Impact of Complete Surgical Resection of Metastatic Lesions in Patients with Advanced Renal Cell Carcinoma in the Era of Tyrosine Kinase Inhibitors and Immune Checkpoint Inhibitors
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Data Collection
2.3. Statistical Analysis
3. Results
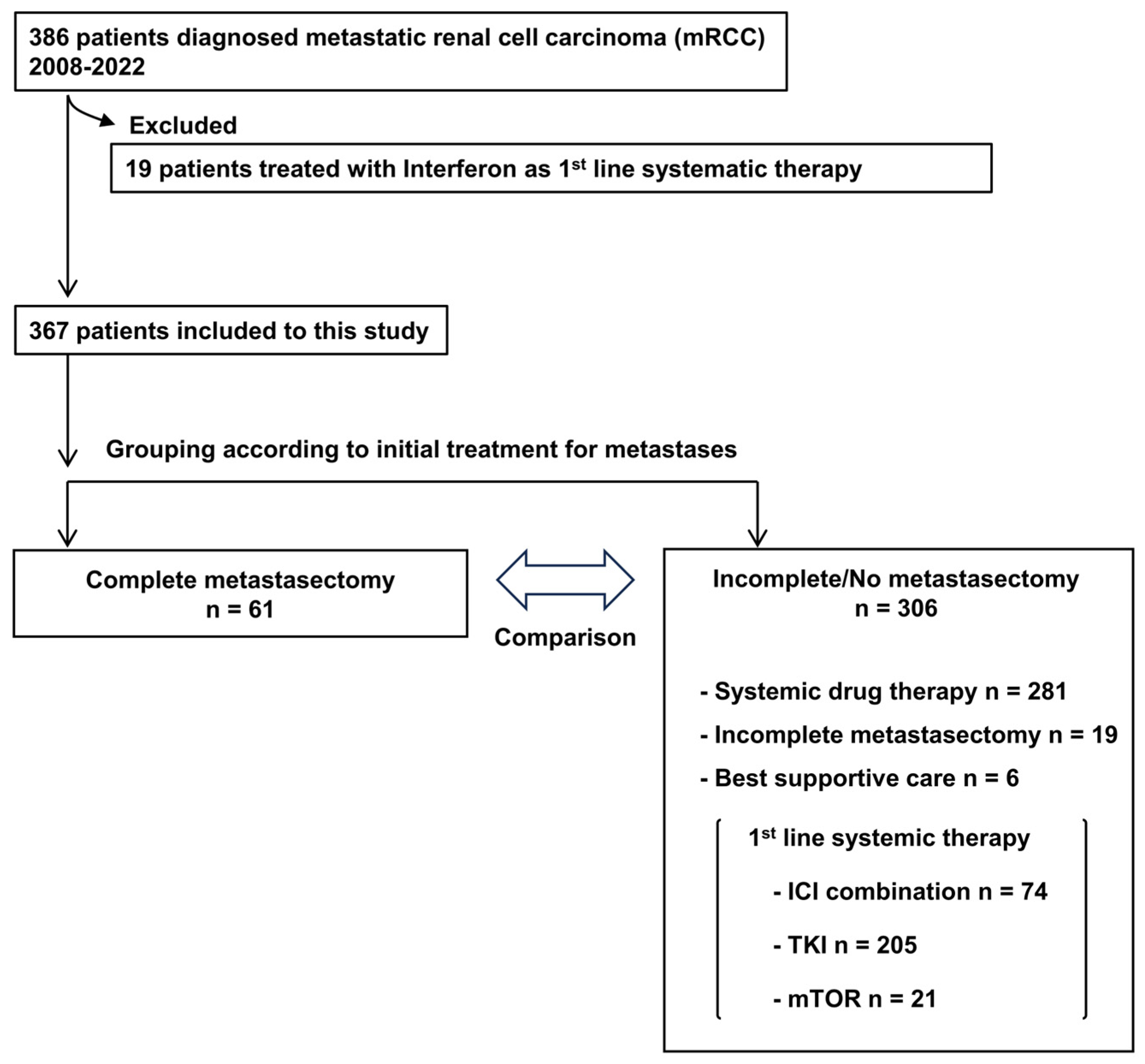
3.1. Cohort of This Study
3.2. Impact of Complete Metastasectomy on Oncological Outcomes
3.3. Prognostic Factors in Patients with Complete Metastasectomy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turajlic, S.; Xu, H.; Litchfield, K.; Rowan, A.; Chambers, T.; Lopez, J.I.; Nicol, D.; O’Brien, T.; Larkin, J.; Horswell, S.; et al. Tracking Cancer Evolution Reveals Constrained Routes to Metastases: TRACERx Renal. Cell 2018, 173, 581–594.e512. [Google Scholar] [CrossRef]
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Arén Frontera, O.; Melichar, B.; Choueiri, T.K.; Plimack, E.R.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus Ipilimumab versus Sunitinib in Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290. [Google Scholar] [CrossRef]
- Motzer, R.J.; Penkov, K.; Haanen, J.; Rini, B.; Albiges, L.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Negrier, S.; Uemura, M.; et al. Avelumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1103–1115. [Google Scholar] [CrossRef]
- Rini, B.I.; Plimack, E.R.; Stus, V.; Gafanov, R.; Hawkins, R.; Nosov, D.; Pouliot, F.; Alekseev, B.; Soulières, D.; Melichar, B.; et al. Pembrolizumab plus Axitinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2019, 380, 1116–1127. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Powles, T.; Burotto, M.; Escudier, B.; Bourlon, M.T.; Zurawski, B.; Oyervides Juárez, V.M.; Hsieh, J.J.; Basso, U.; Shah, A.Y.; et al. Nivolumab plus Cabozantinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N. Engl. J. Med. 2021, 384, 829–841. [Google Scholar] [CrossRef]
- Motzer, R.; Alekseev, B.; Rha, S.-Y.; Porta, C.; Eto, M.; Powles, T.; Grünwald, V.; Hutson, T.E.; Kopyltsov, E.; Méndez-Vidal, M.J.; et al. Lenvatinib plus Pembrolizumab or Everolimus for Advanced Renal Cell Carcinoma. N. Engl. J. Med. 2021, 384, 1289–1300. [Google Scholar] [CrossRef] [PubMed]
- Alt, A.L.; Boorjian, S.A.; Lohse, C.M.; Costello, B.A.; Leibovich, B.C.; Blute, M.L. Survival after complete surgical resection of multiple metastases from renal cell carcinoma. Cancer 2011, 117, 2873–2882. [Google Scholar] [CrossRef]
- Dabestani, S.; Marconi, L.; Hofmann, F.; Stewart, F.; Lam, T.B.; Canfield, S.E.; Staehler, M.; Powles, T.; Ljungberg, B.; Bex, A. Local treatments for metastases of renal cell carcinoma: A systematic review. Lancet Oncol. 2014, 15, e549–e561. [Google Scholar] [CrossRef] [PubMed]
- Zaid, H.B.; Parker, W.P.; Safdar, N.S.; Gershman, B.; Erwin, P.J.; Murad, M.H.; Boorjian, S.A.; Costello, B.A.; Thompson, R.H.; Leibovich, B.C. Outcomes Following Complete Surgical Metastasectomy for Patients with Metastatic Renal Cell Carcinoma: A Systematic Review and Meta-Analysis. J. Urol. 2017, 197, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Psutka, S.P.; Master, V.A. Role of metastasis-directed treatment in kidney cancer. Cancer 2018, 124, 3641–3655. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology Kidney Cancer. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1440 (accessed on 9 January 2024).
- Ljungberg, B.; Albiges, L.; Bedke, J.; Bex, A.; Capitanio, U.; Giles, R.H.; Hora, M.; Klatte, T.; Marconi, L.; Powles, T.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma 2023. Available online: https://uroweb.org/guidelines/renal-cell-carcinoma (accessed on 25 November 2023).
- Eggener, S.E.; Yossepowitch, O.; Kundu, S.; Motzer, R.J.; Russo, P. Risk score and metastasectomy independently impact prognosis of patients with recurrent renal cell carcinoma. J. Urol. 2008, 180, 873–878; discussion 878. [Google Scholar] [CrossRef]
- Yu, X.; Wang, B.; Li, X.; Lin, G.; Zhang, C.; Yang, Y.; Fang, D.; Song, Y.; He, Z.; Zhou, L. The Significance of Metastasectomy in Patients with Metastatic Renal Cell Carcinoma in the Era of Targeted Therapy. Biomed. Res. Int. 2015, 2015, 176373. [Google Scholar] [CrossRef]
- Powles, T.; Tomczak, P.; Park, S.H.; Venugopal, B.; Ferguson, T.; Symeonides, S.N.; Hajek, J.; Gurney, H.; Chang, Y.H.; Lee, J.L.; et al. Pembrolizumab versus placebo as post-nephrectomy adjuvant therapy for clear cell renal cell carcinoma (KEYNOTE-564): 30-month follow-up analysis of a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2022, 23, 1133–1144. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Tomczak, P.; Park, S.H.; Venugopal, B.; Ferguson, T.; Chang, Y.-H.; Hajek, J.; Symeonides, S.N.; Lee, J.L.; Sarwar, N.; et al. Adjuvant Pembrolizumab after Nephrectomy in Renal-Cell Carcinoma. N. Engl. J. Med. 2021, 385, 683–694. [Google Scholar] [CrossRef]
- Pal, S.K.; Uzzo, R.; Karam, J.A.; Master, V.A.; Donskov, F.; Suarez, C.; Albiges, L.; Rini, B.; Tomita, Y.; Kann, A.G.; et al. Adjuvant atezolizumab versus placebo for patients with renal cell carcinoma at increased risk of recurrence following resection (IMmotion010): A multicentre, randomised, double-blind, phase 3 trial. Lancet 2022, 400, 1103–1116. [Google Scholar] [CrossRef]
- Lyon, T.D.; Thompson, R.H.; Shah, P.H.; Lohse, C.M.; Boorjian, S.A.; Costello, B.A.; Cheville, J.C.; Leibovich, B.C. Complete Surgical Metastasectomy of Renal Cell Carcinoma in the Post-Cytokine Era. J. Urol. 2020, 203, 275–282. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Motzer, R.J.; Rini, B.I.; Haanen, J.; Campbell, M.T.; Venugopal, B.; Kollmannsberger, C.; Gravis-Mescam, G.; Uemura, M.; Lee, J.L.; et al. Updated efficacy results from the JAVELIN Renal 101 trial: First-line avelumab plus axitinib versus sunitinib in patients with advanced renal cell carcinoma. Ann. Oncol. 2020, 31, 1030–1039. [Google Scholar] [CrossRef]
- Albiges, L.; Tannir, N.M.; Burotto, M.; McDermott, D.; Plimack, E.R.; Barthelemy, P.; Porta, C.; Powles, T.; Donskov, F.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib for first-line treatment of advanced renal cell carcinoma: Extended 4-year follow-up of the phase III CheckMate 214 trial. ESMO Open 2020, 5, e001079. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Eto, M.; Motzer, R.; De Giorgi, U.; Buchler, T.; Basappa, N.S.; Mendez-Vidal, M.J.; Tjulandin, S.; Hoon Park, S.; Melichar, B.; et al. Lenvatinib plus pembrolizumab versus sunitinib as first-line treatment of patients with advanced renal cell carcinoma (CLEAR): Extended follow-up from the phase 3, randomised, open-label study. Lancet Oncol. 2023, 24, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Motzer, R.J.; Powles, T.; Burotto, M.; Escudier, B.; Bourlon, M.T.; Shah, A.Y.; Suarez, C.; Hamzaj, A.; Porta, C.; Hocking, C.M.; et al. Nivolumab plus cabozantinib versus sunitinib in first-line treatment for advanced renal cell carcinoma (CheckMate 9ER): Long-term follow-up results from an open-label, randomised, phase 3 trial. Lancet Oncol. 2022, 23, 888–898. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Plimack, E.R.; Soulieres, D.; Waddell, T.; Stus, V.; Gafanov, R.; Nosov, D.; Pouliot, F.; Melichar, B.; Vynnychenko, I.; et al. Pembrolizumab plus axitinib versus sunitinib monotherapy as first-line treatment of advanced renal cell carcinoma (KEYNOTE-426): Extended follow-up from a randomised, open-label, phase 3 trial. Lancet Oncol. 2020, 21, 1563–1573. [Google Scholar] [CrossRef]
- Psutka, S.P.; Cheville, J.C.; Costello, B.A.; Stewart-Merrill, S.B.; Lohse, C.M.; Leibovich, B.C.; Boorjian, S.A.; Thompson, R.H. Concordance of Pathologic Features Between Metastatic Sites and the Primary Tumor in Surgically Resected Metastatic Renal Cell Carcinoma. Urology 2016, 96, 106–113. [Google Scholar] [CrossRef]
- Pessoa, R.R.; Nabavizadeh, R.; Quevedo, F.; Joyce, D.D.; Lohse, C.M.; Sharma, V.; Costello, B.A.; Boorjian, S.A.; Thompson, R.H.; Leibovich, B.C.; et al. The Impact of Metastasis Histopathology on Oncologic Outcomes for Patients with Surgically Resected Metastatic Renal Cell Carcinoma. J. Urol. 2023, 210, 611–618. [Google Scholar] [CrossRef]
- Leibovich, B.C.; Cheville, J.C.; Lohse, C.M.; Zincke, H.; Frank, I.; Kwon, E.D.; Merchan, J.R.; Blute, M.L. A scoring algorithm to predict survival for patients with metastatic clear cell renal cell carcinoma: A stratification tool for prospective clinical trials. J. Urol. 2005, 174, 1759–1763; discussion 1763. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.P.; Sun, M.; Karam, J.A.; Leow, J.J.; de Velasco, G.; Pal, S.K.; Chang, S.L.; Trinh, Q.D.; Choueiri, T.K. Complications after Metastasectomy for Renal Cell Carcinoma—A Population-based Assessment. Eur. Urol. 2017, 72, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Dudani, S.; de Velasco, G.; Wells, J.C.; Gan, C.L.; Donskov, F.; Porta, C.; Fraccon, A.; Pasini, F.; Lee, J.L.; Hansen, A.; et al. Evaluation of Clear Cell, Papillary, and Chromophobe Renal Cell Carcinoma Metastasis Sites and Association with Survival. JAMA Netw. Open 2021, 4, e2021869. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Christie, A.; Lin, M.H.; Jung, M.; Weix, D.; Huelsmann, L.; Kuhn, K.; Meyer, J.; Desai, N.; Kim, D.W.N.; et al. Safety and Efficacy of Stereotactic Ablative Radiation Therapy for Renal Cell Carcinoma Extracranial Metastases. Int. J. Radiat. Oncol. Biol. Phys. 2017, 98, 91–100. [Google Scholar] [CrossRef]
- Kothari, G.; Foroudi, F.; Gill, S.; Corcoran, N.M.; Siva, S. Outcomes of stereotactic radiotherapy for cranial and extracranial metastatic renal cell carcinoma: A systematic review. Acta Oncol. 2015, 54, 148–157. [Google Scholar] [CrossRef] [PubMed]


| Variables | Unadjusted Population | p Value | PSM Population | p Value | SMD | |||
|---|---|---|---|---|---|---|---|---|
| Complete Metastasectomy | Complete Metastasectomy | |||||||
| No n = 306 | Yes n = 61 | No n = 39 | Yes n = 39 | |||||
| Age (years old), Median (IQR) | 69 (63–77) | 65 (59–72) | 0.01 ‡ | 66 (59–74) | 64 (57–72) | 0.43 ‡ | 0.18 | |
| 70≤ | 168 (54.9%) | 25 (41.0%) | 0.05 † | 14 (35.9%) | 14 (35.9%) | 1.00 † | <0.001 | |
| Sex | Male | 228 (74.5%) | 42 (68.9%) | 0.42 † | 30 (76.9%) | 28 (71.8%) | 0.80 † | 0.12 |
| Female | 78 (25.5%) | 19 (31.1%) | 9 (23.1%) | 11 (28.2%) | ||||
| Time from diagnosis to treatment | Yes | 100 (32.7%) | 44 (72.1%) | <0.01 † | 29 (74.4%) | 27 (69.2%) | 0.80 † | 0.11 |
| Asynchronous, ≥1 year | No | 206 (67.3%) | 17 (27.9%) | 10 (25.6%) | 12 (30.8%) | |||
| Surgical removal of primary organ | Yes | 238 (77.8%) | 61 (100%) | <0.01 † | 39 (100%) | 39 (100%) | NA | <0.001 |
| No | 68 (22.2%) | 0 (0%) | 0 (0%) | 0 (0%) | ||||
| IMDC risk classfication | favorable | 52 (17.0%) | 23 (37.7%) | <0.01 † | 16 (41.0%) | 15 (38.5%) | 0.51 † | 0.32 |
| intermediate | 179 (58.5%) | 32 (52.5%) | 22 (56.4%) | 20 (51.3%) | ||||
| poor | 75 (24.5%) | 6 (9.8%) | 1 (2.6%) | 4 (10.3%) | ||||
| Histology | ccRCC | 197 (64.4%) | 48 (88.7%) | 0.23 † | 37 (94.9%) | 33 (84.6%) | 0.26 † | 0.34 |
| Non-ccRCC | 47 (15.4%) | 13 (21.3%) | 2 (5.1%) | 6 (15.4%) | ||||
| Sarcomatoid change (+) | 27 (8.9%) | 7 (11.5%) | 0.63 † | 4 (10.3%) | 3 (7.7%) | 0.63 † | 0.09 | |
| NA | 62 (20.3%) | 0 (0%) | ||||||
| Fuhrman Grade | G1,G2 | 106 (34.6%) | 29 (47.5%) | 0.28 † | 20 (51.3%) | 22 (56.4%) | 1.00 † | 0.10 |
| G3,G4 | 127 (39.1%) | 23 (37.7%) | 19 (48.7%) | 17 (43.6%) | ||||
| NA | 73 (23.9%) | 9 (14.8%) | ||||||
| Metastatic sites or target lesions | Lymph node | 106 (34.6%) | 8 (13.1%) | 3 (7.7%) | 6 (15.4%) | 0.48 † | 0.24 | |
| Lung | 172 (56.2%) | 34 (55.7%) | 26 (66.7%) | 22 (56.4%) | 0.49 † | 0.21 | ||
| Liver | 25 (8.2%) | 2 (3.4%) | 25 (8.2%) | 2 (3.4%) | 1.00 † | <0.001 | ||
| Bone | 69 (22.5%) | 13 (21.3%) | 6 (15.4%) | 7 (17.9%) | 1.00 † | 0.07 | ||
| Brain | 5 (1.5%) | 6 (9.8%) | 1 (2.6%) | 3 (7.7%) | 0.62 † | 0.23 | ||
| Others | 87 (28.4%) | 17 (27.4%) | 5 (12.8%) | 6 (15.4%) | 1.00 † | 0.07 | ||
| Number of metastases | 230 (75.2%) | 51 (83.6%) | 0.19 † | 35 (89.7%) | 34 (87.2%) | 1.00 † | 0.08 | |
| 2≤ | 76 (24.8%) | 10 (16.4%) | 4 (10.3%) | 5 (12.8%) | ||||
| Follow-up period (month), median (IQR) | 32 (9–49) | 58 (28–80) | 41 (14–60) | 54 (28–76) | ||||
| Variables | Progression-Free Survival | Overall Survival | |||||
|---|---|---|---|---|---|---|---|
| Multivariate Analysis | Multivariate Analysis | ||||||
| HR | 95% CI | p Value | HR | 95% CI | p Value | ||
| Age | ≥ 70 vs. <70 | 2.42 | 0.90–6.51 | 0.08 | |||
| Time from diagnosis to treatment | <1 year vs. ≥1 year | 0.35 | 0.09–1.32 | 0.12 | |||
| IMDC | Intermediate/Poor vs. Favorable | 4.37 | 1.05–4.37 | 0.036 * | 2.31 | 0.57–9.33 | 0.24 |
| Fuhrman grade | 3, 4 vs. 1, 2 | 2.09 | 0.63–6.96 | 0.23 | |||
| Site of metastasectomy | |||||||
| Lymph node | Yes vs. No | 2.31 | 0.54–9.96 | 0.26 | |||
| Lung | Yes vs. No | 1.33 | 0.33–5.32 | 0.68 | |||
| Liver | Yes vs. No | ||||||
| Bone | Yes vs. No | 0.86 | 0.39–1.89 | 0.71 | 3.21 | 0.75–13.7 | 0.12 |
| Brain | Yes vs. No | 2.1 | 0.63–6.96 | 0.38 | |||
| Number of metastasis | Multi vs. Mono | 3.74 | 1.61–8.71 | 0.002 * | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu, T.; Miyake, M.; Nishimura, N.; Yoshida, T.; Itami, Y.; Tachibana, A.; Omori, C.; Oda, Y.; Kohashi, M.; Tomizawa, M.; et al. Impact of Complete Surgical Resection of Metastatic Lesions in Patients with Advanced Renal Cell Carcinoma in the Era of Tyrosine Kinase Inhibitors and Immune Checkpoint Inhibitors. Cancers 2024, 16, 841. https://doi.org/10.3390/cancers16040841
Shimizu T, Miyake M, Nishimura N, Yoshida T, Itami Y, Tachibana A, Omori C, Oda Y, Kohashi M, Tomizawa M, et al. Impact of Complete Surgical Resection of Metastatic Lesions in Patients with Advanced Renal Cell Carcinoma in the Era of Tyrosine Kinase Inhibitors and Immune Checkpoint Inhibitors. Cancers. 2024; 16(4):841. https://doi.org/10.3390/cancers16040841
Chicago/Turabian StyleShimizu, Takuto, Makito Miyake, Nobutaka Nishimura, Takanori Yoshida, Yoshitaka Itami, Akira Tachibana, Chihiro Omori, Yuki Oda, Mikiko Kohashi, Mitsuru Tomizawa, and et al. 2024. "Impact of Complete Surgical Resection of Metastatic Lesions in Patients with Advanced Renal Cell Carcinoma in the Era of Tyrosine Kinase Inhibitors and Immune Checkpoint Inhibitors" Cancers 16, no. 4: 841. https://doi.org/10.3390/cancers16040841
APA StyleShimizu, T., Miyake, M., Nishimura, N., Yoshida, T., Itami, Y., Tachibana, A., Omori, C., Oda, Y., Kohashi, M., Tomizawa, M., Onishi, K., Hori, S., Morizawa, Y., Dotoh, D., Nakai, Y., Torimoto, K., Tanaka, N., & Fujimoto, K. (2024). Impact of Complete Surgical Resection of Metastatic Lesions in Patients with Advanced Renal Cell Carcinoma in the Era of Tyrosine Kinase Inhibitors and Immune Checkpoint Inhibitors. Cancers, 16(4), 841. https://doi.org/10.3390/cancers16040841







