The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review
Abstract
Simple Summary
Abstract
1. Introduction
2. Aim
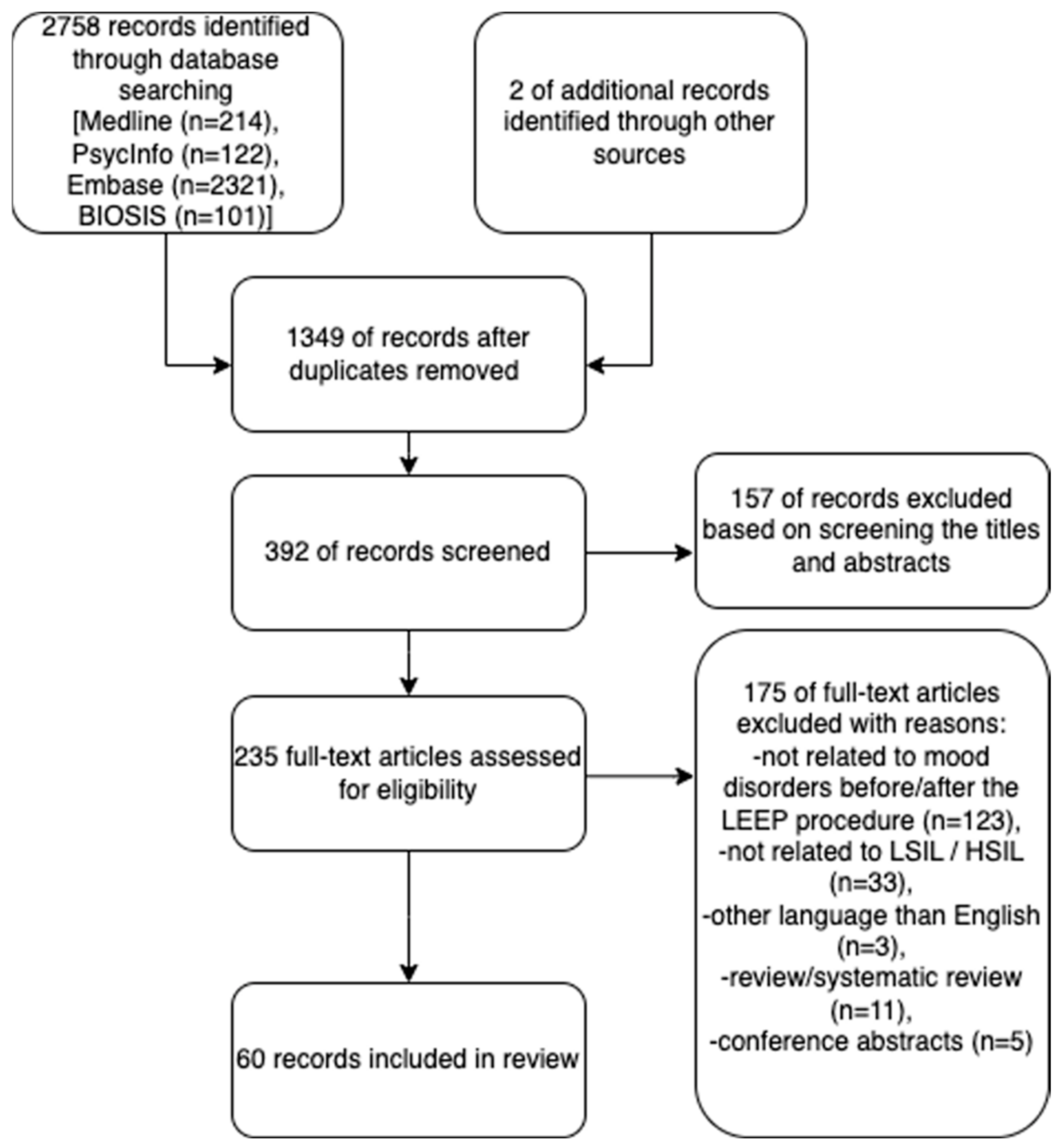
3. Methods
4. Results
4.1. Study Characteristics
4.2. Quality Assessment
4.3. Impact of HPV Diagnosis on Anxiety, Depression, Quality of Life, and Sexual Functions
4.4. Impact of the LEEP Procedure on Anxiety, Depression, Quality of Life, and Sexual Functions
5. Discussion
Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Human Papillomavirus (HPV). Available online: https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/human-papillomavirus (accessed on 8 December 2022).
- Human Papillomavirus (HPV)—NHS. Available online: https://www.nhs.uk/conditions/human-papilloma-virus-hpv/ (accessed on 8 December 2022).
- Human Papillomavirus (HPV) Infection—STI Treatment Guidelines. Available online: https://www.cdc.gov/std/treatment-guidelines/hpv.htm (accessed on 22 October 2022).
- What Can I Do to Reduce My Risk of Cervical Cancer?|CDC. Available online: https://www.cdc.gov/cancer/cervical/basic_info/prevention.htm (accessed on 22 October 2022).
- Wejbert-Wąsiewicz, E.; Pęczkowska, E. Problemy edukacji seksualnej w Polsce. Przegląd Socjol. 2009, 3, 173–192. [Google Scholar]
- Marlow, L.A.V.; McBride, E.; Ridout, D.; Forster, A.S.; Kitchener, H.; Waller, J. Patterns of anxiety and distress over 12 months following participation in HPV primary screening. Sex. Transm. Infect. 2022, 98, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Drolet, M.; Brisson, M.; Maunsell, E.; Franco, E.L.; Coutlée, F.; Ferenczy, A.; Fisher, W.; Mansi, J.A. The psychosocial impact of an abnormal cervical smear result. Psychooncology 2012, 21, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Heinonen, A.; Tapper, A.M.; Leminen, A.; Sintonen, H.; Roine, R.P. Health-related quality of life and perception of anxiety in women with abnormal cervical cytology referred for colposcopy: An observational study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 387–391. [Google Scholar] [CrossRef]
- Kwan, T.T.; Cheung, A.N.; Lo, S.S.; Lee, P.W.; Tam, K.-F.; Chan, K.K.; Ngan, H.Y. Psychological burden of testing positive for high-risk human papillomavirus on women with atypical cervical cytology: A prospective study. Acta Obstet. Gynecol. Scand. 2011, 90, 445–451. [Google Scholar] [CrossRef]
- McBride, E.; Marlow, L.A.; Forster, A.S.; Ridout, D.; Kitchener, H.; Patnick, J.; Waller, J. Anxiety and distress following receipt of results from routine HPV primary testing in cervical screening: The psychological impact of primary screening (PIPS) study. Int. J. Cancer 2020, 146, 2113. [Google Scholar] [CrossRef]
- Chadwick, V.; Bennett, K.F.; McCaffery, K.J.; Brotherton, J.M.L.; Dodd, R.H. Psychosocial impact of testing human papillomavirus positive in Australia’s human papillomavirus-based cervical screening program: A cross-sectional survey. Psychooncology 2022, 31, 1110–1119. [Google Scholar] [CrossRef]
- Arrossi, S.; Almonte, M.; Herrero, R.; Gago, J.; Antelo, V.S.; Szwarc, L.; Thouyaret, L.; Paolino, M.; Wiesner, C. Psycho-social impact of positive human papillomavirus testing in Jujuy, Argentina results from the Psycho-Estampa study. Prev. Med. Rep. 2020, 18, 101070. [Google Scholar] [CrossRef]
- Inna, N.; Phianmongkhol, Y.; Charoenkwan, K. Sexual function after loop electrosurgical excision procedure for cervical dysplasia. J. Sex. Med. 2010, 7, 1291–1297. [Google Scholar] [CrossRef]
- Gaurav, A.; Verma, P.; Heda, A.; Kapur, D.; Arora, S.; Panda, S.; Khoiwal, K.; Chaturvedi, J. Psychosexual Health After Loop Electrosurgical Excision Procedure (LEEP) among Women with Cervical Intraepithelial Neoplasia in North Indian tertiary Centre: A Prospective Observational Study. Arch. Gynecol. Obstet. 2022. [Google Scholar] [CrossRef]
- Michaan, N.; Loboda, N.; Ochshorn, I.; Tzur, Y.; Cohen, A.; Grisaru, D.; Laskov, I. The Effect of Cervical Conization on Women’s’ Sexual Function and Psychological Health, A Prospective Observational Study. J. Sex. Med. 2022, 19, 257–262. [Google Scholar] [CrossRef]
- Hellsten, C.; Lindqvist, P.G.; Sjöström, K. A longitudinal study of sexual functioning in women referred for colposcopy: A 2-year follow up. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 205–211. [Google Scholar] [CrossRef]
- Serati, M.; Salvatore, S.; Cattoni, E.; Zanirato, M.; Mauri, S.; Siesto, G.; Cromi, A.; Ghezzi, F.; Bolis, P. The impact of the loop electrosurgical excisional procedure for cervical intraepithelial lesions on female sexual function. J. Sex. Med. 2010, 7, 2267–2272. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Rask, M.; Swahnberg, K.; Oscarsson, M. Swedish women’s awareness of human papillomavirus, and health-related quality of life, anxiety, and depression after a notification of an abnormal Pap smear result: A cross-sectional study. Eur. J. Cancer Prev. 2019, 28, 96–101. [Google Scholar] [CrossRef]
- Rask, M.; Swahnberg, K.; Oscarsson, M. Notification of an abnormal Pap smear result: An intervention study. Eur. J. Cancer Care 2019, 28, e12969. [Google Scholar] [CrossRef]
- Leite, V.; Santos, B.D.; Pereira, M.G. Psychosocial impact of human papillomavirus on women’s sexual dissatisfaction and quality of life. J. Psychosom. Obstet. Gynecol. 2018, 40, 232–238. [Google Scholar] [CrossRef]
- Fei Ngu, S.; Wei, N.; Kwan, T.T.C.; Chu, M.M.Y.; Tse, K.Y.; Chan, K.K.L.; Ngan, H.Y.S. Impact of different educational interventions on psychosocial well-being of women with a positive high-risk human papillomavirus and normal cervical cytology: A randomised trial. J. Psychosom. Obstet. Gynecol. 2018, 39, 146–155. [Google Scholar] [CrossRef]
- Santos, B.D.; Moreira, C.S.; Vilhena, E.; Carvalho, E.; Pereira, M.G. Validation of the HPV Impact Profile in Portuguese women with human papilloma virus. Curr. Med. Res. Opin. 2019, 35, 1275–1282. [Google Scholar] [CrossRef]
- Le, T.; Hopkins, L.; Menard, C.; Lefebvre, J.; Fung, M.F.K.; Hicks-Boucher, W. Psychologic morbidities prior to loop electrosurgical excision procedure in the treatment of cervical intraepithelial neoplasia. Int. J. Gynecol. Cancer 2006, 16, 1089–1093. [Google Scholar] [CrossRef]
- Atallah, D.M.; El Feghaly, C.; El Feghaly, M.; Arab, W.; Khaddage, A.; Akiki, M.; El Kassis, N.; Abboud, S.; Chahine, G.; Moubarak, M. Validation of the Human Papillomavirus Impact Profile in Lebanese Women With Human Papillomavirus or Associated Lesions. J. Low. Genit. Tract Dis. 2022, 26, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Atallah, D.M.; El Feghaly, C.; El Feghaly, M.; Arab, W.; Khaddage, A.; Akiki, M.; El Kassis, N.; Chakra, R.A.; Chahine, G.; Moubarak, M. Does Social and Religious Background Matter? A Study of the Psychosocial Impact of Human Papillomavirus on Lebanese Women. J. Low. Genit. Tract Dis. 2022, 26, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Fielding, S.; Rothnie, K.; Gray, N.M.; Little, J.; Cruickshank, M.E.; Neal, K.; Walker, L.G.; Whynes, D.; Cotton, S.C.; Sharp, L. Psychosocial morbidity in women with abnormal cervical cytology managed by cytological surveillance or initial colposcopy: Longitudinal analysis from the TOMBOLA randomised trial. Psychooncology 2017, 26, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.Y.; Sharp, L.; Cotton, S.C.; Harris, C.A.; Gray, N.M.; Little, J. Human Papillomavirus Infection and Anxiety: Analyses in Women with Low-Grade Cervical Cytological Abnormalities Unaware of Their Infection Status. PLoS ONE 2011, 6, e21046. [Google Scholar] [CrossRef] [PubMed]
- Mercan, R.; Mercan, S.; Durmaz, B.; Sur, H.; Kilciksiz, C.M.; Kacar, A.S.; Apaydin, Z.; Ayhan, C.; Ata, B. Sexual dysfunction in women with human papilloma virus infection in the Turkish population. J. Obstet. Gynaecol. 2019, 39, 659–663. [Google Scholar] [CrossRef]
- Sparić, R.; Papoutsis, D.; Kadija, S.; Stefanović, R.; Antonakou, A.; Nejković, L.; Kesić, V. Psychosexual outcomes in women of reproductive age at more than two-years from excisional cervical treatment—A cross-sectional study. J. Psychosom. Obstet. Gynecol. 2019, 40, 128–137. [Google Scholar] [CrossRef]
- Alay, I.; Kaya, C.; Karaca, I.; Yildiz, S.; Baghaki, S.; Cengiz, H.; Ekin, M.; Yasar, L. The effect of being diagnosed with human papillomavirus infection on women’s sexual lives. J. Med. Virol. 2020, 92, 1290–1297. [Google Scholar] [CrossRef]
- Nahidi, M.; Nahidi, Y.; Saghebi, A.; Kardan, G.; Jarahi, L.; Aminzadeh, B.; Shojaei, P.; Bordbar, M.R.F. Evaluation of Psychopathology and Quality of Life in Patients with Anogenital Wart Compared to Control Group. Iran. J. Med. Sci. 2018, 43, 65. [Google Scholar]
- Dodd, R.H.; Mac, O.; Brotherton, J.M.L.; Cvejic, E.; McCaffery, K.J. Levels of anxiety and distress following receipt of positive screening tests in Australia’s HPV-based cervical screening programme: A cross-sectional survey. Sex. Transm. Infect. 2020, 96, 166–172. [Google Scholar] [CrossRef]
- Hsu, Y.Y.; Wang, W.M.; Fetzer, S.J.; Cheng, Y.M.; Hsu, K.F. Longitudinal psychosocial adjustment of women to human papillomavirus infection. J. Adv. Nurs. 2018, 74, 2523–2532. [Google Scholar] [CrossRef]
- McCaffery, K.J.; Irwig, L.; Turner, R.; Chan, S.F.; Macaskill, P.; Lewicka, M.; Clarke, J.; Weisberg, E.; Barratt, A. Psychosocial outcomes of three triage methods for the management of borderline abnormal cervical smears: An open randomised trial. BMJ 2010, 340, 460. [Google Scholar] [CrossRef]
- McBride, E.; Marlow, L.A.V.; Bennett, K.F.; Stearns, S.; Waller, J. Exploring reasons for variations in anxiety after testing positive for human papillomavirus with normal cytology: A comparative qualitative study. Psychooncology 2021, 30, 84. [Google Scholar] [CrossRef]
- McBride, E.; Marlow, L.A.V.; Chilcot, J.; Moss-Morris, R.; Waller, J. Distinct Illness Representation Profiles Are Associated With Anxiety in Women Testing Positive for Human Papillomavirus. Ann. Behav. Med. 2022, 56, 78–88. [Google Scholar] [CrossRef]
- McCaffery, K.; Waller, J.; Forrest, S.; Cadman, L.; Szarewski, A.; Wardle, J. Testing positive for human papillomavirus in routine cervical screening: Examination of psychosocial impact. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 1437–1443. [Google Scholar] [CrossRef]
- Plotti, F.; Rossini, G.; Ficarola, F.; Nardone, C.D.C.; Montera, R.; Guzzo, F.; Luvero, D.; Fabris, S.; Angioli, R.; Terranova, C. Early Mini-Invasive Treatment of Persistent Cervical Dysplasia: Clinical Outcome and Psycho-Relational Impact. Front. Surg. 2022, 9, 888457. [Google Scholar] [CrossRef]
- Rosen, N.O.; Knäuper, B.; Di Dio, P.; Morrison, E.; Tabing, R.; Feldstain, A.; Amsel, R.; Mayrand, M.-H.; Franco, E.L.; Rosberger, Z. The impact of intolerance of uncertainty on anxiety after receiving an informational intervention about HPV: A randomised controlled study. Psychol. Health 2010, 25, 651–668. [Google Scholar] [CrossRef]
- Sakin, Ö.; Uzun, S.B.; Koyuncu, K.; Giray, B.; Akalın, E.E.; Anğın, A.D. Cervix human papilloma virus positivity: Does it cause sexual dysfunction? Turk. J. Obstet. Gynecol. 2019, 16, 235. [Google Scholar] [CrossRef]
- Giovannetti, O.; Tomalty, D.; Greco, S.; Adams, M. Self-Report Assessment of Sexual Function After LEEP in Women who Report Negative Outcomes. J. Sex. Med. 2022, 19, S15–S16. [Google Scholar] [CrossRef]
- Garcés-Palacio, I.C.; Sanchez, G.I.; Zapata, A.B.; Sanchez, V.C.; Cosme, Y.U.; Zabala, D.R.; Osorio, M.A.R. Psychosocial impact of inclusion of HPV test on the management of women with atypical squamous cells of undetermined significance: A study within a randomised pragmatic trial in a middle-income country. Psychol. Health 2019, 35, 750–769. [Google Scholar] [CrossRef]
- Lee, T.S.; Kothari-Talwar, S.; Singhal, P.K.; Yee, K.; Kulkarni, A.; Lara, N.; Roset, M.; Giuliano, A.R.; Garland, S.M.; Ju, W. Cross-sectional study estimating the psychosocial impact of genital warts and other anogenital diseases in South Korea. BMJ Open 2019, 9, e025035. [Google Scholar] [CrossRef]
- Andreassen, T.; Hansen, B.T.; Engesaeter, B.; Hashim, D.; Støer, N.C.; Tropé, A.; Moen, K.; Ursin, G.; Weiderpass, E. Psychological effect of cervical cancer screening when changing primary screening method from cytology to high-risk human papilloma virus testing. Int. J. Cancer 2019, 145, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Conaglen, H.M.; Hughes, R.; Conaglen, J.V.; Morgan, J. A prospective study of the psychological impact on patients of first diagnosis of human papillomavirus. Int. J. STD AIDS 2001, 12, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Nagele, E.; Trutnovsky, G.; Greimel, E.; Dorfer, M.; Haas, J.; Reich, O. Do different treatment strategies influence women’s level of psychosexual distress? Observational cohort study of women with premalignant HPV-associated genital lesions. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 236, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Nagele, E.; Reich, O.; Greimel, E.; Dorfer, M.; Haas, J.; Trutnovsky, G. Sexual Activity, Psychosexual Distress, and Fear of Progression in Women With Human Papillomavirus-Related Premalignant Genital Lesions. J. Sex. Med. 2016, 13, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Sénécal, M.; Brisson, M.; Maunsell, E.; Ferenczy, A.; Franco, E.; Ratnam, S.; Coutlée, F.; Palefsky, J.M.; Mansi, J.A. Loss of quality of life associated with genital warts: Baseline analyses from a prospective study. Sex. Transm. Infect. 2011, 87, 209–215. [Google Scholar] [CrossRef]
- Ferenidou, F.; Salakos, N.; Vaidakis, N.; Paltoglou, G.; Bakalianou, K.; Papadimitriou, G.; Creatsas, G. The impact of HPV diagnosis on women’s sexual and mental health: Preliminary findings. Clin. Exp. Obstet. Gynecol. 2012, 39, 79–82. [Google Scholar]
- Filiberti, A.; Tamburini, M.; Stefanon, B.; Merola, M.; Bandieramonte, G.; Ventafridda, V.; De Palo, G. Psychological aspects of genital human papillomavirus infection: A preliminary report. J. Psychosom. Obstet. Gynecol. 1993, 14, 145–152. [Google Scholar] [CrossRef]
- Maggino, T.; Casadei, D.; Panontin, E.; Fadda, E.; Zampieri, M.; Donà, M.; Soldà, M.; Altoè, G. Impact of an HPV diagnosis on the quality of life in young women. Gynecol. Oncol. 2007, 107, S175–S179. [Google Scholar] [CrossRef]
- Ciavattini, A.; Carpini, G.D.; Giannella, L.; Del Fabro, A.; Banerji, V.M.; Hall, G.B.; Barbero, M.; Sopracordevole, F. An online survey on emotions, impact on everyday life, and educational needs of women with HPV positivity or abnormal Pap smear result. Medicine 2021, 100, e27177. [Google Scholar] [CrossRef]
- Clarke, P.; Ebel, C.; Catotti, D.N.; Stewart, S. The psychosocial impact of human papillomavirus infection: Implications for health care providers. Int. J. STD AIDS 1996, 7, 197–200. [Google Scholar] [CrossRef]
- Giannella, L.; Mfuta, K.; Lamantea, R.; Boselli, F.; Torrini, B.; Prandi, S. Loop electrosurgical excision procedure as a life event that impacts on postmenopausal women. J. Obstet. Gynaecol. Res. 2013, 39, 842–848. [Google Scholar] [CrossRef]
- McCaffery, K.; Irwig, L. Australian women’s needs and preferences for information about human papillomavirus in cervical screening. J. Med. Screen. 2005, 12, 134–141. [Google Scholar] [CrossRef]
- Jentschke, M.; Lehmann, R.; Drews, N.; Hansel, A.; Schmitz, M.; Hillemanns, P. Psychological distress in cervical cancer screening: Results from a German online survey. Arch Gynecol. Obstet. 2020, 302, 699. [Google Scholar] [CrossRef]
- Monsonego, J.; Cortes, J.; da Silva, D.P.; Jorge, A.F.; Klein, P. Psychological impact, support and information needs for women with an abnormal Pap smear: Comparative results of a questionnaire in three European countries. BMC Women’s Health 2011, 11, 18. [Google Scholar] [CrossRef]
- O’Connor, M.; O’Leary, E.; Waller, J.; Gallagher, P.; Martin, C.M.; O’Leary, J.J.; Sharp, L. Socio-economic variations in anticipated adverse reactions to testing HPV positive: Implications for the introduction of primary HPV-based cervical screening. Prev. Med. 2018, 115, 90–96. [Google Scholar] [CrossRef]
- Pereira-Caldeira, N.M.V.; Góes, F.G.B.; De Almeida-Cruz, M.C.M.; De Souza Caliari, J.; Pereira-Ávila, F.M.V.; Gir, E. Quality of Life for Women with Human Papillomavirus-induced Lesions. Rev. Bras. Ginecol. Obstet. 2020, 42, 211–217. [Google Scholar] [CrossRef]
- Waller, J.; McCaffery, K.; Kitchener, H.; Nazroo, J.; Wardle, J. Women’s experiences of repeated HPV testing in the context of cervical cancer screening: A qualitative study. Psychooncology 2007, 16, 196–204. [Google Scholar] [CrossRef]
- McCaffery, K.; Waller, J.; Nazroo, J.; Wardle, J. Social and psychological impact of HPV testing in cervical screening: A qualitative study. Sex. Transm. Infect. 2006, 82, 1s–174. [Google Scholar] [CrossRef]
- Lee Mortensen, G.; Adeler, A.L. Qualitative study of women’s anxiety and information needs after a diagnosis of cervical dysplasia. J. Public Health 2010, 18, 473–482. [Google Scholar] [CrossRef]
- Patel, H.; Moss, E.L.; Sherman, S.M. HPV primary cervical screening in England: Women’s awareness and attitudes. Psychooncology 2018, 27, 1559–1564. [Google Scholar] [CrossRef]
- Waller, J.; Marlow, L.A.V.; Wardle, J. The association between knowledge of HPV and feelings of stigma, shame and anxiety. Sex. Transm. Infect. 2007, 83, 155. [Google Scholar] [CrossRef] [PubMed]
- Waller, J.; Marlow, L.A.V.; Wardle, J. Anticipated shame and worry following an abnormal Pap test result: The impact of information about HPV. Prev. Med. 2009, 48, 415–419. [Google Scholar] [CrossRef]
- Kitchener, H.C.; Fletcher, I.; Roberts, C.; Wheeler, P.; Almonte, M.; Maguire, P. The psychosocial impact of human papillomavirus testing in primary cervical screening-a study within a randomized trial. Int. J. Gynecol. Cancer 2008, 18, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Landy, R.; Pesola, F.; Castañón, A.; Sasieni, P. Impact of cervical screening on cervical cancer mortality: Estimation using stage-specific results from a nested case–control study. Br. J. Cancer 2016, 115, 1140–1146. [Google Scholar] [CrossRef] [PubMed]
- Sørbye, S.W.; Fismen, S.; Gutteberg, T.J.; Mortensen, E.S.; Skjeldestad, F.E. Primary cervical cancer screening with an HPV mRNA test: A prospective cohort study. BMJ Open 2016, 6, e011981. [Google Scholar] [CrossRef]
- Sundström, K.; Dillner, J. How Many Human Papillomavirus Types Do We Need to Screen For? J. Infect. Dis. 2021, 223, 1510–1511. [Google Scholar] [CrossRef]
- McCredie, M.R.; Sharples, K.J.; Paul, C.; Baranyai, J.; Medley, G.; Jones, R.W.; Skegg, D.C. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: A retrospective cohort study. Lancet Oncol. 2008, 9, 425–434. [Google Scholar] [CrossRef]
- Malagón, T.; Mayrand, M.H.; Ogilvie, G.; Gotlieb, W.H.; Blake, J.; Bouchard, C.; Franco, E.L.; Kulasingam, S. Modeling the Balance of Benefits and Harms of Cervical Cancer Screening with Cytology and Human Papillomavirus Testing. Cancer Epidemiol. Biomark. Prev. 2020, 29, 1436–1446. [Google Scholar] [CrossRef]
- Santos, B.D.; Carvalho, E.C.; Pereira, M.G. Dyadic Adjustment in HPV-Infected Women One Year After Diagnosis. Psychiatry 2019, 82, 216–227. [Google Scholar]
- Dellino, M.; Cascardi, E.; Tomasone, V.; Zaccaro, R.; Maggipinto, K.; Giacomino, M.E.; De Nicolò, M.; De Summa, S.; Cazzato, G.; Scacco, S.; et al. Communications Is Time for Care: An Italian Monocentric Survey on Human Papillomavirus (HPV) Risk Information as Part of Cervical Cancer Screening. J. Pers. Med. 2022, 12, 1387. [Google Scholar] [CrossRef]
- Dellino, M.; Cascardi, E.; Laganà, A.S.; Di Vagno, G.; Malvasi, A.; Zaccaro, R.; Maggipinto, K.; Cazzato, G.; Scacco, S.; Tinelli, R.; et al. Lactobacillus crispatus M247 oral administration: Is it really an effective strategy in the management of papillomavirus-infected women? Infect. Agents Cancer 2022, 17, 53. [Google Scholar] [CrossRef]
- Cunningham, S.D.; Tschann, J.; Gurvey, J.E.; Fortenberry, J.D.; Ellen, J.M. Attitudes about sexual disclosure and perceptions of stigma and shame. Sex. Transm. Infect. 2002, 78, 334–338. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sikorska, M.; Pawłowska, A.; Antosik-Wójcińska, A.; Zyguła, A.; Suchońska, B.; Dominiak, M. The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review. Cancers 2023, 15, 2226. https://doi.org/10.3390/cancers15082226
Sikorska M, Pawłowska A, Antosik-Wójcińska A, Zyguła A, Suchońska B, Dominiak M. The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review. Cancers. 2023; 15(8):2226. https://doi.org/10.3390/cancers15082226
Chicago/Turabian StyleSikorska, Michalina, Adriana Pawłowska, Anna Antosik-Wójcińska, Aleksandra Zyguła, Barbara Suchońska, and Monika Dominiak. 2023. "The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review" Cancers 15, no. 8: 2226. https://doi.org/10.3390/cancers15082226
APA StyleSikorska, M., Pawłowska, A., Antosik-Wójcińska, A., Zyguła, A., Suchońska, B., & Dominiak, M. (2023). The Impact of HPV Diagnosis and the Electrosurgical Excision Procedure (LEEP) on Mental Health and Sexual Functioning: A Systematic Review. Cancers, 15(8), 2226. https://doi.org/10.3390/cancers15082226






