Survival of Patients with Sinonasal Cancers in a Population-Based Registry, Lombardy, Italy, 2008–2023
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. The Lombardy Sinonasal Cancer Registry
2.2. Statistical Analysis
3. Results
3.1. Patient Characteristics
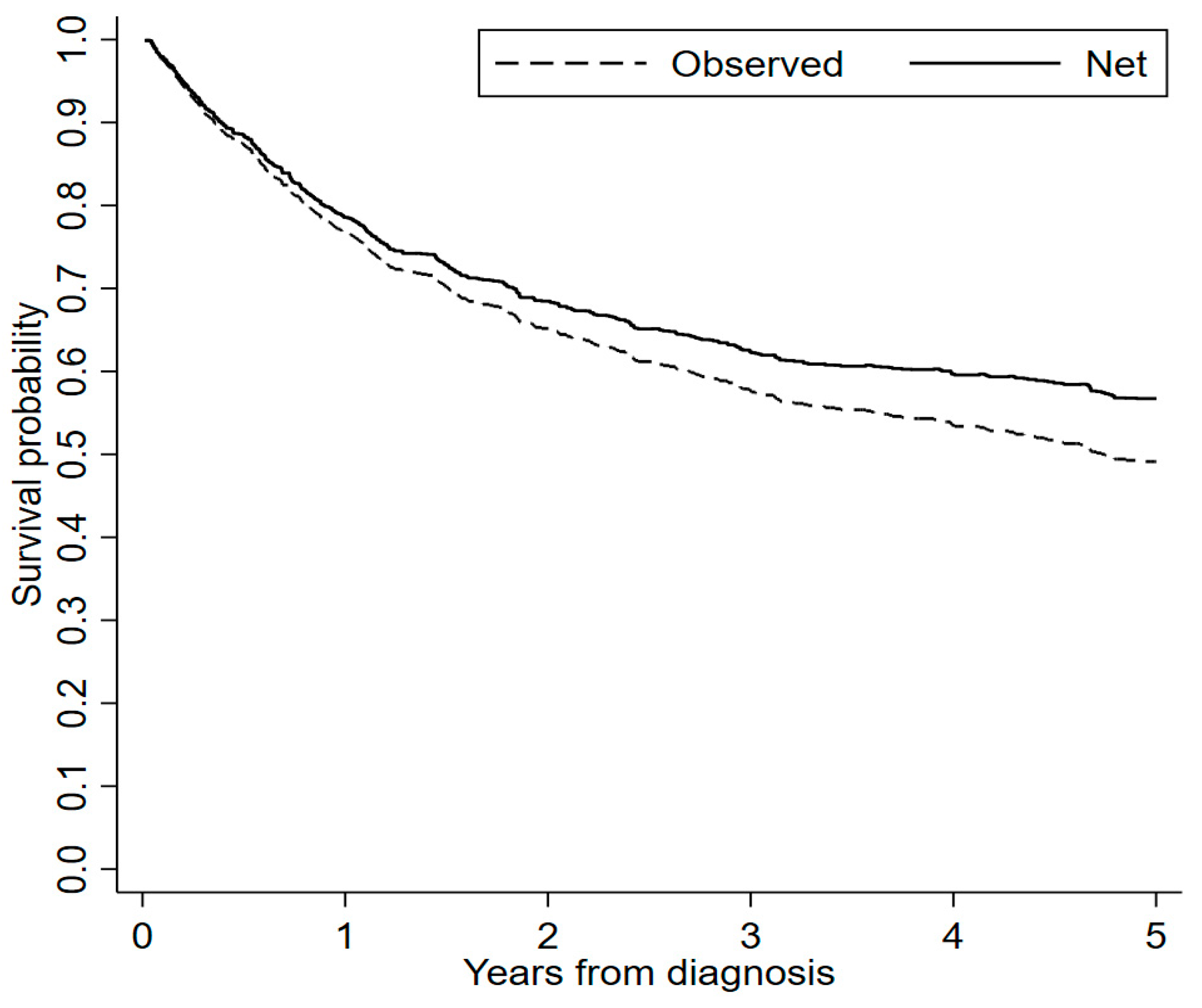
3.2. Survival Analysis
4. Discussion
4.1. Strengths and Limitations
4.2. Comparison with Other Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Taylor, M.A.; Saba, N.F. Cancer of the paranasal sinuses. Hematol. Oncol. Clin. 2021, 35, 949–962. [Google Scholar] [CrossRef] [PubMed]
- Gatta, G.; Capocaccia, R.; Trama, A.; Martínez-García, C.; RARECARE Working Group. The burden of rare cancers in Europe. Adv. Exp. Med. Biol. 2010, 686, 285–303. [Google Scholar] [PubMed]
- Turner, J.H.; Reh, D.D. Incidence and survival in patients with sinonasal cancer: A historical analysis of population-based data. Head Neck 2012, 34, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Sjöstedt, S.; Jensen, D.H.; Jakobsen, K.K.; Grønhøj, C.; Geneser, C.; Karnov, K.; Specht, L.; Agander, T.K.; von Buchwald, C. Incidence and survival in sinonasal carcinoma: A Danish population-based, nationwide study from 1980 to 2014. Acta Oncol. 2018, 57, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Dutta, R.; Dubal, P.M.; Svider, P.F.; Liu, J.K.; Baredes, S.; Eloy, J.A. Sinonasal malignancies: A population-based analysis of site-specific incidence and survival. Laryngoscope 2015, 125, 2491–2497. [Google Scholar] [CrossRef]
- Kuijpens, J.H.L.P.; Louwman, M.W.J.; Takes, R.; Slootweg, P.J.; Burdorf, A.; van Dijk, B.A.C. Sinonasal cancer in The Netherlands: Follow-up of a population-based study 1989–2014 and incidence of occupation-related adenocarcinoma. Head Neck 2018, 40, 2462–2468. [Google Scholar] [CrossRef]
- Binazzi, A.; Corfiati, M.; Di Marzio, D.; Cacciatore, A.M.; Zajacovà, J.; Mensi, C.; Galli, P.; Miligi, L.; Calisti, R.; Romeo, E.; et al. Sinonasal cancer in the Italian national surveillance system: Epidemiology, occupation, and public health implications. Am. J. Ind. Med. 2018, 61, 239–250. [Google Scholar] [CrossRef]
- Anschuetz, L.; Hohenberger, R.; Kaecker, C.; Elicin, O.; Giger, R.; Caversaccio, M. Sinonasal malignancies: Histopathological entities, regional involvement and long-term outcome. J. Otolaryngol. Head Neck Surg. 2023, 52, 36. [Google Scholar] [CrossRef]
- Lombo, C.; Castro Silva, J.; Monteiro, E. Sinonasal adenocarcinomas: Retrospective analysis from an oncology center. Acta Otorrinolaringol. 2023, 74, 15–22. [Google Scholar] [CrossRef]
- Qedair, J.; Haider, A.S.; Balasubramanian, K.; Palmisciano, P.; Hassan, T.; Shahbandi, A.; Sabahi, M.; Kharbat, A.F.; Abou-Al-Shaar, H.; Yu, K.; et al. Orbital exenteration for craniofacial lesions: A systematic review and meta-analysis of patient characteristics and survival outcomes. Cancers 2023, 15, 4285. [Google Scholar] [CrossRef]
- ’t Mannetje, A.; Kogevinas, M.; Luce, D.; Demers, P.A.; Bégin, D.; Bolm-Audorff, U.; Comba, P.; Hardell, L.; Hayes, R.B.; Leclerc, A.; et al. Sinonasal cancer, occupation, and tobacco smoking in European women and men. Am. J. Ind. Med. 1999, 36, 101–107. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer (IARC). List of Classifications by Cancer Sites with Sufficient or Limited Evidence in Humans; IARC Monographs; IARC: Lyon, France, 2023; Volume 1–135. Available online: https://monographs.iarc.who.int/list-of-classifications. (accessed on 21 November 2023).
- Binazzi, A.; Mensi, C.; Miligi, L.; Di Marzio, D.; Zajacova, J.; Galli, P.; Camagni, A.; Calisti, R.; Balestri, A.; Murano, S.; et al. Exposures to IARC carcinogenic agents in work settings not traditionally associated with sinonasal cancer risk: The experience of the Italian National Sinonasal Cancer Registry. Int. J. Environ. Res. Public Health 2021, 18, 12593. [Google Scholar] [CrossRef] [PubMed]
- Mensi, C.; Consonni, D.; Sieno, C.; De Matteis, S.; Riboldi, L.; Bertazzi, P.A. Sinonasal cancer and occupational exposure in a population-based registry. Int. J. Otolaryngol. 2013, 2013, 672621. [Google Scholar] [CrossRef]
- El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.; Slootweg, P.J. WHO Classification of Head and Neck Tumours, 4th ed.; IARC WHO Classification of Tumors: Lyon, France, 2017; Volume 9, pp. 1–348. [Google Scholar]
- Royston, P.; Lambert, P.C. Flexible Parametric Survival Analysis Using Stata: Beyond the Cox Model; Stata Press: College Station, TX, USA, 2011. [Google Scholar]
- Istituto Nazionale di Statistica, ISTAT. Mortality Tables of Resident Population. Available online: https://demo.istat.it/app/?i=TVM&l=it (accessed on 21 November 2023).
- Bower, H.; Crowther, M.J.; Lambert, P.C. Strcs: A command for fitting flexible parametric survival models on the log-hazard scale. Stata J. 2016, 16, 989–1012. [Google Scholar] [CrossRef]
- StataCorp. Stata 18. Statistical Software, StataCorp LLC.: College Station, TX, USA, 2023.
- Sarfati, D.; Blakely, T.; Pearce, N. Measuring cancer survival in populations: Relative survival vs cancer-specific survival. Int. J. Epidemiol. 2010, 39, 598–610. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Mattavelli, D.; Tomasoni, M.; Raffetti, E.; Bossi, P.; Schreiber, A.; Orlandi, E.; Taboni, S.; Rampinelli, V.; Gualtieri, T.; et al. The MUSES∗: A prognostic study on 1360 patients with sinonasal cancer undergoing endoscopic surgery-based treatment: ∗MUlti-institutional collaborative Study on Endoscopically treated Sinonasal cancers. Eur. J. Cancer 2022, 171, 161–182. [Google Scholar] [CrossRef]
- Llorente, J.L.; López, F.; Suárez, C.; Hermsen, M.A. Sinonasal carcinoma: Clinical, pathological, genetic and therapeutic advances. Nat. Rev. Clin. Oncol. 2014, 11, 460–472. [Google Scholar] [CrossRef]
- Morand, G.B.; Anderegg, N.; Vital, D.; Ikenberg, K.; Huber, G.F.; Soyka, M.B.; Egger, M.; Holzmann, D. Outcome by treatment modality in sinonasal undifferentiated carcinoma (SNUC): A case-series, systematic review and meta-analysis. Oral. Oncol. 2017, 75, 28–34. [Google Scholar] [CrossRef]
- Rooper, L.M. Proceedings of the 2023 North American Society of Head and Neck Pathology Companion Meeting, New Orleans, LA, March 12, 2023: Navigating New Developments in High Grade Sinonasal Neuroendocrine and Neuroectodermal Neoplasms. Head Neck Pathol. 2023, 17, 299–312. [Google Scholar] [CrossRef]
- Binazzi, A.; Ferrante, P.; Marinaccio, A. Occupational exposure and sinonasal cancer: A systematic review and meta-analysis. BMC Cancer 2015, 15, 49. [Google Scholar] [CrossRef]
- Siew, S.S.; Kauppinen, T.; Kyyrönen, P.; Heikkilä, P.; Pukkala, E. Occupational exposure to wood dust and formaldehyde and risk of nasal, nasopharyngeal, and lung cancer among Finnish men. Cancer Manag. Res. 2012, 4, 223–232. [Google Scholar] [CrossRef] [PubMed]
- d’Errico, A.; Pasian, S.; Baratti, A.; Zanelli, R.; Alfonzo, S.; Gilardi, L.; Beatrice, F.; Bena, A.; Costa, G. A case-control study on occupational risk factors for sino-nasal cancer. Occup. Environ. Med. 2009, 66, 448–455. [Google Scholar] [CrossRef] [PubMed]
| Variable | Males | Females | p-Value a | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| No. of subjects | 553 | 100.0 | 274 | 100.0 | |
| Age (median, min–max) | 69.0 | 25.7–93.1 | 68.3 | 21.1–99.7 | 0.18 |
| Period of diagnosis | |||||
| 2008–2012 | 215 | 38.9 | 109 | 39.8 | 0.97 |
| 2013–2016 | 159 | 28.8 | 77 | 28.1 | |
| 2017–2020 | 179 | 32.4 | 88 | 32.1 | |
| Cancer site (ICD-10 code) | |||||
| Nasal cavity (C30.0) | 215 | 38.9 | 99 | 36.1 | 0.01 |
| Maxillary sinus (C31.0) | 95 | 17.2 | 72 | 26.3 | |
| Ethmoidal sinus (C31.1) | 73 | 13.2 | 21 | 7.7 | |
| Frontal sinus (C31.2) | 2 | 0.4 | 3 | 1.1 | |
| Sphenoidal sinus (C31.3) | 13 | 2.4 | 11 | 4.0 | |
| Multiple sites (C31.8) | 155 | 28.1 | 68 | 24.8 | |
| Cancer morphology | |||||
| Squamous cell carcinoma and variants | 255 | 46.1 | 145 | 52.9 | 0.03 |
| Adenocarcinoma | 214 | 38.7 | 78 | 28.5 | |
| Neuroendocrine carcinoma | 19 | 3.4 | 7 | 2.6 | |
| Other epithelial neoplasm b | 55 | 10.0 | 32 | 11.7 | |
| Malignant tumour | 2 | 0.4 | 2 | 0.7 | |
| Unknown c | 8 | 1.5 | 10 | 3.7 | |
| Interview | |||||
| Patient | 352 | 63.7 | 159 | 58.0 | 0.05 |
| Next of kin | 133 | 24.1 | 64 | 23.4 | |
| Not performed | 68 | 12.3 | 51 | 18.6 | |
| Cigarette smoking | |||||
| Never | 154 | 27.9 | 122 | 44.5 | <0.001 |
| Former | 207 | 37.4 | 55 | 20.1 | |
| Current | 162 | 29.3 | 74 | 27.0 | |
| Unknown | 30 | 5.4 | 23 | 8.4 | |
| Occupational exposure | |||||
| Never exposed | 268 | 48.5 | 187 | 68.3 | |
| Ever exposed (any agent) | 217 | 39.2 | 36 | 13.1 | <0.001 |
| Wood dusts | 150 | 27.1 | 13 | 4.7 | <0.001 |
| Leather dusts | 65 | 11.8 | 20 | 7.3 | 0.01 |
| Nickel compounds | 9 | 1.6 | 3 | 1.1 | 0.05 |
| Chromium VI compounds | 18 | 3.3 | 3 | 1.1 | 0.01 |
| Formaldehyde | 3 | 0.5 | 1 | 0.4 | 0.05 |
| Unknown | 68 | 12.3 | 51 | 18.6 | <0.001 |
| Variable | 1-Year (95% CI) | 3-Year (95% CI) | 5-Year (95% CI) |
|---|---|---|---|
| All patients | 77 (74–79) | 58 (54–61) | 49 (46–53) |
| Gender | |||
| Male | 77 (73–80) | 57 (53–61) | 49 (45–54) |
| Female | 76 (71–81) | 59 (53–64) | 49 (43–55) |
| Age | |||
| 0–49 | 85 (77–90) | 67 (57–74) | 59 (49–67) |
| 50–69 | 85 (81–89) | 69 (64–74) | 62 (57–67) |
| 70+ | 68 (63–72) | 46 (41–51) | 36 (31–41) |
| Period of diagnosis | |||
| 2008–2012 | 76 (71–81) | 58 (52–63) | 50 (44–55) |
| 2013–2016 | 77 (71–82) | 56 (50–62) | 47 (40–53) |
| 2017–2020 | 77 (72–82) | 59 (53–65) | 51 (45–57) |
| Cancer site (ICD-10 code) | |||
| Nasal cavity (C30.0) | 79 (72–83) | 64 (58–69) | 57 (51–62) |
| Paranasal sinuses (C31) | 75 (71–79) | 54 (50–58) | 44 (40–49) |
| Cancer morphology | |||
| Squamous cell carcinoma and variants | 79 (74–82) | 61 (56–66) | 53 (47–57) |
| Adenocarcinoma | 82 (77–86) | 65 (59–70) | 54 (48–59) |
| Neuroendocrine carcinoma | 73 (52–86) | 31 (15–49) | 27 (12–44) |
| Other epithelial neoplasm a | 63 (62–72) | 39 (29–49) | 37 (27–47) |
| Variable | 1-Year (95% CI) a | 3-Year (95% CI) a | 5-Year (95% CI) a |
|---|---|---|---|
| All patients | 79 (76–82) | 62 (59–66) | 57 (53–61) |
| Gender | |||
| Male | 79 (76–83) | 63 (59–68) | 59 (54–64) |
| Female | 77 (72–83) | 62 (56–68) | 53 (47–60) |
| Age | |||
| 0–49 | 85 (78–92) | 67 (59–76) | 59 (51–69) |
| 50–69 | 86 (82–90) | 71 (66–76) | 65 (60–71) |
| 70+ | 71 (66–76) | 55 (49–61) | 50 (43–57) |
| Period of diagnosis | |||
| 2008–2012 | 78 (73–83) | 62 (56–68) | 57 (51–63) |
| 2013–2016 | 79 (73–85) | 61 (55–69) | 55 (48–64) |
| 2017–2020 | 79 (74–84) | 64 (58–71) | 58 (51–67) |
| Cancer site (ICD-10 code) | |||
| Nasal cavity (C30.0) | 81 (76–86) | 69 (63–75) | 65 (58–72) |
| Paranasal sinuses (C31) | 77 (73–81) | 59 (54–64) | 52 (47–58) |
| Cancer morphology | |||
| Squamous cell carcinoma and variants | 80 (76–85) | 65 (60–71) | 60 (54–66) |
| Adenocarcinoma | 84 (80–89) | 71 (65–77) | 64 (57–71) |
| Neuroendocrine carcinoma | 74 (59–93) | 32 (19–56) | 29 (16–54) |
| Other epithelial neoplasm b | 64 (55–75) | 41 (31–53) | 39 (29–51) |
| Variable | Deaths N (%) | Crude EHR | 95% CI | Adjusted EHR a | 95% CI |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 169 (61.7) | 1.00 | Reference | 1.00 | Reference |
| Male | 345 (62.4) | 0.91 | 0.71–1.15 | 0.94 | 0.74–1.20 |
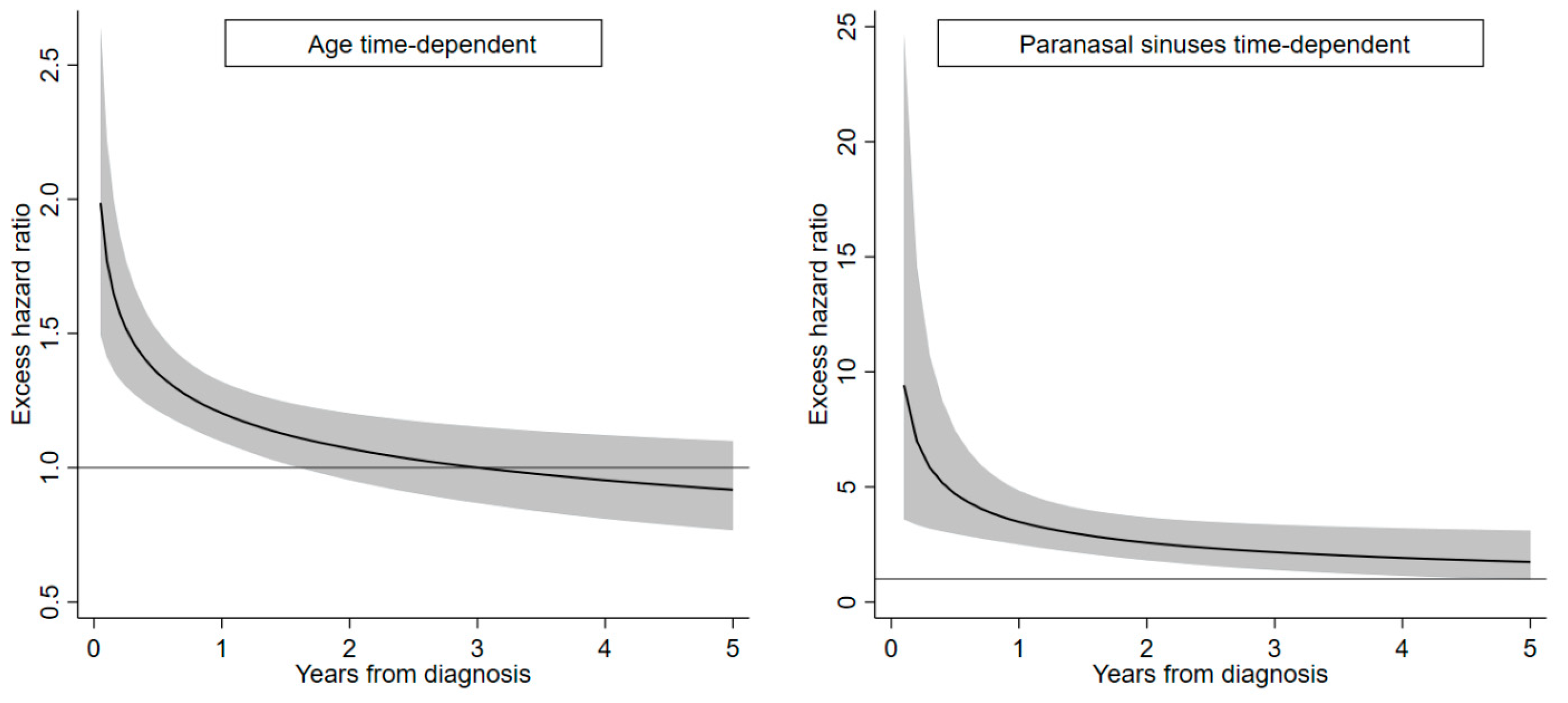
| Age (continuous, 10 years) | 1.00 | 0.89–1.13 | 1.05 | 0.93–1.19 | |
| 0.5 years from diagnosis | 1.32 | 1.19–1.47 | 1.35 | 1.12–1.51 | |
| 2.5 years from diagnosis | 0.97 | 0.86–1.10 | 1.03 | 0.90–1.17 | |
| 4.5 years from diagnosis | 0.87 | 0.73–1.02 | 0.93 | 0.78–1.11 | |
| Period of diagnosis | |||||
| 2008–2012 | 237 (73.2) | 1.00 | Reference | 1.00 | Reference |
| 2013–2016 | 150 (63.6) | 1.02 | 0.77–1.35 | 1.06 | 0.79–1.41 |
| 2017–2020 | 127 (47.6) | 0.89 | 0.67–1.18 | 0.97 | 0.73–1.28 |
| Cancer site (ICD-10 code) | |||||
| Nasal cavity (C30.0) | 152 (48.4) | 1.00 | Reference | 1.00 | Reference |
| Paranasal sinuses (C31) | 362 (70.6) | 3.32 | 2.43–4.53 | 2.46 | 1.69–3.58 |
| 0.5 years from diagnosis | 4.48 | 2.85–7.03 | 4.70 | 2.96–7.47 | |
| 2.5 years from diagnosis | 2.37 | 1.61–3.51 | 2.34 | 1.57–3.48 | |
| 4.5 years from diagnosis | 1.88 | 1.10–3.21 | 1.81 | 1.05–3.14 | |
| Cancer morphology | |||||
| Squamous cell carcinoma and variants | 234 (58.5) | 1.00 | Reference | 1.00 | Reference |
| Adenocarcinoma | 176 (60.3) | 0.86 | 0.65–1.14 | 0.69 | 0.52–0.91 |
| Neuroendocrine carcinoma | 23 (88.5) | 2.23 | 1.35–3.69 | 1.78 | 1.07–2.95 |
| Other epithelial neoplasm b | 60 (69.0) | 1.94 | 1.38–2.71 | 1.68 | 1.20–2.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Consonni, D.; Stella, S.; Denaro, N.; Binazzi, A.; Dallari, B.; Rugarli, S.; Borello, F.; Coviello, E.; Mensi, C. Survival of Patients with Sinonasal Cancers in a Population-Based Registry, Lombardy, Italy, 2008–2023. Cancers 2024, 16, 896. https://doi.org/10.3390/cancers16050896
Consonni D, Stella S, Denaro N, Binazzi A, Dallari B, Rugarli S, Borello F, Coviello E, Mensi C. Survival of Patients with Sinonasal Cancers in a Population-Based Registry, Lombardy, Italy, 2008–2023. Cancers. 2024; 16(5):896. https://doi.org/10.3390/cancers16050896
Chicago/Turabian StyleConsonni, Dario, Simona Stella, Nerina Denaro, Alessandra Binazzi, Barbara Dallari, Sabrina Rugarli, Flavia Borello, Enzo Coviello, and Carolina Mensi. 2024. "Survival of Patients with Sinonasal Cancers in a Population-Based Registry, Lombardy, Italy, 2008–2023" Cancers 16, no. 5: 896. https://doi.org/10.3390/cancers16050896
APA StyleConsonni, D., Stella, S., Denaro, N., Binazzi, A., Dallari, B., Rugarli, S., Borello, F., Coviello, E., & Mensi, C. (2024). Survival of Patients with Sinonasal Cancers in a Population-Based Registry, Lombardy, Italy, 2008–2023. Cancers, 16(5), 896. https://doi.org/10.3390/cancers16050896









