Global Burden of Pancreatic Cancer Among Individuals Aged 15–59 Years in 204 Countries and Territories, 1990–2021: A Systematic Analysis for the GBD 2021 and Projections to 2045
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design and Population
2.3. Statistical Analysis
2.4. Data Visualization
2.5. Ethical Considerations
3. Results
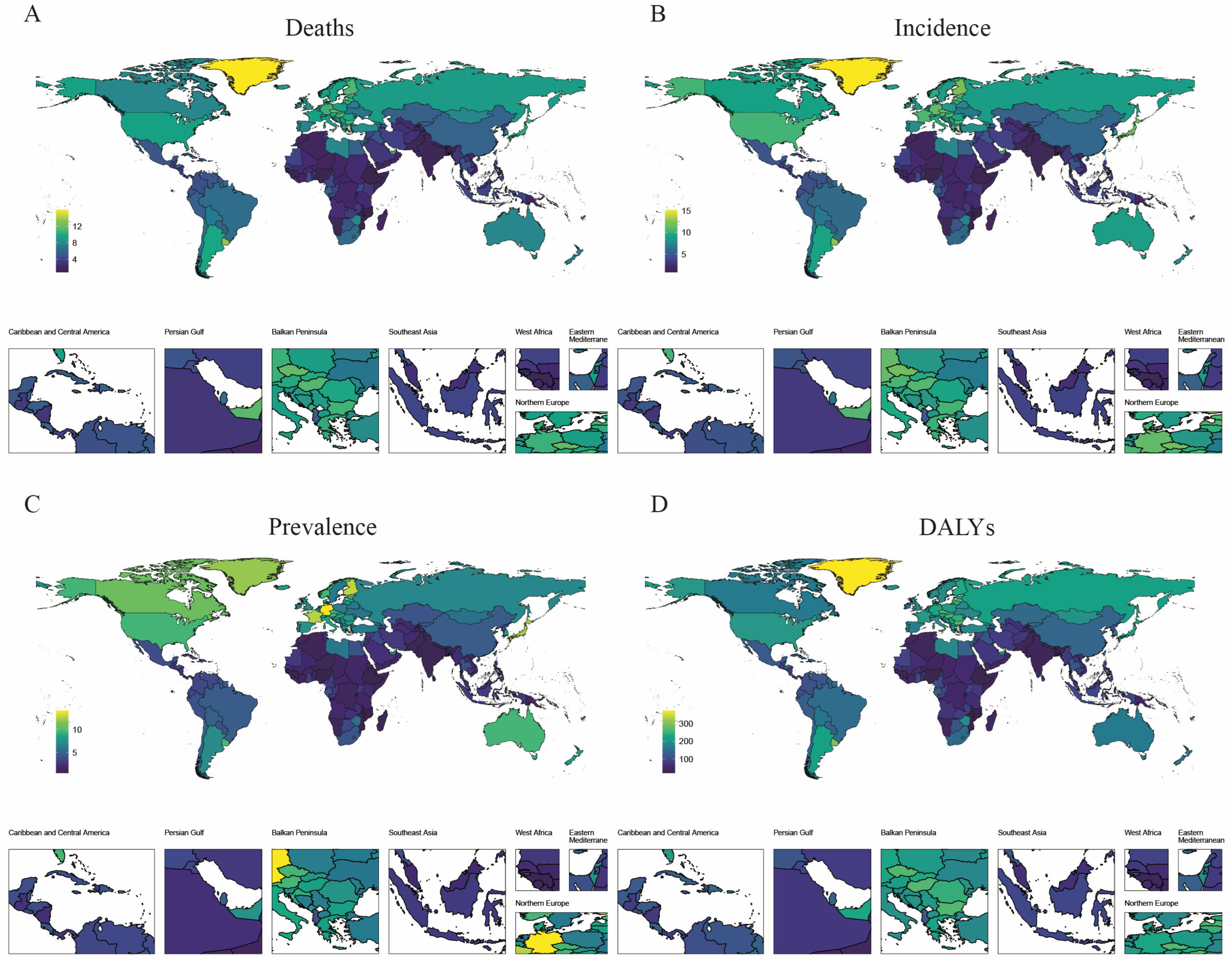
3.1. Disease Burden Due to Pancreatic Cancer by Regions and Countries
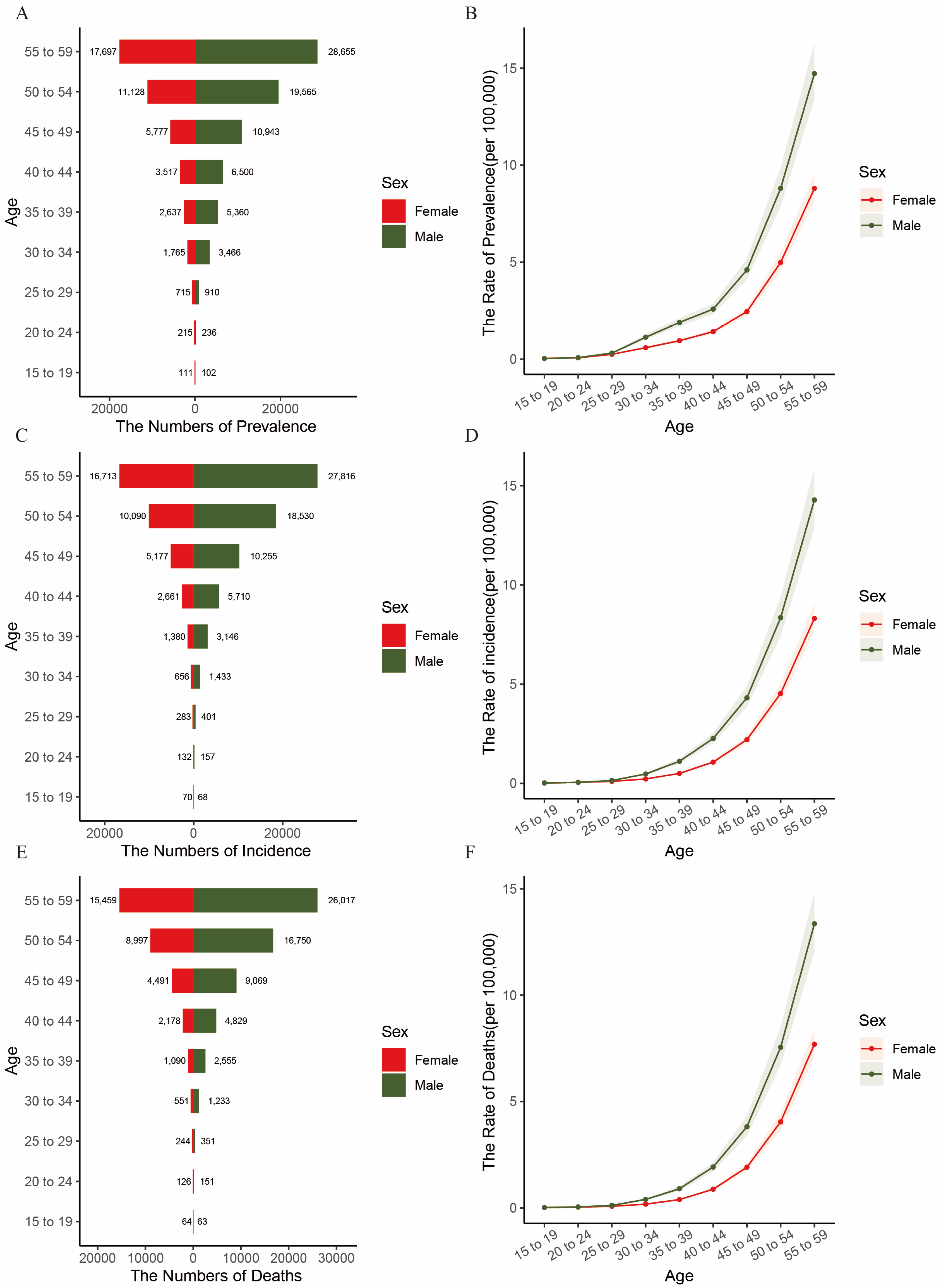
3.2. Incidence, Prevalence and Mortality of Pancreatic Cancer in China, 2021
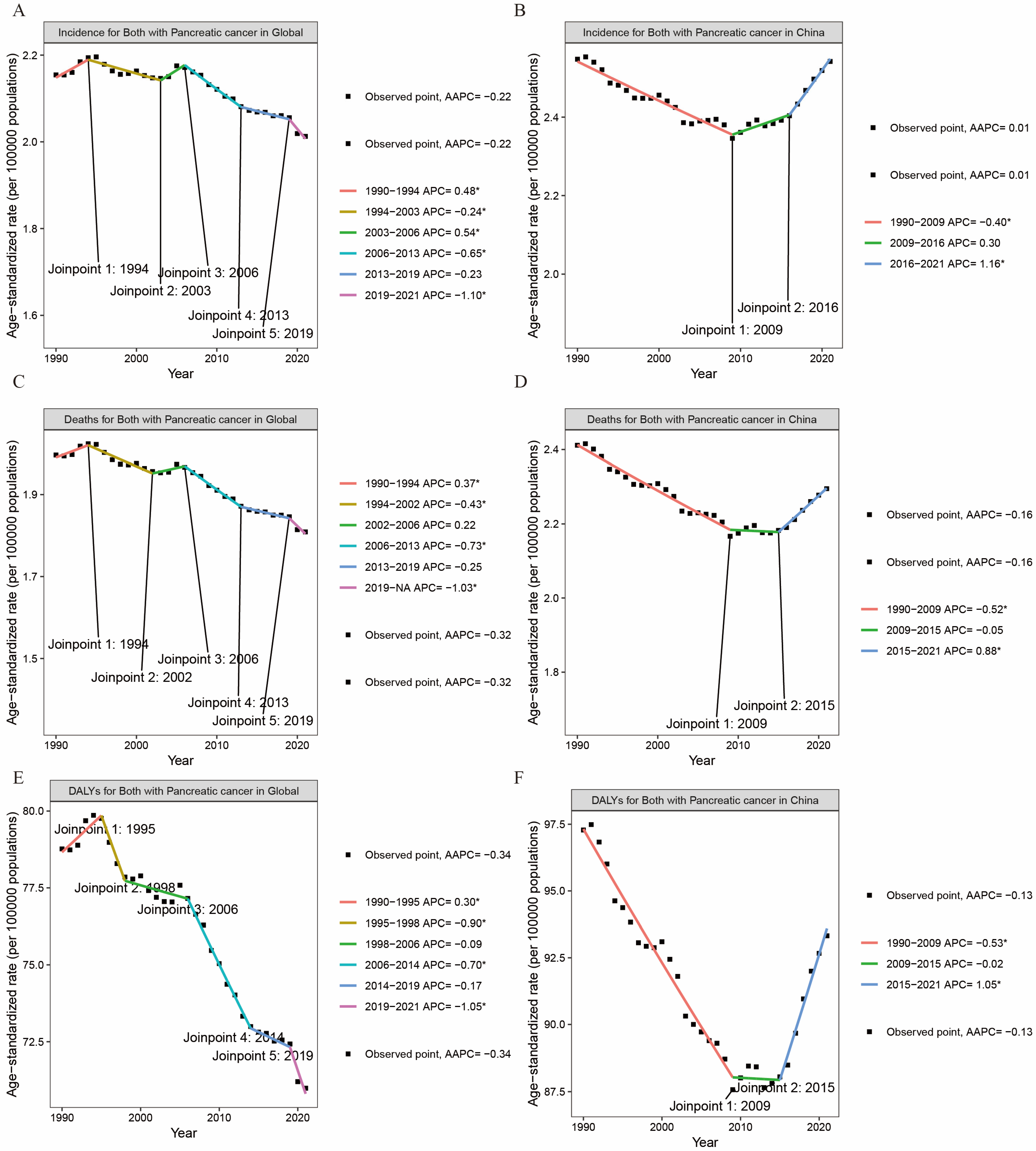
3.3. Analysis of Trends by Gender Based on the Joinpoint Regression Model, 1992–2021
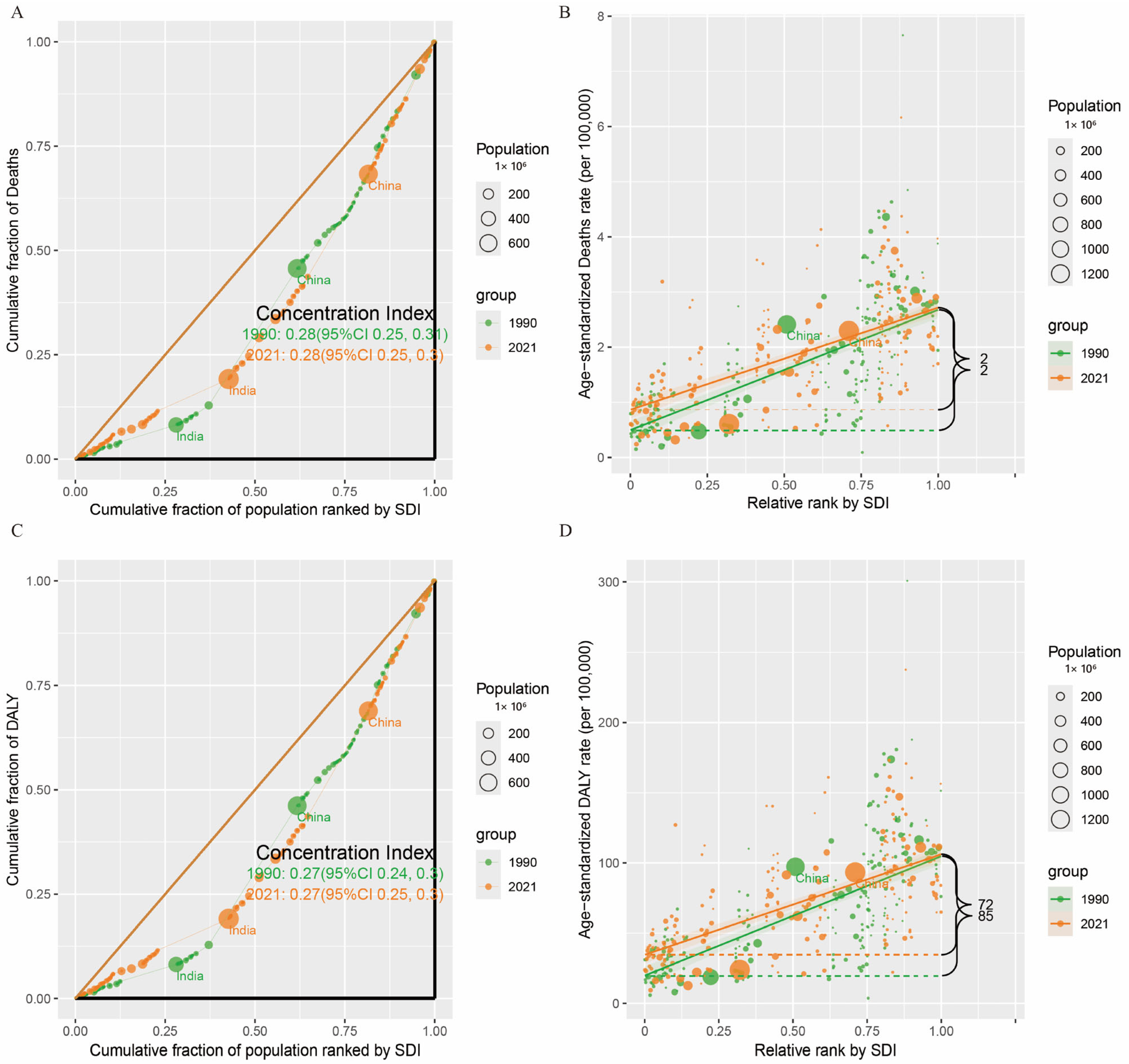
3.4. Cross-Country Social Inequalities Analysis
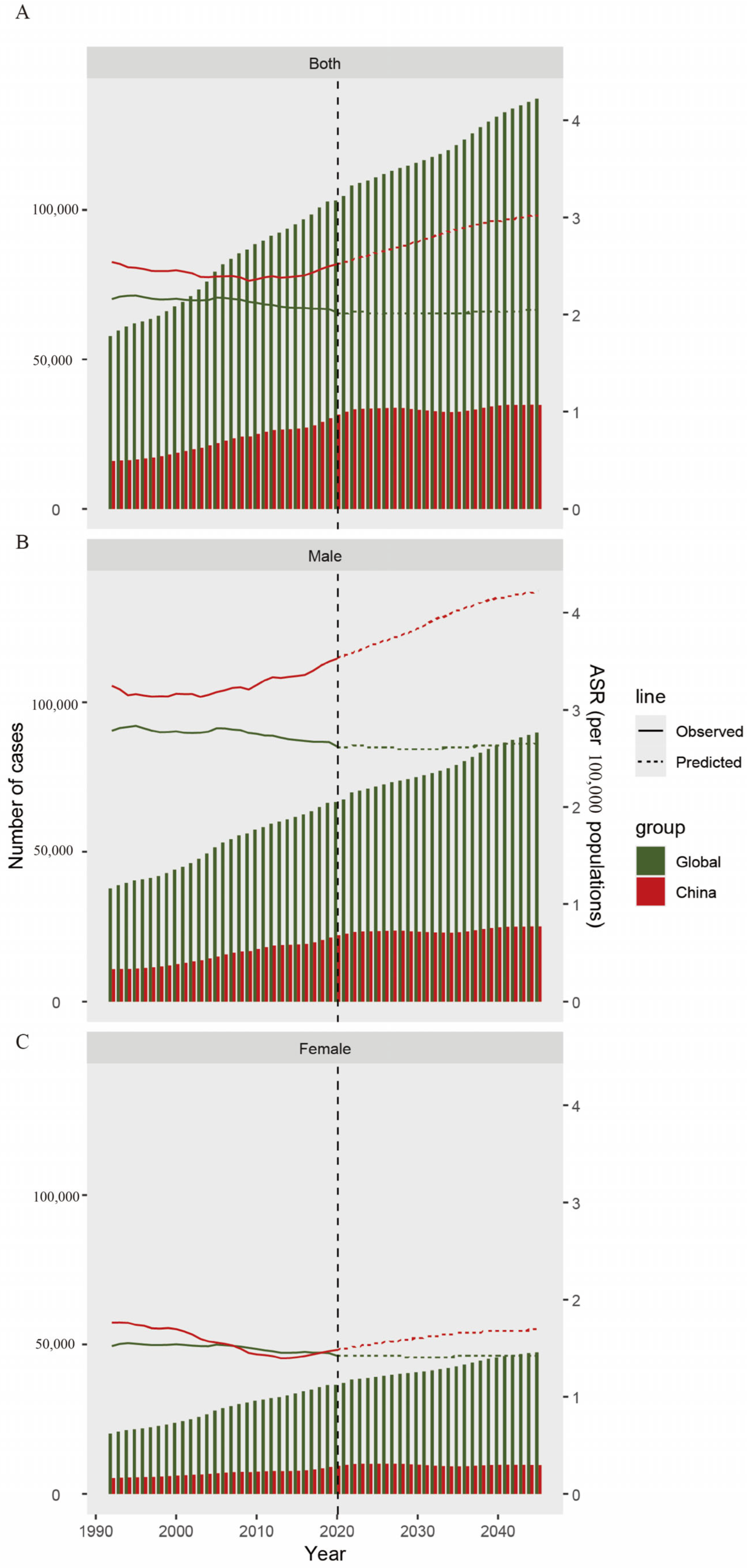
3.5. Predictions of Disease Burden
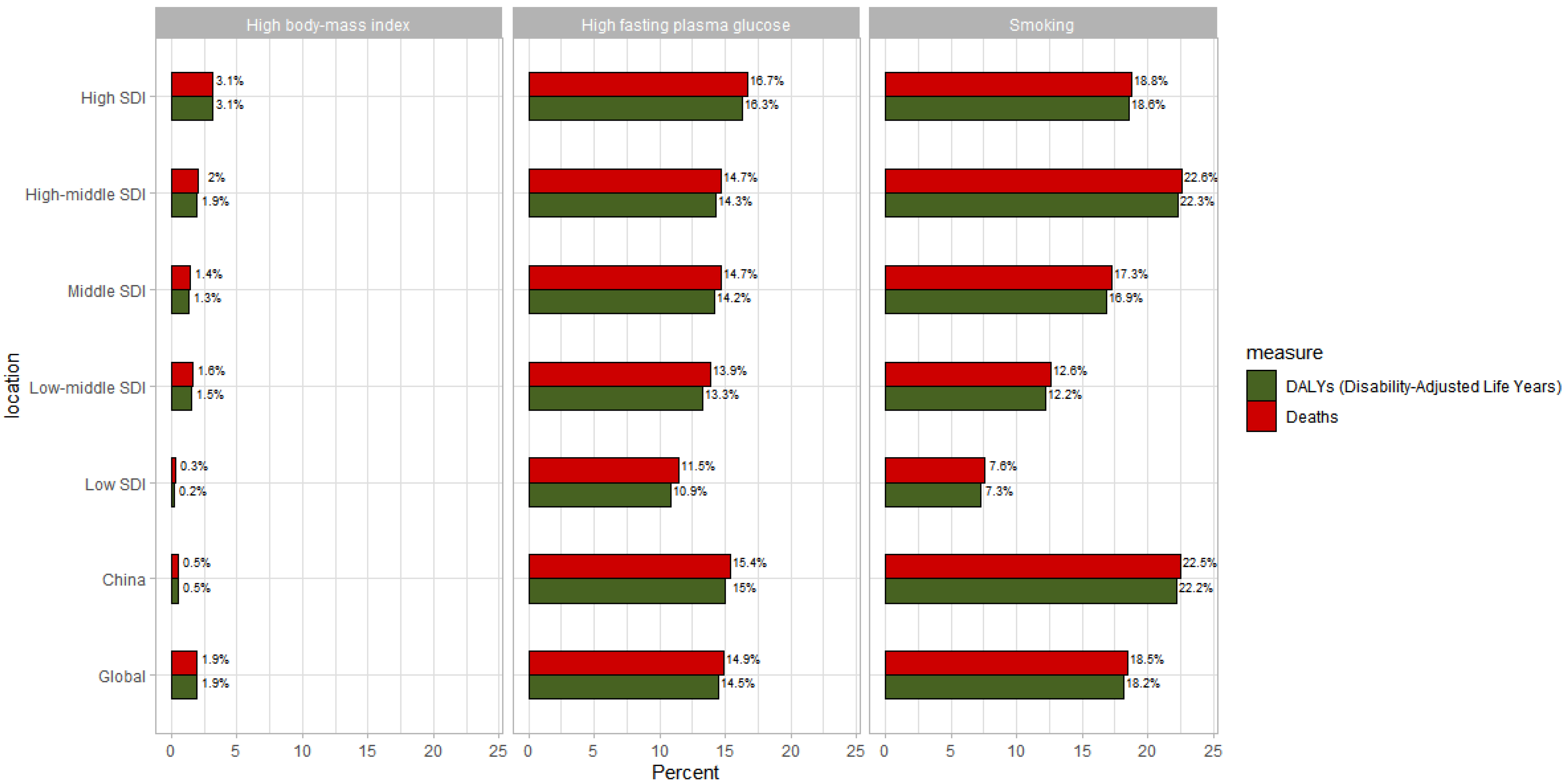
3.6. Attribution Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DALYs | Disability-adjusted life-years |
| ASDR | Age-standardized death rate |
| ASIR | Age-standardized incidence rate |
| ASPR | Age-standardized prevalence rate |
| PC | Pancreatic cancer |
| APC | Age-period-cohort |
| ASR | Age-standardized rate |
References
- Siegel, R.L.; Kratzer, T.B.; Giaquinto, A.N.; Sung, H.; Jemal, A. Cancer statistics, 2025. CA Cancer J. Clin. 2025, 75, 10–45. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wood, L.D.; Canto, M.I.; Jaffee, E.M.; Simeone, D.M. Pancreatic Cancer: Pathogenesis, Screening, Diagnosis, and Treatment. Gastroenterology 2022, 163, 386–402.e1. [Google Scholar] [CrossRef] [PubMed]
- Rahib, L.; Smith, B.D.; Aizenberg, R.; Rosenzweig, A.B.; Fleshman, J.M.; Matrisian, L.M. Projecting cancer incidence and deaths to 2030: The unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014, 74, 2913–2921. [Google Scholar] [CrossRef]
- Siegel Rebecca, L.; Kimberly, D. Miller, Nikita Sandeep Wagle, Ahmedin Jemal. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar]
- Li, Z.; Zhang, X.; Guo, C.; Sun, C.; Li, Z.; Fei, H.; Chen, Y.; Zhao, D. Exploration of the lymphadenectomy strategy for elderly pancreatic ductal adenocarcinoma patients undergoing curative-intent resection. Am. J. Cancer Res. 2023, 13, 1938–1951. [Google Scholar]
- Bleyer, W.A.; Barr, R.D.; Ries, L.; Whelan, J.; Ferrari, A. Cancer in Adolescents and Young Adults; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Bhatia, S.; Pappo, A.S.; Acquazzino, M.; Allen-Rhoades, W.A.; Barnett, M.; Borinstein, S.C.; Casey, R.; Choo, S.; Chugh, R.; Dinner, S.; et al. Adolescent and young adult (AYA) oncology, version 2.2024, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2023, 21, 851–880. [Google Scholar] [CrossRef]
- Patterson, P.; McDonald, F.E.J.; Zebrack, B.; Medlow, S. Emerging issues among adolescent and young adult cancer survivors. Semin. Oncol. Nurs. 2015, 31, 53–59. [Google Scholar] [CrossRef]
- Chen, S.; Cao, Z.; Prettner, K.; Kuhn, M.; Yang, J.; Jiao, L.; Wang, Z.; Li, W.; Geldsetzer, P.; Bärnighausen, T.; et al. Estimates and projections of the global economic cost of 29 cancers in 204 countries and territories from 2020 to 2050. JAMA Oncol. 2023, 9, 465. [Google Scholar] [CrossRef]
- Turgeman, I.; West, H. Adolescents and young adults with cancer. JAMA Oncol. 2023, 9, 440. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2162–2203, Erratum in Lancet 2024, 404, 244. [Google Scholar] [CrossRef]
- GBD 2021 Demographics Collaborators. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: A comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 1989–2056. [Google Scholar] [CrossRef]
- Kim, H.J.; Chen, H.S.; Byrne, J.; Wheeler, B.; Feuer, E.J. Twenty years since Joinpoint 1.0: Two major enhancements. their justification, and impact. Stat. Med. 2022, 41, 3102–3130. [Google Scholar] [CrossRef]
- Tu, Y.K.; Krämer, N.; Lee, W.C. Addressing the identification problem in age-period-cohort analysis: A tutorial on the use of partial least squares and principal components analysis. Epidemiology 2012, 23, 583–593. [Google Scholar] [CrossRef]
- Kirkegaard, J. Incidence of pancreatic cancer in Greenland 2000–2010. Int. J. Circumpolar Health 2012, 71, 18368. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, Z.; Zhang, X.; Sun, C.; Li, Z.; Fei, H.; Zhao, D. Global, regional, and national burdens of early onset pancreatic cancer in adolescents and adults aged 15–49 years from 1990 to 2019 based on the Global Burden of Disease Study 2019: A cross-sectional study. Int. J. Surg. 2024, 110, 1929–1940. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer. Cancer today. The Global Cancer Observatory. Available online: https://gco.iarc.fr/today/home (accessed on 5 November 2024).
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Brenner, D.R.; Ruan, Y.; Shaw, E.; O’Sullivan, D.; Poirier, A.E.; Heer, E.; Villeneuve, P.J.; Walter, S.D.; Friedenreich, C.M.; Smith, L.; et al. Age-standardized cancer-incidence trends in Canada, 1971–2015. CMAJ 2019, 191, E1262–E1273. [Google Scholar] [CrossRef]
- Gordon-Dseagu, V.L.; Devesa, S.S.; Goggins, M.; Stolzenberg-Solomon, R. Pancreatic cancer incidence trends: Evidence from the Surveillance, Epidemiology and End Results (SEER) population-based data. Int. J. Epidemiol. 2018, 47, 427–439. [Google Scholar] [CrossRef]
- Huang, J.; Lok, V.; Ngai, C.H.; Zhang, L.; Yuan, J.; Lao, X.Q.; Ng, K.; Chong, C.; Zheng, Z.J.; Wong, M.C. Worldwide burden of, risk factors for, and trends in pancreatic cancer. Gastroenterology 2021, 160, 744–754. [Google Scholar] [CrossRef]
- Gupta, S.; Wang, F.; Holly, E.A.; Bracci, P.M. Risk of pancreatic cancer by alcohol dose, duration, and pattern of consumption, including binge drinking: A population-based study. Cancer Causes Control 2010, 21, 1047–1059. [Google Scholar] [CrossRef] [PubMed]
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Benbrahim-Tallaa, L.; Bouvard, V.; Bianchini, F.; Straif, K. International Agency for Research on Cancer Handbook Working Group. Body fatness and cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Body-Mass Index: Evolution of BMI over Time. NCD Risk Factor Collaboration. 2017. Available online: http://ncdrisc.org/obesity-prevalence-line-ado.html (accessed on 8 February 2019).
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [PubMed]
- Huang, J.; Patel, H.K.; Boakye, D.; Chandrasekar, V.T.; Koulaouzidis, A.; Iii, D.E.L.-P.; Ngai, C.H.; Pun, C.N.; Bai, Y.; Lok, V.; et al. Worldwide distribution, associated factors, and trends of gallbladder cancer: A global country-level analysis. Cancer Lett. 2021, 521, 238–251. [Google Scholar]
- Sung, J.J.; Chiu, H.-M.; Jung, K.-W.; Jun, J.K.; Sekiguchi, M.; Matsuda, T.; Kyaw, M.H. Increasing trend in young-onset colorectal cancer in Asia: More cancers in men and more rectal cancers. Am. J. Gastroenterol. 2019, 114, 322–329. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Huang, J.; Pang, T.W.Y. Worldwide incidence and prevalence of metabolic syndrome: A systematic review and meta-analysis of 14.6 million individuals. Gastroenterology 2020, 158, S-1003. [Google Scholar] [CrossRef]
- Collaborators GBDPC. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 934–947. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Jiang, J.Y.; Liang, M.; Fang, Y.; Yeung, M.S.; Sung, J.J.Y. Global temporal patterns of pancreatic cancer and association with socioeconomic development. Sci. Rep. 2017, 7, 3165. [Google Scholar] [CrossRef]
- Poruk, K.E.; Firpo, M.A.; Adler, D.G.; Mulvihill, S.J. Screening for pancreatic cancer: Why, how, and who? Ann. Surg. 2013, 257, 17–26. [Google Scholar] [CrossRef]
- Flor, L.S.; Reitsma, M.B.; Gupta, V.; Ng, M.; Gakidou, E. The effects of tobacco control policies on global smoking prevalence. Nat. Med. 2021, 27, 239–243. [Google Scholar] [CrossRef]
- GBD 2019 Tobacco Collaborators Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021, 397, 2337–2360. [CrossRef] [PubMed]
- GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2100–2132, Erratum in Lancet 2024, 403, 1988. [Google Scholar] [CrossRef] [PubMed]
| Measure | Location | Val | Upper | Lower |
|---|---|---|---|---|
| Deaths | Greenland | 6.163709 | 8.339102 | 4.3568361 |
| Bulgaria | 4.465164 | 5.432986 | 3.6239335 | |
| Latvia | 4.372814 | 5.401602 | 3.5037153 | |
| Romania | 4.175437 | 5.054531 | 3.3858231 | |
| Uruguay | 4.134278 | 4.856886 | 3.4793197 | |
| Incidence | Greenland | 6.653686 | 8.981315 | 4.7168994 |
| Latvia | 4.799047 | 5.927480 | 3.8498763 | |
| Bulgaria | 4.786269 | 5.831670 | 3.8642011 | |
| Monaco | 4.562883 | 7.189736 | 2.6233051 | |
| Uruguay | 4.491356 | 5.278130 | 3.7705617 | |
| DALYs | Greenland | 237.61867 | 322.12296 | 167.39080 |
| Bulgaria | 173.03564 | 210.83126 | 140.01923 | |
| Latvia | 170.78119 | 211.53262 | 136.72399 | |
| Romania | 161.27127 | 195.47092 | 130.79996 | |
| Uruguay | 160.94532 | 189.21098 | 135.16508 | |
| Prevalence | France | 7.838120 | 9.508800 | 6.3849828 |
| Germany | 7.675885 | 9.226489 | 6.3230564 | |
| Greenland | 6.928199 | 9.393575 | 4.8729118 | |
| Monaco | 5.832303 | 9.342838 | 3.249271 | |
| Latvia | 5.037147 | 6.210564 | 4.041666 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xia, Z.; Han, W.; Niu, H.; Dong, H. Global Burden of Pancreatic Cancer Among Individuals Aged 15–59 Years in 204 Countries and Territories, 1990–2021: A Systematic Analysis for the GBD 2021 and Projections to 2045. Cancers 2025, 17, 1757. https://doi.org/10.3390/cancers17111757
Xia Z, Han W, Niu H, Dong H. Global Burden of Pancreatic Cancer Among Individuals Aged 15–59 Years in 204 Countries and Territories, 1990–2021: A Systematic Analysis for the GBD 2021 and Projections to 2045. Cancers. 2025; 17(11):1757. https://doi.org/10.3390/cancers17111757
Chicago/Turabian StyleXia, Zeyu, Wenping Han, Haigang Niu, and Hui Dong. 2025. "Global Burden of Pancreatic Cancer Among Individuals Aged 15–59 Years in 204 Countries and Territories, 1990–2021: A Systematic Analysis for the GBD 2021 and Projections to 2045" Cancers 17, no. 11: 1757. https://doi.org/10.3390/cancers17111757
APA StyleXia, Z., Han, W., Niu, H., & Dong, H. (2025). Global Burden of Pancreatic Cancer Among Individuals Aged 15–59 Years in 204 Countries and Territories, 1990–2021: A Systematic Analysis for the GBD 2021 and Projections to 2045. Cancers, 17(11), 1757. https://doi.org/10.3390/cancers17111757





