The Psychological Distress of Cancer Patients following the COVID-19 Pandemic First Lockdown: Results from a Large French Survey
Abstract
:Simple Summary
Abstract
1. Introduction
2. Material and Methods
2.1. Participants
2.2. Assessments Tools
2.3. Statistical Analysis
3. Results
3.1. Description of the Study Population
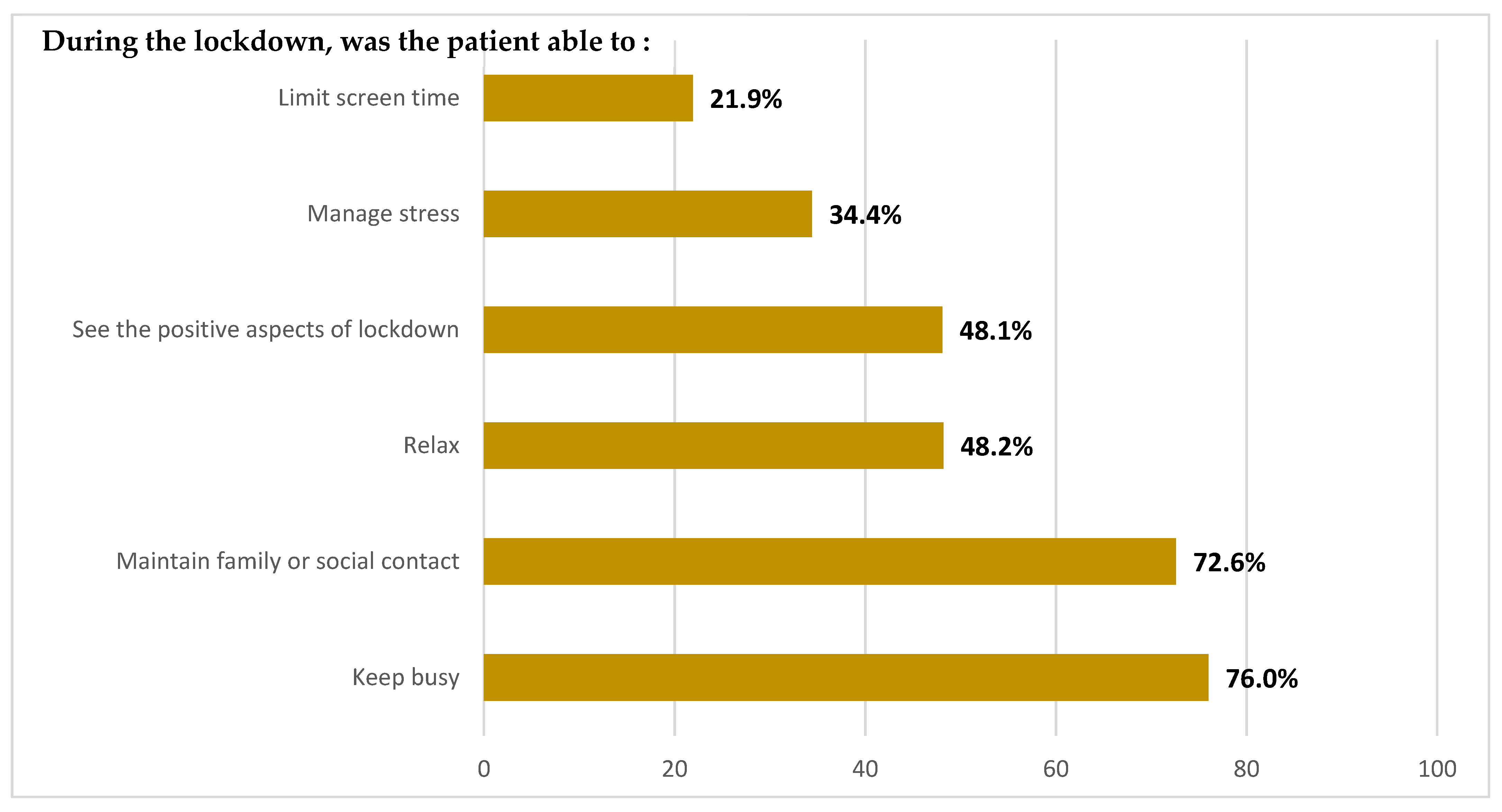
3.2. Univariate Analyses
3.3. Factors Associated with Anxiety One Month Following COVID-19-Related Lockdown
3.4. Factors Associated with Post-Traumatic Stress Disorder One Month Following COVID-19-Related Lockdown
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van de Haar, J.; Hoes, L.R.; Coles, C.E.; Seamon, K.; Frohling, S.; Jäger, D.; Valenza, F.; De Braud, F.; De Petris, L.; Bergh, J.; et al. Caring for patients with cancer in the COVID-19 era. Nat. Med. 2020, 26, 665–671. [Google Scholar] [CrossRef] [Green Version]
- Van Dorn, A.V. COVID-19 and readjusting clinical trials. Lancet 2020, 396, 523–524. [Google Scholar] [CrossRef]
- You, B.; Ravaud, A.; Canivet, A.; Ganem, G.; Giraud, P.; Guimbaud, R.; Kaluzinski, L.; Krakowski, I.; Mayeur, D.; Grellety, T.; et al. The official French guidelines to protect patients with cancer against SARS-CoV-2 infection. Lancet 2020, 21, 619–621. [Google Scholar] [CrossRef] [Green Version]
- Liang, W.; Guan, W.; Chen, R.; Wang, W.; Li, J.; Xu, K.; Li, C.; Ai, Q.; Lu, W.; Liang, H. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020, 21, 335–337. [Google Scholar] [CrossRef]
- Dai, M.; Liu, D.; Zhou, F.; Zhou, F.; Li, G.; Chen, Z.; Zhang, Z.; You, H.; Wu, M.; Zheng, Q.; et al. Patients with cancer appear more vulnerable to SARS-CoV-2: A multicenter study during the COVID-19 outbreak. Cancer Discov. 2020, 10, 783–791. [Google Scholar]
- Miyashita, H.; Mikami, T.; Chopra, N.; Yamada, T.; Chernyavsky, S.; Rizk, D.; Cruz, C. Do Patients with Cancer Have a Poorer Prognosis of COVID-19? An Experience in New York City. Ann. Oncol. 2020, 31, 1088–1089. [Google Scholar] [CrossRef]
- Wang, Q.; Berger, N.A.; Xu, R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021, 7, 220–227. [Google Scholar] [CrossRef]
- Mac Gregor, M.C.; Lei, X.; Zhao, H.; Scheet, P.; Giordano, S.H. Evaluation of COVID-19 Mortality and Adverse Outcomes in US Patients With or Without Cancer. JAMA Oncol. 2022, 8, 69–78. [Google Scholar] [CrossRef]
- Hanna, T.; Evans, G.A.; Booth, C. Cancer, COVID-19 and the precautionary principle: Prioritizing treatment during a global pandemic. Nat. Rev. Clin. Oncol. 2020, 17, 268–270. [Google Scholar] [CrossRef]
- Ueda, M.; Martins, R.; Hendrie, P. Managing Cancer Care During the COVID-19 Pandemic: Agility and Collaboration Toward a Common Goal. J. Natl. Compr. Cancer Netw. 2020, 18, 366–369. [Google Scholar] [CrossRef] [Green Version]
- Curigliano, G.; Banerjee, S.; Cervantes, A.; Garassino, M.; Garrido, P.; Girard, N.; Haanen, J.; Jordan, K.; Lordick, F.; Machiels, J.P.; et al. Managing cancer patients during the COVID-19 pandemic: An ESMO multidisciplinary expert consensus. Ann. Oncol. 2020, 31, 1320–1335. [Google Scholar] [CrossRef] [PubMed]
- Miaskowski, C.; Paul, S.M.; Snowberg, K.; Abbott, M.; Borno, H.; Chang, S.; Chen, L.M.; Cohen, B.; Cooper, B.A.; Hammer, M.J.; et al. Oncology patients’ perceptions of and experiences with COVID-19. Support. Care Cancer 2021, 29, 1941–1950. [Google Scholar] [CrossRef] [PubMed]
- Guven, D.C.; Sahin, T.K.; Aktepe, O.H.; Yildirim, H.C.; Aksoy, S.; Aksoy, S.; Kilickap, S. Perspectives, knowledge, and fears of cancer patients about COVID-19. Front. Oncol. 2020, 10, 1553. [Google Scholar] [CrossRef] [PubMed]
- Singer, S.; Das-Munshi, J.; Brahler, E. Prevalence of mental health conditions in cancer patients in acute care—A meta-analysis. Ann. Oncol. 2010, 21, 925–930. [Google Scholar] [CrossRef]
- Cordova, M.; Riba, M.; Spiegel, D. Post-traumatic stress disorder and cancer. Lancet Psychiatry 2017, 4, 330–338. [Google Scholar] [CrossRef] [Green Version]
- de Joode, K.; Dumoulin, D.W.; Engelen, V.; Bloemendal, H.J.; Verheij, M.; van Laarhoven, H.W.; Dingemans, I.H.; Dingemans, A.C.; van der Veldt, A.M. Impact of the coronavirus disease 2019 pandemic on cancer treatment: The patients’ perspective. Eur. J. Cancer 2020, 136, 132–139. [Google Scholar] [CrossRef]
- Rodler, S.; Apfelbeck, M.; Schulz, G.B.; Ivanova, T.; Buchner, A.; Staehler, M.; Heinemann, V.; Stief, C.; Casuscelli, J. Telehealth in uro-oncology beyond the pandemic: Toll or lifesaver? Eur. Urol. Focus 2020, 6, 1097–1103. [Google Scholar] [CrossRef]
- Joly, F.; Rigal, O.; Guittet, L.; Lefèvre-Arbogast, S.; Grellard, J.M.; Binarelli, G.; Lange, M.; Rieux, C.; Fernette, M.; Tron, L.; et al. Post-traumatic stress symptomatology and adjustment of medical oncology practice during the COVID-19 pandemic among adult patients with cancer in a day care hospital. Cancer 2021, 127, 4636–4645. [Google Scholar] [CrossRef]
- Yang, S.; Dong, D.; Gu, H.; Gale, R.P.; Ma, J.; Huang, X. Impact of stopping therapy during the SARS-CoV-2 pandemic in persons with lymphoma. J. Cancer Res. Clin. Oncol. 2020, 147, 1469–1479. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Weiss, D.S.; Marmar, C.R. The impact of event scale–revised. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar] [CrossRef] [Green Version]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale Revised. Behav. Res. Ther. 2003, 41, 1489–1496. [Google Scholar] [CrossRef]
- Simard, S.; Savard, J. Fear of Cancer Recurrence Inventory: Development and initial validation of a multidimensional measure of fear of cancer recurrence. Support. Care Cancer 2008, 17, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Ayubi, E.; Bashirian, S.; Khazaei, S. Depression and Anxiety Among Patients with Cancer During COVID-19 Pandemic: A Systematic Review and Meta-analysis. J. Gastrointest. Cancer 2021, 52, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Santa-Maria, C.A.; Feng, H.; Wang, L.; Zhang, P.; Xu, Y.; Tan, Y.; Liu, Z.; Du, B.; Lan, M.; et al. Patient-reported Outcomes of Patients With Breast Cancer During the COVID-19 Outbreak in the Epicenter of China: A Cross-sectional Survey Study. Clin. Breast Cancer 2020, 20, e651–e662. [Google Scholar] [CrossRef]
- Mitchell, A.; Chan, M.; Bhatti, H.; Halton, M.; Grassi, L.; Johansen, C.; Meader, N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011, 12, 160–174. [Google Scholar] [CrossRef]
- Pitman, A.; Suleman, S.; Hyde, N.; Hodgkiss, A. Depression and anxiety in patients with cancer. BMJ 2018, 361, k1415. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Duan, Z.; Ma, Z.; Mao, Y.; Li, X.; Wilson, A.; Qin, H.; Ou, J.; Peng, K.; Zhou, F.; et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl. Psychiatry 2020, 10, 263. [Google Scholar] [CrossRef]
- Brandenbarg, D.; Maass, S.; Geerse, O.P.; Stegmann, M.E.; Handberg, C.; Schroevers, M.J.; Duijts, S. A systematic review on the prevalence of symptoms of depression, anxiety and distress in long-term cancer survivors: Implications for primary care. Eur. J. Cancer Care 2019, 28, e13086. [Google Scholar] [CrossRef]
- Edge, R.; Meyers, J.; Tiernan, G.; Tiernan, G.; Li, Z.; Schiavuzzi, A.; Chan, P.; Vassallo, A.; Morrow, A.; Mazariego, C.; et al. Cancer care disruption and reorganisation during the COVID-19 pandemic in Australia: A patient, carer and healthcare worker perspective. PLoS ONE 2021, 16, e0257420. [Google Scholar] [CrossRef]
- Walker, J.; Holm Hansen, C.; Martin, P.; Sawhney, A.; Thekkumpurath, P.; Beale, C.; Symeonides, S.; Wall, L.; Murray, G.; Sharpe, M. Prevalence of depression in adults with cancer: A systematic review. Ann. Oncol. 2013, 24, 895–900. [Google Scholar] [CrossRef]
- Härtl, K.; Schennach, R.; Müller, M.; Engel, J.; Reinecker, H.; Sommer, H.; Friese, K. Quality of life, anxiety, and oncological factors: A follow-up study of breast cancer patients. Psychosomatics 2010, 51, 112–123. [Google Scholar] [CrossRef]
- Hagen, K.B.; Aas, T.; Kvaløy, J.T.; Eriksen, H.R.; Søiland, H.; Lind, R. Fatigue, anxiety and depression overrule the role of oncological treatment in predicting self-reported health complaints in women with breast cancer compared to healthy controls. Breast 2016, 28, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Schubart, J.R.; Emerich, M.; Farnan, M.; Smith, J.S.; Kauffman, G.L.; Kass, R.B. Screening for Psychological Distress in Surgical Breast Cancer Patients. Ann. Surg. Oncol. 2014, 21, 3348–3353. [Google Scholar] [CrossRef] [PubMed]
- Carreira, H.; Williams, R.; Müller, M.; Harewood, R.; Stanway, S.; Bhaskaran, K. Associations between breast cancer survivorship and adverse mental health outcomes: A systematic review. J. Natl. Cancer Inst. 2018, 110, 1311–1327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Gray, N.S.; O’Connor, C.; Knowles, J.; Pink, J.; Simkiss, N.J.; Williams, S.D.; Snowden, R.J. The Influence of the COVID-19 Pandemic on Mental Well-Being and Psychological Distress: Impact upon a Single Country. Front. Psychiatry 2020, 11, 594115. [Google Scholar] [CrossRef]
- Sigorski, D.; Sobczuk, P.; Osmola, M.; Kuć, K.; Walerzak, A.; Wilk, M.; Ciszewski, T.; Kopeć, S.; Hryń, K.; Rutkowski, P.; et al. Impact of COVID-19 on anxiety levels among patients with cancer actively treated with systemic therapy. ESMO Open 2020, 5, e000970. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2021, 26, 13–22. [Google Scholar] [CrossRef] [Green Version]
| Variables | Total n = 1097 | Anxiety Level (STAI-S) n = 962 | Post-Traumatic Stress Disorder (IES-R) n = 810 | ||
|---|---|---|---|---|---|
| n (%) | Absence of Anxiety + n = 669 (69.5%) | Presence of Anxiety ++ n = 293 (30.5%) | Low * Level of Post-Traumatic Stress Disorder n = 691 (85.3%) | Moderate/Severe ** Level of Post-Traumatic Stress Disorder n = 119 (14.7%) | |
| Factors related of COVID-19 health crisis | |||||
| Contracted COVID-19 | p = 0.675 | p = 0.100 | |||
| No | 999 (92.3) | 613 (92.5) | 264 (91.7) | 638 (93.1) | 103 (88.8) |
| Yes | 83 (7.7) | 50 (7.5) | 24 (8.3) | 47 (6.9) | 13 (11.2) |
| Living status during lockdown | p = 0.235 | p = 0.137 | |||
| Living alone | 228 (21.3) | 126 (19.2) | 67 (23.4) | 138 (20.3) | 31 (26.5) |
| Living with others | 800 (75.0) | 511 (77.9) | 209 (72.8) | 522 (76.6) | 80 (68.4) |
| Was not in lockdown | 39 (3.7) | 19 (2.9) | 11 (3.8) | 21 (3.1) | 6 (5.1) |
| Overall ‘lockdown experience’ scoreMean (SD) | p< 0.001 | p< 0.001 | |||
| 46.5 (26.1) | 51.4 (25.9) | 38.9 (24.8) | 50.0 (26.6) | 37.0 (24.2) | |
| Completely satisfied with the current management of their cancer | p< 0.001 | p= 0.001 | |||
| Yes | 798 (74.2) | 529 (80.1) | 178 (61.8) | 522 (76.3) | 72 (62.1) |
| No | 278 (25.8) | 131 (19.9) | 110 (38.2) | 162 (23.7) | 44 (37.9) |
| Completely satisfied with the measures put in place at the hospital to reduce their exposure to COVID-19 | p< 0.001 | p= 0.001 | |||
| Yes | 769 (76.0) | 497 (79.8) | 189 (68.7) | 510 (77.9) | 72 (63.7) |
| No | 243 (24.0) | 126 (20.2) | 86 (31.3) | 145 (22.1) | 41 (36.3) |
| Fear of going to hospital for treatment because of the risk of COVID-19 contamination | p< 0.001 | p< 0.001 | |||
| No | 858 (80.4) | 555 (84.9) | 204 (70.8) | 582 (86.0) | 71 (60.7) |
| Yes | 209 (19.6) | 99 (15.1) | 84 (29.2) | 95 (14.0) | 46 (39.3) |
| Consulted a psychologist or psychiatrist during the pandemic | p< 0.001 | p= 0.001 | |||
| No, never | 910 (84.9) | 573 (87.3) | 231 (79.4) | 586 (86.1) | 92 (78.0) |
| Yes, only once | 86 (8.0) | 55 (8.4) | 23 (7.9) | 60 (8.8) | 8 (6.8) |
| Yes, several times | 76 (7.1) | 28 (4.3) | 37 (12.7) | 35 (5.1) | 18 (15.2) |
| Cancer-related factors | |||||
| Type of cancer | p= 0.001 | p = 0.066 | |||
| Hematological | 252 (24.3) | 168 (26.5) | 57 (20.2) | 163 (24.7) | 27 (23.5) |
| Urological | 111 (10.7) | 83 (13.1) | 20 (7.1) | 83 (12.6) | 5 (4.3) |
| Digestive | 164 (15.8) | 97 (15.3) | 43 (15.2) | 104 (15.8) | 16 (13.9) |
| Breast/Gynecological | 429 (41.4) | 232 (36.7) | 142 (50.4) | 259 (39.3) | 57 (49.6) |
| Other | 81 (7.8) | 53 (8.4) | 20 (7.1) | 50 (7.6) | 10 (8.7) |
| Treatment phase | p< 0.001 | p = 0.209 | |||
| On treatment | 647 (60.6) | 386 (59.4) | 186 (64.1) | 419 (62.1) | 66 (56.4) |
| Post-treatment follow-up | 327 (30.7) | 223 (34.3) | 68 (23.5) | 206 (30.5) | 37 (31.6) |
| About to initiate treatment | 93 (8.7) | 41 (6.3) | 36 (12.4) | 50 (7.4) | 14 (12.0) |
| Fear of cancer recurrence (severity subscale) | p< 0.001 | p< 0.001 | |||
| No (score < 13) | 301 (35.1) | 254 (44.3) | 23 (10.0) | 243 (41.0) | 12 (11.8) |
| Yes (score ≥ 13) | 557 (64.9) | 319 (55.7) | 206 (90.0) | 349 (59.0) | 90 (88.2) |
| Sociodemographic factors | |||||
| Gender | p< 0.001 | p< 0.001 | |||
| Women | 691 (63.2) | 376 (56.3) | 220 (75.3) | 406 (59.0) | 91 (76.5) |
| Men | 403 (36.8) | 292 (43.7) | 72 (24.7) | 282 (41.0) | 28 (23.5) |
| Age (years) | p= 0.002 | p = 0.074 | |||
| 22–50 | 156 (14.4) | 86 (13.0) | 63 (21.6) | 105 (15.4) | 28 (23.9) |
| 51–70 | 516 (47.7) | 343 (52.0) | 127 (43.6) | 355 (52.1) | 55 (47.0) |
| 71–92 | 409 (37.9) | 230 (35.0) | 101 (34.7) | 221 (32.5) | 34 (29.1) |
| Living alone at home | p = 0.152 | p= 0.012 | |||
| No | 806 (75.0) | 506 (76.9) | 206 (72.5) | 522 (76.9) | 78 (66.1) |
| Yes | 269 (25.0) | 152 (23.1) | 78 (27.5) | 157 (23.1) | 40 (33.9) |
| Education level | p = 0.071 | p = 0.282 | |||
| No schooling/primary school | 95 (8.8) | 44 (6.7) | 22 (7.6) | 44 (6.5) | 12 (10.2) |
| Secondary school | 457 (42.4) | 264 (40.1) | 137 (47.2) | 298 (43.8) | 46 (39.0) |
| Higher education | 521 (48.8) | 351 (53.2) | 131 (45.2) | 339 (49.8) | 60 (50.8) |
| Professional situation before lockdown | p= 0.025 | p= 0.031 | |||
| Active | 173 (15.9) | 112 (16.8) | 47 (16.2) | 122 (17.8) | 22 (18.6) |
| Inactive | 262 (24.0) | 156 (23.5) | 92 (31.7) | 170 (24.8) | 42 (35.6) |
| Retirement | 654 (60.1) | 397 (59.7) | 151 (52.1) | 394 (57.4) | 54 (45.8) |
| Had experienced difficult elements of life in the previous 6 months (i.e., before COVID-19 pandemic) | p< 0.001 | p< 0.001 | |||
| No | 501 (45.7) | 358 (53.6) | 85 (29.1) | 336 (48.7) | 34 (28.6) |
| Yes | 594 (54.3) | 310 (46.4) | 207 (70.9) | 354 (51.3) | 85 (71.4) |
| Ref: Absence of Anxiety + | Presence of Anxiety (STAI-S) ++ n = 763 | Ref: No/Low-Level of Post-Traumatic Stress Disorder * | Moderate/Severe Level of Post-Traumatic Stress Disorder (IES-R) n= 635 | ||
|---|---|---|---|---|---|
| aOR | 95% CI | aOR | 95% CI | ||
| Gender(Ref: Men) | Gender(Ref: Men) | ||||
| Woman | 1.62 | 1.09–2.41 | Woman | 1.97 | 1.18–3.29 |
| Age(Ref: 51–70) | Living alone at home(Ref: No) | ||||
| 22–50 | 1.54 | 0.97–2.44 | Yes | 1.63 | 1.01–2.63 |
| 71–92 | 1.65 | 1.08–2.51 | Overall ‘lockdown experience’ score | 0.98 | 0.97–0.99 |
| Treatment phase (Ref: On treatment) | 0.83 | 0.55–1.25 | Fear of coming to the hospital for treatment because of the risk of COVID-19 contamination(Ref: No) | ||
| Post-treatment follow-up | Yes | 3.49 | 2.11–5.79 | ||
| About to initiate treatment | 2.31 | 1.25–4.28 | |||
| Fear of cancer recurrence (severity subscale) (Ref: No (score < 13)) | |||||
| Yes (score ≥ 13) | 5.02 | 3.07–8.18 | |||
| Had experienced difficult elements of life in the previous 6 months (i.e., before COVID-19 pandemic) (Ref: No) | |||||
| Yes | 2.11 | 1.45–3.07 | |||
| Completely satisfied with the current management of their cancer (Ref: Yes) | |||||
| No | 2.36 | 1.62–3.44 | |||
| Fear of going to hospital for treatment because of the risk of COVID-19 contamination(Ref: No) | |||||
| Yes | 2.43 | 1.61–3.67 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marino, P.; Touzani, R.; Pakradouni, J.; Ben Soussan, P.; Gravis, G. The Psychological Distress of Cancer Patients following the COVID-19 Pandemic First Lockdown: Results from a Large French Survey. Cancers 2022, 14, 1794. https://doi.org/10.3390/cancers14071794
Marino P, Touzani R, Pakradouni J, Ben Soussan P, Gravis G. The Psychological Distress of Cancer Patients following the COVID-19 Pandemic First Lockdown: Results from a Large French Survey. Cancers. 2022; 14(7):1794. https://doi.org/10.3390/cancers14071794
Chicago/Turabian StyleMarino, Patricia, Rajae Touzani, Jihane Pakradouni, Patrick Ben Soussan, and Gwenaelle Gravis. 2022. "The Psychological Distress of Cancer Patients following the COVID-19 Pandemic First Lockdown: Results from a Large French Survey" Cancers 14, no. 7: 1794. https://doi.org/10.3390/cancers14071794
APA StyleMarino, P., Touzani, R., Pakradouni, J., Ben Soussan, P., & Gravis, G. (2022). The Psychological Distress of Cancer Patients following the COVID-19 Pandemic First Lockdown: Results from a Large French Survey. Cancers, 14(7), 1794. https://doi.org/10.3390/cancers14071794







