Targetable Pathways in the Treatment of Retroperitoneal Liposarcoma
Abstract
:Simple Summary
Abstract
1. Introduction
2. Current Therapies in RPLPS
2.1. Chemotherapy Strategies
2.2. Radiotherapy Strategies
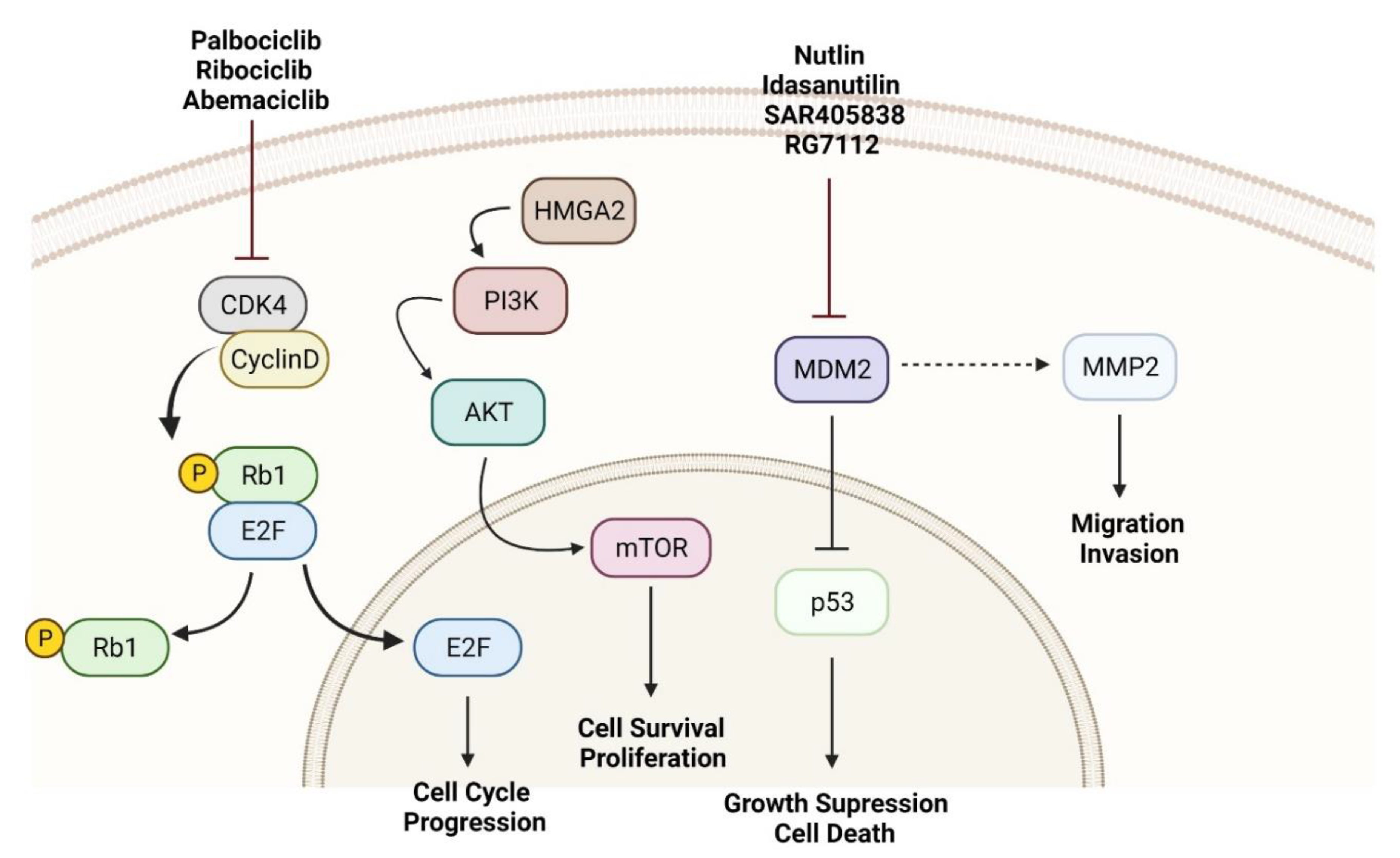
3. Molecular Mechanisms as Targets for RPLPS Treatment
3.1. MDM2 as a Molecular Driver and Target
3.2. CDK4 Inhibitors
3.3. Aurora Kinase Inhibitors
3.4. Other Kinases Associated with LPS
3.5. Immune Checkpoint Inhibitors
3.6. miRNAs and RPLPS Microenvironment
4. Conclusions and Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Gamboa, A.C.; Gronchi, A.; Cardona, K. Soft-tissue sarcoma in adults: An update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J. Clin. 2020, 70, 200–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, C.-C.; Chen, T.W.-W. Next frontiers in systemic therapy for soft tissue sarcoma. Chin. Clin. Oncol. 2018, 7, 43. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Grignol, V.P.; Gronchi, A.; Luo, C.-H.; Pollock, R.E.; Tseng, W.W. Surgical management of retroperitoneal sarcoma and opportunities for global collaboration. Chin. Clin. Oncol. 2018, 7, 39. [Google Scholar] [CrossRef]
- Bill, K.L.J.; Casadei, L.; Prudner, B.C.; Iwenofu, H.; Strohecker, A.M.; Pollock, R.E. Liposarcoma: Molecular targets and therapeutic implications. Cell. Mol. Life Sci. 2016, 73, 3711–3718. [Google Scholar] [CrossRef] [PubMed]
- Tfayli, Y.; Baydoun, A.; Naja, A.S.; Saghieh, S. Management of myxoid liposarcoma of the extremity (Review). Oncol. Lett. 2021, 22, 596. [Google Scholar] [CrossRef]
- Pérez-Losada, J.; Sánchez-Martín, M.; Rodríguez-García, M.A.; Pérez-Mancera, P.A.; Pintado, B.; Flores, T.; Battaner, E.; Sánchez-García, I. Liposarcoma initiated by FUS/TLS-CHOP: The FUS/TLS domain plays a critical role in the pathogenesis of liposarcoma. Oncogene 2000, 19, 6015–6022. [Google Scholar] [CrossRef] [Green Version]
- Antonescu, C.R.; Tschernyavsky, S.J.; Decuseara, R.; Leung, D.H.; Woodruff, J.M.; Brennan, M.F.; Bridge, J.A.; Neff, J.R.; Goldblum, J.R.; Ladanyi, M. Prognostic impact of P53 status, TLS-CHOP fusion transcript structure, and histological grade in myxoid liposarcoma: A molecular and clinicopathologic study of 82 cases. Clin. Cancer Res. 2001, 7, 3977–3987. [Google Scholar]
- Wang, L.; Luo, R.; Xiong, Z.; Xu, J.; Fang, D. Pleomorphic liposarcoma. Medicine 2018, 97, e9986. [Google Scholar] [CrossRef]
- Wan, L.; Tu, C.; Qi, L.; Li, Z. Survivorship and prognostic factors for pleomorphic liposarcoma: A population-based study. J. Orthop. Surg. Res. 2021, 16, 175. [Google Scholar] [CrossRef]
- Lewis, J.J.; Leung, D.; Woodruff, J.M.; Brennan, M.F. Retroperitoneal Soft-Tissue Sarcoma: Analysis of 500 Patients Treated and Followed at a Single Institution. Ann. Surg. 1998, 228, 355–365. [Google Scholar] [CrossRef]
- Bonvalot, S.; Rivoire, M.; Castaing, M.; Stoeckle, E.; Le Cesne, A.; Blay, J.Y.; Laplanche, A. Primary Retroperitoneal Sarcomas: A Multivariate Analysis of Surgical Factors Associated with Local Control. J. Clin. Oncol. 2009, 27, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Stahl, J.M.; Corso, C.D.; Park, H.S.; An, Y.; Rutter, C.E.; Han, D.; Roberts, K.B. The effect of microscopic margin status on survival in adult retroperitoneal soft tissue sarcomas. Eur. J. Surg. Oncol. (EJSO) 2017, 43, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Mullinax, J.E.; Zager, J.S.; Gonzalez, R.J. Current diagnosis and management of retroperitoneal sarcoma. Cancer Control 2011, 18, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Bremjit, P.J.; Jones, R.L.; Chai, X.; Kane, G.; Rodler, E.T.; Loggers, E.T.; Pollack, S.M.; Pillarisetty, V.G.; Mann, G.N. A Contemporary Large Single-Institution Evaluation of Resected Retroperitoneal Sarcoma. Ann. Surg. Oncol. 2014, 21, 2150–2158. [Google Scholar] [CrossRef]
- Miura, J.T.; Charlson, J.; Gamblin, T.C.; Eastwood, D.; Banerjee, A.; Johnston, F.M.; Turaga, K.K. Impact of chemotherapy on survival in surgically resected retroperitoneal sarcoma. Eur. J. Surg. Oncol. (EJSO) 2015, 41, 1386–1392. [Google Scholar] [CrossRef]
- Young, R.J.; Litière, S.; Lia, M.; Hogendoorn, P.C.W.; Fisher, C.; Mechtersheimer, G.; Daugaard, S.; Sciot, R.; Collin, F.; Messiou, C.; et al. Predictive and prognostic factors associated with soft tissue sarcoma response to chemotherapy: A subgroup analysis of the European Organisation for Research and Treatment of Cancer 62012 study. Acta Oncol. 2017, 56, 1013–1020. [Google Scholar] [CrossRef] [Green Version]
- Le Cesne, A.; Blay, J.-Y.; Domont, J.; Tresch-Bruneel, E.; Chevreau, C.; Bertucci, F.; Delcambre, C.; Saada-Bouzid, E.; Piperno-Neumann, S.; Bay, J.-O.; et al. Interruption versus continuation of trabectedin in patients with soft-tissue sarcoma (T-DIS): A randomised phase 2 trial. Lancet Oncol. 2015, 16, 312–319. [Google Scholar] [CrossRef]
- Schöffski, P.; Chawla, S.; Maki, R.G.; Italiano, A.; Gelderblom, H.; Choy, E.; Grignani, G.; Camargo, V.; Bauer, S.; Rha, S.Y.; et al. Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: A randomised, open-label, multicentre, phase 3 trial. Lancet 2016, 387, 1629–1637. [Google Scholar] [CrossRef]
- Dickson, M.A.; Schwartz, G.K.; Keohan, M.L.; D’Angelo, S.P.; Gounder, M.M.; Chi, P.; Antonescu, C.R.; Landa, J.; Qin, L.-X.; Crago, A.M.; et al. Progression-Free Survival Among Patients with Well-Differentiated or Dedifferentiated Liposarcoma Treated WithCDK4Inhibitor Palbociclib: A Phase 2 Clinical Trial. JAMA Oncol. 2016, 2, 937–940. [Google Scholar] [CrossRef] [Green Version]
- Lam, M.B.; Baldini, E.H.; Reijers, S.J.M.; Haas, R.L.; DeLaney, T.F. Role of Radiation Therapy for Newly Diagnosed Retroperitoneal Sarcoma. Curr. Treat. Options Oncol. 2021, 22, 75. [Google Scholar] [CrossRef]
- Bonvalot, S.; Gronchi, A.; Le Péchoux, C.; Swallow, C.J.; Strauss, D.; Meeus, P.; van Coevorden, F.; Stoldt, S.; Stoeckle, E.; Rutkowski, P.; et al. Preoperative radiotherapy plus surgery versus surgery alone for patients with primary retroperitoneal sarcoma (EORTC-62092: STRASS): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2020, 21, 1366–1377. [Google Scholar] [CrossRef]
- Tyler, R.; Wanigasooriya, K.; Taniere, P.; Almond, M.; Ford, S.; Desai, A.; Beggs, A. A review of retroperitoneal liposarcoma genomics. Cancer Treat. Rev. 2020, 86, 102013. [Google Scholar] [CrossRef] [PubMed]
- Gisselsson, D.; Höglund, M.; Mertens, F.; Johansson, B.; Dal Cin, P.; Van den Berghe, H.; Earnshaw, W.C.; Mitelman, F.; Mandahl, N. The structure and dynamics of ring chromosomes in human neoplastic and non-neoplastic cells. Qual. Life Res. 1999, 104, 315–325. [Google Scholar] [CrossRef]
- Szymanska, J.; Tarkkanen, M.; Wiklund, T.; Virolainen, M.; Blomqvist, C.; Asko-Seljavaara, S.; Tukiainen, E.; Elomaa, I.; Knuutila, S. Gains and losses of DNA sequences in liposarcomas evaluated by comparative genomic hybridization. Genes Chromosom. Cancer 1996, 15, 89–94. [Google Scholar] [CrossRef]
- Nishio, J. Contributions of Cytogenetics and Molecular Cytogenetics to the Diagnosis of Adipocytic Tumors. J. Biomed. Biotechnol. 2011, 2011, 524067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Momand, J.; Jung, D.; Wilczynski, S.; Niland, J. The MDM2 gene amplification database. Nucleic Acids Res. 1998, 26, 3453–3459. [Google Scholar] [CrossRef] [PubMed]
- Konopleva, M.; Martinelli, G.; Daver, N.; Papayannidis, C.; Wei, A.; Higgins, B.; Ott, M.; Mascarenhas, J.; Andreeff, M. MDM2 inhibition: An important step forward in cancer therapy. Leukemia 2020, 34, 2858–2874. [Google Scholar] [CrossRef]
- Bill, K.L.J.; Garnett, J.; Meaux, I.; Ma, X.; Creighton, C.J.; Bolshakov, S.; Barriere, C.; Debussche, L.; Lazar, A.J.; Prudner, B.C.; et al. SAR405838: A Novel and Potent Inhibitor of the MDM2:p53 Axis for the Treatment of Dedifferentiated Liposarcoma. Clin. Cancer Res. 2016, 22, 1150–1160. [Google Scholar] [CrossRef] [Green Version]
- Holzer, P.; Masuya, K.; Furet, P.; Kallen, J.; Valat-Stachyra, T.; Ferretti, S.; Berghausen, J.; Bouisset-Leonard, M.; Buschmann, N.; Pissot-Soldermann, C.; et al. Discovery of a Dihydroisoquinolinone Derivative (NVP-CGM097): A Highly Potent and Selective MDM2 Inhibitor Undergoing Phase 1 Clinical Trials in p53wt Tumors. J. Med. Chem. 2015, 58, 6348–6358. [Google Scholar] [CrossRef]
- Jeay, S.; Chène, P.; Ferretti, S.; Furet, P.; Gruenenfelder, B.; Guagnano, V.; Guerreiro, N.; Halilovic, E.; Hofmann, F.; Kallen, J.; et al. Abstract 1225: NVP-HDM201: Cellular and in vivo profile of a novel highly potent and selective PPI inhibitor of p53-Mdm2. In Proceedings of the Experimental and Molecular Therapeutics, New Orleans, LA, USA, 16–20 April 2016; Volume 76, p. 1225. [Google Scholar]
- Jeay, S.; Berghausen, J.; Buschmann, N.; Chène, P.; Cozens, R.; Erdmann, D.; Ferretti, S.; Furet, P.; Gabriel, T.; Gessier, F.; et al. Abstract 1797: Discovery of NVP-CGM097, a highly potent and optimized small molecule inhibitor of Mdm2 under evaluation in a Phase I clinical trial. In Proceedings of the Experimental and Molecular Therapeutics, San Diego, CA, USA, 5–9 April 2014; Volume 74, p. 1797. [Google Scholar]
- Barbieri, E.; Mehta, P.; Chen, Z.; Zhang, L.; Slack, A.; Berg, S.; Shohet, J.M. MDM2 inhibition sensitizes neuroblastoma to chemotherapy-induced apoptotic cell death. Mol. Cancer Ther. 2006, 5, 2358–2365. [Google Scholar] [CrossRef] [Green Version]
- Welliver, M.X.; Van Tine, B.A.; Houghton, P.; Rudek, M.A.; Pollock, R.E.; Kane, J.M.; Schwartz, G.K.; Zhang, P.; Kirsch, D.G.; Wakely, P.; et al. MDM2 inhibitor AMG-232 and radiation therapy in treating patients with soft tissue sarcoma with wild-type TP53: A phase IB study (NRG-DT001). J. Clin. Oncol. 2019, 37, TPS11076. [Google Scholar] [CrossRef]
- Casadei, L.; Choudhury, A.; Sarchet, P.; Sundaram, P.M.; Lopez, G.; Braggio, D.; Balakirsky, G.; Pollock, R.; Prakash, S. Cross-flow microfiltration for isolation, selective capture and release of liposarcoma extracellular vesicles. J. Extracell. Vesicles 2021, 10, e12062. [Google Scholar] [CrossRef] [PubMed]
- Casadei, L.; Pollock, R.E. Extracellular vesicle cross-talk in the liposarcoma microenvironment. Cancer Lett. 2020, 487, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Casadei, L.; Calore, F.; Braggio, D.A.; Zewdu, A.; Deshmukh, A.A.; Fadda, P.; Lopez, G.; Wabitsch, M.; Song, C.; Leight, J.L.; et al. MDM2 Derived from Dedifferentiated Liposarcoma Extracellular Vesicles Induces MMP2 Production from Preadipocytes. Cancer Res. 2019, 79, 4911–4922. [Google Scholar] [CrossRef] [Green Version]
- Poltavets, V.; Kochetkova, M.; Pitson, S.M.; Samuel, M.S. The Role of the Extracellular Matrix and Its Molecular and Cellular Regulators in Cancer Cell Plasticity. Front. Oncol. 2018, 8, 431. [Google Scholar] [CrossRef] [Green Version]
- Kessenbrock, K.; Plaks, V.; Werb, Z. Matrix metalloproteinases: Regulators of the tumor microenvironment. Cell 2010, 141, 52–67. [Google Scholar] [CrossRef] [Green Version]
- Benassi, M.S.; Gamberi, G.; Magagnoli, G.; Molendini, L.; Ragazzini, P.; Merli, M.; Chiesa, F.; Balladelli, A.; Manfrini, M.; Bertoni, F.; et al. Metalloproteinase expression and prognosis in soft tissue sarcomas. Ann. Oncol. 2001, 12, 75–80. [Google Scholar] [CrossRef]
- Pazzaglia, L.; Ponticelli, F.; Magagnoli, G.; Magagnoli, G.; Gamberi, G.; Ragazzini, P.; Balladelli, A.; Picci, P.; Benassi, M. Activation of metalloproteinases-2 and -9 by interleukin-1alpha in S100A4-positive liposarcoma cell line: Correlation with cell invasiveness. Anticancer Res. 2004, 24, 967–972. [Google Scholar]
- Sbaraglia, M.; Bellan, E.; Tos, A.P.D. The 2020 WHO Classification of Soft Tissue Tumours: News and perspectives. Pathologica 2020, 113, 70–84. [Google Scholar] [CrossRef]
- Beird, H.C.; Wu, C.-C.; Ingram, D.R.; Wang, W.-L.; Alimohamed, A.; Gumbs, C.; Little, L.; Song, X.; Feig, B.W.; Roland, C.L.; et al. Genomic profiling of dedifferentiated liposarcoma compared to matched well-differentiated liposarcoma reveals higher genomic complexity and a common origin. Mol. Case Stud. 2018, 4, a002386. [Google Scholar] [CrossRef] [Green Version]
- Italiano, A.; Bianchini, L.; Gjernes, E.; Keslair, F.; Ranchere-Vince, D.; Dumollard, J.-M.; Haudebourg, J.; Leroux, A.; Mainguené, C.; Terrier, P.; et al. Clinical and Biological Significance of CDK4 Amplification in Well-Differentiated and Dedifferentiated Liposarcomas. Clin. Cancer Res. 2009, 15, 5696–5703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.J.; Kim, M.; Park, H.K.; Yu, D.B.; Jung, K.; Song, K.; Choi, Y.-L. Co-expression of MDM2 and CDK4 in transformed human mesenchymal stem cells causes high-grade sarcoma with a dedifferentiated liposarcoma-like morphology. Lab. Investig. 2019, 99, 1309–1320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musgrove, E.A.; Caldon, C.E.; Barraclough, J.; Stone, A.; Sutherland, R.L. Cyclin D as a therapeutic target in cancer. Nat. Cancer 2011, 11, 558–572. [Google Scholar] [CrossRef] [PubMed]
- Schettini, F.; De Santo, I.; Rea, C.G.; De Placido, P.; Formisano, L.; Giuliano, M.; Arpino, G.; De Laurentiis, M.; Puglisi, F.; De Placido, S.; et al. CDK 4/6 Inhibitors as Single Agent in Advanced Solid Tumors. Front. Oncol. 2018, 8, 608. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.-X.; Sicinska, E.; Czaplinski, J.T.; Remillard, S.P.; Moss, S.; Wang, Y.; Brain, C.; Loo, A.; Snyder, E.L.; Demetri, G.D.; et al. Antiproliferative Effects of CDK4/6 Inhibition in CDK4-Amplified Human Liposarcoma In Vitro and In Vivo. Mol. Cancer Ther. 2014, 13, 2184–2193. [Google Scholar] [CrossRef] [Green Version]
- Laroche-Clary, A.; Chaire, V.; Algeo, M.-P.; Derieppe, M.-A.; Loarer, F.L.; Italiano, A. Combined targeting of MDM2 and CDK4 is synergistic in dedifferentiated liposarcomas. J. Hematol. Oncol. 2017, 10, 123. [Google Scholar] [CrossRef] [Green Version]
- Dickson, M.A.; Koff, A.; D’Angelo, S.P.; Gounder, M.M.; Keohan, M.L.; Kelly, C.M.; Chi, P.; Antonescu, C.R.; Landa, J.; Qin, L.-X.; et al. Phase 2 study of the CDK4 inhibitor abemaciclib in dedifferentiated liposarcoma. J. Clin. Oncol. 2019, 37, 11004. [Google Scholar] [CrossRef]
- Razak, A.A.; Bauer, S.; Blay, J.-Y.; Quek, R.; Suárez, C.; Lin, C.-C.; Hütter-Krönke, M.L.; Cubedo, R.; Ferretti, S.; Meille, C.; et al. Abstract CT009: Results of a dose- and regimen-finding Phase Ib study of HDM201 in combination with ribociclib in patients with locally advanced or metastatic liposarcoma. In Proceedings of the Clinical Trials, Washington, DC, USA, 27–30 September 2018; Volume 78, p. CT009. [Google Scholar]
- Vader, G.; Lens, S.M. The Aurora kinase family in cell division and cancer. Biochim. Biophys. Acta 2008, 1786, 60–72. [Google Scholar] [CrossRef]
- Crago, A.M.; Singer, S. Clinical and molecular approaches to well differentiated and dedifferentiated liposarcoma. Curr. Opin. Oncol. 2011, 23, 373–378. [Google Scholar] [CrossRef] [Green Version]
- Yen, C.-C.; Chen, S.-C.; Hung, G.-Y.; Wu, P.-K.; Chua, W.-Y.; Lin, Y.-C.; Yen, C.-H.; Chen, Y.-C.; Wang, J.-Y.; Yang, M.-H.; et al. Expression profile-driven discovery of AURKA as a treatment target for liposarcoma. Int. J. Oncol. 2019, 55, 938–948. [Google Scholar] [CrossRef]
- Mattei, J.C.; Bouvier-Labit, C.; Barets, D.; Macagno, N.; Chocry, M.; Chibon, F.; Morando, P.; Rochwerger, R.A.; Duffaud, F.; Olschwang, S.; et al. Pan Aurora Kinase Inhibitor: A Promising Targeted-Therapy in Dedifferentiated Liposarcomas With Differential Efficiency Depending on Sarcoma Molecular Profile. Cancers 2020, 12, 583. [Google Scholar] [CrossRef] [PubMed]
- Noronha, S.; Alt, L.A.C.; Scimeca, T.E.; Zarou, O.; Obrzut, J.; Zanotti, B.; Hayward, E.A.; Pillai, A.; Mathur, S.; Rojas, J.; et al. Preclinical evaluation of the Aurora kinase inhibitors AMG 900, AZD1152-HQPA, and MK-5108 on SW-872 and 93T449 human liposarcoma cells. Vitr. Cell. Dev. Biology. Anim. 2018, 54, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.S.; Schwartz, G.K. MLN-8237: A dual inhibitor of aurora A and B in soft tissue sarcomas. Oncotarget 2016, 7, 12893–12903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asano, N.; Yoshida, A.; Mitani, S.; Kobayashi, E.; Shiotani, B.; Komiyama, M.; Fujimoto, H.; Chuman, H.; Morioka, H.; Matsumoto, M.; et al. Frequent amplification of receptor tyrosine kinase genes in well-differentiated/dedifferentiated liposarcoma. Oncotarget 2017, 8, 12941–12952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanojia, D.; Garg, M.; Martinez, J.; MT, A.; Luty, S.B.; Doan, N.B.; Said, J.W.; Forscher, C.; Tyner, J.W.; Koeffler, H.P. Kinase profiling of liposarcomas using RNAi and drug screening assays identified druggable targets. J. Hematol. Oncol. 2017, 10, 173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lierman, E.; Smits, S.; Cools, J.; Dewaele, B.; Debiec-Rychter, M.; Vandenberghe, P. Ponatinib is active against imatinib-resistant mutants of FIP1L1-PDGFRA and KIT, and against FGFR1-derived fusion kinases. Leukemia 2012, 26, 1693–1695. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Wozniak, A.; Sciot, R.; Cornillie, J.; Wellens, J.; Van Looy, T.; Vanleeuw, U.; Stas, M.; Hompes, D.; Debiec-Rychter, M.; et al. Pazopanib, a Receptor Tyrosine Kinase Inhibitor, Suppresses Tumor Growth through Angiogenesis in Dedifferentiated Liposarcoma Xenograft Models. Transl. Oncol. 2014, 7, 665–671. [Google Scholar] [CrossRef] [Green Version]
- Samuels, B.L.; Chawla, S.P.; Somaiah, N.; Staddon, A.P.; Skubitz, K.M.; Milhem, M.M.; Kaiser, P.E.; Portnoy, D.C.; Priebat, D.A.; Walker, M.S.; et al. Results of a prospective phase 2 study of pazopanib in patients with advanced intermediate-grade or high-grade liposarcoma. Cancer 2017, 123, 4640–4647. [Google Scholar] [CrossRef] [Green Version]
- E Chamberlain, F.E.; Wilding, C.; Jones, R.L.; Huang, P. Pazopanib in patients with advanced intermediate-grade or high-grade liposarcoma. Expert Opin. Investig. Drugs 2019, 28, 505–511. [Google Scholar] [CrossRef] [Green Version]
- Zhu, M.M.T.; Shenasa, E.; Nielsen, T.O. Sarcomas: Immune biomarker expression and checkpoint inhibitor trials. Cancer Treat. Rev. 2020, 91, 102115. [Google Scholar] [CrossRef]
- Yan, L.; Wang, Z.; Cui, C.; Guan, X.; Dong, B.; Zhao, M.; Wu, J.; Tian, X.; Hao, C. Comprehensive immune characterization and T-cell receptor repertoire heterogeneity of retroperitoneal liposarcoma. Cancer Sci. 2019, 110, 3038–3048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, B.; Lee, J.S.; Kim, S.J.; Hong, D.; Park, J.B.; Lee, K.-Y. Anti-tumor effects of anti-PD-1 antibody, pembrolizumab, in humanized NSG PDX mice xenografted with dedifferentiated liposarcoma. Cancer Lett. 2020, 478, 56–69. [Google Scholar] [CrossRef] [PubMed]
- Saerens, M.; Brusselaers, N.; Rottey, S.; Decruyenaere, A.; Creytens, D.; Lapeire, L. Immune checkpoint inhibitors in treatment of soft-tissue sarcoma: A systematic review and meta-analysis. Eur. J. Cancer 2021, 152, 165–182. [Google Scholar] [CrossRef] [PubMed]
- Tawbi, H.A.; Burgess, M.; Bolejack, V.; Van Tine, B.A.; Schuetze, S.M.; Hu, J.; D’Angelo, S.; Attia, S.; Riedel, R.F.; Priebat, D.A.; et al. Pembrolizumab in advanced soft-tissue sarcoma and bone sarcoma (SARC028): A multicentre, two-cohort, single-arm, open-label, phase 2 trial. Lancet Oncol. 2017, 18, 1493–1501. [Google Scholar] [CrossRef]
- Keung, E.Z.; Burgess, M.; Salazar, R.; Parra, E.R.; Rodrigues-Canales, J.; Bolejack, V.; Van Tine, B.A.; Schuetze, S.M.; Attia, S.; Riedel, R.F.; et al. Correlative Analyses of the SARC028 Trial Reveal an Association Between Sarcoma-Associated Immune Infiltrate and Response to Pembrolizumab. Clin. Cancer Res. 2020, 26, 1258–1266. [Google Scholar] [CrossRef]
- Nakata, E.; Fujiwara, T.; Kunisada, T.; Ito, T.; Takihira, S.; Ozaki, T. Immunotherapy for sarcomas. Jpn J. Clin. Oncol. 2021, 51, 523–537. [Google Scholar] [CrossRef]
- Esquela-Kerscher, A.; Slack, F.J. Oncomirs—microRNAs with a role in cancer. Nat. Cancer 2006, 6, 259–269. [Google Scholar] [CrossRef]
- Calin, G.A.; Croce, C.M. MicroRNA Signatures in Human Cancers. Nat. Rev. Cancer 2006, 6, 857–866. [Google Scholar] [CrossRef]
- Igaz, I.; Igaz, P. Tumor surveillance by circulating microRNAs: A hypothesis. Cell. Mol. Life Sci. CMLS 2014, 71, 4081–4087. [Google Scholar] [CrossRef] [Green Version]
- Vincenzi, B.; Iuliani, M.; Zoccoli, A.; Pantano, F.; Fioramonti, M.; De Lisi, D.; Frezza, A.M.; Rabitti, C.; Perrone, G.; Muda, A.O.; et al. Deregulation of dicer and mir-155 expression in liposarcoma. Oncotarget 2015, 6, 10586–10591. [Google Scholar] [CrossRef] [Green Version]
- Kapodistrias, N.; Mavridis, K.; Batistatou, A.; Gogou, P.; Karavasilis, V.; Sainis, I.; Briasoulis, E.; Scorilas, A. Assessing the clinical value of microRNAs in formalin-fixed paraffin-embedded liposarcoma tissues: Overexpressed miR-155 is an indicator of poor prognosis. Oncotarget 2017, 8, 6896–6913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, D.H.; Amanat, S.; Goff, C.; Weiss, L.M.; Said, J.W.; Doan, N.B.; Sato-Otsubo, A.; Ogawa, S.; Forscher, C.; Koeffler, H.P. Overexpression of miR-26a-2 in human liposarcoma is correlated with poor patient survival. Oncogenesis 2013, 2, e47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohama, I.; Asano, N.; Matsuzaki, J.; Yamamoto, Y.; Yamamoto, T.; Takahashi, R.-U.; Kobayashi, E.; Takizawa, S.; Sakamoto, H.; Kato, K.; et al. Comprehensive serum and tissue microRNA profiling in dedifferentiated liposarcoma. Oncol. Lett. 2021, 22, 623. [Google Scholar] [CrossRef] [PubMed]
- Casadei, L.; Calore, F.; Creighton, C.J.; Guescini, M.; Batte, K.; Iwenofu, O.H.; Zewdu, A.; Braggio, D.A.; Bill, K.L.; Fadda, P.; et al. Exosome-Derived miR-25-3p and miR-92a-3p Stimulate Liposarcoma Progression. Cancer Res. 2017, 77, 3846–3856. [Google Scholar] [CrossRef] [Green Version]
| Trial Name | Status | Primary Aims/Findings |
|---|---|---|
| Retroperitoneal Sarcoma Registry: an International Prospective Initiative—NCT03838718 | Recruiting |
|
| Proton or Photon RT for Retroperitoneal Sarcomas—NCT01659203 | Recruiting |
|
| Navtemadlin and Radiation Therapy in Treating Patients with Soft Tissue Sarcoma—NCT03217266 | Recruiting |
|
| Neoadjuvant Chemotherapy and Retifanlimab in Patients with Selected Retroperitoneal Sarcomas (TORNADO)—NCT04968106 | Not yet recruiting |
|
| Surgery With or Without Neoadjuvant Chemotherapy in High-Risk Retroperitoneal Sarcoma (STRASS2)—NCT04031677 | Recruiting |
|
| Preoperative Ultra-hypofractionated Radiotherapy Followed by Surgery for Retroperitoneal Sarcoma—NCT05224934 | Recruiting |
|
| Nivolumab and BO-112 Before Surgery for the Treatment of Resectable Soft Tissue Sarcoma—NCT04420975 | Recruiting |
|
| Treatment of Milademetan Versus Trabectedin in Patient With Dedifferentiated Liposarcoma (MANTRA)—NCT04979442 | Recruiting |
|
| SARC041: Study of Abemaciclib Versus Placebo in Patients With Advanced Dedifferentiated Liposarcoma—NCT04967521 | Recruiting |
|
| Palbociclib and INCMGA00012 in People With Advanced Liposarcoma—NCT04438824 | Recruiting |
|
| Phase II Trial of Ribociclib and Everolimus in Advanced Dedifferentiated Liposarcoma (DDL) and Leiomyosarcoma (LMS)—NCT03114527 | Recruiting |
|
| Retroperitoneal Soft-Tissue Sarcomas—NCT05044624 | Completed (6/2021) |
|
| Surgery With or Without Radiation Therapy in Untreated Nonmetastatic Retroperitoneal Sarcoma (STRASS)—NCT01344018 | Completed (1/2018) |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casadei, L.; de Faria, F.C.C.; Lopez-Aguiar, A.; Pollock, R.E.; Grignol, V. Targetable Pathways in the Treatment of Retroperitoneal Liposarcoma. Cancers 2022, 14, 1362. https://doi.org/10.3390/cancers14061362
Casadei L, de Faria FCC, Lopez-Aguiar A, Pollock RE, Grignol V. Targetable Pathways in the Treatment of Retroperitoneal Liposarcoma. Cancers. 2022; 14(6):1362. https://doi.org/10.3390/cancers14061362
Chicago/Turabian StyleCasadei, Lucia, Fernanda Costas Casal de Faria, Alexandra Lopez-Aguiar, Raphael E. Pollock, and Valerie Grignol. 2022. "Targetable Pathways in the Treatment of Retroperitoneal Liposarcoma" Cancers 14, no. 6: 1362. https://doi.org/10.3390/cancers14061362
APA StyleCasadei, L., de Faria, F. C. C., Lopez-Aguiar, A., Pollock, R. E., & Grignol, V. (2022). Targetable Pathways in the Treatment of Retroperitoneal Liposarcoma. Cancers, 14(6), 1362. https://doi.org/10.3390/cancers14061362







