Real-World Impact of Deep Targeted Sequencing on Erythrocytosis and Thrombocytosis Diagnosis: A Reference Centre Experience
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Next-Generation Sequencing of a Panel of Myeloid Genes
2.3. Statistical Analysis
3. Results
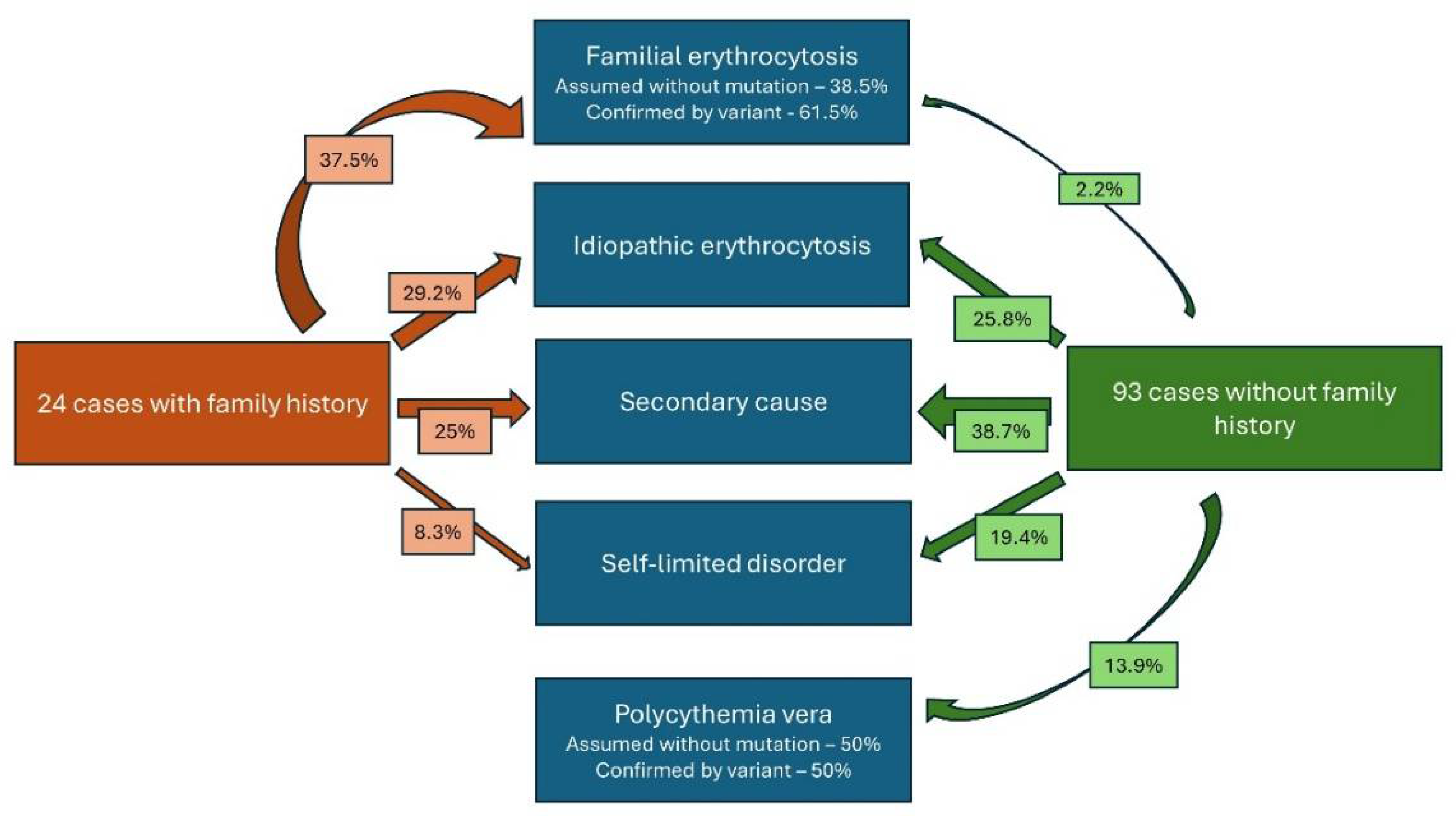
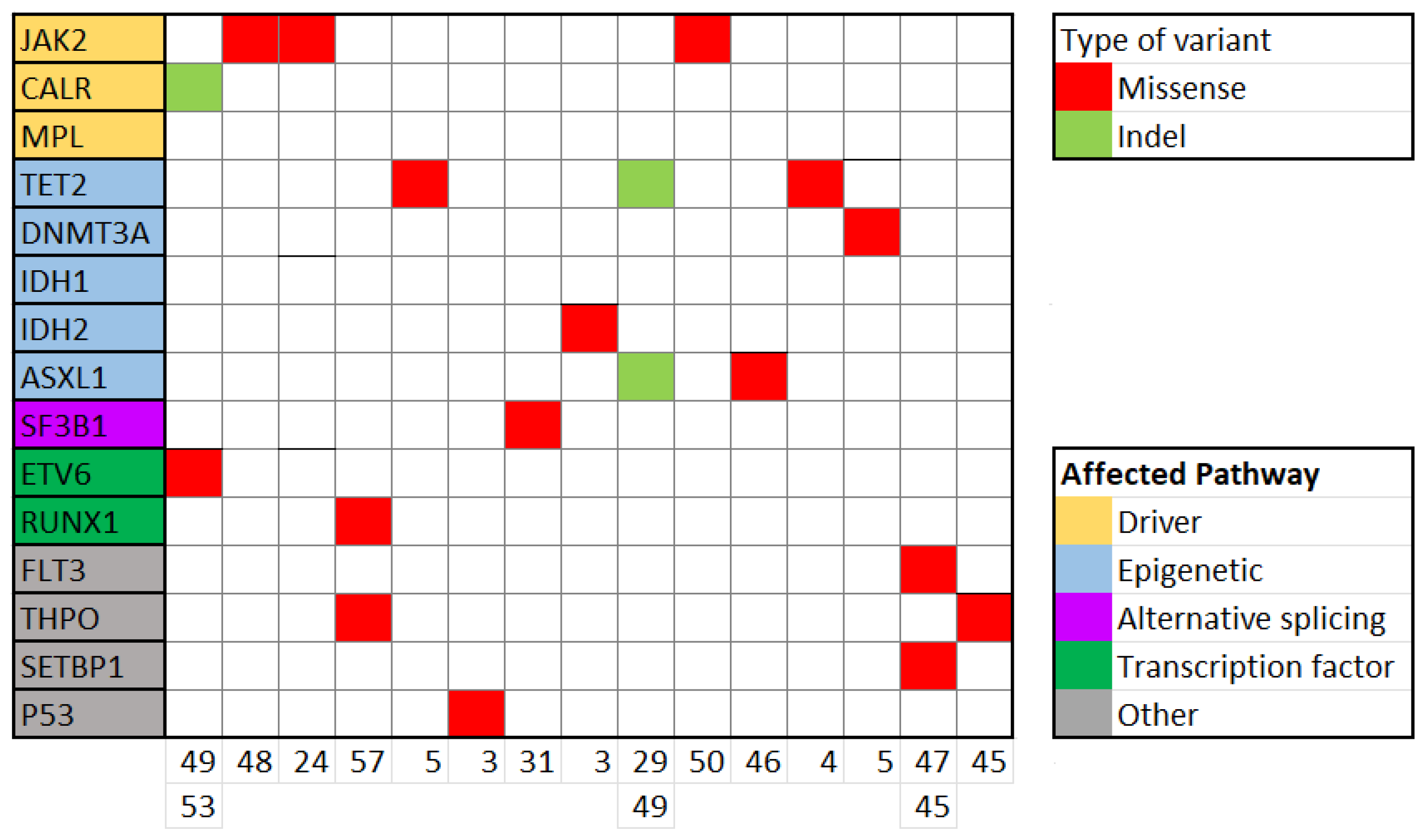
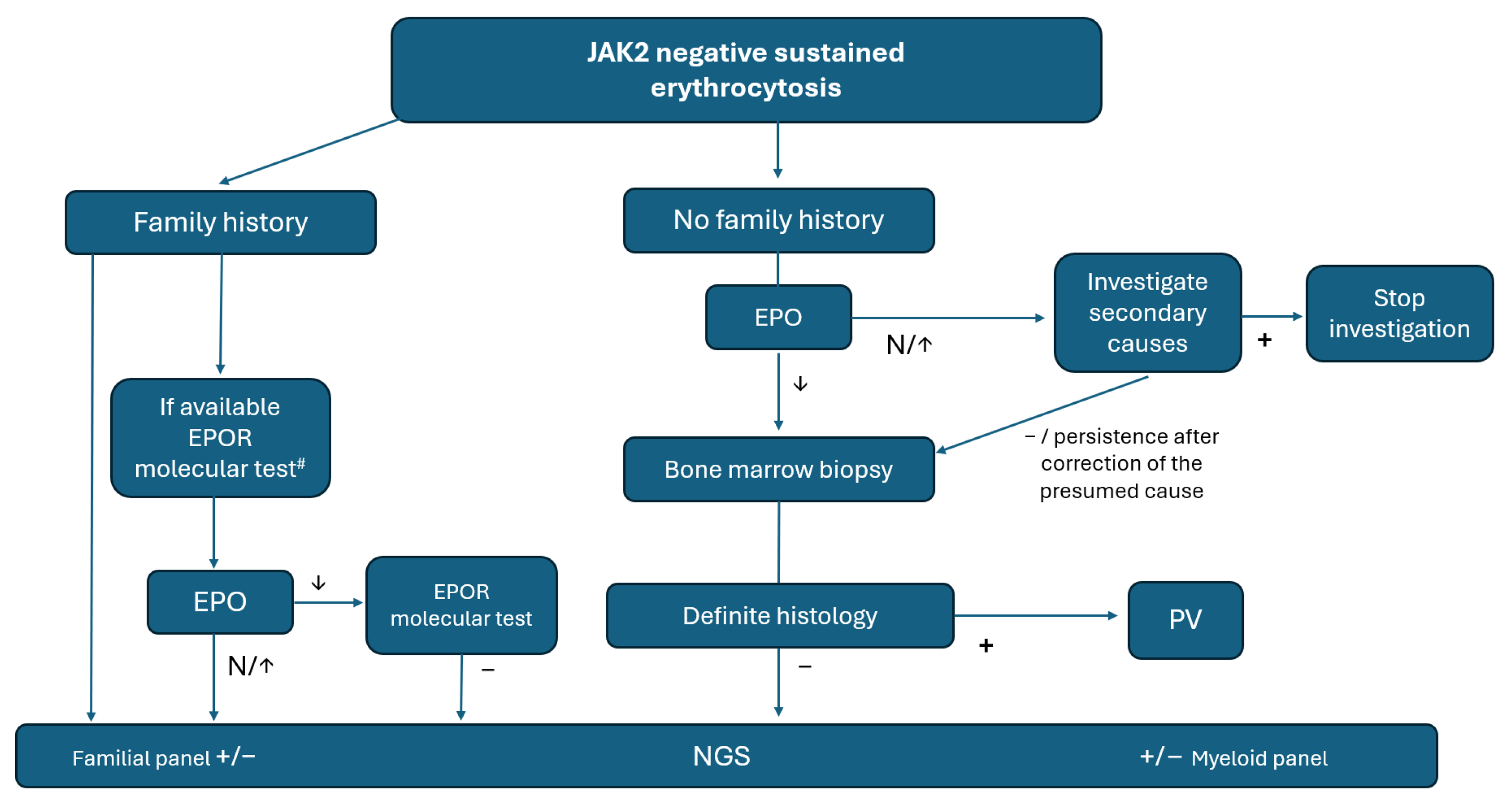
3.1. Erythrocytosis
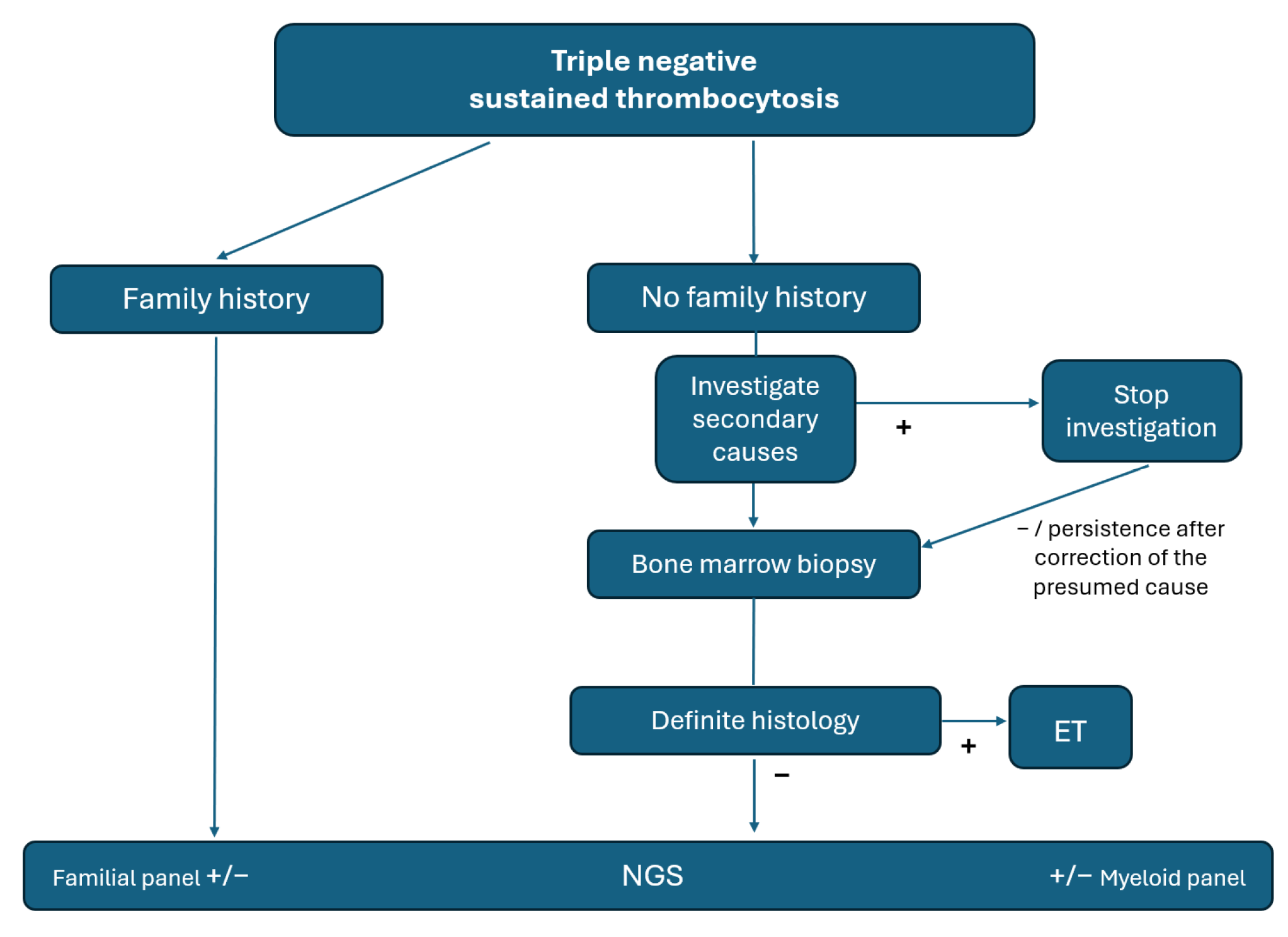
3.2. Thrombocytosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McMullin, M.F.; Harrison, C.N.; Ali, S.; Cargo, C.; Chen, F.; Ewing, J.; Garg, M.; Godfrey, A.; Knapper, S.; McLornan, D.P.; et al. A guideline for the diagnosis and management of polycythaemia vera. A British Society for Haematology Guideline. Br. J. Haematol. 2019, 184, 176–191. [Google Scholar] [CrossRef] [PubMed]
- Pizzi, M.; Croci, G.A.; Ruggeri, M.; Tabano, S.; Dei Tos, A.P.; Sabattini, E.; Gianelli, U. The classification of myeloproliferative neoplasms: Rationale, historical background and future perspectives with focus on unclassifiable cases. Cancers 2021, 13, 5666. [Google Scholar] [CrossRef] [PubMed]
- Tefferi, A.; Barbui, T. Polycythemia vera and essential thrombocythemia: 2021 update on diagnosis, risk-stratification and management. Am. J. Hematol. 2020, 95, 1599–1613. [Google Scholar] [CrossRef]
- Ng, W.Y.; Erber, W.N.; Grigg, A.; Dunne, K.; Perkins, A.; Forsyth, C.; Ross, D.M. Variability of bone marrow biopsy reporting affects accuracy of diagnosis of myeloproliferative neoplasms: Data from the ALLG MPN01 registry. Pathology 2024, 56, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Kralovics, R.; Passamonti, F.; Buser, A.S.; Teo, S.S.; Tiedt, R.; Passweg, J.R.; Tichelli, A.; Cazzola, M.; Skoda, R.C. A Gain-of-Function Mutation of JAK2 in Myeloproliferative Disorders. N. Engl. J. Med. 2005, 352, 1779–1790. [Google Scholar] [CrossRef] [PubMed]
- Nangalia, J.; Massie, C.E.; Baxter, E.J.; Nice, F.L.; Gundem, G.; Wedge, D.C.; Avezov, E.; Li, J.; Kollmann, K.; Kent, D.G.; et al. Somatic CALR Mutations in Myeloproliferative Neoplasms with Nonmutated JAK2. N. Engl. J. Med. 2013, 369, 2391–2405. [Google Scholar] [CrossRef]
- Vannucchi, A.M.; Antonioli, E.; Guglielmelli, P.; Pancrazzi, A.; Guerini, V.; Barosi, G.; Ruggeri, M.; Specchia, G.; Lo-Coco, F.; Delaini, F.; et al. Characteristics and clinical correlates of MPL 515W>L/K mutation in essential thrombocythemia. Blood 2008, 112, 844–847. [Google Scholar] [CrossRef]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) Myeloproliferative Neoplasms Version 2.2024–8 August 2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/mpn.pdf (accessed on 5 September 2024).
- Rumi, E.; Cazzola, M. Diagnosis, risk stratification, and response evaluation in classical myeloproliferative neoplasms. Blood 2017, 129, 680–692. [Google Scholar] [CrossRef]
- Gangat, N.; Szuber, N.; Pardanani, A.; Tefferi, A. JAK2 unmutated erythrocytosis: Current diagnostic approach and therapeutic views. Leukemia 2021, 35, 2166–2181. [Google Scholar] [CrossRef]
- Cattaneo, D.; Croci, G.A.; Bucelli, C.; Tabano, S.; Cannone, M.G.; Gaudioso, G.; Barbanti, M.C.; Barbullushi, K.; Bianchi, P.; Fermo, E.; et al. Triple-Negative Essential Thrombocythemia: Clinical-Pathological and Molecular Features. A Single-Center Cohort Study. Front. Oncol. 2021, 11, 637116. [Google Scholar] [CrossRef]
- Mcmullin, M.F. Idiopathic erythrocytosis: A disappearing entity. Hematol. Am. Soc. Hematol. Educ. Program. 2009, 2009, 629–635. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sandes, A.F.; Gonçalves, M.V.; Chauffaille, M.L. Frequency of polycythemia in individuals with normal complete blood cell counts according to the new 2016 WHO classification of myeloid neoplasms. Int. J. Lab. Hematol. 2017, 39, 528–531. [Google Scholar] [CrossRef] [PubMed]
- Broséus, J.; Park, J.H.; Carillo, S.; Hermouet, S.; Girodon, F. Presence of calreticulin mutations in JAK2-negative polycythemia vera. Blood 2014, 124, 3964–3966. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.T.; Simonds, E.F.; Jones, C.; Hale, M.B.; Goltsev, Y.; Gibbs, K.D.; Merker, J.D.; Zehnder, J.L.; Nolan, G.P.; Gotlib, J. Novel mutations in the inhibitory adaptor protein LNK drive JAK-STAT signaling in patients with myeloproliferative neoplasms. Blood 2010, 116, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Han, E.Y.; Catherwood, M.; McMullin, M.F. Hereditary thrombocytosis: The genetic landscape. Br. J. Haematol. 2021, 194, 1098–1105. [Google Scholar] [CrossRef]
- Carreño-Tarragona, G.; Varghese, L.N.; Sebastián, E.; Gálvez, E.; Marín-Sánchez, A.; López-Muñoz, N.; Nam-Cha, S.; Martínez-López, J.; Constantinescu, S.N.; Sevilla, J.; et al. A typical acute lymphoblastic leukemia JAK2 variant, R683G, causes an aggressive form of familial thrombocytosis when germline. Leukemia 2021, 35, 3295–3298. [Google Scholar] [CrossRef]
- Bellanné-Chantelot, C.; Mosca, M.; Marty, C.; Favier, R.; Vainchenker, W.; Plo, I. Identification of MPL R102P Mutation in Hereditary Thrombocytosis. Front. Endocrinol. 2017, 8, 235. [Google Scholar] [CrossRef]
- Hansen, M.C.; Haferlach, T.; Nyvold, C.G. A decade with whole exome sequencing in haematology. Br. J. Haematol. 2020, 188, 367–382. [Google Scholar] [CrossRef]
- Ramkissoon, L.A.; Montgomery, N.D. Applications of next-generation sequencing in hematologic malignancies. Hum. Immunol. 2021, 82, 859–870. [Google Scholar] [CrossRef]
- Camps, C.; Petousi, N.; Bento, C.; Cario, H.; Copley, R.R.; McMullin, M.F.; van Wijk, R.; Ratcliffe, P.J.; Robbins, P.A.; Taylor, J.C. Gene panel sequencing improves the diagnostic work-up of patients with idiopathic erythrocytosis and identifies new mutations. Haematologica 2016, 101, 1306–1318. [Google Scholar] [CrossRef]
- Almanaseer, A.; Chin-Yee, B.; Ho, J.; Lazo-Langner, A.; Schenkel, L.; Bhai, P.; Sadikovic, B.; Chin-Yee, I.H.; Hsia, C.C. An Approach to the Investigation of Thrombocytosis: Differentiating between Essential Thrombocythemia and Secondary Thrombocytosis. Adv. Hematol. 2024, 2024, 3056216. [Google Scholar] [CrossRef] [PubMed]
- Bhai, P.; Chin-Yee, B.; Pope, V.; Cheong, I.; Matyashin, M.; Levy, M.A.; Foroutan, A.; Stuart, A.; Hsia, C.C.; Lin, H.; et al. Mutational Landscape of Patients Referred for Elevated Hemoglobin Level. Curr. Oncol. 2022, 29, 7209–7217. [Google Scholar] [CrossRef] [PubMed]
- Benetti, A.; Bertozzi, I.; Ceolotto, G.; Cortella, I.; Regazzo, D.; Biagetti, G.; Cosi, E.; Randi, M.L. Coexistence of multiple gene variants in some patients with erythrocytoses. Mediterr. J. Hematol. Infect. Dis. 2024, 16, e2024021. [Google Scholar] [CrossRef]
- Jalowiec, K.A.; Vrotniakaite-Bajerciene, K.; Jalowiec, J.; Frey, N.; Capraru, A.; Wojtovicova, T.; Joncourt, R.; Angelillo-Scherrer, A.; Tichelli, A.; Porret, N.A.; et al. JAK2 Unmutated Polycythaemia—Real-World Data of 10 Years from a Tertiary Reference Hospital. J. Clin. Med. 2022, 11, 3393. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Seo, S.H.; Kim, J.; Kim, S.A.; Lee, J.Y.; Lee, J.O.; Bang, S.M.; Park, K.U.; Hwang, S.M. Diagnostic Approaches to Investigate JAK2-Unmutated Erythrocytosis Based on a Single Tertiary Center Experience. Mol. Diagn. Ther. 2024, 28, 311–318. [Google Scholar] [CrossRef]
- Feenstra, J.D.M.; Nivarthi, H.; Gisslinger, H.; Leroy, E.; Rumi, E.; Chachoua, I.; Bagienski, K.; Kubesova, B.; Pietra, D.; Gisslinger, B.; et al. Whole-exome sequencing identifies novel MPL and JAK2 mutations in triple-negative myeloproliferative neoplasms. Blood 2016, 127, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Li, M.M.; Datto, M.; Duncavage, E.J.; Kulkarni, S.; Lindeman, N.I.; Roy, S.; Tsimberidou, A.M.; Vnencak-Jones, C.L.; Wolff, D.J.; Younes, A.; et al. Standards and Guidelines for the Interpretation and Reporting of Sequence Variants in Cancer. J. Mol. Diagn. 2017, 19, 4–23. [Google Scholar] [CrossRef]
- Chin-Yee, B.; Cheong, I.; Matyashin, M.; Lazo-Langner, A.; Chin-Yee, I.; Bhayana, V.; Bhai, P.; Lin, H.; Sadikovic, B.; Hsia, C.C. Serum erythropoietin levels in 696 patients investigated for erythrocytosis with JAK2 mutation analysis. Am. J. Hematol. 2022, 97, E150. [Google Scholar] [CrossRef]
- Hamilton, K.V.; Fox, L.C.; Nichols, K.E. How I Communicate with Patients and Families about Germline Genetic Information. Blood 2023, 141, 3143–3152. [Google Scholar] [CrossRef]
- Godley, L.A.; Shimamura, A. Genetic predisposition to hematologic malignancies: Management and surveillance. Blood 2017, 130, 424–432. [Google Scholar] [CrossRef]
- Gondek, L.P.; DeZern, A.E. Assessing clonal haematopoiesis: Clinical burdens and benefits of diagnosing myelodysplastic syndrome precursor states. Lancet Haematol. 2020, 7, e73–e81. [Google Scholar] [CrossRef]
- Geay, A.; Aral, B.; Bourgeois, V.; Martin, P.; Airaud, F.; Garrec, C.; Bézieau, S.; Gardie, B.; Girodon, F. Diagnosis of exon 12-positive polycythemia vera rescued by NGS. Clin. Case Rep. 2020, 8, 790–792. [Google Scholar] [CrossRef] [PubMed]
- Wouters, H.J.C.M.; Mulder, R.; van Zeventer, I.A.; Schuringa, J.J.; van der Klauw, M.M.; van der Harst, P.; Diepstra, A.; Mulder, A.B.; Huls, G. Erythrocytosis in the general population: Clinical characteristics and association with clonal hematopoiesis. Blood Adv. 2020, 4, 6353–6363. [Google Scholar] [CrossRef] [PubMed]
- Lemoine, S.; Mornet, C.; Quintin-Roue, I.; Rousselet, M.C.; Cottin, L.; Georgeais, A.; Dubouis, L.; Boyer, F.; Orvain, C.; Caillon, C.; et al. Histological and genetic characterization and follow-up of 130 patients with chronic triple-negative thrombocytosis. Haematologica 2022, 107, 2725–2731. [Google Scholar] [CrossRef] [PubMed]
- Acha, P.; Xandri, M.; Fuster-Tormo, F.; Palomo, L.; Xicoy, B.; Cabezón, M.; Marcé, S.; Granada, I.; Vela, D.; Sagüés, M.; et al. Diagnostic and prognostic contribution of targeted NGS in patients with triple-negative myeloproliferative neoplasms. Am. J. Hematol. 2019, 94, E264–E267. [Google Scholar] [CrossRef] [PubMed]
- Michail, O.; McCallion, P.; McGimpsey, J.; Hindley, A.; Greenfield, G.; McAllister, R.; Feerick, J.; Arnold, C.; Cross, N.; Cuthbert, R.; et al. Mutational profiling in suspected triple-negative essential thrombocythaemia using targeted next-generation sequencing in a real-world cohort. J. Clin. Pathol. 2021, 74, 808–811. [Google Scholar] [CrossRef]
- Gisslinger, H.; Jeryczynski, G.; Gisslinger, B.; Wölfler, A.; Burgstaller, S.; Buxhofer-Ausch, V.; Schalling, M.; Krauth, M.T.; Schiefer, A.I.; Kornauth, C.; et al. Clinical impact of bone marrow morphology for the diagnosis of essential thrombocythemia: Comparison between the BCSH and the WHO criteria. Leukemia 2016, 30, 1126–1132. [Google Scholar] [CrossRef]
- Harrison, C.N.; Bareford, D.; Butt, N.; Campbell, P.; Conneally, E.; Drummond, M.; Erber, W.; Everington, T.; Green, A.R.; Hall, G.W.; et al. Guideline for investigation and management of adults and children presenting with a thrombocytosis. Br. J. Haematol. 2010, 149, 352–375. [Google Scholar] [CrossRef]
- Grinfeld, J.; Nangalia, J.; Baxter, E.J.; Wedge, D.C.; Angelopoulos, N.; Cantrill, R.; Godfrey, A.L.; Papaemmanuil, E.; Gundem, G.; MacLean, C.; et al. Classification and Personalized Prognosis in Myeloproliferative Neoplasms. N. Eng. J. Med. 2018, 379, 1416–1430. [Google Scholar] [CrossRef]
| Clinical Characteristics (n = 117) | |
|---|---|
| Age at the time of NGS | 59 (43–75) |
| Male (n, %) | 87 (74.4%) |
| Female (n, %) | 30 (25.6%) |
| Previous thrombosis (n, %) | 13 (11.1%) |
| Complete blood count (at first visit) | |
| Haemoglobin (g/dL) | 17.6 (17.1–18.1) |
| Haematocrit (%) | 53.1 (51.6–54.6) |
| Leucocytes (×109/L) | 6.9 (5.8–8) |
| Platelets (×109/L) | 225 (187–263) |
| Other objective parameters | |
| Normal or elevated EPO (n, %) | 98 (83.8%) |
| Low EPO (n, %) | 15 (12.8%) |
| Not available (n, %) | 4 (3.4%) |
| Bone marrow available (n, %) | 34 (29.1%) |
| Bone marrow consistent with MPN (n, %) | 6 (17.6%) |
| Bone marrow inconclusive (n, %) | 14 (41.2%) |
| Normal histology, excluding PV (n, %) | 14 (41.2%) |
| Abdominal ultrasonography available (n, %) | 100 (85.5%) |
| No splenomegaly (n, %) | 100 (100%) |
| No Mutation (n = 103) | Diagnostic Variant (n = 14) | p | PV Variant (n = 6) | p | Familial Variant (n = 8) | p | |
|---|---|---|---|---|---|---|---|
| Male, % | 78.6% | 71.4% | 0.7 | 83.3% | 1 | 62.5% | 0.6 |
| Age at first visit (years) | 49.9 ± 7 | 58.7 ± 9 | 0.1 | 59.6 ± 22 | 0.2 | 56.7 ± 15.9 | 0.4 |
| Hb at first visit (g/dL) | 17.5 ± 0.6 | 17.6 ± 0.4 | 0.6 | 17.5 ± 0.5 | 0.6 | 17.6 ± 1 | 0.9 |
| Hct at first visit (%) | 52.9 ± 2.4 | 53.4 ± 1.9 | 0.7 | 54.7 ± 4.2 | 0.3 | 52.4 ± 3.6 | 0.6 |
| Leucocytes (×109/L) | 7.3 ± 0.8 | 6.7 ± 0.5 | 0.3 | 6.2 ± 0.9 | 0.2 | 7.3 ± 0.7 | 0.9 |
| Platelets (×109/L) | 223 ± 18.5 | 234 ± 24 | 0.3 | 225 ± 71 | 0.7 | 242 ± 33 | 0.3 |
| Previous thrombosis | 7.8% | 28.6% | 0.015 | 50% | 0.01 | 12.5% | 0.4 |
| Low EPO | 9.4% | 83.3% | 0.01 | ||||
| Family history | 19.4% | 50% | 0.65 | ||||
| 66.6% | 0.02 * |
| Clinical Characteristics (n = 58) | |
|---|---|
| Age at the time of NGS | 54.5 (46.6–62.4) |
| Male (n, %) | 12 (20.7%) |
| Female (n, %) | 46 (79.3%) |
| Previous thrombosis (n, %) | 4 (6.9%) |
| Complete blood count (at first visit) | |
| Haemoglobin (g/dL) | 14 (13.4–14.6) |
| Haematocrit (%) | 41.8 (39.5–44.2) |
| Leucocytes (×109/L) | 8.9 (7.4–10.4) |
| Platelets (×109/L) | 618 (523–713) |
| Other objective parameters | |
| Bone marrow available | 46 (79.3%) |
| Bone marrow consistent | 16 (34.8%) |
| Bone marrow inconclusive | 18 (39.1%) |
| Bone marrow normal | 12 (26.1%) |
| Abdominal ultrasonography available | 40 (69%) |
| No splenomegaly | 100 (100%) |
| No Mutation (n = 43) | Diagnostic Variant (n = 15) | p | |
|---|---|---|---|
| Female | 82.9% | 70.6% | 0.3 |
| Age at the time of NGS (y) | 56 ± 11.5 | 59 ± 13 | |
| Platelets at first visit | 575 ± 115 | 725 ± 200 | 0.8 |
| Hb at first visit (g/dL) | 13.9 ± 0.8 | 14.1 ± 1.1 | 0.9 |
| Hct at first visit (%) | 41.2 ± 3 | 44.3 ± 2.3 | 0.6 |
| Leucocytes at first visit (×109/L) | 8.3 ± 1.3 | 8.2 ± 3.1 | 0.5 |
| Thrombosis at first visit (×109/L) | 4.9% | 11.8% | 0.3 |
| Bone marrow consistent | 28.1% | 40% | |
| Bone marrow inconclusive | 43.8% | 40% | |
| Bone marrow normal | 28.1% | 20% | 0.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blanco-Sánchez, A.; Gil-Manso, R.; de Nicolás, R.; López-Muñoz, N.; Colmenares, R.; Mas, R.; Sánchez, R.; Rapado, I.; Martínez-López, J.; Díaz, R.A.; et al. Real-World Impact of Deep Targeted Sequencing on Erythrocytosis and Thrombocytosis Diagnosis: A Reference Centre Experience. Cancers 2024, 16, 3149. https://doi.org/10.3390/cancers16183149
Blanco-Sánchez A, Gil-Manso R, de Nicolás R, López-Muñoz N, Colmenares R, Mas R, Sánchez R, Rapado I, Martínez-López J, Díaz RA, et al. Real-World Impact of Deep Targeted Sequencing on Erythrocytosis and Thrombocytosis Diagnosis: A Reference Centre Experience. Cancers. 2024; 16(18):3149. https://doi.org/10.3390/cancers16183149
Chicago/Turabian StyleBlanco-Sánchez, Alberto, Rodrigo Gil-Manso, Rodrigo de Nicolás, Nieves López-Muñoz, Rafael Colmenares, Reyes Mas, Ricardo Sánchez, Inmaculada Rapado, Joaquín Martínez-López, Rosa Ayala Díaz, and et al. 2024. "Real-World Impact of Deep Targeted Sequencing on Erythrocytosis and Thrombocytosis Diagnosis: A Reference Centre Experience" Cancers 16, no. 18: 3149. https://doi.org/10.3390/cancers16183149
APA StyleBlanco-Sánchez, A., Gil-Manso, R., de Nicolás, R., López-Muñoz, N., Colmenares, R., Mas, R., Sánchez, R., Rapado, I., Martínez-López, J., Díaz, R. A., & Carreño-Tarragona, G. (2024). Real-World Impact of Deep Targeted Sequencing on Erythrocytosis and Thrombocytosis Diagnosis: A Reference Centre Experience. Cancers, 16(18), 3149. https://doi.org/10.3390/cancers16183149






