Antibiotics Significantly Decrease the Survival of Head and Neck Carcinoma Patients with Immunotherapy: A Real-World Analysis of More Than 3000 Cases
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
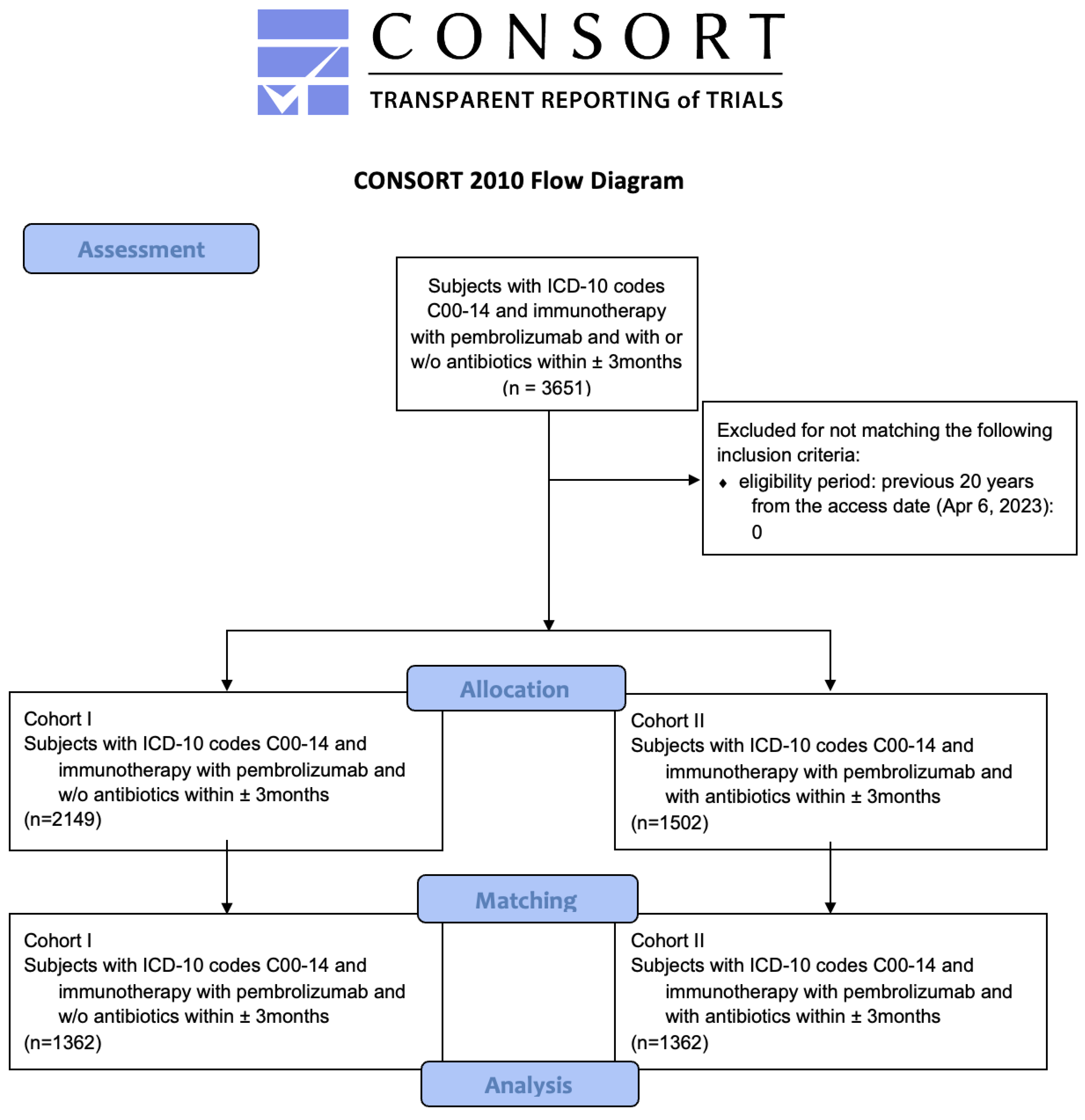
2.1. Data Acquisition, Allocation and Matching
2.2. Data Analysis
3. Results
3.1. Assessment, Allocation and Matching
3.2. Survival Analysis
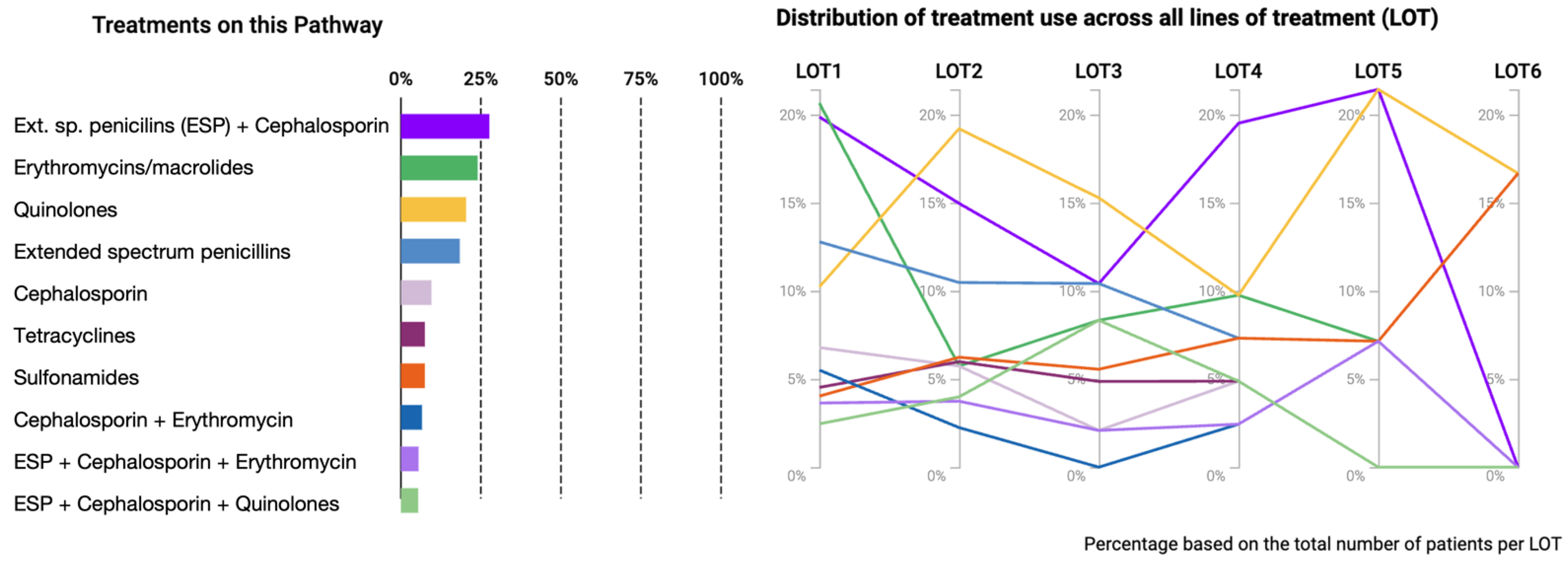
3.3. Treatment Pathways
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HCO | heath care organization |
| HPV | human papillomavirus |
| ICD-10 | International Classification of Diseases 10 |
| OR | odds ratio |
| HR | hazard ratio |
| HNSCC | head and neck squamous cell carcinoma |
| RR | risk ratio |
| UICC | Union Internationale Contre le Cancer |
| WHO | World Health Organization |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Parmar, K.; Mohamed, A.; Vaish, E.; Thawani, R.; Cetnar, J.; Thein, K. Immunotherapy in head and neck squamous cell carcinoma: An updated review. Cancer Treat. Res. Commun. 2022, 33, 100649. [Google Scholar] [CrossRef] [PubMed]
- Burtness, B.; Harrington, K.J.; Greil, R.; Soulières, D.; Tahara, M.; de Castro, G., Jr.; Psyrri, A.; Basté, N.; Neupane, P.; Bratland, A.; et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): A randomised, open-label, phase 3 study. Lancet 2019, 394, 1915–1928. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.E.W.; Soulières, D.; Le Tourneau, C.; Dinis, J.; Licitra, L.; Ahn, M.-J.; Soria, A.; Machiels, J.-P.; Mach, N.; Mehra, R.; et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): A randomised, open-label, phase 3 study. Lancet 2019, 393, 156–167. [Google Scholar] [CrossRef]
- Ferris, R.L.; Blumenschein, G., Jr.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Harrington, K.; Kasper, S.; Vokes, E.E.; Even, C.; et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N. Engl. J. Med. 2016, 375, 1856–1867. [Google Scholar] [CrossRef] [PubMed]
- Borcoman, E.; Marret, G.; Le Tourneau, C. Paradigm Change in First-Line Treatment of Recurrent and/or Metastatic Head and Neck Squamous Cell Carcinoma. Cancers 2021, 13, 2573. [Google Scholar] [CrossRef]
- Sahu, M.; Suryawanshi, H. Immunotherapy: The future of cancer treatment. J. Oral Maxillofac. Pathol. 2021, 25, 371. [Google Scholar]
- Harrington, K.J.; Burtness, B.; Greil, R.; Soulières, D.; Tahara, M.; de Castro, G.; Psyrri, A.; Brana, I.; Basté, N.; Neupane, P.; et al. Pembrolizumab With or Without Chemotherapy in Recurrent or Metastatic Head and Neck Squamous Cell Car-cinoma: Updated Results of the Phase III KEYNOTE-048 Study. J. Clin. Oncol. 2023, 41, 790–802. [Google Scholar] [CrossRef]
- Singh, P.; McDonald, L.; Waldenberger, D.; Welslau, M.; Heyde, E.; Gauler, T.; Dietz, A. Pooled analysis of nivolumab treatment in patients with recurrent/metastatic squamous cell carcinoma of the head and neck in the United States and Germany. Head Neck 2021, 43, 3540–3551. [Google Scholar] [CrossRef]
- Hirsch, L.; Zitvogel, L.; Eggermont, A.; Marabelle, A. PD-Loma: A cancer entity with a shared sensitivity to the PD-1/PD-L1 pathway blockade. Br. J. Cancer 2019, 120, 3–5. [Google Scholar] [CrossRef]
- De Roest, R.H.; Mes, S.W.; Poell, J.B.; Brink, A.; Van De Wiel, M.A.; Bloemena, E.; Thai, E.; Poli, T.; Leemans, C.R.; Brakenhoff, R.H. Molecular Characterization of Locally Relapsed Head and Neck Cancer after Concomitant Chemoradiotherapy. Clin. Cancer Res. 2019, 25, 7256–7265. [Google Scholar] [CrossRef] [PubMed]
- Weber, P.; Künstner, A.; Hess, J.; Unger, K.; Marschner, S.; Idel, C.; Ribbat-Idel, J.; Baumeister, P.; Gires, O.; Walz, C.; et al. Therapy-Related Transcriptional Subtypes in Matched Primary and Recurrent Head and Neck Cancer. Clin. Cancer Res. 2022, 28, 1038–1052. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, J.D.; Hanna, G.J.; Jo, V.Y.; Rawal, B.; Chen, Y.H.; Catalano, P.S.; Lako, A.; Ciantra, Z.; Weirather, J.L.; Criscitiello, S.; et al. Neoadjuvant Nivolumab or Nivolumab Plus Ipilimumab in Untreated Oral Cavity Squamous Cell Carcinoma: A Phase 2 Open-Label Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1563–1570. [Google Scholar] [CrossRef] [PubMed]
- Uppaluri, R.; Campbell, K.M.; Egloff, A.M.; Zolkind, P.; Skidmore, Z.L.; Nussenbaum, B.; Paniello, R.C.; Rich, J.T.; Jackson, R.; Pipkorn, P.; et al. Neoadjuvant and Adjuvant Pembrolizumab in Resectable Locally Advanced, Human Papillomavirus-Unrelated Head and Neck Cancer: A Multicenter, Phase 2 Trial. Clin. Cancer Res. 2020, 26, 5140–5152. [Google Scholar] [CrossRef] [PubMed]
- Vos, J.L.; Elbers, J.B.W.; Krijgsman, O.; Traets, J.J.H.; Qiao, X.; van der Leun, A.M.; Lubeck, Y.; Seignette, I.M.; Smit, L.A.; Willems, S.M.; et al. Neoadjuvant immunotherapy with nivolumab and ipilimumab induces major pathological responses in patients with head and neck squamous cell carcinoma. Nat. Commun. 2021, 12, 7348. [Google Scholar] [CrossRef]
- Routy, B.; le Chatelier, E.; DeRosa, L.; Duong, C.P.M.; Alou, M.T.; Daillère, R.; Fluckiger, A.; Messaoudene, M.; Rauber, C.; Roberti, M.P.; et al. Gut microbiome influences efficacy of PD-1–based immunotherapy against epithelial tumors. Science 2018, 359, 91–97. [Google Scholar] [CrossRef]
- Zitvogel, L.; Ma, Y.; Raoult, D.; Kroemer, G.; Gajewski, T.F. The microbiome in cancer immunotherapy: Diagnostic tools and therapeutic strategies. Science 2018, 359, 1366–1370. [Google Scholar] [CrossRef]
- Dempsey, J.L.; Cui, J.Y. Microbiome Is a Functional Modifier of P450 Drug Metabolism. Curr. Pharmacol. Rep. 2019, 5, 481–490. [Google Scholar] [CrossRef]
- Weersma, R.K.; Zhernakova, A.; Fu, J. Interaction between drugs and the gut microbiome. Gut 2020, 69, 1510–1519. [Google Scholar] [CrossRef]
- Elkrief, A.; Derosa, L.; Kroemer, G.; Zitvogel, L.; Routy, B. The negative impact of antibiotics on outcomes in cancer patients treated with immunotherapy: A new independent prognostic factor? Ann. Oncol. 2019, 30, 1572–1579. [Google Scholar] [CrossRef]
- Fessler, J.; Matson, V.; Gajewski, T.F. Exploring the emerging role of the microbiome in cancer immunotherapy. J. Immunother. Cancer 2019, 7, 108. [Google Scholar] [CrossRef] [PubMed]
- Mura, C.; Preissner, S.; Nahles, S.; Heiland, M.; Bourne, P.E.; Preissner, R. Real-world evidence for improved outcomes with histamine antagonists and aspirin in 22,560 COVID-19 patients. Signal Transduct. Target. Ther. 2021, 6, 267. [Google Scholar] [CrossRef] [PubMed]
- Takiishi, T.; Fenero, C.I.M.; Câmara, N.O.S. Intestinal barrier and gut microbiota: Shaping our immune responses throughout life. Tissue Barriers 2017, 5, e1373208. [Google Scholar] [CrossRef] [PubMed]
- Wastyk, H.C.; Fragiadakis, G.K.; Perelman, D.; Dahan, D.; Merrill, B.D.; Yu, F.B.; Topf, M.; Gonzalez, C.G.; Van Treuren, W.; Han, S.; et al. Gut-microbiota-targeted diets modulate human immune status. Cell 2021, 184, 4137–4153.e14. [Google Scholar] [CrossRef] [PubMed]
- Andrews, M.C.; Duong, C.P.M.; Gopalakrishnan, V.; Iebba, V.; Chen, W.-S.; Derosa, L.; Khan, A.W.; Cogdill, A.P.; White, M.G.; Wong, M.C.; et al. Gut microbiota signatures are associated with toxicity to combined CTLA-4 and PD-1 blockade. Nat. Med. 2021, 27, 1432–1441. [Google Scholar] [CrossRef]
- Gopalakrishnan, V.; Helmink, B.A.; Spencer, C.N.; Reuben, A.; Wargo, J.A. The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy. Cancer Cell 2018, 33, 570–580. [Google Scholar] [CrossRef]
- Gopalakrishnan, V.; Spencer, C.N.; Nezi, L.; Reuben, A.; Andrews, M.C.; Karpinets, T.V.; Prieto, P.A.; Vicente, D.; Hoffman, K.; Wei, S.C.; et al. Gut microbiome modulates response to anti–PD-1 immunotherapy in melanoma patients. Science 2018, 359, 97–103. [Google Scholar] [CrossRef]
- Li, W.; Deng, Y.; Chu, Q.; Zhang, P. Gut microbiome and cancer immunotherapy. Cancer Lett. 2019, 447, 41–47. [Google Scholar] [CrossRef]
- Roviello, G.; Iannone, L.F.; Bersanelli, M.; Mini, E.; Catalano, M. The gut microbiome and efficacy of cancer immunotherapy. Pharmacol. Ther. 2021, 231, 107973. [Google Scholar] [CrossRef]
- Sepich-Poore, G.D.; Zitvogel, L.; Straussman, R.; Hasty, J.; Wargo, J.A.; Knight, R. The microbiome and human cancer. Science 2021, 371, eabc4552. [Google Scholar] [CrossRef]
- Iizumi, T.; Battaglia, T.; Ruiz, V.; Perez Perez, G.I. Gut Microbiome and Antibiotics. Arch. Med. Res. 2017, 48, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Lange, K.; Buerger, M.; Stallmach, A.; Bruns, T. Effects of Antibiotics on Gut Microbiota. Dig. Dis. 2016, 34, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Reyman, M.; van Houten, M.A.; Watson, R.L.; Chu, M.L.J.N.; Arp, K.; de Waal, W.J.; Schiering, I.; Plötz, F.B.; Willems, R.J.L.; van Schaik, W.; et al. Effects of early-life antibiotics on the developing infant gut microbiome and resistome: A randomized trial. Nat. Commun. 2022, 13, 893. [Google Scholar] [CrossRef] [PubMed]
- Al-Qadami, G.; Bowen, J.; Van Sebille, Y.; Secombe, K.; Dorraki, M.; Verjans, J.; Wardill, H.; Le, H. Baseline gut microbiota composition is associated with oral mucositis and tumour recurrence in patients with head and neck cancer: A pilot study. Support. Care Cancer 2023, 31, 98. [Google Scholar] [CrossRef]
- Nenclares, P.; Bhide, S.A.; Sandoval-Insausti, H.; Pialat, P.; Gunn, L.; Melcher, A.; Newbold, K.; Nutting, C.M.; Harrington, K.J. Impact of antibiotic use during curative treatment of locally advanced head and neck cancers with chemotherapy and radiotherapy. Eur. J. Cancer 2020, 131, 9–15. [Google Scholar] [CrossRef]
- Yu, Y.; Zheng, P.; Gao, L.; Li, H.; Tao, P.; Wang, D.; Ding, F.; Shi, Q.; Chen, H. Effects of Antibiotic Use on Outcomes in Cancer Patients Treated Using Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. J. Immunother. 2020, 44, 76–85. [Google Scholar] [CrossRef]
- Anthony, W.E.; Wang, B.; Sukhum, K.V.; D’souza, A.W.; Hink, T.; Cass, C.; Seiler, S.; Reske, K.A.; Coon, C.; Dubberke, E.R.; et al. Acute and persistent effects of commonly used antibiotics on the gut microbiome and resistome in healthy adults. Cell Rep. 2022, 39, 110649. [Google Scholar] [CrossRef]
- Shanahan, F. Changing the narrative on antibiotics. Gut 2015, 64, 1674–1675. [Google Scholar] [CrossRef]
- Huang, C.; Shi, G. Smoking and microbiome in oral, airway, gut and some systemic diseases. J. Transl. Med. 2019, 17, 225. [Google Scholar] [CrossRef]
- Langenau, J.; Boeing, H.; Bergmann, M.M.; Nöthlings, U.; Oluwagbemigun, K. The Association between Alcohol Consumption and Serum Metabolites and the Modifying Effect of Smoking. Nutrients 2019, 11, 2331. [Google Scholar] [CrossRef]
- Shahi, F.; Redeker, K.; Chong, J. Rethinking antimicrobial stewardship paradigms in the context of the gut microbiome. JAC-Antimicrob. Resist. 2019, 1, dlz015. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Song, J.; Hu, J.; Fu, H.; Feng, Y.; Mu, R.; Xing, Z.; Wang, Z.; Wang, L.; Zhang, J.; et al. Smectite promotes probiotic biofilm formation in the gut for cancer immunotherapy. Cell Rep. 2021, 34, 108706. [Google Scholar] [CrossRef] [PubMed]
| Propensity Score Density Function—Before (Left) and after (Right) Matching (Cohort I—Purple, Cohort II—Green) | |
|---|---|
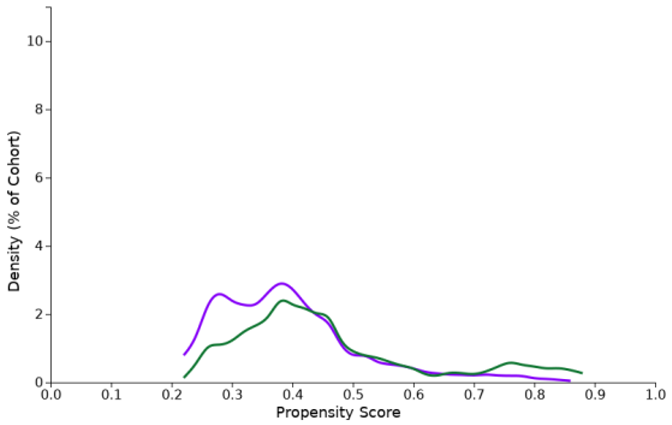 | 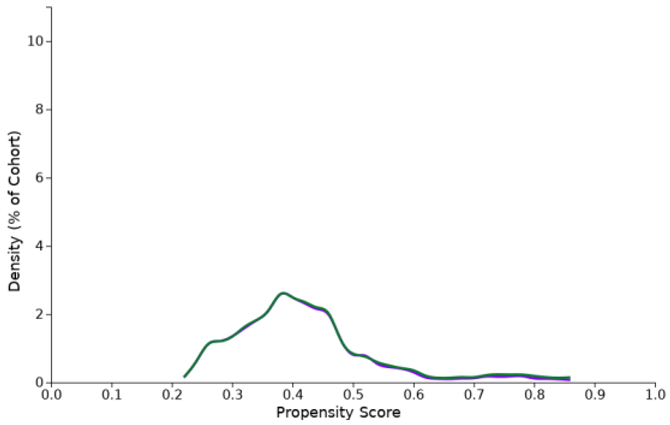 |
| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| Patients (n) | Cohort I | Cohort II | p-Value | Standardized Mean Difference | Cohort I | Cohort II | p-Value | Standardized Mean Difference |
| Total | 2149 | 1502 | 1362 | 1362 | ||||
| Age at index | 65.7 | 64.0 | <0.001 | 0.141 | 64.5 | 64.4 | 0.773 | 0.011 |
| Standard deviation | 12.1 | 12.2 | 12.1 | 12.1 | ||||
| Males | 1579 73.5% | 1117 74.4% | 0.546 | 0.020 | 1043 76.6% | 1007 73.9% | 0.110 | 0.061 |
| Females | 570 26.5% | 385 25.6% | 0.546 | 0.020 | 319 23.4% | 355 26.1% | 0.110 | 0.061 |
| BMI | 24.8 | 23.9 | <0.001 | 0.148 | 24.6 | 24.1 | 0.065 | 0.086 |
| Standard deviation | 5.6 | 5.4 | 5.4 | 5.4 | ||||
| Metastases | 1126 31.8% | 890 40.1% | <0.001 | 0.138 | 785 57.6% | 788 57.9% | 0.907 | 0.004 |
| Tobacco use | 684 32.1% | 603 35.4% | 0.059 | 0.070 | 524 38.5% | 523 38.4% | 0.969 | 0.002 |
| Feeding device | 363 16.9% | 423 28.1% | <0.001 | 0.138 | 319 23.5% | 322 23.6% | 0.961 | 0.002 |
| Severe sepsis | 41 1.9% | 145 9.7% | <0.001 | 0.337 | 40 2.9% | 43 3.2% | 0.738 | 0.013 |
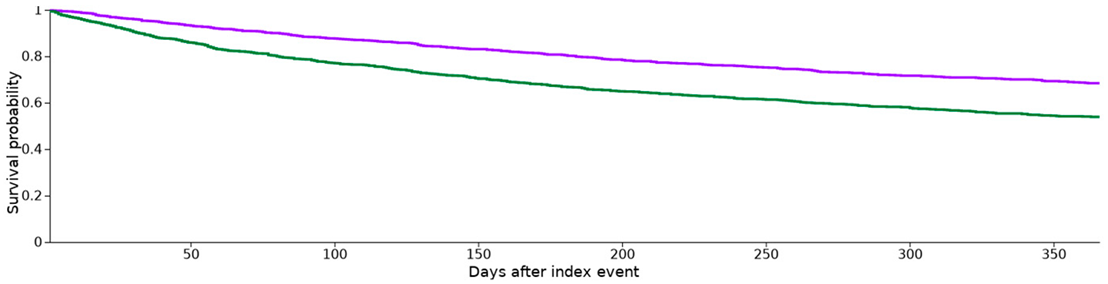
| Cohort | Patients in Cohort | Patients with Outcome | Median Survival (days) | Survival Probability at End of Time Window | ||
|---|---|---|---|---|---|---|
| I | w/o antibiotics | 1362 | 346 | -- | 68.42% | |
| II | w antibiotics | 1362 | 511 | -- | 53.89% | |
| χ2 | df | p | ||||
| Log-rank test | 61.522 | 1 | 0.000 | |||
| Hazard Ratio | 95% CI | χ2 | df | p | ||
| Hazard ratio and proportionality | 0.58 | (0.51, 0.67) | 6.52 | 1 | 0.011 | |
 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Preissner, S.; Heiland, M.; Preissner, R.; Wirth, M.; Wollenberg, B. Antibiotics Significantly Decrease the Survival of Head and Neck Carcinoma Patients with Immunotherapy: A Real-World Analysis of More Than 3000 Cases. Cancers 2023, 15, 2342. https://doi.org/10.3390/cancers15082342
Preissner S, Heiland M, Preissner R, Wirth M, Wollenberg B. Antibiotics Significantly Decrease the Survival of Head and Neck Carcinoma Patients with Immunotherapy: A Real-World Analysis of More Than 3000 Cases. Cancers. 2023; 15(8):2342. https://doi.org/10.3390/cancers15082342
Chicago/Turabian StylePreissner, Saskia, Max Heiland, Robert Preissner, Markus Wirth, and Barbara Wollenberg. 2023. "Antibiotics Significantly Decrease the Survival of Head and Neck Carcinoma Patients with Immunotherapy: A Real-World Analysis of More Than 3000 Cases" Cancers 15, no. 8: 2342. https://doi.org/10.3390/cancers15082342
APA StylePreissner, S., Heiland, M., Preissner, R., Wirth, M., & Wollenberg, B. (2023). Antibiotics Significantly Decrease the Survival of Head and Neck Carcinoma Patients with Immunotherapy: A Real-World Analysis of More Than 3000 Cases. Cancers, 15(8), 2342. https://doi.org/10.3390/cancers15082342








