1. Introduction
Considerable efforts have been invested in recent years in the development of less toxic effective drugs for targeted cancer therapy. Currently, this diverse group of drugs includes monoclonal antibodies, immunomodulators (such as PD-1 or PDL-1 inhibitors), proteasome inhibitors, tyrosine kinase inhibitors, and deacetylation agents [
1,
2]. Another approach to treating malignancies is the use of chimeric proteins. Chimeric proteins, designed and constructed by gene fusion techniques, comprise both a cell-targeting component and an active component. Over the last few years, we have utilized human pro-apoptotic proteins as the active components of chimeric proteins [
3]. Here, we propose for the first time to explore the possibility of using components of the ubiquitin protein degradation system to induce death of target cells. We hypothesize that upon entry of the chimeric protein into cancerous cells, it will induce downstream degradation processes, leading to cell death. In this way, the cancer cells will program their own death in a non-inflammatory pathway. To test our hypothesis, we chose to use the known targeting molecule interleukin 2 (IL-2)
, a monomeric, secreted glycoprotein known mainly as a T cell growth factor [
4].
IL-2 is the natural ligand of the IL2 receptor (IL-2R), which is composed of a complex of three subunits, IL-2Rα (CD25), IL-2Rβ (CD122), and IL-2Rγc (CD132). The high-affinity (Kd = 10
−11 M) IL-2R contains all three subunits [
5]. High IL-2Rα expression, which increases the affinity to IL-2, has been demonstrated in an array of abnormal cells including malignant cells in patients with adult T-cell leukemia, cutaneous T-cell lymphoma, anaplastic large-cell lymphoma, hairy cell B-cell leukemia, and the Reed Sternberg and associated polyclonal T cells in Hodgkin’s disease as well as acute and chronic granulocytic leukemia cells [
6,
7]. As a targeting component, IL-2 has been proven to be successful in creating specificity to the targeted cell as a result of the high affinity to the IL-2R, which is over-expressed on activated lymphocytes and is involved in many human diseases [
8,
9].
An example of an IL2-based chimeric protein is the FDA-approved drug Ontak
®, a fusion molecule of diphtheria toxin domains linked to IL2 (IL2-DT), which due to production issues was discontinued for use in humans. A new version, E7777, which shares an amino acid sequence with IL2-DT, but has improved purity and an increased percentage of active monomer, has received regulatory approval for use in Japan and is in the process of approval by the FDA in the USA [
10,
11]. Another example of an immunotoxin with FDA approval is Moxetumomab pasudotox-tdfk (LUMOXITI™), an anti CD22 recombinant immunotoxin, for the treatment of hairy cell leukemia [
12].
However, a major impediment to the success of such chimeras is the human immune response they elicit, mainly against the bacterial killing component. It is clear that in order to avoid immunogenicity, the killing component has to be of human origin. Therefore, a new generation of chimeric proteins was developed in our lab, mainly composed of human, non-immunogenic toxins, taking advantage of apoptosis-inducing proteins as novel killing components, such as IL2-Bax [
13,
14]. These targeting molecules are still at the stage of pre-clinical evaluation and meanwhile we are continuing our search for a new human-based killing component, which would cause a natural cell death. As part of this search, we decided to utilize the natural components of the cells’ protein degradation system.
The degradation pathway for many proteins is via the ubiquitin proteasome system (UPS). This system is mostly controlled by a cascade that involves several types of enzymes including E1, ubiquitin activating enzymes; E2, ubiquitin-conjugating enzymes; and E3, ubiquitin–protein ligases [
15]. E3 enzymes, also known as ubiquitin ligases, contain substrate-specific recognition domains and catalyze the final step in ubiquitin transfer. The human genome encodes several types of E3 ligases that are mainly characterized by the presence of a HECT (homologous to E6-associated protein C-terminus), a RING (really interesting new gene) or a U-box domain [
16]. While RING and U-box E3 ligases act as scaffolding proteins that bring substrates and E2 enzymes together, HECT E3 ligases can directly catalyze the conjugation of the ubiquitin molecule to the target protein [
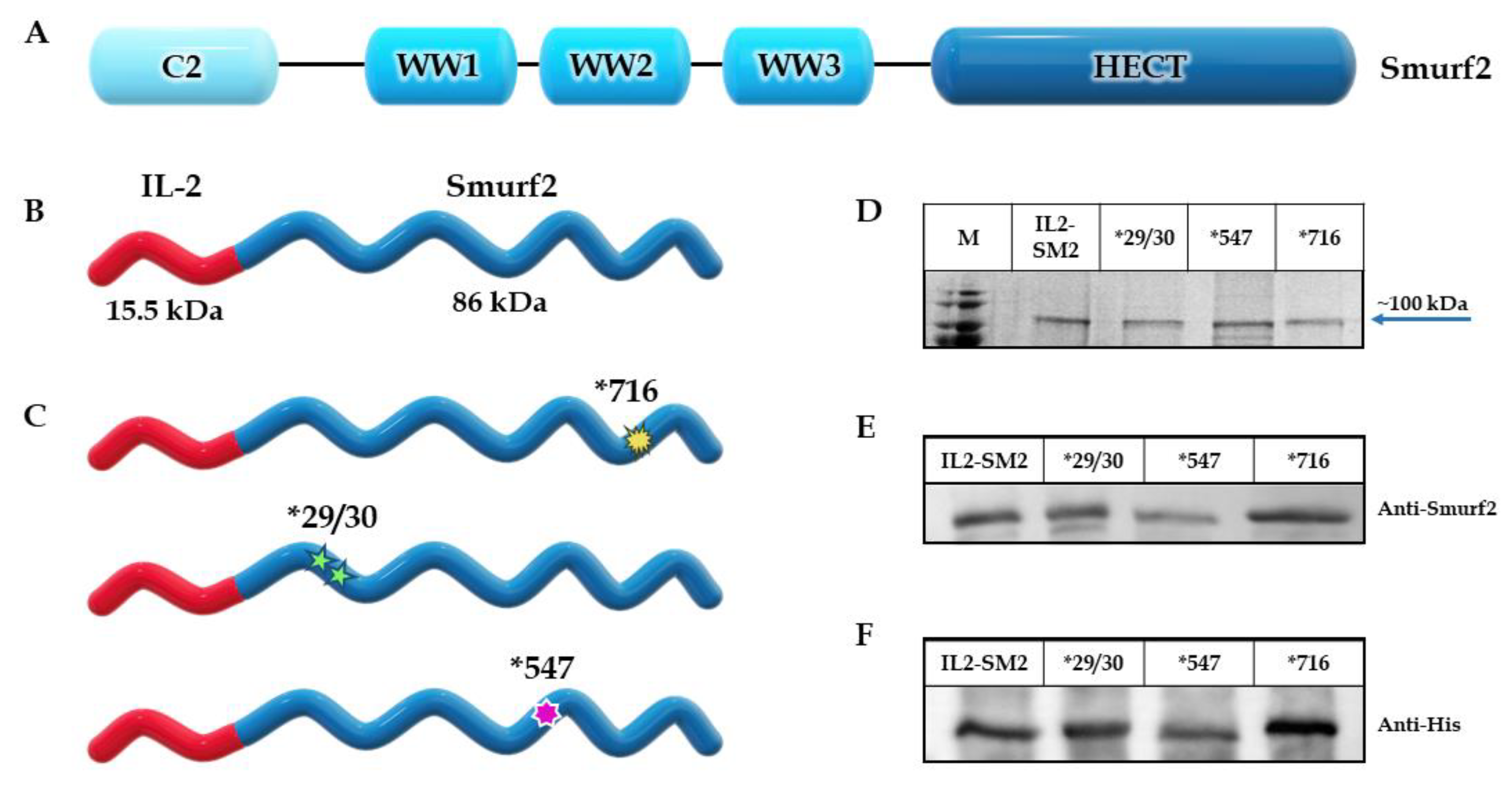
17]. Smad ubiquitylation regulatory factor 2 (Smurf2) is a member of the HECT family of ligases (with a C2-WW-HECT architecture). Smurf2 has 748 amino acids (86 kDa) and is involved in many biological processes in which it controls the stability of several important proteins with central roles in cell-cycle progression, proliferation, metastasis, genomic stability, senescence and more [
18]. In addition, Smurf2 has a critical role in the regulation of many signaling pathways, such as transforming growth factor β (TGF-β) and bone morphogenetic protein (BMP) signaling pathways [
19,
20], as well as the Wnt [
21] and RhoA pathways [
22]. Smurf2-deficient mice have increased susceptibility to spontaneous tumorigenesis in various tissues including the liver, lung, pituitary and mammary gland [
23,
24].
In addition, mice deficient in the E3 ubiquitin ligase Smurf2 spontaneously develop B-cell lymphomas that resemble human diffuse large B-cell lymphoma (DLBCL) with molecular features of germinal center or post-germinal center B cells [
25]. Smurf2 expression was also significantly decreased in primary human DLBCL samples, and low levels of Smurf2 expression correlated with inferior survival in DLBCL patients [
26].
Protein levels of Smurf2 were found to be lower in human lymphoma and breast cancer tissues relative to non-cancer tissues [
24]. In a study of prostate cancers, Smurf2 mRNA levels were lower in advanced tumors compared to less advanced organ-confined tumors, suggesting an association of Smurf2 downregulation with tumor progression [
27]. The ability of Smurf2 to ubiquitinate and degrade RNF20, a RING-family E3 that controls histone H2B ubiquitination and genome stability, has been implicated in the tumor suppressive role of Smurf2 in a wide spectrum of tumors [
18,
24]. Smurf2 E3 ubiquitin ligase plays a crucial role in cell differentiation and apoptosis through regulation of the stability of potential substrate molecules, as evidenced by various reports to date [
28,
29,
30].
Components of the ubiquitination system, such as Smurf2, have not yet been utilized or explored for targeted cancer therapy in the form of chimeric proteins, thus represent a novel approach to cancer treatment. Through regulation of a large number of proteins in multiple cellular compartments, and as part of the HECT family, with its intrinsic catalytic activity, Smurf2 functions as a tumor suppressor as described, and as such was chosen as the killing component of the chimeric proteins in this study.
We constructed, expressed and purified a novel IL2-Smurf2 chimeric protein and tested its cell entry and its effect on cell viability, then confirmed its activity as an E3 ligase. In addition, we characterized the cell death induced by IL2-Smurf2 chimeric protein. Furthermore, we produced a variant chimeric protein with an inactive killing component for confirmation that the effects seen were caused by the Smurf2 component of the chimeric protein. We also designed and produced two variants of the chimeric protein with over-active killing moieties to increase the activity. Finally, we tested the effect of the various variants of IL2-Smurf2 chimeric proteins in an in vivo mouse model.
2. Materials and Methods
2.1. Construction of the Plasmids Encoding IL2-Smurf2 Chimeric Proteins
A plasmid encoding the IL2-Bax sequence, pre-existing in the laboratory [
31], was cut with EcoRI and BlpI restriction enzymes to remove the Bax coding sequence. The full length human Smurf2 was generated and amplified by PCR using a Smurf2 clone as a template (clone number: 7939721, GE Healthcare Dharmacon Inc., Lafayette, CO, USA) with the following synthetic oligonucleotide primers covering the whole coding sequence: 5′ AAGGAATTCTCTAACCCCGGAGGC 3′ (sense), 5′ TTATTGCTCAGCTCATTCCA CAGCAAATCCA 3′ (anti-sense). The Smurf2 fragment, cut with the same restriction enzymes, was ligated into the vector fragment using Quick Ligation Kit (New England Biolabs, Ipswich, MA, USA), 3′ to the IL-2 coding sequence, so producing the plasmid encoding the IL2-Smurf2 chimeric protein. The coding sequence of IL2-Smurf2 chimeric protein was confirmed by sequencing analysis.
As a negative control, a plasmid containing a known deactivating mutation (introducing a point mutation at aa 716, from Cys to Ala) [
32] in the active site of Smurf2 was designed and generated. First, two PCR reactions were carried out using: (1) the sense primer containing the mutation 5′ AGCCCACACTGCCTTCAATCGAA 3′ and T7 terminator primer; (2) F1 5′ CTGCAGATGATTCTGAACGGCAT 3′ (sense) and the primer containing the point mutation 5′ TTCGATTGAAGGCAGTGTGGGCT 3′ (anti-sense). Second, both PCR products were used as a template for a third PCR reaction using F1 and the T7 terminator primers. The PCR product was cut with EcoRI and BlpI restriction enzymes and ligated into the vector fragment mentioned above containing the IL2 coding sequence. The coding sequence of IL2-Smurf2*716 (termed *716) chimeric protein was confirmed by sequencing analysis and was found to have the sequence coding the Ala residue.
Two more plasmids, Smurf2*547 and *29/30, were produced in a similar process. In IL2-Smurf2*547 (termed *547), a known activating mutation (introducing a point mutation at aa 547, from His to Phe) [
32] was generated in the HECT domain of Smurf2 using two PCR steps: (1) the sense primer containing the mutation 5′ GTGTTTTGGACTTTACCTTCTGTGTT 3′ and T7 terminator primer (anti-sense); (2) F1 5′CTGCAGATGATTCTGAACGGCAT 3′ (sense) and the primer containing the point mutation 5′ AACACAGAAGGTAAAGTCCAAAACACC 3′ (anti-sense). In IL2-Smurf2*29/30 (termed *29/30), a known activating mutation (introducing both mutations at aa 29/30, from Phe Phe to Ala Ala) [
33] was generated in the C2 domain of Smurf2 using two PCR steps. First, two PCR reactions were carried out using: (1) the sense primer containing the mutation 5′ AAAACCTGGTGAAAAAGGATGCTGCCCGACTTCCT GATCCATTTGC 3′ and T7 terminator primer (anti-sense); (2) F1 5′ CTGCAGATGATTCTGAACGGCAT 3′ (sense) and the primer containing the point mutation 5′ GCAAATGGATCAGGAAGTCGGGCAGCATCCTTTTTCACCAGGTTTT 3′ (anti-sense). For both activating variant plasmids, in the next step both PCR products were used as a template for a third PCR reaction using F1 and the T7 terminator primers. The PCR products were cut and ligated into the vector fragment mentioned above containing the IL2 coding sequence. The coding sequence of each variant chimeric protein was confirmed by sequencing analysis.
2.2. Expression and Production of the Chimeric Proteins
Plasmids were transformed into the Rosetta Escherichia coli strain, and 0.1 M potassium glutamate and 0.1% glycerol were added when an OD600 of 0.2–0.3 was reached. The temperature was then raised to 42 °C for 25 min followed by growth at 37 °C until an OD600 of 0.7–0.8 was reached. Protein expression was induced by incubating with 1 mM isopropyl-1-thio-D-galactopyranoside (IPTG), at 16 °C overnight. The cells were then centrifuged for 20 min at 4000× g, and the pellet was frozen at −80 °C at least for 30 min. The frozen cells were thawed and suspended in lysis buffer (20 mM Tris-HCl, pH 8.8; 0.05 M NaCl; 0.2 mg/mL lysozyme; 1 mM phenylsulfonyl fluoride (PMSF)) for 30 min at room temperature, followed by sonication. A sample was taken from the lysed cells and marked as whole cell extract (WCE). The remaining cells were then centrifuged at 29,000× g for 30 min. The supernatant (marked as soluble fraction; sol) was removed and the pellet (containing inclusion bodies) was suspended in denaturation buffer (6 M urea; 20 mM Tris-HCl, pH 8.8; 0.05 M NaCl) and continuously stirred for 90 min. The solution was cleared by centrifugation at 29,000× g for 30 min. The supernatant, containing denatured proteins, was collected and marked as inclusion bodies (IB).
2.3. Purification of IL2-Smurf2 Chimeric Proteins
The various IL2-Smurf2 denatured chimeric proteins in 6 M urea (see above) were filtrated and a final concentration of 10 mM imidazole was added. The protein was subjected to immobilized metal affinity chromatography using 5 mL His-Trap columns (GE Healthcare, Sweden) and was eluted with a linear imidazole gradient of 10–500 mM. Fractions containing the chimeric protein were pooled and slowly diluted 1:80 (v/v) in refolding buffer (20 mM Tris-HCl, pH 8.8; 2 mM β-mercaptoethanol; 1 mM EDTA; 0.05 M NaCl; 1 mM DTT) and then incubated at 4 °C for 72 h. The refolded chimeric protein solution was then subjected to ion exchange chromatography using a Q-Sepharose column (GE Healthcare, Sweden). Protein was eluted with linear gradient of 0.05–1 M NaCl in refolding buffer. Fractions containing the protein were pooled. Desalting and buffer exchange to phosphate-buffered saline (PBS) was performed using dialysis. The various variant chimeric proteins were aliquoted and kept at −20 °C. All purification procedures were carried out using the FPLC system ÄKTA (GE Healthcare, Sweden).
2.4. Characterization of the Chimeric Protein
2.4.1. Structure Prediction
IL2-Smurf2 protein models were generated by AlphaFold v2.0 [
34]. Sequences were submitted to the AlphaFold Colab server with the default settings. Each structural model was validated by analyzing the confidence score as generated by the pLDDT (predicted lDDT-Cα). Molecular graphics and superimposition analysis were performed with UCSF ChimeraΧ-1.2.5 [
35].
2.4.2. Protein Concentration
Protein concentration was measured according to the Bradford method [
36], using Bradford reagent and a standard curve of BSA. Protein concentration was determined at a wavelength of 595 nm.
2.4.3. Separation of Proteins by Gel Electrophoresis
Samples from the various protein sub-cellular fractions (WCE, Sol and IB) were separated on 12% SDS-PAGE gels and stained with Coomassie blue for visualization of the proteins.
2.4.4. Western Blot Analysis
Following separation on SDS-PAGE gel, the proteins were then electro-transferred onto a polyvinylidene fluoride (PVDF) membrane (Bio-Rad, Hercules, CA, USA). The membrane was then blotted with one of the following antibodies: rabbit anti-Smurf2 (1:2000) (SC-25511; Santa Cruz Biotechnology Inc., Dallas, TX, USA), mouse anti-His (1:3000) (27-4710-01; Amersham-Pharmacia Biotech, Uppsala, Sweden), rabbit anti-RNF20 (1:1500) (ab181104; Abcam, Cambridge, UK), mouse anti-FK2 (1:1000) (BML-PW8810; Enzo, Farmingdale NY, USA), rabbit anti-K48 (1:1000) (#8081, Cell Signaling Technology, Danvers, MA, USA), mouse anti-β Actin (1:5000) (A5441; Sigma-Aldrich, St. Louis, MO, USA), mouse anti-tubulin (1:10,000) (ab7291; Abcam, Cambridge, UK), mouse anti-lamin (1:1000) (ab8983; Abcam, Cambridge, UK). The secondary antibodies used were goat anti-rabbit or goat anti-mouse HRP conjugated (1:10,000) (Jackson ImmunoResearch Laboratories Inc., West Grove, PA, USA). Band visualization was performed using the EZ-ECL chemiluminescence detection kit (Biological Industries, Israel).
2.5. Cell Lines and Cultures
Mouse lymphocytic leukemia L1210 and human T-cell lymphoma SUDHL-1 cells were grown in RPMI 1640 medium supplemented with 10% heat inactivated fetal bovine serum (HIFBS), 2 mM L-glutamine, 100 units/mL penicillin, 100 µg/mL streptomycin. Karpas, a human non-Hodgkin’s large cell lymphoma cell line, was grown similarly, but supplemented with 10% FBS. Human T-cell lymphoblast YC cells were grown similarly but supplemented with 20% HIFBS. Human T-cell lymphoma HUT102 cells were grown in RPMI 1640 medium supplemented with 10% HIFBS, 2 mM L-glutamine, 100 units/mL penicillin, 100 µg/mL streptomycin, 1 mM sodium pyruvate, 5 mM Hepes buffer solution and 5 µM β-mercaptoethanol. All cells were maintained in flasks and grown in a highly humidified atmosphere of 5% CO2 at 37 °C.
2.6. Cell Viability Assay
Cells for viability assays were seeded in 96-well plates, 104/100 µL/well and incubated for 1 h. Cells were treated with the chimeric proteins, PBS or a positive control in triplicates and incubated for 24/48/72 h. Cell death was determined using the kit cellTiter-Blue® (Promega, Madison, WI, USA) according to manufacturer’s instructions.
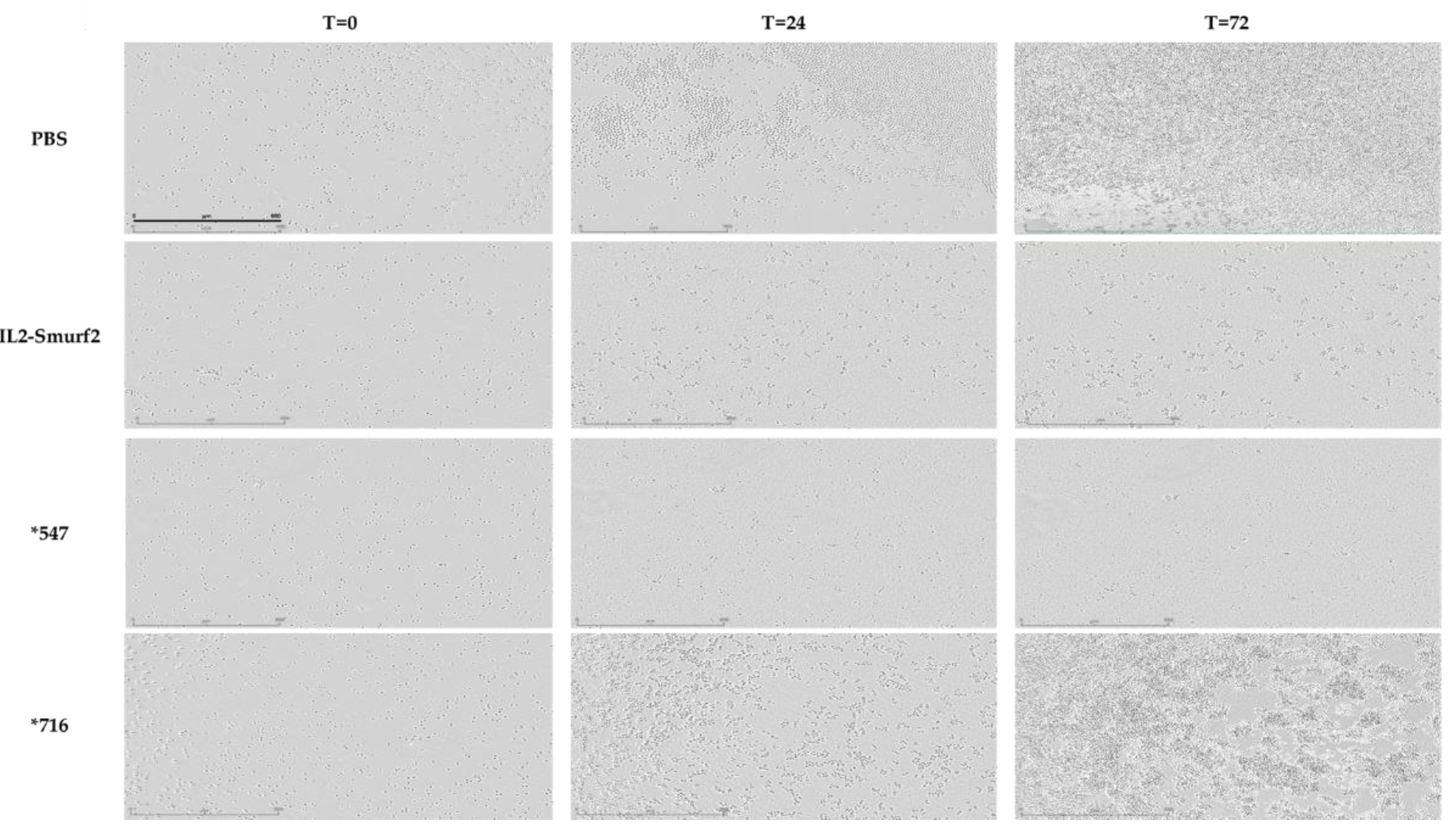
In addition, L1210 cells treated as described above were incubated in the IncuCyte® S3 Live-Cell Analysis System and tracked for up to 72 h. Images of each well were obtained every 2 h. The data were analyzed using IncuCyte® S3 Software 2019A (Sartorius, Gottingen, Germany).
2.7. Internalization of the Chimeric Protein into IL-2R Expressing Cells
1 × 106 L1210, HUT102 or SUDHL-1 cells were seeded in 12-well plates and treated with the chimeric proteins (final concentration 15 μg/mL) or PBS (same volume as chimeric protein treatments) and incubated for 24 h. Internalization of the chimeric protein into target cells was examined by Western blot analysis of treated cell extracts using anti- Smurf2 antibodies.
2.8. Ubiquitination Asssays in Lysates of IL-2R Expressing Cells
1 × 106 L1210 cells were seeded in 12-well plates and treated with the chimeric proteins or PBS and incubated for 24 h. For testing proteasomal inhibition, additional 1 × 106 L1210 cells were seeded in 12-well plates and treated first with 0.05 µM MG132 and incubated for 24 h, after which they were treated with the chimeric proteins or PBS and incubated for 24 h. Ubiquitination assay was examined by Western blot analysis of treated cell extracts using anti-FK2 antibodies.
2.9. Subcellular Fractionation of Target Cells
2.5 × 10
6 L1210 and HUT102 cells were seeded in 6-well plates and treated with the chimeric proteins or PBS and incubated for 24 h. Subcellular fractionation was performed using the Abcam protocol [
37].
2.10. In Vitro Caspase3 Activity Assay
L1210 cells (104/100 µL/well in 96-well plates) were treated with the chimeric protein for 48/72 h, and with IL2-Bax and Doxorubicin as positive controls(13,30). Caspase3 activity within the cells was assessed by Apo-ONE® Homogeneous Caspase3/7 Assay Kit (Promega, Madison, WI, USA). Experiments were carried in parallel with cell viability assays. The Caspase3 activity was analyzed using a FLUOstar plate reader at excitation/emission 485/520 nm.
2.11. Cell Cycle Analysis by Propidium Iodide Staining
2 × 106 L1210 cells were seeded in 12-well plates and treated with 15 µg/mL IL2-Smurf2 or PBS and incubated for 48 h. Samples were removed for assaying cell viability. Remaining cells (1 × 106 cells) were washed with PBS twice then treated with 1 mL Nicoletti buffer (50 µg/mL propidium iodide, 0.1% sodium citrate, 0.1% Triton X-100). The cells were incubated at 4 °C for 1 h. Cell cycle analysis of the cells was performed using FACScan and the CellQuest program and was analyzed using FCS Express 4.
2.12. Real-Time PCR Analysis of Apoptosis-Related mRNAs in Treated Cells
1 × 10
6 L1210 cells were treated in 12-well plates with 6 µg/mL IL2-Smurf2 or PBS and incubated for 24 or 48 h. Total RNA was extracted from cells using a commercial kit (NucleoBond Xtra Midi, Macherey-Nagel, Düren, Germany). RNA concentrations were determined using a NanoDrop spectrophotometer (Thermo scientific, Waltham, MA, USA). One µg of each mRNA sample was reverse transcribed using a reverse transcription kit (qScript cDNA Synthesis Kit, Quantabio, Beverly, MA, USA).. Individual mRNA levels were quantified using real-time PCR. Each sample contained 2 µL cDNA (20 ng), 1 µL primers (10 ng), 5 µL SYBR
® Green and 3 µL H
2O in a total volume of 10 µL per sample. The primers used are listed in
Table 1. The data were analyzed using the primer express program (Applied Biosystems, Foster City, CA, USA).
2.13. Mice and Toxicity Studies
Female, 5–6 weeks old DBA/2J SPF mice were obtained from Jackson Laboratory (Bar Harbor, ME, USA). All animal welfare and experimental protocols were approved by the Committee for the Ethics of Animal Experiments of the Hebrew University of Jerusalem (MD-18-15680-5). Mice were housed at a 12 h dark/light cycle and were allowed free access to food and water. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. Adequate measures were taken to minimize pain and suffering. For 10 days, all mice were injected intravenously or intraperitoneally with 15, 30 or 50 µg/mouse/day of IL2-Smurf2. The mice were monitored and weighed 3 times a week.
2.14. Induction of Cancer and Experimental Design
A single dose of 106 L1210 mouse lymphocytic leukemia cells was injected intravenously in all mice (day 0). For the following 10 days (days 1–10), the mice were injected with 50 µg/100 µL/mouse/day of IL2-Smurf2, *716, *29/30, *547 or PBS. Following the injection of the proteins or PBS, each mouse was monitored until it reached a predefined humane endpoint. The mice were monitored and weighed 3 times a week.
2.15. Statistical Analyses
Results of cells’ viability assays are the average of 3–6 independent biological experiments ± SD. The results of the Western blot analyses were evaluated by densitometry using the Image Lab Software version 5.2.1 (Bio-Rad, Hercules, CA, USA). Statistical analysis was performed using Microsoft Excel 2017 and an unpaired, two-tailed t test was used to determine
p values. Survival plot and hazard ratio (HR) were visualized and calculated by package “survminer” in R. Pair-wise comparisons were tested with default parameters using the same package [
38].
4. Discussion
The development of specific targeting agents remains a major goal in the treatment of human diseases. The hallmark of an effective therapeutic modality is its specificity, the ability to interact with the target cells without undesirable effects in the human recipient. One of the approaches to solve this problem lies in chimeric cytotoxic proteins, whose development has flourished over recent years [
42,
43]. In cancer research, the goal is to find a killing component that can efficiently kill the targeted cells with high potency but with low levels of damage to the neighboring cells, since it is fused to a precise targeting component.
Earlier developments concentrated on plant or bacterial toxins, which though highly potent, caused severe dose-dependent general toxicity, limiting the maximal dose that could be given to patients. More importantly, the non-human origin of the toxins caused an immune response which resulted in impaired efficacy. Several drugs based on this method were approved by the FDA, for example ONTAK
® and Elzonris
®, and others are currently being researched. The idea of using bacterial toxins for tumor therapy is still attractive but needs further development to achieve better results [
44].
It has become clear that the killing moieties should be of human origin, which led our laboratory to the use of human pro-apoptotic proteins as the killing component, hoping that this will prevent an immunogenic response as well as leading to a therapy that is less harmful to healthy cells. However, since these human apoptosis-inducing chimeric proteins are still under development, it is well worth pursuing other directions meanwhile.
The UPS is the main way that cells degrade their proteins. Massive degradation of proteins within cells may lead to cell death. Much research is being conducted on the relationship between different proteins in the UPS and how we can utilize these relationships in drug development [
45]. However, the use of a member of the UPS in a chimeric protein has not yet been examined. In this work, we aimed to develop a new chimeric protein prototype based on a protein from the UPS, namely the E3 ligase, Smurf2, as a new “killing” component. Smurf2 specifically has been shown to have an ambivalent role in cell functions [
18], but has also been shown to have a connection to cancer, as described in the introduction. We attempted to utilize the UPS in the targeted cells to induce apoptotic cell death. We have described here our approach for developing a chimeric protein that can be used for targeted therapy in hematological cancers.
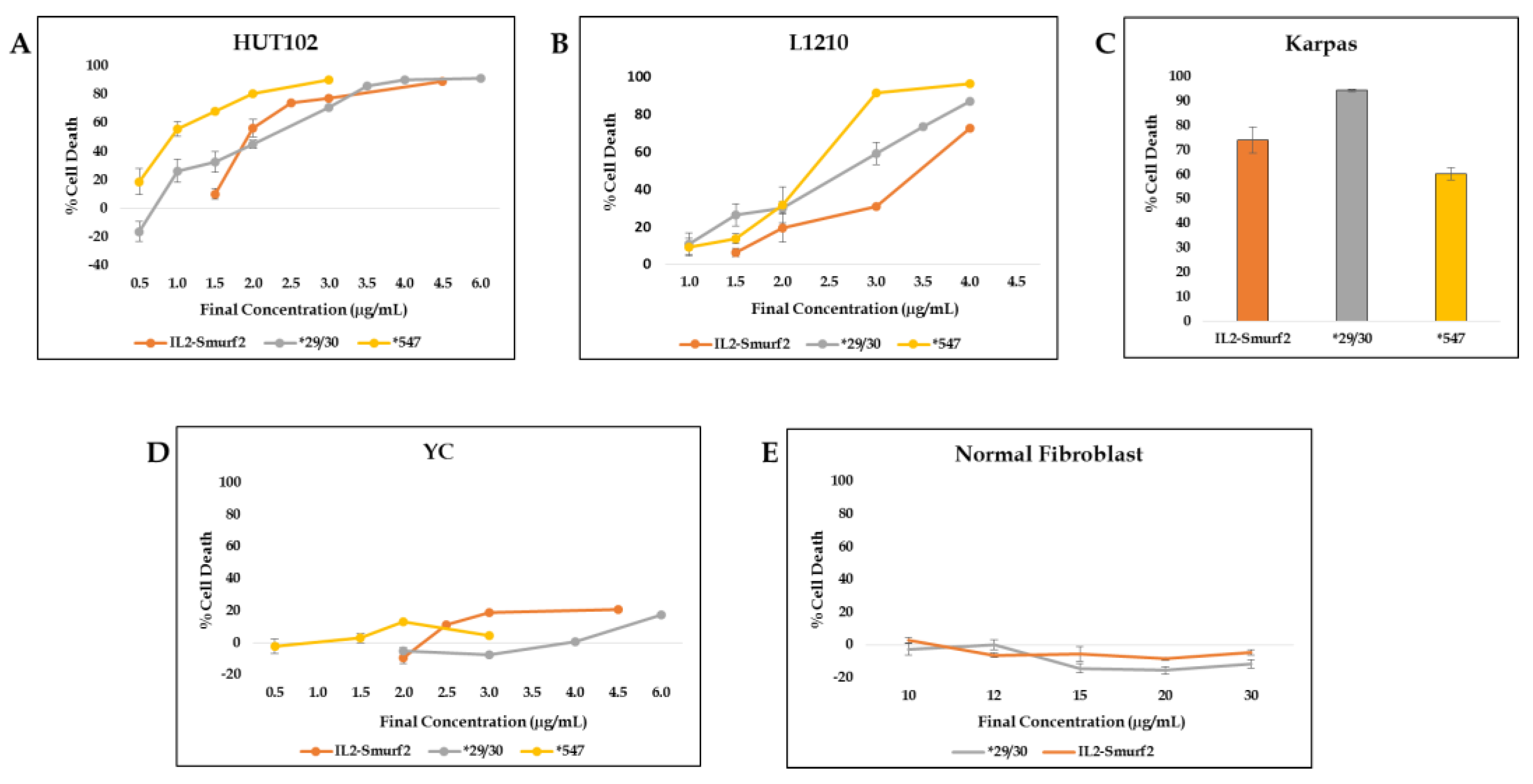
The chimeric protein IL2-Smurf2 was designed, cloned and expressed in E. coli bacteria. When testing the chimeric protein on target cells we found that IL2-Smurf2 is able to target, enter and efficiently kill cells expressing IL-2R, with the ability of the chimeric protein to cause cell death being time- and concentration-dependent.
When studying the mechanism of action of IL2-Smurf2 chimeric proteins after entering the cells, we found that the chimera causes the degradation of proteins specifically targeted by Smurf2, such as RNF20, as well as a general increase in the level of ubiquitinylated proteins. More specifically, when human and mouse cells were incubated with IL2-Smurf2, we saw an increase in the number of proteins marked with ubiquitin and so designated for degradation (by their ubiquitination at lysine 48) (
Figure 4C–F). Put together, these results indicate that not only does the targeting component successfully target the cells, but the killing component also shows the expected biological activity; IL2-Smurf2 is active as an E3 ligase and is able to cause massive ubiquitination and degradation of target proteins when entering the target cells, causing finally cell death.
Smurf2 is known to regulate RNF20, whose high expression strongly correlates with tumor formation [
46]. As we have shown (
Figure 4G,H), the entry of IL2-Smurf2 to the targeted cells caused RNF20 expression levels to significantly decrease, while the mutated chimera did not. This provides evidence that the chimeric protein has tumor suppressor traits in addition to its ability to cause cell death [
24].
Remarkably, we found that manipulating the killing component, either by making it inactive or by increasing its activity with point mutations, resulted in a corresponding activity in the targeted cells. While all mutant proteins were expressed and produced in a similar way as the original chimeric protein, and all chimeras were able to enter cells, when the active site cysteine was replaced with alanine, there was no effect on Smurf2 targeted proteins, ubiquitination levels or cell death. Chimeras with increased activity caused greater and quicker cell death. Put together, these results demonstrate that IL2-Smurf2 is active through the cysteine site in the HECT domain in Smurf2. These results further strengthen the notion that the chimeric protein functions as an E3 ligase after entering target cells and so causes mass protein degradation.
The ability of the chimeric protein to function as an E3 ligase indicates that E3 is able to function independently from the UPS cascade, which includes the E1 and E2 enzymes, with its activation raising the total level of ubiquitinated proteins. This phenotype is surprising when considering the high dependency of E3 ligases on the cascade. It is possible that upon entering the target cells in high concentrations, the chimeric proteins activate the other members of the cascade and that way perhaps force activation.
We then studied the nature of the cell death caused by treatment with IL2-Smurf2 chimeric protein. By measuring Caspase3 activity, performing cell cycle analysis and by real-time PCR for apoptotic-related proteins, we found that the chimeric protein, most probably leads to apoptotic cell death, as expected; however, further details are needed. Smurf2 stands out as an E3 that can cause apoptosis itself in downstream reactions, as described earlier [
18]. We also hypothesized that a large amount of Smurf2 entering the cell at once would cause massive protein degradation. It may be that Smurf2 has two pathways by which it causes apoptotic cell death—a direct downstream cascade as well as an indirect effect caused by massive degradation. The possibility that Smurf2 has two pathways by which it can cause cell death makes it an even stronger killing component. Originally, Smurf2 was chosen due to its HECT auto-catalyzing traits, which would allow it to cause massive degradation once it enters the targeted cell. However, the choice of Smurf2 has been proven to be beneficial in that in addition, it has a direct pathway that can cause apoptosis.
Finally, we tested the various chimeric proteins in vivo and found that the over-active proteins show a significantly lower hazard ratio, while the inactive chimera had very similar effects as those seen in the control group. We observed that some of the mice in the group that received the mutant *29/30 protein reached the 30th day with no noticeable endpoints, which could indicate full recovery. Many questions remain to be answered, such as the optimization of the concentration and scheduling of treatments and whether this can improve the results. In addition, the stability of the chimeric protein after entering the blood stream and the conditions for optimizing the treatment need to be established. Further understanding of these conditions may highlight the differences between the variant chimeras of IL2-Smurf2.
Immunotherapy, especially CAR T-cell therapy, has demonstrated outstanding response rates in subgroups of patients with hematological malignancies, leading to emergence of CAR T-cells as a breakthrough in cancer immunotherapy [
47,
48]. Additionally, in recent years, anti-PD therapy has become applicable to a broad spectrum of cancer types, including one clinical trial in Hodgkin’s lymphoma with 87% objective response rates [
49]. The efficacy of the therapy depends on many variables including the expression pattern of PD-L1 in the tumor microenvironment, the ability to target tumor-induced immune defects and repair the impaired host immune response [
50,
51]. While immunotherapy seems to be effective for several malignancies, in some hematological malignancies, response rates are low, and patients still relapse. There also appears to be an issue with the development of drug resistance to some treatments and these therapeutic approaches still need to be optimized in regard to their safety and efficacy. We therefore believe that a combination of such a therapy with our chimeric proteins, in various types of lymphoma and leukemia could potentially perform with higher efficacy, quicker responses and longer survival rates.
It is worth considering conducting a screen to test the combination of IL2-Smurf2 chimeric proteins with small molecular weight drugs, and also to identify enhancing agents to increase its activity, as was conducted for PE-based immunotoxins [
52]. Such screening could identify enhancing agents that already have approval for use in the treatment of humans which would increase potency at lower concentrations of both the molecule and the chimera it was given with, thus hopefully reducing any unwanted side effects and shortening treatment duration.
This study has demonstrated the ability to utilize the UPS to suppress tumors and cause-specific cell death, which is a novel and important result. The UPS is endogenous in humans and therefore we expect no or minimal immunogenic response. We have successfully attempted to manipulate this system for the desirable outcome of eliminating cancer cells without compromising their healthy surroundings, a serious problem for many chemotherapeutic drugs. Furthermore, these results may open the door to further investigation of the utilization of E3s for the purpose of causing targeted cell death. Smurf2 is one of the smaller E3s, at ~86 kDa; however, perhaps following the successful shortening of the protein, this can be adapted to other E3s.
In the course of this work, we established for the first time the feasibility of using Smurf2 as a killing component in targeted chimeric proteins. This is the first investigation of a protein from the UPS family connected to a targeting component, and despite previous reports of tumor-enhancing traits of the Smurf2 protein [
18], our findings clearly demonstrate the tumor-suppressive activity of the Smurf2 component. The IL2-Smurf2 chimeric protein effectively and specifically caused death by targeting cancer cells, thus opening new approaches in the fight against cancer.