The Role of Liquid Biopsy in Gastroenteropancreatic Neuroendocrine Neoplasms
Abstract
Simple Summary
Abstract
1. Introduction
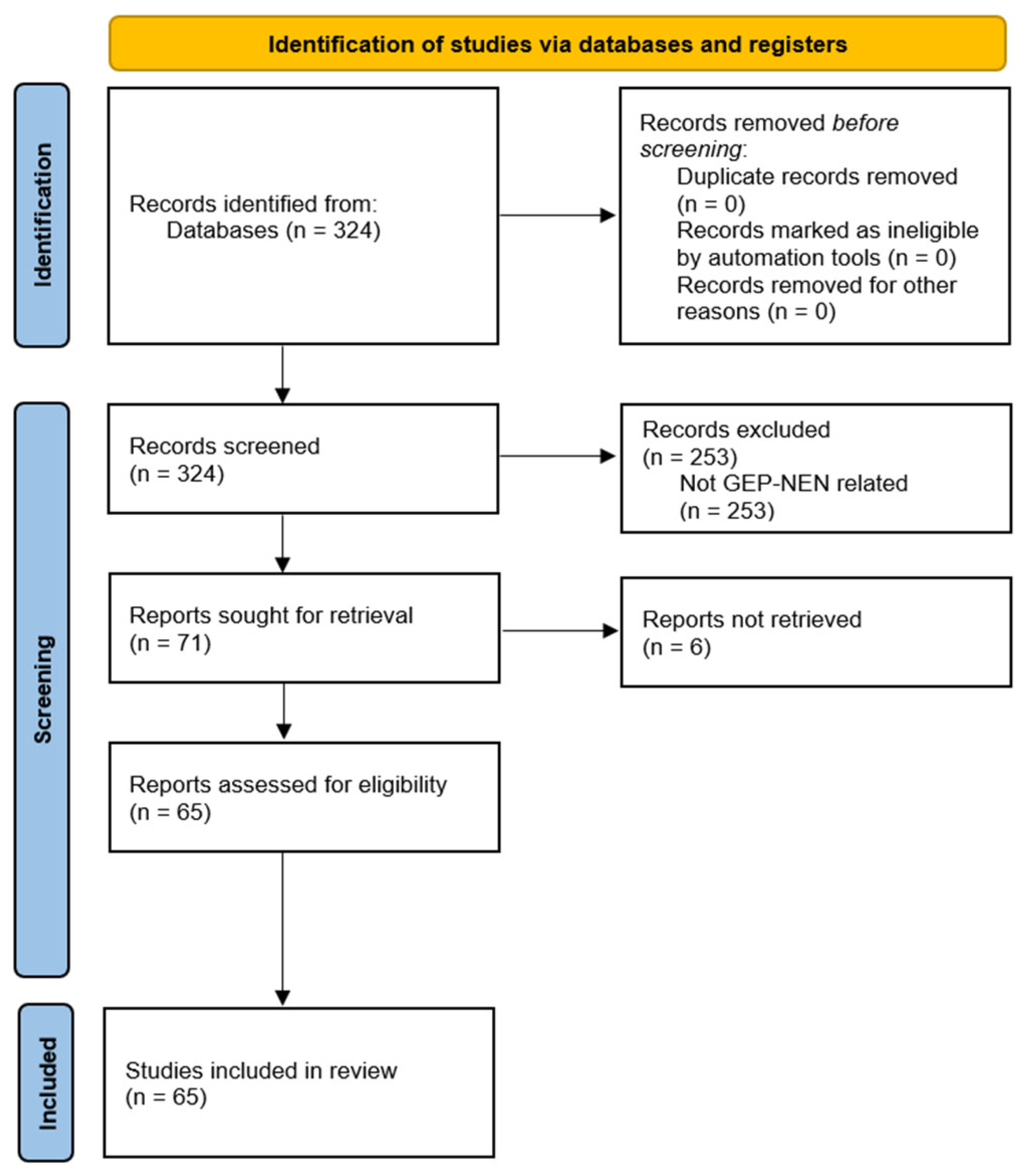
2. Materials and Methods
3. Results
3.1. Types of Liquid Biopsies
3.1.1. Circulating Tumour Cells (CTCs)
3.1.2. Circulating Tumour DNA (ctDNA)
3.1.3. Micro RNA (miRNA)
3.1.4. Messenger RNA (mRNA)
3.1.5. Extracellular Vesicles
3.2. Potential Applications in Clinical Practice
3.2.1. Diagnosis and Characterisation
3.2.2. Prognostic and Predictive Value
3.2.3. Monitoring Treatment Response and Prediction of Recurrence
4. Discussion
Current Applications and Future Perspectives
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Shah, M.H.; Goldner, W.S.; Benson, A.B.; Bergsland, E.; Blaszkowsky, L.S.; Brock, P.; Chan, J.; Das, S.; Dickson, P.V.; Fanta, P.; et al. Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2021, 19, 839–868. [Google Scholar] [CrossRef]
- Pavel, M.; Öberg, K.; Falconi, M.; Krenning, E.P.; Sundin, A.; Perren, A.; Berruti, A. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2020, 31, 844–860. [Google Scholar] [CrossRef] [PubMed]
- Martins, I.; Ribeiro, I.P.; Jorge, J.; Gonçalves, A.C.; Sarmento-Ribeiro, A.B.; Melo, J.B.; Carreira, I.M. Liquid Biopsies: Applications for Cancer Diagnosis and Monitoring. Genes 2021, 12, 349. [Google Scholar] [CrossRef] [PubMed]
- Heidrich, I.; Ačkar, L.; Mossahebi Mohammadi, P.; Pantel, K. Liquid biopsies: Potential and challenges. Int. J. Cancer 2021, 148, 528–545. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Zhu, L.; Song, J.; Wang, G.; Li, P.; Li, W.; Luo, P.; Sun, X.; Wu, J.; Liu, Y.; et al. Liquid biopsy at the frontier of detection, prognosis and progression monitoring in colorectal cancer. Mol. Cancer 2022, 21, 86. [Google Scholar] [CrossRef] [PubMed]
- Jayaprakasam, V.S.; Bodei, L. Neuroendocrine Tumor Therapy Response Assessment. PET Clin. 2023, 18, 267–286. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, F.M.; Meyer, T. Liquid Biopsies for Neuroendocrine Tumors: Circulating Tumor Cells, DNA, and MicroRNAs. Endocrinol. Metab. Clin. N. Am. 2018, 47, 471–483. [Google Scholar] [CrossRef]
- Boons, G.; Vandamme, T.; Peeters, M.; Van Camp, G.; Op De Beeck, K. Clinical applications of (epi)genetics in gastroenteropancreatic neuroendocrine neoplasms: Moving towards liquid biopsies. Rev. Endocr. Metab. Disord. 2019, 20, 333–351. [Google Scholar] [CrossRef]
- Barriuso, J.; Custodio, A.; Afonso, R.; Alonso, V.; Astudillo, A.; Capdevila, J.; García-Carbonero, R.; Grande, E.; Jimenez-Fonseca, P.; Marazuela, M.; et al. Prognostic and predictive biomarkers for somatostatin analogs, peptide receptor radionuclide therapy and serotonin pathway targets in neuroendocrine tumours. Cancer Treat. Rev. 2018, 70, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Kalligeros, M.; Diamantopoulos, L.; Toumpanakis, C. Biomarkers in Small Intestine NETs and Carcinoid Heart Disease: A Comprehensive Review. Biology 2021, 10, 950. [Google Scholar] [CrossRef]
- Komarnicki, P.; Musiałkiewicz, J.; Stańska, A.; Maciejewski, A.; Gut, P.; Mastorakos, G.; Ruchała, M. Circulating Neuroendocrine Tumor Biomarkers: Past, Present and Future. J. Clin. Med. 2022, 11, 5542. [Google Scholar] [CrossRef] [PubMed]
- Smolkova, B.; Kataki, A.; Earl, J.; Ruz-Caracuel, I.; Cihova, M.; Urbanova, M.; Buocikova, V.; Tamargo, S.; Rovite, V.; Niedra, H.; et al. Liquid biopsy and preclinical tools for advancing diagnosis and treatment of patients with pancreatic neuroendocrine neoplasms. Crit. Rev. Oncol. Hematol. 2022, 180, 103865. [Google Scholar] [CrossRef] [PubMed]
- Malla, M.; Loree, J.M.; Kasi, P.M.; Parikh, A.R. Using Circulating Tumor DNA in Colorectal Cancer: Current and Evolving Practices. J. Clin. Oncol. 2022, 40, 2846–2857. [Google Scholar] [CrossRef]
- Dasari, A.; Morris, V.K.; Allegra, C.J.; Atreya, C.; Benson, A.B.; Boland, P.; Chung, K.; Copur, M.S.; Corcoran, R.B.; Deming, D.A.; et al. ctDNA applications and integration in colorectal cancer: An NCI Colon and Rectal–Anal Task Forces whitepaper. Nat. Rev. Clin. Oncol. 2020, 17, 757–770. [Google Scholar] [CrossRef] [PubMed]
- Malczewska, A.; Frampton, A.E.; Prado, M.M.; Ameri, S.; Dabrowska, A.F.; Zagorac, S.; Clift, A.K.; Kos-Kudla, B.; Faiz, O.; Stebbing, J.; et al. Circulating MicroRNAs in Small-bowel Neuroendocrine Tumors: A Potential Tool for Diagnosis and Assessment of Effectiveness of Surgical Resection. Ann. Surg. 2021, 274, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Ciobanu, O.; Martin, S.; Fica, S. Perspectives on the diagnostic, predictive and prognostic markers of neuroendocrine neoplasms (Review). Exp. Ther. Med. 2021, 22, 1479. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, C.J.; Agarwal, M.; Pottakkat, B.; Haroon, N.N.; George, A.S.; Pappachan, J.M. Gastroenteropancreatic neuroendocrine neoplasms: A clinical snapshot. World J. Gastrointest. Surg. 2021, 13, 231–255. [Google Scholar] [CrossRef] [PubMed]
- Modlin, I.M.; Drozdov, I.; Kidd, M. The Identification of Gut Neuroendocrine Tumor Disease by Multiple Synchronous Transcript Analysis in Blood. PLoS ONE 2013, 8, e63364. [Google Scholar] [CrossRef] [PubMed]
- Modlin, I.M.; Kidd, M.; Malczewska, A.; Drozdov, I.; Bodei, L.; Matar, S.; Chung, K.-M. The NETest. Endocrinol. Metab. Clin. N. Am. 2018, 47, 485–504. [Google Scholar] [CrossRef]
- Modlin, I.M.; Kidd, M.; Falconi, M.; Filosso, P.L.; Frilling, A.; Malczewska, A.; Toumpanakis, C.; Valk, G.; Pacak, K.; Bodei, L.; et al. A multigenomic liquid biopsy biomarker for neuroendocrine tumor disease outperforms CgA and has surgical and clinical utility. Ann. Oncol. 2021, 32, 1425–1433. [Google Scholar] [CrossRef]
- Öberg, K.; Califano, A.; Strosberg, J.R.; Ma, S.; Pape, U.; Bodei, L.; Kaltsas, G.; Toumpanakis, C.; Goldenring, J.R.; Frilling, A.; et al. A meta-analysis of the accuracy of a neuroendocrine tumor mRNA genomic biomarker (NETest) in blood. Ann. Oncol. 2020, 31, 202–212. [Google Scholar] [CrossRef] [PubMed]
- Malczewska, A.; Kos-Kudła, B.; Kidd, M.; Drozdov, I.; Bodei, L.; Matar, S.; Oberg, K.; Modlin, I.M. The clinical applications of a multigene liquid biopsy (NETest) in neuroendocrine tumors. Adv. Med. Sci. 2020, 65, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Van Treijen, M.J.C.; Korse, C.M.; Van Leeuwaarde, R.S.; Saveur, L.J.; Vriens, M.R.; Verbeek, W.H.M.; Tesselaar, M.E.T.; Valk, G.D. Blood Transcript Profiling for the Detection of Neuroendocrine Tumors: Results of a Large Independent Validation Study. Front. Endocrinol. 2018, 9, 740. [Google Scholar] [CrossRef] [PubMed]
- Al-Toubah, T.; Cives, M.; Valone, T.; Blue, K.; Strosberg, J. Sensitivity and Specificity of the NETest: A Validation Study. Neuroendocrinology 2021, 111, 580–585. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, Y.; Gao, X.; Yuan, Y.; Zhao, J.; Zhou, S.; Wang, H.; Wang, L.; Xu, G.; Li, X.; et al. Plasma-Derived Exosomal ALIX as a Novel Biomarker for Diagnosis and Classification of Pancreatic Cancer. Front. Oncol. 2021, 11, 628346. [Google Scholar] [CrossRef]
- Khan, M.S.; Kirkwood, A.A.; Tsigani, T.; Lowe, H.; Goldstein, R.; Hartley, J.A.; Caplin, M.E.; Meyer, T. Early Changes in Circulating Tumor Cells Are Associated with Response and Survival Following Treatment of Metastatic Neuroendocrine Neoplasms. Clin Cancer Res. 2016, 22, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Genç, C.G.; Jilesen, A.P.J.; Nieveen Van Dijkum, E.J.M.; Klümpen, H.-J.; Van Eijck, C.H.J.; Drozdov, I.; Malczewska, A.; Kidd, M.; Modlin, I. Measurement of circulating transcript levels (NETest) to detect disease recurrence and improve follow-up after curative surgical resection of well-differentiated pancreatic neuroendocrine tumors. J. Surg. Oncol. 2018, 118, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Boons, G.; Vandamme, T.; Mariën, L.; Lybaert, W.; Roeyen, G.; Rondou, T.; Papadimitriou, K.; Janssens, K.; Op De Beeck, B.; Simoens, M.; et al. Longitudinal Copy-Number Alteration Analysis in Plasma Cell-Free DNA of Neuroendocrine Neoplasms is a Novel Specific Biomarker for Diagnosis, Prognosis, and Follow-up. Clin. Cancer Res. 2022, 28, 338–349. [Google Scholar] [CrossRef]
- Knappskog, S.; Grob, T.; Venizelos, A.; Amstutz, U.; Hjortland, G.O.; Lothe, I.M.; Kersten, C.; Hofsli, E.; Sundlöv, A.; Elvebakken, H.; et al. Mutation Spectrum in Liquid Versus Solid Biopsies From Patients with Advanced Gastroenteropancreatic Neuroendocrine Carcinoma. JCO Precis. Oncol. 2023, 7, e2200336. [Google Scholar] [CrossRef]
- Zakka, K.; Nagy, R.; Drusbosky, L.; Akce, M.; Wu, C.; Alese, O.B.; El-Rayes, B.F.; Kasi, P.M.; Mody, K.; Starr, J.; et al. Blood-based next-generation sequencing analysis of neuroendocrine neoplasms. Oncotarget 2020, 11, 1749–1757. [Google Scholar] [CrossRef]
- Lamarca, A.; Frizziero, M.; Barriuso, J.; Kapacee, Z.; Mansoor, W.; McNamara, M.G.; Hubner, R.A.; Valle, J.W. Molecular Profiling of Well-Differentiated Neuroendocrine Tumours: The Role of ctDNA in Real-World Practice. Cancers 2022, 14, 1017. [Google Scholar] [CrossRef]
- Liu, E.; Paulson, S.; Gulati, A.; Freudman, J.; Grosh, W.; Kafer, S.; Wickremesinghe, P.C.; Salem, R.R.; Bodei, L. Assessment of NETest Clinical Utility in a U.S. Registry-Based Study. Oncologist 2019, 24, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Pavel, M.; Jann, H.; Prasad, V.; Drozdov, I.; Modlin, I.M.; Kidd, M. NET Blood Transcript Analysis Defines the Crossing of the Clinical Rubicon: When Stable Disease Becomes Progressive. Neuroendocrinology 2017, 104, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Kidd, M.; Kitz, A.; Drozdov, I.; Modlin, I. Neuroendocrine Tumor Omic Gene Cluster Analysis Amplifies the Prognostic Accuracy of the NETest. Neuroendocrinology 2021, 111, 490–504. [Google Scholar] [CrossRef] [PubMed]
- Ćwikła, J.B.; Bodei, L.; Kolasinska-Ćwikła, A.; Sankowski, A.; Modlin, I.M.; Kidd, M. Circulating Transcript Analysis (NETest) in GEP-NETs Treated with Somatostatin Analogs Defines Therapy. J. Clin. Endocrinol. Metab. 2015, 100, E1437–E1445. [Google Scholar] [CrossRef] [PubMed]
- Bodei, L.; Raj, N.; Do, R.K.; Mauguen, A.; Krebs, S.; Reidy-Lagunes, D.; Schöder, H. Interim Analysis of a Prospective Validation of 2 Blood-Based Genomic Assessments (PPQ and NETest) to Determine the Clinical Efficacy of 177Lu-DOTATATE in Neuroendocrine Tumors. J. Nucl. Med. 2023, 64, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Bodei, L.; Kidd, M.S.; Singh, A.; Van Der Zwan, W.A.; Severi, S.; Drozdov, I.A.; Malczewska, A.; Baum, R.P.; Kwekkeboom, D.J.; Paganelli, G.; et al. PRRT neuroendocrine tumor response monitored using circulating transcript analysis: The NETest. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 895–906. [Google Scholar] [CrossRef]
- Kidd, M.; Modlin, I.M. The role of liquid biopsies to manage and predict PRRT for NETs. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 331–332. [Google Scholar] [CrossRef]
- Malczewska, A.; Witkowska, M.; Wójcik-Giertuga, M.; Kuśnierz, K.; Bocian, A.; Walter, A.; Rydel, M.; Robek, A.; Pierzchała, S.; Malczewska, M.; et al. Prospective Evaluation of the NETest as a Liquid Biopsy for Gastroenteropancreatic and Bronchopulmonary Neuroendocrine Tumors: An ENETS Center of Excellence Experience. Neuroendocrinology 2021, 111, 304–319. [Google Scholar] [CrossRef]
- Modlin, I.M.; Drozdov, I.; Alaimo, D.; Callahan, S.; Teixiera, N.; Bodei, L.; Kidd, M. A multianalyte PCR blood test outperforms single analyte ELISAs (chromogranin A, pancreastatin, neurokinin A) for neuroendocrine tumor detection. Endocr. Relat. Cancer 2014, 21, 615–628. [Google Scholar] [CrossRef] [PubMed]
- Modlin, I.M.; Kidd, M.; Bodei, L.; Drozdov, I.; Aslanian, H. The Clinical Utility of a Novel Blood-Based Multi-Transcriptome Assay for the Diagnosis of Neuroendocrine Tumors of the Gastrointestinal Tract. Am. J. Gastroenterol. 2015, 110, 1223–1232. [Google Scholar] [CrossRef] [PubMed]
- Malczewska, A.; Witkowska, M.; Makulik, K.; Bocian, A.; Walter, A.; Pilch-Kowalczyk, J.; Zajęcki, W.; Bodei, L.; Oberg, K.; Kos-Kudła, B. NETest liquid biopsy is diagnostic of small intestine and pancreatic neuroendocrine tumors and correlates with imaging. Endocr. Connect. 2019, 8, 442–453. [Google Scholar] [CrossRef] [PubMed]
- Mettler, E.; Fottner, C.; Bakhshandeh, N.; Trenkler, A.; Kuchen, R.; Weber, M.M. Quantitative Analysis of Plasma Cell-Free DNA and Its DNA Integrity and Hypomethylation Status as Biomarkers for Tumor Burden and Disease Progression in Patients with Metastatic Neuroendocrine Neoplasias. Cancers 2022, 14, 1025. [Google Scholar] [CrossRef]
- Partelli, S.; Andreasi, V.; Muffatti, F.; Schiavo Lena, M.; Falconi, M. Circulating Neuroendocrine Gene Transcripts (NETest): A Postoperative Strategy for Early Identification of the Efficacy of Radical Surgery for Pancreatic Neuroendocrine Tumors. Ann. Surg. Oncol. 2020, 27, 3928–3936. [Google Scholar] [CrossRef]
- Modlin, I.M.; Kidd, M.; Oberg, K.; Falconi, M.; Filosso, P.L.; Frilling, A.; Malczewska, A.; Salem, R.; Toumpanakis, C.; Laskaratos, F.-M.; et al. Early Identification of Residual Disease After Neuroendocrine Tumor Resection Using a Liquid Biopsy Multigenomic mRNA Signature (NETest). Ann. Surg. Oncol. 2021, 28, 7506–7517. [Google Scholar] [CrossRef] [PubMed]
- van Treijen, M.J.C.; van der Zee, D.; Heeres, B.C.; Staal, F.C.R.; Vriens, M.R.; Saveur, L.J.; Verbeek, W.H.M.; Korse, C.M.; Maas, M.; Valk, G.D.; et al. Blood Molecular Genomic Analysis Predicts the Disease Course of Gastroenteropancreatic Neuroendocrine Tumor Patients: A Validation Study of the Predictive Value of the NETest®. Neuroendocrinology 2021, 111, 586–598. [Google Scholar] [CrossRef] [PubMed]
- Laskaratos, F.-M.; Liu, M.; Malczewska, A.; Ogunbiyi, O.; Watkins, J.; Luong, T.V.; Mandair, D.; Caplin, M.; Toumpanakis, C. Evaluation of circulating transcript analysis (NETest) in small intestinal neuroendocrine neoplasms after surgical resection. Endocrine 2020, 69, 430–440. [Google Scholar] [CrossRef]
- Modlin, I.M.; Kidd, M.; Frilling, A.; Falconi, M.; Filosso, P.L.; Malczewska, A.; Kitz, A. Molecular Genomic Assessment Using a Blood-based mRNA Signature (NETest) is Cost-effective and Predicts Neuroendocrine Tumor Recurrence with 94% Accuracy. Ann. Surg. 2021, 274, 481–490. [Google Scholar] [CrossRef]
- Van Treijen, M.J.C.; Korse, C.M.; Verbeek, W.H.; Tesselaar, M.E.T.; Valk, G.D. NETest: Serial liquid biopsies in gastroenteropancreatic NET surveillance. Endocr. Connect. 2022, 11, e220146. [Google Scholar] [CrossRef] [PubMed]
- Bodei, L.; Kidd, M.; Modlin, I.M.; Severi, S.; Drozdov, I.; Nicolini, S.; Kwekkeboom, D.J.; Krenning, E.P.; Baum, R.P.; Paganelli, G. Measurement of circulating transcripts and gene cluster analysis predicts and defines therapeutic efficacy of peptide receptor radionuclide therapy (PRRT) in neuroendocrine tumors. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 839–851. [Google Scholar] [CrossRef]
- Childs, A.; Steele, C.D.; Vesely, C.; Rizzo, F.M.; Ensell, L.; Lowe, H.; Dhami, P.; Vaikkinen, H.; Luong, T.V.; Conde, L.; et al. Whole-genome sequencing of single circulating tumor cells from neuroendocrine neoplasms. Endocr. Relat. Cancer 2021, 28, 631–644. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.-J.; Shin, S.H.; Kim, H.H.; Min, N.Y.; Lim, Y.; Joo, T.; Lee, K.J.; Jeong, M.-S.; Kim, H.; Yun, S.; et al. Advances in methylation analysis of liquid biopsy in early cancer detection of colorectal and lung cancer. Sci. Rep. 2023, 13, 13502. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, G.M.; Quaini, O.; Mizuno, K.; Orlando, F.; Ciani, Y.; Ku, S.-Y.; Sigouros, M.; Rothmann, E.; Alonso, A.; Benelli, M.; et al. Noninvasive Detection of Neuroendocrine Prostate Cancer through Targeted Cell-free DNA Methylation. Cancer Discov. 2024, 14, 424–445. [Google Scholar] [CrossRef] [PubMed]
- Lau, B.T.; Almeda, A.; Schauer, M.; McNamara, M.; Bai, X.; Meng, Q.; Partha, M.; Grimes, S.M.; Lee, H.; Heestand, G.M.; et al. Single-molecule methylation profiles of cell-free DNA in cancer with nanopore sequencing. Genome Med. 2023, 15, 33. [Google Scholar] [CrossRef]
- Sorbye, H.; Hjortland, G.; Vestermark, L. NETest in advanced high-grade gastroenteropancreatic neuroendocrine neoplasms. J. Neuroendocrinol. 2024, e13428. [Google Scholar] [CrossRef]
| Types of Liquid Biopsy | Main Clinical Applications |
|---|---|
| Circulating Tumour Cells (CTCs) | Predictive value on disease progression and survival; treatment response [8,9,10,26,27] |
| Circulating tumour DNA (ctDNA) | Diagnosis and characterisation; predictive value on disease recurrence [5,12,13,28,29,30,31,32,33,34,35,36,37,38] |
| Micro RNA (miRNA) | Diagnosis and characterisation [17] |
| Messenger RNA (mRNA) | Diagnosis; prognostic and predictive value on disease recurrence; monitoring treatment response [20,21,39,40,41,42,43,44,45,46,47,48,49] |
| Extracellular vesicles | Characterisation [25] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almeida, C.; Gervaso, L.; Frigè, G.; Spada, F.; Benini, L.; Cella, C.A.; Mazzarella, L.; Fazio, N. The Role of Liquid Biopsy in Gastroenteropancreatic Neuroendocrine Neoplasms. Cancers 2024, 16, 3349. https://doi.org/10.3390/cancers16193349
Almeida C, Gervaso L, Frigè G, Spada F, Benini L, Cella CA, Mazzarella L, Fazio N. The Role of Liquid Biopsy in Gastroenteropancreatic Neuroendocrine Neoplasms. Cancers. 2024; 16(19):3349. https://doi.org/10.3390/cancers16193349
Chicago/Turabian StyleAlmeida, Catarina, Lorenzo Gervaso, Gianmaria Frigè, Francesca Spada, Lavinia Benini, Chiara Alessandra Cella, Luca Mazzarella, and Nicola Fazio. 2024. "The Role of Liquid Biopsy in Gastroenteropancreatic Neuroendocrine Neoplasms" Cancers 16, no. 19: 3349. https://doi.org/10.3390/cancers16193349
APA StyleAlmeida, C., Gervaso, L., Frigè, G., Spada, F., Benini, L., Cella, C. A., Mazzarella, L., & Fazio, N. (2024). The Role of Liquid Biopsy in Gastroenteropancreatic Neuroendocrine Neoplasms. Cancers, 16(19), 3349. https://doi.org/10.3390/cancers16193349







