MicroRNA Expression Profiling Predicts Nodal Status and Disease Recurrence in Patients Treated with Curative Intent for Colorectal Cancer
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Workup and Colorectal Cancer Staging
2.2. MiRNA Targets
2.3. RNA Isolation and Storage
2.4. Analysis of miRNA Gene Expression
2.5. Statistical Analysis
2.6. Patient Follow-Up and Definitions
3. Results
3.1. Included Colorectal Cancer Patients
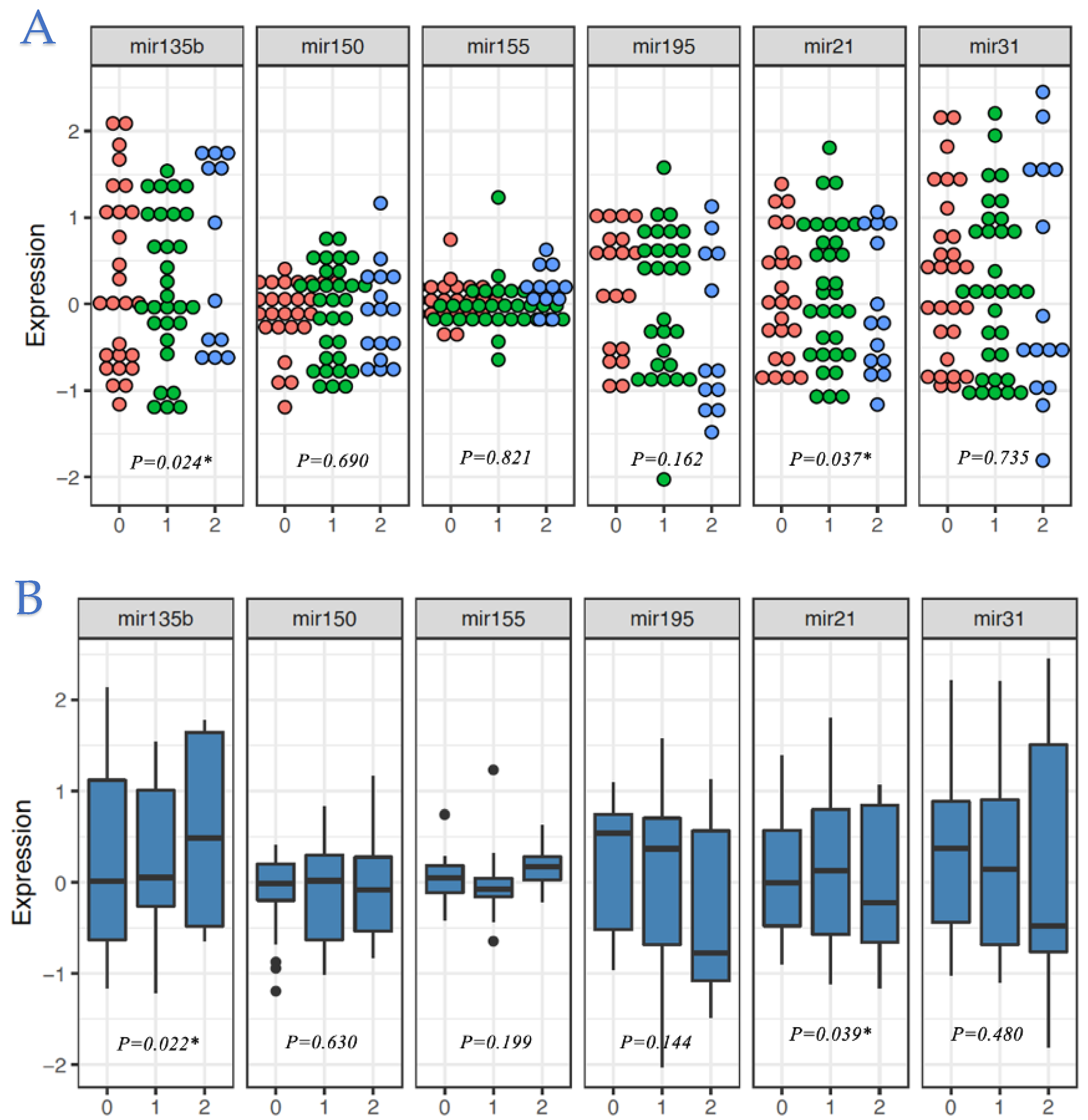
3.2. Associations between Clinicopathological Characteristics and miRNA Expression Profiles
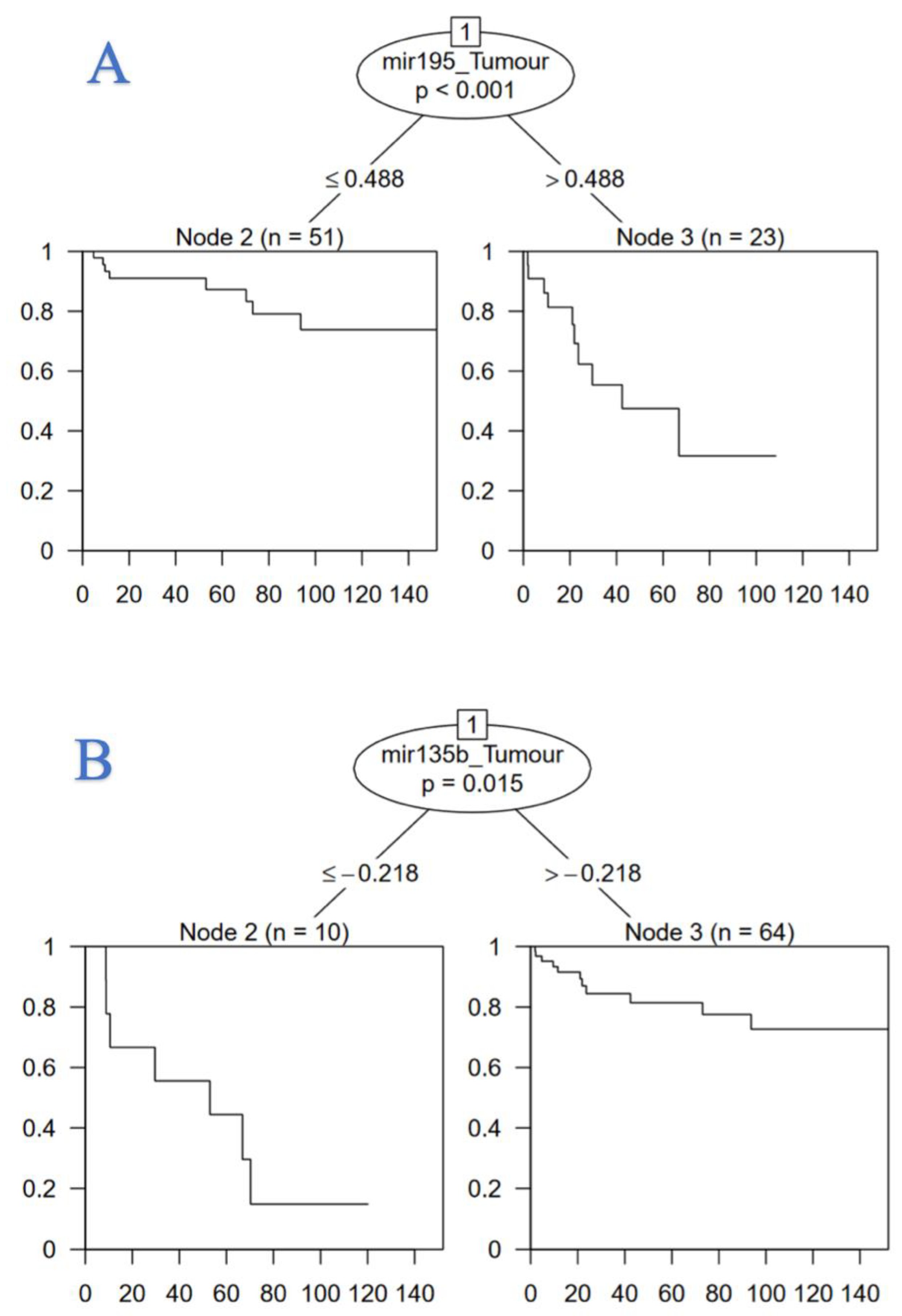
3.3. MiRNA as Biomarkers of Colorectal Cancer Recurrence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boyle, P.; Ferlay, J. Cancer incidence and mortality in Europe, 2004. Ann. Oncol. 2005, 16, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brouwer, N.P.; Bos, A.C.; Lemmens, V.E.; Tanis, P.; Hugen, N.; Nagtegaal, I.; De Wilt, J.H.; Verhoeven, R. An overview of 25 years of incidence, treatment and outcome of colorectal cancer patients. Int. J. Cancer 2018, 143, 2758–2766. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.-J.; Wu, X.-J.; Zhao, Q.; Li, L.-R.; Lu, Z.-H.; Ding, P.-R.; Zhang, R.-X.; Kong, L.-H.; Wang, F.-L.; Lin, J.-Z.; et al. Hospital-Based Colorectal Cancer Survival Trend of Different Tumor Locations from 1960s to 2000s. PLoS ONE 2013, 8, e73528. [Google Scholar] [CrossRef]
- Dulskas, A.; Gaizauskas, V.; Kildusiene, I.; Samalavicius, N.E.; Smailyte, G. Improvement of Survival over Time for Colorectal Cancer Patients: A Population-Based Study. J. Clin. Med. 2020, 9, 4038. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterol. Rev. 2019, 14, 89–103. [Google Scholar] [CrossRef]
- Guren, M.G.; Kørner, H.; Pfeffer, F.; Myklebust, T.; Eriksen, M.T.; Edna, T.-H.; Larsen, S.G.; Knudsen, K.O.; Nesbakken, A.; Wasmuth, H.H.; et al. Nationwide improvement of rectal cancer treatment outcomes in Norway, 1993–2010. Acta Oncol. 2015, 54, 1714–1722. [Google Scholar] [CrossRef]
- Allemani, C.; Weir, H.K.; Carreira, H.; Harewood, R.; Spika, D.; Wang, X.S.; Bannon, F.; Ahn, J.V.; Johnson, C.J.; Bonaventure, A.; et al. Global surveillance of cancer survival 1995-2009: Analysis of individual data for 25, 676, 887 patients from 279 population-based registries in 67 countries (CON-CORD-2). Lancet 2015, 385, 977–1010. [Google Scholar] [CrossRef] [Green Version]
- van Steenbergen, L.N.; Elferink, M.A.G.; Krijnen, P.; Lemmens, V.E.P.P.; Siesling, S.; Rutten, H.J.T.; Richel, D.J.; Karim-Kos, H.E.; Coebergh, J.W.W. Improved survival of colon cancer due to improved treatment and detection: A nationwide population-based study in The Netherlands 1989–2006. Ann. Oncol. 2010, 21, 2206–2212. [Google Scholar] [CrossRef]
- Malakorn, S.; Ouchi, A.; Hu, C.-Y.; Sandhu, L.; Dasari, A.; You, Y.-Q.N.; Kopetz, E.S.; Ellis, L.M.; Chang, G.J. Tumor Sidedness, Recurrence, and Survival After Curative Resection of Localized Colon Cancer. Clin. Color. Cancer 2020, 20, e53–e60. [Google Scholar] [CrossRef]
- Böckelman, C.; Engelmann, B.E.; Kaprio, T.; Hansen, T.F.; Glimelius, B. Risk of recurrence in patients with colon cancer stage II and III: A systematic review and meta-analysis of recent literature. Acta Oncol. 2015, 54, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Kunst, N.; Alarid-Escudero, F.; Aas, E.; Coupé, V.M.; Schrag, D.; Kuntz, K.M. Estimating Population-Based Recurrence Rates of Colorectal Cancer over Time in the United States. Cancer Epidemiol. Biomarkers Prev. 2020, 29, 2710–2718. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.S.; Davey, M.G.; Ryan, É.J.; Hogan, A.M.; Kerin, M.J.; Joyce, M. The use of radiomic analysis of magnetic resonance imaging in predicting distant metastases of rectal carcinoma following surgical resection: A systematic review and me-ta-analysis. Colorectal Dis. 2021, 23, 3065–3072. [Google Scholar] [CrossRef] [PubMed]
- Verberne, C.J.; Zhan, Z.; Heuvel, E.R.V.D.; Oppers, F.; de Jong, A.M.; Grossmann, I.; Klaase, J.M.; de Bock, G.H.; Wiggers, T. Survival analysis of the CEAwatch multicentre clustered randomized trial. Br. J. Surg. 2017, 104, 1069–1077. [Google Scholar] [CrossRef]
- Ryan, E.; Khaw, Y.L.; Creavin, B.; Geraghty, R.; Ryan, E.; Gibbons, D.; Hanly, A.; Martin, S.T.; O’Connell, P.R.; Winter, D.C.; et al. Tumor Budding and PDC Grade Are Stage Independent Predictors of Clinical Outcome in Mismatch Repair Deficient Colorectal Cancer. Am. J. Surg. Pathol. 2018, 42, 60–68. [Google Scholar] [CrossRef]
- Bhangu, A.; Fitzgerald, J.E.F.; Slesser, A.; Northover, J.M.; Faiz, O.; Tekkis, P. Prognostic significance of extramural vascular invasion in T4 rectal cancer. Color. Dis. 2013, 15. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.-H.; Joo, Y.-E. Novel biomarkers for the diagnosis and prognosis of colorectal cancer. Intest. Res. 2020, 18, 168–183. [Google Scholar] [CrossRef]
- Davey, M.G.; Lowery, A.J.; Miller, N.; Kerin, M.J. MicroRNA Expression Profiles and Breast Cancer Chemotherapy. Int. J. Mol. Sci. 2021, 22, 10812. [Google Scholar] [CrossRef]
- Davey, M.; Davies, M.; Lowery, A.; Miller, N.; Kerin, M. The Role of MicroRNA as Clinical Biomarkers for Breast Cancer Surgery and Treatment. Int. J. Mol. Sci. 2021, 22, 8290. [Google Scholar] [CrossRef]
- Richard, V.; Davey, M.G.; Annuk, H.; Miller, N.; Dwyer, R.M.; Lowery, A.; Kerin, M.J. MicroRNAs in Molecular Classification and Pathogenesis of Breast Tumors. Cancers 2021, 13, 5332. [Google Scholar] [CrossRef]
- Heneghan, H.M.; Miller, N.; Lowery, A.J.; Sweeney, K.J.; Newell, J.; Kerin, M.J. Circulating microRNAs as Novel Minimally Invasive Biomarkers for Breast Cancer. Ann. Surg. 2010, 251, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.S.; Parkin, R.K.; Kroh, E.M.; Fritz, B.R.; Wyman, S.K.; Pogosova-Agadjanyan, E.L.; Peterson, A.; Noteboom, J.; O’Briant, K.C.; Allen, A.; et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl. Acad. Sci. USA 2008, 105, 10513–10518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan, G.; Lim, Q.E.; Too, H.P. High-performance quantification of mature microRNAs by real-time RT-PCR using deoxyuri-dine-incorporated oligonucleotides and hemi-nested primers. RNA 2010, 16, 1436–1445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waldron, R.M.; Moloney, B.M.; Gilligan, K.; Lowery, A.J.; Joyce, M.R.; Holian, E.; Kerin, M.J.; Miller, N. MicroRNAs as biomarkers of multimodal treatment for rectal cancer. Br. J. Surg. 2021, 108, e260–e261. [Google Scholar] [CrossRef]
- McGuire, A.; Casey, M.-C.; Waldron, R.M.; Heneghan, H.; Kalinina, O.; Holian, E.; McDermott, A.; Lowery, A.J.; Newell, J.; Dwyer, R.M.; et al. Prospective Assessment of Systemic MicroRNAs as Markers of Response to Neoadjuvant Chemotherapy in Breast Cancer. Cancers 2020, 12, 1820. [Google Scholar] [CrossRef]
- Ding, L.; Lan, Z.; Xiong, X.; Ao, H.; Feng, Y.; Gu, H.; Yu, M.; Cui, Q. The Dual Role of MicroRNAs in Colorectal Cancer Progression. Int. J. Mol. Sci. 2018, 19, 2791. [Google Scholar] [CrossRef] [Green Version]
- Nanda, N.; Mahmood, S.; Bhatia, A.; Mahmood, A.; Dhawan, D.K. Chemopreventive role of olive oil in colon carcinogenesis by targeting noncoding RNAs and methylation machinery. Int. J. Cancer 2018, 144, 1180–1194. [Google Scholar] [CrossRef]
- Weiser, M.R. AJCC 8th Edition: Colorectal Cancer. Ann. Surg. Oncol. 2018, 25, 1454–1455. [Google Scholar] [CrossRef] [Green Version]
- Chu, P.G.; Weiss, L.M. Keratin expression in human tissues and neoplasms. Histopathology 2002, 40, 403–439. [Google Scholar] [CrossRef]
- Werling, R.W.; Yaziji, H.; Bacchi, C.E.; Gown, A.M. CDX2, a highly sensitive and specific marker of adenocarcinomas of in-testinal origin: An immunohistochemical survey of 476 primary and metastatic carcinomas. Am. J. Surg. Pathol. 2003, 27, 303–310. [Google Scholar] [CrossRef]
- Kahn, H.J.; Marks, A. A New Monoclonal Antibody, D2-40, for Detection of Lymphatic Invasion in Primary Tumors. Lab. Investig. 2002, 82, 1255–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Z.; Xu, S.; Xu, W.; Huang, J.; Zhang, G.; Lei, L.; Shao, X.; Wang, X. Expression of cluster of differentiation 34 and vascular endothelial growth factor in breast cancer, and their prognostic significance. Oncol. Lett. 2015, 10, 723–729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, I.S. Pathology of Perineural Spread. J. Neurol. Surg. Part B Skull Base 2016, 77, 124–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roxburgh, C.S.D.; McMillan, D.C.; Anderson, J.H.; McKee, R.F.; Horgan, P.G.; Foulis, A.K. Elastica Staining for Venous Invasion Results in Superior Prediction of Cancer-Specific Survival in Colorectal Cancer. Ann. Surg. 2010, 252, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Slaby, O.; Svoboda, M.; Fabian, P.; Smerdova, T.; Knoflickova, D.; Bednarikova, M.; Nenutil, R.; Vyzula, R. Altered Expression of miR-21, miR-31, miR-143 and miR-145 Is Related to Clinicopathologic Features of Colorectal Cancer. Oncology 2007, 72, 397–402. [Google Scholar] [CrossRef]
- Nezu, Y.; Hagiwara, K.; Yamamoto, Y.; Fujiwara, T.; Matsuo, K.; Yoshida, A.; Kawai, A.; Saito, T.; Ochiya, T. miR-135b, a key regulator of malignancy, is linked to poor prognosis in human myxoid liposarcoma. Oncogene 2016, 35, 6177–6188. [Google Scholar] [CrossRef] [Green Version]
- Aherne, S.T.; Madden, S.F.; Hughes, D.J.; Pardini, B.; Naccarati, A.; Levy, M.; Vodicka, P.; Neary, P.; Dowling, P.; Clynes, M. Circulating miRNAs miR-34a and miR-150 associated with colorectal cancer progression. BMC Cancer 2015, 15, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Cao, H.; Huang, S.; Liu, A. Up-regulated expression of miR-155 in human colonic cancer. J. Cancer Res. Ther. 2018, 14, 604–607. [Google Scholar] [CrossRef]
- McDermott, A.M.; Kerin, M.; Miller, N. Identification and Validation of miRNAs as Endogenous Controls for RQ-PCR in Blood Specimens for Breast Cancer Studies. PLoS ONE 2013, 8, e83718. [Google Scholar] [CrossRef] [Green Version]
- Hellemans, J.; Mortier, G.; De Paepe, A.; Speleman, F.; Vandesompele, J. qBase relative quantification framework and software for management and automated analysis of real-time quantitative PCR data. Genome Biol. 2007, 8, R19. [Google Scholar] [CrossRef] [Green Version]
- Xue, X.; Agalliu, I.; Kim, M.Y.; Wang, T.; Lin, J.; Ghavamian, R.; Strickler, H.D. New methods for estimating follow-up rates in cohort studies. BMC Med. Res. Methodol. 2017, 17, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartzberg, L.; Kim, E.S.; Liu, D.; Schrag, D. Precision Oncology: Who, How, What, When, and When Not? Am. Soc. Clin. Oncol. Educ. Book 2017, 37, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Garraway, L.A.; Verweij, J.; Ballman, K.V. Precision Oncology: An Overview. J. Clin. Oncol. 2013, 31, 1803–1805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, W.; Liang, X.; Li, X.; Zhang, Y.; Sun, Z.; Liu, Y.; Wang, J. MicroRNA-195: A review of its role in cancers. OncoTargets Ther. 2018, 11, 7109–7123. [Google Scholar] [CrossRef] [Green Version]
- Flavin, R.J.; Smyth, P.C.; Laios, A.; O′Toole, S.A.; Barrett, C.; Finn, S.P.; Russell, S.; Ring, M.; Denning, K.M.; Li, J.; et al. Potentially important microRNA cluster on chromosome 17p13.1 in primary peritoneal carcinoma. Mod. Pathol. 2008, 22, 197–205. [Google Scholar] [CrossRef] [Green Version]
- He, J.-F.; Luo, Y.-M.; Wan, X.-H.; Jiang, D. Biogenesis of MiRNA-195 and its role in biogenesis, the cell cycle, and apoptosis. J. Biochem. Mol. Toxicol. 2011, 25, 404–408. [Google Scholar] [CrossRef]
- Yang, I.-P.; Tsai, H.-L.; Miao, Z.-F.; Huang, C.-W.; Kuo, C.-H.; Wu, J.-Y.; Wang, W.-M.; Juo, S.-H.H.; Wang, J.-Y. Development of a deregulating microRNA panel for the detection of early relapse in postoperative colorectal cancer patients. J. Transl. Med. 2016, 14, 108. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Zhao, Y.; Liu, C.; Chen, X.; Qi, Y.; Jiang, Y.; Zou, C.; Zhang, X.; Liu, S.; Wang, X.; et al. Analysis of MiR-195 and MiR-497 expression, regulation and role in breast cancer. Clin. Cancer Res. 2011, 17, 1722–1730. [Google Scholar]
- Sun, M.; Song, H.; Wang, S.; Zhang, C.; Zheng, L.; Chen, F.; Shi, D.; Chen, Y.; Yang, C.; Xiang, Z.; et al. Integrated analysis identifies microRNA-195 as a suppressor of Hippo-YAP pathway in colorectal cancer. J. Hematol. Oncol. 2017, 10, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.; Tan, Z.; Song, Y. Study on the molecular regulatory mechanism of MicroRNA-195 in the invasion and metastasis of colorectal carcinoma. Int. J. Clin. Exp. Med. 2015, 8, 3793–3800. [Google Scholar]
- Jinling, W.; Sijing, S.; Jie, Z.; Guinian, W. Prognostic value of circulating microRNA-21 for breast cancer: A systematic review and meta-analysis. Artif. Cells Nanomed. Biotechnol. 2016, 45, 1216–1221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pop-Bica, C.; Pintea, S.; Magdo, L.; Cojocneanu, R.; Gulei, D.; Ferracin, M.; Berindan-Neagoe, I. The Clinical Utility of miR-21 and let-7 in Non-small Cell Lung Cancer (NSCLC). A Systematic Review and Meta-Analysis. Front. Oncol. 2020, 10, 516850. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Xu, X.; Lv, L.; Dai, H.; Chen, J.; Chen, B. miR-21 Overexpression Promotes Esophageal Squamous Cell Carcinoma Invasion and Migration by Repressing Tropomyosin 1. Gastroenterol. Res. Pract 2020, 2020, 1–10. [Google Scholar] [CrossRef]
- Li, C.; Zhao, L.; Chen, Y.; He, T.; Chen, X.; Mao, J.; Li, C.; Lyu, J.; Meng, Q.H. MicroRNA-21 promotes proliferation, migration, and invasion of colorectal cancer, and tumor growth associated with down-regulation of sec23a expression. BMC Cancer 2016, 16, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Y.; Gao, X.; Wei, F.; Zhang, X.; Yu, J.; Zhao, H.; Sun, Q.; Yan, F.; Yan, C.; Li, H.; et al. Diagnostic and prognostic value of circulating miR-21 for cancer: A systematic review and meta-analysis. Gene 2014, 533, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Song, Y.; Xiong, Y.; Wang, X.; Xu, K.; Han, B.; Bai, Y.; Liming, Z.; Zhang, Y.; Zhou, L. MicroRNA-21 (Mir-21) Promotes Cell Growth and Invasion by Repressing Tumor Suppressor PTEN in Colorectal Cancer. Cell. Physiol. Biochem. 2017, 43, 945–958. [Google Scholar] [CrossRef] [PubMed]
- Kalinina, T.S.; Kononchuk, V.V.; Yakovleva, A.K.; Alekseenok, E.Y.; Sidorov, S.V.; Gulyaeva, L.F. Association between Lymph Node Status and Expression Levels of Androgen Receptor, miR-185, miR-205, and miR-21 in Breast Cancer Subtypes. Int. J. Breast Cancer 2020, 2020, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Xu, Y.; Sun, J.; Xu, J.; Li, Q.; Guo, Y.; Zhang, Q. miR-21 Is a Promising Novel Biomarker for Lymph Node Metastasis in Patients with Gastric Cancer. Gastroenterol. Res. Pract. 2012, 2012, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Jin, X.-H.; Lu, S.; Wang, A.-F. Expression and clinical significance of miR-4516 and miR-21-5p in serum of patients with colo-rectal cancer. BMC Cancer 2020, 20, 241. [Google Scholar] [CrossRef] [Green Version]
- Emelyanov, A.; Bulavin, D.V. Wip1 phosphatase in breast cancer. Oncogene 2014, 34, 4429–4438. [Google Scholar] [CrossRef] [Green Version]
- Bulavin, D.V.; Demidov, O.; Saito, S.; Kauraniemi, P.; Phillips, C.; Amundson, S.A.; Ambrosino, C.; Sauter, G.; Nebreda, A.R.; Anderson, C.W.; et al. Amplification of PPM1D in human tumors abrogates p53 tumor-suppressor activity. Nat. Genet. 2002, 31, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, C.; Schiff, R. HER2: Biology, detection, and clinical implications. Arch. Pathol. Lab. Med. 2011, 135, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.G.; Kerin, E.; O’Flaherty, C.; Maher, E.; Richard, V.; McAnena, P.; McLaughlin, R.P.; Sweeney, K.J.; Barry, M.K.; Malone, C.M.; et al. Clinicopathological response to neoadjuvant therapies and pathological complete response as a biomarker of survival in human epidermal growth factor receptor-2 enriched breast cancer—A retrospective cohort study. Breast 2021, 59, 67–75. [Google Scholar] [CrossRef]
- Liu, Y.; Xu, J.; Choi, H.H.; Han, C.; Fang, Y.; Li, Y.; Van Der Jeught, K.; Xu, H.; Zhang, L.; Frieden, M.; et al. Targeting 17q23 amplicon to overcome the resistance to anti-HER2 therapy in HER2+ breast cancer. Nat. Commun. 2018, 9, 1–16. [Google Scholar] [CrossRef]
- Conradi, L.-C.; Styczen, H.; Sprenger, T.; Wolff, H.A.; Rödel, C.; Nietert, M.; Homayounfar, K.; Gaedcke, J.; Kitz, J.; Talaulicar, R.; et al. Frequency of HER-2 Positivity in Rectal Cancer and Prognosis. Am. J. Surg. Pathol. 2013, 37, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Marx, A.H.; Burandt, E.C.; Choschzick, M.; Simon, R.; Yekebas, E.; Kaifi, J.T.; Mirlacher, M.; Atanackovic, D.; Bokemeyer, C.; Fiedler, W.; et al. Heterogenous high-level HER-2 amplifi-cation in a small subset of colorectal cancers. Hum. Pathol. 2010, 41, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.H.; Wu, F.; Loeb, G.B.; Hsu, R.; Heidersbach, A.; Brincat, A.; Horiuchi, D.; Lebbink, R.J.; Mo, Y.-Y.; Goga, A.; et al. Up-regulation of miR-21 by HER2/neu signaling promotes cell invasion. J. Biol. Chem. 2009, 284, 18515–18524. [Google Scholar] [CrossRef] [Green Version]
- Yuki, D.; Lin, Y.-M.; Fujii, Y.; Nakamura, Y.; Furukawa, Y. Isolation of LEM domain-containing 1, a novel testis-specific gene expressed in colorectal cancers. Oncol. Rep. 2004, 12, 275–280. [Google Scholar] [CrossRef]
- Nagel, R.; Le Sage, C.; Diosdado, B.; Van Der Waal, M.; Vrielink, J.A.O.; Bolijn, A.; Meijer, G.A.; Agami, R. Regulation of the Adenomatous Polyposis Coli Gene by the miR-135 Family in Colorectal Cancer. Cancer Res. 2008, 68, 5795–5802. [Google Scholar] [CrossRef] [Green Version]
- Liu, B.; Liu, Y.; Zhao, L.; Pan, Y.; Shan, Y.; Lifen, Z.; Yujia, S. Upregulation of microRNA-135b and microRNA-182 promotes chemoresistance of colorectal cancer by targeting ST6GALNAC2 via PI3K/AKT pathway. Mol. Carcinog. 2017, 56, 2669–2680. [Google Scholar] [CrossRef]
- Moustakas, A.; Heldin, C.H. The regulation of TGFbeta signal transduction. Development 2009, 136, 3699–3714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khatri, R.; Subramanian, S. MicroRNA-135b and Its Circuitry Networks as Potential Therapeutic Targets in Colon Cancer. Front. Oncol. 2013, 3, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandrés, E.; Cubedo, E.; Agirre, X.; Malumbres, R.; Zárate, R.; Ramirez, N.; Abajo, A.; Navarro, A.; Moreno, I.; Monzó, M.; et al. Identification by Real-time PCR of 13 mature microRNAs differentially expressed in colorectal cancer and non-tumoral tissues. Mol. Cancer 2006, 5, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarver, A.L.; French, A.J.; Borralho, P.M.; Thayanithy, V.; Oberg, A.L.; Silverstein, K.A.T.; Morlan, B.W.; Riska, S.M.; Boardman, L.A.; Cunningham, J.M.; et al. Human colon cancer profiles show differential microRNA expression depending on mismatch repair status and are characteristic of undifferentiated pro-liferative states. BMC Cancer 2009, 9, 401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.; Wang, Z.; Yang, P.; Yang, J.; Liang, J.; Chen, Y.; Wang, H.; Wei, G.; Ye, S.; Zhou, Y. MicroRNA-135b regulates metastasis suppressor 1 expression and promotes migration and invasion in colorectal cancer. Mol. Cell. Biochem. 2013, 388, 249–259. [Google Scholar] [CrossRef]
- Tong, G.-J.; Zhang, G.-Y.; Liu, J.; Zheng, Z.-Z.; Chen, Y.; Niu, P.-P.; Xu, X.-T. Comparison of the eighth version of the American Joint Committee on Cancer manual to the seventh version for colorectal cancer: A retrospective review of our data. World J. Clin. Oncol. 2018, 9, 148–161. [Google Scholar] [CrossRef]
- David, W.; Hosmer, S.L. Applied Logistic Regression, 2nd ed.; Wiley Online Library: Hoboken, NJ, USA, 2020. [Google Scholar]
- Ryan, É.J.; Creavin, B.; Sheahan, K. Delivery of Personalized Care for Locally Advanced Rectal Cancer: Incorporating Patho-logical, Molecular Genetic, and Immunological Biomarkers Into the Multimodal Paradigm. Front. Oncol. 2020, 10, 1369. [Google Scholar] [CrossRef]
| Clinicopathological Parameter | Patients with Colorectal Cancer (N = 74) |
|---|---|
| Mean age (±SD, range) | 67.8 years (±12.5, 38–90 years) |
| Gender Male Female | 51 (68.9%) 23 (31.1%) |
| Tumour Location Colon Rectum | 52 (70.3%) 22 (29.7%) |
| Presentation Emergency Elective | 12 (16.2%) 62 (83.8%) |
| Histological subtype Adenocarcinoma Mucinous Other/Missing | 53 (68.0%) 3 (3.8%) 22 (28.2) |
| Tumour Stage T1 T2 T3 T4 TX | 2 (2.7%) 5 (6.8%) 25 (33.8%) 18 (24.3%) 24 (32.4%) |
| Nodal Stage N0 N1 N2 NX | 15 (20.3%) 20 (27.0%) 10 (13.5%) 29 (39.2%) |
| Chemotherapy Received NAC Received AC Did not receive/Unknown | 12 (16.2%) 40 (54.1%) 22 (29.7%) |
| Recurrence Recurrence No Recurrence | 18 (24.3%) 56 (75.7%) |
| Recurrence Location Liver Lung Adrenal Liver and Lung Adrenal and Liver Mediastinum Pelvis None | 7 (9.0%) 3 (3.9%) 2 (2.6%) 1 (1.3%) 1 (1.3%) 1 (1.3%) 3 (3.9%) 56 (75.7%) |
| Survival Alive RIP | 43 (58.1%) 31 (41.9%) |
| 5-Year DFS | 51/74 (68.9%) |
| 5-Year OS | 53/74 (71.6%) |
| Target | MiRNA Function | Expression Levels | CT Difference | Efficiencies |
|---|---|---|---|---|
| miR-21 | Well-described oncogenic miRNA in several malignancies [21] | Increased | 12.19 | 97% |
| miR-31 | Previously reported oncogenic miRNA in CRC [33] | Increased | 14.42 | 101% |
| miR-135b | Modulatory role in malignancy and CRC [34] | Decreased | 14.13 | 99% |
| miR-150 | Associated with disease progression and metastases in CRC [35] | Increased | 10.88 | 106% |
| miR-155 | Correlated to CRC development, invasion, and metastasis [36] | Increased | 13.83 | 108% |
| miR-195 | Known oncogenic biomarker in malignancy [21] | Increased | 11.88 | 93% |
| miR-16 | Endogenous control [37] | Stable | 0.00 | - |
| miR-345 | Endogenous control [37] | Stable | 0.00 | - |
| Parameter | Comparing Means | |||||
|---|---|---|---|---|---|---|
| miR-21 | miR-31 | miR-135b | miR-150 | miR-155 | miR-195 | |
| Tumour Stage ▯ | 0.399 | 0.561 | 0.509 | 0.079 | 0.008 * | 0.308 |
| Nodal Stage ▯ | 0.037 * | 0.735 | 0.024 * | 0.690 | 0.821 | 0.162 |
| EMVI ▯ | 0.957 | 0.349 | 0.860 | 0.456 | 0.507 | 0.029 * |
| LVI ▯ | 0.899 | 0.249 | 0.341 | 0.982 | 1.000 | 0.748 |
| Colon vs. Rectal ▯ | 0.850 | 0.035 * | 0.284 | 0.052 | 0.272 | 0.327 |
| Differentiation ▯ | 0.887 | 0.275 | 0.307 | 0.051 | 0.179 | 0.532 |
| Histology ▯ | 0.224 | 0.083 | 0.629 | 0.045 * | 0.048 * | 0.118 |
| Recurrence ▯ | 0.857 | 0.550 | 0.013 * | 0.538 | 0.602 | 0.001 * |
| Mortality ▯ | 0.431 | 0.800 | 0.980 | 0.955 | 0.979 | 0.609 |
| Parameter | Comparing Medians | |||||
| miR-21 | miR-31 | miR-135b | miR-150 | miR-155 | miR-195 | |
| Tumour Stage † | 0.365 | 0.652 | 0.628 | 0.103 | 0.139 | 0.226 |
| Nodal Stage † | 0.039 * | 0.480 | 0.022 * | 0.630 | 0.199 | 0.144 |
| EMVI † | 0.889 | 0.711 | 0.889 | 0.667 | 0.500 | 0.095 |
| LVI † | 0.141 | 0.221 | 0.781 | 0.891 | 0.233 | 0.256 |
| Colon vs. Rectal † | 0.614 | 0.068 | 0.393 | 0.024 * | 0.757 | 0.199 |
| Differentiation † | 0.889 | 0.581 | 0.222 | 0.183 | 0.222 | 0.889 |
| Histology † | 0.424 | 0.078 | 0.547 | 0.053 | 0.051 | 0.100 |
| Recurrence † | 0.354 | 0.677 | 0.023 * | 0.370 | 0.818 | 0.006 * |
| Mortality † | 0.386 | 0.930 | 0.831 | 0.889 | 0.791 | 0.934 |
| Binary Outcome-Recurrence | Cox Regression-Recurrence | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | β-Coefficient (SE) | p-Value | β-Coefficient (SE) | p-Value | HR (95% CIs) | p-Value | HR (95% CIs) | p-Value |
| Univariable | Multivariable | Univariable | Multivariable | |||||
| miR-21 | 0.282 (0.579) | 0.626 | 0.372 (1.138) | 0.744 | 1.303 (0.430–4.130) | 0.626 | 1.450 (0.160–13.490) | 0.744 |
| miR-31 | 0.403 (0.413) | 0.330 | −0.125 (0.770) | 0.873 | 1.500 (0.670–3.360) | 0.330 | 0.880 (0.200–3.990) | 0.871 |
| miR-135b | −1.126 (0.467) | 0.017 * | −0.515 (0.808) | 0.524 | 0.320 (0.130–0.810) | 0.017 * | 0.600 (0.120–2.910) | 0.524 |
| miR-150 | 1.156 (0.630) | 0.067 | 1.023 (1.040) | 0.325 | 3.180 (0.920–0.91) | 0.067 | 2.780 (0.360–21.340) | 0.325 |
| miR-155 | −0.016 (0.702) | 0.982 | 3.175 (2.139) | 0.138 | 0.980 (0.250–3.900) | 0.982 | 23.910 (0.360–21.340) | 0.138 |
| miR-195 | 1.442 (0.446) | 0.001 * | 3.187 (1.419) | 0.025 * | 4.230 (1.77–10.13) | 0.001 * | 24.210 (1.500–390.780) | 0.025 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davey, M.G.; Feeney, G.; Annuk, H.; Paganga, M.; Holian, E.; Lowery, A.J.; Kerin, M.J.; Miller, N. MicroRNA Expression Profiling Predicts Nodal Status and Disease Recurrence in Patients Treated with Curative Intent for Colorectal Cancer. Cancers 2022, 14, 2109. https://doi.org/10.3390/cancers14092109
Davey MG, Feeney G, Annuk H, Paganga M, Holian E, Lowery AJ, Kerin MJ, Miller N. MicroRNA Expression Profiling Predicts Nodal Status and Disease Recurrence in Patients Treated with Curative Intent for Colorectal Cancer. Cancers. 2022; 14(9):2109. https://doi.org/10.3390/cancers14092109
Chicago/Turabian StyleDavey, Matthew G., Gerard Feeney, Heidi Annuk, Maxwell Paganga, Emma Holian, Aoife J. Lowery, Michael J. Kerin, and Nicola Miller. 2022. "MicroRNA Expression Profiling Predicts Nodal Status and Disease Recurrence in Patients Treated with Curative Intent for Colorectal Cancer" Cancers 14, no. 9: 2109. https://doi.org/10.3390/cancers14092109
APA StyleDavey, M. G., Feeney, G., Annuk, H., Paganga, M., Holian, E., Lowery, A. J., Kerin, M. J., & Miller, N. (2022). MicroRNA Expression Profiling Predicts Nodal Status and Disease Recurrence in Patients Treated with Curative Intent for Colorectal Cancer. Cancers, 14(9), 2109. https://doi.org/10.3390/cancers14092109






