Simple Summary
Telemedicine became widespread during the COVID-19 pandemic, but little is known about its persistence in routine cancer care after the pandemic’s peak. This study examined telemedicine use for breast and prostate cancer patients at a New York City cancer center before, during, and after the pandemic’s peak. Telemedicine usage increased from 2% before the pandemic to 50% during the peak and then decreased to 30% after the peak. Both during and after the peak, psychiatry, social work, and nutrition conducted almost all visits remotely, while surgery and nursing maintained low telemedicine usage. Most departments continued to use telemedicine at or above peak levels, except for medicine, neurology, and survivorship. Anesthesiology and neurology used telemedicine more for follow-ups, while nursing used it more for new visits. These findings highlight specific contexts where patients and providers choose telemedicine even when other options are available. However, more research is needed to assess telemedicine’s suitability for and impact on cancer care.
Abstract
While COVID-19 catalyzed a shift to telemedicine, little is known about the persistence of remote cancer care in non-emergent times. We assessed telemedicine use at a high-volume academic cancer center in New York City and analyzed breast and prostate cancer visits pre-COVID-19, peak COVID-19, and post-peak. Descriptive statistics assessed visit mode (in person, telemedicine) and type (new, follow-up, other) by department/specialty, with Fisher’s exact tests comparing peak/post-peak differences. The study included 602,233 visits, with telemedicine comprising 2% of visits pre-COVID-19, 50% peak COVID-19, and 30% post-peak. Notable variations emerged by department/specialty and visit type. Post-peak, most departments/specialties continued using telemedicine near or above peak levels, except medicine, neurology, and survivorship, where remote care fell. In psychiatry, social work, and nutrition, nearly all visits were conducted remotely during and after peak COVID-19, while surgery and nursing maintained low telemedicine usage. Post-peak, anesthesiology and neurology used telemedicine seldom for new visits but often for follow-ups, while nursing showed the opposite pattern. These trends suggest department- and visit-specific contexts where providers and patients choose telemedicine in non-emergent conditions. More research is needed to explore these findings and evaluate telemedicine’s appropriateness and impact across the care continuum.
1. Introduction
Telemedicine holds great promise for augmenting and enhancing the delivery of cancer care across the continuum, improving patient access, convenience, and overall quality of care. However, the contexts in which cancer patients and providers select remote care remain relatively unexplored. Only a few studies have examined these issues, mostly focused on a single specialty, patient population, or treatment scenario (e.g., neurosurgery, radiotherapy) [1,2,3,4,5,6,7,8]. What is clear, however, is that telemedicine “is not ideally suited for all patients and/or clinical scenarios, for a wide range of reasons” [9]. Better understanding patterns in telemedicine’s use is therefore crucial for optimizing its integration and maximizing its benefits.
The COVID-19 pandemic provides unique opportunities to explore these vital issues. While few oncologists in the U.S. used telemedicine pre-pandemic, the emergence of COVID-19 obliged them to deliver as much care as possible via telemedicine—by necessity, even when in-person visits might have been more appropriate or optimal [9,10,11,12]. As in-person options have returned, post-peak care patterns can indicate situations where telemedicine has persisted as a part of routine care.
Leveraging these data, this study assessed trends in telemedicine use for breast and prostate cancer patients at a high-volume academic cancer center in New York City before, during, and after the peak of the COVID-19 pandemic. We hypothesized that trends by department/specialty and visit type—particularly in the post-peak period—could distinguish specific contexts in which telemedicine was frequently chosen by providers and patients after in-person options re-emerged. The findings offer new insights around the use of telemedicine in routine cancer care and suggest promising areas for future research into telemedicine appropriateness.
2. Materials and Methods
Setting: This retrospective study analyzed trends in telemedicine utilization at Memorial Sloan Kettering Cancer Center (MSK), a high-volume academic cancer center in New York City. The study period was divided into three phases: pre-COVID-19 (March 2019 to February 2020), peak COVID-19 (March 2020 to February 2021), and post-peak (March 2021 to February 2022). We focused on visits by breast and prostate cancer patients, the two most common non-dermatologic malignancies in women and men [13,14,15]. Our sample was part of a larger study of these populations, as reviewed and approved by MSK’s Institutional Review Board.
Data sources: Data were obtained from electronic health records (EHR) and administrative databases for clinical visits deemed to be feasible by telemedicine, meaning they did not require diagnostic studies, treatments, or procedures. Data captured for each visit included department/specialty, visit mode (telephone, video, or in person), and visit type (new, follow-up, or other). As recorded in the EHR, “new visits” included appointments for patients visiting MSK for the first time, as well as for established patients seeing a new department/specialty. Thus, the “new visits” category spanned the continuum of care, from patients’ initial appointment at MSK to developments anywhere along the continuum where additional departments/specialties became involved. “Follow-up visits” were those in which established patients were returning to a department/specialty for additional consultations. “Other” visits encompassed a heterogeneous range of services labeled as neither “new” nor “follow-up” in the EHR. We also captured the total number of unique patients in the 3 study periods, as well as their demographic characteristics (age, race, ethnicity, gender, cancer type, primary language).
Data analysis: We combined telephone and video visits into a single category of “telemedicine visits.” We used descriptive statistics to assess frequencies of telemedicine versus in person, as well as new, follow-up, and other visits by specialty/department over time. We used Fishers’ exact tests to assess significant changes in usage patterns from the peak to post-peak period. A p-value < 0.05 was considered statistically significant for these analyses. Analyses were conducted using the R software program (version 4.3.1).
3. Results
The study included a total of 602,233 visits, of which 26% (158,986) were conducted via telemedicine. We found no notable differences in the numbers of patients or visits over time, and patients’ characteristics were also comparable across the pre-COVID-19, peak-COVID-19, and post-peak periods (Table 1).

Table 1.
Patient characteristics, by time period.
Institution-level trends: As to be expected, we found significant fluctuations in the usage of telemedicine across the three study periods overall: During the pre-COVID-19 period, telemedicine accounted for only 2% (3344) of feasible visits. However, with the onset of the pandemic, there was a dramatic shift towards telemedicine, with utilization reaching 50% (89,915) during the peak COVID-19 time-frame. Subsequently, in the post-peak period, telemedicine utilization decreased to 30% (65,727) as in-person care regained prominence (Table 2).

Table 2.
Proportion of telemedicine and in-person consultations over time, by department.
Trends by department/specialty: We also found striking temporal variations by department/specialty. In departments such as anesthesiology, integrative medicine, and neurosurgery, the majority of all feasible visits were conducted via telemedicine during peak COVID-19, and this pattern persisted post-peak. Indeed, in cardiology, nutrition, psychiatry, and social work, nearly all visits (94%, 96%, 96%, and 97%, respectively) continued to be conducted remotely post-peak. Conversely, nursing and surgery demonstrated the lowest rates of growth in telemedicine utilization, with post-peak telemedicine rates of only 8% and 17%, respectively. Medicine, neurology, and survivorship showed relatively robust telemedicine growth during peak COVID-19, but usage dropped significantly post-peak to 32%, 39%, and 27%, respectively (Table 2, Figure 1).
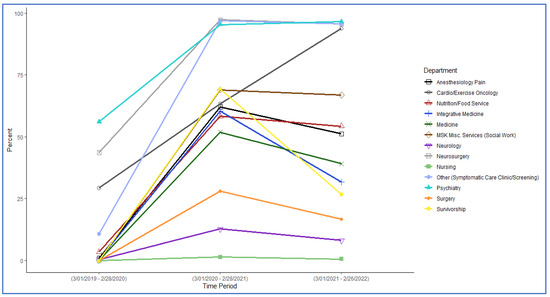
Figure 1.
Telemedicine usage by department before, during, and after the pandemic’s peak.
Trends by visit type: While few visits of any kind were conducted remotely pre-COVID-19, we observed variations in peak and post-peak telemedicine utilization by visit type. During the peak period, about half of new and follow-up visits, and nearly all other visits, occurred via telemedicine. Post-peak, less than a third of new and follow-up visits (8647 and 49,527, respectively) occurred remotely, but nearly all other visits continued to be conducted via telemedicine (Table 3). These visit-type usage patterns further diverged by department/specialty (Table 3). For instance, post-peak, few visits of any type occurred via telemedicine in surgery and survivorship. However, cardiology, nutrition, and psychiatry conducted the vast majority (in excess of 70%) of new, follow-up, and other visits by telemedicine. Integrative medicine, medicine, and social work also showed frequent telemedicine use (30% or greater) for all visit types. In anesthesiology and neurology, telemedicine was rare for new and other visits but common for follow-ups. In contrast, nursing showed the opposite pattern, with telemedicine used very often for new and other visits but rarely for follow-up consultations.

Table 3.
Peak and post-peak telemedicine usage, by visit type and department/specialty.
4. Discussion
Appropriately leveraged, telemedicine can enhance patient access, improve care coordination, and provide patient-centered services, but few studies have identified the acceptable contexts for remote cancer care. To this end, our study investigated trends in telemedicine utilization for breast and prostate cancer patients at a high-volume academic cancer center before, during, and after the peak of COVID-19.
Overall, we found an exponential, institution-wide increase in telemedicine visits during the peak COVID-19 period to the point where about half of feasible encounters were being delivered remotely. This indicates the adaptability of telemedicine in delivering care during emergencies and its potential to ensure the continuity of care in challenging circumstances. In the post-peak period, the proportion of feasible visits conducted via telemedicine dropped significantly but was still 30%, well above the pre-pandemic baseline. This is consistent with national trends, in which the arrival of vaccines, relaxation of restrictions, improved safety measures, policy changes, and patient and clinician preferences influenced this shift back to traditional care delivery methods [1,16,17,18,19,20]. In addition, as we hypothesized, the pandemic likely highlighted for many clinicians and patients numerous clinical contexts where remote care was suitable.
The specific decision about when to have an encounter via telemedicine as opposed to in person involves a multi-factorial set of considerations, including the goals of the encounter, time and cost to patients of an in-person experience, patient comfort with technology, and patient and physician preferences. Our data show that patients and providers are continuing to choose remote interactions as an acceptable and perhaps even preferable option. Understanding how each of these factors plays into the decision should be the focus of future research.
We also found dramatic variations by specialty and visit type in the proportion of visits provided remotely peak and post-peak. For instance, we found that the post-peak decline in telemedicine was mostly driven by drops in utilization by the departments of medicine, neurology, and survivorship; most other departments/specialties continued telemedicine use near or above peak frequencies. Psychiatry, social work, and nutrition departments, especially, demonstrated very high proportions of telemedicine visits both during and after the peak COVID-19 period. This finding suggests that these services successfully and widely embraced telemedicine as a means to deliver routine counseling, support, and education remotely—results that align with other studies [1,19,20,21,22]. In contrast, departments such as surgery and nursing showed relatively limited growth in telemedicine utilization during the peak period and correspondingly modest declines post-peak. This is likely due to the procedural and hands-on nature of care in these departments, which largely necessitate in-person visits for examinations, interventions, and complex treatments. These diverse findings underscore the importance of tailoring telemedicine strategies to match the specific needs and challenges faced by different specialists and their patients, as highlighted by prior studies [22,23]. Further research should examine this variability in greater depth to determine if there are best practices for telemedicine use that could be disseminated across institutions.
Our findings also suggest that telemedicine is used variably across the cancer care continuum. In other studies, it has been used effectively for follow-up and supportive care [1,19,24,25,26,27,28]. Similarly, we observed high utilization in departments like psychiatry, social work, and nutrition. These services largely involve ongoing communication, counseling, and education, which can often be effectively delivered through remote consultations. On the other hand, departments such as surgery and nursing, which often involve hands-on assessments and interventions at the diagnostic, treatment, and survivorship phases of care, may have more limited potential for telemedicine. Future studies are needed to understand how best to optimize the integration of telemedicine across the cancer care continuum.
Our study also found that departmental telemedicine use patterns varied significantly by visit type. Some departments showed relatively frequent telemedicine use for new, follow-up, and other visits, indicating that remote care is often an acceptable option in many contexts in these specialties. However, several departments diverged from this trend. Surgery and survivorship, for instance, rarely conducted any visit types remotely during or after the pandemic’s peak—suggesting in-person care is almost always considered by providers and patients to be optimal in these specialties. In anesthesiology and neurology, telemedicine visits were common only for follow-ups—reflecting a lesser need for in-person care among established patients receiving ongoing care. Nursing showed the opposite pattern, with telemedicine rarely used for follow-up consultations. Taken together, these diverse patterns extend prior findings [7,29,30,31,32,33,34] by suggesting important department- and visit-specific contexts across the continuum where telemedicine may be suitable.
There are some limitations to consider. First, we use post-peak telemedicine use as an indicator for acceptability; however, true acceptability might differ, and additional factors should be considered when making these determinations. Second, the visits included in the “other” visit category are diverse and include many different types of care. Future work is needed to better understand these visit categories and identify more nuanced clinical contexts for continued telemedicine use. Third, our data are from a single institution, and telemedicine use might be dictated by several factors such as decisions at the leadership level and technology availability.
Understanding the patterns of telemedicine use in different circumstances is crucial to determining how it might best be folded into routine care. To this end, our study identified specific variations in telemedicine use by department and visit type, suggesting distinct contexts where remote care may be frequently selected by patients and providers even when in-person options are available. Further research is warranted to explore the reasons behind these observed variations, identify context-specific barriers to telemedicine adoption, and assess patient and provider satisfaction with remote care delivery. These insights can inform the development of tailored telemedicine strategies that align with specific needs and contexts across the care continuum to enhance oncology care quality, access, cost-effectiveness, and ultimately patient outcomes.
5. Conclusions
This study highlights the disparate patterns of telemedicine adoption across different specialties and visit types for breast and prostate cancer patients, reflecting the diverse nature of oncology care. Future research is needed to explore the appropriate contexts for remote care across the continuum and to tailor telemedicine implementation strategies accordingly.
Author Contributions
Conceptualization, S.C., A.L.-S. and G.K.; methodology, A.L.-S., C.W. and K.S.; formal analysis, S.C., A.L.-S., C.W., K.S. and G.K.; data curation, Z.S. and N.C.; writing—original draft preparation, S.C.; writing—review and editing, S.C., A.L.-S. and G.K.; visualization, Z.S. and N.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748. It was also funded by NIH/NCI Cancer Moonshot Grant P50.
Institutional Review Board Statement
This study was part of a larger study, which was reviewed and approved by the IRB at MSKCC (IRB# 23-057).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available from the authors upon request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Sirintrapun, S.J.; Lopez, A.M. Telemedicine in Cancer Care. In American Society of Clinical Oncology Educational Book; American Society of Clinical Oncology: Alexandria, VA, USA, 2018; Volume 38, pp. 540–545. [Google Scholar]
- Shirke, M.M.; Shaikh, S.A.; Harky, A. Implications of Telemedicine in Oncology during the COVID-19 Pandemic. Acta Biomed. 2020, 91, e2020022. [Google Scholar]
- Daggubati, L.C.; Eichberg, D.G.; Ivan, M.E.; Hanft, S.; Mansouri, A.; Komotar, R.J.; D’Amico, R.S.; Zacharia, B.E. Telemedicine for Outpatient Neurosurgical Oncology Care: Lessons Learned for the Future During the COVID-19 Pandemic. World Neurosurg. 2020, 139, e859–e863. [Google Scholar] [CrossRef]
- Bizot, A.; Karimi, M.; Rassy, E.; Heudel, P.E.; Levy, C.; Vanlemmens, L.; Uzan, C.; Deluche, E.; Genet, D.; Saghatchian, M.; et al. Multicenter evaluation of breast cancer patients’ satisfaction and experience with oncology telemedicine visits during the COVID-19 pandemic. Br. J. Cancer 2021, 125, 1486–1493. [Google Scholar] [CrossRef]
- Doolittle, G.C.; Spaulding, A.O. Providing access to oncology care for rural patients via telemedicine. J. Oncol. Pract. 2006, 2, 228. [Google Scholar] [CrossRef] [PubMed]
- Shaverdian, N.; Gillespie, E.F.; Cha, E.; Kim, S.Y.; Benvengo, S.; Chino, F.; Kang, J.J.; Li, Y.; Atkinson, T.M.; Lee, N.; et al. Impact of telemedicine on patient satisfaction and perceptions of care quality in radiation oncology. J. Natl. Compr. Cancer Netw. 2021, 19, 1174–1180. [Google Scholar] [CrossRef]
- Pang, N.-Q.; Lau, J.; Fong, S.-Y.; Wong, C.Y.-H.; Tan, K.-K. Telemedicine acceptance among older adult patients with cancer: Scoping review. J. Med. Internet Res. 2022, 24, e28724. [Google Scholar] [CrossRef] [PubMed]
- Orazem, M.; Oblak, I.; Spanic, T.; Ratosa, I. Telemedicine in Radiation Oncology Post–COVID-19 Pandemic: There Is No Turning Back; Elsevier: Amsterdam, The Netherlands, 2020; pp. 411–415. [Google Scholar]
- West, H.J.; Barzi, A.; Wong, D. Telemedicine in Cancer Care Beyond the COVID-19 Pandemic: Oncology 2.0? Curr. Oncol. Rep. 2022, 24, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.Y.; Mehrotra, A.; Huskamp, H.A.; Uscher-Pines, L.; Ganguli, I.; Barnett, M.L. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern. Med. 2021, 181, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Ftouni, R.; AlJardali, B.; Hamdanieh, M.; Ftouni, L.; Salem, N. Challenges of Telemedicine during the COVID-19 pandemic: A systematic review. BMC Med. Inf. Decis. Mak. 2022, 22, 207. [Google Scholar] [CrossRef]
- Panet, F.; Tétreault-Langlois, M.; Morin, V.; Sultanem, K.; Melnychuk, D.; Panasci, L. The risks associated with the widespread use of telemedicine in oncology: Four cases and review of the literature. Cancer Rep. 2022, 5, e1531. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef]
- Xia, C.; Dong, X.; Li, H.; Cao, M.; Sun, D.; He, S.; Yang, F.; Yan, X.; Zhang, S.; Li, N.; et al. Cancer statistics in China and United States, 2022: Profiles, trends, and determinants. Chin. Med. J. 2022, 135, 584–590. [Google Scholar] [CrossRef]
- De, B.; Fu, S.; Chen, Y.; Das, P.; Ku, K.; Maroongroge, S.; Woodhouse, K.D.; Hoffman, K.E.; Nguyen, Q.; Reed, V.K.; et al. Patient, physician, and policy factors underlying variation in use of telemedicine for radiation oncology cancer care. Cancer Med. 2022, 11, 2096–2105. [Google Scholar] [CrossRef]
- Lee, E.C.; Grigorescu, V.; Enogieru, I.; Smith, S.R.; Samson, L.W.; Conmy, A.; De Lew, N. Updated National Survey Trends in Telehealth Utilization and Modality: 2021–2022 (Issue Brief No. HP-2023-09); Office of the Assistant Secretary for Planning and Evaluation, Ed.; US Department of Health and Human Services: Washington, DC, USA, 2023.
- Donner, C.F.; ZuWallack, R.; Nici, L. The Role of Telemedicine in Extending and Enhancing Medical Management of the Patient with Chronic Obstructive Pulmonary Disease. Medicina 2021, 57, 726. [Google Scholar] [CrossRef]
- Chan, R.; Crichton, M.; Crawford-Williams, F.; Agbejule, O.; Yu, K.; Hart, N.; Alves, F.d.A.; Ashbury, F.; Eng, L.; Fitch, M.; et al. The efficacy, challenges, and facilitators of telemedicine in post-treatment cancer survivorship care: An overview of systematic reviews. Ann. Oncol. 2021, 32, 1552–1570. [Google Scholar] [CrossRef]
- Doarn, C.R. Telemedicine and psychiatry-a natural match. Mhealth 2018, 4, 60. [Google Scholar] [CrossRef] [PubMed]
- Riemer-Reiss, M.L. Utilizing Distance Technology for Mental Health Counseling. J. Ment. Health Couns. 2000, 22, 189. [Google Scholar]
- ConnDrake, C.; Lian, T.; Cameron, B.; Medynskaya, K.; Bosworth, H.B.; Shah, K. Understanding Telemedicine’s “New Normal”: Variations in Telemedicine Use by Specialty Line and Patient Demographics. Telemed. e-Health 2022, 28, 51–59. [Google Scholar]
- Sheets, L.R.; Wallach, E.; Khairat, S.; Mutrux, R.; Edison, K.; Becevic, M. Similarities and Differences Between Rural and Urban Telemedicine Utilization. Perspect. Health Inf. Manag. 2021, 18, 1e. [Google Scholar]
- Donelan, K.; Barreto, E.A.; Sossong, S.; Michael, C.; Estrada, J.J.; Cohen, A.B.; Wozniak, J.; Schwamm, L.H. Patient and clinician experiences with telehealth for patient follow-up care. Am. J. Manag. Care 2019, 25, 40–44. [Google Scholar]
- Hennemann-Krause, L.; Lopes, A.J.; Araújo, J.A.; Petersen, E.M.; Nunes, R.A. The assessment of telemedicine to support outpatient palliative care in advanced cancer. Palliat. Support. Care 2015, 13, 1025–1030. [Google Scholar] [CrossRef] [PubMed]
- Spelten, E.; Hardman, R.; Pike, K.; Yuen, E.; Wilson, C. Best practice in the implementation of telehealth-based supportive cancer care: Using research evidence and discipline-based guidance. Patient Educ. Couns. 2021, 104, 2682–2699. [Google Scholar] [CrossRef]
- Worster, B.; Swartz, K. Telemedicine and Palliative Care: An Increasing Role in Supportive Oncology. Curr. Oncol. Rep. 2017, 19, 37. [Google Scholar] [CrossRef] [PubMed]
- Uppal, A.; Kothari, A.N.; Scally, C.P.; Roland, C.L.; Bednarski, B.K.; Katz, M.H.; Vauthey, J.-N.; Chang, G.J.; in collaboration with the D3CODE Team. Adoption of Telemedicine for Postoperative Follow-Up After Inpatient Cancer-Related Surgery. JCO Oncol. Pract. 2022, 18, e1091–e1099. [Google Scholar] [CrossRef]
- Sitter, K.E.; Wong, D.H.; Bolton, R.E.; Vimalananda, V.G. Clinical Appropriateness of Telehealth: A Qualitative Study of Endocrinologists’ Perspectives. J. Endocr. Soc. 2022, 6, bvac089. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Parks, A.M.; Sousa, J.; Raja, P.; Mehrotra, A.; Huskamp, H.A.; Busch, A.B. Appropriateness of Telemedicine Versus In-Person Care: A Qualitative Exploration of Psychiatrists’ Decision Making. Psychiatr. Serv. 2022, 73, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Hasson, S.P.; Waissengrin, B.; Shachar, E.; Hodruj, M.; Fayngor, R.; Brezis, M.; Nikolaevski-Berlin, A.; Pelles, S.; Safra, T.; Geva, R.; et al. Rapid implementation of telemedicine during the COVID-19 pandemic: Perspectives and preferences of patients with cancer. Oncologist 2021, 26, e679–e685. [Google Scholar] [CrossRef]
- Tripepi, M.; Pizzocaro, E.; Giardino, A.; Frigerio, I.; Guglielmi, A.; Butturini, G. Telemedicine and pancreatic cancer: A systematic review. Telemed. e-Health 2023, 29, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Cha, E.E.; Lynch, K.; Cahlon, O.; Gomez, D.R.; Shaverdian, N.; Gillespie, E.F. Radiation Oncologist Perceptions of Telemedicine from Consultation to Treatment Planning: A Mixed-Methods Study; Elsevier: Amsterdam, The Netherlands, 2020; pp. 421–429. [Google Scholar]
- Tevaarwerk, A.J.; Chandereng, T.; Osterman, T.; Arafat, W.; Smerage, J.; Polubriaginof, F.C.G.; Heinrichs, T.; Sugalski, J.; Martin, D.B. Oncologist perspectives on telemedicine for patients with cancer: A National Comprehensive Cancer Network survey. JCO Oncol. Pract. 2021, 17, e1318–e1326. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).