Impact of Age, Period, Cohort, Region, Race, and Health Services on Bladder Cancer Mortality in Brazil: A 23-Year Ecological Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Type of Study and Ethical Aspects
2.2. Population
2.3. Inclusion and Exclusion Criteria
2.4. Database and Variables Analyzed
2.5. Statistical Analysis
3. Results
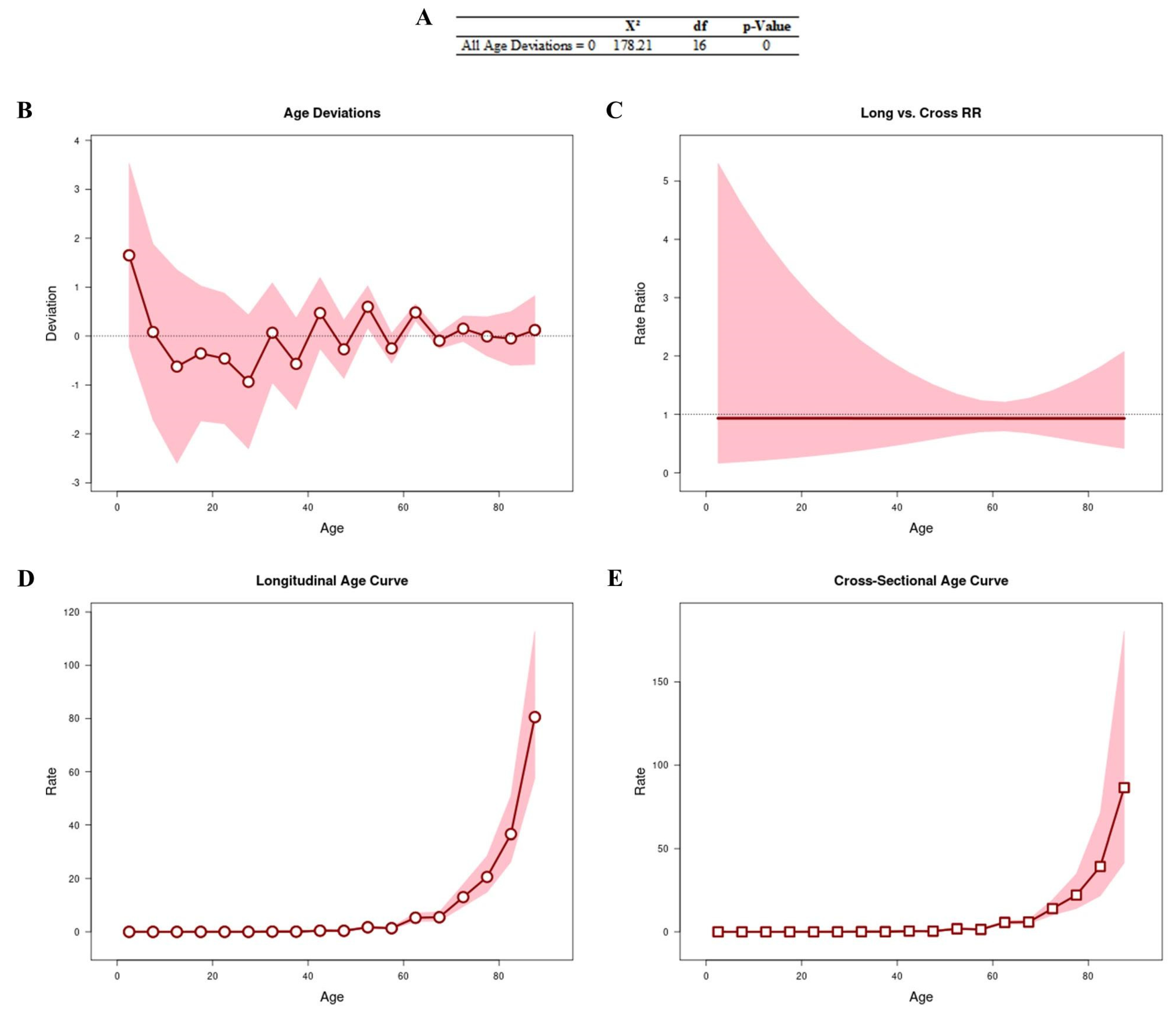
3.1. Age–Period–Cohort Effect
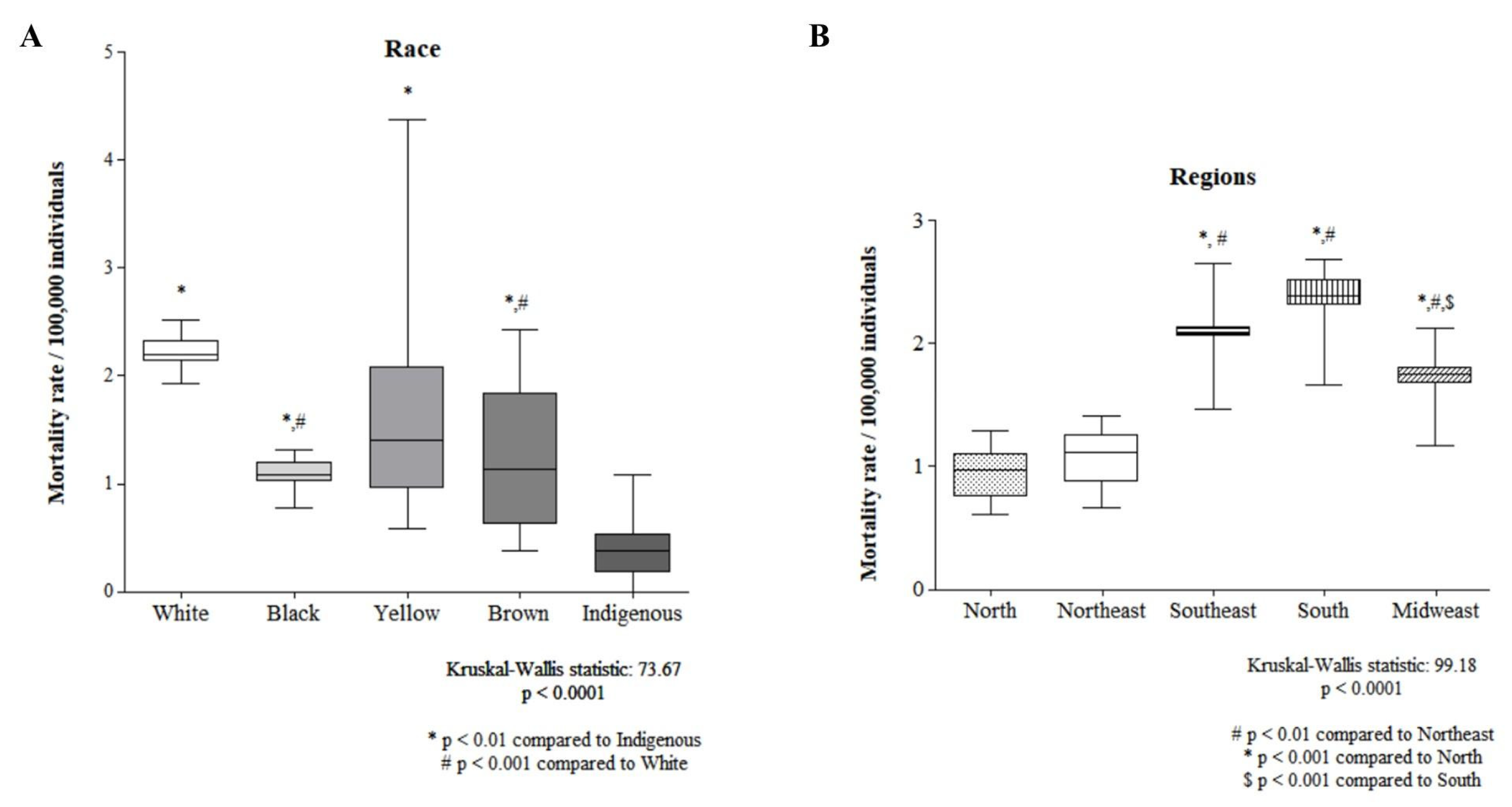
3.2. Sociodemographic Factors
3.3. Health Services, Diagnosis, and Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jubber, I.; Ong, S.; Bukavina, L.; Black, P.C.; Compérat, E.; Kamat, A.M.; Kiemeney, L.; Lawrentschuk, N.; Lerner, S.P.; Meeks, J.J.; et al. Epidemiology of Bladder Cancer in 2023: A Systematic Review of Risk Factors. Eur. Urol. 2023, 84, 176–190. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0302283823027070 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2024, 74, 229–263. Available online: https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21834 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Van Hoogstraten, L.M.C.; Vrieling, A.; Van Der Heijden, A.G.; Kogevinas, M.; Richters, A.; Kiemeney, L.A. Global trends in the epidemiology of bladder cancer: Challenges for public health and clinical practice. Nat. Rev. Clin. Oncol. 2023, 20, 287–304. Available online: https://www.nature.com/articles/s41571-023-00744-3 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Wéber, A.; Vignat, J.; Shah, R.; Morgan, E.; Laversanne, M.; Nagy, P.; Kenessey, I.; Znaor, A. Global burden of bladder cancer mortality in 2020 and 2040 according to GLOBOCAN estimates. World J. Urol. 2024, 42, 237. Available online: https://link.springer.com/10.1007/s00345-024-04949-8 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Instituto Nacional de Câncer. Estimativa 2023: Incidência de câncer no Brasil; Instituto Nacional De Câncer: Rio de Janeiro, Brasil, 2023. [Google Scholar]
- Chielle, E.O.; Kuiava, V.; Perin, A.T. Epidemiologia da neoplasia maligna de bexiga: Um estudo das taxas de mortalidade e de internação hospitalar. Rev. Atenção Saúde 2020, 17, 62. Available online: https://seer.uscs.edu.br/index.php/revista_ciencias_saude/article/view/5633 (accessed on 26 June 2024).
- Timoteo, F.; Korkes, F.; Baccaglini, W.; Glina, S. Bladder cancer trends and mortality in the brazilian public health system. Int. Braz. J. Urol. 2020, 46, 224–233. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1677-55382020000200224&tlng=en (accessed on 26 June 2024). [CrossRef] [PubMed]
- Teoh, J.Y.; Huang, J.; Ko, W.Y.; Lok, V.; Choi, P.; Ng, C.F.; Sengupta, S.; Mostafid, H.; Kamat, A.M.; Black, P.C.; et al. Global Trends of Bladder Cancer Incidence and Mortality, and Their Associations with Tobacco Use and Gross Domestic Product Per Capita. Eur. Urology 2020, 78, 893–906. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0302283820306977 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Paster, I.C.; Zeng, J.; Recio-Boiles, A.; Chipollini, J. Gender, Racial and Ethnic Differences in Pathologic Response Following Neoadjuvant Chemotherapy for Bladder Cancer Patients. Urology 2023, 178, 105–113. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0090429523004466 (accessed on 26 June 2024). [CrossRef] [PubMed]
- Thiese, M.S. Observational and interventional study design types; an overview. Biochem. Med. 2014, 24, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Wells, R.H.C.; Bay-Nielsen, H.; Braun, R.; Israel, R.A.; Laurenti, R.; Maguin, P.; Taylor, E. CID-10: Classificação Estatística Internacional de Doenças e Problemas Relacionados à Saúde; EDUSP: São Paulo, Brazil, 2011. [Google Scholar]
- Ahmad, O.B.; Boschi Pinto, C.; Lopez, A.D. Age Standardization of Rates: A New WHO Standard. GPE Discussion Paper Series: No 31. 2001; pp.10–12. Available online: https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf (accessed on 26 June 2024).
- Rosenberg, P.S.; Check, D.P.; Anderson, W.F. A Web Tool for Age–Period–Cohort Analysis of Cancer Incidence and Mortality Rates. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2296–2302. Available online: https://aacrjournals.org/cebp/article/23/11/2296/14669/A-Web-Tool-for-Age-Period-Cohort-Analysis-of (accessed on 4 July 2024). [CrossRef] [PubMed]
- Nascimento, A.Q.; Dantas, D.B.; Melo, G.S.; Gomes, F.D.C.; De Melo Neto, J.S. Impact of sociodemographic factors and screening, diagnosis, and treatment strategies on colorectal cancer mortality in Brazil: A 20-year ecological study. Patel GK, organizador. PLoS ONE 2022, 17, e0274572. Available online: https://dx.plos.org/10.1371/journal.pone.0274572 (accessed on 4 July 2024). [CrossRef] [PubMed]
- Palmeira, I.P.; Guimarães, L.D.S.; Santos, A.K.T.D.; Andrade, R.L.B.D.; Figueiredo, M.B.G.D.A.; Nunes, M.A.P.; Jesus, C.V.F.; Lima, S.O. Evolução comparativa e temporal das tendências de mortalidade por Câncer Colorretal em Sergipe e Nordeste no período de 2008 a 2018. BJHR 2020, 3, 9058–9074. Available online: https://www.brazilianjournals.com/index.php/BJHR/article/view/13712/11485 (accessed on 5 July 2024). [CrossRef]
- Morais Neto, J.F.D.; Mendes, L.M.C.; Ferreira Filho, M.A.G.; Mendes, L.C.; Lino, L.A.; Silva, A.P.D.; Matos, L.F.F.; Garcia, J.P.; Madeira, J.P.B.; Delgado, R.L.O. Análise da internação por neoplasia maligna da bexiga no Brasil entre o período de 2011 a agosto de 2022. RSD 2023, 12, e27112240205. Available online: https://rsdjournal.org/index.php/rsd/article/view/40205 (accessed on 4 July 2024). [CrossRef]
- Chakora, E.S. Política Nacional de Atenção Integral à Saúde do Homem. Esc. Anna Nery 2014, 18. Available online: https://www.scielo.br/j/ean/a/YT4pgHZWTmrzVRdmCn8bTLw/?lang=pt&format=pdf (accessed on 4 July 2024).
- Gomes, S.C.; Esperidião, M.A. Acesso dos usuários indígenas aos serviços de saúde de Cuiabá, Mato Grosso, Brasil. Cad. Saúde Pública 2017, 33, 5. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0102-311X2017000505010&lng=pt&tlng=pt (accessed on 4 July 2024). [CrossRef] [PubMed]
- Mourão, T.C.; Curado, M.P.; De Oliveira, R.A.R.; Santana, T.B.M.; Favaretto, R.D.L.; Guimarães, G.C. Epidemiology of Urological Cancers in Brazil: Trends in Mortality Rates Over More Than Two Decades. J. Epidemiol. Glob. Health 2022, 12, 239–247. Available online: https://link.springer.com/10.1007/s44197-022-00042-8 (accessed on 4 July 2024). [CrossRef] [PubMed]
- Tamalunas, A.; Volz, Y.; Schlenker, B.A.; Buchner, A.; Kretschmer, A.; Jokisch, F.; Rodler, S.; Schulz, G.; Eismann, L.; Pfitzinger, P.; et al. Is It Safe to Offer Radical Cystectomy to Patients above 85 Years of Age? A Long-Term Follow-Up in a Single-Center Institution. Urol Int. 2020, 104, 975–981. Available online: https://pubmed.ncbi.nlm.nih.gov/32871580/ (accessed on 14 August 2024). [CrossRef] [PubMed]
- Hsueh, T.Y.; Huang, Y.H.; Chiu, A.W.; Huan, S.K.; Lee, Y.H. Survival analysis in patients with upper urinary tract transitional cell carcinoma: A comparison between open and hand-assisted laparoscopic nephroureterectomy. BJU Int. 2007, 99, 632–636. Available online: https://bjui-journals.onlinelibrary.wiley.com/doi/10.1111/j.1464-410X.2006.06665.x (accessed on 20 August 2024). [CrossRef] [PubMed]
- Saika, T.; Suyama, B.; Murata, T.; Manabe, D.; Kurashige, T.; Nasu, Y.; Tsushima, T.; Kumon, H. Orthotopic neobladder reconstruction in elderly bladder cancer patients. Int. J. Urol. 2008, 8, 533–538. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1442-2042.2001.00367.x?sid=nlm%3Apubmed (accessed on 20 August 2024). [CrossRef] [PubMed]

| Variables | Descriptions | Information Systems Consulted | Collection Period |
|---|---|---|---|
| Dependent | |||
| Age-adjusted atandardized mortality ratio | Rate resulting from the application of crude bladder cancer mortality rates standardized by the world standard population and adjusted by age group (expressed in the number of deaths per 100,000 inhabitants). | SIM | 2000–2022 |
| Independent | |||
| Socioeconomic factors | |||
| Region of residence | Refers to the place of residence according to the territorial division of Brazil with particular characteristics. Categories: North, Northeast, Midwest, Southeast, and South. | SIM | 2000–2022 |
| Race | Refers to the classification of the population according to characteristics related to ethnic and racial origin. Categories: white, black, brown, yellow, and indigenous. | SIM | 2000–2022 |
| Gross domestic product (GDP) per capita | Percentage generated by dividing the GDP by the number of inhabitants in the region and measures how much of the GDP would go to each individual in a country if they all received equal shares. | IDB | 2000–2010 |
| Gini index of per capita household income | A measure of the degree of concentration of the distribution of household income per capita of a given population and in a given geographical space. | IDB | 2000–2012 |
| Access factors and expenditure on public services | |||
| Number of health professionals per inhabitant | The number of health professionals in activity per thousand inhabitants according to categories in a given geographical area in the year considered. | IDB | 2000–2010 |
| Expenditure on public health actions and services as a proportion of the GDP | Percentage of the national GDP that corresponds to federal public spending on health in the year considered. | IDB | 2000–2010 |
| Consultations per inhabitants by region according to year | Number of medical consultations in the Unified Health System per inhabitant per year according to regions. | IDB | 2000–2012 |
| Diagnosis | |||
| Urinary tract ultrasound (0205020054) | The number of noninvasive imaging tests used in the evaluation of the organs of the urinary system (kidneys, ureters, urethra, bladder, and prostate). | SIA | 2008–2022 |
| Lower abdomen CT scan (0206030037) | The number of imaging exams that, through axial cuts, provide a detailed study of different structures of the human body, facilitate localization, detect very small alterations in tissues, organs, and other structures of the lower abdomen, and provide greater precision in clinical and surgical interventions. | SIA | 2008–2022 |
| Lower abdominal and pelvic magnetic resonance imaging (MRI) (0207030022) | The number of magnetic resonance imaging exams that combine several image sequences, including T1-weighted images, T2-weighted images, and diffusion-weighted images (dwi), among others, to provide detailed information about the lower abdomen in order to confirm the suspicion of cancer. | SIA | 2008–2022 |
| Relief bladder catheterization (0301100047) | The number of sterile procedures that consist of inserting a tube into the bladder through the urethra in order to drain urine, which is removed once the purpose of the procedure has been achieved. | SIA | 2008–2022 |
| Delay bladder catheterization (0301100055) | The number of sterile procedures of a sterile catheter in the bladder through the urethra, with the aim of draining urine in situations of bladder incompetence and urinary incontinence. | SIA | 2008–2022 |
| Suprapubic aspiration (0409010359) | The number of procedures where a needle is inserted into the bladder through the anterior abdominal wall—crudely—to access the organ in order to collect or introduce substances for diagnostic or therapeutic purposes or drainage. | SIA | 2008–2022 |
| Cystoscopy and/or ureteroscopy and/or urethroscopy (0209020016) | The number of endoscopic examinations, without cuts, simple, and with low risks, carried out in patients with suspected diseases of the bladder or urethra (urine channel). They can be performed with rigid and flexible apparatus, with or without sedation. | SIA | 2008–2022 |
| Bladder biopsy (0201010062) | The number of procedures in which a tissue sample is removed and referred for analysis to a pathologist, a doctor who specializes in diagnosing diseases by analyzing tissues with a microscope. | SIA | 2008–2022 |
| Treatment | |||
| Cystostomy (0304040070) | The number of urinary diversion surgeries, which make it possible to drain the bladder by the supra-pubic route, in situations where the urethra does not allow its emptying. | SIA | 2008–2022 |
| Chemotherapy for bladder cancer (0304040070) | The number of chemotherapies consisting of the use of anticancer drugs to destroy tumor cells in the bladder. | SIA | 2008–2022 |
| Endoscopic resection of bladder lesions (0409010383) | The number of surgeries in which the device is introduced through the urethra, under anesthesia, to inspect the bladder and remove the tumor in fragments for biopsy. | SIH | 2008–2022 |
| Partial cystectomy (040910022) | The number of surgeries of high complexity used to remove malignant tumors in the affected organ, when the function and structure of the organ can be partially preserved. | SIH | 2008–2022 |
| Total cystectomy (0409010030) | The number of highly complex surgeries used to remove the organ affected by malignant tumors. | SIH | 2008–2022 |
| Cystoenteroplasty (0409010057) | The number of bladder reconstruction surgeries with bowel loops after bladder cancer surgery. | SIH | 2008–2022 |
| Cystectomy with a shunt in only 1 time in oncology (0416010024) | The number of complete or partial resections of the bladder affected by malignant tumors, with or without ureteroenterostomy, in the case of a simple shunt with or without nephrostomy or ureterostomy. | SIH | 2008–2022 |
| Brazil n = 78,015 (%) | North n = 2261 (%) | Northeast n = 12,392 (%) | Southeast n = 42,126 (%) | South n = 16,627 (%) | Midwest n = 4609 (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||||
| Male | 53,658 | 68.78 | 1569 | 69.40 | 8147 | 65.75 | 28,925 | 68.66 | 11,884 | 71.47 | 3133 | 67.98 |
| Female | 24,350 | 31.21 | 692 | 30.60 | 4245 | 24.25 | 13,194 | 31.32 | 4743 | 28.53 | 1476 | 32.02 |
| Unknown | 7 | 0.008 | 0 | 0.00 | 0 | 0.00 | 7 | 0.02 | 0 | 0.00 | 0 | 0.00 |
| Race | ||||||||||||
| White | 53,382 | 68.42 | 717 | 31.71 | 4334 | 34.97 | 31,010 | 73.61 | 14,783 | 88.90 | 2538 | 55.06 |
| Black | 3975 | 5.09 | 103 | 4.55 | 899 | 7.25 | 2286 | 5.42 | 442 | 2.65 | 245 | 5.31 |
| Yellow | 582 | 0.74 | 10 | 0.44 | 32 | 0.25 | 438 | 1.03 | 71 | 0.42 | 31 | 0.67 |
| Brown | 16,497 | 21.14 | 1350 | 59.70 | 6280 | 50.67 | 6499 | 15.42 | 772 | 4.64 | 1596 | 34.62 |
| Indigenous | 62 | 0.07 | 11 | 0.48 | 17 | 0.13 | 13 | 0.03 | 7 | 0.04 | 14 | 0.30 |
| Unknown | 3517 | 4.50 | 70 | 3.09 | 830 | 6.69 | 1880 | 4.46 | 552 | 3.31 | 185 | 4.01 |
| Age (years) | ||||||||||||
| ≤29 | 214 | 0.27 | 24 | 1.06 | 58 | 0.46 | 82 | 0.19 | 29 | 0.17 | 21 | 0.45 |
| 30 to 39 | 501 | 0.64 | 31 | 1.37 | 143 | 1.15 | 205 | 0.48 | 84 | 0.50 | 38 | 0.82 |
| 40 to 49 | 2084 | 2.67 | 109 | 4.82 | 455 | 3.67 | 958 | 2.27 | 412 | 2.47 | 150 | 3.25 |
| 50 to 59 | 7221 | 9.25 | 271 | 11.98 | 1224 | 9.87 | 3733 | 8.86 | 1546 | 9.29 | 450 | 9.76 |
| 60 to 69 | 16,603 | 21.28 | 483 | 21.36 | 2553 | 20.59 | 9029 | 21.43 | 3568 | 21.45 | 970 | 21.04 |
| ≥70 | 51,371 | 65.84 | 1342 | 59.35 | 7953 | 64.16 | 28,109 | 66.72 | 10,987 | 66.07 | 2980 | 64.65 |
| Unknown | 21 | 0.02 | 1 | 0.04 | 9 | 0.07 | 10 | 0.02 | 1 | 0.006 | 0 | 0.00 |
| North | Northeast | Southeast | South | Midwest | Brazil | ||
|---|---|---|---|---|---|---|---|
| Gross domestic product (GDP) per capita | β | −0.110 | 0.357 | −0.735 | −0.907 | −0.296 | −0.532 |
| t | −0.333 | 1.148 | −3.248 | −3.618 | −0.929 | −1.884 | |
| p | 0.747 | 0.280 | 0.010 * | 0.007 * | 0.377 | 0.092 | |
| Gini index | β | −0.079 | −0.434 | −0.141 | −0.361 | −0.343 | −0.400 |
| t | −0.222 | −1.363 | −0.545 | −1.440 | −0.951 | −1.306 | |
| p | 0.830 | 0.210 | 0.601 | 0.188 | 0.369 | 0.228 |
| North | Northeast | Southeast | South | Midwest | Brazil | ||
|---|---|---|---|---|---|---|---|
| Health services | |||||||
| Number of health professionals per inhabitant | β | 0.026 | 0.585 | −0.682 | −0.087 | −0.237 | - |
| t | 0.075 | 0.807 | −13.208 | −0.327 | −0.510 | - | |
| p | 0.942 | 0.446 | <0.0001 * | 0.753 | 0.626 | - | |
| Expenses for public health actions and services as a proportion of GDP | β | −0.445 | 0.575 | −0.652 | −0.034 | 0.479 | −0.055 |
| t | −1.287 | 2.110 | −12.635 | −0.123 | 1.123 | −0.131 | |
| p | 0.234 | 0.064 | <0.0001 * | 0.906 | 0.298 | 0.899 | |
| Consultations per inhabitant by region | β | −0.565 | −0.024 | −0.577 | −0.722 | −0.207 | −0.355 |
| t | −0.685 | −0.047 | −1.278 | −2.733 | −0.539 | −0.852 | |
| p | 0.515 | 0.964 | 0.242 | 0.029 * | 0.607 | 0.419 | |
| Diagnostic | |||||||
| Urinary tract ultrasound | β | 0.053 | - | −0.578 | - | 0.391 | −0.154 |
| t | 0.200 | - | −1.137 | - | 0.876 | 0.416 | |
| p | 0.845 | - | 0.285 | - | 0.415 | 0.687 | |
| Tomography of the lower abdomen | β | - | 0.341 | 0.338 | - | −0.874 | - |
| t | - | 1.864 | 0.657 | - | −1.404 | - | |
| p | - | 0.092 | 0.528 | - | 0.210 | - | |
| MRI of pelvis and pelvis/lower abdomen | β | 0.107 | - | - | −0.273 | - | −0.479 |
| t | 0.604 | - | - | −1.135 | - | −1.411 | |
| p | 0.559 | - | - | 0.283 | - | 0.192 | |
| Bladder puncture/aspiration | β | - | −0.643 | −0.526 | −0.980 | −0.516 | −2.134 |
| t | - | −2.930 | −0.820 | −4.170 | −0.923 | −5.933 | |
| p | - | 0.015 * | 0.433 | 0.002 * | 0.391 | <0.0001 * | |
| Cystoscopy and/or ureteroscopy and/or urethroscopy | β | −0.563 | 0.066 | 0.604 | −0.016 | 1.517 | 0.247 |
| t | −2.448 | 0.377 | 1.241 | −0.087 | 2.504 | 0.776 | |
| p | 0.034 * | 0.714 | 0.246 | 0.933 | 0.046 * | 0.457 | |
| Bladder biopsy | β | −0.366 | −0.065 | 0.691 | 0.064 | −1.777 | 1.266 |
| t | −1.265 | −0.390 | 1.203 | 0.359 | −2.988 | 4.567 | |
| p | 0.235 | 0.705 | 0.260 | 0.727 | 0.024 * | 0.001 * |
| North | Northeast | Southeast | South | Midwest | Brazil | ||
|---|---|---|---|---|---|---|---|
| Cystostomy | β | −1.223 | −0.349 | 0.080 | −0.106 | −0.104 | −0.391 |
| t | −6.385 | −0.816 | 0.330 | −0.141 | −0.158 | −0.571 | |
| p | 0.001 * | 0.452 | 0.753 | 0.893 | 0.881 | 0.589 | |
| Chemotherapy for bladder carcinoma | β | - | 0.942 | - | 0.142 | −0.736 | - |
| t | - | 2.329 | - | 0.124 | −1.209 | - | |
| p | - | 0.067 | - | 0.906 | 0.281 | - | |
| Bladder catheterization | β | 0.026 | −0.349 | 0.225 | 0.263 | 0.138 | −0.087 |
| t | 0.199 | −0.816 | 1.639 | 0.465 | 0.444 | −0.217 | |
| p | 0.849 | 0.452 | 0.152 | 0.661 | 0.676 | 0.835 | |
| Endoscopic resection of bladder lesions | β | 0.248 | −0.295 | −0.359 | 0.516 | 0.764 | 0.079 |
| t | 1.797 | −0.751 | −1.452 | 0.513 | 1.452 | 0.174 | |
| p | 0.122 | 0.486 | 0.197 | 0.630 | 0.206 | 0.868 | |
| Partial cystectomy | β | 0.026 | 0.209 | 0.101 | 0.171 | 0.294 | −0.345 |
| t | 0.127 | 0.768 | 0.462 | 0.191 | 0.844 | −1.190 | |
| p | 0.903 | 0.477 | 0.660 | 0.856 | 0.437 | 0.279 | |
| Total cystectomy | β | 0.646 | 0.032 | −1.215 | 0.505 | −0.027 | −0.520 |
| t | 3.612 | 0.118 | −4.948 | 0.720 | −0.097 | −0.765 | |
| p | 0.011 * | 0.911 | 0.003 * | 0.504 | 0.927 | 0.473 | |
| Cystoenteroplasty | β | 0.386 | 0.200 | 0.015 | −0.250 | 0.537 | 0.057 |
| t | 2.665 | 0.617 | 0.098 | −0.222 | 1.031 | 0.136 | |
| p | 0.037 * | 0.564 | 0.925 | 0.833 | 0.350 | 0.896 | |
| Cystectomy with a single shunt in oncology | β | 0.239 | −0.068 | 0.042 | 0.289 | −0.977 | 0.720 |
| t | 1.615 | −0.211 | 0.251 | 0.328 | −1.644 | 1.647 | |
| p | 0.157 | 0.841 | 0.810 | 0.757 | 0.161 | 0.151 | |
| Total cystectomy with a single shunt in oncology | β | 0.558 | 0.010 | 0.032 | −0.029 | −0.465 | 0.425 |
| t | 4.752 | 0.038 | 0.193 | −0.041 | −1.373 | 1.040 | |
| p | 0.003 * | 0.971 | 0.853 | 0.969 | 0.228 | 0.339 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Melo Neto, J.S.; Miguez, S.F.; Rabelo, A.L.R.; Silva, A.M.d.; Sacramento, D.S.; das Neves, D.B.S.; Rego, I.N.; Garcia, R.L.M.; Galhardo, D.d.R.; Neves, A.L.M.d. Impact of Age, Period, Cohort, Region, Race, and Health Services on Bladder Cancer Mortality in Brazil: A 23-Year Ecological Study. Cancers 2024, 16, 3038. https://doi.org/10.3390/cancers16173038
de Melo Neto JS, Miguez SF, Rabelo ALR, Silva AMd, Sacramento DS, das Neves DBS, Rego IN, Garcia RLM, Galhardo DdR, Neves ALMd. Impact of Age, Period, Cohort, Region, Race, and Health Services on Bladder Cancer Mortality in Brazil: A 23-Year Ecological Study. Cancers. 2024; 16(17):3038. https://doi.org/10.3390/cancers16173038
Chicago/Turabian Stylede Melo Neto, João Simão, Sâmia Feitosa Miguez, Amanda Lia Rebelo Rabelo, Amanda Marinho da Silva, Daniel Souza Sacramento, Dária Barroso Serrão das Neves, Iana Nogueira Rego, Riter Lucas Miranda Garcia, Deizyane dos Reis Galhardo, and André Luiz Machado das Neves. 2024. "Impact of Age, Period, Cohort, Region, Race, and Health Services on Bladder Cancer Mortality in Brazil: A 23-Year Ecological Study" Cancers 16, no. 17: 3038. https://doi.org/10.3390/cancers16173038
APA Stylede Melo Neto, J. S., Miguez, S. F., Rabelo, A. L. R., Silva, A. M. d., Sacramento, D. S., das Neves, D. B. S., Rego, I. N., Garcia, R. L. M., Galhardo, D. d. R., & Neves, A. L. M. d. (2024). Impact of Age, Period, Cohort, Region, Race, and Health Services on Bladder Cancer Mortality in Brazil: A 23-Year Ecological Study. Cancers, 16(17), 3038. https://doi.org/10.3390/cancers16173038






