Progression of Femoral Osteolytic Metastases after Intramedullary Nailing and Subsequent Salvage Techniques
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Data Collection
2.3. Technique of Antegrade Femoral Nailing
2.4. Technique of Salvage Percutaneous Radiofrequency Ablation and Cementoplasty
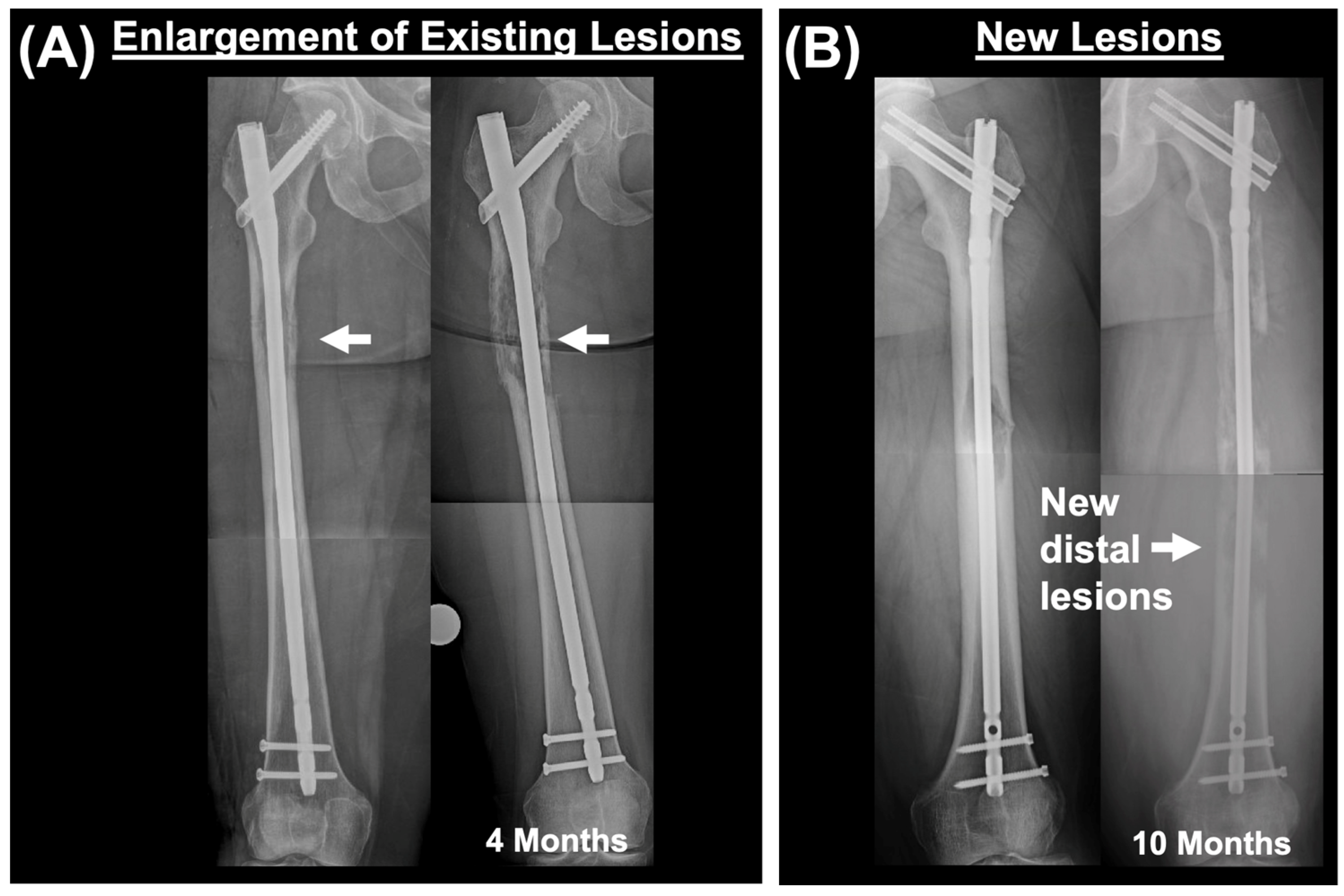
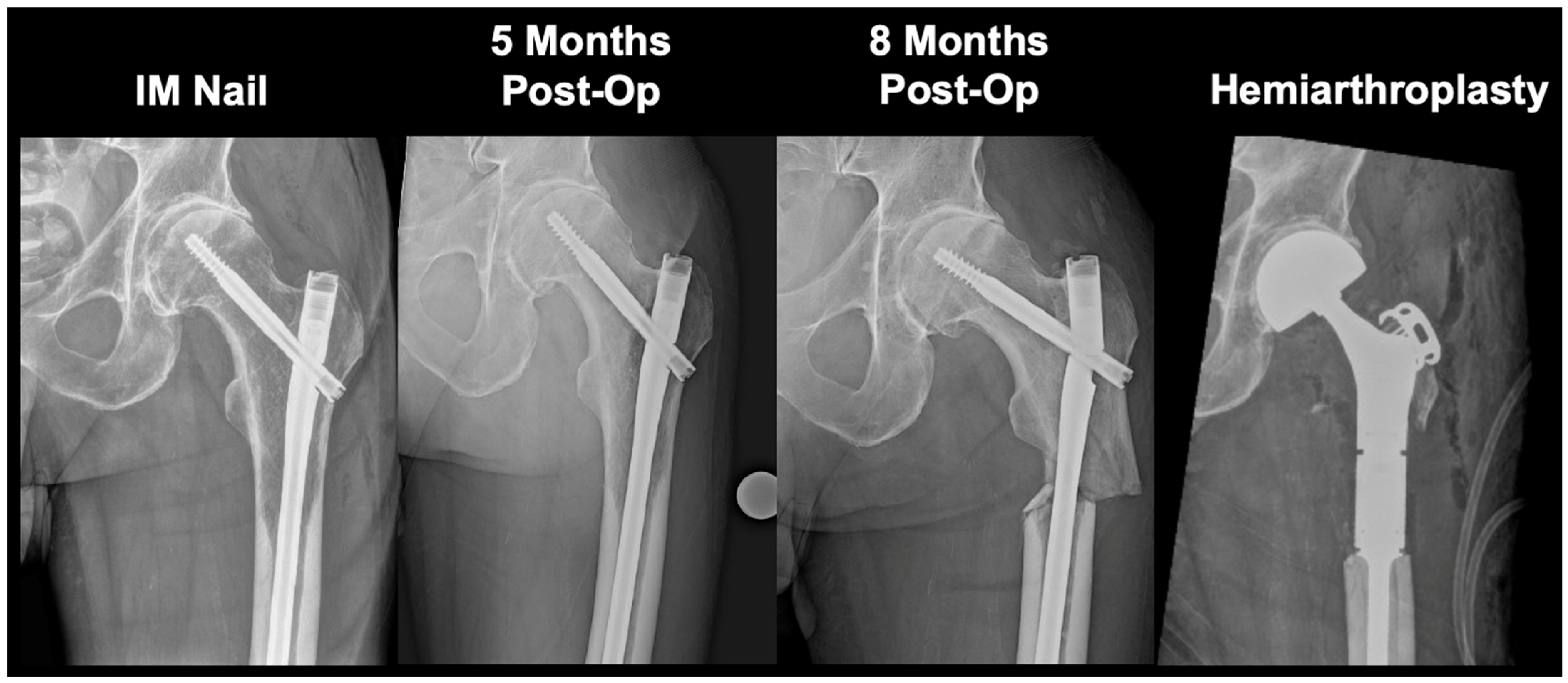
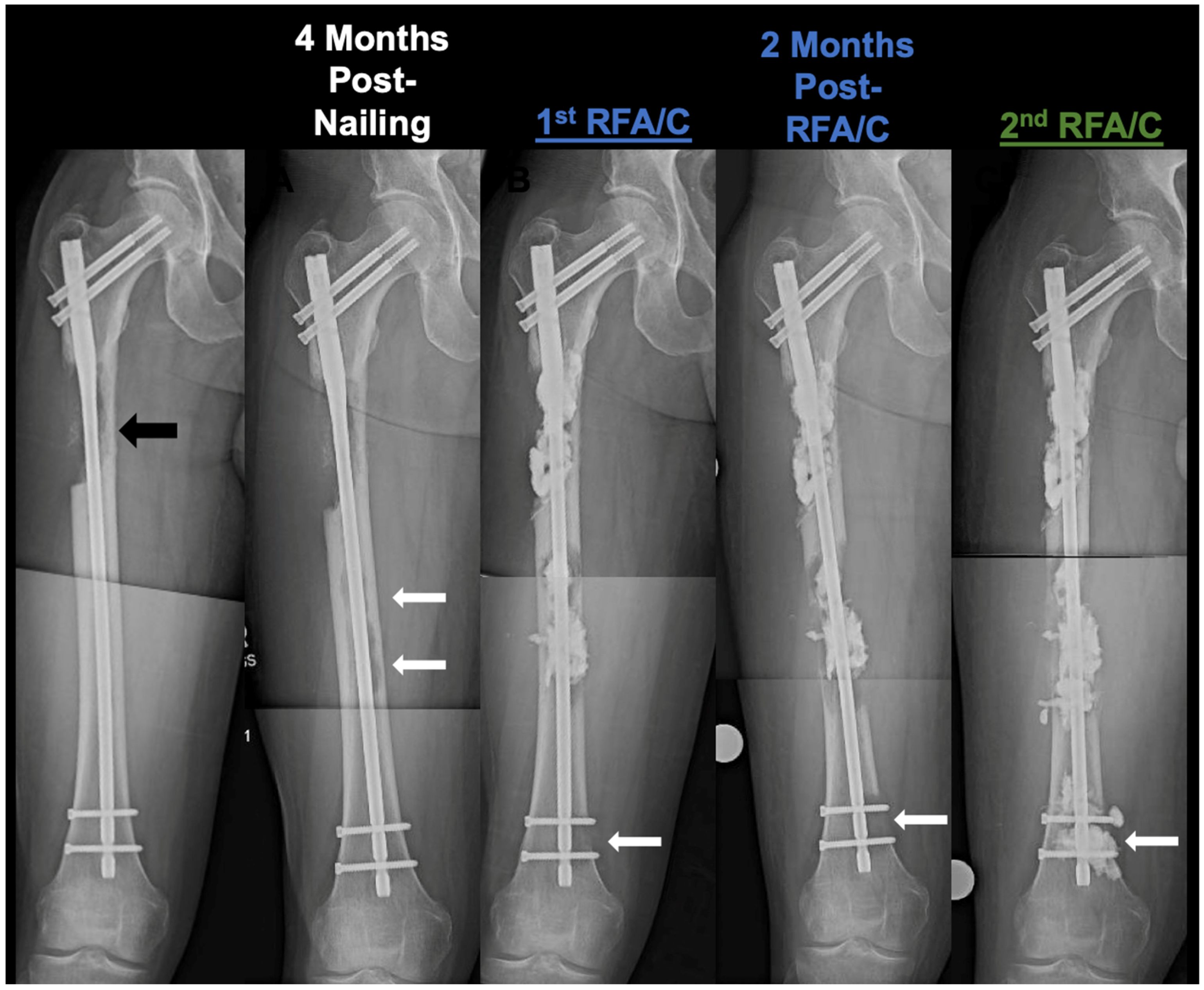
3. Results
3.1. Summary of 113 Intramedullary Nailing Patients
3.2. Percutaneous Salvage Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tanaka, T.; Imanishi, J.; Charoenlap, C.; Choong, P.F. Intramedullary nailing has sufficient durability for metastatic femoral fractures. World J. Surg. Oncol. 2016, 14, 80. [Google Scholar] [CrossRef] [PubMed]
- Breuer, E.; Hebeisen, M.; Schneider, M.A.; Roth, L.; Pauli, C.; Frischer-Ordu, K.; Eden, J.; Pache, B.; Steffen, T.; Hübner, M.; et al. Site of Recurrence and Survival After Surgery for Colorectal Peritoneal Metastasis. J. Natl. Cancer Inst. 2021, 113, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Guzik, G. Oncological and functional results after surgical treatment of bone metastases at the proximal femur. BMC Surg. 2018, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.A.; Jensen, H.; Virgilsen, L.F.; Falborg, A.Z.; Møller, H.; Vedsted, P. Time from incident primary cancer until recurrence or second primary cancer: Risk factors and impact in general practice. Eur. J. Cancer Care 2019, 28, e13123. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Friedlaender, G.; Lindskog, D.; Latich, I.; Lee, F.Y. Comparison of Percutaneous Interventional Ablation-Osteoplasty-Reinforcement-Internal Fixation (AORIF), Long Intramedullary Nailing, and Hemiarthroplasty for the Treatment of Focal Metastatic Osteolytic Lesions in the Femoral Head and Neck. Cardiovasc. Interv. Radiol. 2023, 46, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Toombs, C.; Conway, D.; Munger, A.; Alder, K.; Latich, I.; Lee, F. Ablation, Osteoplasty, Reinforcement, and Internal Fixation for Percutaneous Endoskeletal Reconstruction of Periacetabular and Other Periarticular Osteolytic Metastases. Instr. Course Lect. 2021, 70, 503–514. [Google Scholar] [PubMed]
- Back, J.; Nguyen, M.N.; Li, L.; Lee, S.; Lee, I.; Chen, F.; Gillinov, L.; Chung, Y.-H.; Alder, K.D.; Kwon, H.-K.; et al. Inflammatory conversion of quiescent osteoblasts by metastatic breast cancer cells through pERK1/2 aggravates cancer-induced bone destruction. Bone Res. 2021, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.J.; Soni, E.E.; Gibbs, C.P.; Scarborough, M.T. Intramedullary nails for long bone metastases: Why do they fail? Orthopedics 2011, 34. [Google Scholar] [CrossRef] [PubMed]
- Arpornsuksant, P.; Morris, C.D.; Forsberg, J.A.; Levin, A.S. What Factors Are Associated With Local Metastatic Lesion Progression After Intramedullary Nail Stabilization? Clin. Orthop. Relat. Res. 2022, 480, 932–945. [Google Scholar] [CrossRef]
- Sebghati, J.; Khalili, P.; Tsagkozis, P. Surgical treatment of metastatic bone disease of the distal extremities. World J. Orthop. 2021, 12, 743–750. [Google Scholar] [CrossRef]
- Lee, F.Y.; Latich, I.; Toombs, C.; Mungur, A.; Conway, D.; Alder, K.; Ibe, I.; Lindskog, D.; Friedlaender, G. Minimally Invasive Image-Guided Ablation, Osteoplasty, Reinforcement, and Internal Fixation (AORIF) for Osteolytic Lesions in the Pelvis and Periarticular Regions of Weight-Bearing Bones. J. Vasc. Interv. Radiol. 2020, 31, 649–658.e641. [Google Scholar] [CrossRef] [PubMed]
- Dussik, C.M.; Toombs, C.; Alder, K.D.; Yu, K.E.; Berson, E.R.; Ibe, I.K.; Li, F.; Lindskog, D.M.; Friedlaender, G.E.; Latich, I.; et al. Percutaneous Ablation, Osteoplasty, Reinforcement, and Internal Fixation for Pain and Ambulatory Function in Periacetabular Osteolytic Malignancies. Radiology 2023, 307, e221401. [Google Scholar] [CrossRef] [PubMed]
- Bartelstein, M.K.; Yerramilli, D.; Christ, A.B.; Kenan, S.; Ogura, K.; Fujiwara, T.; Fabbri, N.; Healey, J.H. Postradiation Fractures after Combined Modality Treatment in Extremity Soft Tissue Sarcomas. Sarcoma 2021, 2021, 8877567. [Google Scholar] [CrossRef] [PubMed]
- Willeumier, J.J.; Kaynak, M.; van der Zwaal, P.; Meylaerts, S.A.G.; Mathijssen, N.M.C.; Jutte, P.C.; Tsagozis, P.; Wedin, R.; van de Sande, M.A.J.; Fiocco, M.; et al. What Factors Are Associated With Implant Breakage and Revision After Intramedullary Nailing for Femoral Metastases? Clin. Orthop. Relat. Res. 2018, 476, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Alvi, H.M.; Damron, T.A. Prophylactic stabilization for bone metastases, myeloma, or lymphoma: Do we need to protect the entire bone? Clin. Orthop. Relat. Res. 2013, 471, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Epstein-Peterson, Z.D.; Sullivan, A.; Krishnan, M.; Chen, J.T.; Ferrone, M.; Ready, J.; Baldini, E.H.; Balboni, T. Postoperative radiation therapy for osseous metastasis: Outcomes and predictors of local failure. Pract. Radiat. Oncol. 2015, 5, e531–e536. [Google Scholar] [CrossRef] [PubMed]
- Narod, S.A. Disappearing breast cancers. Curr. Oncol. 2012, 19, 59–60. [Google Scholar] [CrossRef]
- Ghomashchi, S.; Whyne, C.M.; Chinnery, T.; Habach, F.; Akens, M.K. Impact of radiofrequency ablation (RFA) on bone quality in a murine model of bone metastases. PLoS ONE 2021, 16, e0256076. [Google Scholar] [CrossRef]
- Thanos, L.; Mylona, S.; Galani, P.; Tzavoulis, D.; Kalioras, V.; Tanteles, S.; Pomoni, M. Radiofrequency ablation of osseous metastases for the palliation of pain. Skelet. Radiol. 2008, 37, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, S.S.; Birdwell, R.L.; Ikeda, D.M.; Daniel, B.L.; Nowels, K.W.; Dirbas, F.M.; Griffey, S.M. Radiofrequency Ablation of Breast Cancer: First Report of an Emerging Technology. Arch. Surg. 1999, 134, 1064–1068. [Google Scholar] [CrossRef]
- Cazzato, R.L.; Palussière, J.; Auloge, P.; Rousseau, C.; Koch, G.; Dalili, D.; Buy, X.; Garnon, J.; De Marini, P.; Gangi, A. Complications Following Percutaneous Image-guided Radiofrequency Ablation of Bone Tumors: A 10-year Dual-Center Experience. Radiology 2020, 296, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Govaert, K.M.; van Kessel, C.S.; Lolkema, M.; Ruers, T.J.; Borel Rinkes, I.H. Does Radiofrequency Ablation Add to Chemotherapy for Unresectable Liver Metastases? Curr. Color. Cancer Rep. 2012, 8, 130–137. [Google Scholar] [CrossRef]
- Piccioli, A.; Rossi, B.; Scaramuzzo, L.; Spinelli, M.S.; Yang, Z.; Maccauro, G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014, 45, 412–417. [Google Scholar] [CrossRef]
- Wang, K.; Wang, C.; Jiang, H.; Zhang, Y.; Lin, W.; Mo, J.; Jin, C. Combination of Ablation and Immunotherapy for Hepatocellular Carcinoma: Where We Are and Where to Go. Front. Immunol. 2021, 12, 792781. [Google Scholar] [CrossRef] [PubMed]
- Senders, Z.J.; Martin, R.C.G., 2nd. Intratumoral Immunotherapy and Tumor Ablation: A Local Approach with Broad Potential. Cancers 2022, 14, 1754. [Google Scholar] [CrossRef]
- Friedman, M.V.; Hillen, T.J.; Wessell, D.E.; Hildebolt, C.F.; Jennings, J.W. Hip chondrolysis and femoral head osteonecrosis: A complication of periacetabular cryoablation. J. Vasc. Interv. Radiol. 2014, 25, 1580–1588. [Google Scholar] [CrossRef] [PubMed]
- Marcove, R.C.; Weis, L.D.; Vaghaiwalla, M.R.; Pearson, R.; Huvos, A.G. Cryosurgery in the treatment of giant cell tumors of bone. A report of 52 consecutive cases. Cancer 1978, 41, 957–969. [Google Scholar] [CrossRef]
- Zhao, W.; Peng, Z.-H.; Chen, J.-Z.; Hu, J.-H.; Huang, J.-Q.; Jiang, Y.-N.; Luo, G.; Yi, G.-F.; Wang, H.; Jin, S.; et al. Thermal effect of percutaneous radiofrequency ablation with a clustered electrode for vertebral tumors: In vitro and vivo experiments and clinical application. J. Bone Oncol. 2018, 12, 69–77. [Google Scholar] [CrossRef]
- Park, J.W.; Lim, H.J.; Kang, H.G.; Kim, J.H.; Kim, H.S. Percutaneous Cementoplasty for the Pelvis in Bone Metastasis: 12-Year Experience. Ann. Surg. Oncol. 2022, 29, 1413–1422. [Google Scholar] [CrossRef]
- Hoffmann, R.T.; Jakobs, T.F.; Trumm, C.; Weber, C.; Helmberger, T.K.; Reiser, M.F. Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J. Vasc. Interv. Radiol. 2008, 19, 419–425. [Google Scholar] [CrossRef]
- McMahon, S.; Hawdon, G.; Bare, J.; Sim, Y.; Bertollo, N.; Walsh, W.R. Thermal necrosis and pmma—A cause for concern? Orthop. Proc. 2012, 94-B, 64. [Google Scholar] [CrossRef]
- Stoops, K.; Brown, J.M.; Santoni, B.; Groundland, J. Thermal properties of polymethyl methacrylate vary depending on brand and type. J. Orthop. Res. 2022, 41, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Karpinski, R.; Szabelski, J.; Krakowski, P.; Jonak, J.; Falkowicz, K.; Jojczuk, M.; Nogalski, A.; Przekora, A. Effect of various admixtures on selected mechanical properties of medium viscosity bone cements: Part 2—Hydroxyapatite. Compos. Struct. 2024, 343, 118308. [Google Scholar] [CrossRef]
- Moon, B.S.; Dunbar, D.J.; Lin, P.P.; Satcher, R.L.; Bird, J.E.; Lewis, V.O. Is It Appropriate to Treat Sarcoma Metastases With Intramedullary Nailing? Clin. Orthop. Relat. Res. 2017, 475, 212. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Zhang, H.; Xu, H.R.; Liu, J.Z.; Pan, J.; Zhai, H.Z.; Lu, C.Y.; Zhao, X.; Chen, Y.Q.; Zhou, L.L.; et al. Analgesia of percutaneous thermal ablation plus cementoplasty for cancer bone metastases. J. Bone Oncol. 2019, 19, 100266. [Google Scholar] [CrossRef]
- Umer, M.; Mohib, Y.; Atif, M.; Nazim, M. Skeletal metastasis in renal cell carcinoma: A review. Ann. Med. Surg. 2018, 27, 9–16. [Google Scholar] [CrossRef]




| Age (median (IQR); years) | 66.8 [16.4] |
| Follow-Up (median (IQR); months) | 6.0 [14.5] |
| Total Patients (n) | 113 |
| Unilateral (n) | 111 (98.2%) |
| Bilateral (n) | 2 (1.8%) |
| Total Procedures (n) | 115 |
| Right (n) | 59 (51.3%) |
| Left (n) | 56 (48.7%) |
| Sex | |
| Female (n) | 61 (54.0%) |
| Male (n) | 52 (46.0%) |
| Primary Malignancy | |
| Breast (n) | 20 (17.7%) |
| Lung (n) | 20 (17.7%) |
| Renal Cell Carcinoma (n) | 19 (16.8%) |
| Multiple Myeloma (n) | 17 (15.0%) |
| Prostate (n) | 9 (8.0%) |
| Bladder (n) | 8 (7.1%) |
| Melanoma (n) | 5 (4.4%) |
| Leukemia/Lymphoma (n) | 3 (2.7%) |
| Head and Neck (n) | 3 (2.7%) |
| Other (n) | 11 (9.7%) |
| Procedure Characteristics | |
| Procedure Duration (median (IQR)) | 70.0 [29.0] min |
| Estimated Blood Loss (median (IQR)) | 150.0 [100.0] mL |
| Transfusions (n) | 8 (7.0%) |
| Infection (n) | 0 (0.0%) |
| 30-Day Complications (n) | 11 (9.6%) |
| Length of Stay (median (IQR)) | 2.0 [3.0] days |
| Surgical Outcome | |
| Combined Pain and Ambulatory Score (Pre-Op) (median (IQR)) | 6.0 [2.0] |
| Combined Pain and Ambulatory Score (Post-Op) (median (IQR)) | 7.0 [1.0] |
| Chemotherapy (Pre-Op) (n) | 72 (63.7%) |
| Chemotherapy (Post-Op) (n) | 93 (82.3%) |
| Radiation Therapy (Pre-Op) (n) | 18 (15.9%) |
| Radiation Therapy (Post-Op) (n) | 54 (47.8%) |
| Patient | Age | Primary | Largest Lesion Diameter | Radiation | Chemo | Bone Modifying Agents | Cortical Bone Loss | Mirel’s Score | Cancer Progression | Salvage Type | Time to Salvage | Surgeries after Salvage |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 68F | Multiple Myeloma | 10.3 cm | Post-Op | Post-Op | Post-Op | Yes | 11 | Enlargement; nail breakage | Open (resection + prosthesis) | 30 months | No |
| 2 * | 65M | RCC | 7.7 cm | Pre-Op | Both | Both | Yes | 12 | Enlargement; nail breakage | Open (Hemi- arthroplasty) | 20 months | No |
| 3 | 65F | RCC | 5.9 cm | Post-Op | Post-Op | Post-Op | Yes | 12 | Enlargement; nail breakage | Open (Hemi-arthroplasty) | 4 months | No |
| 4 * | 83F | Lung | 3.1 cm | None | Pre-Op | None | Yes | 12 | Enlargement | Deceased (3 months) | NA | No |
| 5 * | 68F | Breast | 14.7 cm | Post-Op | Both | Both | Yes | 11 | Enlargement | Deceased (56 months) | NA | No |
| 6 | 72F | Breast | 5.9 cm | Post-Op | Both | Pre-Op | Yes | 12 | Enlargement | Patient Declined (new chemo) | NA | No |
| 7 * | 76F | Lymphoma | 3.9 cm | Post-Op | Post-Op | Post-Op | Yes | 11 | Enlargement | Deceased (5 months) | NA | No |
| 8 * | 60F | Lung | 8.4 cm | Pre-Op | Both | None | Yes | 11 | Enlargement | Deceased (8 months) | NA | No |
| 9 * | 60M | Bladder | 4.9 cm | Post-Op | Pre-Op | Post-Op | Yes | 11 | Enlargement | Deceased (2 months) | NA | No |
| 10 * | 65F | Multiple Myeloma | 5.6 cm | Post-Op | Both | Both | Yes | 12 | Enlargement; new distal lesion | Percutaneous | 21 months | No |
| 11 * | 63M | RCC | 5.1 cm | None | Both | Post-Op | Yes | 12 | Enlargement | Percutaneous | 4 months | No |
| 12 * | 47M | Thyroid | 7.5 cm | Pre-Op | Post-Op | None | Yes | 11 | Enlargement; new distal lesion; soft tissue extension | Percutaneous | 9 months | No |
| 13 * | 43M | RCC | 11.8 cm | Post-Op | Post-Op | None | Yes | 12 | Enlargement; new distal lesion | Percutaneous | 31 months | Open (plate) |
| 14 * | 37F | melanoma | 6.0 cm | Post-Op | Post-Op | Post-Op | Yes | 11 | Enlargement | Percutaneous | 4 months | No |
| 15 | 61F | bladder | 7.0 cm | Post-Op | Both | None | Yes | 12 | Enlargement | Percutaneous | 32 months | Open (prosthesis) |
| 16 * | 62M | RCC | 6.0 cm | Post-Op | Both | None | Yes | 11 | Enlargement | Percutaneous | 9 months | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, W.; Latich, I.; Lindskog, D.; Friedlaender, G.; Lee, F.Y. Progression of Femoral Osteolytic Metastases after Intramedullary Nailing and Subsequent Salvage Techniques. Cancers 2024, 16, 2812. https://doi.org/10.3390/cancers16162812
Jiang W, Latich I, Lindskog D, Friedlaender G, Lee FY. Progression of Femoral Osteolytic Metastases after Intramedullary Nailing and Subsequent Salvage Techniques. Cancers. 2024; 16(16):2812. https://doi.org/10.3390/cancers16162812
Chicago/Turabian StyleJiang, Will, Igor Latich, Dieter Lindskog, Gary Friedlaender, and Francis Y. Lee. 2024. "Progression of Femoral Osteolytic Metastases after Intramedullary Nailing and Subsequent Salvage Techniques" Cancers 16, no. 16: 2812. https://doi.org/10.3390/cancers16162812
APA StyleJiang, W., Latich, I., Lindskog, D., Friedlaender, G., & Lee, F. Y. (2024). Progression of Femoral Osteolytic Metastases after Intramedullary Nailing and Subsequent Salvage Techniques. Cancers, 16(16), 2812. https://doi.org/10.3390/cancers16162812





