Predicting Complications following Surgical Resection of Hepatocellular Carcinoma Using Newly Developed Neo-Glasgow Prognostic Score with ALBI Grade: Comparison of Open and Laparoscopic Surgery Cases
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Underlying Liver Disease
2.2. Liver Function and Nutritional Status Assessments
2.3. Clinicopathologic Variables, HCC Treatment Algorithm, and Surgical Procedures
2.4. Evaluation of Complications following Surgical Resection
2.5. Statistical Analysis
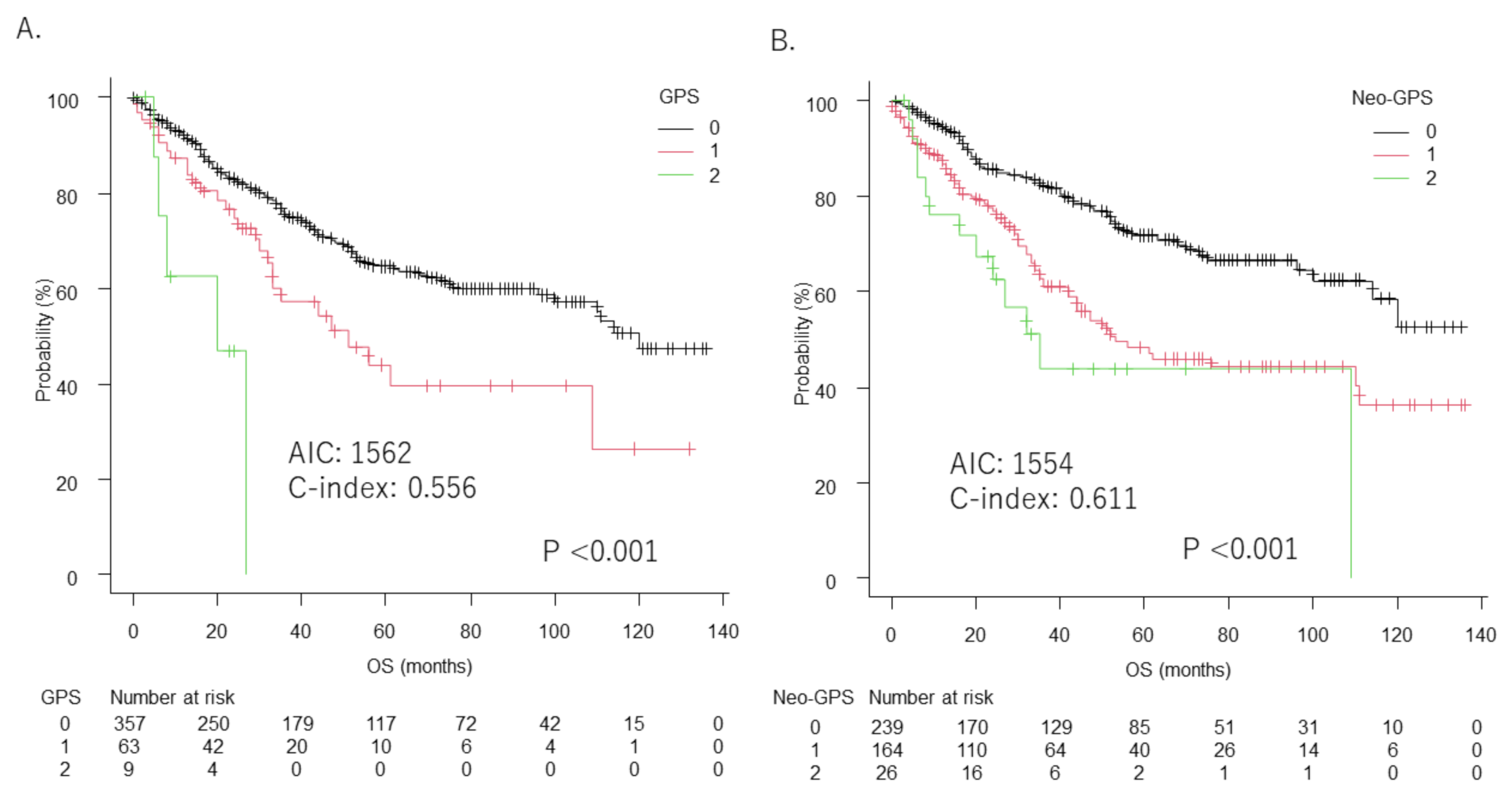
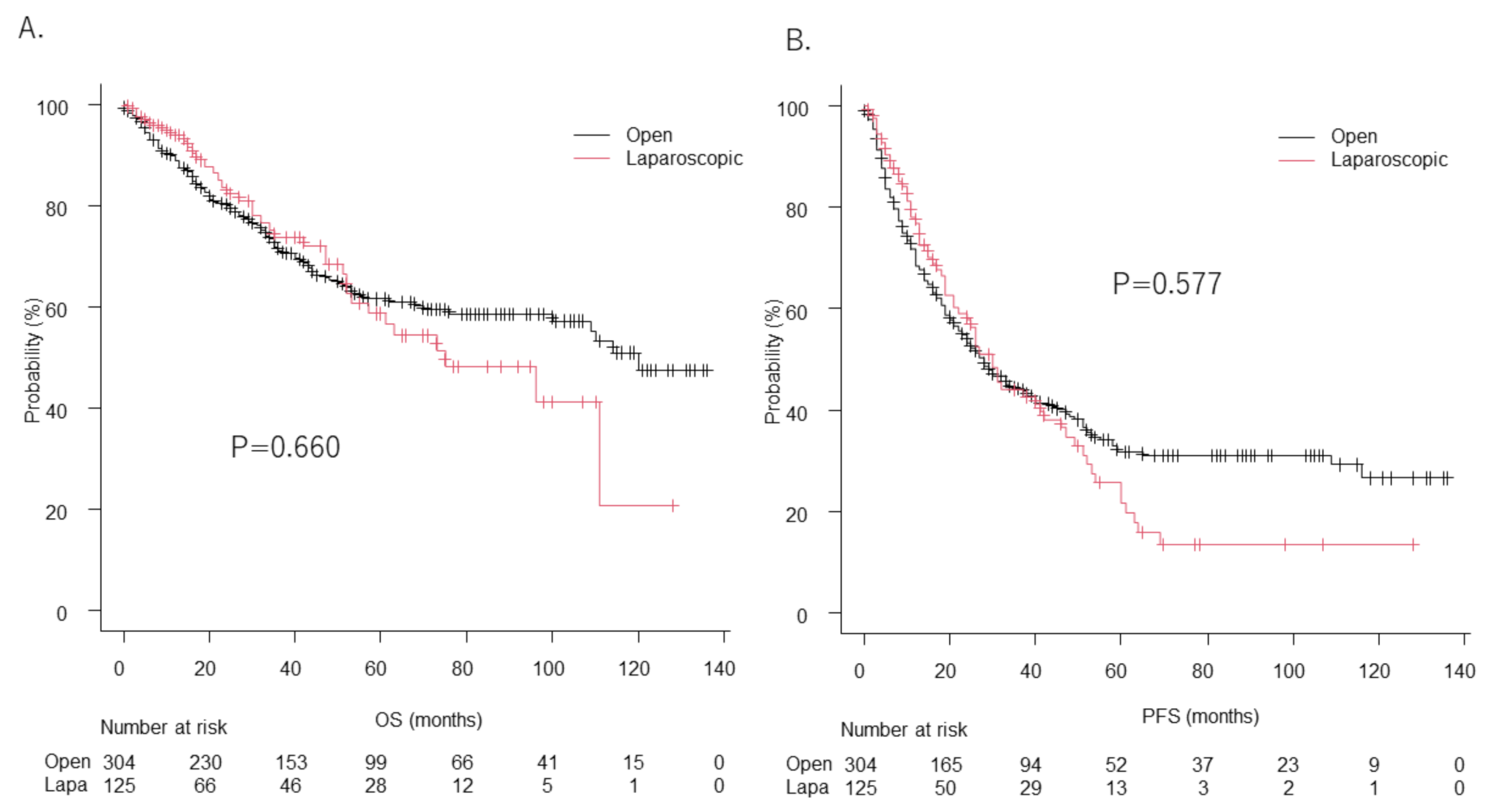
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parkin, D.M.; Bray, F.; Ferlay, J.; Pisani, P. Estimating the world cancer burden: Globocan 2000. Int. J. Cancer 2001, 94, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Han, H.S.; Shehta, A.; Ahn, S.; Yoon, Y.S.; Cho, J.Y.; Choi, Y. Laparoscopic versus open liver resection for hepatocellular carcinoma: Case-matched study with propensity score matching. J. Hepatol. 2015, 63, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Ban, D.; Tanabe, M.; Kumamaru, H.; Nitta, H.; Otsuka, Y.; Miyata, H.; Kakeji, Y.; Kitagawa, Y.; Kaneko, H.; Wakabayashi, G.; et al. Safe Dissemination of Laparoscopic Liver Resection in 27,146 Cases Between 2011 and 2017 from the National Clinical Database of Japan. Ann. Surg. 2021, 274, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Forrest, L.M.; McMillan, D.C.; McArdle, C.S.; Angerson, W.J.; Dunlop, D.J. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br. J. Cancer 2003, 89, 1028–1030. [Google Scholar] [CrossRef] [Green Version]
- Elahi, M.M.; McMillan, D.C.; McArdle, C.S.; Angerson, W.J.; Sattar, N. Score based on hypoalbuminemia and elevated C-reactive protein predicts survival in patients with advanced gastrointestinal cancer. Nutr. Cancer 2004, 48, 171–173. [Google Scholar] [CrossRef]
- Crumley, A.B.; McMillan, D.C.; McKernan, M.; McDonald, A.C.; Stuart, R.C. Evaluation of an inflammation-based prognostic score in patients with inoperable gastro-oesophageal cancer. Br. J. Cancer 2006, 94, 637–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinoshita, A.; Onoda, H.; Imai, N.; Iwaku, A.; Oishi, M.; Fushiya, N.; Koike, K.; Nishino, H.; Tajiri, H. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br. J. Cancer 2012, 107, 988–993. [Google Scholar] [CrossRef]
- Shimoda, Y.; Fujikawa, H.; Komori, K.; Watanabe, H.; Kano, K.; Yamada, T.; Shiozawa, M.; Morinaga, S.; Katsumata, K.; Tsuchida, A.; et al. Preoperative Utility of the Glasgow Prognostic Score on Outcomes of Patients with Locally Advanced Gastric Cancer. J. Gastrointest Cancer 2021. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kato, M.; Marui, K.; Murakami, T.; Onishi, K.; Adachi, T.; Matsuoka, J.; Ueki, H.; Yoshino, T.; Tsuruta, M.; et al. Easy clinical predictor for low BCAA to tyrosine ratio in chronic liver disease patients with hepatocellular carcinoma: Usefulness of ALBI score as nutritional prognostic marker. Cancer Med. 2021, 10, 3584–3592. [Google Scholar] [CrossRef]
- European Association For The Study Of The Liver. EASL clinical practical guidelines: Management of alcoholic liver disease. J. Hepatol. 2012, 57, 399–420. [Google Scholar] [CrossRef]
- Mittal, S.; El-Serag, H.B. Epidemiology of hepatocellular carcinoma: Consider the population. J. Clin. Gastroenterol. 2013, 47, S2–S6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pugh, R.N.; Murray-Lyon, I.M.; Dawson, J.L.; Pietroni, M.C.; Williams, R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 1973, 60, 646–649. [Google Scholar] [CrossRef] [PubMed]
- Johnson, P.J.; Berhane, S.; Kagebayashi, C.; Satomura, S.; Teng, M.; Reeves, H.L.; O’Beirne, J.; Fox, R.; Skowronska, A.; Palmer, D.; et al. Assessment of liver function in patients with hepatocellular carcinoma: A new evidence-based approach-the ALBI grade. J. Clin. Oncol. 2015, 33, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, A.; Kumada, T.; Michitaka, K.; Toyoda, H.; Tada, T.; Ueki, H.; Kaneto, M.; Aibiki, T.; Okudaira, T.; Kawakami, T.; et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2016, 31, 1031–1036. [Google Scholar] [CrossRef]
- Kokudo, N.; Takemura, N.; Hasegawa, K.; Takayama, T.; Kubo, S.; Shimada, M.; Nagano, H.; Hatano, E.; Izumi, N.; Kaneko, S.; et al. Clinical practice guidelines for hepatocellular carcinoma: The Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatol. Res. 2019, 49, 1109–1113. [Google Scholar] [CrossRef]
- Strasberg, S.M.; Belghiti, J.; Clavien, P.A.; Gadzijev, E.; Garden, J.O.; Lau, W.Y.; Makuuchi, M.; Strong, R.W. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000, 2, 333–339. [Google Scholar] [CrossRef]
- Couinaud, C. Le Foie: Études Anatomiques et Chirurgicales; Masson: Paris, France, 1957. [Google Scholar]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Akaike, H. Information theory as an extension of the maximum likelihood principle. In Proceedings of the 2nd International Symposium on Information Theory, Budapest, Hungary, 2–8 September 1971; Petrov, B.N., Caski, F., Eds.; Springer: New York, NY, USA; Akadimiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Shafaee, Z.; Kazaryan, A.M.; Marvin, M.R.; Cannon, R.; Buell, J.F.; Edwin, B.; Gayet, B. Is laparoscopic repeat hepatectomy feasible? A tri-institutional analysis. J. Am. Coll. Surg. 2011, 212, 171–179. [Google Scholar] [CrossRef]
- Shelat, V.G.; Serin, K.; Samim, M.; Besselink, M.G.; Al Saati, H.; Gioia, P.D.; Pearce, N.W.; Abu Hilal, M. Outcomes of repeat laparoscopic liver resection compared to the primary resection. World J. Surg. 2014, 38, 3175–3180. [Google Scholar] [CrossRef]
- Goh, B.K.P.; Teo, J.Y.; Chan, C.Y.; Lee, S.Y.; Cheow, P.C.; Chung, A.Y.F. Laparoscopic repeat liver resection for recurrent hepatocellular carcinoma. ANZ J. Surg. 2017, 87, E143–E146. [Google Scholar] [CrossRef] [PubMed]
- Ome, Y.; Hashida, K.; Yokota, M.; Nagahisa, Y.; Yamaguchi, K.; Okabe, M.; Kawamoto, K. The feasibility and efficacy of pure laparoscopic repeat hepatectomy. Surg. Endosc. 2018, 32, 3474–3479. [Google Scholar] [CrossRef] [PubMed]
- Noda, T.; Eguchi, H.; Wada, H.; Iwagami, Y.; Yamada, D.; Asaoka, T.; Gotoh, K.; Kawamoto, K.; Takeda, Y.; Tanemura, M.; et al. Short-term surgical outcomes of minimally invasive repeat hepatectomy for recurrent liver cancer. Surg. Endosc. 2018, 32, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Okamura, Y.; Yamamoto, Y.; Sugiura, T.; Ito, T.; Ashida, R.; Ohgi, K.; Uesaka, K. Novel patient risk factors and validation of a difficulty scoring system in laparoscopic repeat hepatectomy. Sci. Rep. 2019, 9, 17653. [Google Scholar] [CrossRef]
- Onoe, T.; Yamaguchi, M.; Irei, T.; Ishiyama, K.; Sudo, T.; Hadano, N.; Kojima, M.; Kubota, H.; Ide, R.; Tazawa, H.; et al. Feasibility and efficacy of repeat laparoscopic liver resection for recurrent hepatocellular carcinoma. Surg. Endosc. 2020, 34, 4574–4581. [Google Scholar] [CrossRef]
- van der Poel, M.J.; Barkhatov, L.; Fuks, D.; Berardi, G.; Cipriani, F.; Aljaiuossi, A.; Lainas, P.; Dagher, I.; D’Hondt, M.; Rotellar, F.; et al. Multicentre propensity score-matched study of laparoscopic versus open repeat liver resection for colorectal liver metastases. Br. J. Surg. 2019, 106, 783–789. [Google Scholar] [CrossRef]
- Morise, Z.; Aldrighetti, L.; Belli, G.; Ratti, F.; Belli, A.; Cherqui, D.; Tanabe, M.; Wakabayashi, G. Laparoscopic repeat liver resection for hepatocellular carcinoma: A multicentre propensity score-based study. Br. J. Surg. 2020, 107, 889–895. [Google Scholar] [CrossRef]
- Morise, Z. Status and perspective of laparoscopic repeat liver resection. World J. Hepatol. 2018, 10, 479–484. [Google Scholar] [CrossRef]
- Morise, Z. Laparoscopic repeat liver resection. Ann. Gastroenterol. Surg. 2020, 4, 485–489. [Google Scholar] [CrossRef]
- Kanazawa, A.; Tsukamoto, T.; Shimizu, S.; Kodai, S.; Yamamoto, S.; Yamazoe, S.; Ohira, G.; Nakajima, T. Laparoscopic liver resection for treating recurrent hepatocellular carcinoma. J. Hepato-Biliary-Pancreat. Sci. 2013, 20, 512–517. [Google Scholar] [CrossRef]
- Peng, L.; Zhou, Z.; Xiao, W.; Hu, X.; Cao, J.; Mao, S. Systematic review and meta-analysis of laparoscopic versus open repeat hepatectomy for recurrent liver cancer. Surg. Oncol. 2019, 28, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.W.; Liu, F.; Li, H.Y.; Wei, Y.G.; Li, B. Outcomes following laparoscopic versus open major hepatectomy for hepatocellular carcinoma in patients with cirrhosis: A propensity score-matched analysis. Surg. Endosc. 2018, 32, 712–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuks, D.; Cauchy, F.; Ftériche, S.; Nomi, T.; Schwarz, L.; Dokmak, S.; Scatton, O.; Fusco, G.; Belghiti, J.; Gayet, B.; et al. Laparoscopy Decreases Pulmonary Complications in Patients Undergoing Major Liver Resection: A Propensity Score Analysis. Ann. Surg. 2016, 263, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Witowski, J.; Rubinkiewicz, M.; Mizera, M.; Wysocki, M.; Gajewska, N.; Sitkowski, M.; Małczak, P.; Major, P.; Budzyński, A.; Pędziwiatr, M. Meta-analysis of short- and long-term outcomes after pure laparoscopic versus open liver surgery in hepatocellular carcinoma patients. Surg. Endosc. 2019, 33, 1491–1507. [Google Scholar] [CrossRef] [Green Version]
- Hiraoka, A.; Michitaka, K.; Kumada, T.; Izumi, N.; Kadoya, M.; Kokudo, N.; Kubo, S.; Matsuyama, Y.; Nakashima, O.; Sakamoto, M.; et al. Validation and Potential of Albumin-Bilirubin Grade and Prognostication in a Nationwide Survey of 46,681 Hepatocellular Carcinoma Patients in Japan: The Need for a More Detailed Evaluation of Hepatic Function. Liver Cancer 2017, 6, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Broggi, M.S.; Patil, D.; Baum, Y.; Nieh, P.T.; Alemozaffar, M.; Pattaras, J.G.; Ogan, K.; Master, V.A. Onodera’s Prognostic Nutritional Index as an Independent Prognostic Factor in Clear Cell Renal Cell Carcinoma. Urology 2016, 96, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Yoshiji, H.; Nagoshi, S.; Akahane, T.; Asaoka, Y.; Ueno, Y.; Ogawa, K.; Kawaguchi, T.; Kurosaki, M.; Sakaida, I.; Shimizu, M.; et al. Evidence-based clinical practice guidelines for liver cirrhosis 2020. Hepatol. Res. 2021, 51, 725–749. [Google Scholar] [CrossRef]
- Yoshiji, H.; Nagoshi, S.; Akahane, T.; Asaoka, Y.; Ueno, Y.; Ogawa, K.; Kawaguchi, T.; Kurosaki, M.; Sakaida, I.; Shimizu, M.; et al. Evidence-based clinical practice guidelines for Liver Cirrhosis 2020. J. Gastroenterol. 2021, 56, 593–619. [Google Scholar] [CrossRef]

| Age, years * | 73 (66–78) |
| Gender, male:female | 326:103 |
| Body mass index, kg/m2 * | 23.2 (20.9–25.8) |
| Etiology, HCV:HBV:HBV&HCV:alcohol:others | 154:74:5:53:143 |
| Positive for diabetes mellitus, n (%) | 141 (32.9) |
| Aspartate transaminase, U/L * | 34 (25–49) |
| Alanine aminotransferase, U/L * | 28 (18–46) |
| Platelets, 104/µL * | 15.7 (11.9–20.7) |
| Total bilirubin, mg/dL * | 0.7 (0.6–1.0) |
| Albumin, g/dL * | 4.0 (3.7–4.3) |
| Prothrombin time, % * | 87.9 (81.5–97.0) |
| Child–Pugh score, 5:6 | 326:103 |
| Creatinine, mg/dL * | 0.79 (0.67–0.94) |
| CRP, mg/dL * | 0.09 (0.04–0.25) |
| CRP ≤ 1.0 mg/dL, n (%) * | 37 (8.6) |
| ALBI score * | −2.68 (−2.39 to −2.94) |
| mALBI grade, 1:2a:2b | 249:115:65 |
| ICG-R15 (%) * | 14.4 (9.3–20.9) |
| Positive for esophageal varices, n (%) | 56 (13.1%) |
| FIB-4 index * | 3.06 (2.06–4.24) |
| AFP, ng/mL * | 9.4 (3.9–56.9) |
| Single tumor, n (%) | 340 (79.2) |
| Maximum tumor size, cm * | 3.5 (2.4–5.5) |
| Open:laparoscopic | 304:125 |
| Hepatectomy, non-anatomic:segmentectomy:sectionectomy:hemitectomy | 141:61:130:97 |
| Microvascular invasion present, n (%) | 297 (69.2) |
| Operation time, minutes * | 323 (256–409) |
| Blood loss, mL * | 858 (257–1121) |
| Observation period, months * | 35 (15–68) |
| GPS, 0:1:2 | 357:63:9 |
| Neo-GPS, 0:1:2 | 239:164:26 |
| Clavien–Dindo classification ≥ 3, n (%) | 83 (19.3) |
| Cause of death, (liver failure:HCC:resection complication:other:unknown) | 15:85:8:27:9 |
| Open Hepatectomy (n = 304) | Laparoscopic Hepatectomy (n = 125) | p-Value | |
|---|---|---|---|
| Age, years * | 73 (67–78) | 73 (65–80) | 0.772 |
| Gender, male:female | 238:66 | 88:37 | 0.105 |
| Body mass index, kg/m2 * | 23.1 (20.8–25.5) | 23.5 (20.926.0) | 0.261 |
| Etiology, HCV:HBV:HBV&HCV:alcohol:others | 106:54:5:33:106 | 48:20:0:20:37 | 0.399 |
| Positive for diabetes mellitus, n (%) | 103 (33.9) | 38 (30.4) | 0.500 |
| Aspartate transaminase, U/L * | 35 (25–50) | 31 (25–46) | 0.356 |
| Alanine aminotransferase, U/L * | 29 (18–46) | 24 (19–41) | 0.260 |
| Platelets, 104/µL * | 16.3 (12.4–21.2) | 14.7 (11.018.6) | 0.006 |
| Total bilirubin, mg/dL * | 0.7 (0.6–1.0) | 0.8 (0.7–1.0) | 0.007 |
| Albumin, g/dL * | 4.0 (3.7–4.3) | 4.1 (3.7–4.4) | 0.266 |
| Prothrombin time (%) * | 88.5 (81.8–88.1) | 87.0 (78.9–93.9) | 0.016 |
| Child–Pugh score, 5:6 | 237:67 | 89:36 | 0.138 |
| Creatinine, mg/dL * | 0.79 (0.67–0.94) | 0.80 (0.68–0.94) | 0.549 |
| CRP, mg/dL * | 0.11 (0.04–0.31) | 0.07 (0.04–0.15) | 0.004 |
| CRP ≤1.0 mg/dL, n (%) * | 34 (11.2) | 3 (2.4) | 0.002 |
| ALBI score * | −2.65 (−2.41 to −2.91) | −2.70 (−2.36 to −2.99) | 0.590 |
| mALBI grade, 1:2a:2b | 177:84:43 | 72:31:22 | 0.613 |
| ICG-R15 (%) * | 13.8 (9.1–19.2) | 16.4 (10.7–25.8) | 0.002 |
| Positive for esophageal varices, n (%) | 35 (11.5) | 21 (16.8) | 0.113 |
| FIB-4 index * | 3.04 (2.01–4.14) | 3.09 (2.29–4.62) | 0.221 |
| AFP, ng/mL * | 9.5 (3.9–69.6) | 9.4 (3.9–45.0) | 0.773 |
| Single tumor, n (%) | 227 (74.7) | 113 (90.4) | <0.001 |
| Maximum tumor size, cm * | 4.0 (2.5–6.6) | 2.7 (2.0–3.5) | <0.001 |
| Hepatectomy, non-anatomic:segmentectomy:sectionectomy:hemitectomy | 87:33:103:81 | 54:28:27:16 | <0.001 |
| Microvascular invasion present, n (%) | 218 (71.7) | 79 (63.2) | 0.086 |
| Operation time, minutes * | 333 (262–407) | 298 (239–416) | 0.253 |
| Blood loss, mL * | 750 (458–1337) | 167 (70.0–341) | <0.001 |
| Observation period, months * | 40 (20–71) | 24 (9–53) | <0.001 |
| GPS, 0:1 or more | 251:53 | 106:19 | 0.670 |
| Neo-GPS, 0:1 or more | 168:136 | 71:54 | 0.831 |
| Clavien–Dindo classification ≥ 3, n (%) | 69 (22.7) | 14 (11.2) | 0.007 |
| Cause of death, liver failure:HCC:resection complication:other:unknown | 9:66:7:20:6 | 6:19:1:7:3 | 0.570 |
| Clavien–Dindo Classification ≤ 2 (n = 346) | Clavien–Dindo Classification ≥ 3 (n = 83) | p-Value | |
|---|---|---|---|
| GPS 0 | 301 (87.0%) | 56 (67.5%) | |
| GPS ≥ 1 | 45 (13.0%) | 27 (32.5%) | <0.001 |
| Neo-GPS 0 | 210 (60.8%) | 29 (34.9%) | |
| Neo-GPS ≥ 1 | 136 (39.2%) | 54 (65.1%) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaibori, M.; Hiraoka, A.; Matsui, K.; Matsushima, H.; Kosaka, H.; Yamamoto, H.; Yamaguchi, T.; Yoshida, K.; Sekimoto, M. Predicting Complications following Surgical Resection of Hepatocellular Carcinoma Using Newly Developed Neo-Glasgow Prognostic Score with ALBI Grade: Comparison of Open and Laparoscopic Surgery Cases. Cancers 2022, 14, 1402. https://doi.org/10.3390/cancers14061402
Kaibori M, Hiraoka A, Matsui K, Matsushima H, Kosaka H, Yamamoto H, Yamaguchi T, Yoshida K, Sekimoto M. Predicting Complications following Surgical Resection of Hepatocellular Carcinoma Using Newly Developed Neo-Glasgow Prognostic Score with ALBI Grade: Comparison of Open and Laparoscopic Surgery Cases. Cancers. 2022; 14(6):1402. https://doi.org/10.3390/cancers14061402
Chicago/Turabian StyleKaibori, Masaki, Atsushi Hiraoka, Kosuke Matsui, Hideyuki Matsushima, Hisashi Kosaka, Hidekazu Yamamoto, Takashi Yamaguchi, Katsunori Yoshida, and Mitsugu Sekimoto. 2022. "Predicting Complications following Surgical Resection of Hepatocellular Carcinoma Using Newly Developed Neo-Glasgow Prognostic Score with ALBI Grade: Comparison of Open and Laparoscopic Surgery Cases" Cancers 14, no. 6: 1402. https://doi.org/10.3390/cancers14061402
APA StyleKaibori, M., Hiraoka, A., Matsui, K., Matsushima, H., Kosaka, H., Yamamoto, H., Yamaguchi, T., Yoshida, K., & Sekimoto, M. (2022). Predicting Complications following Surgical Resection of Hepatocellular Carcinoma Using Newly Developed Neo-Glasgow Prognostic Score with ALBI Grade: Comparison of Open and Laparoscopic Surgery Cases. Cancers, 14(6), 1402. https://doi.org/10.3390/cancers14061402







