A Review of Biomarkers and Their Clinical Impact in Resected Early-Stage Non-Small-Cell Lung Cancer
Abstract
Simple Summary
Abstract
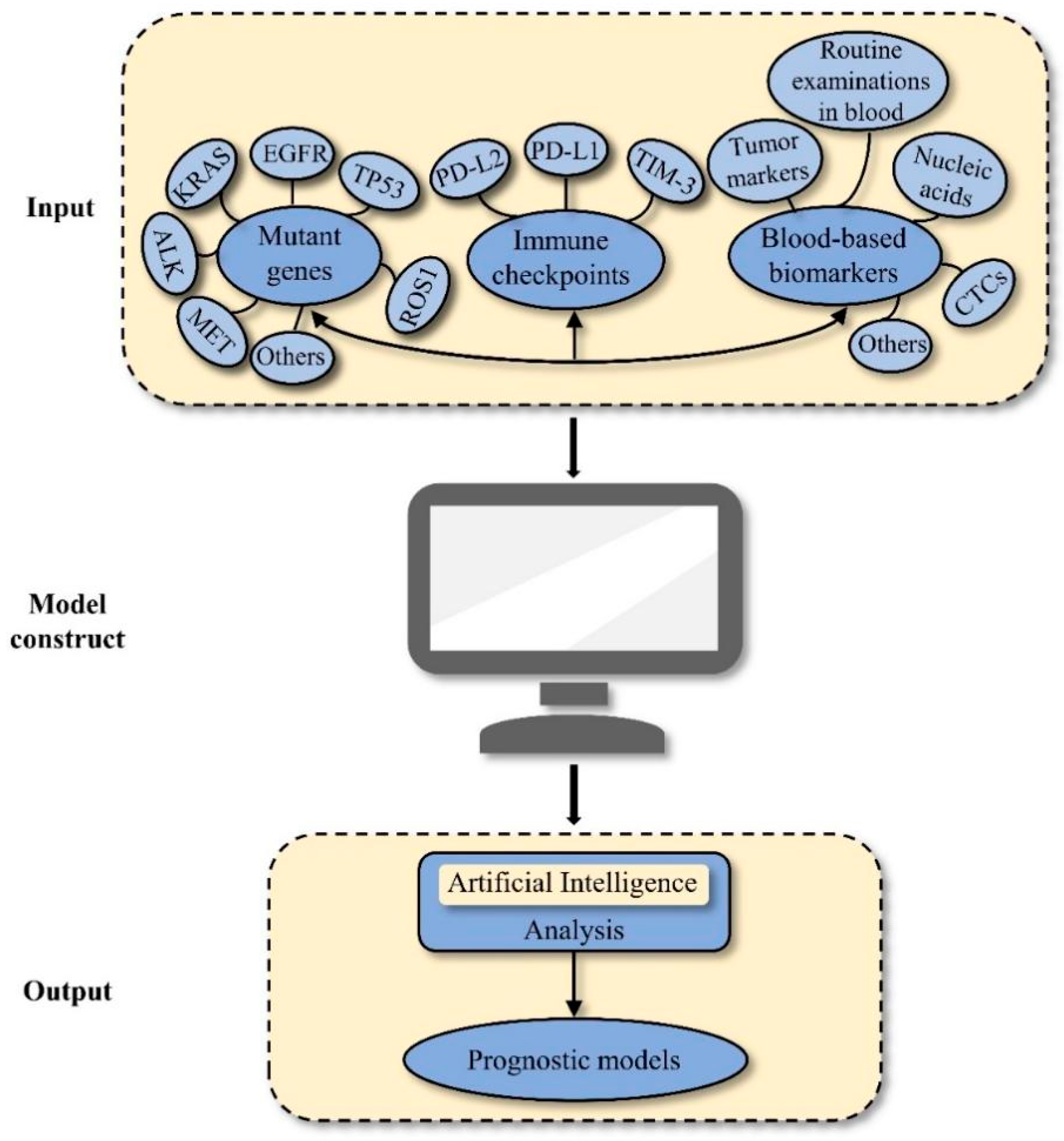
1. Introduction
2. Methods
3. Results
3.1. Genetic Alterations
3.1.1. EGFR Alterations
3.1.2. KRAS Alterations
3.1.3. ALK Alterations
3.1.4. MET Alterations
3.1.5. ROS1 Alterations
3.1.6. TP53 Alterations
3.1.7. Other Genetic Alterations
3.2. Immune-Related Indicators
3.2.1. PD-L1
3.2.2. Other Immune-Related Markers
3.3. Blood-Based Biomarkers
3.3.1. CTCs
3.3.2. Routine Examinations in Blood
Hemoglobin (Hb)
Platelet (PLT)
White Blood Cells
3.3.3. Circulating Nucleic Acids
Circulating Tumour DNA (ctDNA)
MicroRNAs (MiRNAs)
3.3.4. Tumour Markers
Carcinoembryonic Antigen (CEA)
CYFRA 21-1
Other Tumour Markers
3.3.5. Other Blood Biomarkers
C-Reactive Protein (CRP)
Fibrinogen and D-Dimer
Albumin
Osteopontin (OPN)
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Duma, N.; Santana-Davila, R.; Molina, J.R. Non-Small Cell Lung Cancer: Epidemiology, Screening, Diagnosis, and Treatment. Mayo Clin. Proc. 2019, 94, 1623–1640. [Google Scholar] [CrossRef] [PubMed]
- Howington, J.A.; Blum, M.G.; Chang, A.C.; Balekian, A.A.; Murthy, S.C. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013, 143 (Suppl. S5), e278S–e313S. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Asamura, H.; Bankier, A.A.; Beasley, M.B.; Detterbeck, F.; Flieder, D.B.; Goo, J.M.; MacMahon, H.; Naidich, D.; Nicholson, A.G.; et al. The IASLC Lung Cancer Staging Project: Proposals for Coding T Categories for Subsolid Nodules and Assessment of Tumor Size in Part-Solid Tumors in the Forthcoming Eighth Edition of the TNM Classification of Lung Cancer. J. Thorac. Oncol. 2016, 11, 1204–1223. [Google Scholar] [CrossRef] [PubMed]
- da Cunha Santos, G.; Shepherd, F.A.; Tsao, M.S. EGFR mutations and lung cancer. Annu. Rev. Pathol. 2011, 6, 49–69. [Google Scholar] [CrossRef]
- Reck, M.; Carbone, D.P.; Garassino, M.; Barlesi, F. Targeting KRAS in non-small-cell lung cancer: Recent progress and new approaches. Ann. Oncol. 2021, 32, 1101–1110. [Google Scholar] [CrossRef]
- Yu, H.; Boyle, T.A.; Zhou, C.; Rimm, D.L.; Hirsch, F.R. PD-L1 Expression in Lung Cancer. J. Thorac. Oncol. 2016, 11, 964–975. [Google Scholar] [CrossRef]
- Dyck, L.; Mills, K.H.G. Immune checkpoints and their inhibition in cancer and infectious diseases. Eur. J. Immunol. 2017, 47, 765–779. [Google Scholar] [CrossRef]
- Takahashi, T.; Sakai, K.; Kenmotsu, H.; Yoh, K.; Daga, H.; Ohira, T.; Ueno, T.; Aoki, T.; Hayashi, H.; Yamazaki, K.; et al. Predictive value of EGFR mutation in non-small-cell lung cancer patients treated with platinum doublet postoperative chemotherapy. Cancer Sci. 2022, 113, 287–296. [Google Scholar] [CrossRef]
- Deng, C.; Zhang, Y.; Ma, Z.; Fu, F.; Deng, L.; Li, Y.; Chen, H. Prognostic value of epidermal growth factor receptor gene mutation in resected lung adenocarcinoma. J. Thorac. Cardiovasc. Surg. 2021, 162, 664–674.e7. [Google Scholar] [CrossRef]
- Ito, M.; Miyata, Y.; Tsutani, Y.; Ito, H.; Nakayama, H.; Imai, K.; Ikeda, N.; Okada, M. Positive EGFR mutation status is a risk of recurrence in pN0-1 lung adenocarcinoma when combined with pathological stage and histological subtype: A retrospective multi-center analysis. Lung Cancer 2020, 141, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Liu, Z.; Wang, Y.; Zhang, Y.; Qian, F.; Lu, J.; Wang, H.; Gu, P.; Hu, M.; Chen, Y.; et al. The clinicopathological and molecular characteristics of resected EGFR-mutant lung adenocarcinoma. Cancer Med. 2022, 11, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Shimizu, S.; Okuda, K.; Kawano, O.; Yukiue, H.; Yano, M.; Fujii, Y. Epidermal growth factor receptor gene amplification in surgical resected Japanese lung cancer. Lung Cancer 2009, 64, 295–300. [Google Scholar] [CrossRef]
- Isaka, T.; Nakayama, H.; Ito, H.; Yokose, T.; Yamada, K.; Masuda, M. Impact of the epidermal growth factor receptor mutation status on the prognosis of recurrent adenocarcinoma of the lung after curative surgery. BMC Cancer 2018, 18, 959. [Google Scholar] [CrossRef] [PubMed]
- Izar, B.; Sequist, L.; Lee, M.; Muzikansky, A.; Heist, R.; Iafrate, J.; Dias-Santagata, D.; Mathisen, D.; Lanuti, M. The impact of EGFR mutation status on outcomes in patients with resected stage I non-small cell lung cancers. Ann. Thorac. Surg. 2013, 96, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.-P.; Wu, H.-D.I.; Chang, J.W.-C.; Wu, Y.-C.; Yang, H.-Y.; Chen, Y.-T.; Hsieh, W.-Y.; Chen, Y.-T.; Chen, Y.-R.; Huang, S.-F. Prognostic implications of epidermal growth factor receptor and KRAS gene mutations and epidermal growth factor receptor gene copy numbers in patients with surgically resectable non-small cell lung cancer in Taiwan. J. Thorac. Oncol. 2010, 5, 1175–1184. [Google Scholar] [CrossRef]
- Isaka, T.; Ito, H.; Nakayama, H.; Yokose, T.; Yamada, K.; Masuda, M. Effect of epidermal growth factor receptor mutation on early-stage non-small cell lung cancer according to the 8th TNM classification. Lung Cancer 2020, 145, 111–118. [Google Scholar] [CrossRef]
- Na, I.I.; Rho, J.K.; Choi, Y.J.; Kim, C.H.; Koh, J.S.; Ryoo, B.-Y.; Yang, S.H.; Lee, J.C. Clinical features reflect exon sites of EGFR mutations in patients with resected non-small-cell lung cancer. J. Korean Med. Sci. 2007, 22, 393–399. [Google Scholar] [CrossRef]
- Renaud, S.; Seitlinger, J.; Guerrera, F.; Reeb, J.; Beau-Faller, M.; Voegeli, A.-C.; Siat, J.; Clément-Duchêne, C.; Tiotiu, A.; Santelmo, N.; et al. Prognostic Value of Exon 19 Versus 21 EGFR Mutations Varies According to Disease Stage in Surgically Resected Non-small Cell Lung Cancer Adenocarcinoma. Ann. Surg. Oncol. 2018, 25, 1069–1078. [Google Scholar] [CrossRef]
- Isaka, T.; Nakayama, H.; Yokose, T.; Ito, H.; Miyagi, Y.; Matsuzaki, T.; Nagata, M.; Furumoto, H.; Nishii, T.; Katayama, K.; et al. Epidermal Growth Factor Receptor Mutations and Prognosis in Pathologic N1-N2 Pulmonary Adenocarcinoma. Ann. Thorac. Surg. 2016, 102, 1821–1828. [Google Scholar] [CrossRef]
- Hayasaka, K.; Shiono, S.; Matsumura, Y.; Yanagawa, N.; Suzuki, H.; Abe, J.; Sagawa, M.; Sakurada, A.; Katahira, M.; Takahashi, S.; et al. Epidermal Growth Factor Receptor Mutation as a Risk Factor for Recurrence in Lung Adenocarcinoma. Ann. Thorac. Surg. 2018, 105, 1648–1654. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, Y.; Kawaguchi, T.; Watanabe, M.; Isa, S.-I.; Ando, M.; Tamiya, A.; Kubo, A.; Kitagawa, C.; Yoshimoto, N.; Koh, Y. Prognostic impact of pretreatment T790M mutation on outcomes for patients with resected, EGFR-mutated, non-small cell lung cancer. BMC Cancer 2022, 22, 775. [Google Scholar] [CrossRef] [PubMed]
- Sonnweber, B.; Dlaska, M.; Skvortsov, S.; Dirnhofer, S.; Schmid, T.; Hilbe, W. High predictive value of epidermal growth factor receptor phosphorylation but not of EGFRvIII mutation in resected stage I non-small cell lung cancer (NSCLC). J. Clin. Pathol. 2006, 59, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.D.; Caso, R.; Tan, K.S.; Mastrogiacomo, B.; Sanchez-Vega, F.; Liu, Y.; Connolly, J.G.; Murciano-Goroff, Y.R.; Bott, M.J.; Adusumilli, P.S.; et al. Mutation is Associated with Increased Risk of Recurrence in Surgically Resected Lung Adenocarcinoma. Clin. Cancer Res. 2021, 27, 2604–2612. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, S.P.; Janjigian, Y.Y.; Ahye, N.; Riely, G.J.; Chaft, J.E.; Sima, C.S.; Shen, R.; Zheng, J.; Dycoco, J.; Kris, M.G.; et al. Distinct clinical course of EGFR-mutant resected lung cancers: Results of testing of 1118 surgical specimens and effects of adjuvant gefitinib and erlotinib. J. Thorac. Oncol. 2012, 7, 1815–1822. [Google Scholar] [CrossRef]
- Izar, B.; Zhou, H.; Heist, R.S.; Azzoli, C.G.; Muzikansky, A.; Scribner, E.E.F.; Bernardo, L.A.; Dias-Santagata, D.; Iafrate, A.J.; Lanuti, M. The prognostic impact of KRAS, its codon and amino acid specific mutations, on survival in resected stage I lung adenocarcinoma. J. Thorac. Oncol. 2014, 9, 1363–1369. [Google Scholar] [CrossRef]
- Kadota, K.; Sima, C.S.; Arcila, M.E.; Hedvat, C.; Kris, M.G.; Jones, D.R.; Adusumilli, P.S.; Travis, W.D. KRAS Mutation Is a Significant Prognostic Factor in Early-stage Lung Adenocarcinoma. Am. J. Surg. Pathol. 2016, 40, 1579–1590. [Google Scholar] [CrossRef]
- Kneuertz, P.J.; Carbone, D.P.; D’Souza, D.M.; Shilo, K.; Abdel-Rasoul, M.; Zhao, W.; Williams, T.M.; Jones, D.; Merritt, R.E. Prognostic value and therapeutic implications of expanded molecular testing for resected early stage lung adenocarcinoma. Lung Cancer 2020, 143, 60–66. [Google Scholar] [CrossRef]
- Ayyoub, M.; Memeo, L.; Alvarez-Fernández, E.; Colarossi, C.; Costanzo, R.; Aiello, E.; Martinetti, D.; Valmori, D. Assessment of MAGE-A expression in resected non-small cell lung cancer in relation to clinicopathologic features and mutational status of EGFR and KRAS. Cancer Immunol. Res. 2014, 2, 943–948. [Google Scholar] [CrossRef]
- Fujibayashi, Y.; Tane, S.; Kitazume, M.; Kuroda, S.; Kimura, K.; Kitamura, Y.; Nishio, W. Resected stage I anaplastic lymphoma kinase-positive lung adenocarcinoma has a negative impact on recurrence-free survival. Thorac. Cancer 2022, 13, 1109–1116. [Google Scholar] [CrossRef]
- Chaft, J.E.; Dagogo-Jack, I.; Santini, F.C.; Eng, J.; Yeap, B.Y.; Izar, B.; Chin, E.; Jones, D.R.; Kris, M.G.; Shaw, A.T.; et al. Clinical outcomes of patients with resected, early-stage ALK-positive lung cancer. Lung Cancer 2018, 122, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Matsuura, Y.; Ninomiya, H.; Ichinose, J.; Nakao, M.; Okumura, S.; Nishio, M.; Mun, M. Prognostic impact and distinctive characteristics of surgically resected anaplastic lymphoma kinase-rearranged lung adenocarcinoma. J. Thorac. Cardiovasc. Surg. 2022, 163, 441–451.e1. [Google Scholar] [CrossRef] [PubMed]
- Tao, H.; Shi, L.; Zhou, A.; Li, H.; Gai, F.; Huang, Z.; Che, N.; Liu, Z. Distribution of EML4-ALK fusion variants and clinical outcomes in patients with resected non-small cell lung cancer. Lung Cancer 2020, 149, 154–161. [Google Scholar] [CrossRef]
- Sun, J.-M.; Lira, M.; Pandya, K.; Choi, Y.-L.; Ahn, J.S.; Mao, M.; Han, J.; Park, K.; Ahn, M.-J.; Kim, J. Clinical characteristics associated with ALK rearrangements in never-smokers with pulmonary adenocarcinoma. Lung Cancer 2014, 83, 259–264. [Google Scholar] [CrossRef]
- Paik, J.H.; Choi, C.-M.; Kim, H.; Jang, S.J.; Choe, G.; Kim, D.K.; Kim, H.J.; Yoon, H.; Lee, C.-T.; Jheon, S.; et al. Clinicopathologic implication of ALK rearrangement in surgically resected lung cancer: A proposal of diagnostic algorithm for ALK-rearranged adenocarcinoma. Lung Cancer 2012, 76, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.-H.; Lee, I.H.; Lee, J.E.; Hong, S.H.; Kim, T.-J.; Lee, K.-Y.; Kim, Y.K.; Kim, S.J.; Sung, S.W.; Park, J.K.; et al. Clinical Significance of C-MET Overexpression and Epidermal Growth Factor Receptor Mutation in Platinum-Based Adjuvant Chemotherapy Outcome in Surgically Resected Lung Adenocarcinoma. Ann. Surg. Oncol. 2017, 24, 770–777. [Google Scholar] [CrossRef]
- Cappuzzo, F.; Marchetti, A.; Skokan, M.; Rossi, E.; Gajapathy, S.; Felicioni, L.; Del Grammastro, M.; Sciarrotta, M.G.; Buttitta, F.; Incarbone, M.; et al. Increased MET gene copy number negatively affects survival of surgically resected non-small-cell lung cancer patients. J. Clin. Oncol. 2009, 27, 1667–1674. [Google Scholar] [CrossRef]
- Bubendorf, L.; Dafni, U.; Schöbel, M.; Finn, S.P.; Tischler, V.; Sejda, A.; Marchetti, A.; Thunnissen, E.; Verbeken, E.K.; Warth, A.; et al. Prevalence and clinical association of MET gene overexpression and amplification in patients with NSCLC: Results from the European Thoracic Oncology Platform (ETOP) Lungscape project. Lung Cancer 2017, 111, 143–149. [Google Scholar] [CrossRef]
- Lee, G.D.; Lee, S.E.; Oh, D.-Y.; Yu, D.-B.; Jeong, H.M.; Kim, J.; Hong, S.; Jung, H.S.; Oh, E.; Song, J.-Y.; et al. MET Exon 14 Skipping Mutations in Lung Adenocarcinoma: Clinicopathologic Implications and Prognostic Values. J. Thorac. Oncol. 2017, 12, 1233–1246. [Google Scholar] [CrossRef]
- Kim, I.A.; Hur, J.Y.; Kim, H.J.; Park, J.H.; Hwang, J.J.; Lee, S.A.; Lee, S.E.; Kim, W.S.; Lee, K.Y. Targeted Next-Generation Sequencing Analysis for Recurrence in Early-Stage Lung Adenocarcinoma. Ann. Surg. Oncol. 2021, 28, 3983–3993. [Google Scholar] [CrossRef]
- Chen, Y.-F.; Hsieh, M.-S.; Wu, S.-G.; Chang, Y.-L.; Shih, J.-Y.; Liu, Y.-N.; Tsai, M.-F.; Tsai, T.-H.; Yu, C.-J.; Yang, J.C.-H.; et al. Clinical and the prognostic characteristics of lung adenocarcinoma patients with ROS1 fusion in comparison with other driver mutations in East Asian populations. J. Thorac. Oncol. 2014, 9, 1171–1179. [Google Scholar] [CrossRef] [PubMed]
- Jao, K.; Tomasini, P.; Kamel-Reid, S.; Korpanty, G.J.; Mascaux, C.; Sakashita, S.; Labbé, C.; Leighl, N.B.; Liu, G.; Feld, R.; et al. The prognostic effect of single and multiple cancer-related somatic mutations in resected non-small-cell lung cancer. Lung Cancer 2018, 123, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Wang, Y.; Ren, F.; Li, X.; Ren, D.; Dong, M.; Chen, G.; Song, Z.; Chen, J. Impact of genetic alterations on outcomes of patients with stage I nonsmall cell lung cancer: An analysis of the cancer genome atlas data. Cancer Med. 2020, 9, 7686–7694. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Sanchez-Vega, F.; Caso, R.; Tan, K.S.; Brandt, W.S.; Jones, G.D.; Yan, S.; Adusumilli, P.S.; Bott, M.; Huang, J.; et al. Analysis of Tumor Genomic Pathway Alterations Using Broad-Panel Next-Generation Sequencing in Surgically Resected Lung Adenocarcinoma. Clin. Cancer Res. 2019, 25, 7475–7484. [Google Scholar] [CrossRef] [PubMed]
- Ludovini, V.; Pistola, L.; Gregorc, V.; Floriani, I.; Rulli, E.; Piattoni, S.; Di Carlo, L.; Semeraro, A.; Darwish, S.; Tofanetti, F.R.; et al. Plasma DNA, microsatellite alterations, and p53 tumor mutations are associated with disease-free survival in radically resected non-small cell lung cancer patients: A study of the perugia multidisciplinary team for thoracic oncology. J. Thorac. Oncol. 2008, 3, 365–373. [Google Scholar] [CrossRef]
- Laudanski, J.; Niklinska, W.; Burzykowski, T.; Chyczewski, L.; Niklinski, J. Prognostic significance of p53 and bcl-2 abnormalities in operable nonsmall cell lung cancer. Eur. Respir. J. 2001, 17, 660–666. [Google Scholar] [CrossRef]
- McGowan, M.; Hoven, A.S.; Lund-Iversen, M.; Solberg, S.; Helland, Å.; Hirsch, F.R.; Brustugun, O.T. PIK3CA mutations as prognostic factor in squamous cell lung carcinoma. Lung Cancer 2017, 103, 52–57. [Google Scholar] [CrossRef]
- Song, Z.; Yu, X.; Zhang, Y. Mutation and prognostic analyses of PIK3CA in patients with completely resected lung adenocarcinoma. Cancer Med. 2016, 5, 2694–2700. [Google Scholar] [CrossRef]
- Imperatori, A.; Sahnane, N.; Rotolo, N.; Franzi, F.; Nardecchia, E.; Libera, L.; Romualdi, C.; Cattoni, M.; Sessa, F.; Dominioni, L.; et al. LINE-1 hypomethylation is associated to specific clinico-pathological features in Stage I non-small cell lung cancer. Lung Cancer 2017, 108, 83–89. [Google Scholar] [CrossRef]
- Lee, J.S.; Kim, H.R.; Lee, C.Y.; Shin, M.; Shim, H.S. EGFR and TTF-1 gene amplification in surgically resected lung adenocarcinomas: Clinicopathologic significance and effect on response to EGFR-tyrosine kinase inhibitors in recurred cases. Ann. Surg. Oncol. 2013, 20, 3015–3022. [Google Scholar] [CrossRef]
- Liu, D.-H.; Zhao, Z.-R.; Lin, Y.-B.; Zhou, W.-J.; Hou, J.-Y.; Ye, Z.-H.; Long, H. Prognostic Effect of TP53 and PKD Co-Mutations in Patients with Resected Epidermal Growth Factor Receptor-Mutated Lung Adenocarcinoma. Ann. Surg. Oncol. 2019, 26, 1934–1941. [Google Scholar] [CrossRef] [PubMed]
- Lemmon, M.A.; Schlessinger, J.; Ferguson, K.M. The EGFR family: Not so prototypical receptor tyrosine kinases. Cold Spring Harb. Perspect. Biol. 2014, 6, a020768. [Google Scholar] [CrossRef] [PubMed]
- London, M.; Gallo, E. Epidermal growth factor receptor (EGFR) involvement in epithelial-derived cancers and its current antibody-based immunotherapies. Cell Biol. Int. 2020, 44, 1267–1282. [Google Scholar] [CrossRef]
- Wheeler, D.L.; Dunn, E.F.; Harari, P.M. Understanding resistance to EGFR inhibitors-impact on future treatment strategies, nature reviews. Clin. Oncol. 2010, 7, 493–507. [Google Scholar]
- Lai, Y.; Zhang, Z.; Li, J.; Sun, D.; Zhou, Y.A.; Jiang, T.; Han, Y.; Huang, L.; Zhu, Y.; Li, X.; et al. EGFR mutations in surgically resected fresh specimens from 697 consecutive Chinese patients with non-small cell lung cancer and their relationships with clinical features. Int. J. Mol. Sci. 2013, 14, 24549–24559. [Google Scholar] [CrossRef] [PubMed]
- Midha, A.; Dearden, S.; McCormack, R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: A systematic review and global map by ethnicity (mutMapII). Am. J. Cancer Res. 2015, 5, 2892–2911. [Google Scholar]
- Herbst, R.S.; Wu, Y.-L.; John, T.; Grohe, C.; Majem, M.; Wang, J.; Kato, T.; Goldman, J.W.; Laktionov, K.; Kim, S.-W.; et al. Adjuvant Osimertinib for Resected EGFR-Mutated Stage IB–IIIA Non-Small-Cell Lung Cancer: Updated Results From the Phase III Randomized ADAURA Trial. J. Clin. Oncol. 2023, 41, 1830–1840. [Google Scholar] [CrossRef]
- Tsuboi, M.; Herbst, R.S.; John, T.; Kato, T.; Majem, M.; Grohé, C.; Wang, J.; Goldman, J.W.; Lu, S.; Su, W.-C.; et al. Overall Survival with Osimertinib in Resected EGFR-Mutated NSCLC. N. Engl. J. Med. 2023, 389, 137–147. [Google Scholar] [CrossRef]
- Zhong, W.-Z.; Wang, Q.; Mao, W.-M.; Xu, S.-T.; Wu, L.; Shen, Y.; Liu, Y.-Y.; Chen, C.; Cheng, Y.; Xu, L.; et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II–IIIA (N1-N2) EGFR-mutant NSCLC (ADJUVANT/CTONG1104): A randomised, open-label, phase 3 study. Lancet Oncol. 2018, 19, 139–148. [Google Scholar] [CrossRef]
- Zhong, W.-Z.; Chen, K.-N.; Chen, C.; Gu, C.-D.; Wang, J.; Yang, X.-N.; Mao, W.-M.; Wang, Q.; Qiao, G.-B.; Cheng, Y.; et al. Erlotinib Versus Gemcitabine Plus Cisplatin as Neoadjuvant Treatment of Stage IIIA-N2 EGFR-Mutant Non-Small-Cell Lung Cancer (EMERGING-CTONG 1103): A Randomized Phase II Study. J. Clin. Oncol. 2019, 37, 2235–2245. [Google Scholar] [CrossRef]
- Malumbres, M.; Barbacid, M. RAS oncogenes: The first 30 years. Nat. Rev. Cancer 2003, 3, 459–465. [Google Scholar] [CrossRef]
- Meng, D.; Yuan, M.; Li, X.; Chen, L.; Yang, J.; Zhao, X.; Ma, W.; Xin, J. Prognostic value of K-RAS mutations in patients with non-small cell lung cancer: A systematic review with meta-analysis. Lung Cancer 2013, 81, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.W.; Kirstein, M.N.; Valentine, M.B.; Dittmer, K.G.; Shapiro, D.N.; Saltman, D.L.; Look, A.T. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science 1994, 263, 1281–1284. [Google Scholar] [CrossRef] [PubMed]
- Hallberg, B.; Palmer, R.H. The role of the ALK receptor in cancer biology. Ann. Oncol. 2016, 27 (Suppl. S3), iii4–iii15. [Google Scholar] [CrossRef]
- Koch, J.P.; Aebersold, D.M.; Zimmer, Y.; Medová, M. MET targeting: Time for a rematch. Oncogene 2020, 39, 2845–2862. [Google Scholar] [CrossRef] [PubMed]
- Drilon, A.; Jenkins, C.; Iyer, S.; Schoenfeld, A.; Keddy, C.; Davare, M.A. ROS1-dependent cancers—Biology, diagnostics and therapeutics. Nature reviews. Clin. Oncol. 2021, 18, 35–55. [Google Scholar]
- Borrero, L.J.H.; El-Deiry, W.S. Tumor suppressor p53: Biology, signaling pathways, and therapeutic targeting. Biochim. Biophys. Acta Rev. Cancer 2021, 1876, 188556. [Google Scholar] [CrossRef]
- Ibáñez, C.F. Structure and physiology of the RET receptor tyrosine kinase. Cold Spring Harb. Perspect. Biol. 2013, 5, a009134. [Google Scholar] [CrossRef] [PubMed]
- Zaman, A.; Wu, W.; Bivona, T.G. Targeting Oncogenic BRAF: Past, Present, and Future. Cancers 2019, 11, 1197. [Google Scholar] [CrossRef]
- Cha, Y.J.; Kim, H.R.; Lee, C.Y.; Cho, B.C.; Shim, H.S. Clinicopathological and prognostic significance of programmed cell death ligand-1 expression in lung adenocarcinoma and its relationship with p53 status. Lung Cancer 2016, 97, 73–80. [Google Scholar] [CrossRef]
- Kim, M.; Chung, Y.S.; Kim, K.A.; Shim, H.S. Prognostic factors of acinar- or papillary-predominant adenocarcinoma of the lung. Lung Cancer 2019, 137, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Takamori, S.; Takada, K.; Azuma, K.; Jogo, T.; Shimokawa, M.; Toyokawa, G.; Hirai, F.; Tagawa, T.; Kawahara, A.; Akiba, J.; et al. Prognostic Impact of Programmed Death-Ligand 2 Expression in Primary Lung Adenocarcinoma Patients. Ann. Surg. Oncol. 2019, 26, 1916–1924. [Google Scholar] [CrossRef] [PubMed]
- Takada, K.; Okamoto, T.; Shoji, F.; Shimokawa, M.; Akamine, T.; Takamori, S.; Katsura, M.; Suzuki, Y.; Fujishita, T.; Toyokawa, G.; et al. Clinical Significance of PD-L1 Protein Expression in Surgically Resected Primary Lung Adenocarcinoma. J. Thorac. Oncol. 2016, 11, 1879–1890. [Google Scholar] [CrossRef] [PubMed]
- Takada, K.; Okamoto, T.; Toyokawa, G.; Kozuma, Y.; Matsubara, T.; Haratake, N.; Akamine, T.; Takamori, S.; Katsura, M.; Shoji, F.; et al. The expression of PD-L1 protein as a prognostic factor in lung squamous cell carcinoma. Lung Cancer 2017, 104, 7–15. [Google Scholar] [CrossRef]
- Azuma, K.; Ota, K.; Kawahara, A.; Hattori, S.; Iwama, E.; Harada, T.; Matsumoto, K.; Takayama, K.; Takamori, S.; Kage, M.; et al. Association of PD-L1 overexpression with activating EGFR mutations in surgically resected nonsmall-cell lung cancer. Ann. Oncol. 2014, 25, 1935–1940. [Google Scholar] [CrossRef]
- Saw, S.P.L.; Ng, W.P.; Zhou, S.; Lai, G.G.Y.; Tan, A.C.; Ang, M.-K.; Lim, W.-T.; Kanesvaran, R.; Ng, Q.S.; Jain, A.; et al. PD-L1 score as a prognostic biomarker in asian early-stage epidermal growth factor receptor-mutated lung cancer. Eur. J. Cancer 2023, 178, 139–149. [Google Scholar] [CrossRef]
- Kim, S.-H.; Go, S.-I.; Song, D.H.; Park, S.W.; Kim, H.R.; Jang, I.; Kim, J.D.; Lee, J.S.; Lee, G.-W. Prognostic impact of CD8 and programmed death-ligand 1 expression in patients with resectable non-small cell lung cancer. Br. J. Cancer 2019, 120, 547–554. [Google Scholar] [CrossRef]
- Handa, Y.; Tsutani, Y.; Shiroma, N.; Kai, Y.; Mimae, T.; Miyata, Y.; Takeshima, Y.; Arihiro, K.; Okada, M. Prognostic Impact of Programmed Death-ligand 1 and Surrounding Immune Status on Stage I Lung Cancer. Clin. Lung Cancer 2020, 21, e302–e314. [Google Scholar] [CrossRef]
- Yang, C.-Y.; Lin, M.-W.; Chang, Y.-L.; Wu, C.-T.; Yang, P.-C. Programmed cell death-ligand 1 expression in surgically resected stage I pulmonary adenocarcinoma and its correlation with driver mutations and clinical outcomes. Eur. J. Cancer 2014, 50, 1361–1369. [Google Scholar] [CrossRef]
- Cooper, W.A.; Tran, T.; Vilain, R.E.; Madore, J.; Selinger, C.I.; Kohonen-Corish, M.; Yip, P.; Yu, B.; O’Toole, S.A.; McCaughan, B.C.; et al. PD-L1 expression is a favorable prognostic factor in early stage non-small cell carcinoma. Lung Cancer 2015, 89, 181–188. [Google Scholar] [CrossRef]
- Teramoto, K.; Igarashi, T.; Kataoka, Y.; Ishida, M.; Hanaoka, J.; Sumimoto, H.; Daigo, Y. Biphasic prognostic significance of PD-L1 expression status in patients with early- and locally advanced-stage non-small cell lung cancer. Cancer Immunol. Immunother. 2021, 70, 1063–1074. [Google Scholar] [CrossRef]
- Song, Z.; Yu, X.; Cheng, G.; Zhang, Y. Programmed death-ligand 1 expression associated with molecular characteristics in surgically resected lung adenocarcinoma. J. Transl. Med. 2016, 14, 188. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.; Zhu, S.; Guo, H.; Li, X.; Zhao, S.; Wang, Y.; Lei, X.; Huang, D.; Peng, L.; Li, Z.; et al. The Impact of Programmed Death-Ligand 1 Expression on the Prognosis of Early Stage Resected Non-Small Cell Lung Cancer: A Meta-Analysis of Literatures. Front. Oncol. 2021, 11, 567978. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Xie, H.; Dai, C.; Ren, Y.; She, Y.; Xu, L.; Chen, D.; Xie, D.; Zhang, L.; Jiang, G.; et al. Characterization of TIM-3 expression and its prognostic value in patients with surgically resected lung adenocarcinoma. Lung Cancer 2018, 121, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Ruel, L.-J.; Li, Z.; Gaudreault, N.; Henry, C.; Armero, V.S.; Boudreau, D.K.; Zhang, T.; Landi, M.T.; Labbé, C.; Couture, C.; et al. Tumor Mutational Burden by Whole-Genome Sequencing in Resected NSCLC of Never Smokers. Cancer Epidemiol. Biomarkers Prev. 2022, 31, 2219–2227. [Google Scholar] [CrossRef] [PubMed]
- Bubendorf, L.; Zoche, M.; Dafni, U.; Rüschoff, J.H.; Prince, S.S.; Marti, N.; Stavrou, A.; Kammler, R.; Finn, S.P.; Moch, H.; et al. Prognostic impact of tumour mutational burden in resected stage I and II lung adenocarcinomas from a European Thoracic Oncology Platform Lungscape cohort. Lung Cancer 2022, 174, 27–35. [Google Scholar] [CrossRef]
- He, Y.; Zhang, X.; Jia, K.; Dziadziuszko, R.; Zhao, S.; Deng, J.; Wang, H.; Hirsch, F.R.; Zhou, C. OX40 and OX40L protein expression of tumor infiltrating lymphocytes in non-small cell lung cancer and its role in clinical outcome and relationships with other immune biomarkers. Transl. Lung Cancer Res. 2019, 8, 352–366. [Google Scholar] [CrossRef]
- Massarelli, E.; Lam, V.K.; Parra, E.R.; Rodriguez-Canales, J.; Behrens, C.; Diao, L.; Wang, J.; Blando, J.; Byers, L.A.; Yanamandra, N.; et al. High OX-40 expression in the tumor immune infiltrate is a favorable prognostic factor of overall survival in non-small cell lung cancer. J. Immunother. Cancer 2019, 7, 351. [Google Scholar] [CrossRef]
- Gross, D.J.; Chintala, N.K.; Vaghjiani, R.G.; Grosser, R.; Tan, K.S.; Li, X.; Choe, J.; Li, Y.; Aly, R.G.; Emoto, K.; et al. Tumor and Tumor-Associated Macrophage Programmed Death-Ligand 1 Expression Is Associated with Adjuvant Chemotherapy Benefit in Lung Adenocarcinoma. J. Thorac. Oncol. 2022, 17, 89–102. [Google Scholar] [CrossRef]
- Felip, E.; Altorki, N.; Zhou, C.; Csőszi, T.; Vynnychenko, I.; Goloborodko, O.; Luft, A.; Akopov, A.; Martinez-Marti, A.; Kenmotsu, H.; et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): A randomised, multicentre, open-label, phase 3 trial. Lancet 2021, 398, 1344–1357. [Google Scholar] [CrossRef]
- Forde, P.M.; Spicer, J.; Lu, S.; Provencio, M.; Mitsudomi, T.; Awad, M.M.; Felip, E.; Broderick, S.R.; Brahmer, J.R.; Swanson, S.J.; et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N. Engl. J. Med. 2022, 386, 1973–1985. [Google Scholar] [CrossRef] [PubMed]
- Shu, C.A.; Gainor, J.F.; Awad, M.M.; Chiuzan, C.; Grigg, C.M.; Pabani, A.; Garofano, R.F.; Stoopler, M.B.; Cheng, S.K.; White, A.; et al. Neoadjuvant atezolizumab and chemotherapy in patients with resectable non-small-cell lung cancer: An open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020, 21, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Dandachi, N.; Tiran, V.; Lindenmann, J.; Brcic, L.; Fink-Neuboeck, N.; Kashofer, K.; Absenger, G.; Bezan, A.; Cote, R.J.; Datar, R.; et al. Frequency and clinical impact of preoperative circulating tumor cells in resectable non-metastatic lung adenocarcinomas. Lung Cancer 2017, 113, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Hofman, V.; Bonnetaud, C.; Ilie, M.I.; Vielh, P.; Vignaud, J.M.; Fléjou, J.F.; Lantuejoul, S.; Piaton, E.; Mourad, N.; Butori, C.; et al. Preoperative circulating tumor cell detection using the isolation by size of epithelial tumor cell method for patients with lung cancer is a new prognostic biomarker. Clin. Cancer Res. 2011, 17, 827–835. [Google Scholar] [CrossRef]
- Li, H.; Li, B.; Pan, Y.; Zhang, Y.; Xiang, J.; Zhang, Y.; Sun, Y.; Yu, X.; He, W.; Hu, H. Preoperative Folate Receptor-Positive Circulating Tumor Cell Level Is a Prognostic Factor of Long Term Outcome in Non-Small Cell Lung Cancer Patients. Front. Oncol. 2020, 10, 621435. [Google Scholar] [CrossRef]
- Manjunath, Y.; Upparahalli, S.V.; Avella, D.M.; Deroche, C.B.; Kimchi, E.T.; Staveley-O’Carroll, K.F.; Smith, C.J.; Li, G.; Kaifi, J.T. PD-L1 Expression with Epithelial Mesenchymal Transition of Circulating Tumor Cells Is Associated with Poor Survival in Curatively Resected Non-Small Cell Lung Cancer. Cancers 2019, 11, 806. [Google Scholar] [CrossRef]
- de Miguel-Pérez, D.; Bayarri-Lara, C.I.; Ortega, F.G.; Russo, A.; Rodriguez, M.J.M.; Alvarez-Cubero, M.J.; Serrano, E.M.; Lorente, J.A.; Rolfo, C.; Serrano, M.J. Post-Surgery Circulating Tumor Cells and AXL Overexpression as New Poor Prognostic Biomarkers in Resected Lung Adenocarcinoma. Cancers 2019, 11, 1750. [Google Scholar] [CrossRef]
- Yoon, S.O.; Kim, Y.T.; Jung, K.C.; Jeon, Y.K.; Kim, B.-H.; Kim, C.-W. TTF-1 mRNA-positive circulating tumor cells in the peripheral blood predict poor prognosis in surgically resected non-small cell lung cancer patients. Lung Cancer 2011, 71, 209–216. [Google Scholar] [CrossRef]
- Li, J.; Shi, S.-B.; Shi, W.-L.; Wang, Y.; Yu, L.-C.; Zhu, L.-R.; Ge, L.-P. LUNX mRNA-positive cells at different time points predict prognosis in patients with surgically resected nonsmall cell lung cancer. Transl. Res. J. Lab. Clin. Med. 2014, 163, 27–35. [Google Scholar] [CrossRef]
- Crosbie, P.A.J.; Shah, R.; Krysiak, P.; Zhou, C.; Morris, K.; Tugwood, J.; Booton, R.; Blackhall, F.; Dive, C. Circulating Tumor Cells Detected in the Tumor-Draining Pulmonary Vein Are Associated with Disease Recurrence after Surgical Resection of NSCLC. J. Thorac. Oncol. 2016, 11, 1793–1797. [Google Scholar] [CrossRef]
- Chemi, F.; Rothwell, D.G.; McGranahan, N.; Gulati, S.; Abbosh, C.; Pearce, S.P.; Zhou, C.; Wilson, G.A.; Jamal-Hanjani, M.; Birkbak, N.; et al. Pulmonary venous circulating tumor cell dissemination before tumor resection and disease relapse. Nat. Med. 2019, 25, 1534–1539. [Google Scholar] [CrossRef]
- Wankhede, D.; Grover, S.; Hofman, P. Circulating Tumor Cells as a Predictive Biomarker in Resectable Lung Cancer: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 6112. [Google Scholar] [CrossRef]
- Gauthier, I.; Ding, K.; Winton, T.; Shepherd, F.A.; Livingston, R.; Johnson, D.H.; Rigas, J.R.; Whitehead, M.; Graham, B.; Seymour, L. Impact of hemoglobin levels on outcomes of adjuvant chemotherapy in resected non-small cell lung cancer: The JBR.10 trial experience. Lung Cancer 2007, 55, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Sulibhavi, A.; Asokan, S.; Miller, M.I.; Moreira, P.; Daly, B.D.; Fernando, H.C.; Litle, V.R.; Suzuki, K. Peripheral Blood Lymphocytes and Platelets Are Prognostic in Surgical pT1 Non-Small Cell Lung Cancer. Ann. Thorac. Surg. 2020, 109, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Hou, C.; Jiang, F.; Ma, H.; Zhu, Q.; Wang, Z.; Zhao, B.; Xue, T.; Tan, S.; Yang, R.; Qian, Y.; et al. Prognostic role of preoperative platelet, fibrinogen, and D-dimer levels in patients with non-small cell lung cancer: A multicenter prospective study. Thorac. Cancer 2019, 10, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Carus, A.; Ladekarl, M.; Hager, H.; Pilegaard, H.; Nielsen, P.S.; Donskov, F. Tumor-associated neutrophils and macrophages in non-small cell lung cancer: No immediate impact on patient outcome. Lung Cancer 2013, 81, 130–137. [Google Scholar] [CrossRef]
- Kobayashi, N.; Usui, S.; Kikuchi, S.; Goto, Y.; Sakai, M.; Onizuka, M.; Sato, Y. Preoperative lymphocyte count is an independent prognostic factor in node-negative non-small cell lung cancer. Lung Cancer 2012, 75, 223–227. [Google Scholar] [CrossRef]
- Zhang, J.; Huang, S.-H.; Li, H.; Li, Y.; Chen, X.-L.; Zhang, W.-Q.; Chen, H.-G.; Gu, L.-J. Preoperative lymphocyte count is a favorable prognostic factor of disease-free survival in non-small-cell lung cancer. Med. Oncol. 2013, 30, 352. [Google Scholar] [CrossRef]
- Mitchell, K.G.; Diao, L.; Karpinets, T.; Negrao, M.V.; Tran, H.T.; Parra, E.R.; Corsini, E.M.; Reuben, A.; Federico, L.; Bernatchez, C.; et al. Neutrophil expansion defines an immunoinhibitory peripheral and intratumoral inflammatory milieu in resected non-small cell lung cancer: A descriptive analysis of a prospectively immunoprofiled cohort. J. Immunother. Cancer 2020, 8, e000405. [Google Scholar] [CrossRef]
- Manjunath, Y.; Mitchem, J.B.; Suvilesh, K.N.; Avella, D.M.; Kimchi, E.T.; Staveley-O’Carroll, K.F.; Deroche, C.B.; Pantel, K.; Li, G.; Kaifi, J.T. Circulating Giant Tumor-Macrophage Fusion Cells Are Independent Prognosticators in Patients With NSCLC. J. Thorac. Oncol. 2020, 15, 1460–1471. [Google Scholar] [CrossRef]
- Takahashi, Y.; Horio, H.; Hato, T.; Harada, M.; Matsutani, N.; Morita, S.; Kawamura, M. Prognostic Significance of Preoperative Neutrophil-Lymphocyte Ratios in Patients with Stage I Non-small Cell Lung Cancer After Complete Resection. Ann. Surg. Oncol. 2015, 22 (Suppl. S3), S1324–S1331. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Qu, X.; Kam, N.-W.; Wang, K.; Shen, H.; Liu, Q.; Du, J. An inflammation-related nomogram for predicting the survival of patients with non-small cell lung cancer after pulmonary lobectomy. BMC Cancer 2018, 18, 692. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Jiang, Y.; Qu, X.; Shen, H.; Liu, Q.; Du, J. Evaluation of preoperative hematologic markers as prognostic factors and establishment of novel risk stratification in resected pN0 non-small-cell lung cancer. PLoS ONE 2014, 9, e111494. [Google Scholar] [CrossRef] [PubMed]
- Seitlinger, J.; Prieto, M.; Guerrera, F.; Streit, A.; Gauchotte, G.; Siat, J.; Falcoz, P.-E.; Massard, G.; Ferri, L.; Spicer, J.; et al. Neutrophil-to-lymphocyte ratio is correlated to driver gene mutations in surgically-resected non-small cell lung cancer and its post-operative evolution impacts outcomes. Clin. Lung Cancer 2022, 23, e29–e42. [Google Scholar] [CrossRef]
- Cao, W.; Yu, H.; Zhu, S.; Lei, X.; Li, T.; Ren, F.; Zhou, N.; Tang, Q.; Zu, L.; Xu, S. Clinical significance of preoperative neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in the prognosis of resected early-stage patients with non-small cell lung cancer: A meta-analysis. Cancer Med. 2022, 12, 7065–7076. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Shen, H.; Wang, G.; Zhang, P.; Liu, Q.; Du, J. Prognostic significance of systemic inflammation-based lymphocyte- monocyte ratio in patients with lung cancer: Based on a large cohort study. PLoS ONE 2014, 9, e108062. [Google Scholar] [CrossRef]
- Yang, Z.; Li, S.; Zhao, L.; Lv, W.; Ju, J.; Zhang, W.; Li, J.; Che, G. Serum uric acid to lymphocyte ratio: A novel prognostic biomarker for surgically resected early-stage lung cancer. A propensity score matching analysis. Clin. Chim. Acta 2020, 503, 35–44. [Google Scholar] [CrossRef]
- Yan, X.; Li, G. Preoperative systemic immune-inflammation index predicts prognosis and guides clinical treatment in patients with non-small cell lung cancer. Biosci. Rep. 2020, 40, BSR20200352. [Google Scholar] [CrossRef]
- Chen, K.; Zhao, H.; Shi, Y.; Yang, F.; Wang, L.T.; Kang, G.; Nie, Y.; Wang, J. Perioperative Dynamic Changes in Circulating Tumor DNA in Patients with Lung Cancer (DYNAMIC). Clin. Cancer Res. 2019, 25, 7058–7067. [Google Scholar] [CrossRef]
- Waldeck, S.; Mitschke, J.; Wiesemann, S.; Rassner, M.; Andrieux, G.; Deuter, M.; Mutter, J.; Lüchtenborg, A.-M.; Kottmann, D.; Titze, L.; et al. Early assessment of circulating tumor DNA after curative-intent resection predicts tumor recurrence in early-stage and locally advanced non-small-cell lung cancer. Mol. Oncol. 2022, 16, 527–537. [Google Scholar] [CrossRef]
- Yang, W.; You, N.; Jia, M.; Yeung, S.-C.J.; Ou, W.; Yu, M.; Wang, Y.; Fu, X.; Zhang, Z.; Yang, J.; et al. Undetectable circulating tumor DNA levels correlate with low risk of recurrence/metastasis in postoperative pathologic stage I lung adenocarcinoma patients. Lung Cancer 2020, 146, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Qiu, B.; Guo, W.; Zhang, F.; Lv, F.; Ji, Y.; Peng, Y.; Chen, X.; Bao, H.; Xu, Y.; Shao, Y.; et al. Dynamic recurrence risk and adjuvant chemotherapy benefit prediction by ctDNA in resected NSCLC. Nat. Commun. 2021, 12, 6770. [Google Scholar] [CrossRef] [PubMed]
- Xia, L.; Mei, J.; Kang, R.; Deng, S.; Chen, Y.; Yang, Y.; Feng, G.; Deng, Y.; Gan, F.; Lin, Y.; et al. Perioperative ctDNA-Based Molecular Residual Disease Detection for Non-Small Cell Lung Cancer: A Prospective Multicenter Cohort Study (LUNGCA-1). Clin. Cancer Res. 2022, 28, 3308–3317. [Google Scholar] [CrossRef]
- Li, N.; Wang, B.-X.; Li, J.; Shao, Y.; Li, M.-T.; Li, J.-J.; Kuang, P.-P.; Liu, Z.; Sun, T.-Y.; Wu, H.-Q.; et al. Perioperative circulating tumor DNA as a potential prognostic marker for operable stage I to IIIA non-small cell lung cancer. Cancer 2022, 128, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Gale, D.; Heider, K.; Ruiz-Valdepenas, A.; Hackinger, S.; Perry, M.; Marsico, G.; Rundell, V.; Wulff, J.; Sharma, G.; Knock, H.; et al. Residual ctDNA after treatment predicts early relapse in patients with early-stage non-small cell lung cancer. Ann. Oncol. 2022, 33, 500–510. [Google Scholar] [CrossRef]
- Hu, Z.; Chen, X.; Zhao, Y.; Tian, T.; Jin, G.; Shu, Y.; Chen, Y.; Xu, L.; Zen, K.; Zhang, C.; et al. Serum microRNA signatures identified in a genome-wide serum microRNA expression profiling predict survival of non-small-cell lung cancer. J. Clin. Oncol. 2010, 28, 1721–1726. [Google Scholar] [CrossRef]
- Heegaard, N.H.H.; Schetter, A.J.; Welsh, J.A.; Yoneda, M.; Bowman, E.D.; Harris, C.C. Circulating micro-RNA expression profiles in early stage nonsmall cell lung cancer. Int. J. Cancer 2012, 130, 1378–1386. [Google Scholar] [CrossRef]
- Kanaoka, R.; Iinuma, H.; Dejima, H.; Sakai, T.; Uehara, H.; Matsutani, N.; Kawamura, M. Usefulness of Plasma Exosomal MicroRNA-451a as a Noninvasive Biomarker for Early Prediction of Recurrence and Prognosis of Non-Small Cell Lung Cancer. Oncology 2018, 94, 311–323. [Google Scholar] [CrossRef]
- Han, B.; Molins, L.; He, Y.; Viñolas, N.; Sánchez-Lorente, D.; Boada, M.; Guirao, A.; Díaz, T.; Martinez, D.; Ramirez, J.; et al. Characterization of the MicroRNA Cargo of Extracellular Vesicles Isolated from a Pulmonary Tumor-Draining Vein Identifies miR-203a-3p as a Relapse Biomarker for Resected Non-Small Cell Lung Cancer. Int. J. Mol. Sci. 2022, 23, 7138. [Google Scholar] [CrossRef]
- Sawabata, N.; Ohta, M.; Takeda, S.-I.; Hirano, H.; Okumura, Y.; Asada, H.; Maeda, H. Serum carcinoembryonic antigen level in surgically resected clinical stage I patients with non-small cell lung cancer. Ann. Thorac. Surg. 2002, 74, 174–179. [Google Scholar] [CrossRef]
- Okada, M.; Sakamoto, T.; Nishio, W.; Uchino, K.; Tsubota, N. Characteristics and prognosis of patients after resection of nonsmall cell lung carcinoma measuring 2 cm or less in greatest dimension. Cancer 2003, 98, 535–541. [Google Scholar] [CrossRef]
- Sakao, Y.; Nakazono, T.; Sakuragi, T.; Natsuaki, M.; Itoh, T. Predictive factors for survival in surgically resected clinical IA peripheral adenocarcinoma of the lung. Ann. Thorac. Surg. 2004, 77, 1157–1161. [Google Scholar] [CrossRef] [PubMed]
- Fukai, R.; Sakao, Y.; Sakuraba, M.; Oh, S.; Shiomi, K.; Sonobe, S.; Saitoh, Y.; Miyamoto, H. The prognostic value of carcinoembryonic antigen in T1N1M0 and T2N1M0 non-small cell carcinoma of the lung. Eur. J. Cardio-Thorac. Surg. 2007, 32, 440–444. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Higashi, K.; Sakuma, T.; Ito, K.; Niho, S.; Ueda, Y.; Kobayashi, T.; Sekiguchi, R.; Takahashi, T.; Kato, T.; Tonami, H. Combined evaluation of preoperative FDG uptake on PET, ground-glass opacity area on CT, and serum CEA level: Identification of both low and high risk of recurrence in patients with resected T1 lung adenocarcinoma. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Hanagiri, T.; Sugaya, M.; Takenaka, M.; Oka, S.; Baba, T.; Shigematsu, Y.; Nagata, Y.; Shimokawa, H.; Uramoto, H.; Takenoyama, M.; et al. Preoperative CYFRA 21-1 and CEA as prognostic factors in patients with stage I non-small cell lung cancer. Lung Cancer 2011, 74, 112–117. [Google Scholar] [CrossRef]
- Kozu, Y.; Maniwa, T.; Takahashi, S.; Isaka, M.; Ohde, Y.; Nakajima, T. Risk factors for both recurrence and survival in patients with pathological stage I non-small-cell lung cancer. Eur. J. Cardio-Thorac. Surg. 2013, 44, e53–e58. [Google Scholar] [CrossRef][Green Version]
- Kuo, S.-W.; Chen, J.-S.; Huang, P.-M.; Hsu, H.-H.; Lai, H.-S.; Lee, J.-M. Prognostic significance of histologic differentiation, carcinoembryonic antigen value, and lymphovascular invasion in stage I non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2014, 148, 1200–1207.e3. [Google Scholar] [CrossRef][Green Version]
- Hashinokuchi, A.; Haratake, N.; Takenaka, T.; Matsudo, K.; Nagano, T.; Watanabe, K.; Kosai, K.; Oku, Y.; Ono, Y.; Takamori, S.; et al. Clinical significance of the combination of preoperative SUVmax and CEA in patients with clinical stage IA lung adenocarcinoma. Thorac. Cancer 2022, 13, 2624–2632. [Google Scholar] [CrossRef]
- Sawabata, N.; Maeda, H.; Yokota, S.; Takeda, S.-I.; Koma, M.; Tokunaga, T.; Ito, M. Postoperative serum carcinoembryonic antigen levels in patients with pathologic stage IA nonsmall cell lung carcinoma: Subnormal levels as an indicator of favorable prognosis. Cancer 2004, 101, 803–809. [Google Scholar] [CrossRef]
- Yamazaki, M.; Ishikawa, H.; Kunii, R.; Tasaki, A.; Sato, S.; Ikeda, Y.; Yoshimura, N.; Hashimoto, T.; Tsuchida, M.; Aoyama, H. A combination of preoperative CT findings and postoperative serum CEA levels improves recurrence prediction for stage I lung adenocarcinoma. Eur. J. Radiol. 2015, 84, 178–184. [Google Scholar] [CrossRef]
- Wang, Y.; Zheng, D.; Chen, T.; Zhang, J.; Yao, F.; Chen, H. Survival Prediction and Adjuvant Chemotherapy Based on Tumor Marker for Stage IB Lung Adenocarcinoma. Ann. Thorac. Surg. 2020, 109, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Kashiwabara, K.; Saeki, S.; Sasaki, J.-I.; Nomura, M.; Kohrogi, H. Combined evaluation of postoperative serum levels of carcinoembryonic antigen less than or equal to 2.5 ng/mL and absence of vascular invasion may predict no recurrence of stage I adenocarcinoma lung cancer. J. Thorac. Oncol. 2008, 3, 1416–1420. [Google Scholar] [CrossRef] [PubMed]
- Reinmuth, N.; Brandt, B.; Semik, M.; Kunze, W.-P.; Achatzy, R.; Scheld, H.H.; Broermann, P.; Berdel, W.E.; Macha, H.N.; Thomas, M. Prognostic impact of Cyfra21-1 and other serum markers in completely resected non-small cell lung cancer. Lung Cancer 2002, 36, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Lee, J.G.; Kim, J.; Park, Y.; Lee, S.K.; Bae, M.K.; Lee, C.Y.; Kim, D.J.; Chung, K.Y. Preoperative serum CYFRA 21-1 level as a prognostic factor in surgically treated adenocarcinoma of lung. Lung Cancer 2013, 79, 156–160. [Google Scholar] [CrossRef]
- Mizuguchi, S.; Nishiyama, N.; Iwata, T.; Nishida, T.; Izumi, N.; Tsukioka, T.; Inoue, K.; Uenishi, T.; Wakasa, K.; Suehiro, S. Serum Sialyl Lewis x and cytokeratin 19 fragment as predictive factors for recurrence in patients with stage I non-small cell lung cancer. Lung Cancer 2007, 58, 369–375. [Google Scholar] [CrossRef]
- Muley, T.; Fetz, T.-H.; Dienemann, H.; Hoffmann, H.; Herth, F.J.F.; Meister, M.; Ebert, W. Tumor volume and tumor marker index based on CYFRA 21-1 and CEA are strong prognostic factors in operated early stage NSCLC. Lung Cancer 2008, 60, 408–415. [Google Scholar] [CrossRef]
- Ma, S.; Shen, L.; Qian, N.; Chen, K. The prognostic values of CA125, CA19.9, NSE, AND SCC for stage I NSCLC are limited. Cancer Biomark. 2011, 10, 155–162. [Google Scholar] [CrossRef]
- Yu, D.; Du, K.; Liu, T.; Chen, G. Prognostic value of tumor markers, NSE, CA125 and SCC, in operable NSCLC Patients. Int. J. Mol. Sci. 2013, 14, 11145–11156. [Google Scholar] [CrossRef]
- Isaksson, S.; George, A.M.; Jönsson, M.; Cirenajwis, H.; Jönsson, P.; Bendahl, P.-O.; Brunnström, H.; Staaf, J.; Saal, L.H.; Planck, M. Pre-operative plasma cell-free circulating tumor DNA and serum protein tumor markers as predictors of lung adenocarcinoma recurrence. Acta Oncol. 2019, 58, 1079–1086. [Google Scholar] [CrossRef]
- O’Dowd, C.; McRae, L.A.; McMillan, D.C.; Kirk, A.; Milroy, R. Elevated preoperative C-reactive protein predicts poor cancer specific survival in patients undergoing resection for non-small cell lung cancer. J. Thorac. Oncol. 2010, 5, 988–992. [Google Scholar] [CrossRef]
- Alifano, M.; Falcoz, P.E.; Seegers, V.; Roche, N.; Schussler, O.; Younes, M.; Antonacci, F.; Forgez, P.; Dechartres, A.; Massard, G.; et al. Preresection serum C-reactive protein measurement and survival among patients with resectable non-small cell lung cancer. J. Thorac. Cardiovasc. Surg. 2011, 142, 1161–1167. [Google Scholar] [CrossRef]
- Sheng, L.; Luo, M.; Sun, X.; Lin, N.; Mao, W.; Su, D. Serum fibrinogen is an independent prognostic factor in operable nonsmall cell lung cancer. Int. J. Cancer 2013, 133, 2720–2725. [Google Scholar] [CrossRef]
- Zhang, P.P.; Sun, J.W.; Wang, X.Y.; Liu, X.M.; Li, K. Preoperative plasma D-dimer levels predict survival in patients with operable non-small cell lung cancer independently of venous thromboembolism. Eur. J. Surg. Oncol. 2013, 39, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.-G.; Li, J.; Shi, S.-B.; Chen, P.; Ge, L.-P.; Jiang, Q.; Tang, X.-P. Value of fibrinogen and D-dimer in predicting recurrence and metastasis after radical surgery for non-small cell lung cancer. Med. Oncol. 2014, 31, 22. [Google Scholar] [CrossRef] [PubMed]
- Kawai, H.; Ota, H. Low perioperative serum prealbumin predicts early recurrence after curative pulmonary resection for non-small-cell lung cancer. World J. Surg. 2012, 36, 2853–2857. [Google Scholar] [CrossRef]
- Okada, S.; Shimada, J.; Kato, D.; Tsunezuka, H.; Teramukai, S.; Inoue, M. Clinical Significance of Prognostic Nutritional Index After Surgical Treatment in Lung Cancer. Ann. Thorac. Surg. 2017, 104, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, Y.; Safi, S.; Muley, T.; Warth, A.; Herth, F.J.F.; Dienemann, H.; Hoffmann, H.; Eichhorn, M.E. C-reactive protein-albumin ratio is an independent prognostic predictor of tumor recurrence in stage IIIA-N2 lung adenocarcinoma patients. Lung Cancer 2017, 114, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Qin, S.; Sun, X.; Liu, D.; Zhang, B.; Xiao, G.; Ren, H. Prognostic Significance of Albumin-Globulin Score in Patients with Operable Non-Small-Cell Lung Cancer. Ann. Surg. Oncol. 2018, 25, 3647–3659. [Google Scholar] [CrossRef]
- Guo, X.; Shao, J.; Zhai, B.; Zou, Q.; Yan, J.; Gu, H.; Wang, G. Relationship and prognostic significance between preoperative serum albumin to globulin ratio and CT features of non-small cell lung cancer. Eur. J. Radiol. 2020, 128, 109039. [Google Scholar] [CrossRef]
- Takenaka, M.; Hanagiri, T.; Shinohara, S.; Yasuda, M.; Chikaishi, Y.; Oka, S.; Shimokawa, H.; Nagata, Y.; Nakagawa, M.; Uramoto, H.; et al. Serum level of osteopontin as a prognostic factor in patients who underwent surgical resection for non-small-cell lung cancer. Clin. Lung Cancer 2013, 14, 288–294. [Google Scholar] [CrossRef]
- Rud, A.K.; Boye, K.; Oijordsbakken, M.; Lund-Iversen, M.; Halvorsen, A.R.; Solberg, S.K.; Berge, G.; Helland, A.; Brustugun, O.T.; Mælandsmo, G.M. Osteopontin is a prognostic biomarker in non-small cell lung cancer. BMC Cancer 2013, 13, 540. [Google Scholar] [CrossRef]
- Lin, D.; Shen, L.; Luo, M.; Zhang, K.; Li, J.; Yang, Q.; Zhu, F.; Zhou, D.; Zheng, S.; Chen, Y.; et al. Circulating tumor cells: Biology and clinical significance. Signal Transduct. Target Ther. 2021, 6, 404. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Guo, C.; He, J.; Tan, Q.; Mei, J.; Yang, Z.; Liu, C.; Pu, Q.; Ma, L.; Yuan, Y.; et al. Effect of Vein-First vs Artery-First Surgical Technique on Circulating Tumor Cells and Survival in Patients with Non-Small Cell Lung Cancer: A Randomized Clinical Trial and Registry-Based Propensity Score Matching Analysis. JAMA Surg. 2019, 154, e190972. [Google Scholar] [CrossRef] [PubMed]
- Szilágyi, M.; Pös, O.; Márton, É.; Buglyó, G.; Soltész, B.; Keserű, J.; Penyige, A.; Szemes, T.; Nagy, B. Circulating Cell-Free Nucleic Acids: Main Characteristics and Clinical Application. Int. J. Mol. Sci. 2020, 21, 6827. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yu, H.; Gan, Y.; Wu, Z.; Li, E.; Li, X.; Cao, J.; Zhu, Y.; Wang, L.; Deng, H.; et al. Mining whole-lung information by artificial intelligence for predicting EGFR genotype and targeted therapy response in lung cancer: A multicohort study. Lancet Digit. Health 2022, 4, e309–e319. [Google Scholar] [CrossRef]
- Kawakami, E.; Tabata, J.; Yanaihara, N.; Ishikawa, T.; Koseki, K.; Iida, Y.; Saito, M.; Komazaki, H.; Shapiro, J.S.; Goto, C.; et al. Application of Artificial Intelligence for Preoperative Diagnostic and Prognostic Prediction in Epithelial Ovarian Cancer Based on Blood Biomarkers. Clin. Cancer Res. 2019, 25, 3006–3015. [Google Scholar] [CrossRef]
| Mutant Genes | Ref. (NOP) | Study Design | Histology | Phase | Ethnicity | Median Follow-Up (Months) | Percentage of Genetic Alterations | Prognostic Implication |
|---|---|---|---|---|---|---|---|---|
| EGFR | ||||||||
| EGFR alterations | [9] (374) | RCT | Ns-NSCLC | II–IIIA | Japanese | NA | 37.2% | Worse RFS |
| EGFR alterations | [10] (1512) | R | LUAD | I–III | Chinese | 53.2 | 61.8% | Worse RFS |
| EGFR alterations | [11] (1155) | R | LUAD | I–IIIA (N0-1) | Japanese | 36 | 50.6% | Worse RFS |
| EGFR amplification | [12] (637) | P | LUAD | I–IIIA (≤3 cm) | Chinese | 30.57 | 5.8% | Worse RFS |
| EGFR amplification | [13] (109) | R | NSCLC | I–III | Japanese | NA | 5.5% | Worse OS |
| EGFR alterations | [14] (237) | P | LUAD | I–III | Japanese | NA | 45.5% | Improved RFS |
| EGFR alterations | [15] (307) | R | NSCLC | I | American | 30 | 20.2% | Improved DFS and OS |
| EGFR alterations | [16] (164) | R | NSCLC | I–IIIA | Chinese | NA | 31.7% | Improved OS |
| EGFR alterations | [17] (1231) | R | NSCLC | I | Japanese | 36 | 44.3% | IA: No impact on survival; IB: Improved DSS and OS |
| EGFR exons 18-19 | [18] (133) | P | NSCLC | I–III | Korean | 29 | 7.5% | Improved OS |
| EGFR exon 19 | [19] (276) | R | LUAD | I–III | French/Italian | 46 | 55.1% | Stage I: No impact on OS; Stage II/III: Improved OS |
| EGFR exon 19 | [20] (202) | R | LUAD | II–IIIA (N1-2) | Japanese | NA | 27.2% | Improved DFS and OS |
| EGFR exon 19 | [21] (835) | R | LUAD | I–III | Japanese | 47 | 21% | Worse RFS |
| EGFR T790M | [22] (373) | P | NSCLC | I–IIIB | Japanese | 48.6 | 79.9% | Worse RFS and OS |
| Phosphorylated EGFR | [23] (49) | P | NSCLC | I | Austrian | 29.3 | NA | Worse survival |
| KRAS | ||||||||
| KRAS G12C | [24] (604) | P | LUAD | I–III | American | 30.1 | 16% | Worse DFS |
| KRAS alterations | [25] (1118) | R | LUAD | I–III | American | 27 | 25% | No impact on OS |
| KRAS alterations | [26] (312) | R | LUAD | I | American | 36 | 41% | Worse DFS and OS |
| KRAS alterations | [27] (482) | R | LUAD | I–II | American | 56.8 | 27% | Worse OS |
| KRAS alterations | [28] (324) | R | LUAD | I–III | American | 33.67 | 38.1% | Worse DFS and OS |
| KRAS alterations | [16] (164) | R | NSCLC | I–IIIA | Chinese | NA | 4.3% | Worse OS |
| KRAS alterations | [29] (216) | R | NSCLC | I–IIIA | Spanish | 14.25 | 13.4% | Improved DSS |
| ALK | ||||||||
| ALK rearrangement | [30] (124) | R | LUAD | I | Japanese | NA | 19.4% | Worse RFS; No impact on OS |
| ALK rearrangement | [31] (764) | R | NSCLC | I–III | American | 60.5 | 4% | Worse RFS; No impact on OS |
| ALK rearrangement | [32] (1925) | R | LUAD | I–IIIB | Japanese | 72 | 3.9% | Improved CSS and OS |
| EML4-ALK fusion variant 3 | [33] (55) | R | NSCLC | I–III | Chinese | 34.8 | 34.6% | Worse DFS |
| ALK rearrangement | [34] (231) | R | LUAD | I–IIIB | Korean | 26 | 9% | No impact on DFS and OS |
| ALK rearrangement | [35] (735) | R | NSCLC | I–III | Korean | 45 | 3.8% | No impact on DFS and OS |
| MET | ||||||||
| MET alterations | [36] (311) | R | LUAD | IB–IIIA | Korean | 22.8 | 45.3% | Worse RFS and OS in EGFRmut (-) group |
| MET alterations | [37] (265) | R | NSCLC | I–II | Italian | 40 | NA | Worse OS |
| MET amplification | [38] (1540) | R | NSCLC | I–III | International | 57.3 | 22.8% | No impact on OS |
| METex14 skipping | [39] (795) | R | LUAD | I–III | Korean | NA | 2.1% | No impact on OS |
| ROS1 | ||||||||
| ROS1 fusion | [40] (230) | R | LUAD | I–II | Korean | 49 | NA | Worse RFS |
| ROS1 fusion | [41] (160) | P | LUAD | I–IIIA | Chinese | 50.1 | 3.1% | No impact on OS |
| TP53 | ||||||||
| TP53 alterations | [12] (637) | P | LUAD | I–IIIA (≤3 cm) | Chinese | 30.57 | 28.1% | Worse RFS |
| TP53 alterations | [40] (230) | R | LUAD | I–II | Korean | 49 | 18.3% | Worse RFS |
| TP53 alterations | [42] (214) | R | NSCLC | I–III | Canadian | 54 | 50% | Worse DFS and OS |
| TP53 alterations | [43] (50) | R | NSCLC | IA | American | NA | NA | LUAD: Worse OS; No impact on DFS; LUSC: No effect on DFS and OS |
| p53 pathway alterations | [44] (492) | P | LUAD | I–III | American | 19 | NA | Worse DFS |
| p53 alterations | [45] (76) | P | NSCLC | I–IIIB | Italian | 23 | 54% | Worse DFS |
| p53 alterations | [46] (102) | P | NSCLC | I–IIIA | Polish | 28 | NA | Worse OS |
| Others | ||||||||
| RET fusion | [40] (230) | R | LUAD | I–II | Korean | 49 | NA | Worse RFS |
| BRAF alterations | [28] (324) | R | LUAD | I–III | American | 33.67 | 5.9% | Worse DFS and OS |
| PIK3CA alterations | [47] (308) | P | LUSC | I–III | Norwegian | 67.6 | 11.4% | Improved OS and TTR |
| PIK3CA alterations | [48] (810) | R | LUAD | I–IIIA | Chinese | NA | 2.8% | Worse OS |
| PIK3CA alterations | [49] (167) | R | NSCLC | I | Italian | 120 | 3.6% | Worse survival |
| TTF-1 amplification | [50] (118) | R | LUAD | I–III | Korean | NA | 12.7% | Worse DFS and OS |
| PKD and TP53 co-alterations | [51] (147) | P | LUAD | I–III | Chinese | 31.3 | 7% | Worse DFS; No impact on OS |
| Immune-Related Indicators | Ref. (NOP) | Study Design | Histology | Phase | Ethnicity | Median Follow-Up (Months) | Percentage of Indicators Overexpression | Prognostic Implication |
|---|---|---|---|---|---|---|---|---|
| PD-L1 | [70] (316) | R | LUAD | I–III | Korean | NA | 18.6% | Worse RFS and OS |
| PD-L1 | [71] (193) | R | LUAD | I–III | Korean | NA | 21.2% | Worse RFS and OS |
| PD-L1; PD-L2 | [72] (433) | R | LUAD | I–III | Japanese | NA | NA | Worse DFS and OS |
| PD-L1 | [73] (417) | R | LUAD | I–III | Japanese | NA | 34.5% | Worse DFS and OS |
| PD-L1 | [74] (205) | R | LUSC | I–III | Japanese | NA | 51.7% | Worse OS |
| PD-L1 | [75] (164) | R | NSCLC | I–IIIB | Japanese | 55.6 | 50% | Worse OS |
| PD-L1 | [76] (455) | R | NSCLC | I–IIIA | Asian | 47 | NA | Worse DFS and OS |
| PD-L1 | [77] (136) | R | NSCLC | I–III | Korean | 84 | 25.7% | Worse RFS and OS |
| PD-L1 | [78] (126) | R | NSCLC | I | Japanese | 47.5 | 18.3% | CD8-high cohort: No impact on RFS; CD8-low cohort: Worse RFS |
| PD-L1 | [79] (163) | R | LUAD | I | Chinese | 71 | 39.9% | Improved RFS; No impact on OS |
| PD-L1 | [80] (678) | R | NSCLC | I–III | Australian | NA | 7.4% | Improved OS |
| PD-L1 | [81] (228) | R | NSCLC | I–IIIA | Japanese | NA | 24.1% | Stage I: Improved RFS; Stage II–IIIA: Worse RFS |
| PD-L1 | [82] (386) | R | LUAD | I–III | Chinese | 54 | 48.3% | No impact on DFS and OS |
| PD-L1 | [83] (3790) | Meta | NSCLC | I–III | International | NA | NA | Worse DFS and OS |
| TIM-3 | [84] (223) | R | LUAD | I–III | Chinese | NA | 48% | Worse RFS and OS |
| TMB | [85] (92) | R | NSCLC | I–III | Canadian | NA | NA | Worse OS |
| TMB | [86] (78) | R | LUAD | I–II | Caucasian | 56.1 | NA | No impact on RFS and OS |
| OX40 | [87] (139) | R | NSCLC | I | Polish | NA | NA | Worse RFS and OS |
| OX40 | [88] (100) | R | NSCLC | I–III | American | NA | NA | Improved OS |
| Blood-Based Biomarkers | Ref. (NOP) | Study Design | Histology | Phase | Ethnicity | Median Follow-Up (Months) | Prognostic Implications |
|---|---|---|---|---|---|---|---|
| CTCs | |||||||
| CTCs | [93] (40) | P | LUAD | I–IIIA | Austrian | 16 | Worse DFS |
| CTCs | [94] (137) | P | NSCLC | I–II | French | NA | Worse DFS and OS |
| FR+ CTCs | [95] (52) | P | NSCLC | I–III | Chinese | NA | Worse RFS and OS |
| PD-L1+/EMT+ CTCs | [96] (30) | P | NSCLC | I–IIIA | American | 14.3 | Worse RFS and OS |
| CTCs | [97] (97) | P | NSCLC | I–III | Spanish | LAUD: 30.5; LUSC: 32 | LUAD: Worse RFS and OS; LUSC: No impact on survival |
| TTF-1+ CTCs | [98] (79) | P | NSCLC | I–III | Korean | NA | Worse PFS |
| LUNX+ CTCS | [99] (68) | P | NSCLC | I–IIIA | Chinese | 39.5 | Worse DFS and OS |
| CTCs | [100] (30) | P | NSCLC | I–III | British | 22 | Worse DFS and OS |
| CTCs | [101] (100) | P | NSCLC | I–III | British | 33.1 | Worse DFS |
| CTCs | [102] (1321) | Meta | NSCLC | I–IIIA | International | Range: 13–84 | Worse DFS and OS |
| Routine examinations of blood | |||||||
| Hb | [103] (482) | R | NSCLC | IB–II | Canadian | NA | Baseline Hb: Worse OS; During-treatment Hb: Improved RFS and OS |
| PLT; Lymphocyte | [104] (103) | R | NSCLC | I | American | 42 | Worse RFS |
| PLT | [105] (395) | P | NSCLC | I–III | Chinese | 13.2 | Worse PFS |
| White blood cells | [106] (335) | P | NSCLC | I–IIIA | Danish | NA | Worse RFS and OS |
| Lymphocyte; Neutrophil | [107] (237) | R | NSCLC | I–III | Japanese | NA | Lymphocyte: Improved OS; Neutrophil: No impact on OS |
| Lymphocyte; Neutrophil | [108] (142) | R | NSCLC | IB–IIIA | Chinese | NA | Lymphocyte: Improved DFS/No impact on OS; Neutrophil: No impact on survival |
| Neutrophil; Lymphocyte | [109] (1524) | P | NSCLC | I–IIIA | American | 60.7 | Neutrophil: Worse OS; Lymphocyte: No impact on OS |
| TMFs | [110] (115) | P | NSCLC | I–IIIA | Colombian | 26.6 | Worse DFS and OS |
| NLR | [111] (343) | R | NSCLC | I | Japanese | 73.5 | Worse RFS and OS |
| NLR | [112] (952) | R | NSCLC | I–III | Chinese | 40 | Worse OS |
| NLR; PLR | [113] (400) | R | NSCLC | I–II (N0) | Chinese | 46 | NLR: Worse DFS and OS; PLR: No impact on survival |
| NLR | [114] (2027) | R | NSCLC | I–III | French | 69 | Worse OS and TTR |
| NLR; PLR | [115] (14,242) | Meta | NSCLC | I–III | International | NA | Worse DFS and OS |
| LMR | [116] (1453) | R | NSCLC | I–III | Chinese | NA | Improved DFS and OS |
| ULR | [117] (335) | P | NSCLC | I–II | Chinese | 51 | Worse DFS and OS |
| SII | [118] (538) | R | NSCLC | I–IIIA | Chinese | 54 | Worse DFS and OS |
| Circulating nucleic acids | |||||||
| ctDNA | [119] (205) | P | NSCLC | I–IIIA | Chinese | 17.6 | Worse RFS and OS |
| ctDNA | [120] (33) | P | NSCLC | I–IIIB | German | 26.2 | Worse PFS and OS |
| ctDNA | [121] (82) | P | LUAD | I | Chinese | 22.83 | Worse DFS |
| ctDNA | [122] (89) | P | LUAD | IIB–IIIA | Chinese | NA | Worse RFS |
| ctDNA | [123] (330) | P | NSCLC | I–III | Chinese | 35.6 | Worse RFS |
| ctDNA | [124] (119) | P | NSCLC | I–IIIA | Chinese | 30.7 | Worse RFS and OS |
| ctDNA | [125] (88) | P | NSCLC | I–III | British | 36 | Worse RFS and OS |
| Four-miRNA signature (miR-486 and miR-30d, miR-1, miR-499) | [126] (303) | R | NSCLC | I–IIIA | Chinese | NA | High miR-486 and miR-30d; Low miR-1 and miR-499: Worse OS |
| MiR-let-7b | [127] (220) | R | NSCLC | I–II | American | NA | Improved CSS |
| MiR-451a | [128] (285) | R | NSCLC | I–III | Japanese | 24 | Worse DFS and OS |
| MiR-203a-3p | [129] (88) | R | NSCLC | I–III | Spanish | Screening/Validation cohort: 66.07/54.23 | Worse TTR |
| Tumour markers | |||||||
| CEA | [130] (253) | R | NSCLC | I–II | Japanese | NA | Worse OS |
| CEA | [131] (265) | R | NSCLC | I–IIIB | Japanese | 43 | Worse DSS and OS |
| CEA | [132] (65) | R | LUAD | IA | Japanese | NA | Worse DFS and OS |
| CEA | [133] (45) | R | NSCLC | T1-2N1M0 | Japanese | 39.8 | Worse OS |
| CEA | [134] (87) | R | LUAD | I–IIIB (≤3 cm) | Japanese | NA | Worse DFS |
| CEA; CYFRA 21-1 | [135] (341) | R | NSCLC | I | Japanese | NA | Worse OS |
| CEA; CYFRA 21-1 | [136] (467) | R | NSCLC | I | Japanese | 54 | CEA: Worse DFS and OS; CYFRA 21-1: No impact on survival |
| CEA | [137] (758) | R | NSCLC | I | Chinese | NA | Worse PFS |
| Combination of SUVmax and CEA | [138] (410) | R | LUAD | IA | Japanese | NA | Worse RFS and OS |
| CEA | [139] (242) | R | NSCLC | IA | Japanese | 64 | Worse survival |
| CEA | [140] (250) | R | LUAD | I | Japanese | 73.2 | Worse DFS |
| CEA | [141] (600) | R | LUAD | IB | Chinese | 46.7 | Worse RFS and OS |
| CEA | [142] (136) | R | LUAD | I | Japanese | 28.3 | Worse RFS |
| CYFRA 21-1; NSE; SCC-Ag | [143] (67) | P | NSCLC | I–IIIA | German | 86 | CYFRA 21-1: Worse DFS and OS; NSE; SCC-Ag: No impact on survival |
| CYFRA 21-1 | [144] (298) | R | LUAD | I–III | Korean | 43.3 | Worse DFS and OS |
| Combination of CYFRA 21-1 and SLX | [145] (137) | R | NSCLC | I | Japanese | NA | Worse survival |
| TMI | [146] (261) | R | NSCLC | I–II | German | 59.8 | Worse OS |
| NSE; SCC-Ag; CA125; CA199 | [147] (164) | R | NSCLC | I | Chinese | 26 | No impact on survival |
| NSE; CA125; SCC-Ag | [148] (481) | R | NSCLC | I–IIIB | Chinese | NA | NSE; CA125: Worse DFS and OS; SCC-Ag: No impact on survival |
| CA125; CA199 | [149] (58) | R | LUAD | I–IIIA | Swedish | 39.6 | Worse RFS |
| Other blood biomarkers | |||||||
| CRP | [150] (96) | R | NSCLC | I–III | British | 75 | Worse CSS |
| CRP | [151] (229) | R | NSCLC | I–II | French | 89.2 | Worse OS |
| Fibrinogen | [152] (567) | R | NSCLC | I–IIIB | Chinese | NA | Worse PFS and OS |
| D-dimer | [153] (232) | R | NSCLC | I–IIIA | Chinese | 47 | Worse OS |
| Fibrinogen; D-dimer | [154] (184) | R | NSCLC | I–IIIA | Chinese | 18.5 | Worse DFS and OS |
| Fibrinogen; D-dimer | [105] (395) | P | NSCLC | I–III | Chinese | 13.2 | Worse PFS |
| Prealbumin | [155] (44) | P | NSCLC | I–III | Japanese | NA | Improved DFS |
| PNI | [156] (248) | R | NSCLC | I–III | Japanese | 51 | Improved RFS and OS |
| CAR | [157] (156) | R | NSCLC | IIIA (N2) | German | NA | Worse RFS |
| AGS | [158] (312) | R | NSCLC | I–III | Chinese | 41 | Worse DFS and OS |
| AGR | [159] (180) | R | NSCLC | I–III | Chinese | NA | Improved OS |
| OPN | [160] (244) | R | NSCLC | I–III | Japanese | NA | Worse survival |
| OPN | [161] (201) | R | NSCLC | I–III | Norwegian | 34 | No impact on survival |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, W.; Tang, Q.; Zeng, J.; Jin, X.; Zu, L.; Xu, S. A Review of Biomarkers and Their Clinical Impact in Resected Early-Stage Non-Small-Cell Lung Cancer. Cancers 2023, 15, 4561. https://doi.org/10.3390/cancers15184561
Cao W, Tang Q, Zeng J, Jin X, Zu L, Xu S. A Review of Biomarkers and Their Clinical Impact in Resected Early-Stage Non-Small-Cell Lung Cancer. Cancers. 2023; 15(18):4561. https://doi.org/10.3390/cancers15184561
Chicago/Turabian StyleCao, Weibo, Quanying Tang, Jingtong Zeng, Xin Jin, Lingling Zu, and Song Xu. 2023. "A Review of Biomarkers and Their Clinical Impact in Resected Early-Stage Non-Small-Cell Lung Cancer" Cancers 15, no. 18: 4561. https://doi.org/10.3390/cancers15184561
APA StyleCao, W., Tang, Q., Zeng, J., Jin, X., Zu, L., & Xu, S. (2023). A Review of Biomarkers and Their Clinical Impact in Resected Early-Stage Non-Small-Cell Lung Cancer. Cancers, 15(18), 4561. https://doi.org/10.3390/cancers15184561





