Efficacy of Empirical Radioiodine Therapy in Patients with Differentiated Thyroid Cancer and Elevated Serum Thyroglobulin without Evidence of Structural Disease: A Propensity Score Analysis
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
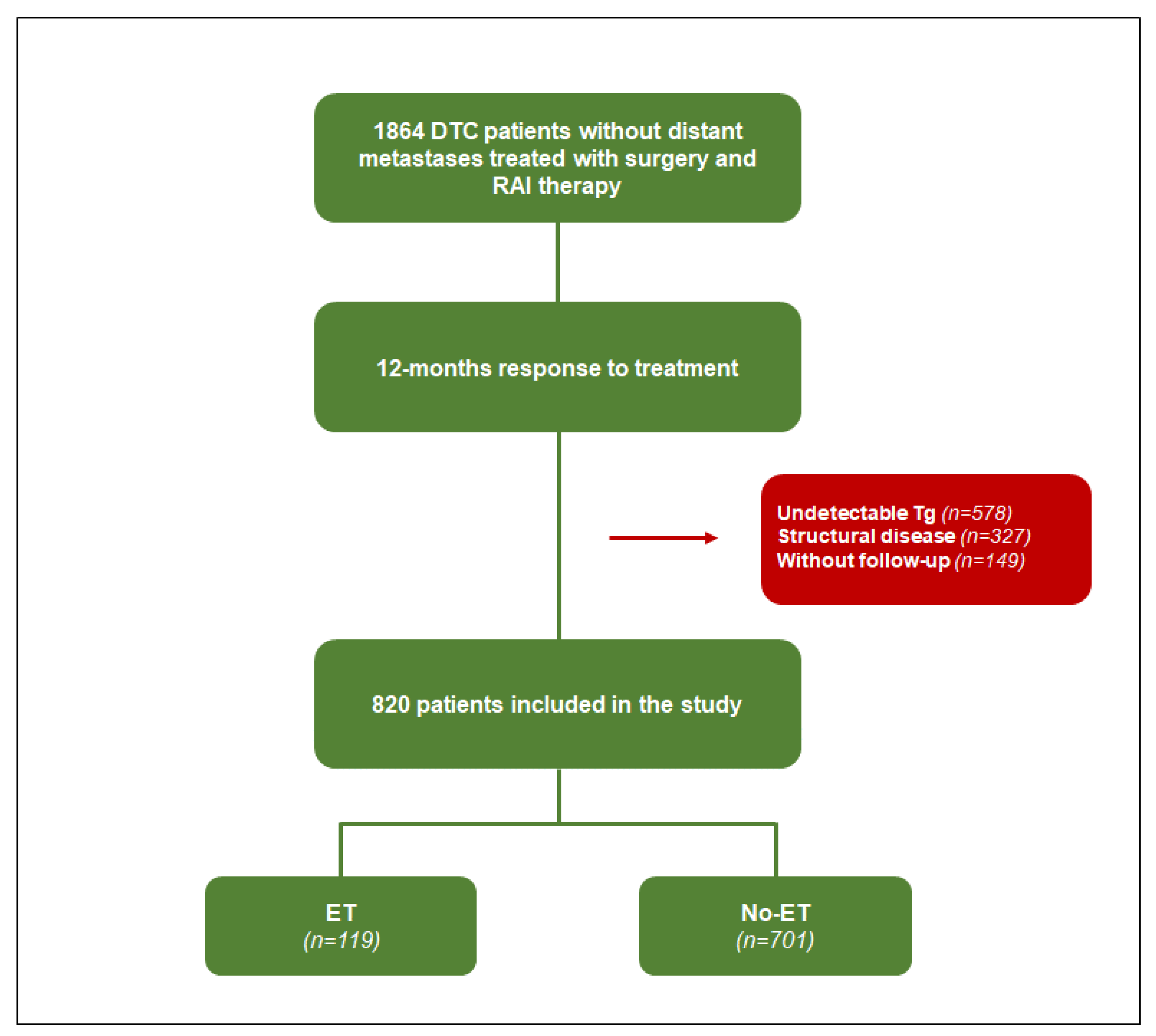
2.1. Study Population
2.2. Follow-Up
2.3. Statistical Analysis
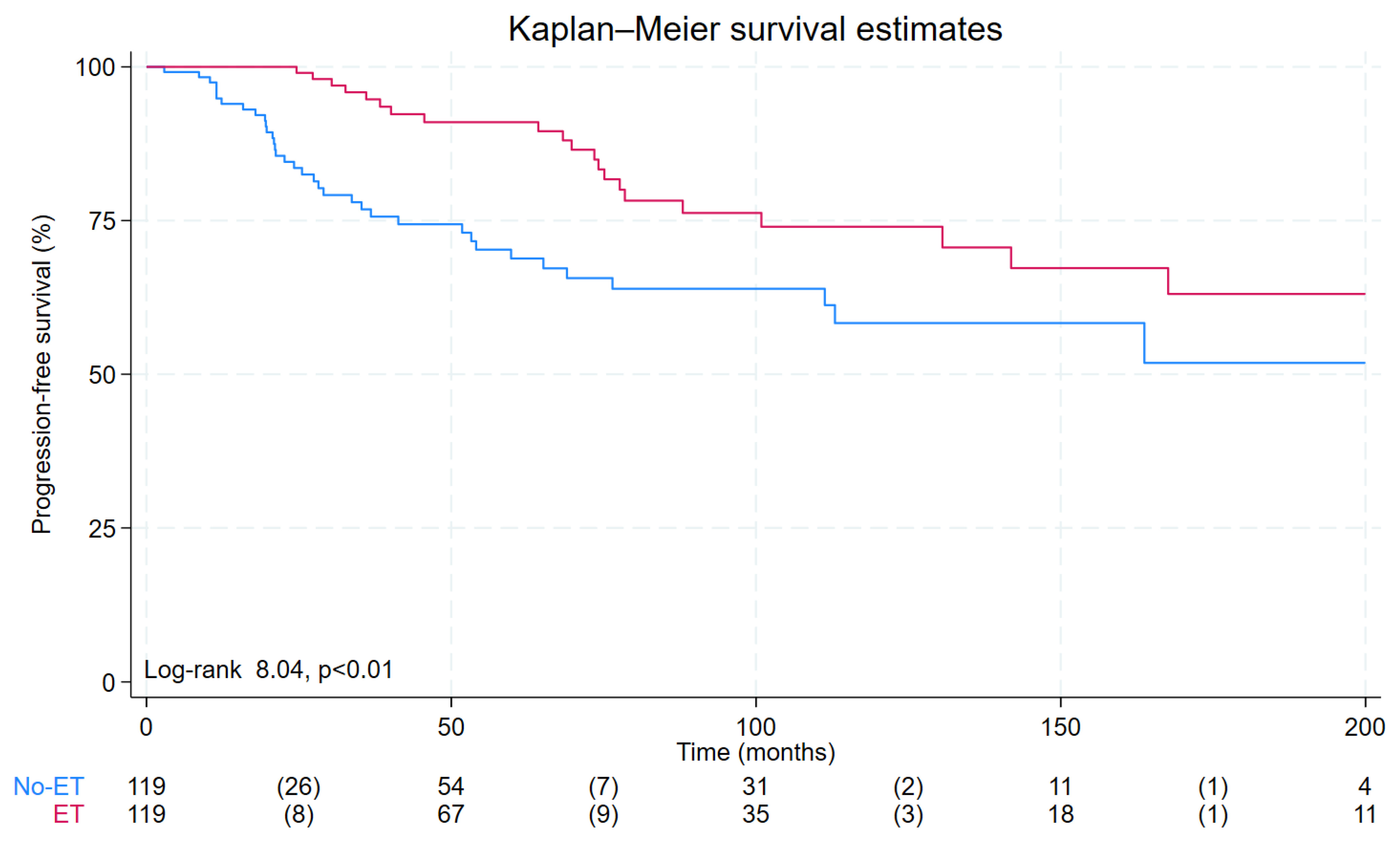
3. Results
3.1. Patients Characteristics before and after Matching
3.2. Predictors of Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed]
- Mazzaferri, E.L.; Jhiang, S.M. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am. J. Med. 1994, 97, 418–428, Erratum in: Am. J. Med. 1995, 98, 215. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, R.M.; Tala, H.; Shah, J.; Leboeuf, R.; Gonen, M.; Brokhin, M.; Omry, G.; Fagin, J.A.; Ghaznavi, S.A.; Ganly, I.; et al. Estimating Risk of Recurrence in Differentiated Thyroid Cancer After Total Thyroidectomy and Radioactive Iodine Remnant Ablation: Using Response to Therapy Variables to Modify the Initial Risk Estimates Predicted by the New American Thyroid Association Staging System. Thyroid 2010, 20, 1341–1349. [Google Scholar] [CrossRef] [PubMed]
- Mancusi, F.; Baudin, E.; Pacini, F.; Scott, E.; Learoyd, D.; Clifton-Bligh, R.J.; Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; et al. 131I Therapy for Elevated Thyroglobulin Levels. Thyroid 1997, 7, 273–276. [Google Scholar] [CrossRef]
- Sabra, M.M.; Grewal, R.K.; Tala, H.; Larson, S.M.; Tuttle, R.M.; Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; et al. Clinical Outcomes Following Empiric Radioiodine Therapy in Patients with Structurally Identifiable Metastatic Follicular Cell–Derived Thyroid Carcinoma with Negative Diagnostic but Positive Post-Therapy 131I Whole-Body Scans. Thyroid 2012, 22, 877–883. [Google Scholar] [CrossRef]
- Mazzaferri, E.L.; Kloos, R.T. Is Diagnostic Iodine-131 Scanning with Recombinant Human TSH Useful in the Follow-Up of Differentiated Thyroid Cancer after Thyroid Ablation? J. Clin. Endocrinol. Metab. 2002, 87, 1490–1498. [Google Scholar] [CrossRef]
- Klain, M.; Zampella, E.; Piscopo, L.; Volpe, F.; Manganelli, M.; Masone, S.; Pace, L.; Salvatore, D.; Schlumberger, M.; Cuocolo, A. Long-Term Prognostic Value of the Response to Therapy Assessed by Laboratory and Imaging Findings in Patients with Differentiated Thyroid Cancer. Cancers 2021, 13, 4338. [Google Scholar] [CrossRef]
- Klain, M.; Pace, L.; Zampella, E.; Mannarino, T.; Limone, S.; Mazziotti, E.; De Simini, G.; Cuocolo, A. Outcome of Patients with Differentiated Thyroid Cancer Treated With 131-Iodine on the Basis of a Detectable Serum Thyroglobulin Level After Initial Treatment. Front. Endocrinol. 2019, 10, 146. [Google Scholar] [CrossRef]
- Yuan, L.; Wang, J.; Pan, L.; Feng, H.; Chen, P.; Luo, J.; Xie, J.; Xiong, X.; Wu, J.; Ouyang, W. Outcome of patients with differentiated thyroid cancer treated with empirical radioiodine therapy on the basis of Thyroglobulin Elevation Negative Iodine Scintigraphy (TENIS) syndrome without structural disease: A retrospective cohort study. Ann. Nucl. Med. 2022, 37, 18–25. [Google Scholar] [CrossRef]
- Perrier, N.D.; Brierley, J.D.; Tuttle, R.M. Differentiated and anaplastic thyroid carcinoma: Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 68, 55–63. [Google Scholar] [CrossRef]
- Leuven, E.; Sianesi, B. PSMATCH2: Stata Module to Perform Full Mahalanobis and Propensity Score Matching, Common Sup-Port Graphing, and Covariate Imbalance Testing; Statistical Software Components S432001; Boston College Department of Economics: Chestnut Hill, MA, USA, 2003; (revised 19 July 2012). [Google Scholar]
- Klain, M.; Nappi, C.; Zampella, E.; Cantoni, V.; Green, R.; Piscopo, L.; Volpe, F.; Manganelli, M.; Caiazzo, E.; Petretta, M.; et al. Ablation rate after radioactive iodine therapy in patients with differentiated thyroid cancer at intermediate or high risk of recurrence: A systematic review and a meta-analysis. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 4437–4444. [Google Scholar] [CrossRef] [PubMed]
- Cuéllar, D.I.; Reyes, A.D.L.; Llamas-Olier, A. Modified dynamic risk stratification system further predicts individual outcome in patients with intermediate-risk papillary thyroid cancer. Ann. d’Endocrinologie 2022, 84, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Pacini, F.; Basolo, F.; Bellantone, R.; Boni, G.; Cannizzaro, M.A.; De Palma, M.; Durante, C.; Elisei, R.; Fadda, G.; Frasoldati, A.; et al. Italian consensus on diagnosis and treatment of differentiated thyroid cancer: Joint statements of six Italian societies. J. Endocrinol. Investig. 2018, 41, 849–876. [Google Scholar] [CrossRef] [PubMed]
- Baudin, E.; Cao, C.D.; Cailleux, A.F.; Leboulleux, S.; Travagli, J.P.; Schlumberger, M. Positive Predictive Value of Serum Thyroglobulin Levels, Measured during the First Year of Follow-Up after Thyroid Hormone Withdrawal, in Thyroid Cancer Patients. J. Clin. Endocrinol. Metab. 2003, 88, 1107–1111. [Google Scholar] [CrossRef]
- Pacini, F.; Capezzone, M.; Elisei, R.; Ceccarelli, C.; Taddei, D.; Pinchera, A. Diagnostic 131-Iodine Whole-Body Scan May Be Avoided in Thyroid Cancer Patients Who Have Undetectable Stimulated Serum Tg Levels After Initial Treatment. J. Clin. Endocrinol. Metab. 2002, 87, 1499–1501. [Google Scholar] [CrossRef]
- Ashcraft, M.W.; Van Herle, A.J. The comparative value of serum thyroglobulin measurements and iodine 131 total body scans in the follow-up study of patients with treated differentiated thyroid cancer. Am. J. Med. 1981, 71, 806–814. [Google Scholar] [CrossRef]
- Padovani, R.P.; Robenshtok, E.; Brokhin, M.; Tuttle, R.M.; Santos, M.J.; Bugalho, M.J.; Zakavi, S.R.; Kashat, L.; Orlov, S.; Orlov, D.; et al. Even Without Additional Therapy, Serum Thyroglobulin Concentrations Often Decline for Years After Total Thyroidectomy and Radioactive Remnant Ablation in Patients with Differentiated Thyroid Cancer. Thyroid 2012, 22, 778–783. [Google Scholar] [CrossRef]
- Yim, J.H.; Kim, E.Y.; Kim, W.B.; Kim, T.Y.; Ryu, J.-S.; Gong, G.; Hong, S.J.; Yoon, J.H.; Shong, Y.K.; Cooper, D.S.; et al. Long-Term Consequence of Elevated Thyroglobulin in Differentiated Thyroid Cancer. Thyroid 2013, 23, 58–63. [Google Scholar] [CrossRef]
- Tramontin, M.Y.; Nobre, G.M.; Lopes, M.; Carneiro, M.P.; Alves, P.A.G.; de Andrade, F.A.; Vaisman, F.; Corbo, R.; Bulzico, D. High thyroglobulin and negative whole-body scan: No long-term benefit of empiric radioiodine therapy. Endocrine 2021, 73, 398–406. [Google Scholar] [CrossRef]
- Pace, L.; Klain, M.; Albanese, C.; Salvatore, B.; Storto, G.; Soricelli, A.; Salvatore, M. Short-term outcome of differentiated thyroid cancer patients receiving a second iodine-131 therapy on the basis of a detectable serum thyroglobulin level after initial treatment. Eur. J. Nucl. Med. Mol. Imaging 2005, 33, 179–183. [Google Scholar] [CrossRef]
- Salvatore, B.; Klain, M.; Nicolai, E.; D’Amico, D.; De Matteis, G.; Raddi, M.; Fonti, R.; Pellegrino, T.; Storto, G.; Cuocolo, A.; et al. Prognostic role of FDG PET/CT in patients with differentiated thyroid cancer treated with 131-iodine empiric therapy. Medicine 2017, 96, e8344. [Google Scholar] [CrossRef] [PubMed]
- Pace, L.; Klain, M.; Salvatore, B.; Nicolai, E.; Zampella, E.; Assante, R.; Pellegrino, T.; Storto, G.; Fonti, R.; Salvatore, M. Prognostic Role of 18F-FDG PET/CT in the Postoperative Evaluation of Differentiated Thyroid Cancer Patients. Clin. Nucl. Med. 2015, 40, 111–115. [Google Scholar] [CrossRef]
- Ryu, J.-S.; Kim, E.Y.; Lee, J.H.; Baek, J.H.; Yoon, J.H.; Hong, S.J.; Kim, E.S.; Kim, T.Y.; Kim, W.B.; Shong, Y.K. Empiric High-Dose 131-Iodine Therapy Lacks Efficacy for Treated Papillary Thyroid Cancer Patients with Detectable Serum Thyroglobulin, but Negative Cervical Sonography and 18F-Fluorodeoxyglucose Positron Emission Tomography Scan. J. Clin. Endocrinol. Metab. 2010, 95, 1169–1173. [Google Scholar] [CrossRef]
- Zampella, E.; Klain, M.; Pace, L.; Cuocolo, A. PET/CT in the management of differentiated thyroid cancer. Diagn. Interv. Imaging 2021, 102, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Kaliszewski, K.; Diakowska, D.; Nowak, Ł.; Wojtczak, B.; Rudnicki, J. The age threshold of the 8th edition AJCC classification is useful for indicating patients with aggressive papillary thyroid cancer in clinical practice. BMC Cancer 2020, 20, 1166. [Google Scholar] [CrossRef] [PubMed]

| Before Matching | After Matching | |||||||
|---|---|---|---|---|---|---|---|---|
| All Patients (n = 820) | No-ET (n = 701) | ET (n = 119) | p Value | All Patients (n = 238) | No-ET (n = 119) | ET (n = 119) | p Value | |
| Age (years) | 44 ± 15 | 44 ± 14 | 44 ± 17 | 0.69 | 45 ± 17 | 45 ± 17 | 44 ± 17 | 0.76 |
| Female gender, n (%) | 660 (80) | 567 (81) | 93 (78) | 0.49 | 183 (77) | 90 (76) | 93 (78) | 0.64 |
| ATA risk categories | ||||||||
| Low risk, n (%) | 201 (24) | 181 (26) | 20 (17) | <0.05 | 38 (16) | 19 (16) | 20 (17) | 0.85 |
| Intermediate risk, n (%) | 438 (54) | 382 (54) | 56 (47) | 0.11 | 105 (44) | 48 (40) | 56 (47) | 0.29 |
| High risk, n (%) | 181 (22) | 138 (20) | 43 (36) | <0.001 | 95 (40) | 52 (44) | 43 (36) | 0.23 |
| Follicular type, n (%) | 117 (14) | 94 (13) | 23 (19) | 0.09 | 40 (17) | 17 (14) | 23 (19) | 0.29 |
| Tumor size >2 cm, n (%) | 359 (44) | 294 (42) | 65 (55) | <0.01 | 140 (59) | 75 (63) | 65 (55) | 0.19 |
| Neck dissection, n (%) | 241 (29) | 197 (28) | 44 (37) | <0.05 | 88 (37) | 44 (37) | 44 (37) | 1 |
| Lymph node involvement, n (%) | 161 (20) | 125 (18) | 36 (30) | <0.01 | 68 (29) | 32 (27) | 36 (30) | 0.57 |
| Time interval surgery/RAI therapy (days) | 132 ± 194 | 670 ± 61 | 124 ± 159 | 0.06 | 735 ± 480 | 125 ± 116 | 124 ± 159 | 0.37 |
| Administered 131I activity (MBq) | 3368 ± 1034 | 982 ± 38 | 1266 ± 119 | <0.001 | 3652 ± 1073 | 3640 ± 871 | 1266 ± 119 | 0.769 |
| Pre-therapy Tg (ng/mL) | 34 ± 98 | 25 ± 83 | 88 ± 146 | <0.001 | 74 ± 132 | 60 ± 115 | 88 ± 146 | 0.481 |
| Neck uptake at WBS, n (%) | 802 (98) | 685 (98) | 117 (98) | 0.68 | 233 (98) | 116 (97) | 117 (98) | 0.65 |
| 12-month follow-up Tg (ng/mL) | 17 ± 19 | 17 ± 18 | 14 ± 18 | 0.67 | 12 ± 18 | 9 ± 19 | 14 ± 18 | 0.07 |
| Event (n = 57) | No Event (n = 181) | p Value | |
|---|---|---|---|
| Age (years) | 53 ± 17 | 42 ± 16 | <0.001 |
| Female gender, n (%) | 38 (67) | 145 (80) | <0.05 |
| ATA risk categories | |||
| Low risk, n (%) | 6 (11) | 33 (188) | 0.17 |
| Intermediate risk, n (%) | 19 (33) | 84 (46) | 0.08 |
| High risk, n (%) | 32 (56) | 64 (35) | <0.01 |
| Follicular type, n (%) | 25 (44) | 88 (49) | 0.52 |
| Tumor size >2 cm, n (%) | 35 (61) | 105 (58) | 0.65 |
| Neck dissection, n (%) | 26 (46) | 62 (34) | 0.12 |
| Lymph node involvement, n (%) | 21 (37) | 47 (26) | 0.11 |
| Time interval surgery/RAI therapy (days) | 140 ± 134 | 155 ± 550 | 0.74 |
| Administered 131I activity (MBq) | 3863 ± 1157 | 3580 ± 1037 | 0.08 |
| Pre-therapy Tg (ng/mL) | 109 ± 148 | 62 ± 125 | <0.01 |
| Neck uptake at WBS, n (%) | 56 (98) | 177 (98) | 0.44 |
| 12-month follow-up Tg (ng/mL) | 10 ± 17 | 15 ± 21 | 0.06 |
| Empiric therapy, n (%) | 21 (37) | 98 (54) | <0.05 |
| No empiric therapy, n (%) | 36 (63) | 83 (46) | <0.05 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value | |
| Age | 10.3 (1.01–1.05) | <0.001 | 1.03 (1.01–1.05) | <0.01 |
| Female sex | 0.49 (0.28–0.86) | <0.05 | 0.62 (0.35–1.11) | 0.11 |
| ATA risk categories | ||||
| Low risk (reference) | ||||
| Intermediate risk | 1.25 (0.61–3.83) | 0.36 | 1.60 (0.62–4.12) | 0.33 |
| High risk | 3.01 (1.22–7.24) | <0.05 | 2.04 (0.37–4.95) | 0.12 |
| Pre-therapy Tg ng/mL | 1.00 (1.00–1.01) | <0.01 | 1.00 (1.00–1.01) | <0.05 |
| Empiric RAI therapy | 14.2 (4.11–48.7) | <0.001 | 0.43 (0.24–0.75) | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piscopo, L.; Zampella, E.; Volpe, F.; Gaudieri, V.; Nappi, C.; Cutillo, P.; Volpicelli, F.; Falzarano, M.; Pace, L.; Cuocolo, A.; et al. Efficacy of Empirical Radioiodine Therapy in Patients with Differentiated Thyroid Cancer and Elevated Serum Thyroglobulin without Evidence of Structural Disease: A Propensity Score Analysis. Cancers 2023, 15, 4196. https://doi.org/10.3390/cancers15164196
Piscopo L, Zampella E, Volpe F, Gaudieri V, Nappi C, Cutillo P, Volpicelli F, Falzarano M, Pace L, Cuocolo A, et al. Efficacy of Empirical Radioiodine Therapy in Patients with Differentiated Thyroid Cancer and Elevated Serum Thyroglobulin without Evidence of Structural Disease: A Propensity Score Analysis. Cancers. 2023; 15(16):4196. https://doi.org/10.3390/cancers15164196
Chicago/Turabian StylePiscopo, Leandra, Emilia Zampella, Fabio Volpe, Valeria Gaudieri, Carmela Nappi, Paolo Cutillo, Federica Volpicelli, Maria Falzarano, Leonardo Pace, Alberto Cuocolo, and et al. 2023. "Efficacy of Empirical Radioiodine Therapy in Patients with Differentiated Thyroid Cancer and Elevated Serum Thyroglobulin without Evidence of Structural Disease: A Propensity Score Analysis" Cancers 15, no. 16: 4196. https://doi.org/10.3390/cancers15164196
APA StylePiscopo, L., Zampella, E., Volpe, F., Gaudieri, V., Nappi, C., Cutillo, P., Volpicelli, F., Falzarano, M., Pace, L., Cuocolo, A., & Klain, M. (2023). Efficacy of Empirical Radioiodine Therapy in Patients with Differentiated Thyroid Cancer and Elevated Serum Thyroglobulin without Evidence of Structural Disease: A Propensity Score Analysis. Cancers, 15(16), 4196. https://doi.org/10.3390/cancers15164196








