Simple Summary
High-grade gliomas almost inevitably recur after standard therapy, leaving limited treatment options. We evaluated stereotactic radiosurgery as a targeted re-irradiation strategy for small tumor recurrences, focusing on survival, local control, and treatment-related tissue damage. Our results show that this approach can provide meaningful disease control with acceptable safety, although radiation necrosis was frequent, particularly in tumors near the ventricular system. We also explored the role of artificial intelligence for tumor segmentation, which proved useful but still requires expert validation and advanced imaging. These findings support stereotactic radiosurgery as a feasible salvage treatment and highlight the need for improved strategies to reduce side effects and refine target definition.
Abstract
Background/Objectives: Despite multimodal therapeutic concepts, treatment of recurrent malignant gliomas remains challenging. Stereotactic radiosurgery (SRS) may be a possible safe and effective non-invasive salvage treatment. In this study, we aim to investigate the SRS treatment outcomes using partly 18F-Fluorethylthyrosine (FET)-PET-imaging sequences for SRS treatment planning focusing on overall survival, event-free survival, and the incidence and factors influencing radiation necrosis (RN) occurrence. Additionally, we evaluated the potential application of AI-based tumor segmentation. Methods: We conducted a retrospective analysis of patients with recurrent malignant glioma treated with single-fraction or hypofractionated SRS at our institution. The outcomes assessed included local control, overall survival (OS), and local event-free survival (LEFS, defined as the interval until tumor recurrence or the onset of RN). We also performed a simulation analysis to assess the potential of AI-based tumor segmentation. Results: The study included 27 patients with a median age of 57 years and 41 lesions. The median OS post-SRS was 9.6 months and an LEFS of 5.2 months. Factors positively influencing OS and LEFS included the gross tumor volume (GTV) of the lesions before SRS therapy, presence of an IDH mutation, and lomustine treatment post-SRS. The incidence of RN post-SRS was 31.7%. RN was confirmed histopathologically in 15.4%, based on MRI in 46.2% and by FET-PET in 38.5% of lesions. In a simulation analysis, AI-based tumor segmentation reliably delineated all lesions, requiring only minimal manual adjustments to define target volumes. Conclusions: High-dose SRS is a feasible salvage treatment for small-volume recurrent high-grade gliomas, achieving local control and survival outcomes comparable to other re-irradiation strategies. IDH mutation, smaller tumor volume, and lomustine therapy were associated with improved survival. RN occurred frequently, particularly in periventricular lesions. AI-based tumor segmentation showed promise in well-defined satellite recurrences, but remains limited in cavity-adjacent lesions, underlining the need for expert review and 18FET-PET imaging.
1. Introduction
High-grade gliomas (HGGs) are among the most aggressive adult brain tumors, with an incidence of 3.2 per 100,000 people [1]. Despite multimodal treatment—resection, chemoradiation, and agents like temozolomide (TMZ) or lomustine [2,3]—recurrence within 6–9 months is common due to diffuse infiltration [4]. Management of recurrent HGG remains difficult, with limited treatment options and poor progression-free survival [5]. No consensus exists, though guidelines suggest re-resection, second-line chemotherapy, targeted therapy, or re-irradiation, all with modest efficacy and considerable side-effects [6]. As recurrences often arise near the prior radiation site, re-irradiation decisions hinge on timing, lesion size, proximity to organs at risk, age, Karnofsky Performance Status (KPS), and risk of radionecrosis (RN) [7,8]. Re-irradiation is generally recommended no earlier than 6 months after initial radiotherapy [9,10]. Stereotactic radiosurgery (SRS), delivered in single or hypofractionated sessions, offers a potential alternative for recurrent HGG, particularly for small lesions [11]. However, despite the technical advantages of SRS, the efficacy and safety of such treatment protocols in larger cohorts remain a topic of debate. Limited evidence and lack of large-scale studies continue to pose challenges in conclusively validating these approaches. Thereby, SRS known for its conformality, steep dose gradient, and precise targeting capabilities, may be particularly advantageous for administering radiation treatment to recurrent HGG located in close proximity to critical anatomical structures, such as the optic system or brainstem. This approach allows for re-irradiation while respecting the dose constraints of organs at risk (OAR), aiming to minimize radiation-induced damage to these vital areas [12,13]. While a small number of previous retrospective studies have indicated feasibility of robotic SRS [14,15,16,17,18,19], definitive reports on treatment outcome for selected patients with small inoperable recurrent HGG remain rare. Furthermore, the value of 18F-Fluorethylthyrosine (FET)-PET imaging for target volume determination is still controversial. Despite precise dose application, RN remains a common and severe side effect and factors influencing its occurrence are not yet fully understood. Furthermore, AI-based contouring emerges as a technical advantage for more accurate target volumes [20]. Therefore, the aim of the following study was to evaluate our institutional experience after SRS re-irradiation for recurrent HGG in terms of overall survival, event-free survival with a focus on incidence and factors influencing RN occurrence. In addition, also evaluate the potential of an AI-based tumor segmentation for future SRS planning.
2. Materials and Methods
2.1. Study Design and Patient Cohort
This retrospective single-center study was approved by the local ethics committee (EA 1/289/19) and conducted in accordance with the Declaration of Helsinki. All patients with recurrent WHO grade III or IV gliomas treated with single- or hypofractionated SRS using the CyberKnife-VSI-System (Accuray, Madison, WI, USA) between 2011 and 2021 were included. No exclusion criteria were applied.
2.2. SRS Treatment
Patients with small-volume recurrence ≥6 months after standard therapy (surgery/biopsy coupled with a course of radiotherapy and chemotherapy) were evaluated for salvage SRS by an interdisciplinary neuro-oncological board. Small-volume recurrence was defined by a GTV < 12 cm3, in line with clinical decision-making thresholds applied at our institution for SRS eligibility. Resolutions to proceed with re-irradiation utilizing robotic SRS were ultimately ratified by the interdisciplinary board following comprehensive evaluations of the individual cases. Treatment parameters, including dose and fractionation, were tailored based on prior radiation, lesion location, and OAR constraints per contemporary guidelines.
Planning computed tomography (CT, 0.75 mm, contrast-enhanced) was co-registered with MRI (contrast-enhanced T1-weighted 3D gradient-echo and fat-suppressed sequences). In selected cases, additional (18F-FET)-PET/MRI was fused for target definition. In our study, we used a tumor-to-brain ratio (TBR_max ≥ 2.0) as the reference threshold for defining metabolically active tumor regions. Although the PET-RANO expert panel later recommended a standardized lower cutoff (TBR_max ≥ 1.6) for identifying PET-positive tumor tissue, we maintained the institutional threshold of 2.0 for consistency within the retrospective dataset [21]. For target volume delineation, the attenuation-corrected FET-PET sequence and the contrast-enhanced T1-weighted MPRAGE MRI were fused with the planning CT. Only manual contouring was applied; no semi-automated PET-based biological tumor volume segmentation was used, as such approaches may be confounded by post-surgical changes and nonspecific tracer uptake [22]. FET-PET information served as a supportive modality alongside MRI, and the same TBR threshold (≥2.0) was consistently applied for both planning and follow-up evaluation to differentiate recurrence from radionecrosis.
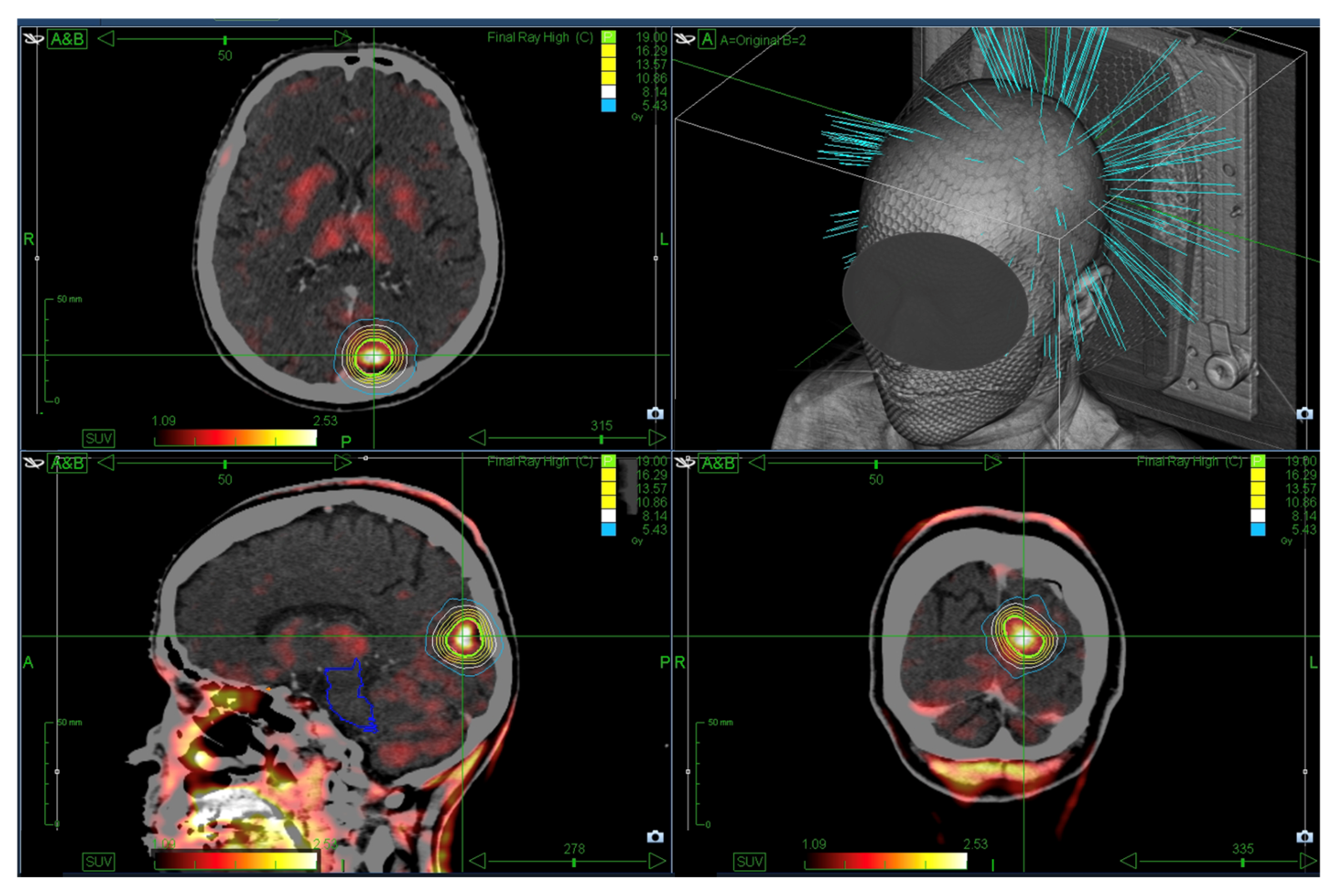
The gross tumor volume (GTV) was delineated using the most recent imaging, with a 0–2 mm margin to generate the planning target volume (PTV). Until June 2019, treatment planning was conducted using the MultiPlan (Accuray, Madison, WI, USA, versions 4.6.0 and 4.6.1) and subsequently with the Precision system (Accuray, Madison, WI, USA, versions 2.0.0.1, 2.0.1.1 and 3.2.0.0). Figure 1 displays an exemplary SRS treatment plan.
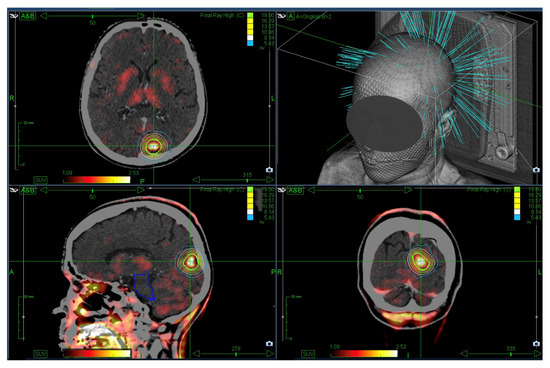
Figure 1.
Exemplary single-session SRS plan showing a prescription dose of 1 × 19 Gy (green) enclosing the PTV. The planning CT was fused with FET-PET for target definition.
All patients received 4 mg dexamethasone post-SRS, with additional doses in the case of treatment-related edema or symptoms of raised intracranial pressure.
2.3. Data Collection
Patient data including age, gender, Karnofsky Performance Status (KPS), tumor volume, laterality and location, extent of resection (gross total [GTR], subtotal [STR], or biopsy), histopathological and molecular markers (WHO grade, IDH mutation, MGMT promoter methylation, ATRX loss, TP53 status), prior treatments, radiographic response, and treatment-related toxicity were retrospectively reviewed. WHO classification valid at the time of treatment was applied. SRS treatment parameters (prescription dose, isodose, planning target volume [PTV], treatment time) were also recorded. Follow-up included clinical evaluation and MRI every three months. Recurrence location was categorized as (i) within, (ii) marginal to, or (iii) outside the previously irradiated field. Marginal recurrence was defined as tumor regrowth at the periphery of the prior field where dose gradients were lower. Tumor response was classified according to RANO criteria: complete response (CR), partial response (PR), stable disease (SD), progressive disease (PD), and radiation necrosis (RN). RN was diagnosed via MRI (new or increased contrast enhancement within the radiation field) and confirmed with (FET)-PET (maximum tumor-to-brain-uptake-ratio < 2) or histology, where available. RN was categorized as definitive (dRN, PET- or histology-confirmed) or MRI-based (mRN). Periventricular lesions were defined by contact with the ventricular system. Overall survival (OS) was defined from initial diagnosis to death or last follow-up; local event-free survival (LEFS) as time to recurrence or RN. Adverse events were graded using Common Terminology Criteria for Adverse Events (CTCAE, Version 5).
2.4. Simulation of AI-Based GTV Segmentation
To evaluate the potential of AI in SRS planning, GTV_AIs were generated using RT Elements 4.5 (Brainlab AG, Munich, Germany, version 4.5.0.273) for cases with suitable MRI, including 21/26 (80.8%) satellite- and 14/15 (93.3%) resection-cavity-adjacent lesions (SL, RCL), and then reviewed by a radiosurgeon. In case of revision, corrected GTVs (GTV_AIc) were generated as reference and compared to GTV_AIs for volume overlap, potentially left out, and excess target volume in the simulation. The AI-based autosegmentation was performed exclusively on contrast-enhanced MRI data; FET-PET information was not included in the AI workflow. Manual contours used for comparison were also generated on MRI without the integration of PET data. Thus, the evaluation represents a direct comparison between MRI-based AI segmentations and MRI-based manual delineations. The AI-based Cranial Tumor Segmentation from RT Elements 4.5 (Brainlab AG, Munich, Germany, version 4.5.0.273) used in this study is a vendor-trained, commercially available model. No local retraining or fine-tuning was performed.
2.5. Statistical Analysis
Statistical analyses were performed using SPSS (v25.0), RStudio (v2023.06.0), and GraphPad Prism (v10). Data are presented as medians with interquartile ranges [IQRs] due to non-normal distribution. Statistical significance was defined as p ≤ 0.05. Given the exploratory nature of the study and limited sample size, no corrections for multiple testing were applied. Kaplan–Meier analysis with log-rank tests was used for survival comparisons. Univariate Cox regression was conducted using R packages survival, gtsummary, and survminer. Wilcoxon signed-rank tests were also applied where appropriate. For comparison of GTVs in simulation, we used descriptive volume comparisons and Dice-Coefficient.
3. Results
3.1. Baseline and SRS Treatment Characteristics
We included 27 patients (41 lesions) with a median age of 57 years [IQR 49.5–65] and 40.7% female. Epileptic seizures were the most common symptoms (41%). Median KPS at baseline was 80 [IQR 60–100] (see Table 1). FET-PET/MRI was performed in 13 of 27 patients (48.1%) prior re-irradiation and served as a complementary imaging modality.

Table 1.
Baseline characteristics of included patients.
WHO grade 3 tumors accounted for 20%, grade 4 for 80%. Most recurrences (68%) occurred within the previous radiation field, and 24% in marginal areas (see Table 2).

Table 2.
Characteristic of treated lesions.
SRS was delivered in single fraction (75.6%) or hypofractionated regimens (24.4%), with doses ranging from 14 to 27 Gy. The median GTV was 0.78 cm3 [IQR 0.45–3.0] and the median PTV was 1.48 cm3 [IQR 1.0–5.4] (see Table 3).

Table 3.
Treatment characteristics.
3.2. Local Tumor Control and Clinical Outcome
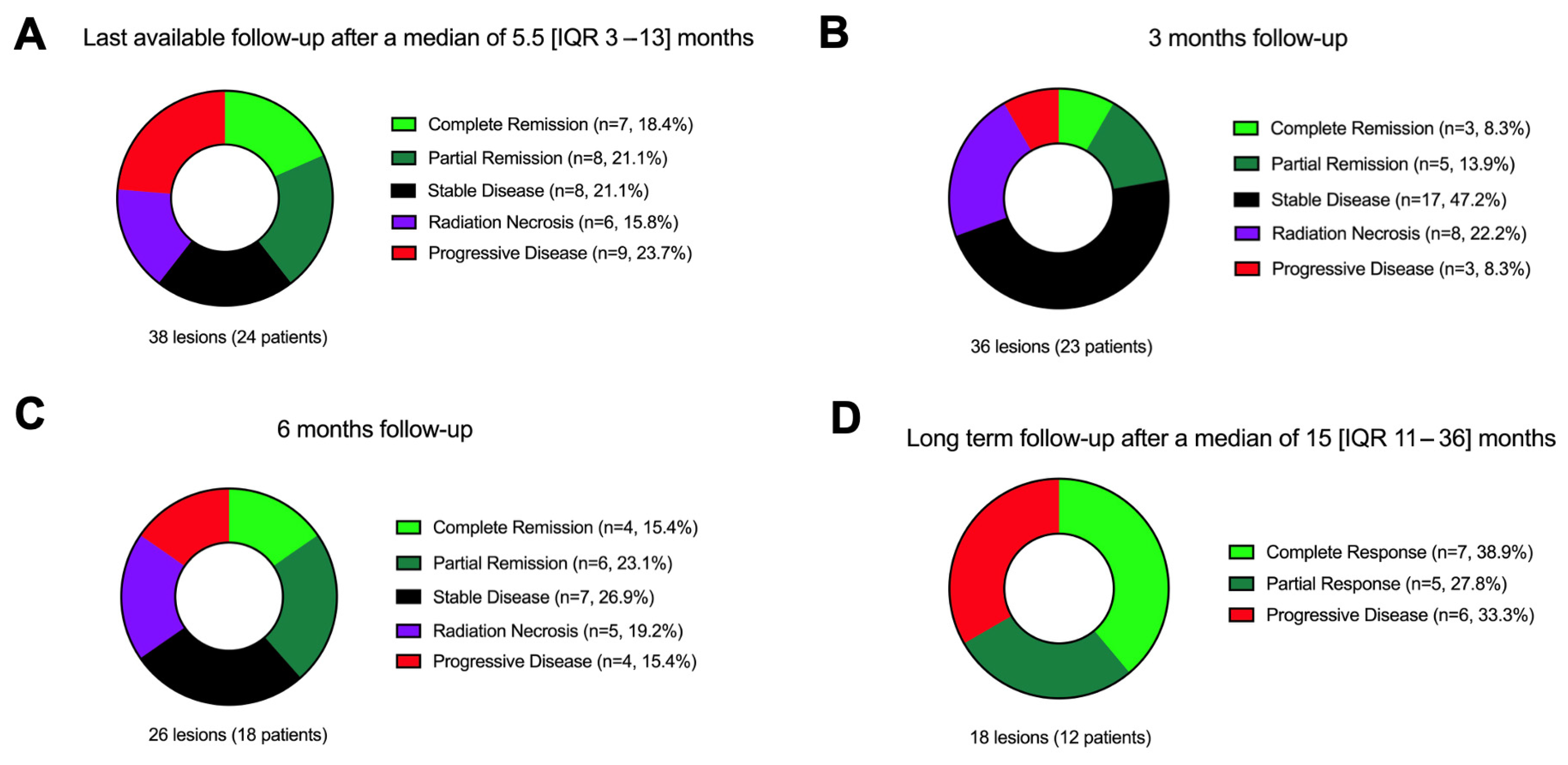
Among 36 evaluable lesions, 8.3% showed complete response, 13.9% partial response, 47.2% stable disease, 8.3% progression, and 22.2% RN (see Figure 2 and Supplement Figures S1 and S2) at a 3-month follow-up. Clinical follow-up was available for 24 patients (median follow-up duration 5.5 [IQR 3–13] months). KPS declined from a median of 80 to 70 (p = 0.005), 52% remained stable or improved, and 48% declined. Complications occurred in six patients (22.2%), and five CTCAE grade 1 and one grade 2 vestibular disorder (not persistent) was observed.
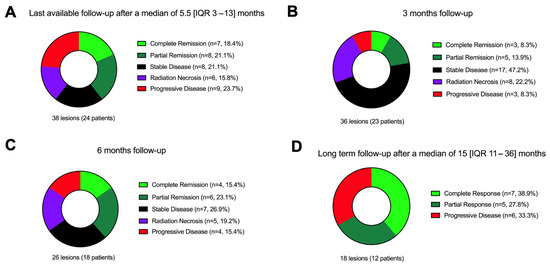
Figure 2.
Local tumor control after SRS therapy divided into the following: (A) Last available follow-up after a median of 5.5 months. (B) A 3-month follow-up. (C) A 6-month follow-up. (D) Long-term follow-up after a median of 15 months. Abbreviations: CR = complete response, PR = partial remission, SD = stable disease, RN = radiation necrosis (both, definite and MRI-based), PD = progressive disease.
3.3. Radiation Necrosis (RN)
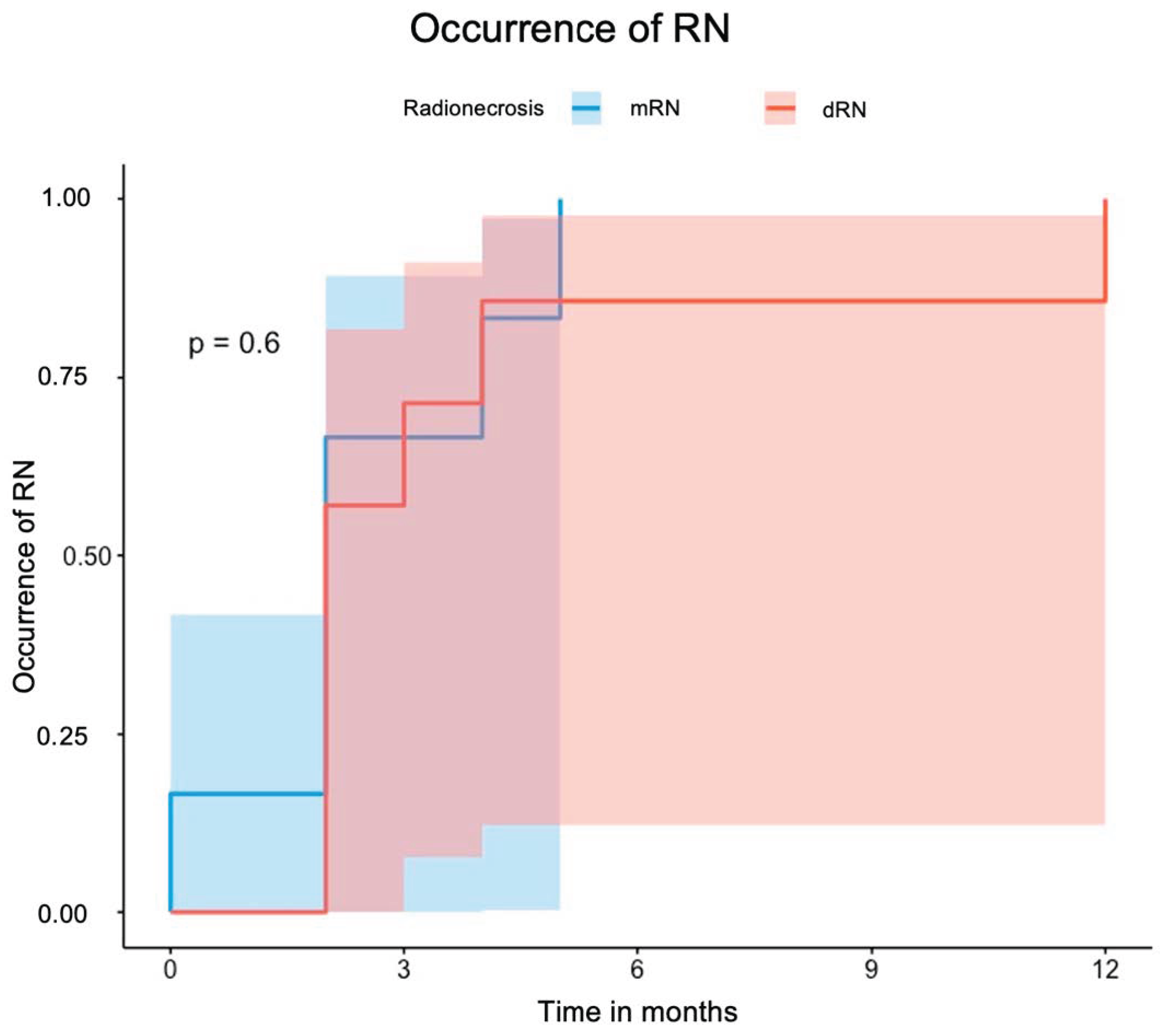
RN was diagnosed in 13 lesions (31.7%) among 11 patients. MRI confirmed six cases (mRN), FET-PET confirmed five, and histopathology confirmed two (dRN total: 7). RN occurred after a median of 2 months [IQR 2–4] post-SRS and was symptomatic in nine cases (69.2%). Symptoms were mostly managed with corticosteroids; two patients required surgery. Of seven post-SRS resections, five confirmed tumor recurrence and two RN. Five patients received bevacizumab. Periventricular location was the only independent predictor of RN (HR 6.13); 7 of 11 periventricular lesions (63.6%) developed RN. Figure 3 illustrates the occurrence of dRN and mRN. Uni- and multivariate analyses are provided in Table 4. Analysis limited to dRN yielded similar results.
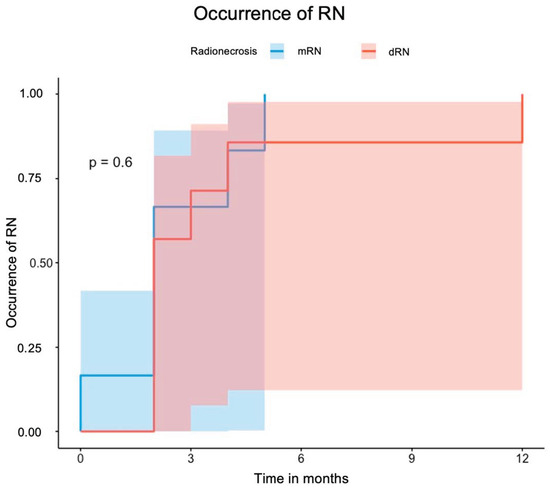
Figure 3.
Curve for the occurrence of RN stratified according to mRN and dRN. Abbreviations: RN = radiation necrosis, dRN = definitive RN (PET- or histology-confirmed), mRN = MRI-based RN.

Table 4.
Risk factors for the occurrence of radionecrosis (RN).
3.4. Overall and Local Event-Free-Survival
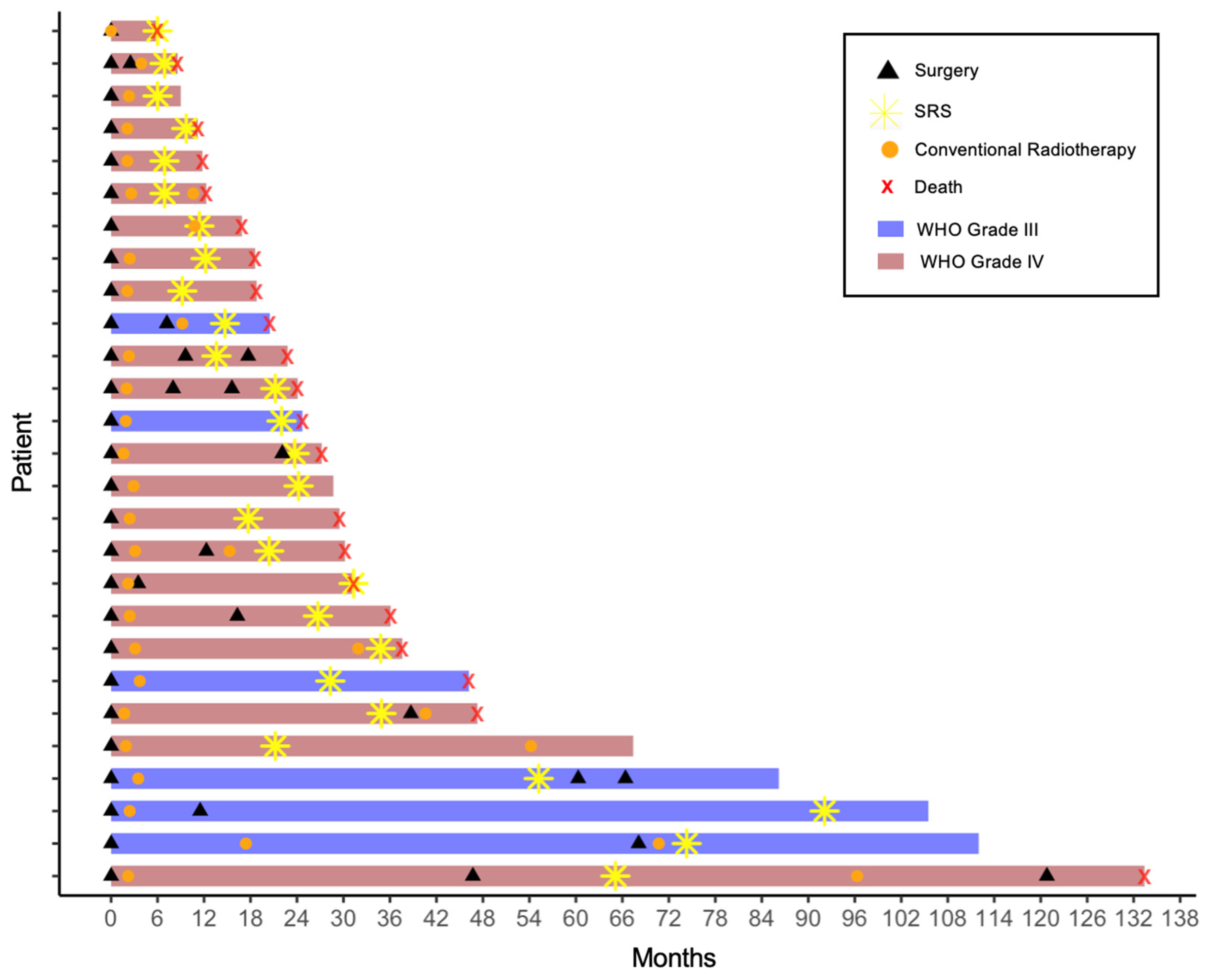
Following SRS, further therapies included re-resection (19.5%), re-irradiation (14.6%), chemotherapy (temozolomide, lomustine ± procarbazine, or bevacizumab), and TTFields (one patient). Figure 4 presents the individual courses from first diagnosis to last follow-up or death as a Swimmer Plot.
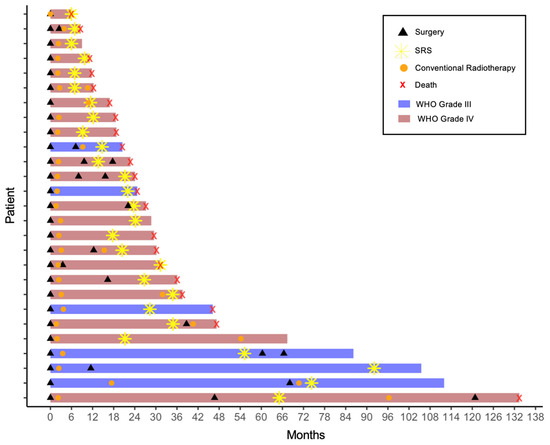
Figure 4.
Swimmer plot illustrating individual patient timelines from first diagnosis to last follow-up or death. Each bar represents a patient, with segments indicating the timing of each intervention (surgery, conventional radiotherapy, stereotactic radiosurgery). Therapeutic modalities such as chemotherapy were omitted for clarity. In all cases the recurrence diagnosis was made immediately prior to the subsequent therapy. Abbreviations: SRS = stereotactic radiosurgery.
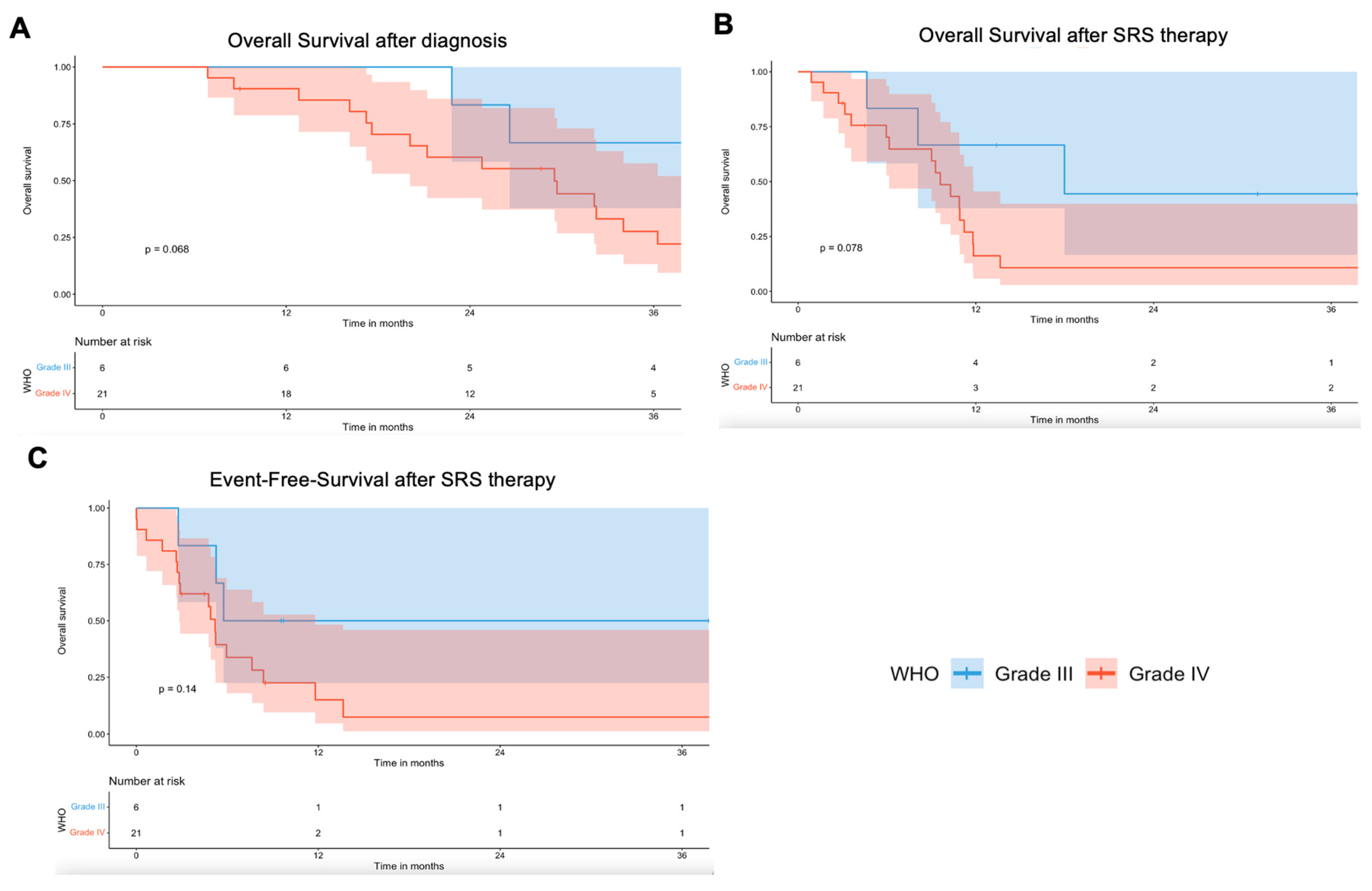
Median overall survival (OS) was 29.5 months [IQR 17.6–46.3]; post-SRS OS was 9.6 months [IQR 4.5–13.4]. Twenty-one patients (77.8%) died during follow-up. Due to limited distinction between pseudoprogression, RN, and tumor progression, all were considered events in calculating local EFS, with a median of 5.2 months [IQR 2.8–8.5]. Kaplan–Meier curves stratified by WHO grade are shown in Figure 5.
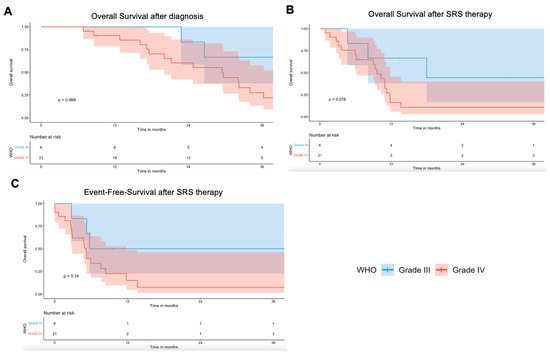
Figure 5.
Kaplan–Meier survival curves for (A). Overall survival after initial diagnosis, (B) overall survival after SRS therapy, and (C) EFS after SRS therapy (censored data).
Univariate analysis identified the GTV (p = 0.01), IDH mutation (p = 0.01), and lomustine post-SRS (p = 0.02) as associated with survival. RN (dRN and mRN) had no significant impact on OS (see Table 5). Analysis restricted to dRN yielded similar results.

Table 5.
Risk factors for poor (event-free-) survival (cox regression).
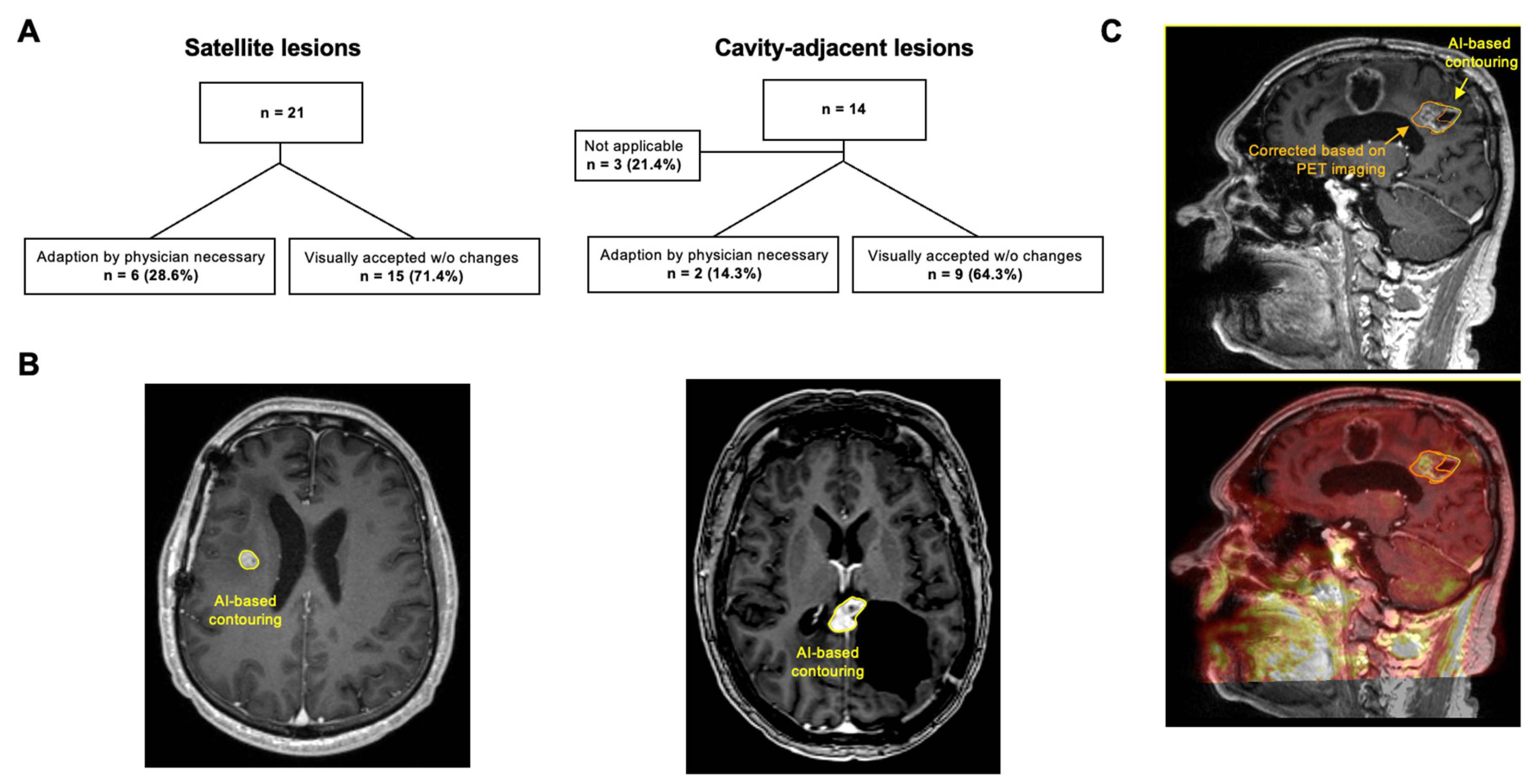
3.5. AI-Based GTV Segmentation
The AI correctly identified all 35 target lesions. In the visual evaluation, 3 of 14 (21.4%) RCLs were excluded from further analysis, as accurate AI-based segmentation was not feasible without additional information such as MRI follow-up or FET-PET (see Figure 6). In 6 out of 21 SLs, minor manual adjustments to GTV_AI were made by the radiosurgeon (Dice-Coefficient 0.64 (range: 0.4–0.76)). Importantly, 5 out of 6 corrected lesions were close to the ventricle. The median volume of SLs was 0.41 cm3 (range: 0.11–1.19 cm3) with a median GTV overlap of 69.7% (range: 28.6–94.1%). Potentially missed or excess volumes accounted for 30.3% (range: 5.9–71.4%) and 7.5% (range: 5.9–9.1%), respectively. For RCLs, minor corrections were needed in 2 of 11 cases, with a median Dice-Coefficient of 0.76. Due to the low number of corrections, no further comparison was performed. To further evaluate segmentation performance, we performed a subgroup comparison between lesions in which the AI correctly delineated the target and those in which segmentation failed or required correction. AI-based segmentation performed particularly well for satellite lesions (SLs) with distinct contrast enhancement and clear margins. Manual corrections were required in six cases, five of which were located near the ventricular system, where the complex anatomy and proximity to cerebrospinal fluid spaces hindered accurate contour generation. For RCLs, corrections were necessary in two cases, mainly due to scar tissue-related contrast enhancement that complicated delineation.
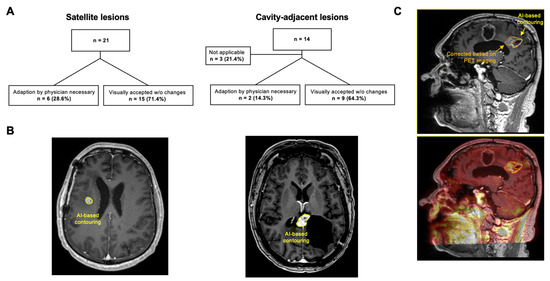
Figure 6.
AI-based GTV segmentation. (A) Overview and results of AI-based segmentation, stratified by satellite lesions and cavity-adjacent lesions. (B) Two examples without the need for manual modifications: MRI imaging of a satellite lesion on the left and a cavity-adjacent lesion on the right. (C) Exemplary case, where AI was deemed not applicable, since the target could not be defined by contrast enhancement alone. Contrast-enhanced T1-weighted MRI with corresponding PET imaging below, showing the AI-generated contour (yellow) and manual PET-guided segmentation (orange). This case underscores the need for additional clinical or imaging data—such as sequential MRIs or PET—to accurately delineate targets near the resection cavity.
4. Discussion
The present data suggest that high-dose SRS is a feasible salvage treatment for small-volume recurrences of HGG offering local control and survival benefits with manageable toxicity. Periventricular location emerged as an independent predictor of RN. AI-based segmentation holds high potential for the SRS planning.
Radiosurgery has been used in case series as a salvage treatment in recurrent high-grade glioma after initial concurrent chemoradiation and other therapies. These initial studies and meta-analysis have shown feasibility concerning a safe treatment and adequate local tumor control but a high risk of development of RN [14,19,23]. Our results are in line with previous studies and show that SRS may a feasible strategy for locally confined recurrence of high-grade gliomas with adequate local control, but a high risk of development of RN.
In the present study nearly half of the patients underwent pretherapeutic FET-PET-MRI imaging (48.1%). The basic procedure of FET-PET SRS planning is comparable to an established protocol used for meningiomas [24]. Importantly, the very recent prospective multicenter randomized trial (NOA 10/ARO 2013-1) analyzed the role of PET in irradiation of recurrent glioblastoma without verifying any advantage of FET-PET-based planning [25,26]. However, here a total of 39 Gy á 3 Gy per day was applied. The role of FET-PET-based planning may be more prominent in radiosurgery where less margins are applied. This should be further analyzed. In our series, FET-PET was primarily used as an adjunct to MRI for target definition in selected cases, particularly when contrast enhancement on MRI was ambiguous or when surgical changes complicated anatomical delineation. Although FET-PET information did not systematically alter the final GTV in our retrospective cohort, it frequently provided additional metabolic information that supported interdisciplinary tumor-board decisions. Moreover, FET-PET proved useful during follow-up, helping to differentiate radionecrosis from true progression in ambiguous cases. While our study was not designed to quantitatively assess the impact of FET-PET on planning or outcome, these findings underscore its supportive role in radiosurgical workflow and the need for standardized integration in future prospective studies.
AI-based advances are increasingly shaping radiotherapy. In our pilot cohort, AI autosegmentation detected all lesions; 71.4% of SLs and 64.3% of RCLs were visually accepted without modification. In cases requiring minor adjustments, differences in volume and the Dice score should be interpreted with caution due to the small lesion sizes. Accuracy was especially limited near ventricles, indicating room for improvement. Importantly, 21.4% of resection cavity-adjacent lesions required additional imaging, such as FET-PET, underscoring the value of combining AI with multimodal imaging and the continued role of clinical expertise. Overall, current AI tools may improve planning efficiency and support more standardized target delineation in clinical practice.
Only 8.3% of lesions showed progression at three months. Median OS was 29.5 [IQR 17.6–46.3] months overall and 9.6 [IQR 4.5–13.4] months post-SRS, indicating that SRS offers a viable salvage option alongside other re-irradiation strategies such as 10 × 3.5 Gy or 13 × 3 Gy. IDH mutation, smaller GTVs, and lomustine therapy were associated with improved survival. The ongoing LEGATO phase III trial (NCT05904119) will further clarify the role of lomustine with or without re-irradiation in recurrent glioblastoma [27].
The survival outcomes in our study align with previous reports. In a large cohort of 128 patients with 161 recurrent HGG lesions, median survival from initial diagnosis was 32 months and 11.5 months after SRS [15]. Guan et al. reported a median OS of 17.6 months following hypofractionated SRS [18]. Even if the survival benefit is modest, single-fraction or hypofractionated therapy offers improved quality of life compared to prolonged treatment regimens, especially in patients with limited prognosis. Lévy et al. [28] found a median survival of 14 months and relapse-free survival of 3.7 months after SRS in 13 patients with recurrent malignant gliomas. Prolonged PFS was associated with patient age, total dose, dose per fraction, and number of fractions. Improved OS after radiosurgery was linked to age < 40 years, prior salvage surgery, and additional post-SRS therapies. Other studies identified performance status at re-irradiation (Karnofsky scale) as a key predictor of PFS. Median OS and PFS after SRS for recurrent malignant gliomas were reported as 9 and 3 months, respectively [29]. A further comprehensive report of the literature regarding SRS for the treatment of HGG can be found in Supplementary Table S1 [5,14,16,17,18,19,23,28,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82].
Despite potential survival benefits, RN remains a relevant complication after SRS for recurrent HGG. Differentiating RN from true progression is clinically challenging but essential for management and prognosis [83]. RN occurred in 31.7% of lesions in our cohort, which is higher than in previous reports [72,83]. This may be attributable to the high radiation dose, the frequent infield re-irradiation, and the inclusion of MRI-based RN without histological or PET confirmation. The underlying mechanisms are multifactorial and include vascular injury, inflammation, and blood–brain barrier disruption [83]. RN was symptomatic in 69.2% of cases in our cohort. In an early study, RN occurred in 4 of 61 glioblastoma patients treated with three to six fractions [72]. In a larger cohort of 128 recurrent HGG patients with 161 lesions, the incidence was ~6%, with no high-grade toxicity reported [15]. Similar RN rates (11.4%) were found elsewhere [29]. In the recent prospective “GLIAA-Trial” [25], RN rates reached up to 25%—more closely aligning with our findings. Our higher incidence may reflect the high cumulative dose in infield re-irradiation and inclusion of MRI-based RN. While total doses >40 Gy have been linked to RN, hypofractionated SRS has been proposed as a safer alternative [10,18,84,85]. Importantly, RN or pseudoprogression does not necessarily indicate poor prognosis; some studies report longer OS in patients with early post-SRS imaging changes [47]. In our cohort, periventricular tumor location significantly increased RN risk. Few prior studies have addressed this association [86,87], but it may relate to the radiosensitivity of neural stem cells in the subependymal zone [88,89]. Further investigation in larger, prospective cohorts is warranted.
This study is limited by its retrospective design, small sample size, and heterogeneous cohort. Diagnostic uncertainty regarding RN versus true progression remains, despite MRI and FET-PET imaging, and no MR spectroscopy was performed. It should be emphasized that the very low hazard ratio for IDH mutation observed in the multivariate Cox regression (HR = 0.07) must be interpreted with caution due to the small number of IDH-mutant cases (n = 8) in our cohort. While this finding is consistent with the well-established prognostic benefit of IDH mutation, the limited sample size increases the risk of effect overestimation. The inclusion of only one IDH-mutant glioblastoma precludes subgroup analysis and limits interpretation under the current WHO classification. Nonetheless, the data reflect real-world outcomes of SRS in recurrent glioma. Given recent evidence supporting hypofractionated SRS [90], prospective studies are warranted to further define its role.
Patients in the post-irradiation setting can develop both radionecrosis and disease progression over time. Due to the study design, it is challenging to fully account for this dynamic process. Furthermore, it should be acknowledged that the AI-based Cranial Tumor Segmentation from RT Elements 4.5 (Brainlab AG, Munich, Germany, version 4.5.0.273) used in this study was not specifically trained on recurrent glioma cases. This limitation may have affected the accuracy of AI-based delineation, particularly in resection cavity-adjacent lesions where MRI alone often provides insufficient contrast and FET-PET can provide valuable complementary information.
5. Conclusions
High-dose SRS combined with multimodal technique like PET imaging and AI for precise target delineation appears a feasible salvage option for small-volume recurrent HGG, offering local control and survival outcomes comparable to other re-irradiation strategies. The high incidence of radionecrosis, particularly in periventricular lesions, highlights the need for further research into risk stratification and optimal treatment protocols.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/cancers17213423/s1; Figure S1: Sankey plot showing the flow of the local tumor control between the 3-month and long-term follow-up. Figure S2: Exemplary 67-year-old female patient. Table S1: Comprehensive report of the literature regarding SRS for the treatment of HGG.
Author Contributions
Conception and design of the study: F.L., C.S. and G.A. Data curation: A.F., F.L., B.B., L.K., C.S., G.A.,G.K., A.K., C.E., J.O. and M.M. Data and Statistical analysis: A.F., F.L., L.K. and K.R. Preparation of Figures: A.F. and F.L. Data interpretation: A.F., F.L., G.A. and C.S. Study Supervision: P.V., D.Z., C.S. and G.A. Drafting the article: A.F., F.L. and G.A. Critically revising the article: A.F., F.L., L.K., J.O., C.S., D.Z. and G.A. Administrative/technical/material support: G.A., C.S., P.V. and D.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Charité—Universitätsmedizin Berlin (code: EA 1/289/19, date: 19 May 2020).
Informed Consent Statement
Patient consent was waived due to the retrospective design of the study and anonymized data analysis, which was approved by the local ethics committee (Local ethics committee Charité Berlin, EA1/037/20. Approval date: 19 May 2020).
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial Intelligence |
| CR | Complete Response |
| CTCAE | Common Terminology Criteria for Adverse Events |
| dRN | Definite Radiation Necrosis |
| mRN | MRI-based Radiation Necrosis |
| FET | Fluorethyltyrosine |
| GTR | Gross Total Resection |
| GTV | Gross Total Volume |
| HGG | High Grade Glioma |
| IQR | Interquartile Range |
| KPS | Karnofsky Performance Score |
| PR | Partial Remission |
| PTV | Planning Target Volume |
| RCL | Resection Cavity-Adjacent Lesion |
| RN | Radiation Necrosis |
| SD | Stable Disease |
| SL | Satellite Lesion |
| STR | Subtotal Resection |
| TMZ | Temozolomide |
References
- Ostrom, Q.T.; Patil, N.; Cioffi, G.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2013–2017. Neuro-Oncology 2020, 22, iv1–iv96. [Google Scholar] [CrossRef]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef]
- Wirsching, H.G.; Galanis, E.; Weller, M. Glioblastoma. Handb. Clin. Neurol. 2016, 134, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Price, S.J.; Gillard, J.H. Imaging biomarkers of brain tumour margin and tumour invasion. Br. J. Radiol. 2011, 84, S159–S167. [Google Scholar] [CrossRef] [PubMed]
- Bergman, D.; Modh, A.; Schultz, L.; Snyder, J.; Mikkelsen, T.; Shah, M.; Ryu, S.; Siddiqui, M.S.; Walbert, T. Randomized prospective trial of fractionated stereotactic radiosurgery with chemotherapy versus chemotherapy alone for bevacizumab-resistant high-grade glioma. J. Neuro-Oncol. 2020, 148, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Andratschke, N.; Heusel, A.; Albert, N.L.; Alongi, F.; Baumert, B.G.; Belka, C.; Castellano, A.; Dhermain, F.; Erridge, S.C.; Grosu, A.-L.; et al. ESTRO/EANO recommendation on reirradiation of glioblastoma. Radiother. Oncol. 2025, 204. [Google Scholar] [CrossRef]
- Kirkpatrick, J.P.; Sampson, J.H. Recurrent malignant gliomas. Semin. Radiat. Oncol. 2014, 24, 289–298. [Google Scholar] [CrossRef]
- Mallick, S.; Benson, R.; Hakim, A.; Rath, G.K. Management of glioblastoma after recurrence: A changing paradigm. J. Egypt. Natl. Cancer Inst. 2016, 28, 199–210. [Google Scholar] [CrossRef]
- Ehret, F.; Wolfgang, J.; Allwohn, L.; Onken, J.; Wasilewski, D.; Roohani, S.; Oertel, J.; Zips, D.; Kaul, D. Outcomes of Isocitrate Dehydrogenase Wild Type Glioblastoma after Re-irradiation. Clin. Transl. Radiat. Oncol. 2023, 42, 100653. [Google Scholar] [CrossRef]
- Straube, C.; Combs, S.E.; Bernhardt, D.; Gempt, J.; Meyer, B.; Zimmer, C.; Schmidt-Graf, F.; Vajkoczy, P.; Grün, A.; Ehret, F.; et al. Adjuvant re-irradiation vs. no early re-irradiation of resected recurrent glioblastoma: Pooled comparative cohort analysis from two tertiary centers. J. Neurooncol. 2024, 168, 49–56. [Google Scholar] [CrossRef]
- Muacevic, A.; Sahgal, A.; Tonn, J.-C. Spinal Robotic Radiosurgery. In Oncology of CNS Tumors; Springer: Berlin/Heidelberg, Germany, 2019; pp. 695–701. [Google Scholar]
- Bucholz, R.D.; Laycock, K.A.; Cuff, L.E. CyberKnife stereotactic radiosurgery for intracranial neoplasms, with a focus on malignant tumors. Technol. Cancer Res. Treat. 2010, 9, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Adler, J.R., Jr.; Chang, S.D.; Murphy, M.J.; Doty, J.; Geis, P.; Hancock, S.L. The Cyberknife: A frameless robotic system for radiosurgery. Stereotact. Funct. Neurosurg. 1997, 69, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Villavicencio, A.T.; Burneikiene, S.; Romanelli, P.; Fariselli, L.; McNeely, L.; Lipani, J.D.; Chang, S.D.; Nelson, E.L.; McIntyre, M.; Broggi, G.; et al. Survival following stereotactic radiosurgery for newly diagnosed and recurrent glioblastoma multiforme: A multicenter experience. Neurosurg. Rev. 2009, 32, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Pinzi, V.; Biagioli, E.; Roberto, A.; Galli, F.; Rizzi, M.; Chiappa, F.; Brenna, G.; Fariselli, L.; Floriani, I. Radiosurgery for intracranial meningiomas: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2017, 113, 122–134. [Google Scholar] [CrossRef]
- Oermann, E.; Collins, B.T.; Erickson, K.T.; Yu, X.; Lei, S.; Suy, S.; Hanscom, H.N.; Kim, J.; Park, H.U.; Eldabh, A.; et al. CyberKnife enhanced conventionally fractionated chemoradiation for high grade glioma in close proximity to critical structures. J. Hematol. Oncol. 2010, 3, 22. [Google Scholar] [CrossRef]
- Lipani, J.D.; Jackson, P.S.; Soltys, S.G.; Sato, K.; Adler, J.R. Survival following CyberKnife radiosurgery and hypofractionated radiotherapy for newly diagnosed glioblastoma multiforme. Technol. Cancer Res. Treat. 2008, 7, 249–255. [Google Scholar] [CrossRef]
- Guan, Y.; Xiong, J.; Pan, M.; Shi, W.; Li, J.; Zhu, H.; Gong, X.; Li, C.; Mei, G.; Liu, X.; et al. Safety and efficacy of Hypofractionated stereotactic radiosurgery for high-grade Gliomas at first recurrence: A single-center experience. BMC Cancer 2021, 21, 123. [Google Scholar] [CrossRef]
- Yoshikawa, K.; Saito, K.; Kajiwara, K.; Nomura, S.; Ishihara, H.; Suzuki, M. CyberKnife stereotactic radiotherapy for patients with malignant glioma. Minim. Invasive Neurosurg. 2006, 49, 110–115. [Google Scholar] [CrossRef]
- Madhugiri, V.S.; Prasad, D. Early experience with an artificial intelligence-based module for brain metastasis detection and segmentation. J. Neuro-Oncol. 2025, 171, 365–372. [Google Scholar] [CrossRef]
- Albert, N.L.; Galldiks, N.; Ellingson, B.M.; van den Bent, M.J.; Chang, S.M.; Cicone, F.; de Groot, J.; Koh, E.-S.; Law, I.; Le Rhun, E. PET-based response assessment criteria for diffuse gliomas (PET RANO 1.0): A report of the RANO group. Lancet Oncol. 2024, 25, e29–e41. [Google Scholar] [CrossRef]
- Holzgreve, A.; Nitschmann, A.; Maier, S.H.; Büttner, M.; Schönecker, S.; Marschner, S.N.; Fleischmann, D.F.; Corradini, S.; Belka, C.; la Fougere, C. FET PET-based target volume delineation for the radiotherapy of glioblastoma: A pictorial guide to help overcome methodological pitfalls. Radiother. Oncol. 2024, 198, 110386. [Google Scholar] [CrossRef]
- Trone, J.C.; Vallard, A.; Sotton, S.; Ben Mrad, M.; Jmour, O.; Magné, N.; Pommier, B.; Laporte, S.; Ollier, E. Survival after hypofractionation in glioblastoma: A systematic review and meta-analysis. Radiat. Oncol. 2020, 15, 145. [Google Scholar] [CrossRef] [PubMed]
- Acker, G.; Kluge, A.; Lukas, M.; Conti, A.; Pasemann, D.; Meinert, F.; Anh Nguyen, P.T.; Jelgersma, C.; Loebel, F.; Budach, V.; et al. Impact of 68Ga-DOTATOC PET/MRI on robotic radiosurgery treatment planning in meningioma patients: First experiences in a single institution. Neurosurg. Focus 2019, 46, E9. [Google Scholar] [CrossRef] [PubMed]
- Oehlke, O.; Mix, M.; Graf, E.; Schimek-Jasch, T.; Nestle, U.; Götz, I.; Schneider-Fuchs, S.; Weyerbrock, A.; Mader, I.; Baumert, B.G. Amino-acid PET versus MRI guided re-irradiation in patients with recurrent glioblastoma multiforme (GLIAA)–protocol of a randomized phase II trial (NOA 10/ARO 2013-1). BMC Cancer 2016, 16, 769. [Google Scholar] [CrossRef] [PubMed]
- Grosu, A.L.; Weber, W.A.; Franz, M.; Stärk, S.; Piert, M.; Thamm, R.; Gumprecht, H.; Schwaiger, M.; Molls, M.; Nieder, C. Reirradiation of recurrent high-grade gliomas using amino acid PET (SPECT)/CT/MRI image fusion to determine gross tumor volume for stereotactic fractionated radiotherapy. J. Radiat. Oncol. Biol. Phys. 2005, 63, 511–519. [Google Scholar] [CrossRef]
- Preusser, M.; Kazda, T.; Le Rhun, E.; Sahm, F.; Smits, M.; Gempt, J.; Koekkoek, J.A.; Monti, A.F.; Csanadi, M.; Pitter, J.G. Lomustine with or without reirradiation for first progression of glioblastoma, LEGATO, EORTC-2227-BTG: Study protocol for a randomized phase III study. Trials 2024, 25, 366. [Google Scholar] [CrossRef]
- Lévy, S.; Chapet, S.; Scher, N.; Debbi, K.; Ruffier, A.; Bernadou, G.; Pointreau, Y.; Calais, G. Reirradiation of gliomas under stereotactic conditions: Prognostic factors for survival without relapse or side effects, a retrospective study at Tours regional university hospital (France). Cancer Radiother. 2017, 21, 759–765. [Google Scholar] [CrossRef]
- Adachi, K.; Hayashi, K.; Kagawa, N.; Kinoshita, M.; Sumida, I.; Akino, Y.; Shiomi, H.; Tamari, K.; Suzuki, O.; Hirayama, R.; et al. Feasibility of Salvage Re-irradiation With Stereotactic Radiotherapy for Recurrent Glioma Using CyberKnife. Anticancer Res. 2019, 39, 2935–2940. [Google Scholar] [CrossRef]
- Dhawan, S.; Patil, C.G.; Chen, C.; Venteicher, A.S. Early versus delayed postoperative radiotherapy for treatment of low-grade gliomas. Cochrane Database Syst. Rev. 2020, 1, Cd009229. [Google Scholar] [CrossRef]
- Khan, L.; Soliman, H.; Sahgal, A.; Perry, J.; Xu, W.; Tsao, M.N. External beam radiation dose escalation for high grade glioma. Cochrane Database Syst. Rev. 2020, 5, Cd011475. [Google Scholar] [CrossRef]
- Azoulay, M.; Chang, S.D.; Gibbs, I.C.; Hancock, S.L.; Pollom, E.L.; Harsh, G.R.; Adler, J.R.; Harraher, C.; Li, G.; Hayden Gephart, M.; et al. A phase I/II trial of 5-fraction stereotactic radiosurgery with 5-mm margins with concurrent temozolomide in newly diagnosed glioblastoma: Primary outcomes. Neuro-Oncology 2020, 22, 1182–1189. [Google Scholar] [CrossRef]
- Brehmer, S.; Grimm, M.A.; Förster, A.; Seiz-Rosenhagen, M.; Welzel, G.; Stieler, F.; Wenz, F.; Groden, C.; Mai, S.; Hänggi, D.; et al. Study Protocol: Early Stereotactic Gamma Knife Radiosurgery to Residual Tumor After Surgery of Newly Diagnosed Glioblastoma (Gamma-GBM). Neurosurgery 2019, 84, 1133–1137. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liu, Q.; Yuan, Z.; Zhao, L.; Wang, X.; Wang, P. Clinical Efficacy of CyberKnife Radiosurgery for Adult Brainstem Glioma: 10 Years Experience at Tianjin CyberKnife Center and Review of the Literature. Front Oncol 2019, 9, 257. [Google Scholar] [CrossRef] [PubMed]
- Navarria, P.; Pessina, F.; Cozzi, L.; Tomatis, S.; Reggiori, G.; Simonelli, M.; Santoro, A.; Clerici, E.; Franzese, C.; Carta, G.; et al. Phase II study of hypofractionated radiation therapy in elderly patients with newly diagnosed glioblastoma with poor prognosis. Tumori 2019, 105, 47–54. [Google Scholar] [CrossRef]
- Song, A.; Andrews, D.W.; Werner-Wasik, M.; Kim, L.; Glass, J.; Bar-Ad, V.; Evans, J.J.; Farrell, C.J.; Judy, K.D.; Daskalakis, C.; et al. Phase I trial of alisertib with concurrent fractionated stereotactic re-irradiation for recurrent high grade gliomas. Radiother. Oncol. 2019, 132, 135–141. [Google Scholar] [CrossRef]
- Hu, Y.J.; Chen, D.; Zhang, L.F.; Chen, J. Efficacy and Safety of Hypofractionated Stereotactic Radiotherapy for Recurrent Malignant Gliomas: A Systematic Review and Meta-analysis. World Neurosurg. 2019, 127, 176–185. [Google Scholar] [CrossRef]
- Abbassy, M.; Missios, S.; Barnett, G.H.; Brewer, C.; Peereboom, D.M.; Ahluwalia, M.; Neyman, G.; Chao, S.T.; Suh, J.H.; Vogelbaum, M.A. Phase I Trial of Radiosurgery Dose Escalation Plus Bevacizumab in Patients With Recurrent/Progressive Glioblastoma. Neurosurgery 2018, 83, 385–392. [Google Scholar] [CrossRef]
- Shi, W.; Blomain, E.S.; Siglin, J.; Palmer, J.D.; Dan, T.; Wang, Y.; Werner-Wasik, M.; Glass, J.; Kim, L.; Bar Ad, V.; et al. Salvage fractionated stereotactic re-irradiation (FSRT) for patients with recurrent high grade gliomas progressed after bevacizumab treatment. J. Neurooncol. 2018, 137, 171–177. [Google Scholar] [CrossRef]
- Repka, M.C.; Lei, S.; Campbell, L.; Suy, S.; Voyadzis, J.M.; Kalhorn, C.; McGrail, K.; Jean, W.; Subramaniam, D.S.; Lischalk, J.W.; et al. Long-Term Outcomes Following Conventionally Fractionated Stereotactic Boost for High-Grade Gliomas in Close Proximity to Critical Organs at Risk. Front. Oncol. 2018, 8, 373. [Google Scholar] [CrossRef]
- Romanelli, P.; Paiano, M.; Crocamo, V.; Beltramo, G.; Bergantin, A.; Pantelis, E.; Antypas, C.; Clerico, A. Staged Image-guided Robotic Radiosurgery and Deferred Chemotherapy to Treat a Malignant Glioma During and After Pregnancy. Cureus 2018, 10, e2141. [Google Scholar] [CrossRef]
- Pinzi, V.; Orsi, C.; Marchetti, M.; Milanesi, I.M.; Bianchi, L.C.; DiMeco, F.; Cuccarini, V.; Farinotti, M.; Ferroli, P.; Finocchiaro, G.; et al. Radiosurgery reirradiation for high-grade glioma recurrence: A retrospective analysis. Neurol. Sci. 2015, 36, 1431–1440. [Google Scholar] [CrossRef]
- Kawano, H.; Hirano, H.; Yonezawa, H.; Yunoue, S.; Yatsushiro, K.; Ogita, M.; Hiraki, Y.; Uchida, H.; Habu, M.; Fujio, S.; et al. Improvement in treatment results of glioblastoma over the last three decades and beneficial factors. Br. J. Neurosurg. 2015, 29, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Omuro, A.; Beal, K.; Gutin, P.; Karimi, S.; Correa, D.D.; Kaley, T.J.; DeAngelis, L.M.; Chan, T.A.; Gavrilovic, I.T.; Nolan, C.; et al. Phase II study of bevacizumab, temozolomide, and hypofractionated stereotactic radiotherapy for newly diagnosed glioblastoma. Clin. Cancer Res. 2014, 20, 5023–5031. [Google Scholar] [CrossRef] [PubMed]
- Dodoo, E.; Huffmann, B.; Peredo, I.; Grinaker, H.; Sinclair, G.; Machinis, T.; Enger, P.O.; Skeie, B.S.; Pedersen, P.H.; Ohlsson, M.; et al. Increased survival using delayed gamma knife radiosurgery for recurrent high-grade glioma: A feasibility study. World Neurosurg. 2014, 82, e623–e632. [Google Scholar] [CrossRef] [PubMed]
- Greto, D.; Livi, L.; Bonomo, P.; Masi, L.; Detti, B.; Meattini, I.; Mangoni, M.; Doro, R.; Favuzza, V.; Cipressi, S.; et al. Cyberknife stereotactic radiosurgery for the re-irradiation of brain lesions: A single-centre experience. Radiol. Med. 2014, 119, 721–726. [Google Scholar] [CrossRef]
- Yazici, G.; Cengiz, M.; Ozyigit, G.; Eren, G.; Yildiz, F.; Akyol, F.; Gurkaynak, M.; Zorlu, F. Hypofractionated stereotactic reirradiation for recurrent glioblastoma. J. Neurooncol. 2014, 120, 117–123. [Google Scholar] [CrossRef]
- Uslu, N.; Karakaya, E.; Dizman, A.; Yegen, D.; Guney, Y. Optic nerve glioma treatment with fractionated stereotactic radiotherapy. J. Neurosurg. Pediatr. 2013, 11, 596–599. [Google Scholar] [CrossRef]
- McKenzie, J.T.; Guarnaschelli, J.N.; Vagal, A.S.; Warnick, R.E.; Breneman, J.C. Hypofractionated stereotactic radiotherapy for unifocal and multifocal recurrence of malignant gliomas. J. Neurooncol. 2013, 113, 403–409. [Google Scholar] [CrossRef]
- Giller, C.A.; Berger, B.D.; Fink, K.; Bastian, E. A volumetric study of CyberKnife hypofractionated stereotactic radiotherapy as salvage for progressive malignant brain tumors: Initial experience. Neurol. Res. 2007, 29, 563–568. [Google Scholar] [CrossRef]
- Einstein, D.B.; Wessels, B.; Bangert, B.; Fu, P.; Nelson, A.D.; Cohen, M.; Sagar, S.; Lewin, J.; Sloan, A.; Zheng, Y.; et al. Phase II trial of radiosurgery to magnetic resonance spectroscopy-defined high-risk tumor volumes in patients with glioblastoma multiforme. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 668–674. [Google Scholar] [CrossRef]
- Conti, A.; Pontoriero, A.; Arpa, D.; Siragusa, C.; Tomasello, C.; Romanelli, P.; Cardali, S.; Granata, F.; De Renzis, C.; Tomasello, F. Efficacy and toxicity of CyberKnife re-irradiation and “dose dense” temozolomide for recurrent gliomas. Acta Neurochir. 2012, 154, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Malmström, A.; Grønberg, B.H.; Marosi, C.; Stupp, R.; Frappaz, D.; Schultz, H.; Abacioglu, U.; Tavelin, B.; Lhermitte, B.; Hegi, M.E.; et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: The Nordic randomised, phase 3 trial. Lancet Oncol. 2012, 13, 916–926. [Google Scholar] [CrossRef] [PubMed]
- Shen, G.; Xu, L.; Xu, M.; Geng, M.; Tan, Y.; Li, F. 1H-MR spectroscopy guided gamma knife radiosurgery for treatment of glioma. Turk. Neurosurg. 2012, 22, 690–694. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Canazza, A.; Calatozzolo, C.; Fumagalli, L.; Bergantin, A.; Ghielmetti, F.; Fariselli, L.; Croci, D.; Salmaggi, A.; Ciusani, E. Increased migration of a human glioma cell line after in vitro CyberKnife irradiation. Cancer Biol. Ther. 2011, 12, 629–633. [Google Scholar] [CrossRef]
- Maranzano, E.; Anselmo, P.; Casale, M.; Trippa, F.; Carletti, S.; Principi, M.; Loreti, F.; Italiani, M.; Caserta, C.; Giorgi, C. Treatment of recurrent glioblastoma with stereotactic radiotherapy: Long-term results of a mono-institutional trial. Tumori 2011, 97, 56–61. [Google Scholar] [CrossRef]
- Canazza, A.; De Grazia, U.; Fumagalli, L.; Brait, L.; Ghielmetti, F.; Fariselli, L.; Croci, D.; Salmaggi, A.; Ciusani, E. In vitro effects of Cyberknife-driven intermittent irradiation on glioblastoma cell lines. Neurol. Sci. 2011, 32, 579–588. [Google Scholar] [CrossRef]
- Balducci, M.; Apicella, G.; Manfrida, S.; Mangiola, A.; Fiorentino, A.; Azario, L.; D’Agostino, G.R.; Frascino, V.; Dinapoli, N.; Mantini, G.; et al. Single-arm phase II study of conformal radiation therapy and temozolomide plus fractionated stereotactic conformal boost in high-grade gliomas: Final report. Strahlenther. Onkol. 2010, 186, 558–564. [Google Scholar] [CrossRef]
- Fogh, S.E.; Andrews, D.W.; Glass, J.; Curran, W.; Glass, C.; Champ, C.; Evans, J.J.; Hyslop, T.; Pequignot, E.; Downes, B.; et al. Hypofractionated stereotactic radiation therapy: An effective therapy for recurrent high-grade gliomas. J. Clin. Oncol. 2010, 28, 3048–3053. [Google Scholar] [CrossRef]
- Wentworth, S.; Pinn, M.; Bourland, J.D.; Deguzman, A.F.; Ekstrand, K.; Ellis, T.L.; Glazier, S.S.; McMullen, K.P.; Munley, M.; Stieber, V.W.; et al. Clinical experience with radiation therapy in the management of neurofibromatosis-associated central nervous system tumors. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 208–213. [Google Scholar] [CrossRef]
- Schwer, A.L.; Kavanagh, B.D.; McCammon, R.; Gaspar, L.E.; Kleinschmidt-De Masters, B.K.; Stuhr, K.; Chen, C. Radiographic and histopathologic observations after combined EGFR inhibition and hypofractionated stereotactic radiosurgery in patients with recurrent malignant gliomas. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1352–1357. [Google Scholar] [CrossRef]
- Schwer, A.L.; Damek, D.M.; Kavanagh, B.D.; Gaspar, L.E.; Lillehei, K.; Stuhr, K.; Chen, C. A phase I dose-escalation study of fractionated stereotactic radiosurgery in combination with gefitinib in patients with recurrent malignant gliomas. Int. J. Radiat. Oncol. Biol. Phys. 2008, 70, 993–1001. [Google Scholar] [CrossRef]
- Smith, K.A.; Ashby, L.S.; Gonzalez, L.F.; Brachman, D.G.; Thomas, T.; Coons, S.W.; Battaglia, M.; Scheck, A. Prospective trial of gross-total resection with Gliadel wafers followed by early postoperative Gamma Knife radiosurgery and conformal fractionated radiotherapy as the initial treatment for patients with radiographically suspected, newly diagnosed glioblastoma multiforme. J. Neurosurg. 2008, 109, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.S.; Lee, J.I.; Park, K.; Kim, J.H.; Lim, D.H.; Nam, D.H. Efficacy of stereotactic radiosurgery as a salvage treatment for recurrent malignant gliomas. Cancer 2008, 112, 2046–2051. [Google Scholar] [CrossRef] [PubMed]
- Ashamalla, H.; Zaki, B.; Mokhtar, B.; Lewis, L.; Lavaf, A.; Nasr, H.; Colella, F.; Dosik, D.; Krishnamurthy, M.; Saad, N.; et al. Fractionated stereotactic radiotherapy boost and weekly paclitaxel in malignant gliomas clinical and pharmacokinetics results. Technol. Cancer Res. Treat. 2007, 6, 169–176. [Google Scholar] [CrossRef]
- Kohshi, K.; Yamamoto, H.; Nakahara, A.; Katoh, T.; Takagi, M. Fractionated stereotactic radiotherapy using gamma unit after hyperbaric oxygenation on recurrent high-grade gliomas. J. Neurooncol. 2007, 82, 297–303. [Google Scholar] [CrossRef]
- Cardinale, R.; Won, M.; Choucair, A.; Gillin, M.; Chakravarti, A.; Schultz, C.; Souhami, L.; Chen, A.; Pham, H.; Mehta, M. A phase II trial of accelerated radiotherapy using weekly stereotactic conformal boost for supratentorial glioblastoma multiforme: RTOG 0023. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 1422–1428. [Google Scholar] [CrossRef]
- Ernst-Stecken, A.; Ganslandt, O.; Lambrecht, U.; Sauer, R.; Grabenbauer, G. Survival and quality of life after hypofractionated stereotactic radiotherapy for recurrent malignant glioma. J. Neurooncol. 2007, 81, 287–294. [Google Scholar] [CrossRef]
- Combs, S.E.; Gutwein, S.; Thilmann, C.; Debus, J.; Schulz-Ertner, D. Reirradiation of recurrent WHO grade III astrocytomas using fractionated stereotactic radiotherapy (FSRT). Strahlenther. Onkol. 2005, 181, 768–773. [Google Scholar] [CrossRef]
- Ulm, A.J., 3rd; Friedman, W.A.; Bradshaw, P.; Foote, K.D.; Bova, F.J. Radiosurgery in the treatment of malignant gliomas: The University of Florida experience. Neurosurgery 2005, 57, 512–517. [Google Scholar] [CrossRef]
- Cho, K.H.; Hall, W.A.; Lo, S.S.; Dusenbery, K.E. Stereotactic radiosurgery versus fractionated stereotactic radiotherapy boost for patients with glioblastoma multiforme. Technol. Cancer Res. Treat. 2004, 3, 41–49. [Google Scholar] [CrossRef]
- Sato, K.; Baba, Y.; Inoue, M.; Omori, R. Radiation necrosis and brain edema association with CyberKnife treatment. Acta Neurochir. Suppl. 2003, 86, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.A.; Prados, M.; Lamborn, K.R.; Smith, V.; Sneed, P.K.; Chang, S.; Nicholas, K.M.; Wara, W.M.; Devriendt, D.; Kunwar, S.; et al. Phase II study of high central dose Gamma Knife radiosurgery and marimastat in patients with recurrent malignant glioma. Int. J. Radiat. Oncol. Biol. Phys. 2002, 54, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Boëthius, J.; Ulfarsson, E.; Rähn, T.; Lippittz, B. Gamma knife radiosurgery for pilocytic astrocytomas. J. Neurosurg. 2002, 97, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Regine, W.F.; Patchell, R.A.; Strottmann, J.M.; Meigooni, A.; Sanders, M.; Young, A.B. Preliminary report of a phase I study of combined fractionated stereotactic radiosurgery and conventional external beam radiation therapy for unfavorable gliomas. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 421–426. [Google Scholar] [CrossRef]
- Regine, W.F.; Patchell, R.A.; Strottmann, J.M.; Meigooni, A.; Sanders, M.; Young, B. Combined stereotactic split-course fractionated gamma knife radiosurgery and conventional radiation therapy for unfavorable gliomas: A phase I study. J. Neurosurg. 2000, 93 (Suppl. 3), 37–41. [Google Scholar] [CrossRef]
- Cardinale, R.M.; Schmidt-Ullrich, R.K.; Benedict, S.H.; Zwicker, R.D.; Han, D.C.; Broaddus, W.C. Accelerated radiotherapy regimen for malignant gliomas using stereotactic concomitant boosts for dose escalation. Radiat. Oncol. Investig. 1998, 6, 175–181. [Google Scholar] [CrossRef]
- Shenouda, G.; Souhami, L.; Podgorsak, E.B.; Bahary, J.P.; Villemure, J.G.; Caron, J.L.; Mohr, G. Radiosurgery and accelerated radiotherapy for patients with glioblastoma. Can. J. Neurol. Sci. 1997, 24, 110–115. [Google Scholar] [CrossRef]
- Hirato, M.; Nakamura, M.; Inoue, H.K.; Ohye, C.; Hirato, J.; Shibazaki, T.; Andou, Y. Gamma Knife radiosurgery for the treatment of brainstem tumors. Stereotact. Funct. Neurosurg. 1995, 64 (Suppl. 1), 32–41. [Google Scholar] [CrossRef]
- Chamberlain, M.C.; Barba, D.; Kormanik, P.; Shea, W.M. Stereotactic radiosurgery for recurrent gliomas. Cancer 1994, 74, 1342–1347. [Google Scholar] [CrossRef]
- Mehta, M.P.; Masciopinto, J.; Rozental, J.; Levin, A.; Chappell, R.; Bastin, K.; Miles, J.; Turski, P.; Kubsad, S.; Mackie, T.; et al. Stereotactic radiosurgery for glioblastoma multiforme: Report of a prospective study evaluating prognostic factors and analyzing long-term survival advantage. Int. J. Radiat. Oncol. Biol. Phys. 1994, 30, 541–549. [Google Scholar] [CrossRef]
- Curran, W.J., Jr.; Scott, C.B.; Weinstein, A.S.; Martin, L.A.; Nelson, J.S.; Phillips, T.L.; Murray, K.; Fischbach, A.J.; Yakar, D.; Schwade, J.G.; et al. Survival comparison of radiosurgery-eligible and -ineligible malignant glioma patients treated with hyperfractionated radiation therapy and carmustine: A report of Radiation Therapy Oncology Group 83-02. J. Clin. Oncol. 1993, 11, 857–862. [Google Scholar] [CrossRef]
- Ali, F.S.; Arevalo, O.; Zorofchian, S.; Patrizz, A.; Riascos, R.; Tandon, N.; Blanco, A.; Ballester, L.Y.; Esquenazi, Y. Cerebral Radiation Necrosis: Incidence, Pathogenesis, Diagnostic Challenges, and Future Opportunities. Curr. Oncol. Rep. 2019, 21, 66. [Google Scholar] [CrossRef]
- Vordermark, D.; Kölbl, O.; Ruprecht, K.; Vince, G.H.; Bratengeier, K.; Flentje, M. Hypofractionated stereotactic re-irradiation: Treatment option in recurrent malignant glioma. BMC Cancer 2005, 5, 55. [Google Scholar] [CrossRef]
- Kossmann, M.R.P.; Ehret, F.; Roohani, S.; Winter, S.F.; Ghadjar, P.; Acker, G.; Senger, C.; Schmid, S.; Zips, D.; Kaul, D. Histopathologically confirmed radiation-induced damage of the brain—An in-depth analysis of radiation parameters and spatio-temporal occurrence. Radiat. Oncol. 2023, 18, 198. [Google Scholar] [CrossRef]
- van de Weijer, T.; Broen, M.P.G.; Moonen, R.P.M.; Hoeben, A.; Anten, M.; Hovinga, K.; Compter, I.; van der Pol, J.A.J.; Mitea, C.; Lodewick, T.M.; et al. The Use of (18)F-FET-PET-MRI in Neuro-Oncology: The Best of Both Worlds—A Narrative Review. Diagnostics 2022, 12, 1202. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, G.; Alshamy, G.; Chan, B.; Abrams, R.; Greenberg, E.; Saxena, A.; Bradbury, M.; Edgar, M.; Gutin, P.; Tabar, V. Long-term impact of radiation on the stem cell and oligodendrocyte precursors in the brain. PLoS ONE 2007, 2, e588. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, D.; König, L.; Grosu, A.; Wiestler, B.; Rieken, S.; Wick, W.; Gempt, J.; Krieg, S.M.; Schmidt-Graf, F.; Sahm, F.; et al. DEGRO practical guideline for central nervous system radiation necrosis part 1: Classification and a multistep approach for diagnosis. Strahlenther. Onkol. 2022, 198, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Iuchi, T.; Hatano, K.; Imagunbai, T.; Kodama, T.; Uchino, Y.; Tohyama, N.; Sakaida, T.; Kawasaki, K.; Hasegawa, Y. Para-ventricular radiation necrosis after radiation therapy for malignant astrocytomas. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, S274. [Google Scholar] [CrossRef]
- Chen, A.T.C.; Serante, A.R.; Ayres, A.S.; Tonaki, J.O.; Moreno, R.A.; Shih, H.; Gattás, G.S.; Lopez, R.V.M.; dos Santos de Jesus, G.R.; de Carvalho, I.T.; et al. Prospective Randomized Phase 2 Trial of Hypofractionated Stereotactic Radiation Therapy of 25 Gy in 5 Fractions Compared With 35 Gy in 5 Fractions in the Reirradiation of Recurrent Glioblastoma. Int. J. Radiat. Oncol. Biol. Phys. 2024, 119, 1122–1132. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).