite health promotion capacity-building program for employers. BMC Public Health 2019, 19, 111. [Google Scholar] [CrossRef]
- Rafie, C.L.; Hauser, L.; Michos, J.; Pinsky, J. Creating a Workplace Culture of Preventive Health: Process and Outcomes of the Colon Cancer–Free Zone at Virginia Cooperative Extension. J. Cancer Educ. 2019, 35, 1135–1140. [Google Scholar] [CrossRef]
- Nobrega, S.; Morocho, C.; Robertson, M.M.; Kurowski, A.; Rice, S.; Henning, R.A.; Punnett, L. A mixed-method approach to tailor the implementation of a participatory Total Worker Health® program. Int. J. Work. Health Manag. 2021, 14, 409–425. [Google Scholar] [CrossRef]
- Bollati, V.; Ferrari, L.; Leso, V.; Iavicoli, I. Personalised Medicine: Implication and perspectives in the field of occupational health. Med. Lav. 2020, 111, 425–444. [Google Scholar] [CrossRef]
- European Commission; COWI.; Directorate-General for Employment; Social Affairs and Inclusion; EPRD.; FoBIG.; RPA.; Garrett, S.; Vencovsky, D.; Collins, H. Study on Collecting Information on Substances with the View to Analyse Health, Socio-Economic and Environ-Mental Impacts in Connection with Possible Amendments of Directive 98/24/EC (Chemical Agents) and Directive 2009/148/EC (Asbestos)–Methodological Note and Data Collection Synopsis, Publications Office. 2021. Available online: https://data.europa.eu/doi/10.2767/734383 (accessed on 14 April 2025).
- Kim, J.Y.; Keane, A. Corporate social responsibility and performance in the workplace: A meta-analysis. Int. J. Educ. Vocat. Guid. 2023, 24, 781–807. [Google Scholar] [CrossRef]
- Velte, P. Meta-analyses on Corporate Social Responsibility (CSR): A literature review. Manag. Rev. Q 2021, 72, 627–675. [Google Scholar] [CrossRef]
- Paruzel, A.; Klug, H.J.P.; Maier, G.W. The Relationship Between Perceived Corporate Social Responsibility and Employee-Related Outcomes: A Meta-Analysis. Front. Psychol. 2021, 12, 607108. [Google Scholar] [CrossRef]
- European Commission; Directorate-General for Employment; Social Affairs and Inclusion. Socio-Economic Costs of Accidents at Work and Work-Related Ill Health–Final Report. 2011. Available online: https://ec.europa.eu/social/BlobServlet?docId=7416&langId=en (accessed on 14 April 2025).
- Eurostat: HICP-Annual Data (Average Index and Rate of Change). 2025. Available online: https://doi.org/10.2908/PRC_HICP_AIND (accessed on 14 April 2025).
- Leal, J.; Luengo-Fernandez, R.; Sullivan, R.; Witjes, J.A. Economic Burden of Bladder Cancer Across the European Union. Eur. Urol. 2016, 69, 438–447. [Google Scholar] [CrossRef]
- Hanly, P.; Ortega, M.O.; Pearce, A.; Cancela, M.d.C.; Soerjomataram, I.; Sharp, L. Estimating Global Friction Periods for Economic Evaluation: A Case Study of Selected OECD Member Countries. PharmacoEconomics 2023, 41, 1093–1101. [Google Scholar] [CrossRef]
- Reframe Cancer: The Employee Experience Report: Living and Working with Cancer. 2024. Available online: https://www.reframe.co.uk/blog/the-1.6-billion-cancer-absence-cost-to-uk-businesses-in-2024 (accessed on 14 April 2025).
- Goulart, K.; Oesch, D. Job tenure in Western Europe, 1993–2021: Decline or stability? Eur. J. Ind. Relat. 2024, 30, 329–346. [Google Scholar] [CrossRef]
- ECIS. ECIS—European Cancer Information System, Estimates of Cancer Incidence and Mortality, 2022, for All Countries; ECIS: Brussels, Belgium, 2025. [Google Scholar]
| Cancer Type | Main Modifiable Risk Factors | Prevention Strategy | OHS Contribution | References | ||
|---|---|---|---|---|---|---|
| Primary | Secondary | Tertiary | ||||
| Lung cancer | Smoking Second-hand smoke Occupational exposures | No smoking/stop smoking Avoid exposure to second-hand smoke Limit occupational exposures Use of PPE at the workplace | Low-dose CT | Rehabilitation programs Return to work programs Psychological support Nutritional counseling Promotion of physical activity and healthy lifestyle Smoking cessation Personalized support via telemedicine Sexual recovery | Occupational exposure limits PPE provision and check Quitting smoking counseling contact Risk profiling | Chow et al., 2012 [8]; Wolf et al., 2024 [36]; Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38] |
| Breast cancer | Obesity Low physical activity Alcohol No breastfeeding Reproductive factors | Promotion of healthy lifestyle and physical activity Health education at any age Promotion of breastfeeding | Mammography Breast ultrasound Mammotome Regular self-examination of the breast | Nutritional counseling Family history investigation Investigation and recommendation of screening and self-examination Physical activity indications Alcohol use investigation and education Recommendation of lifestyle changes Weight monitoring Risk profiling | Chow et al., 2012 [8]; Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38]; Farkas and Nattinger, 2023 [39]; Arends J et al., 2017 [40]; Campbell et al., 2019 [41]; Galiano-Castillo et al., 2016 [42] | |
| Colorectal cancer | Obesity Low physical activity Diet Alcohol Smoking | Promotion of healthy lifestyle and physical activity Health education at any age Nutritional counseling Use of low-dose aspirin Microbiota analysis | Colonoscopy Rectosigmoidoscopy FOBT | Nutritional counseling Family history investigation Investigation and recommendation of screening Physical activity indications Recommendation of lifestyle changes Weight monitoring Risk profiling | Chow et al., 2012 [8]; Loomans Kropp and Umar, 2019 [37]; Arends J et al., 2017 [40]; Campbell et al., 2019 [41]; Ladabaum et al., 2020 [43] | |
| Gastric cancer | Helicobacter pylori Smoking Diet Alcohol | Hp test and treatment Nutritional counseling No smoking/stop smoking | EGDS with biopsy sampling Gastric panel (pepsinogen, gastrin, and Hp IgG) | Hp test-and-treat recommendation Nutritional counseling Recommendation of lifestyle changes Weight monitoring Risk profiling | Collatuzzo and Boffetta, 2023 [4]; Chow et al., 2012 [8]; Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38]; Arends et al., 2017 [40]; Shah et al., 2025 [44] | |
| Cervical cancer | HPV Smoking | HPV vaccination Sex and health education No smoking/stop smoking Regular PAP and HPV test | PPA test HPV test | Investigation and recommendation of screening HPV vaccination Recommendation of lifestyle changes Sexual health education Risk profiling | Collatuzzo and Boffetta, 2023 [4]; Chow et al., 2012 [8]; Simms et al., 2019 [45] | |
| Liver cancer | HCV HBV Alcohol Obesity Low physical activity | HBV vaccination HCV test Promotion of healthy lifestyle and physical activity Health education at any age Serology Nutritional counseling Support for alcohol use disorder | Abdominal ultrasound CT Biomarkers (AFP) | HBV vaccination HBV and HCV screening Alcohol use investigation and education Nutritional counseling Physical activity indications Recommendation of lifestyle changes Weight monitoring Risk profiling | Collatuzzo and Boffetta, 2023 [4]; Chow et al., 2012 [8]; Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38]; Arends et al., 2017 [40]; Campbell et al., 2019 [41]; Yang et al., 2019 [46] | |
| Prostate cancer | Obesity Low physical activity | Promotion of healthy lifestyle and physical activity PSA screening Clinical prostate examination | TRUS | PSA monitoring Physical activity indications Weight monitoring Recommendation of lifestyle changes | Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38]; Campbell et al., 2019 [41]; Pinsky and Parnes, 2023 [47] | |
| Key Characteristics | Challenges | Opportunities | References |
|---|---|---|---|
| Heterogeneous categories of population (including less advantaged subgroups) | Non-compliance, missing unemployed | Equity, addressing socioeconomic barriers, age- and sex-specific interventions | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26] |
| General adult population (age range 18–65) | Specific age range for cancer screenings also covering ages older than 65 | Primary prevention intervention in young adults, health awareness at the workplace with long-term repercussion also after employment age | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26] |
| Structured setting of OHS | Logistics and organization of testing, test results communication, visit duration | Regular follow-up and longitudinal monitoring of the worker’s health and adherence to cancer prevention | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26] |
| Available spaces for medical visits and tests | Availability and quality of instruments and infrastructures (e.g., laboratory) | Adequate environment for test/vaccination provision and storage | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26] |
| Planned administration of questionnaires and tests (drug test, alcohol test, blood sample, visual test, hearing check, etc.) | Required sample collection and preservation, test elimination | Adding cancer screening tests and cancer biomarkers to already planned tests | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26] |
| Interaction of different professionals (occupational physician, occupational nurse, employer, occupational safety representatives) | Multiple expertise required, need for enlightened figures, high responsibilities of the involved figures, increased workload of the occupational health providers | Network made of multidisciplinary team | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26]; Stratil et al., 2017 [77] |
| Hierarchic structure | Hesitancy and reluctance from employers and/or occupational physicians | Welfare policies of the company, enhanced wellbeing and support of workers and stakeholders, financial support | WHO Regional Office for Europe, 2002 [24]; International Labour Office, 1998 [26]; Jimenez et al., 2017 [78] |
| Medical records | Privacy issues, unfit for work | Personalized dataset, risk profiling, 4-P medicine, data cloud | Price and Cohen, 2019 [79] |
| Prevention of injuries, occupation-related diseases and workers’ health vulnerabilities | High effort requirement for extended occupational health approach | Total worker health (one health) | Schill and Chosewood, 2013 [27]; Jimenez et al., 2017 [77]; Price and Cohen, 2019 [79] |
| Focused on risk assessment and early diagnosis | Lack of treatment | Closer to clinics, vaccine administration, recommendation for further diagnostic tests, behavioral interventions (nutrition, physical activity, lifestyle care) | Schill and Chosewood, 2013 [27]; Loomans-Kropp and Umar, 2019 [37]; de Boer et al., 2024 [38]; Zusman et al., 2021 [80] |
| Overall healthy people | Management of high-risk subjects, missing subgroups of population unemployed for medical reasons | Cancer risk assessment, complementary role of occupational physician to general practitioner, support to public health practice on the general population | Schill and Chosewood, 2013 [27]; Stratil et al., 2017 [77]; Zusman et al., 2021 [80]; Persechino et al., 2017 [81] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collatuzzo, G.; Godono, A.; Fiorini, G.; Vencovsky, D.; Giordani, S.; Biagioli, V.; Pinto-Vidal, F.A.; Seyyedsalehi, M.S.; Kostrzewa, M.; Honrado, A.; et al. Expanding Cancer Prevention: Strategies Integrated into Occupational Health Surveillance. Cancers 2025, 17, 3535. https://doi.org/10.3390/cancers17213535
Collatuzzo G, Godono A, Fiorini G, Vencovsky D, Giordani S, Biagioli V, Pinto-Vidal FA, Seyyedsalehi MS, Kostrzewa M, Honrado A, et al. Expanding Cancer Prevention: Strategies Integrated into Occupational Health Surveillance. Cancers. 2025; 17(21):3535. https://doi.org/10.3390/cancers17213535
Chicago/Turabian StyleCollatuzzo, Giulia, Alessandro Godono, Giulia Fiorini, Daniel Vencovsky, Stefano Giordani, Valentina Biagioli, Felipe Augusto Pinto-Vidal, Monireh Sadat Seyyedsalehi, Magdalena Kostrzewa, Angel Honrado, and et al. 2025. "Expanding Cancer Prevention: Strategies Integrated into Occupational Health Surveillance" Cancers 17, no. 21: 3535. https://doi.org/10.3390/cancers17213535
APA StyleCollatuzzo, G., Godono, A., Fiorini, G., Vencovsky, D., Giordani, S., Biagioli, V., Pinto-Vidal, F. A., Seyyedsalehi, M. S., Kostrzewa, M., Honrado, A., Bruno, D., Tardon, A., Mates, D., Schneider-Kamp, A., Fabianova, E., & Boffetta, P. (2025). Expanding Cancer Prevention: Strategies Integrated into Occupational Health Surveillance. Cancers, 17(21), 3535. https://doi.org/10.3390/cancers17213535







