Simple Summary
Pain is a common symptom that affects individuals with cancer. This study, using data from the National Health Interview Survey, explored how household income relates to chronic pain among cancer survivors. It found that lower-income survivors, those below 200% of the federal poverty level (FPL), were more likely to report chronic pain lasting at least 3 months and pain that significantly limited their daily activities. Compared to higher-income survivors (at least 400% FPL), those with lower incomes had higher odds of experiencing chronic pain and its impact on daily life. Additionally, opioid use for pain management was more common among lower-income survivors, while higher-income survivors tended to use alternative methods like yoga, chiropractic care, and physical therapy. This study emphasizes the need for targeted efforts to address healthcare disparities and improve pain management for all cancer survivors, regardless of their income level.
Abstract
Pain is a prevalent issue among cancer patients, yet its link with socioeconomic status has not been thoroughly examined. This study investigated chronic pain (lasting ≥3 months) and high-impact pain (chronic pain limiting activities) among cancer survivors based on household income relative to the federal poverty level (FPL), using data from the National Health Interview Survey (2019–2020). Of the 4585 participants with a history of solid cancers, 1649 (36.3%) reported chronic pain and 554 (12.6%) reported high-impact chronic pain. After adjustment, participants with incomes < 200% FPL had significantly higher odds of chronic pain (adjusted odds ratio [aOR]: 1.60, 95% CI: 1.25–2.05) and high-impact chronic pain (aOR: 1.73, 95% CI: 1.09–2.74) compared to those with incomes ≥ 400% FPL. Opioid use for chronic pain was most prevalent among those with incomes < 200% FPL (28.3%) compared to those with 200–399% (21.3%) and ≥400% (19.0%). Higher-income participants reported greater use of alternative pain management methods such as yoga (50.5%), chiropractic care (44.8%), and physical therapy (44.3%). This study highlights the association between household income and chronic pain outcomes among cancer survivors, emphasizing the necessity for targeted interventions to mitigate healthcare access disparities and improve pain management for all individuals affected by cancer.
1. Introduction
In recent decades, the decline in cancer-related mortality rates has resulted in a substantial increase in the number of long-term cancer survivors []. This increase can be attributed to multi-level factors, including an aging population, advances in cancer screening, and the development of newer, more effective treatments that have reduced cancer-specific mortality []. With this expanding population of cancer survivors comes a pressing need to comprehensively understand the long-term side effects they experience. Among these effects, chronic pain has emerged as a particularly prevalent symptom, profoundly impacting their quality of life [,,]. While chronic pain affects an estimated 21% of United States (U.S.) adults, it afflicts 35% of cancer survivors []. Furthermore, cancer survivors also experience pain-related disability at a disproportionately higher rate, with 13% reporting high-impact chronic pain (i.e., pain that limits life and work activities) compared to just 7% of the general U.S. adult population []. As such, understanding factors that contribute to the disproportionate burden of chronic pain among cancer survivors is of paramount importance.
Socioeconomic status (SES) stands as a crucial determinant for both cancer incidence and chronic pain [], yet the intricate interplay of SES with chronic pain among cancer survivors remains insufficiently explored. Cancer survivors constitute a unique cohort grappling with multifaceted challenges and responsibilities, which often precipitate financial strains [,,]. These may stem from mounting medical costs, cancer-induced disabilities, familial caregiving duties, and the imperative of maintaining professional commitments. The added burden of financial toxicity significantly compounds the complexities of managing chronic cancer pain, particularly among those with inadequate insurance coverage and economically disadvantaged backgrounds. Low SES not only heightens vulnerability to chronic pain but may also shape approaches to pain management [].
The objective of this study was to investigate the relationship between SES and chronic pain among a nationally representative sample of U.S. adult cancer survivors. Specifically, we evaluated the prevalence of chronic pain and high-impact chronic pain and the utilization of pain management methods among cancer survivors, stratified by household income relative to the federal poverty level (FPL).
2. Materials and Methods
2.1. Study Design and Population
This cross-sectional study analyzed combined data from the 2019–2020 National Health Interview Survey (NHIS) to explore the association between household income and chronic pain among solid cancer survivors. The NHIS data comprise annual, cross-sectional household interview national surveys that utilize complex, multi-stage sampling methodologies to generate estimates regarding the noninstitutionalized population of the United States []. The NHIS interviews are conducted using computer-assisted personal interviewing. Face-to-face interviews are conducted in respondents’ homes, but follow-ups to complete interviews may be conducted over the telephone. A comprehensive explanation of the NHIS sampling technique and the procedures for data collection can be accessed via the following link: https://www.cdc.gov/nchs/nhis/index.htm (accessed on 31 January 2024).
This study utilized information derived from the Sample Adult files, including participants who were aged 18 years and older []. All NHIS data featured in this research are based on self-reported diagnosis of solid cancer and participant responses regarding chronic pain and pain management methods. Participants with the following characteristics were excluded from the analysis: (1) participants with no history of solid cancers and (2) those with missing or invalid data (e.g., refused, not ascertained, do not know) on chronic pain. The NHIS is a valuable resource for chronic pain surveillance in the U.S., with questions specifically designed to align with the International Association for the Study of Pain’s definitions of chronic and high-impact chronic pain []. A flow chart illustrating the inclusion and exclusion criteria for participants can be seen in Figure 1. The dataset comprises sampling weights designed to adjust for the cluster design, non-response, and intentional oversampling of specific subgroups. These weights can be integrated into statistical analyses, ensuring that weighted statistics accurately reflect the characteristics of the entire U.S. population []. This study was exempt from Institutional Review Board review because the study utilized de-identified, publicly available datasets.
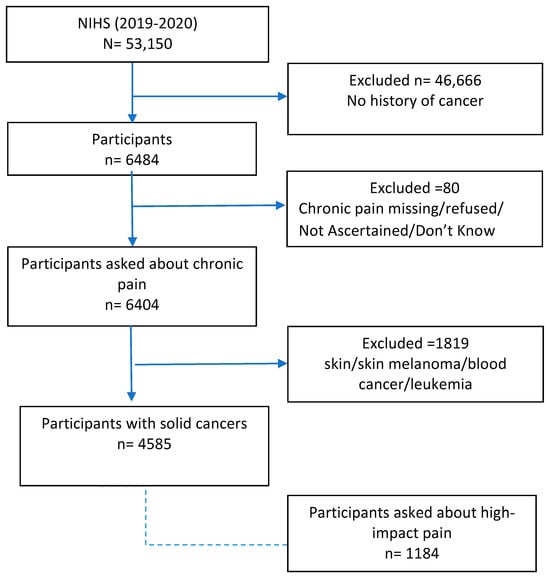
Figure 1.
Participant flow chart.
2.2. Diagnoses of Solid Cancers
Participants were asked, “Have you ever been told by a doctor or other health professional that you had cancer or a malignancy of any kind?” Those who responded with an affirmative response were also asked, “What kind of cancer was it?” and up to three different cancers were recorded. Patients with a history of skin and hematological malignancies, such as leukemia, lymphoma, or myeloma, were excluded [,].
2.3. Ratio of Household Income to Federal Poverty Level
The household income-to-poverty ratio data were obtained from the NHIS, and are calculated as total household income divided by the family’s corresponding federal poverty level multiplied by 100. The FPL is issued annually by the Department of Health and Human Services and is determined by family size. The household income relative to the FPL is used to determine eligibility for federal programs and benefits, including Medicaid. Additional information regarding the income-to-poverty ratio data can be obtained from NHIS documentation []. For this analysis, household income was categorized as less than 200% FPL, 200% to 399% FPL, and 400% or greater FPL [].
2.4. Outcomes
2.4.1. Chronic Pain
The the primary outcome of this study was the presence of chronic pain. Information on pain was obtained through responses to the following questions: “In the past 3 months, how often did you have pain? Would you say never, some days, most days, or every day?” and “Over the past 3 months, how often did pain limit your life or work activities? Would you say never, some days, most days, or every day?” Chronic pain was defined as pain on most days or every day in the past 3 months vs. no pain on most days or every day in the past 3 months []. High-impact pain was assessed among the participants who had reported chronic pain. High-impact chronic pain (secondary outcome) was defined as pain that significantly restricts life or work activities on most days or every day vs. no pain that significantly restricts life or work activities on most days or every day [].
2.4.2. Pain Management Techniques Other than Over-the-Counter Medications
Opioids
Participants were asked about opioid use if they reported the use of prescription medication []. The participants’ use of prescription opioids was determined by inquiring whether they had taken any opioid pain relievers prescribed by a doctor, dentist, or other healthcare professional within the previous 12 months. As per the NHIS criteria, prescription opioid medications included hydrocodone, Vicodin, Norco, Lortab, oxycodone, OxyContin, Percocet, and Percodan. Participants were instructed not to include over-the-counter pain relievers such as aspirin, Tylenol, Advil, or Aleve. If in doubt, the participant was asked to tell the interviewer about the drug, and the interviewer would then determine whether it was an opioid or not. Those who reported usage were further queried regarding their opioid consumption within the past 3 months and also about acute use for short-term pain []. The variables were categorized as yes vs. no.
Alternative Pain Management Methods
Participants who had pain for at least some days were asked about other pain management techniques: (1) physical, occupational, or rehabilitative therapy (yes vs. no); (2) spinal manipulation or other forms of chiropractic care (yes vs. no); (3) talk therapies such as cognitive–behavioral therapy (yes vs. no); (4) yoga or tai chi (yes vs. no); (5) exercise for pain (yes vs. no); (6) massage for pain (yes vs. no); and (7) meditation, guided imagery, or other relaxation (yes vs. no) [].
2.5. Covariates
To address potential confounding between household income and chronic pain, we included the following self-reported sociodemographic, behavioral, and clinical characteristics as covariates: age (categorized as 18–44, 45–64, or ≥65 years); sex (female or male); race/ethnicity (NH (non-Hispanic) White, NH Black, Hispanic, or NH Asian or other); marital status (married/living with a partner or not married); education (less than high school, high school or GED, some college, or more); covered by insurance (yes vs. no); urbanicity (large central metro, large fringe metro, medium and small metro, non-metropolitan); smoking (never, currently, or formerly); BMI (underweight, healthy weight, overweight, or obese); hypertension (yes vs. no); diabetes (yes vs. no); arthritis (yes vs. no); depression (yes vs. no); anxiety (yes vs. no); survey year (2019 or 2020); number of cancers (1 vs. >1), and type of cancer (breast, lung, colorectal, prostate, head and neck (mouth, tongue, lip, larynx, trachea, throat, or pharynx), melanoma, bladder, gynecologic (ovarian, uterine, or cervical), hepatobiliary (liver, hepatocellular, bile duct, or pancreatic), and digestive (stomach or esophageal)).
2.6. Statistical Analysis
Data were analyzed using SAS 9.4® (SAS Institute, Inc.; Cary, NC, USA). All analyses utilized the appropriate NHIS sample weights, stratum, and primary sampling units to address oversampling, non-response, and non-coverage issues, ensuring nationally representative estimates were obtained. Sample characteristics are presented overall and by income-to-poverty level as number of participants and weighted percentages.
To explore the relationship between household income and chronic pain and high-impact pain, weighted logistic regression models were applied using PROC SURVEYLOGISTIC (https://support.sas.com/documentation/onlinedoc/stat/142/surveylogistic.pdf (accessed on 31 January 2024)) to estimate the odds ratio (OR) and corresponding 95% confidence intervals (CIs). Our dataset involved complex survey data with sampling weights, stratification, and clustering. To account for these design elements and ensure that our estimates are representative of the population, we selected weighted logistic regression models. This approach allows for the incorporation of survey weights, providing robust standard errors and accurate confidence intervals necessary for valid inferences about the association between household income and chronic pain. Model 1 adjusted for sex, age, education, race/ethnicity, marital status, BMI, smoking, insurance, and urbanicity. Model 2 additionally included adjustments for hypertension, diabetes, depression, anxiety, and arthritis. The >400% FPL group was designated as the reference level. Parallel analyses were conducted with high-impact pain as the outcome variable. Trend tests for FPL were performed by treating FPL as an ordinal variable within the multivariable logistic regression model. Two-sided p values < 0.05 were considered statistically significant in this study.
3. Results
3.1. Study Participants and Design
We conducted a cross-sectional analysis involving 4585 participants with a history of solid cancers, representing an estimated 17,052,286 U.S. adults aged 18 or older (Figure 1). Table 1 presents weighted descriptive statistics for sample characteristics across income categories. Of the analytic sample of participants, 1333 (29.6%) had household incomes of <200% FPL, 1372 (29.3%) had 200–399% FPL, and 1880 (41.1%) had ≥400% FPL. The majority of the participants were ≥65 years old (57.7%), female (58.9%), NH White (82.9%), married/living with a partner (65.2%), never smokers (51.6%), had some college or more (61.7%), and had hypertension (54.9%). Participants in the <200% FPL category tended to be female (66.1%), not married (53.2%), obese (39.1%), and exhibited higher comorbidities than higher-income groups. Missing data are reported in Table S1.

Table 1.
Participant characteristics of the study population by federal poverty level, NHIS 2019–2020.
3.2. Household Income and Chronic Pain
A total of 1649 participants (36.3%) with a history of cancer reported experiencing chronic pain. Among them, 502 participants (43.5%) reported high-impact chronic pain. Notably, the prevalence of chronic pain (Figure 2a) and high-impact chronic pain (Figure 2b) demonstrated a dose–response effect with a decreasing income-to-poverty ratio. We performed multivariable logistic regression to estimate the association between income-to-poverty ratio and chronic pain, adjusting for covariates (Table 2). In the adjusted Model 1, participants with household incomes < 200% FPL (aOR = 2.00, 95% CI: 159, 2.52) and 200–399% FPL (aOR = 1.38, 95% CI: 1.13, 1.69) had significantly higher odds of chronic pain compared to those with ≥400% FPL (Model 1). However, when additionally adjusting for comorbidities (Model 2), only <200% FPL remained significantly associated with chronic pain (aOR = 1.60, 95% CI: 1·25, 2·05). Among those with chronic pain, a household income <200% FPL was significantly associated with high-impact chronic pain compared to ≥400% FPL. Fully adjusted Model 2 results (Table S3) reveal that chronic pain is significantly associated with age, obesity, arthritis, diabetes, depression, and anxiety, while high-impact pain is significantly associated with hypertension and anxiety.
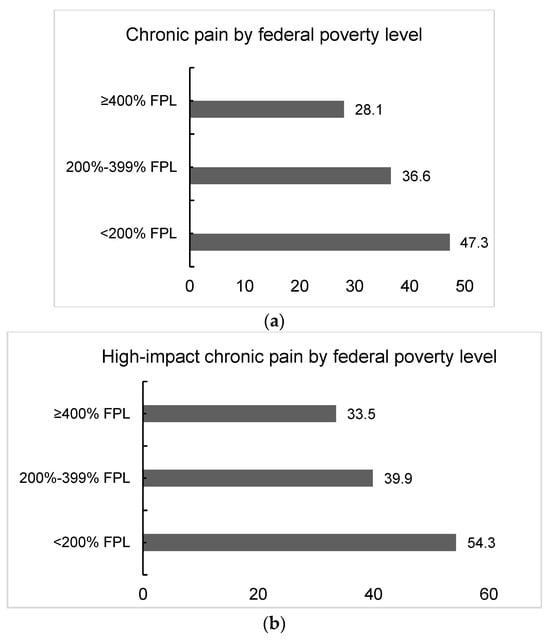
Figure 2.
(a) Distribution of chronic pain by federal poverty level (n = 4585). (b) Distribution of high-impact pain with physical limitations by federal poverty level (n = 1184).

Table 2.
Association between federal poverty level and chronic pain.
3.3. Opioid Use
We assessed the prevalence of opioid and non-opioid pain management methods among cancer survivors (Table 3 and Table S2). Across the 12-month, 3-month, and acute time frames, opioid usage was more common among individuals in the <200% FPL category, followed by the 200–399% category and >400% category, exhibiting a dose–response pattern (Table 3 and Table S2).

Table 3.
Prevalence of chronic pain-relieving methods adopted by cancer survivors by federal poverty level.
3.4. Non-Opioid Pain Management
Thirty-one percent of participants relied solely on non-opioid management strategies to manage their pain. The most prevalent non-opioid pain management technique utilized by cancer survivors for chronic pain was “Other methods for pain” (excluding physical therapy, chiropractic care, talk therapy, cognitive–behavioral therapy, yoga, tai chi, qi gong, massage, and meditation), employed by 19.7% of participants. Among survivors experiencing high-impact chronic pain, 35% relied on “Other methods” for pain relief. However, the prevalence of these techniques varied across the income categories. Following “other” pain relief methods, cancer survivors in the ≥400% FPL category reported the use of physical therapy (12.5%), massage (11.9%), meditation (9.1%), chiropractic care (6.8%), yoga, tai chi, or qi gong (6.8%), and talk therapy (1.3%) (see Table 3). In contrast, cancer survivors in the <200% FPL category showed a preference for meditation (11.9%) and talk therapy (2.1%). The prevalence of pain-relieving methods for high-impact pain was comparable to that for chronic pain (Table S2).
4. Discussion
In this cross-sectional study of a nationally representative sample of U.S. adults aged 18 years or older with a history of solid cancers, household income emerged as a significant social determinant influencing chronic pain. Participants with household incomes <200% FPL exhibited nearly twice the prevalence of chronic pain compared to those with ≥400% FPL. Our findings reveal a clear dose–response relationship between household income and chronic pain, with notably higher prevalence observed among individuals from lower-income households. This trend persisted when examining high-impact chronic pain as the outcome, underscoring the enduring disparities in pain experience linked to socioeconomic status.
4.1. Disparity in Cancer Pain
Our research aligns with extensive prior literature documenting the association between cancer and chronic pain [,,]. However, to our knowledge, there are no prior nationally representative studies that have specifically evaluated the role of socioeconomic status in chronic pain and high-impact chronic pain among cancer survivors, as well as its association with pain management strategies. Chronic pain is best understood as a dynamic interaction of biological, psychological, and social factors [], highlighting the intricate nature of its manifestation and management. Individuals in lower-SES groups encounter barriers to accessing healthcare services [,], including adequate pain management [] and treatment options []. In this study, we found that 47.3% of adult cancer survivors with household income < 200% FPL experienced chronic pain, and 28.3% of them reported using opioids for pain management within the last 12 months. In contrast, only 19.0% of cancer survivors at >400% of the FPL used opioids. Similar differences were noted in the acute use of opioids, too. The differences in opioid use across income levels highlight complex factors influencing pain management choices [,,]. The lower use of opioids at higher income levels can partly be explained by better access to healthcare information and resources. Higher-income individuals are more likely to be aware of newer guidelines aimed at reducing opioid prescriptions due to the significant rise in non-medical opioid use, the stigma associated with opioid addiction, and related problems []. This increased awareness and access to information can lead to a reduction in opioid use among higher-income individuals compared to lower-income groups [,]. Developing guidelines akin to the World Health Organization’s (WHO) three-step ladder for opioid use in individuals undergoing active cancer treatment could prove beneficial [,,].
4.2. Socioeconomic Disparities in Cancer Pain Management
Financial constraints may limit access to non-opioid therapies or medical procedures that could alleviate chronic pain [,,,]. In our study, we found greater use of opioids in the lowest-income group, which suggests that recent practice guidelines that emphasize the use of non-opioid approaches may be unequally applied across socioeconomic statuses []. Notably, there were no substantial differences among the income levels for managing pain with physical therapy and meditation as the most common non-opioid management methods. These findings indicate the need for strategies to ensure safe and effective therapeutic approaches for chronic pain that are accessible to individuals across the entire socioeconomic spectrum.
Addressing the association between SES and chronic pain in cancer survivors requires comprehensive strategies aimed at reducing socioeconomic inequalities in access to healthcare services. Evidence suggests that the management of cancer pain has improved, but undertreatment remains common and impacts quality of life [,]. Policies aimed at expanding healthcare coverage, reducing out-of-pocket costs for essential medical services, and increasing funding for pain management programs in underserved communities are crucial steps in addressing this issue. Furthermore, initiatives aimed at enhancing outcomes in vulnerable cancer populations through education, employment opportunities, and community-based interventions can mitigate socioeconomic determinants of chronic pain and improve overall health outcomes. Our study has some notable strengths and limitations. This study is strengthened by using data from the NHIS, a large-scale survey of a nationally representative sample of the U.S. noninstitutionalized adult population []. The NHIS is a principal source for monitoring the health of the U.S. population. Additionally, the NHIS question about chronic pain was specifically designed based on the definition of pain by the International Association for the Study of Pain. Furthermore, by using the income-to-poverty ratio rather than solely an income measure, we provide a more thorough analysis of socioeconomic status, as it takes into account the household size.
4.3. Limitations
Our study has several limitations. The cancer diagnosis in the NHIS relies on self-reporting, which may result in some under-reporting. Some individuals may not be aware of their cancer and may not have been diagnosed yet, which is particularly relevant as individuals of lower SES tend to be diagnosed at more advanced cancer stages than their higher-SES counterparts []. Consequently, our analysis may have excluded individuals with undiagnosed cancers, potentially leading to an underestimation of the effect of lower income on chronic pain, although this may not have significantly impacted the results regarding lower-income households. We could not examine variations across different cancer types and cancer characteristics, such as treatment modalities or time elapsed since diagnosis, due to limitations of the available data. Our study primarily documented prevalent chronic pain and adjusted for common comorbidities associated with pain. However, a more detailed recognition of pain types could improve the interpretation of our findings and their implications for pain management in cancer care.
Additionally, the self-reported information in the NHIS data may limit the generalizability of our results to all populations. Despite NHIS weighting procedures designed to mitigate coverage and non-response bias, some measurement biases may still persist. Finally, a more comprehensive analysis of social determinants of health, such as food insecurity or lack of housing or transportation, may help identify potential targets for intervention.
5. Conclusions
Our study highlights the significant inverse relationship between household income and chronic pain prevalence, underscoring the need for targeted interventions to address socioeconomic disparities in chronic pain among cancer survivors. Additionally, longitudinal studies could provide insights into how changes in socioeconomic status impact chronic pain and quality of life over time. Addressing disparities is essential to improve pain management and overall quality of life for cancer survivors, particularly those from lower-income households.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/cancers16162847/s1, Table S1: Frequency of missing variables; Table S2: Prevalence of high-impact pain-relieving methods adopted by cancer survivors by Federal Poverty Level (FPL); Table S3: Multivariable logistic regression model for chronic pain and Federal Poverty Level (FPL) using the National Health Interview Survey (NHIS), 2019–2020.
Author Contributions
Conceptualization, N.V. and S.D.K.; methodology, N.V. and S.D.K.; software, S.D.K.; formal analysis, S.D.K. and N.V.; investigation, S.D.K.; resources, S.D.K. and D.B.; data curation, J.A.T., N.V. and S.D.K.; writing—original draft preparation, N.V. and S.D.K.; writing—review and editing, N.V., J.A.T., D.B., R.B.F. and S.D.K.; visualization, S.D.K.; supervision, D.B. and R.B.F.; project administration, S.D.K.; funding acquisition, D.B. All authors have read and agreed to the published version of the manuscript.
Funding
Authors Karanth and Braithwaite were supported by the National Cancer Institute (R01CA284646). Tamargo was supported by National Institute on Aging (T32AG049673).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data utilized for this study are available at the following link: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm (accessed on 31 January 2024).
Acknowledgments
We acknowledge and thank members of the National Center for Health Statistics of the Centers for Disease Control and Prevention, as well as the participants who contributed time and data to the National Health Interview Survey.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- Kline, R.M.; Arora, N.K.; Bradley, C.J.; Brauer, E.R.; Graves, D.L.; Lunsford, N.B.; McCabe, M.S.; Nasso, S.F.; Nekhlyudov, L.; Rowland, J.H. Long-term survivorship care after cancer treatment-summary of a 2017 National Cancer Policy Forum Workshop. JNCI J. Natl. Cancer Inst. 2018, 110, 1300–1310. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L.; Wagner, L.I.; Monahan, P.O.; Daggy, J.; Smith, L.; Cohee, A.; Ziner, K.W.; Haase, J.E.; Miller, K.D.; Pradhan, K. Comparison of younger and older breast cancer survivors and age-matched controls on specific and overall quality of life domains. Cancer 2014, 120, 2237–2246. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Theobald, D.; Wu, J.; Loza, J.K.; Carpenter, J.S.; Tu, W. The association of depression and pain with health-related quality of life, disability, and health care use in cancer patients. J. Pain Symptom Manag. 2010, 40, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Green, C.R.; Hart-Johnson, T.; Loeffler, D.R. Cancer-related chronic pain: Examining quality of life in diverse cancer survivors. Cancer 2011, 117, 1994–2003. [Google Scholar] [CrossRef] [PubMed]
- Rikard, S.M.; Strahan, A.E.; Schmit, K.M.; Guy, G.P., Jr. Chronic Pain Among Adults—United States, 2019–2021. MMWR Morb. Mortal. Wkly. Rep. 2023, 72, 379–385. [Google Scholar] [CrossRef]
- Ham, O.-K.; Chee, W.; Im, E.-O. The influence of social structure on cancer pain and quality of life. West. J. Nurs. Res. 2017, 39, 1547–1566. [Google Scholar] [CrossRef]
- Bestvina, C.M.; Zullig, L.L.; Rushing, C.; Chino, F.; Samsa, G.P.; Altomare, I.; Tulsky, J.; Ubel, P.; Schrag, D.; Nicolla, J. Patient-oncologist cost communication, financial distress, and medication adherence. J. Oncol. Pract. 2014, 10, 162–167. [Google Scholar] [CrossRef]
- Fenn, K.M.; Evans, S.B.; McCorkle, R.; DiGiovanna, M.P.; Pusztai, L.; Sanft, T.; Hofstatter, E.W.; Killelea, B.K.; Knobf, M.T.; Lannin, D.R. Impact of financial burden of cancer on survivors’ quality of life. J. Oncol. Pract. 2014, 10, 332–338. [Google Scholar] [CrossRef]
- Ramsey, S.; Blough, D.; Kirchhoff, A.; Kreizenbeck, K.; Fedorenko, C.; Snell, K.; Newcomb, P.; Hollingworth, W.; Overstreet, K. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 2013, 32, 1143–1152. [Google Scholar] [CrossRef]
- Grol-Prokopczyk, H. Use and opinions of prescription opioids among older American adults: Sociodemographic predictors. J. Gerontol. Ser. B 2019, 74, 1009–1019. [Google Scholar] [CrossRef] [PubMed]
- NHIS Data, Questionnaires and Related Documentation; Centers for Disease Control & Prevention: Atlanta, GA, USA, 2017.
- Duca, L.M.; Helmick, C.G.; Barbour, K.E.; Nahin, R.L.; Von Korff, M.; Murphy, L.B.; Theis, K.; Guglielmo, D.; Dahlhamer, J.; Porter, L.; et al. A Review of Potential National Chronic Pain Surveillance Systems in the United States. J. Pain 2022, 23, 1492–1509. [Google Scholar] [CrossRef] [PubMed]
- Pfeffermann, D. The use of sampling weights for survey data analysis. Stat. Methods Med. Res. 1996, 5, 239–261. [Google Scholar] [CrossRef]
- Jones, K.F.; Osazuwa-Peters, O.L.; Des Marais, A.; Merlin, J.S.; Check, D.K. Substance Use Disorders Among US Adult Cancer Survivors. JAMA Oncol. 2024, 10, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Haenen, V.; Evenepoel, M.; De Baerdemaecker, T.; Meeus, M.; Devoogdt, N.; Morlion, B.; Dams, L.; Van Dijck, S.; Van der Gucht, E.; De Vrieze, T.; et al. Pain prevalence and characteristics in survivors of solid cancers: A systematic review and meta-analysis. Support. Care Cancer 2022, 31, 85. [Google Scholar] [CrossRef] [PubMed]
- Prior HHS Poverty Guidelines and Federal Register References; U.S. Department of Health and Human Services: Washington, DC, USA, 2007. Available online: http://aspe.hhs.gov/poverty/figures-fed-reg.shtml (accessed on 16 April 2024).
- Prior HHS Poverty Guidelines and Federal Register References. Available online: https://aspe.hhs.gov/topics/poverty-economic-mobility/poverty-guidelines/prior-hhs-poverty-guidelines-federal-register-references (accessed on 31 January 2024).
- Cox-Martin, E.; Anderson-Mellies, A.; Borges, V.; Bradley, C. Chronic pain, health-related quality of life, and employment in working-age cancer survivors. J. Cancer Surviv. 2020, 14, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Jiang, C.; Wang, H.; Wang, Q.; Luo, Y.; Sidlow, R.; Han, X. Prevalence of chronic pain and high-impact chronic pain in cancer survivors in the United States. JAMA Oncol. 2019, 5, 1224–1226. [Google Scholar] [CrossRef]
- Sanford, N.N.; Sher, D.J.; Butler, S.S.; Xu, X.; Ahn, C.; Aizer, A.A.; Mahal, B.A. Prevalence of chronic pain among cancer survivors in the United States, 2010–2017. Cancer 2019, 125, 4310–4318. [Google Scholar] [CrossRef] [PubMed]
- Fillingim, R.B. Individual differences in pain: Understanding the mosaic that makes pain personal. Pain 2017, 158 (Suppl. S1), S11–S18. [Google Scholar] [CrossRef]
- Bennett, M.; Paice, J.A.; Wallace, M. Pain and opioids in cancer care: Benefits, risks, and alternatives. Am. Soc. Clin. Oncol. Educ. Book 2017, 37, 705–713. [Google Scholar] [CrossRef]
- Hertz, S.H.; Throckmorton, D.C. US Food and Drug Administration Efforts to Support Pain Management and Opioid Access to Patients with Cancer. J. Oncol. Prat. 2019, 15, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Fereydooni, S.; Lorenz, K.; Azarfar, A.; Luckett, T.; Phillips, J.L.; Becker, W.; Giannitrapani, K. Identifying provider, patient and practice factors that shape long-term opioid prescribing for cancer pain: A qualitative study of American and Australian providers. BMJ Open 2024, 14, e082033. [Google Scholar] [CrossRef] [PubMed]
- Im, E.-O.; Chee, W.; Guevara, E.; Liu, Y.; Lim, H.-J.; Tsai, H.-M.; Clark, M.; Bender, M.; Kim, K.S.; Kim, Y.H. Gender and ethnic differences in cancer pain experience: A multiethnic survey in the United States. Nurs. Res. 2007, 56, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Vitzthum, L.K.; Nalawade, V.; Riviere, P.; Sumner, W.; Nelson, T.; Mell, L.K.; Furnish, T.; Rose, B.; Martínez, M.E.; Murphy, J.D. Racial, ethnic, and socioeconomic discrepancies in opioid prescriptions among older patients with cancer. JCO Oncol. Pract. 2021, 17, e703–e713. [Google Scholar] [CrossRef] [PubMed]
- Cheetham, A.; Picco, L.; Barnett, A.; Lubman, D.I.; Nielsen, S. The Impact of Stigma on People with Opioid Use Disorder, Opioid Treatment, and Policy. Subst. Abus. Rehabil. 2022, 13, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef]
- Häuser, W.; Schug, S.; Furlan, A.D. The opioid epidemic and national guidelines for opioid therapy for chronic noncancer pain: A perspective from different continents. Pain Rep. 2017, 2, e599. [Google Scholar] [CrossRef] [PubMed]
- Fallon, M.; Dierberger, K.; Leng, M.; Hall, P.S.; Allende, S.; Sabar, R.; Verastegui, E.; Gordon, D.; Grant, L.; Lee, R.; et al. An international, open-label, randomised trial comparing a two-step approach versus the standard three-step approach of the WHO analgesic ladder in patients with cancer. Ann. Oncol. 2022, 33, 1296–1303. [Google Scholar] [CrossRef] [PubMed]
- Maltoni, M.; Scarpi, E.; Modonesi, C.; Passardi, A.; Calpona, S.; Turriziani, A.; Speranza, R.; Tassinari, D.; Magnani, P.; Saccani, D. A validation study of the WHO analgesic ladder: A two-step vs three-step strategy. Support. Care Cancer 2005, 13, 888–894. [Google Scholar] [CrossRef]
- Zech, D.F.; Grond, S.; Lynch, J.; Hertel, D.; Lehmann, K.A. Validation of World Health Organization Guidelines for cancer pain relief: A 10-year prospective study. Pain 1995, 63, 65–76. [Google Scholar] [CrossRef]
- Al-Ghabeesh, S.H.; Bashayreh, I.H.; Saifan, A.R.; Rayan, A.; Alshraifeen, A.A. Barriers to effective pain management in cancer patients from the perspective of patients and family caregivers: A qualitative study. Pain Manag. Nurs. 2020, 21, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Halpern, M.T.; de Moor, J.S.; Yabroff, K.R. Impact of pain on employment and financial outcomes among cancer survivors. J. Clin. Oncol. 2022, 40, 24. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, C.; Harding, R.; Teo, I.; Ozdemir, S.; Koh, G.C.; Neo, P.; Lee, L.H.; Kanesvaran, R.; Finkelstein, E.; COMPASS Study team. Financial difficulties are associated with greater total pain and suffering among patients with advanced cancer: Results from the COMPASS study. Support. Care Cancer 2020, 28, 3781–3789. [Google Scholar] [CrossRef] [PubMed]
- Richard, P.; Patel, N.; Lu, Y.C.; Walker, R.; Younis, M. The Financial Burden of Cancer on Families in the United States. Int. J. Environ. Res. Public Health 2021, 18, 3790. [Google Scholar] [CrossRef]
- Greco, M.T.; Roberto, A.; Corli, O.; Deandrea, S.; Bandieri, E.; Cavuto, S.; Apolone, G. Quality of cancer pain management: An update of a systematic review of undertreatment of patients with cancer. J. Clin. Oncol. 2014, 32, 4149–4154. [Google Scholar] [CrossRef] [PubMed]
- Poço Gonçalves, J.; Veiga, D.; Araújo, A. Chronic pain, functionality and quality of life in cancer survivors. Br. J. Pain 2021, 15, 401–410. [Google Scholar] [CrossRef]
- Woods, L.M.; Rachet, B.; Coleman, M. Origins of socio-economic inequalities in cancer survival: A review. Ann. Oncol. 2006, 17, 5–19. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).