Pharmacologic Strategies for Post-Transplant Maintenance in Acute Myeloid Leukemia: It Is Time to Consider!
Abstract
:Simple Summary
Abstract
1. Introduction
2. Prophylaxis or Pre-Emptive?
3. Patient 1: Secondary AML with Adverse Cytogenetics
4. Maintenance with Hypomethylating Agents
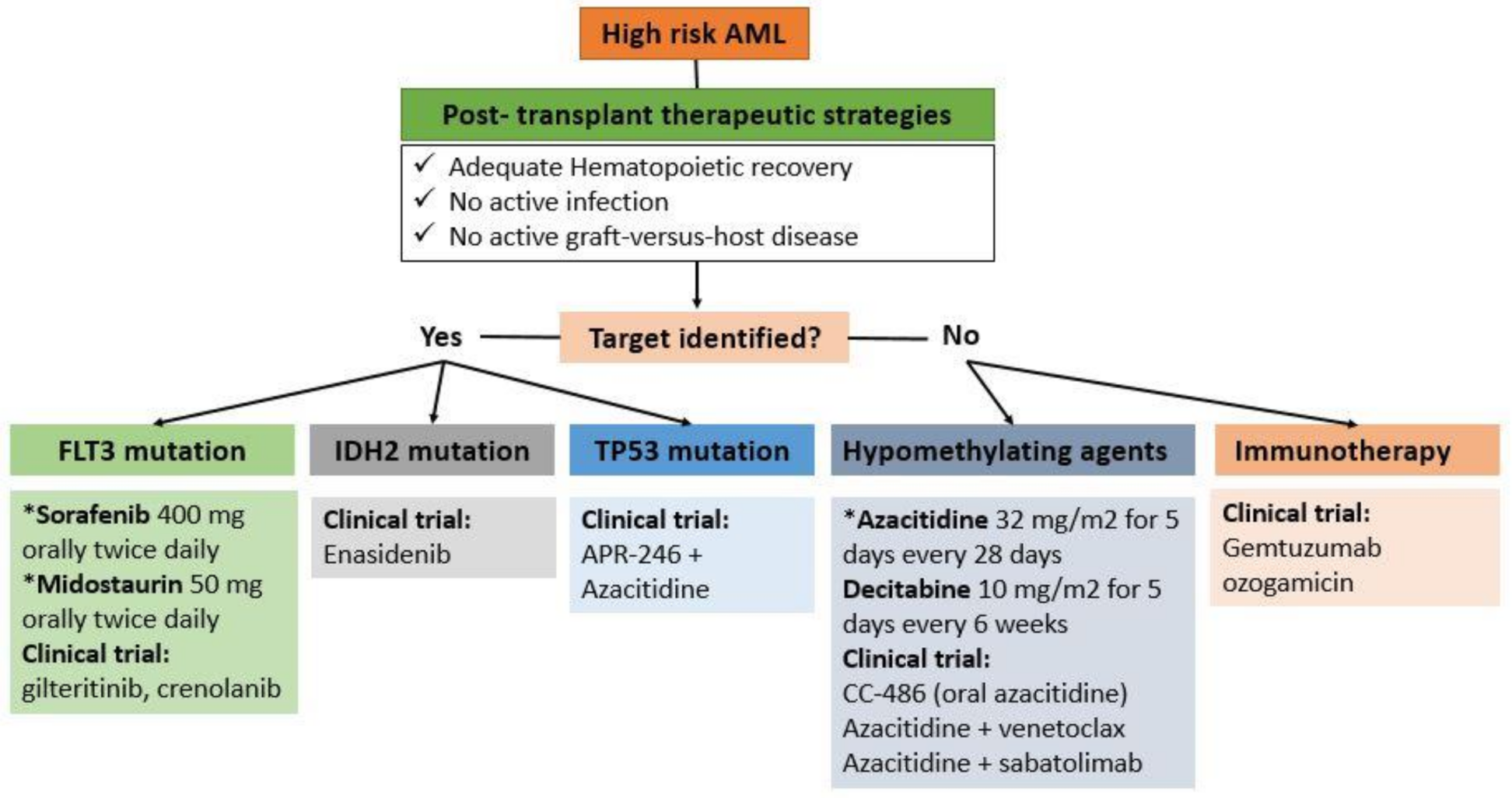
5. Patient 2: A Young Patient with FLT3-ITD Mutant AML in First Remission
6. Maintenance with FLT3-Inhibitors
7. Maintenance with Promising Novel Agents
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Döhner, H.; Estey, E.; Grimwade, D.; Amadori, S.; Appelbaum, F.R.; Büchner, T.; Dombret, H.; Ebert, B.L.; Fenaux, P.; Larson, R.A.; et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 2017, 129, 424–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rambaldi, A.; Grassi, A.; Masciulli, A.; Boschini, C.; Micò, M.C.; Busca, A.; Bruno, B.; Cavattoni, I.; Santarone, S.; Raimondi, R.; et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: An open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015, 16, 1525–1536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fasslrinner, F.; Schetelig, J.; Burchert, A.; Kramer, M.; Trenschel, R.; Hegenbart, U.; Stadler, M.; Schäfer-Eckart, K.; Bätzel, M.; Eich, H.; et al. Long-term efficacy of reduced-intensity versus myeloablative conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: Retrospective follow-up of an open-label, randomised phase 3 trial. Lancet Haematol. 2018, 5, e161–e169. [Google Scholar] [CrossRef] [PubMed]
- Loke, J.; Malladi, R.; Moss, P.; Craddock, C. The role of allogeneic stem cell transplantation in the management of acute myeloid leukaemia: A triumph of hope and experience. Br. J. Haematol. 2020, 188, 129–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bazarbachi, A.; Schmid, C.; Labopin, M.; Beelen, D.; Blau, I.W.; Potter, V.; Niittyvuopio, R.; Socié, G.; Blaise, D.; Sanz, J.; et al. Evaluation of Trends and Prognosis Over Time in Patients with AML Relapsing After Allogeneic Hematopoietic Cell Transplant Reveals Improved Survival for Young Patients in Recent Years. Clin. Cancer Res. 2020, 26, 6475–6482. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Moon, J.H.; Ahn, J.-S.; Kim, Y.-K.; Lee, S.-S.; Ahn, S.-Y.; Jung, S.-H.; Yang, D.-H.; Lee, J.-J.; Choi, S.H.; et al. Next-generation sequencing–based posttransplant monitoring of acute myeloid leukemia identifies patients at high risk of relapse. Blood 2018, 132, 1604–1613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Y.; Othus, M.; Araki, D.; Wood, B.L.; Radich, J.P.; Halpern, A.B.; Mielcarek, M.; Estey, E.H.; Appelbaum, F.R.; Walter, R.B. Pre- and post-transplant quantification of measurable (‘minimal’) residual disease via multiparameter flow cytometry in adult acute myeloid leukemia. Leukemia 2016, 30, 1456–1464. [Google Scholar] [CrossRef] [PubMed]
- Heuser, M.; Heida, B.; Büttner, K.; Wienecke, C.P.; Teich, K.; Funke, C.; Brandes, M.; Klement, P.; Liebich, A.; Wichmann, M.; et al. Posttransplantation MRD monitoring in patients with AML by next-generation sequencing using DTA and non-DTA mutations. Blood Adv. 2021, 5, 2294–2304. [Google Scholar] [CrossRef] [PubMed]
- Craddock, C.; Jackson, A.; Loke, J.; Siddique, S.; Hodgkinson, A.; Mason, J.; Andrew, G.; Nagra, S.; Malladi, R.; Peniket, A.; et al. Augmented Reduced-Intensity Regimen Does Not Improve Postallogeneic Transplant Outcomes in Acute Myeloid Leukemia. J. Clin. Oncol. 2021, 39, 768–778. [Google Scholar] [CrossRef] [PubMed]
- Bader, P.; Beck, J.; Frey, A.; Schlegel, P.G.; Hebarth, H.; Handgretinger, R.; Einsele, H.; Niemeyer, C.; Benda, N.; Faul, C.; et al. Serial and quantitative analysis of mixed hematopoietic chimerism by PCR in patients with acute leukemias allows the prediction of relapse after allogeneic BMT. Bone Marrow Transplant. 1998, 21, 487–495. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.C.; Saliba, R.M.; Rondon, G.; Chen, J.; Charafeddine, Y.; Medeiros, L.J.; Alatrash, G.; Andersson, B.S.; Popat, U.; Kebriaei, P.; et al. Mixed T Lymphocyte Chimerism after Allogeneic Hematopoietic Transplantation Is Predictive for Relapse of Acute Myeloid Leukemia and Myelodysplastic Syndromes. Biol. Blood Marrow Transplant. 2015, 21, 1948–1954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waterhouse, M.; Pfeifer, D.; Duque-Afonso, J.; Follo, M.; Duyster, J.; Depner, M.; Bertz, H.; Finke, J. Droplet digital PCR for the simultaneous analysis of minimal residual disease and hematopoietic chimerism after allogeneic cell transplantation. Clin. Chem. Lab. Med. 2019, 57, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Terwijn, M.; Zeijlemaker, W.; Kelder, A.; Rutten, A.P.; Snel, A.N.; Scholten, W.J.; Pabst, T.; Verhoef, G.; Löwenberg, B.; Zweegman, S.; et al. Leukemic Stem Cell Frequency: A Strong Biomarker for Clinical Outcome in Acute Myeloid Leukemia. PLoS ONE 2014, 9, e107587. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Xu, L.-P.; Wang, Y.; Zhang, X.; Chen, H.; Chen, Y.-H.; Wang, F.; Han, W.; Sun, Y.; Yan, C.; et al. Superiority of Leukemic Stem Cell-Based Minimal Residual Disease Assay to Traditional Multiparameter Flow Cytometry-Based Method for Relapse Prediction in AML Patients: A Prospective Study with Randomized Training and Validation Sets. Blood 2021, 138, 517. [Google Scholar] [CrossRef]
- Heuser, M.; Freeman, S.D.; Ossenkoppele, G.J.; Buccisano, F.; Hourigan, C.S.; Ngai, L.L.; Tettero, J.M.; Bachas, C.; Baer, C.; Béné, M.-C.; et al. 2021 Update on MRD in acute myeloid leukemia: A consensus document from the European LeukemiaNet MRD Working Party. Blood 2021, 138, 2753–2767. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Ritchey, J.; Prior, J.L.; Holt, M.; Shannon, W.D.; Deych, E.; Piwnica-Worms, D.R.; DiPersio, J.F. In vivo administration of hypomethylating agents mitigate graft-versus-host disease without sacrificing graft-versus-leukemia. Blood 2010, 116, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Abarca, L.I.; Gutierrez-Cosio, S.; Santamaría, C.; Caballero-Velazquez, T.; Blanco, B.; Herrero-Sánchez, C.; Garcia, J.; Carrancio, S.; Hernández-Campo, P.; González, F.J.; et al. Immunomodulatory effect of 5-azacytidine (5-azaC): Potential role in the transplantation setting. Blood 2010, 115, 107–121. [Google Scholar] [CrossRef] [Green Version]
- Goodyear, O.C.; Dennis, M.; Jilani, N.Y.; Loke, J.; Siddique, S.; Ryan, G.; Nunnick, J.; Khanum, R.; Raghavan, M.; Cook, M.; et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood 2012, 119, 3361–3369. [Google Scholar] [CrossRef] [PubMed]
- Craddock, C.; Labopin, M.; Robin, M.; Finke, J.; Chevallier, P.; Yakoub-Agha, I.; Bourhis, J.H.; Sengelov, H.; Blaise, D.; Luft, T.; et al. Clinical activity of azacitidine in patients who relapse after allogeneic stem cell transplantation for acute myeloid leukemia. Haematologica 2016, 101, 879–883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Platzbecker, U.; Wermke, M.; Radke, J.R.; Oelschlaegel, U.; Seltmann, F.; Kiani, A.N.; Klut, I.-M.; Knoth, H.; Rollig, C.; Schetelig, J.; et al. Azacitidine for treatment of imminent relapse in MDS or AML patients after allogeneic HSCT: Results of the RELAZA trial. Leukemia 2012, 26, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Platzbecker, U.; Middeke, J.M.; Sockel, K.; Herbst, R.; Wolf, D.; Baldus, C.D.; Oelschlägel, U.; Mütherig, A.; Fransecky, L.; Noppeney, R.; et al. Measurable residual disease-guided treatment with azacitidine to prevent haematological relapse in patients with myelodysplastic syndrome and acute myeloid leukaemia (RELAZA2): An open-label, multicentre, phase 2 trial. Lancet Oncol. 2018, 19, 1668–1679. [Google Scholar] [CrossRef]
- De Lima, M.; Giralt, S.; Thall, P.F.; De Padua Silva, L.; Jones, R.B.; Komanduri, K.; Braun, T.M.; Nguyen, H.Q.; Champlin, R.; Garcia-Manero, G. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: A dose and schedule finding study. Cancer 2010, 116, 5420–5431. [Google Scholar] [CrossRef] [PubMed]
- Craddock, C.; Jilani, N.; Siddique, S.; Yap, C.; Khan, J.; Nagra, S.; Ward, J.; Ferguson, P.; Hazlewood, P.; Buka, R.; et al. Tolerability and Clinical Activity of Post-Transplantation Azacitidine in Patients Allografted for Acute Myeloid Leukemia Treated on the RICAZA Trial. Biol. Blood Marrow Transplant. 2016, 22, 385–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Cheikh, J.; Massoud, R.; Fares, E.; Kreidieh, N.; Mahfouz, R.; Charafeddine, M.; Kharfan-Dabaja, M.A.; Bazarbachi, A. Low-dose 5-azacytidine as preventive therapy for relapse of AML and MDS following allogeneic HCT. Bone Marrow Transplant. 2017, 52, 918–921. [Google Scholar] [CrossRef] [PubMed]
- Oran, B.; De Lima, M.; Garcia-Manero, G.; Thall, P.F.; Lin, R.; Popat, U.; Alousi, A.M.; Hosing, C.; Giralt, S.; Rondon, G.; et al. A phase 3 randomized study of 5-azacitidine maintenance vs observation after transplant in high-risk AML and MDS patients. Blood Adv. 2020, 4, 5580–5588. [Google Scholar] [CrossRef] [PubMed]
- Pusic, I.; Choi, J.; Fiala, M.; Gao, F.; Holt, M.; Cashen, A.F.; Vij, R.; Abboud, C.N.; Stockerl-Goldstein, K.E.; Jacoby, M.A.; et al. Maintenance Therapy with Decitabine after Allogeneic Stem Cell Transplantation for Acute Myelogenous Leukemia and Myelodysplastic Syndrome. Biol. Blood Marrow Transplant. 2015, 21, 1761–1769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, L.; Zhang, Y.; Wang, S.; Kong, P.; Su, Y.; Hu, J.; Jiang, M.; Bai, H.; Lang, T.; Wang, J.; et al. Effect of rhG-CSF Combined With Decitabine Prophylaxis on Relapse of Patients With High-Risk MRD-Negative AML After HSCT: An Open-Label, Multicenter, Randomized Controlled Trial. J. Clin. Oncol. 2020, 38, 4249–4259. [Google Scholar] [CrossRef] [PubMed]
- de Lima, M.; Oran, B.; Champlin, R.E.; Papadopoulos, E.B.; Giralt, S.A.; Scott, B.L.; William, B.M.; Hetzer, J.; Laille, E.; Hubbell, B.; et al. CC-486 Maintenance after Stem Cell Transplantation in Patients with Acute Myeloid Leukemia or Myelodysplastic Syndromes. Biol. Blood Marrow Transplant. 2018, 24, 2017–2024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bewersdorf, J.P.; Tallman, M.S.; Cho, C.; Zeidan, M.A.M.; Stahl, M. Safety and Efficacy of Maintenance Treatment Following Allogeneic Hematopoietic Cell Transplant in Acute Myeloid Leukemia and Myelodysplastic Syndrome—A Systematic Review and Meta-Analysis. Blood 2020, 136, 34–35. [Google Scholar] [CrossRef]
- Kottaridis, P.D.; Gale, R.E.; Frew, M.E.; Harrison, G.; Langabeer, S.E.; Belton, A.A.; Walker, H.; Wheatley, K.; Bowen, D.T.; Burnett, A.K.; et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: Analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 2001, 98, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Döhner, K.; Thiede, C.; Jahn, N.; Panina, E.; Gambietz, A.; Larson, R.A.; Prior, T.W.; Marcucci, G.; Jones, D.; Krauter, J.; et al. Impact of NPM1/FLT3-ITD genotypes defined by the 2017 European LeukemiaNet in patients with acute myeloid leukemia. Blood 2020, 135, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Brunet, S.; Labopin, M.; Esteve, J.; Cornelissen, J.; Socié, G.; Iori, A.P.; Verdonck, L.F.; Volin, L.; Gratwohl, A.; Sierra, J.; et al. Impact of FLT3 Internal Tandem Duplication on the Outcome of Related and Unrelated Hematopoietic Transplantation for Adult Acute Myeloid Leukemia in First Remission: A Retrospective Analysis. J. Clin. Oncol. 2012, 30, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Stone, R.M.; Mandrekar, S.J.; Sanford, B.L.; Laumann, K.; Geyer, S.; Bloomfield, C.D.; Thiede, C.; Prior, T.W.; Döhner, K.; Marcucci, G.; et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N. Engl. J. Med. 2017, 377, 454–464. [Google Scholar] [CrossRef]
- Antar, A.; Kharfan-Dabaja, M.A.; Mahfouz, R.; Bazarbachi, A. Sorafenib Maintenance Appears Safe and Improves Clinical Outcomes in FLT3-ITD Acute Myeloid Leukemia after Allogeneic Hematopoietic Cell Transplantation. Clin. Lymphoma Myeloma Leuk. 2015, 15, 298–302. [Google Scholar] [CrossRef]
- Battipaglia, G.; Ruggeri, A.; Massoud, R.; El Cheikh, J.; Jestin, M.; Antar, A.; Ahmed, S.O.; Rasheed, W.; Shaheen, M.; Belhocine, R.; et al. Efficacy and feasibility of sorafenib as a maintenance agent after allogeneic hematopoietic stem cell transplantation for Fms-like tyrosine kinase 3-mutated acute myeloid leukemia. Cancer 2017, 123, 2867–2874. [Google Scholar] [CrossRef]
- Bazarbachi, A.; Labopin, M.; Battipaglia, G.; Djabali, A.; Passweg, J.R.; Socié, G.; Forcade, E.; Blaise, D.; Chevallier, P.; Orvain, C.; et al. Sorafenib improves survival of FLT3-mutated acute myeloid leukemia in relapse after allogeneic stem cell transplantation: A report of the EBMT Acute Leukemia Working Party. Haematologica 2019, 104, e398–e401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Battipaglia, G.; Massoud, R.; Ahmed, S.O.; Legrand, O.; El Cheikh, J.; Youniss, R.; Aljurf, M.; Mohty, M.; Bazarbachi, A. Efficacy and Feasibility of Sorafenib as a Maintenance Agent After Allogeneic Hematopoietic Stem Cell Transplantation for Fms-like Tyrosine Kinase 3 Mutated Acute Myeloid Leukemia: An Update. Clin. Lymphoma Myeloma Leuk. 2019, 19, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Mathew, N.R.; Baumgartner, F.; Braun, L.; O’Sullivan, D.; Thomas, S.; Waterhouse, M.; Müller, T.; Hanke, K.; Taromi, S.; Apostolova, P.; et al. Sorafenib promotes graft-versus-leukemia activity in mice and humans through IL-15 production in FLT3-ITD-mutant leukemia cells. Nat. Med. 2018, 24, 282–291. [Google Scholar] [CrossRef] [PubMed]
- Metzelder, S.K.; Schroeder, T.; Finck, A.; Scholl, S.; Fey, M.F.; Gotze, K.; Linn, Y.C.; Kröger, M.; Reiter, A.; Salih, H.R.; et al. High activity of sorafenib in FLT3-ITD-positive acute myeloid leukemia synergizes with allo-immune effects to induce sustained responses. Leukemia 2012, 26, 2353–2359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.-B.; Li, S.; Lane, A.A.; Connolly, C.; Del Rio, C.; Valles, B.; Curtis, M.; Ballen, K.; Cutler, C.; Dey, B.R.; et al. Phase I Trial of Maintenance Sorafenib after Allogeneic Hematopoietic Stem Cell Transplantation for Fms-like Tyrosine Kinase 3 Internal Tandem Duplication Acute Myeloid Leukemia. Biol. Blood Marrow Transplant. 2014, 20, 2042–2048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunner, A.M.; Li, S.; Fathi, A.T.; Wadleigh, M.; Ho, V.T.; Collier, K.; Connolly, C.; Ballen, K.K.; Cutler, C.S.; Dey, B.R.; et al. Haematopoietic cell transplantation with and without sorafenib maintenance for patients withFLT3-ITD acute myeloid leukaemia in first complete remission. Br. J. Haematol. 2016, 175, 496–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bazarbachi, A.; Labopin, M.; Battipaglia, G.; Djabali, A.; Forcade, E.; Arcese, W.; Socié, G.; Blaise, D.; Halter, J.; Gerull, S.; et al. Allogeneic Stem Cell Transplantation for FLT3-Mutated Acute Myeloid Leukemia: In vivo T-Cell Depletion and Posttransplant Sorafenib Maintenance Improve Survival. A Retrospective Acute Leukemia Working Party-European Society for Blood and Marrow Transplant Study. Clin. Hematol. Int. 2019, 1, 58–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burchert, A.; Bug, G.; Fritz, L.V.; Finke, J.; Stelljes, M.; Röllig, C.; Wollmer, E.; Wäsch, R.; Bornhäuser, M.; Berg, T.; et al. Sorafenib Maintenance After Allogeneic Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia With FLT3–Internal Tandem Duplication Mutation (SORMAIN). J. Clin. Oncol. 2020, 38, 2993–3002. [Google Scholar] [CrossRef]
- Xuan, L.; Wang, Y.; Huang, F.; Fan, Z.; Xu, Y.; Sun, J.; Xu, N.; Deng, L.; Li, X.; Liang, X.; et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: An open-label, multicentre, randomised phase 3 trial. Lancet Oncol. 2020, 21, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Bazarbachi, A.; Bug, G.; Baron, F.; Brissot, E.; Ciceri, F.; Dalle, I.A.; Döhner, H.; Esteve, J.; Floisand, Y.; Giebel, S.; et al. Clinical practice recommendation on hematopoietic stem cell transplantation for acute myeloid leukemia patients with FLT3-internal tandem duplication: A position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica 2020, 105, 1507–1516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antar, A.I.; Otrock, Z.K.; Jabbour, E.; Mohty, M.; Bazarbachi, A. FLT3 inhibitors in acute myeloid leukemia: Ten frequently asked questions. Leukemia 2020, 34, 682–696. [Google Scholar] [CrossRef] [PubMed]
- Schlenk, R.F.; Weber, D.; Fiedler, W.; Salih, H.R.; Wulf, G.; Salwender, H.; Schroeder, T.; Kindler, T.; Lübbert, M.; Wolf, D.; et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood 2019, 133, 840–851. [Google Scholar] [CrossRef] [PubMed]
- Maziarz, R.T.; Levis, M.; Patnaik, M.M.; Scott, B.L.; Mohan, S.R.; Deol, A.; Rowley, S.D.; Kim, D.D.H.; Hernandez, D.; Rajkhowa, T.; et al. Midostaurin after allogeneic stem cell transplant in patients with FLT3-internal tandem duplication-positive acute myeloid leukemia. Bone Marrow Transplant. 2021, 56, 1180–1189. [Google Scholar] [CrossRef]
- Sandmaier, B.M.; Khaled, S.; Oran, B.; Gammon, G.; Trone, D.; Frankfurt, O. Results of a phase 1 study of quizartinib as maintenance therapy in subjects with acute myeloid leukemia in remission following allogeneic hematopoietic stem cell transplant. Am. J. Hematol. 2018, 93, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Perl, A.E.; Martinelli, G.; Cortes, J.E.; Neubauer, A.; Berman, E.; Paolini, S.; Montesinos, P.; Baer, M.R.; Larson, R.A.; Ustun, C.; et al. Gilteritinib or Chemotherapy for Relapsed or Refractory FLT3-Mutated AML. N. Engl. J. Med. 2019, 381, 1728–1740. [Google Scholar] [CrossRef] [PubMed]
- Levis, M.J.; Hamadani, M.; Logan, B.R.; Rosales, M.; Delgado, D.; Bahceci, E.; Devine, S.; Horowitz, M.M.; Chen, Y.-B. BMT CTN Protocol 1506: A Phase 3 Trial of Gilteritinib as Maintenance Therapy after Allogeneic Hematopoietic Stem Cell Transplantation in Patients with FLT3-ITD+ AML. Blood 2019, 134, 4602. [Google Scholar] [CrossRef]
- Levis, M.J.; Chen, Y.-B.; Hamadani, M.; Horowitz, M.M.; Jones, R.J.; Blood and Marrow Transplant Clinical Trials Network. FLT3 Inhibitor Maintenance After Allogeneic Transplantation: Is a Placebo-Controlled, Randomized Trial Ethical? J. Clin. Oncol. 2019, 37, 1604–1607. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.M.; Dinardo, C.D.; Pollyea, D.A.; Fathi, A.T.; Roboz, G.J.; Altman, J.K.; Stone, R.M.; DeAngelo, D.J.; Levine, R.L.; Flinn, I.W.; et al. Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 2017, 130, 722–731. [Google Scholar] [CrossRef] [PubMed]
- Dinardo, C.D.; Stein, E.M.; DE Botton, S.; Roboz, G.J.; Altman, J.K.; Mims, A.S.; Swords, R.; Collins, R.H.; Mannis, G.N.; Pollyea, D.A.; et al. Durable Remissions with Ivosidenib inIDH1-Mutated Relapsed or Refractory AML. N. Engl. J. Med. 2018, 378, 2386–2398. [Google Scholar] [CrossRef] [PubMed]
- Dinardo, C.D.; Jonas, B.A.; Pullarkat, V.; Thirman, M.J.; Garcia, J.S.; Wei, A.H.; Konopleva, M.; Döhner, H.; Letai, A.; Fenaux, P.; et al. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N. Engl. J. Med. 2020, 383, 617–629. [Google Scholar] [CrossRef]
- Wei, A.H.; Montesinos, P.; Ivanov, V.; Dinardo, C.D.; Novak, J.; Laribi, K.; Kim, I.; Stevens, D.A.; Fiedler, W.; Pagoni, M.; et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: A phase 3 randomized placebo-controlled trial. Blood 2020, 135, 2137–2145. [Google Scholar] [CrossRef] [PubMed]
- Kent, A.; Pollyea, D.A.; Winters, A.; Jordan, C.T.; Smith, C.; Gutman, J.A. Venetoclax Is Safe and Tolerable As Post-Transplant Maintenance Therapy for AML Patients at High Risk for Relapse. Blood 2020, 136, 11–12. [Google Scholar] [CrossRef]
- Schmid, C.; Labopin, M.; Schaap, N.; Veelken, H.; Schleuning, M.; Stadler, M.; Finke, J.; Hurst, E.; Baron, F.; Ringden, O.; et al. Prophylactic donor lymphocyte infusion after allogeneic stem cell transplantation in acute leukaemia—A matched pair analysis by the Acute Leukaemia Working Party of EBMT. Br. J. Haematol. 2019, 184, 782–787. [Google Scholar] [CrossRef]
- Tsirigotis, P.; Gkirkas, K.; Kitsiou, V.; Chondropoulos, S.; Athanassiades, T.; Thomopoulos, T.; Tsirogianni, A.; Stamouli, M.; Karagiannidi, A.; Siafakas, N.; et al. Repetitively Administered Low-Dose Donor Lymphocyte Infusion for Prevention of Relapse after Allogeneic Stem Cell Transplantation in Patients with High-Risk Acute Leukemia. Cancers 2021, 13, 2699. [Google Scholar] [CrossRef] [PubMed]
- El-Cheikh, J.; Crocchiolo, R.; Furst, S.; Ladaique, P.; Castagna, L.; Faucher, C.; Calmels, B.; Oudin, C.; Lemarie, C.; Granata, A.; et al. Donor CD3+ lymphocyte infusion after reduced intensity conditioning allogeneic stem cell transplantation: Single-center experience. Exp. Hematol. 2013, 41, 17–27. [Google Scholar] [CrossRef] [PubMed]
- De Vos, J.; Baudoux, E.; Bay, J.-O.; Calmels, B.; Cras, A.; El Cheikh, J.; Guerout-Verite, M.-A.; Lacassagne, M.-N.; Lamure, S.; Letellier, C.; et al. Donor Lymphocyte Infusions (DLI): Guidelines from the Francophone Society of Bone Marrow Transplantation and Cellular Therapy (SFGM-TC). Bull Cancer 2019, 106, S35–S39. [Google Scholar] [CrossRef] [PubMed]
- Sterling, C.; Webster, J. Harnessing the immune system after allogeneic stem cell transplant in acute myeloid leukemia. Am. J. Hematol. 2020, 95, 529–547. [Google Scholar] [CrossRef] [PubMed]
- Haubner, S.; Perna, F.; Köhnke, T.; Schmidt, C.; Berman, S.; Augsberger, C.; Schnorfeil, F.M.; Krupka, C.; Lichtenegger, F.S.; Liu, X.; et al. Coexpression profile of leukemic stem cell markers for combinatorial targeted therapy in AML. Leukemia 2019, 33, 64–74. [Google Scholar] [CrossRef] [PubMed]
| Treatment | Study Phase | Timing of Intervention | Study Status | Clinical Trial Identifier |
|---|---|---|---|---|
| FLT3 Target | ||||
| Gilteritinib | Phase 3 | Prophylaxis | Active, not recruiting | NCT02997202 |
| Crenolanib | Phase 2 | Prophylaxis | Active, not recruiting | NCT02400255 |
| IDH2 Target | ||||
| Enasidenib | Phase I Phase I | Prophylaxis | Recruiting Active, not recruiting | NCT03728335 NCT03515512 |
| TP53 Target | ||||
| APR−246 + azacitidine | Phase 2 | Prophylaxis | Active, not recruiting | NCT03931291 |
| CD 33 Target | ||||
| Gemtuzumab ozogamicin | Phase 1/2 | Prophylaxis | Recruiting | NCT04849910 |
| No Target Identified | ||||
| Azacitidine + venetoclax | Phase 3 VIALE-T | Prophylaxis | Recruiting | NCT04161885 |
| Phase 2 | Prophylaxis | Recruiting | NCT04128501 | |
| Phase 2 | Pre-emptive | Recruiting | NCT04809181 | |
| Azacitidine + Pevonedistat | Phase 2 | Pre-emptive | Recruiting | NCT04712942 |
| Azacitidine + Valproic acid | Phase 2 | Prophylaxis | Recruiting | NCT02124174 |
| SGI−110 + DLI | Phase 2 | Prophylaxis | Not yet recruiting | NCT03454984 |
| Low dose 5-azacitidine | Phase 2 | Prophylaxis | Recruiting | NCT01995578 |
| Oral Azacitidine (CC−486) | Phase 3 | Prophylaxis | Recruiting | NCT04173533 |
| Sabatolimab ± Azacitidine | Phase Ib/II | Pre-emptive | Recruiting | NCT04623216 |
| Glasdegib | Phase 3 | Prophylaxis | Recruiting | NCT04168502 |
| N−803 IL−15 super-agonist complex | Phase 2 | Prophylaxis | Recruiting | NCT02989844 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abou Dalle, I.; El Cheikh, J.; Bazarbachi, A. Pharmacologic Strategies for Post-Transplant Maintenance in Acute Myeloid Leukemia: It Is Time to Consider! Cancers 2022, 14, 1490. https://doi.org/10.3390/cancers14061490
Abou Dalle I, El Cheikh J, Bazarbachi A. Pharmacologic Strategies for Post-Transplant Maintenance in Acute Myeloid Leukemia: It Is Time to Consider! Cancers. 2022; 14(6):1490. https://doi.org/10.3390/cancers14061490
Chicago/Turabian StyleAbou Dalle, Iman, Jean El Cheikh, and Ali Bazarbachi. 2022. "Pharmacologic Strategies for Post-Transplant Maintenance in Acute Myeloid Leukemia: It Is Time to Consider!" Cancers 14, no. 6: 1490. https://doi.org/10.3390/cancers14061490
APA StyleAbou Dalle, I., El Cheikh, J., & Bazarbachi, A. (2022). Pharmacologic Strategies for Post-Transplant Maintenance in Acute Myeloid Leukemia: It Is Time to Consider! Cancers, 14(6), 1490. https://doi.org/10.3390/cancers14061490






