PSMA-RLT in Patients with Metastatic Hormone-Sensitive Prostate Cancer: A Retrospective Study
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Cohort Population
2.2. PSMA Imaging and Therapy
2.3. Outcomes
2.4. Statistical Analysis
2.5. Ethics
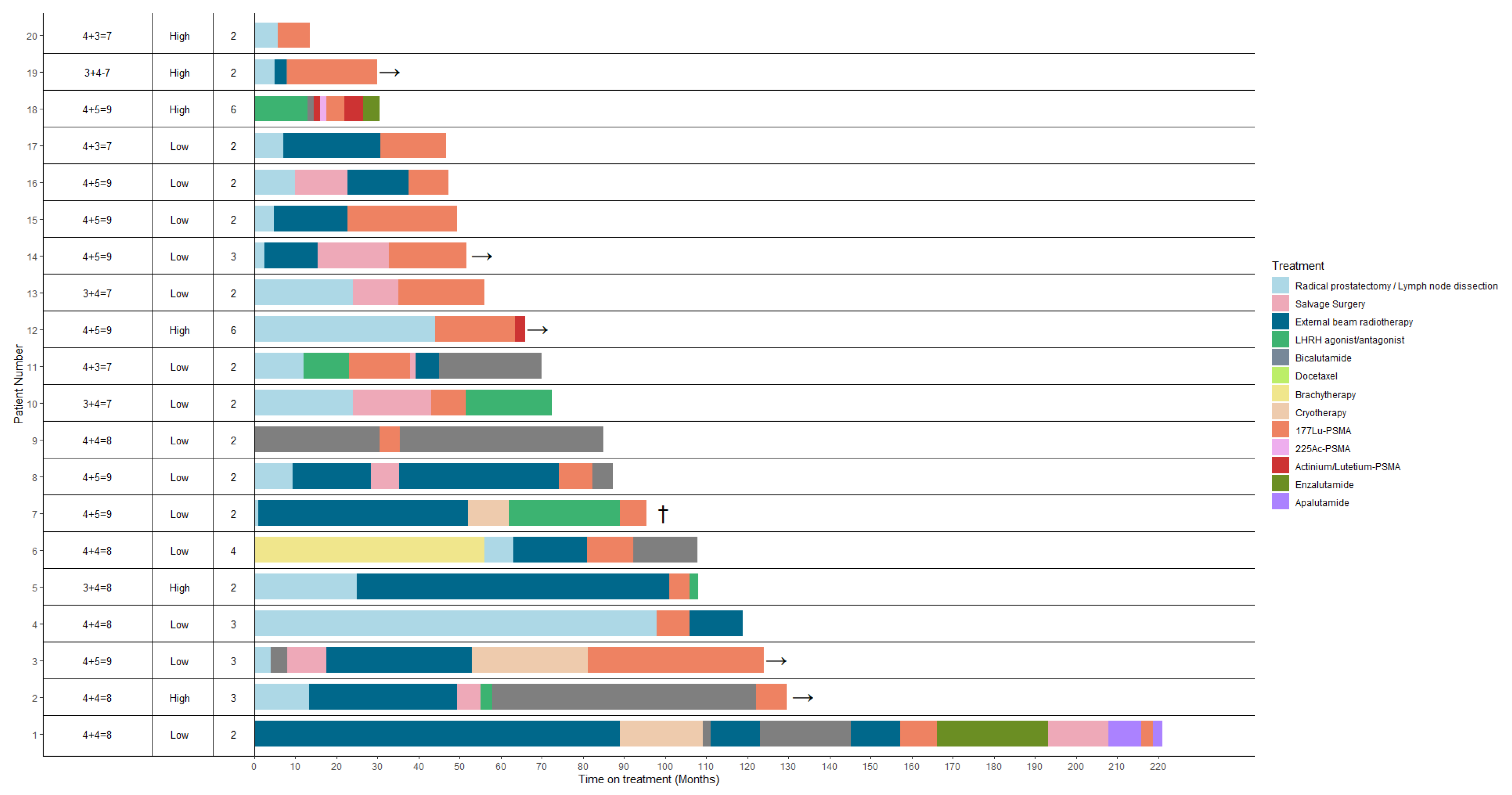
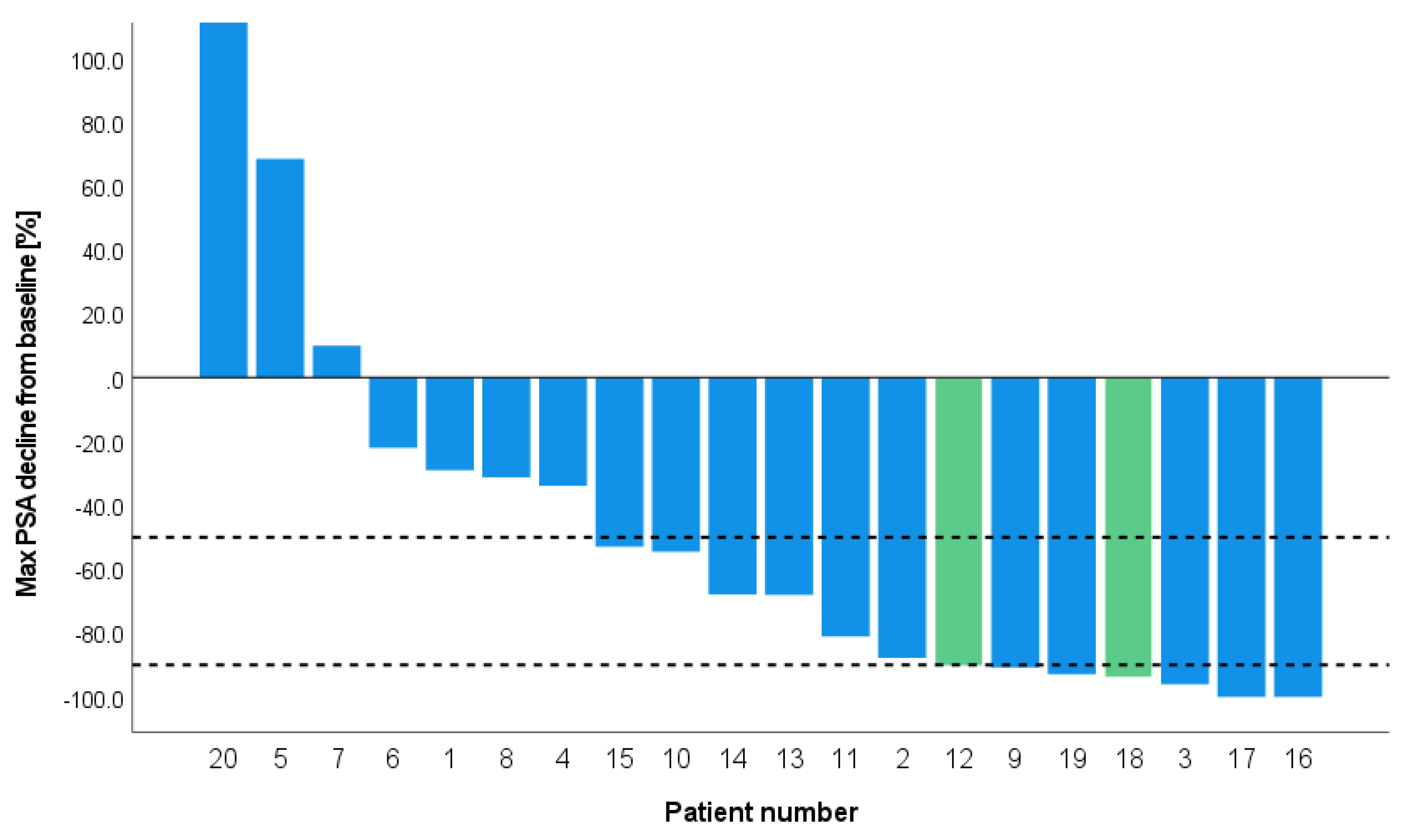
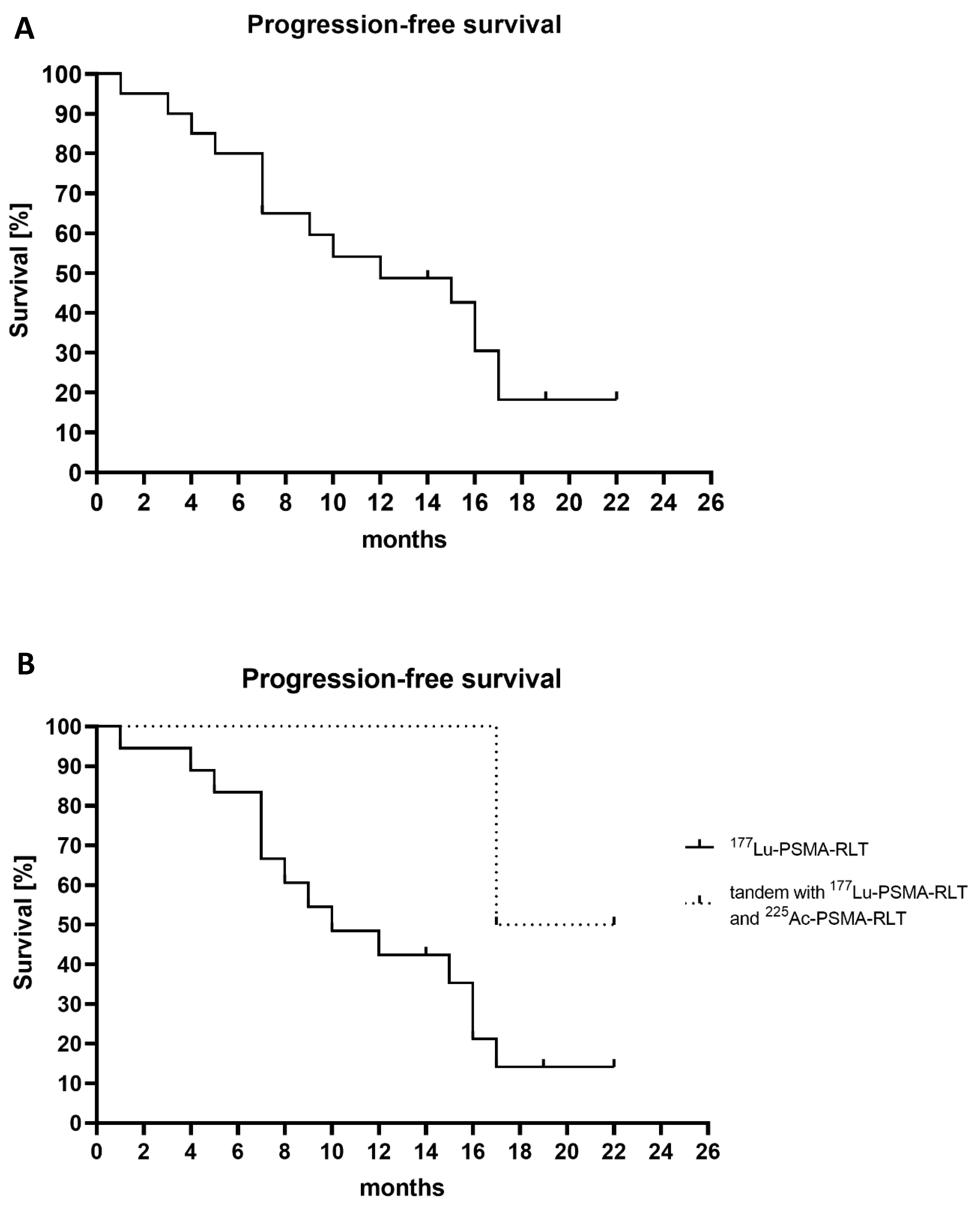
3. Results
3.1. Baseline Characteristics
3.2. Toxicity
3.3. Treatment Outcome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, H.; Daneshmand, S. Androgen deprivation therapy: Evidence-based management of side effects. BJU Int. 2013, 111, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.J.; De Bono, J.S.; Chi, K.N.; Fizazi, K.; Herrmann, K.; Rahbar, K.; Tagawa, S.T.; Nordquist, L.T.; Vaishampayan, N.; El-Haddad, G.; et al. Phase III study of lutetium-177-PSMA-617 in patients with metastatic castration-resistant prostate cancer (VISION). J. Clin. Oncol. 2021, 39, LBA4. [Google Scholar] [CrossRef]
- Privé, B.M.; Peters, S.M.B.; Muselaers, C.H.J.; van Oort, I.M.; Janssen, M.J.R.; Sedelaar, J.P.M.; Konijnenberg, M.W.; Zámecnik, P.; Uijen, M.J.M.; Schilham, M.G.M.; et al. Lutetium-177-PSMA-617 in low-volume hormone-sensitive metastatic prostate cancer: A prospective pilot study. Clin. Cancer Res. 2021, 27, 3595–3601. [Google Scholar] [CrossRef]
- Peters, S.M.B.; Privé, B.M.; de Bakker, M.; de Lange, F.; Jentzen, W.; Eek, A.; Muselaers, C.H.J.; Mehra, N.; Witjes, J.A.; Gotthardt, M.; et al. Intra-therapeutic dosimetry of [177Lu]Lu-PSMA-617 in low-volume hormone-sensitive metastatic prostate cancer patients and correlation with treatment outcome. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 460–469. [Google Scholar] [CrossRef]
- Privé, B.M.; Janssen, M.J.R.; van Oort, I.M.; Muselaers, C.H.J.; Jonker, M.A.; de Groot, M.; Mehra, N.; Verzijlbergen, J.F.; Scheenen, T.W.J.; Zámecnik, P.; et al. Lutetium-177-PSMA-I&T as metastases directed therapy in oligometastatic hormone sensitive prostate cancer, a randomized controlled trial. BMC Cancer. 2020, 20, 884. [Google Scholar]
- Privé, B.M.; Janssen, M.J.R.; van Oort, I.M.; Muselaers, C.H.J.; Jonker, M.A.; van Gemert, W.A.; de Groot, M.; Westdorp, H.; Mehra, N.; Verzijlbergen, J.F.; et al. Update to a randomized controlled trial of lutetium-177-PSMA in Oligo-metastatic hormone-sensitive prostate cancer: The BULLSEYE trial. Trials 2021, 22, 768. [Google Scholar] [CrossRef]
- Privé, B.M.; Slootbeek, P.H.J.; Laarhuis, B.I.; Naga, S.P.; van der Doelen, M.J.; van Kalmthout, L.W.M.; de Keizer, B.; Ezziddin, S.; Kratochwil, C.; Morgenstern, A.; et al. Impact of DNA damage repair defects on response to PSMA radioligand therapy in metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis. 2021, 25, 71–78. [Google Scholar] [CrossRef]
- Rahbar, K.; Ahmadzadehfar, H.; Kratochwil, C.; Haberkorn, U.; Schafers, M.; Essler, M.; Baum, R.P.; Kulkarni, H.R.; Schmidt, M.; Drzezga, A.; et al. German multicenter study investigating 177Lu-PSMA-617 radioligand therapy in advanced prostate cancer patients. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2017, 58, 85–90. [Google Scholar]
- Khreish, F.; Ebert, N.; Ries, M.; Maus, S.; Rosar, F.; Bohnenberger, H.; Stemler, T.; Saar, M.; Bartholomä, M.; Ezziddin, S. 225Ac-PSMA-617/177Lu-PSMA-617 tandem therapy of metastatic castration-resistant prostate cancer: Pilot experience. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 721–728. [Google Scholar] [CrossRef]
- Sathekge, M.; Bruchertseifer, F.; Knoesen, O.; Reyneke, F.; Lawal, I.; Lengana, T.; Davis, C.; Mahapane, J.; Corbett, C.; Vorster, M. Morgenstern A225Ac-PSMA-617 in chemotherapy-naive patients with advanced prostate cancer: A pilot study. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Sathekge, M.; Bruchertseifer, F.; Vorster, M.; Lawal, I.O.; Knoesen, O.; Mahapane, J.; Davis, C.; Reyneke, F.; Maes, A.; Kratochwil, C.; et al. Predictors of overall and disease-free survival in metastatic castration-resistant prostate cancer patients receiving 225Ac-PSMA-617 radioligand therapy. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2020, 61, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Van der Doelen, M.J.; Mehra, N.; van Oort, I.M.; Looijen-Salamon, M.G.; Janssen, M.J.R.; Custers, J.A.E.; Slootbeek, P.H.J.; Kroeze, L.I.; Bruchertseifer, F.; Morgenstern, A.; et al. Clinical outcomes and molecular profiling of advanced metastatic castration-resistant prostate cancer patients treated with 225Ac-PSMA-617 targeted alpha-radiation therapy. Urol. Onco. Semin. Orig. Investig. 2021, 39, 729.e7–729.e16. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Haberkorn, U.; Giesel, F.L. 225Ac-PSMA-617 for therapy of prostate cancer. Semin. Nucl. Med. 2020, 50, 133–140. [Google Scholar] [CrossRef]
- Cardinale, J.; Schafer, M.; Benesova, M.; Bauder-Wust, U.; Leotta, K.; Eder, M.; Neels, O.C.; Haberkorn, U.; Giesel, F.L.; Kopka, K. Preclinical evaluation of 18F-PSMA-1007, a new prostate-specific membrane antigen ligand for prostate cancer imaging. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2017, 58, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Fendler, W.P.; Calais, J.; Eiber, M.; Flavell, R.R.; Mishoe, A.; Feng, F.Y.; Nguyen, H.G.; Reiter, R.E.; Rettig, M.B.; Okamoto, S.; et al. Assessment of 68Ga-PSMA-11 PET accuracy in localizing recurrent prostate cancer: A prospective single-arm clinical trial. JAMA Oncol. 2019, 5, 856–863. [Google Scholar] [CrossRef]
- Kratochwil, C.; Bruchertseifer, F.; Giesel, F.L.; Weis, M.; Verburg, F.A.; Mottaghy, F.; Kopka, K.; Apostolidis, C.; Haberkorn, U.; Morgenstern, A. 225Ac-PSMA-617 for PSMA-targeted alpha-radiation therapy of metastatic castration-resistant prostate cancer. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2016, 57, 1941–1944. [Google Scholar]
- Kratochwil, C.; Giesel, F.L.; Stefanova, M.; Benesova, M.; Bronzel, M.; Afshar-Oromieh, A.; Mier, W.; Eder, M.; Kopka, K.; Haberkorn, U. PSMA-targeted radionuclide therapy of metastatic castration-resistant prostate cancer with 177Lu-Labeled PSMA-617. J. Nucl. Med. Off. Publ. Soc. Nucl. Med. 2016, 57, 1170–1176. [Google Scholar] [CrossRef]
- Aluwini, S.S.; Mehra, N.; Lolkema, M.P.; Oprea-Lager, D.E.; Yakar, D.; Stoevelaar, H.; van der Poel, H.; Dutch Oligometastatic Prostate Cancer Working Group; Busstra, M.; de Jong, I.-J.; et al. Oligometastatic prostate cancer: Results of a Dutch multidisciplinary consensus meeting. Eur. Urol. Oncol. 2019, 3, 231–238. [Google Scholar] [CrossRef]
- Scher, H.I.; Morris, M.J.; Stadler, W.M.; Higano, C.; Basch, E.; Fizazi, K.; Antonarakis, E.S.; Beer, T.M.; Carducci, M.A.; Chi, K.N.; et al. Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the prostate cancer clinical trials working group 3. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2016, 34, 1402–1418. [Google Scholar] [CrossRef]
- Cornford, P.; van den Bergh, R.C.N.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Santis, M.D.; Fanti, S.; Fossati, N.; Gandaglia, G.; et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II—2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer. Eur. Urol. 2021, 79, 263–282. [Google Scholar] [CrossRef] [PubMed]
- Sartor, O.; de Bono, J.; Chi, K.N.; Fizazi, K.; Herrmann, K.; Rahbar, K.; Tagawa, S.T.; Nordquist, L.T.; Vaishampayan, N.; El-Haddad, G.; et al. Lutetium-177–PSMA-617 for metastatic castration-resistant prostate cancer. N. Engl. J. Med. 2021, 385, 1091–1103. [Google Scholar] [CrossRef] [PubMed]
- Thiele, N.A.; Wilson, J.J. Actinium-225 for targeted α therapy: Coordination chemistry and current chelation approaches. Cancer Biother. Radiopharm. 2018, 33, 336–348. [Google Scholar] [CrossRef] [PubMed]
- Satapathy, S.; Das, N.; Sood, A.; Singh, S.K.; Goyal, S.; Madan, R.; Mittal, B.R. Short-course 177Lu-PSMA-617 radioligand therapy in high-volume metastatic hormone-sensitive prostate cancer: Time to take the leap? Eur. Urol. 2021, 80, 390–392. [Google Scholar] [CrossRef] [PubMed]
- Demirkol, M.O.; Kiremit, M.C.; Acar, O.; Falay, O.; Ucar, B.; Esen, T. local salvage treatment of post-brachytherapy recurrent prostate cancer via theranostic application of PSMA-labeled lutetium-177. Clin. Genitourin. Cancer 2018, 16, 99–102. [Google Scholar] [CrossRef]
- Hofman, M.S.; Emmett, L.; Sandhu, S.; Iravani, A.; Joshua, A.M.; Goh, J.C.; Pattison, D.A.; Tan, T.H.; Kirkwood, I.D.; Ng, S.; et al. [177Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): A randomised, open-label, phase 2 trial. Lancet 2021, 397, 797–804. [Google Scholar] [CrossRef]
- Heck, M.M.; Tauber, R.; Schwaiger, S.; Retz, M.; D’Alessandria, C.; Maurer, T.; Gafita, A.; Wester, H.J.; Gschwend, J.E.; Weber, W.A.; et al. Treatment outcome, toxicity, and predictive factors for radioligand therapy with 177Lu-PSMA-I&T in metastatic castration-resistant prostate cancer. Eur. Urol. 2019, 75, 920–926. [Google Scholar]
- Hofman, M.S.; Violet, J.; Hicks, R.J.; Ferdinandus, J.; Thang, S.P.; Akhurst, T.; Iravani, A.; Kong, G.; Ravi Kumar, A.; Murphy, D.G.; et al. [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): A single-centre, single-arm, phase 2 study. Lancet Oncol. 2018, 19, 825–833. [Google Scholar] [CrossRef]
- Phillips, R.; Shi, W.Y.; Deek, M.; Radwan, N.; Lim, S.J.; Antonarakis, E.S.; Rowe, S.P.; Ross, A.E.; Gorin, M.A.; Deville, C.; et al. Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: The ORIOLE phase 2 randomized clinical trial. JAMA Oncol. 2020, 6, 650–659. [Google Scholar] [CrossRef]
- Iravani, A.; Violet, J.; Azad, A.; Hofman, M.S. Lutetium-177 prostate-specific membrane antigen (PSMA) theranostics: Practical nuances and intricacies. Prostate Cancer Prostatic Dis. 2020, 23, 38–52. [Google Scholar] [CrossRef]
- Violet, J.; Jackson, P.; Ferdinandus, J.; Sandhu, S.; Akhurst, T.; Iravani, A.; Kong, G.; Kumar, A.R.; Thang, S.P.; Eu, P.; et al. Dosimetry of 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer: Correlations between pretherapeutic imaging and whole-body tumor dosimetry with treatment outcomes. J. Nucl. Med.: Off. Publ. Soc. Nucl. Med. 2019, 60, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Gaertner, F.C.; Halabi, K.; Ahmadzadehfar, H.; Kurpig, S.; Eppard, E.; Kotsikopoulos, C.; Liakos, N.; Bundschuh, R.A.; Strunk, H.; Essler, M. Uptake of PSMA-ligands in normal tissues is dependent on tumor load in patients with prostate cancer. Oncotarget 2017, 8, 55094–55103. [Google Scholar] [CrossRef]
- Edler von Eyben, F.; Singh, A.; Zhang, J.; Nipsch, K.; Meyrick, D.; Lenzo, N.; Kairemo, K.; Joensuu, T.; Virgolini, I.; Soydal, C.; et al. 177Lu-PSMA radioligand therapy of predominant lymph node metastatic prostate cancer. Oncotarget 2019, 10, 2451–2461. [Google Scholar] [CrossRef][Green Version]
- Paschalis, A.; Sheehan, B.; Riisnaes, R.; Rodrigues, D.N.; Gurel, B.; Bertan, C.; Ferreira, A.; Lambros, M.B.K.; Seed, G.; Yuan, W.; et al. Prostate-specific membrane antigen heterogeneity and DNA repair defects in prostate cancer. Eur. Urol. 2019, 76, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Gafita, A.; Calais, J.; Grogan, T.R.; Hadaschik, B.; Wang, H.; Weber, M.; Sandhu, S.; Kratochwil, C.; Esfandiari, R.; Tauber, R.; et al. Nomograms to predict outcomes after 177Lu-PSMA therapy in men with metastatic castration-resistant prostate cancer: An international, multicentre, retrospective study. Lancet Oncol. 2021, 22, 1115–1125. [Google Scholar] [CrossRef]
- Peters, S.M.B.; Hofferber, R.; Privé, B.M.; de Bakker, M.; Gotthardt, M.; Janssen, M.; de Lange, F.; Muselaers, C.H.J.; Mehra, N.; Witjes, J.A.; et al. [68Ga]Ga-PSMA-11 PET imaging as a predictor for absorbed doses in organs at risk and small lesions in [177Lu]Lu-PSMA-617 treatment. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Privé, B.M.; Derks, Y.H.W.; Rosar, F.; Franssen, G.M.; Peters, S.M.B.; Khreish, F.; Bartholomä, M.; Maus, S.; Gotthardt, M.; Laverman, P.; et al. 89Zr-labeled PSMA ligands for pharmacokinetic PET imaging and dosimetry of PSMA-617 and PSMA-I&T: A preclinical evaluation and first in man. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 2064–2076. [Google Scholar] [PubMed]
- Müller, C.; Umbricht, C.A.; Gracheva, N.; Tschan, V.J.; Pellegrini, G.; Bernhardt, P.; Zeevaart, J.R.; Köster, U.; Schibli, R.; van der Meulen, N.P. Terbium-161 for PSMA-targeted radionuclide therapy of prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1919–1930. [Google Scholar] [CrossRef]
- Müller, C.; Vermeulen, C.; Köster, U.; Johnston, K.; Türler, A.; Schibli, R.; Schibli, R.; van der Meulen, N.P. Alpha-PET with terbium-149: Evidence and perspectives for radiotheragnostics. EJNMMI Radiopharm. Chem. 2016, 1, 5. [Google Scholar] [CrossRef]
- Hindié, E.; Zanotti-Fregonara, P.; Quinto, M.A.; Morgat, C.; Champion, C. Dose deposits from 90Y, 177Lu, 111In, and 161Tb in micrometastases of various sizes: Implications for radiopharmaceutical therapy. J. Nucl. Med. 2016, 57, 759–764. [Google Scholar] [CrossRef]
- Uusijärvi, H.; Bernhardt, P.; Rösch, F.; Maecke, H.R.; Forssell-Aronsson, E. Electron- and positron-emitting radiolanthanides for therapy: Aspects of dosimetry and production. J. Nucl. Med.: Off. Publ. Soc. Nucl. Med. 2006, 47, 807–814. [Google Scholar]
- Morris, M.J.; Corey, E.; Guise, T.A.; Gulley, J.L.; Kevin Kelly, W.; Quinn, D.I.; Quinn, D.I.; Scholz, A.; Sgouros, G. Radium-223 mechanism of action: Implications for use in treatment combinations. Nat. Rev. Urol. 2019, 16, 745–756. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | mHSPC Total (n = 20) | a Tandem of 177Lu-PSMA and 225Ac-PSMA (n = 2) | b 177Lu-PSMA (n = 18) |
|---|---|---|---|
| Age, median (IQR) PSA doubling time >6 months, n (%) | 69 (65.5–74) 5 (25%) | 76 (72–80) 1 (50%) | 68 (64.8–73.3) 4 (22.2%) |
| Previous treatments Radical Prostatectomy, n(%) PLND, n(%) External beam radiotherapy, n (%) Focal Cryotherapy, n(%) Hormonal therapy, n (%)
| 15 (75%) 15 (75%) 15 (75%) 3 (15%) 8 (40%) 3 (15%) 7 (35%) 2 (10%) | 1 (50%) 0 0 0 1 (50%) 1 (50%) 1 (50%) 1 (50%) | 14 (77.8%) 15 (83.3%) 15 (83.3%) 3 (16.7%) 7 (38.9%) 2 (11.1%) 6 (33.3%) 1 (5.6%) |
| Site of disease on PSMA-PET/CT scan * Low volume disease, n (%) Hottest lesion, SUVmax, median (IQR) Lymph nodes, n (%) Bone, n (%) Visceral, n (%) | 16 (80%) 28.8 (11.5–36.3) 20 (100%) 6 (30%) 1 (5%) | 0 (0%) 49.1 (44.3–53.8) 2 (100%) 1 (50%) 1 (50%) | 16 (88.9%) 20.4 (11.1–32.4) 18 (100%) 5 (27.8%) 0 (0%) |
| PSMA radioligand therapy Total number of PSMA-RLT cycles median (range) Administered activity of 177Lu (GBq), per cycle median (IQR) Administered activity of 225Ac (MBq) per cycle median (IQR) | 2 (1–6) 6.2 (5.7–7.4) 4.2 (2.0–6.0) | 6 (6–6) 7.2 (5.7–7.4) 4.2 (2.0–6.0) | 2 (1–4) 6.1 (4.5–7.4) 0 (0–0) |
| Blood analysis Baseline Hemoglobin (mmol/L), median (IQR) Leukocytes (×109/L), median (IQR) Thrombocytes (×109/L), median (IQR) eGFR (mL/min), median (IQR) Creatinine (µmol/L), median (IQR) Alkaline phosphatase (U/L), median (IQR) Lactate dehydrogenase (U/L), median (IQR) PSA (µg/L), median (IQR) | 8.9 (8.4–9.4) 5.7 (4.3–7.5) 232 (175–249) 79.9 (72–90) 81 (75–89) 63 (55.3–71.5) 196 (174–218) 5.9 (1.8–16.9) | 9.5 (9.1–10) 6.1 (6–6.2) 204 (178–229) 77 (77–78) 85 (84–87) 85.0 (72–98) 204.5 (192–217) 146 (20–272) | 8.8 (8.4–9.4) 5.3 (4.1–8.8) 238 (174–250) 84 (71–90) 80 (75–90) 59.5 (54.8–70) 195.5 (172–219) 5.1 (1.8–12.8) |
| Grade 1 | Grade 2 | Grade ≥ 3 | |
|---|---|---|---|
| Xerostomia | 6 (30%) * | 1 (5%) | 0 |
| Fatigue | 8 (40%) * | 1 (5%) | 0 |
| Nausea | 4 (20%) | 0 | 0 |
| Anemia | 1 (5.0%) | 0 | 1 (5%) * |
| Thrombocytopenia | 0 | 0 | 1 (5%) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banda, A.; Privé, B.M.; Allach, Y.; Uijen, M.J.M.; Peters, S.M.B.; Loeff, C.C.; Gotthardt, M.; Muselaers, C.H.J.; Witjes, J.A.; van Oort, I.M.; et al. PSMA-RLT in Patients with Metastatic Hormone-Sensitive Prostate Cancer: A Retrospective Study. Cancers 2023, 15, 297. https://doi.org/10.3390/cancers15010297
Banda A, Privé BM, Allach Y, Uijen MJM, Peters SMB, Loeff CC, Gotthardt M, Muselaers CHJ, Witjes JA, van Oort IM, et al. PSMA-RLT in Patients with Metastatic Hormone-Sensitive Prostate Cancer: A Retrospective Study. Cancers. 2023; 15(1):297. https://doi.org/10.3390/cancers15010297
Chicago/Turabian StyleBanda, Amina, Bastiaan M. Privé, Youssra Allach, Maike J. M. Uijen, Steffie M. B. Peters, Cato C. Loeff, Martin Gotthardt, Constantijn H. J. Muselaers, J. Alfred Witjes, Inge M. van Oort, and et al. 2023. "PSMA-RLT in Patients with Metastatic Hormone-Sensitive Prostate Cancer: A Retrospective Study" Cancers 15, no. 1: 297. https://doi.org/10.3390/cancers15010297
APA StyleBanda, A., Privé, B. M., Allach, Y., Uijen, M. J. M., Peters, S. M. B., Loeff, C. C., Gotthardt, M., Muselaers, C. H. J., Witjes, J. A., van Oort, I. M., Sedelaar, J. P. M., Westdorp, H., Mehra, N., Khreish, F., Ezziddin, S., Sabet, A., Kreissl, M. C., Winkens, T., Seifert, P., ... Nagarajah, J. (2023). PSMA-RLT in Patients with Metastatic Hormone-Sensitive Prostate Cancer: A Retrospective Study. Cancers, 15(1), 297. https://doi.org/10.3390/cancers15010297









