Digital Serious Games for Cancer Education and Behavioural Change: A Scoping Review of Evidence Across Patients, Professionals, and the Public
Simple Summary
Abstract
1. Introduction
- Examine the current evidence on digital serious game interventions aimed at improving cancer-related education, awareness, and behavioural outcomes among adults.
- Explore the reported outcomes of digital serious games across adult cancer patients, healthcare professionals, and the public, including impacts on knowledge, engagement, confidence, communication, self-efficacy, and behavioural intentions.
- Identify gaps in the literature concerning the design, delivery, and evaluation of digital serious games for cancer education and awareness across diverse stakeholder groups.
- Global cancer burden: Cancer is a leading cause of death worldwide, with incidence and mortality expected to rise due to population growth, ageing, and lifestyle factors.
- Importance of awareness and education: Improving public, patient, and healthcare professional awareness and self-efficacy may contribute to early detection, better prevention behaviour, and reduced mortality.
- Potential of digital serious games: Compared to traditional education methods, digital serious games provide more interactive and engaging approaches to improve cancer education, knowledge acquisition, cancer awareness, self-efficacy, and help-seeking intentions.
- Stakeholder diversity: Digital serious games can benefit multiple groups, including cancer patients (self-management), healthcare professionals (training, communication), and the public (awareness and prevention).
- Evidence gap: While previous reviews have examined serious games in specific contexts, no review has comprehensively integrated perspectives from patients, healthcare professionals, and the public on digital serious games for cancer education and behavioural change.
- Scope of current review: This scoping review aims to systematically map existing evidence on digital serious games for cancer awareness, education, and behavioural change among adults, highlighting gaps and informing future research and design strategies.
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. Population
2.2.2. Concept
2.2.3. Context
2.3. Search Strategy
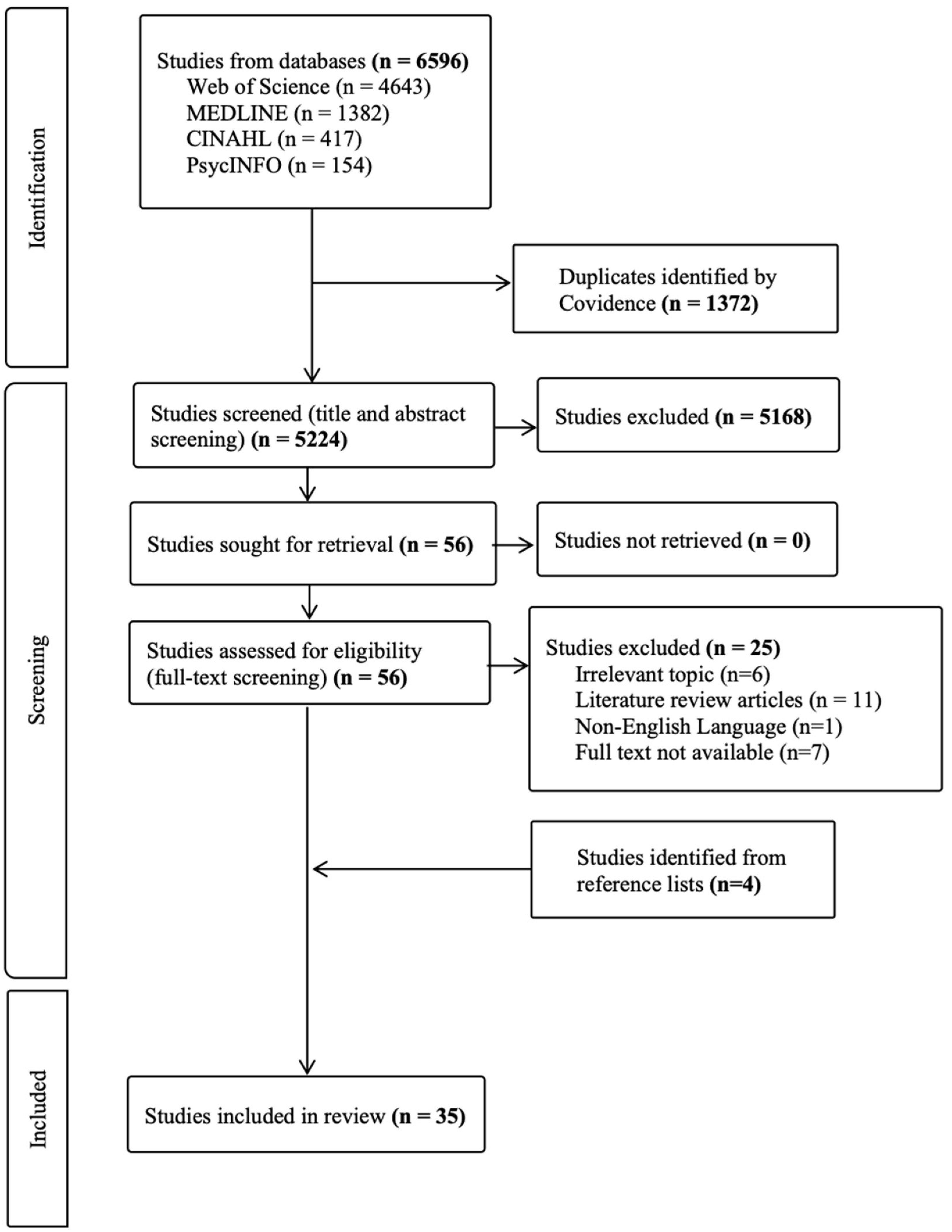
2.4. Selection of Sources of Evidence
2.5. Data Charting
2.6. Data Analysis
3. Results
3.1. Characteristics of Included Studies
3.2. The Role of Serious Games in Cancer Awareness Among Patients
3.2.1. Effective for Health and Behavioural Outcomes
3.2.2. Effective in Educating Cancer Knowledge and Raising Awareness
3.2.3. Challenges in Engagement and Personalisation
3.3. The Role of Serious Games in Cancer Awareness Among Healthcare Professionals
3.4. The Role of Serious Games in Cancer Awareness Among the Public
3.4.1. Improve Awareness, Education, and Behavioural Change
3.4.2. Considerations on User Experience and Game Design
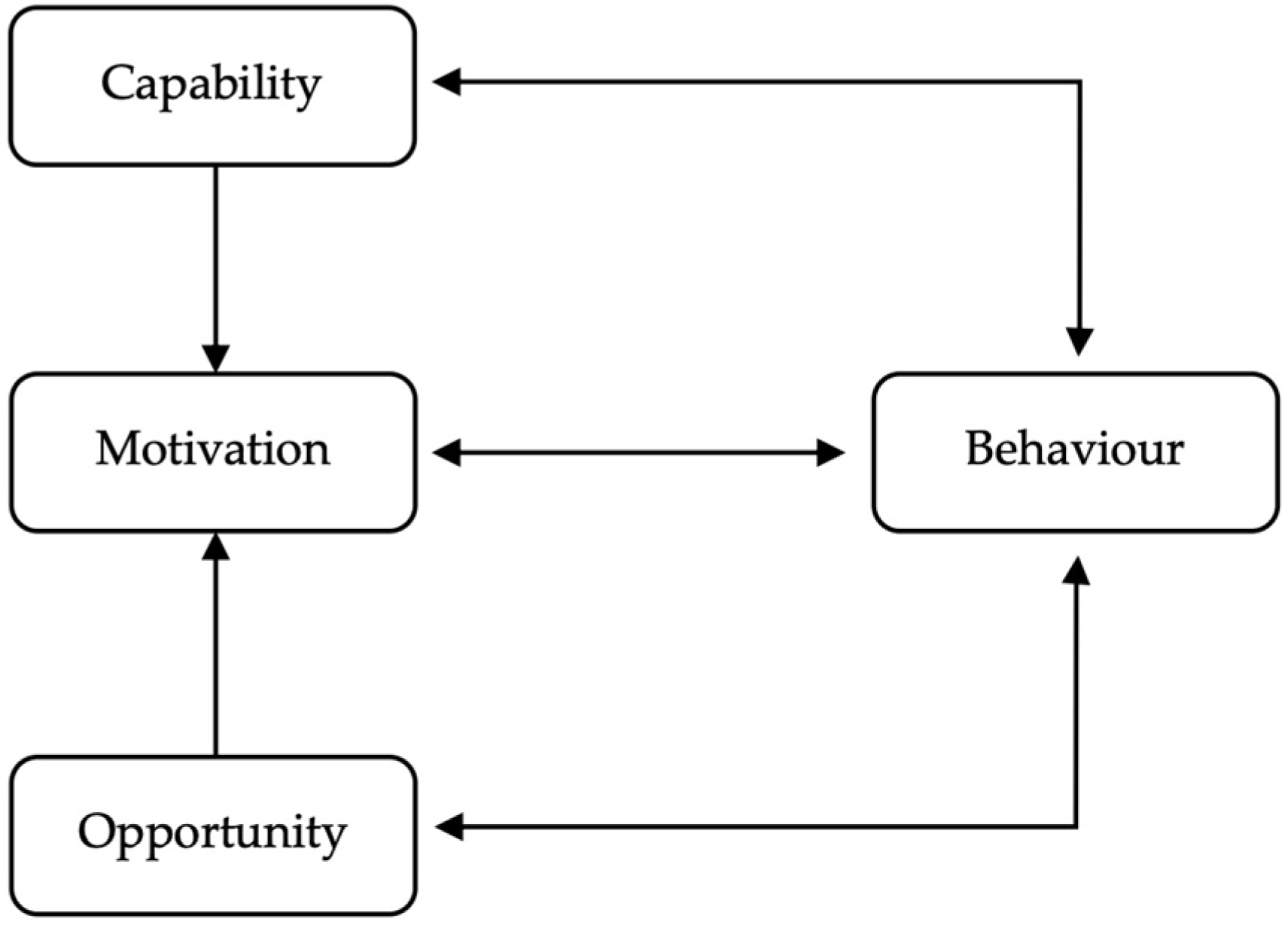
4. Discussion
4.1. Capability
4.2. Opportunity
4.3. Motivation
4.4. Interactions Across COM-B Constructs
4.5. Implications for Design and Implementation
4.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AR | Augmented reality |
| CINV | Chemotherapy-induced nausea and vomiting |
| COM-B | Capability, Opportunity, Motivation-Behaviour |
| GBL | Game-based learning |
| JBI | Joanna Briggs Institute |
| PCC | Population, Concept, and Context |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-analysis extension for Scoping Reviews |
| QoL | Quality of life |
| RCT | Randomized controlled trial |
| UK | United Kingdom |
| USA | United States of America |
| VR | Virtual reality |
| WHO | World Health Organization |
Appendix A
| Reasons for Exclusion | No. | Full Text Articles |
|---|---|---|
| Irrelevant topic (n = 6) | 1 | Chai et al. [76] |
| 2 | Chau et al. [77] | |
| 3 | Chau et al. [78] | |
| 4 | Darville et al. [79] | |
| 5 | Darville-Sanders et al. [80] | |
| 6 | Orumaa et al. [81] | |
| Literature review articles (n = 11) | 7 | Charlier et al [82] |
| 8 | Ejezie et al. [83] | |
| 9 | Fernandes et al. [84] | |
| 10 | Ghazisaeidi et al. [85] | |
| 11 | Huang et al. [86] | |
| 12 | McCann et al. [87] | |
| 13 | Niu et al. [88] | |
| 14 | Poliani et al. [89] | |
| 15 | Robertson et al. [90] | |
| 16 | Safdari et al. [91] | |
| 17 | Savareh et al. [92] | |
| Non-English Language (n = 1) | 18 | Yang et al. [93] |
| Full text not available (n = 7) | 19 | Antoniou et al. [94] |
| 20 | Darville-Sanders et al. [95] | |
| 21 | Khalil et al. [96] | |
| 22 | Roubidoux et al. [97] | |
| 23 | Roubidoux et al. [98] | |
| 24 | Thomas et al. [99] | |
| 25 | You et al. [100]. |
References
- World Health Organization. Cancer Fact Sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 6 July 2025).
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Mao, J.J.; Pillai, G.G.; Andrade, C.J.; Ligibel, J.A.; Basu, P.; Cohen, L.; Khan, I.A.; Mustian, K.M.; Puthiyedath, R.; Dhiman, K.S.; et al. Integrative oncology: Addressing the global challenges of cancer prevention and treatment. CA A Cancer J. Clin. 2022, 72, 144–164. [Google Scholar] [CrossRef]
- Soerjomataram, I.; Bray, F. Planning for tomorrow: Global cancer incidence and the role of prevention 2020–2070. Nat. Rev. Clin. Oncol. 2021, 18, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global cancer incidence and mortality rates and trends—An update. Cancer Epidemiol. Biomark. Prev. 2016, 25, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.J.; Yang, F.; Jin, C.; Fu, D.L. Current status and progress of pancreatic cancer in China. World J. Gastroenterol. 2015, 21, 7988–8003. [Google Scholar] [CrossRef]
- Mettarikanon, D.; Tawanwongsri, W.; Wanchai, A.; Chookerd, N. Comparison of the efficacy between game-based learning and pamphlet on enhancing recognition of common cutaneous malignancies in Thai younger adults. Contemp. Educ. Technol. 2023, 15, ep419. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.Y.; Yang, C.L.; Jen, H.J.; Ogata, H.; Hwang, G.H. Facilitating nursing and health education by incorporating ChatGPT into learning designs. Educ. Technol. Soc. 2024, 27, 215–230. [Google Scholar]
- Fitrianto, I.; Saif, A. The role of virtual reality in enhancing experiential learning: A comparative study of traditional and immersive learning environments. Int. J. Post Axial Futur. Teach. Learn. 2024, 2, 97–110. [Google Scholar]
- Stephenson, C.R.; Bonnes, S.L.; Sawatsky, A.P.; Richards, L.W.; Schleck, C.D.; Mandrekar, J.N.; Beckman, T.J.; Wittich, C.M. The relationship between learner engagement and teaching effectiveness: A novel assessment of student engagement in continuing medical education. BMC Med. Educ. 2020, 20, 403. [Google Scholar] [CrossRef]
- Friedman, A.J.; Cosby, R.; Boyko, S.; Hatton-Bauer, J.; Turnbull, G. Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. J. Cancer Educ. 2011, 26, 12–21. [Google Scholar] [CrossRef]
- Wattanasoontorn, V.; Boada, I.; García, R.; Sbert, M. Serious games for health. Entertain. Comput. 2013, 4, 231–247. [Google Scholar] [CrossRef]
- Wouters, P.; Van Nimwegen, C.; Van Oostendorp, H.; Van Der Spek, E.D. A meta-analysis of the cognitive and motivational effects of serious games. J. Educ. Psychol. 2013, 105, 249. [Google Scholar] [CrossRef]
- Lemos, R.R.; Rudolph, C.M.; Batista, A.V.; Conceição, K.R.; Pereira, P.F.; Bueno, B.S.; Fiuza, P.J.; Mansur, S.S. Design of a Web3D serious game for human anatomy education: A Web3D game for human anatomy education. In Research Anthology on Game Design, Development, Usage, and Social Impact; IGI Global Scientific Publishing: Hershey, PA, USA, 2019; pp. 586–611. [Google Scholar]
- Sturm, D.; Zomick, J.; Loch, I.; McCloskey, D. “Free Will”: A serious game to study the organization of the human brain. In HCI International 2017—Posters’ Extended Abstracts: 19th International Conference; HCI International: Washington, DC, USA, 2017. [Google Scholar]
- Tolks, D.; Schmidt, J.J.; Kuhn, S. The role of AI in serious games and gamification for health: Scoping review. JMIR Serious Games 2024, 12, e48258. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T.; Prue, G.; McDowell, G.; Stark, P.; Brown Wilson, C.; Graham Wisener, L.; Kerr, H.; Caughers, G.; Rogers, K.; Cook, L.; et al. Co-design and evaluation of a digital serious game to promote public awareness about pancreatic cancer. BMC Public Health 2024, 24, 570. [Google Scholar] [CrossRef] [PubMed]
- Carcioppolo, N.; Kim, S.; Sanchez, M.; Mao, B.; Malova, E.; Ryan, A.; Lun, D.; Ewing, C.; Hu, S. Evaluating a game-based randomized experiment to increase melanoma identification among adults living in the U.S. Soc. Sci. Med. 2022, 310, 115281. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, N.; Tavares, P.; Ferreira, C.; Coelho, A. Melanoma prevention using an augmented reality-based serious game. Patient Educ. Couns. 2024, 123, 108226. [Google Scholar] [CrossRef]
- Ruiz-López, T.; Sen, S.; Jakobsen, E.; Tropé, A.; Castle, P.E.; Hansen, B.T.; Nygard, M. FightHPV: Design and evaluation of a mobile game to raise awareness about human papillomavirus and nudge people to take action against cervical cancer. JMIR Serious Games 2019, 7, e8540. [Google Scholar] [CrossRef]
- Gupta, A.; Dhillon, P.K.; Govil, J.; Bumb, D.; Dey, S.; Krishnan, S. Multiple stakeholder perspectives on cancer stigma in north India. Asian Pac. J. Cancer Prev. 2015, 16, 6141–6147. [Google Scholar] [CrossRef]
- Gil, N.; Cox, A.; Whitaker, K.L.; Kerrison, R.S. Cancer risk-factor and symptom awareness among adults with intellectual disabilities, paid and unpaid carers, and healthcare practitioners: A scoping review. J. Intellect. Disabil. Res. 2024, 68, 193–211. [Google Scholar] [CrossRef]
- Dey, S.; Sharma, S.; Mishra, A.; Krishnan, S.; Govil, J.; Dhillon, P.K. Breast cancer awareness and prevention behavior among women of Delhi, India: Identifying barriers to early detection. Breast Cancer Basic Clin. Res. 2016, 10, 147–156. [Google Scholar] [CrossRef]
- Pham, M.T.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; Mclnerney, P.; Godfrey, C.M.; Hanan, K. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Cramer, K.; Wiebe, N.; Moyer, V.; Hartling, L.; Williams, K.; Swingler, G.; Klassen, T.P. Children in reviews: Methodological issues in child-relevant evidence syntheses. BMC Pediatr. 2005, 5, 38. [Google Scholar] [CrossRef][Green Version]
- Chala, M.B.; Elliott, J.; Baker, G.R.; Walton, D.M.; Steele, M.; Schabrun, S. Integrated care for adults with chronic musculoskeletal disorders: A scoping review protocol. JBI Evid. Synth. 2025, 23, 188–196. [Google Scholar] [CrossRef]
- Austoker, J.; Bankhead, C.; Forbes, L.; Atkins, L.; Martin, F.; Robb, K.; Wardle, J.; Ramirez, A. Interventions to promote cancer awareness and early presentation: Systematic review. Nat. Preced. 2009. [Google Scholar] [CrossRef]
- Le Boutillier, C.; Archer, S.; Barry, C.; King, A.; Mansfield, L.; Urch, C. Conceptual framework for living with and beyond cancer: A systematic review and narrative synthesis. Psychooncology 2019, 28, 948–959. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Kato, P.M.; Cole, S.W.; Bradlyn, A.S.; Pollock, B.H. A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics 2008, 122, e305–e317. [Google Scholar] [CrossRef]
- Beale, I.L.; Kato, P.M.; Marin-Bowling, V.M.; Guthrie, N.; Cole, S.W. Improvement in cancer-related knowledge following use of a psychoeducational video game for adolescents and young adults with cancer. J. Adolesc. Health 2007, 41, 263–270. [Google Scholar] [CrossRef]
- Beale, I.L.; Marín-Bowling, V.M.; Guthrie, N.; Kato, P.M. Young cancer patients’ perceptions of a video game used to promote self care. Int. Electron. J. Health Educ. 2006, 9, 202–212. [Google Scholar]
- Cosma, G.; Shopland, N.; Battersby, S.; Seymour-Smith, S.; Pockley, A.G.; Archer, M.; Thompson, R.; Khan, M.; Brown, D. Co-design of a prostate cancer serious game for African Caribbean men. In Proceedings of the 2015 International Conference on Interactive Technologies and Games, Nottingham, UK, 22–23 October 2015. [Google Scholar]
- Cosma, G.; Brown, D.; Shopland, N.; Battersby, S.; Seymour-Smith, S.; Archer, M.; Khan, M.; Pockley, G. PROCEE: A PROstate Cancer Evaluation and Education serious game for African Caribbean men. J. Assist. Technol. 2016, 10, 199–210. [Google Scholar] [CrossRef]
- Horsham, C.; Dutton-Regester, K.; Antrobus, J.; Goldston, A.; Price, H.; Ford, H.; Hacker, E. A virtual reality game to change sun protection behavior and prevent cancer: User-centered design approach. JMIR Serious Games 2021, 9, e24652. [Google Scholar] [CrossRef]
- Oliveira, T.N.C.D.; Figueiredo, J.A.D.; Rodrigues, M.A.F. A Tamagotchi-style game for interactive thyroid cancer care and education. In Proceedings of the 2024 IEEE 12th International Conference on Serious Games and Applications for Health (SeGAH), Funchal, Portugal, 7–9 August 2024. [Google Scholar]
- Brown-Johnson, C.G.; Berrean, B.; Cataldo, J.K. Development and usability evaluation of the mHealth Tool for Lung Cancer (mHealth TLC): A virtual world health game for lung cancer patients. Patient Educ. Couns. 2015, 98, 506–511. [Google Scholar] [CrossRef]
- Loerzel, V.W.; Clochesy, J.M.; Geddie, P.I. Using serious games to increase prevention and self-management of chemotherapy-induced nausea and vomiting in older adults with cancer. Oncol. Nurs. Forum 2020, 47, 567–576. [Google Scholar] [CrossRef]
- Wu, C.H.; Huang, Y.C.; Chiang, D.H.; Yang, Y.Y.; Yang, L.Y.; Kao, S.Y.; Chen, C.H.; Lee, F.Y. A quality improvement pilot project of training nurses to use VR educational aids to increase oral cancer patients pretreatment knowledge and satisfaction. Eur. J. Oncol. Nurs. 2020, 49, 101858. [Google Scholar] [CrossRef] [PubMed]
- Khalil, G.E.; Beale, I.L.; Chen, M.; Prokhorov, A.V. A video game promoting cancer risk perception and information seeking behavior among young-adult college students: A randomized controlled trial. JMIR Serious Games 2016, 4, e5793. [Google Scholar] [CrossRef] [PubMed]
- Zhu, A.; Amith, M.; Tang, L.; Cunningham, R.; Xu, A.; Boom, J.A.; Tao, C. Experimenting with a prototype interactive narrative game to improve knowledge and beliefs for the HPV vaccine. HCI Int. 2021, 13097, 186–201. [Google Scholar]
- Andrew Tong, J.W.; Hee, M.Q. The impact of an online educational game on breast ancer awareness among university female students, Malaysia: A pilot study. BMC Cancer 2023, 23, 947. [Google Scholar] [CrossRef]
- Sharma, A.; Ilyas, M.; Maganty, N.; Zhang, N.; Pittelkow, M.R. An effective game-based learning intervention for improving melanoma recognition. J. Am. Acad. Dermatol. 2018, 79, 587–588. [Google Scholar] [CrossRef]
- Sloan, R.J.S.; Saurin, A. The Enemy Within: Designing a cell-based gameplay system for cancer education. In Extended Abstracts of the Annual Symposium on Computer-Human Interaction in Play Companion Extended Abstracts; Association for Computing Machinery: Barcelona, Spain, 2019; pp. 117–123. [Google Scholar]
- Nirmal, R.; Chang, Y.; Le, M.; Paripoonnanonda, P.; Yi, J. Digital health game on cervical health and its effect on American women’s cervical cancer knowledge. In Proceedings of the 2013 IEEE International Games Innovation Conference (IGIC), Vancouver, BC, Canada, 23–25 September 2013. [Google Scholar]
- You, K.L.; Delaney, R.K.; McKinley, N.; Healy, P.; Thomas, T.H. Who engages and why it matters?: Describing participant engagement in a serious game intervention for patients with advanced cancer. Int. J. Gaming Comput.-Mediat. Simul. (IJGCMS) 2023, 15, 1–13. [Google Scholar] [CrossRef]
- Maganty, N.; Ilyas, M.; Zhang, N.; Sharma, A. Online, game-based education for melanoma recognition: A pilot study. Patient Educ. Couns. 2018, 101, 738–742. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, S.M.; Shin, H.; Jang, J.S.; Kim, Y.I.; Han, D.H. A mobile game for patients with breast cancer for chemotherapy self-management and quality-of-life improvement: Randomized controlled Trial. J. Med. Internet Res. 2018, 20, e273. [Google Scholar] [CrossRef]
- Krebs, P.; Burkhalter, J.; Fiske, J.; Snow, H.; Schofield, E.; Iocolano, M.; Borderud, S.; Ostroff, J.S. The QuitIT coping skills game for promoting tobacco cessation among smokers diagnosed with cancer: Pilot randomized controlled trial. JMIR Mhealth Uhealth 2019, 7, e10071. [Google Scholar] [CrossRef] [PubMed]
- Wanberg, L.J.; Kim, A.; Vogel, R.I.; Sadak, K.T.; Teoh, D. Usability and satisfaction testing of game-based learning Avatar-Navigated Mobile (GLAm), an app for cervical cancer screening: Mixed methods study. JMIR Form. Res. 2023, 7, e45541. [Google Scholar] [CrossRef] [PubMed]
- Kato, P.M.; Beale, I.L. Factors affecting acceptability to young cancer patients of a psychoeducational video game about cancer. J. Pediatr. Oncol. Nurs. 2006, 23, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Reichlin, L.; Mani, N.; McArthur, K.; Harris, A.; Rajan, N.; Dacso, C. Assessing the acceptability and usability of an interactive serious game in aiding treatment decisions for patients with localized prostate cancer. J. Med. Internet Res. 2011, 13, e1519. [Google Scholar] [CrossRef]
- Kayed, J.E.; Akl, T.; Massoud, C.; Margossian, C.; Fayad, H.; Fares, G.; Felefly, T.; Rihana, S. Serious game for radiotherapy training. BMC Med. Educ. 2024, 24, 463. [Google Scholar] [CrossRef]
- Brown, D.; Cosma, G.; Acampora, G.; Seymour-Smith, S.; Close, A. An intelligent serious game for supporting African and African Caribbean men during pre- and post-diagnosis of prostate cancer. In Proceedings of the 2014 International Conference on Interactive Technologies and Games, Nottingham, UK, 16–17 October 2014. [Google Scholar]
- Loerzel, V.; Clochesy, J.; Geddie, P. Using a community advisory board to develop a serious game for older adults undergoing treatment for cancer. Appl. Nurs. Res. 2018, 39, 207–210. [Google Scholar] [CrossRef]
- Cerqueira, F.; Ferreira, M.C.; Campos, M.J.; Fernandes, C.S. PocketOnco®: Prototyping a mobile app for health literacy and self-management of oncological diseases. Comput. Methods Programs Biomed. 2025, 261, 108649. [Google Scholar] [CrossRef]
- Magro, A.; Swarz, J.; Ousley, A. CancerSPACE: An interactive e-learning tool aimed to improve cancer screening rates. J. Comput.-Mediat. Commun. 2010, 15, 482–499. [Google Scholar] [CrossRef]
- Pereira, Y.H.; Ueda, R.; Galhardi, L.B.; Brancher, J.D. Using procedural content generation for storytelling in a serious game called Orange Care. In Proceedings of the 2019 18th Brazilian Symposium on Computer Games and Digital Entertainment (SBGames), Rio de Janeiro, Brazil, 28–31 October 2019. [Google Scholar]
- Swarz, J.; Ousley, A.; Magro, A.; Rienzo, M.; Burns, D.; Lindsey, A.M.; Wilburn, B.; Bolcar, S. CancerSpace: A simulation-based game for improving cancer-screening rates. IEEE Comput. Graph. Appl. 2010, 30, 90–94. [Google Scholar] [CrossRef]
- Anderson, T.; Shattuck, J. Design-based research: A decade of progress in education research? Educ. Res. 2012, 41, 16–25. [Google Scholar] [CrossRef]
- West, R.; Michie, S. A brief introduction to the COM-B Model of behaviour and the PRIME Theory of motivation. Qeios 2020. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Pearson, E.; Byrne-Davis, L.; Bull, E.; Hart, J. Behavior change techniques in health professional training: Developing a coding tool. Transl. Behav. Med. 2020, 10, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Social Change UK. A Guide on the COM-B Model of Behaviour. Available online: https://social-change.co.uk/files/12.01.23_A_guide_on_the_COM-B_model_of_behaviour_.pdf (accessed on 15 August 2025).
- Willmott, T.J.; Pang, B.; Rundle-Thiele, S. Capability, opportunity, and motivation: An across contexts empirical examination of the COM-B model. BMC Public Health 2021, 21, 1014. [Google Scholar] [CrossRef]
- Brown, C.E.; Richardson, K.; Halil-Pizzirani, B.; Atkins, L.; Yücel, M.; Segrave, R.A. Key influences on university students’ physical activity: A systematic review using the Theoretical Domains Framework and the COM-B model of human behaviour. BMC Public Health 2024, 24, 418. [Google Scholar] [CrossRef]
- Marques, M.M.; Wright, A.J.; Corker, E.; Johnston, M.; West, R.; Hastings, J.; Zhang, L.; Michie, S. The behaviour change technique ontology: Transforming the behaviour change technique taxonomy v1. Wellcome Open Res. 2024, 8, 308. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Reardon, C.M.; Widerquist, M.A.; Lowery, J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement. Sci. 2022, 17, 75. [Google Scholar] [CrossRef]
- Wang, Y.; Wong, E.L.; Nilsen, P.; Chung, V.C.; Tian, Y.; Yeoh, E.K. A scoping review of implementation science theories, models, and frameworks—An appraisal of purpose, characteristics, usability, applicability, and testability. Implement. Sci. 2023, 18, 43. [Google Scholar] [CrossRef]
- Western, M.J.; Armstrong, M.E.; Islam, I.; Morgan, K.; Jones, U.F.; Kelson, M.J. The effectiveness of digital interventions for increasing physical activity in individuals of low socioeconomic status: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 148. [Google Scholar] [CrossRef]
- Albarracín, D.; Fayaz-Farkhad, B.; Granados Samayoa, J.A. Determinants of behaviour and their efficacy as targets of behavioural change interventions. Nat. Rev. Psychol. 2024, 3, 377–392. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, K.S.; Cologna, V.; Bauer, J.M.; Berger, S.; Brick, C.; Dietz, T.; Hahnel, U.J.J.; Henn, L.; Lange, F.; Stern, P.C.; et al. Realizing the full potential of behavioural science for climate change mitigation. Nat. Clim. Change 2024, 14, 322–330. [Google Scholar] [CrossRef]
- Tay, P.K.C.; Anderson, T.; Ying, J.S.J.; Siow, E.K.C.; Craig, S.; Mitchell, G.; Wilson, C.B. Evaluation of a digital Dementia Game to promote public awareness about dementia in Singapore. BMC Public Health 2025, 25, 1873. [Google Scholar] [CrossRef] [PubMed]
- Mulyani, S.; Mitchell, G.; Carter, G.; Woods, B.; Warsini, S.; Saifullah, A.D.; Ulayya, A.I.; Wilson, C.B. Validity and reliability of the Approaches to Dementia Questionnaire (ADQ) in Indonesian health students. BMC Med. Educ. 2025, 25, 798. [Google Scholar] [CrossRef]
- Chai, C.W.E.; Lau, B.T.; Tee, M.K.T.; Al Mahmud, A. Evaluating a serious game to improve childhood cancer patients’ treatment adherence. Digit. Health 2022, 8, 20552076221134457. [Google Scholar] [CrossRef]
- Chau, J.P.C.; Lo, S.H.S.; Butt, L.; Lee, V.W.Y.; Lui, G.C.Y.; Lau, A.Y.L. User Engagement on a novel educational health intervention aimed at increasing HPV vaccine uptake in Hong Kong: A qualitative study. J. Cancer Educ. 2023, 38, 772–780. [Google Scholar] [CrossRef]
- Chau, J.P.C.; Lo, S.H.S.; Choi, K.C.; Lee, V.W.Y.; Lui, G.C.Y.; Chan, K.M.; Lau, A.Y.L. Effects of a multidisciplinary team-led school-based human papillomavirus vaccination health-promotion programme on improving vaccine acceptance and uptake among female adolescents: A cluster randomized controlled trial. Medicine 2020, 99, e22072. [Google Scholar] [CrossRef]
- Darville, G.; Burns, J.; Chavanduka, T.; Anderson-Lewis, C. Utilizing theories and evaluation in digital gaming interventions to increase human papillomavirus vaccination among young males: Qualitative study. JMIR Serious Games 2021, 9, e21303. [Google Scholar] [CrossRef]
- Darville-Sanders, G.; Anderson-Lewis, C.; Stellefson, M.; Lee, Y.H.; MacInnes, J.; Pigg, R.M.; Mercado, R.; Gaddis, C. mHealth video gaming for human papillomavirus vaccination among college men—Qualitative inquiry for development. mHealth 2022, 8, 22. [Google Scholar] [CrossRef]
- Orumaa, M.; Campbell, S.; Stoer, N.C.; Castle, P.E.; Sen, S.; Trope, A.; Adedimeji, A.; Nygard, M. Impact of the mobile game FightHPV on cervical cancer screening attendance: Retrospective cohort study. JMIR Serious Games 2022, 10, e36197. [Google Scholar] [CrossRef]
- Charlier, N.; Zupancic, N.; Fieuws, S.; Denhaerynck, K.; Zaman, B.; Moons, P. Serious games for improving knowledge and self-management in young people with chronic conditions: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2016, 23, 230–239. [Google Scholar] [CrossRef]
- Ejezie, C.L.; Sacca, L.; Ayieko, S.; Burgoa, S.; Zerrouki, Y.; Lobaina, D.; Okwaraji, G.; Markham, C. Use of digital health interventions for cancer prevention among people living With disabilities in the United States: A scoping review. Cancer Med. 2025, 14, e70571. [Google Scholar] [CrossRef]
- Fernandes, C.S.; Magalhaes, B.; Santos, C.; Martines-Galiano, J. The use of games in the self-management of oncological disease: An integrative literature review. Online J. Nurs. Inform. 2019, 23, 7-1. [Google Scholar]
- Ghazisaeidi, M.; Safdari, R.; Goodini, A.; Mirzaiee, M.; Farzi, J. Digital games as an effective approach for cancer management: Opportunities and challenges. J. Educ. Health Promot. 2017, 6, 30. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Xiang, X.; Liu, Y.; Wang, Z.; Jiang, Z.; Huang, L. The use of gamification in the self-management of patients with chronic diseases: Scoping review. JMIR Serious Games 2023, 11, e39019. [Google Scholar] [CrossRef] [PubMed]
- McCann, L.; McMillan, K.A.; Pugh, G. Digital interventions to support adolescents and young adults with cancer: Systematic review. JMIR Cancer 2019, 5, e12071. [Google Scholar] [CrossRef]
- Niu, Z.; Bhurosy, T.; Heckman, C.J. Digital interventions for promoting sun protection and skin self-examination behaviours: A systematic review. Prev. Med. Rep. 2022, 26, 101709. [Google Scholar] [CrossRef] [PubMed]
- Poliani, A.; Gnecchi, S.; Villa, G.; Rosa, D.; Manara, D.F. Gamification as an educational approach for oncological patients: A systematic scoping review. Healthcare 2023, 11, 3116. [Google Scholar] [CrossRef]
- Robertson, E.G.; Wakefield, C.E.; Marshall, K.H.; Sansom-Daly, U.M. Strategies to improve adherence to treatment in adolescents and young adults with cancer: A systematic review. Clin. Oncol. Adolesc. Young Adults 2015, 5, 35–49. [Google Scholar] [CrossRef]
- Safdari, R.; Ghazisaeidi, M.; Goodini, A.; Mirzaee, M.; Farzi, J. Electronic game: A key effective technology to promote behavioral change in cancer patients. J. Cancer Res. Ther. 2016, 12, 474–480. [Google Scholar] [CrossRef]
- Savareh, B.A.; Karandish, Z.; Farhoudi, F.; Bashiri, A. Pain management in cancer patients: The effectiveness of digital game-based interventions: A rapid literature review. Healthc. Inform. Res. 2024, 30, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Zhang, R.; Song, D. Research on development expectation of popular science games on treatment and prevention of cancer based on audience psychology. Chin. Nurs. Res. 2017, 31, 4539–4541. [Google Scholar]
- Antoniou, P.E.; Rivera-Romero, O.; Karagianni, M.; Bamidis, P.D. Towards evidence based m-health application design in cancer patient healthy lifestyle interventions. In Proceedings of the 2017 IEEE 30th International Symposium on Computer-Based Medical Systems, Thessaloniki, Greece, 22–24 June 2017; pp. 690–695. [Google Scholar]
- Darville-Sanders, G.; Burns, J.; Chavanduka, T.; Anderson-Lewis, C. The male domain-digital game-based learning for human papillomavirus vaccination among young males. Games Health J. 2022, 11, 312–320. [Google Scholar] [PubMed]
- Khalil, G.E. When losing meas winning: The impact of conflict in a digital game on the young adults’ intentions to get protected from cancer. Games Health J. 2012, 1, 279–286. [Google Scholar] [CrossRef]
- Roubidoux, M.A. Breast cancer detective: A computer game to teach breast cancer screening to native American patients. J. Cancer Educ. 2005, 20 (Suppl. 1), 87–91. [Google Scholar] [CrossRef]
- Roubidoux, M.A.; Hilmes, M.; Abate, S.; Burhansstipanov, L.; Trapp, M.A. Development of computer games to teach breast cancer screening to native American patients and their healthcare providers. J. Women’s Imaging 2005, 7, 77–95. [Google Scholar] [CrossRef]
- Thomas, T.H.; McLaughlin, M.; Hayden, M.; Shumaker, E.; Trybus, J.; Myers, E.; Zabiegalski, A.; Cohen, S.M. Teaching patients with advanced cancer to self-advocate: Development and acceptability of the Strong Together TM serious game. Games Health J. 2019, 8, 55–63. [Google Scholar] [CrossRef]
- You, K.L.; Schenker, Y.; Bender, C.; McKinley, N.; Rosenzweig, P.; Thomas, T. Describing cancer survivors’ engagement in a serious game intervention: Who engages and why it matters. Oncol. Nurs. Forum 2021, 48, 13–14. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Si, G.; Prue, G.; Craig, S.; Anderson, T.; Mitchell, G. Digital Serious Games for Cancer Education and Behavioural Change: A Scoping Review of Evidence Across Patients, Professionals, and the Public. Cancers 2025, 17, 3368. https://doi.org/10.3390/cancers17203368
Si G, Prue G, Craig S, Anderson T, Mitchell G. Digital Serious Games for Cancer Education and Behavioural Change: A Scoping Review of Evidence Across Patients, Professionals, and the Public. Cancers. 2025; 17(20):3368. https://doi.org/10.3390/cancers17203368
Chicago/Turabian StyleSi, Guangyan, Gillian Prue, Stephanie Craig, Tara Anderson, and Gary Mitchell. 2025. "Digital Serious Games for Cancer Education and Behavioural Change: A Scoping Review of Evidence Across Patients, Professionals, and the Public" Cancers 17, no. 20: 3368. https://doi.org/10.3390/cancers17203368
APA StyleSi, G., Prue, G., Craig, S., Anderson, T., & Mitchell, G. (2025). Digital Serious Games for Cancer Education and Behavioural Change: A Scoping Review of Evidence Across Patients, Professionals, and the Public. Cancers, 17(20), 3368. https://doi.org/10.3390/cancers17203368








