Improved Multimodal Tumor Necrosis Imaging with IRDye800CW-DOTA Conjugated to an Albumin-Binding Domain
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Precursor Synthesis and Radiolabeling
2.3. Determination of n-Octanol/PBS Distribution Coefficient (LogD7.4)
2.4. In Vitro Protein Binding
2.5. In Vitro Dead/Alive Cell Binding Assay
2.6. Microscopy
2.7. Animals
2.8. In Vivo Stability
2.9. FLI, BLI, and SPECT/CT Tumor Necrosis Imaging, Ideal Timepoint Determination
2.10. FLI, BLI, and PET/SPECT/CT Tumor Necrosis Imaging Procedure
2.11. Doxorubicin Treatment-Induced Necrosis in MCF7-Luc2
2.12. FLI, BLI, and PET/SPECT/CT Necrosis Imaging in EMT6-Luc2 Tumors
2.13. SPECT/PET/CT Image Processing
2.14. Ex Vivo Analysis
2.15. Statistics
3. Results
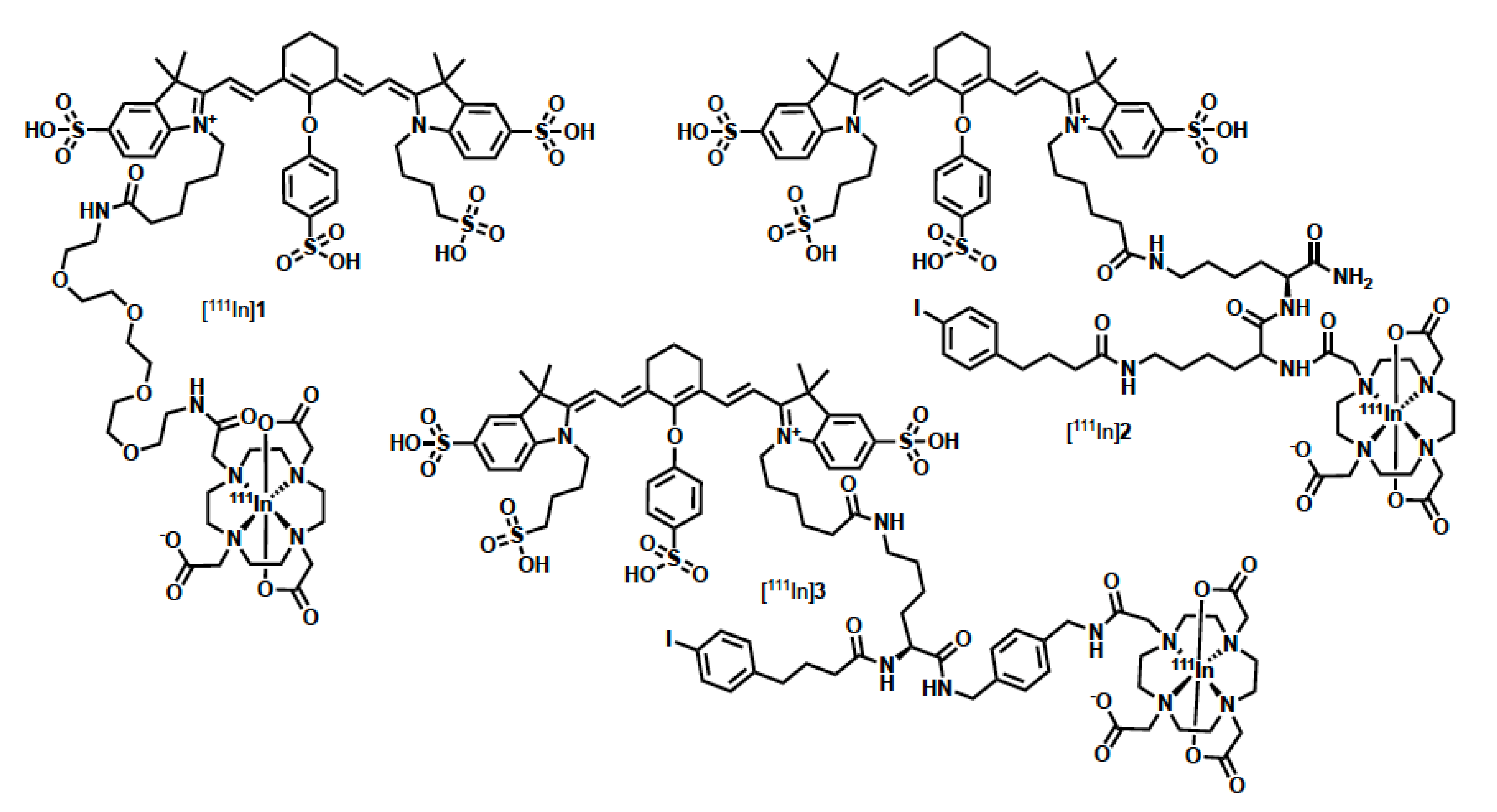
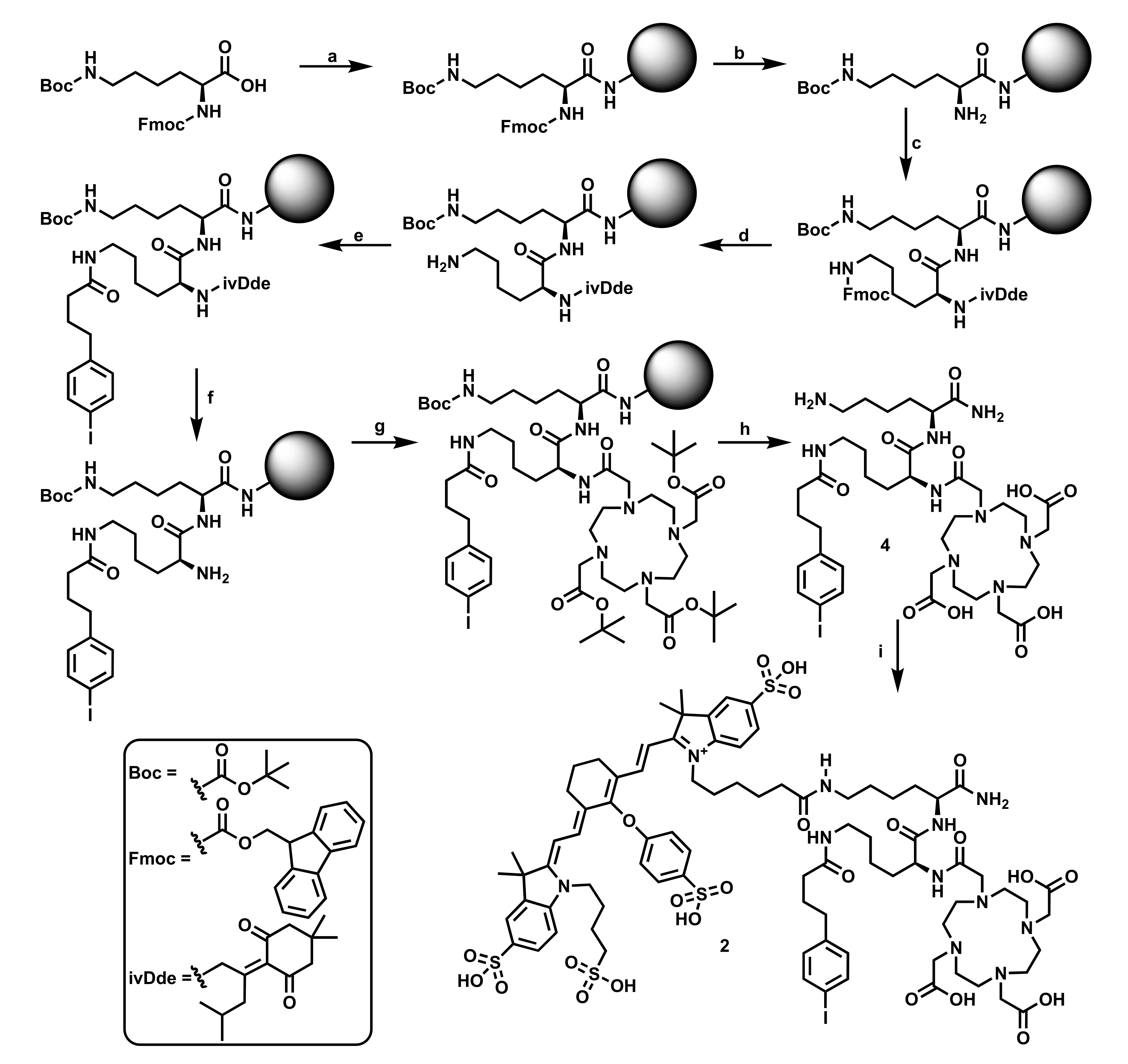
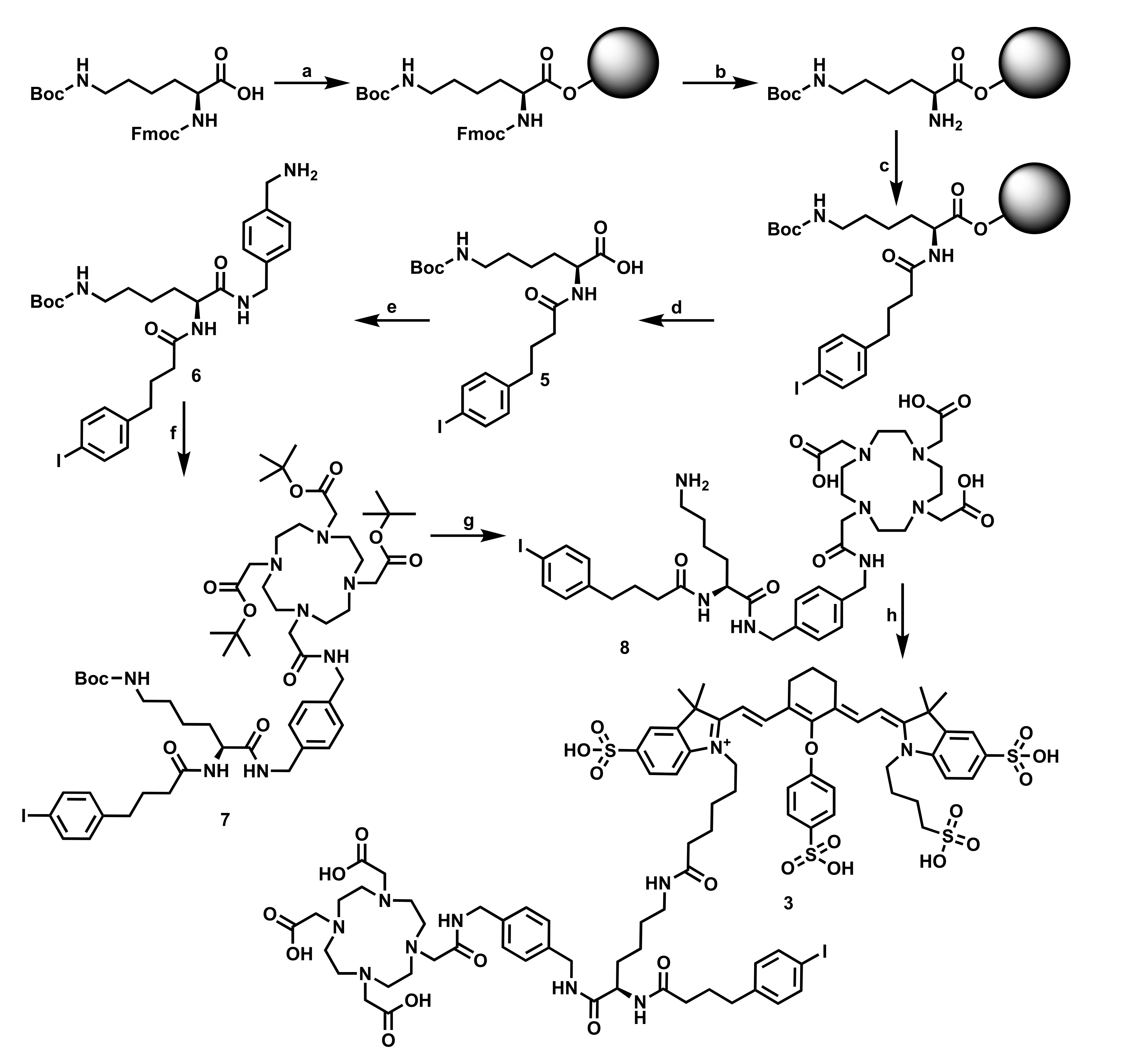
3.1. Precursor Synthesis and Radiolabeling
3.2. Log D and Protein Binding
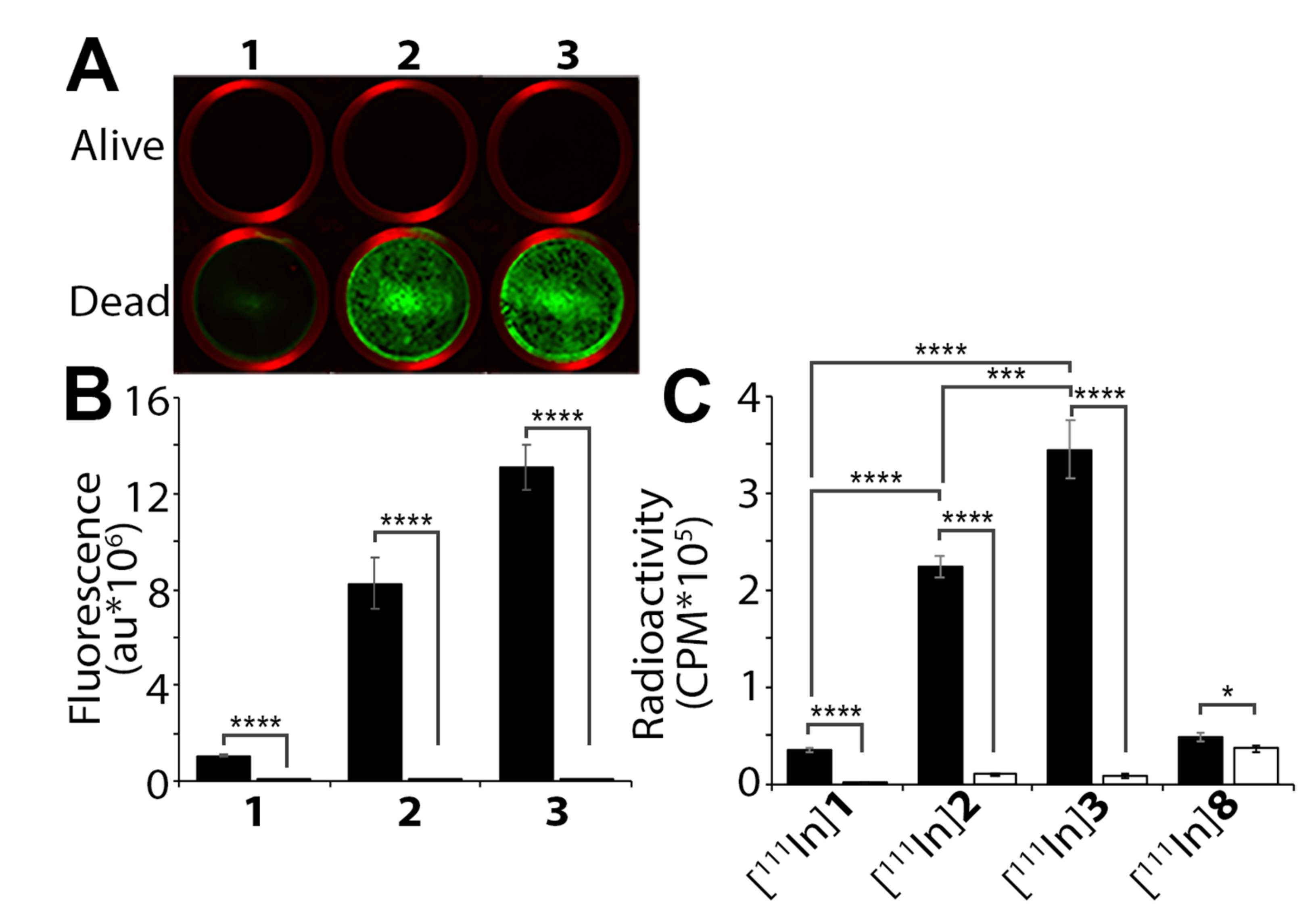
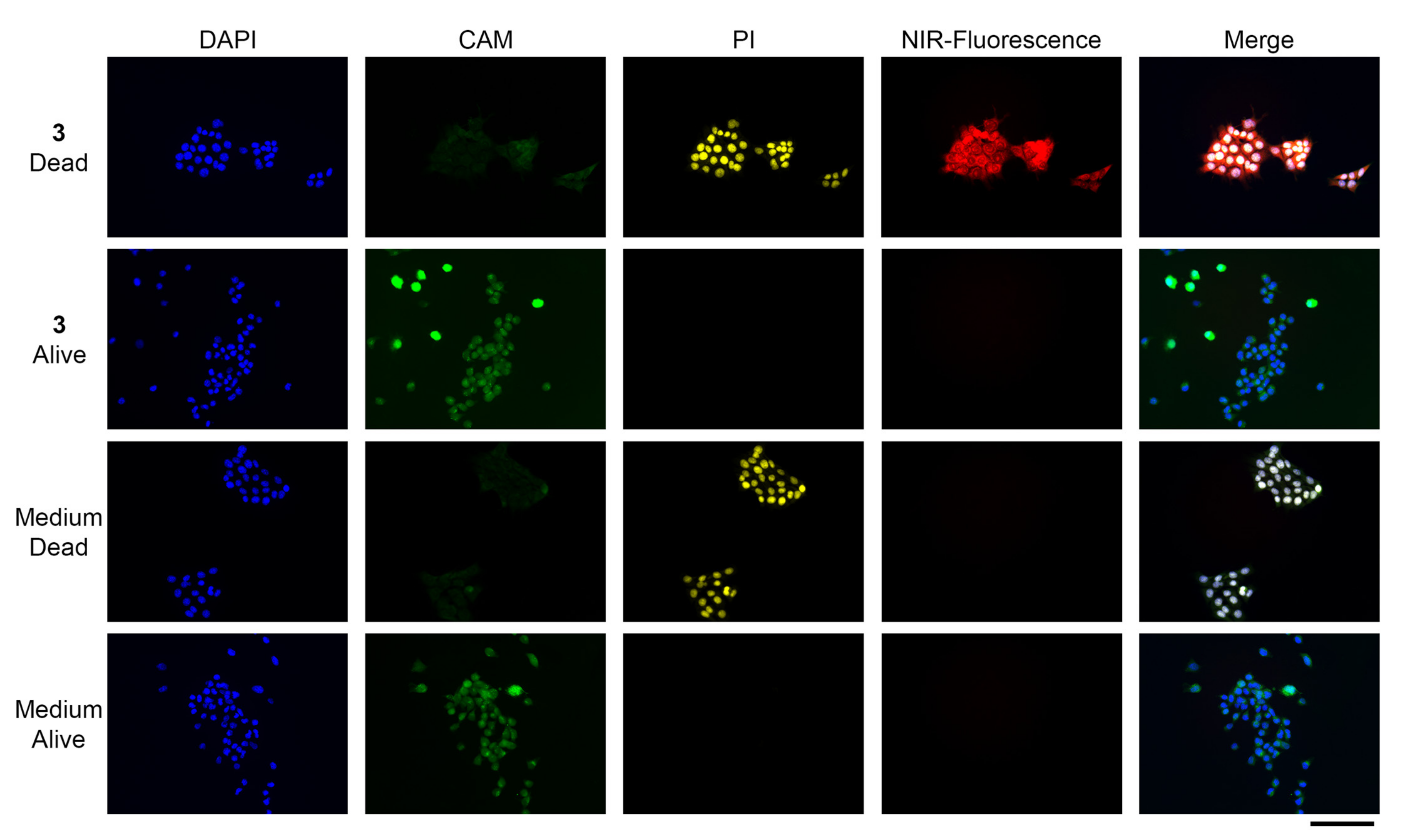
3.3. In Vitro Dead/Alive Cell Binding
3.4. Microscopy
3.5. In Vivo Stability
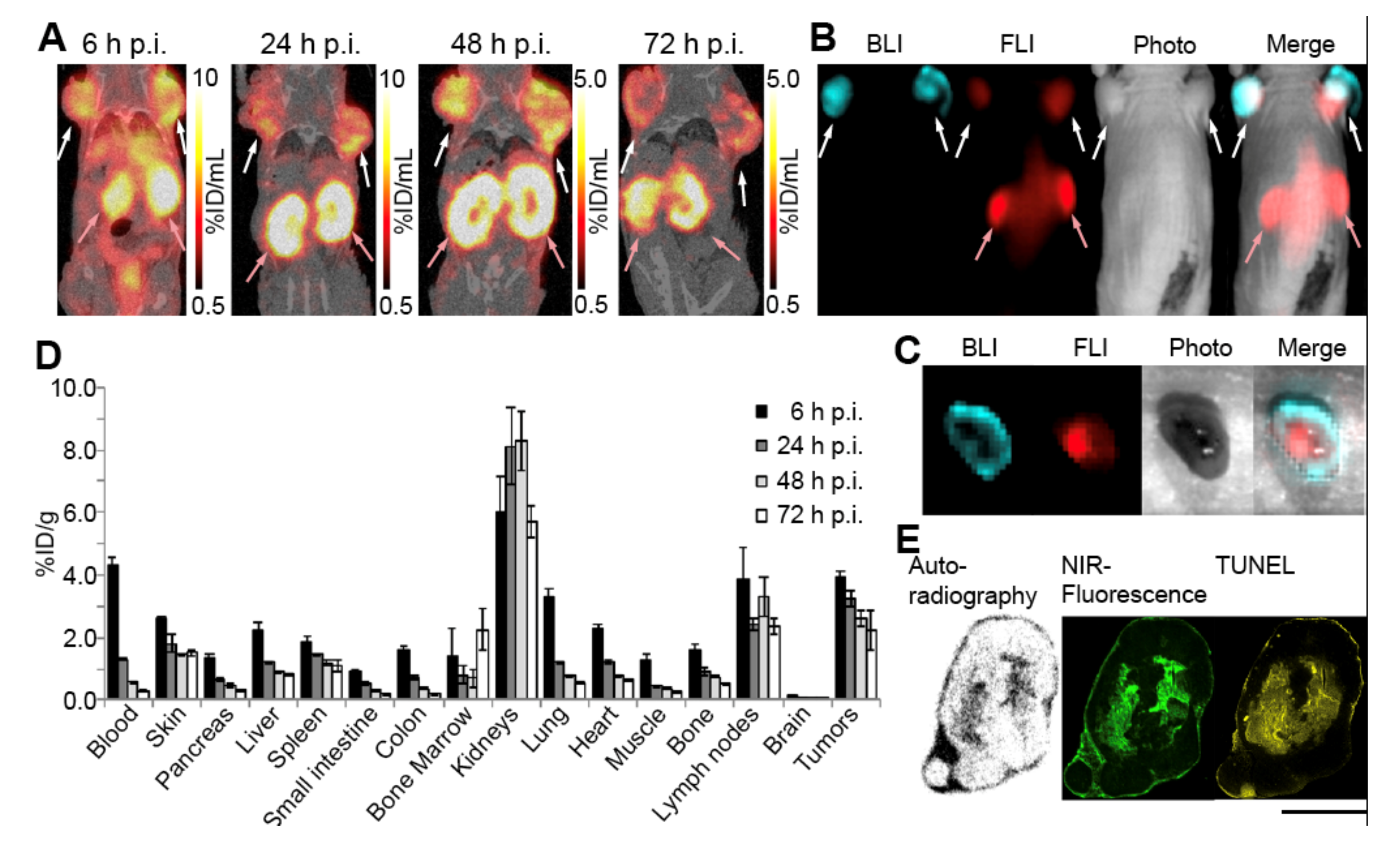
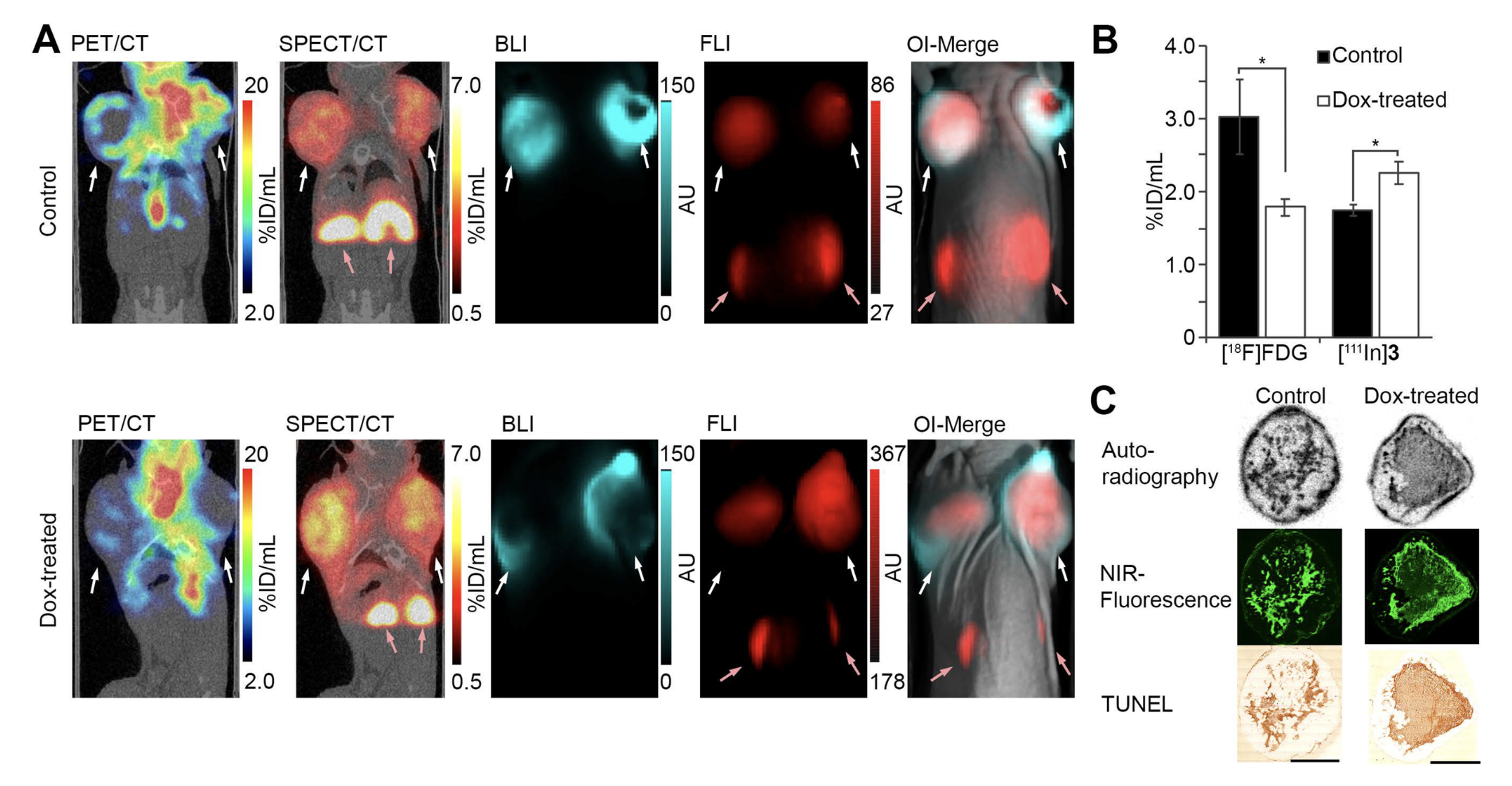
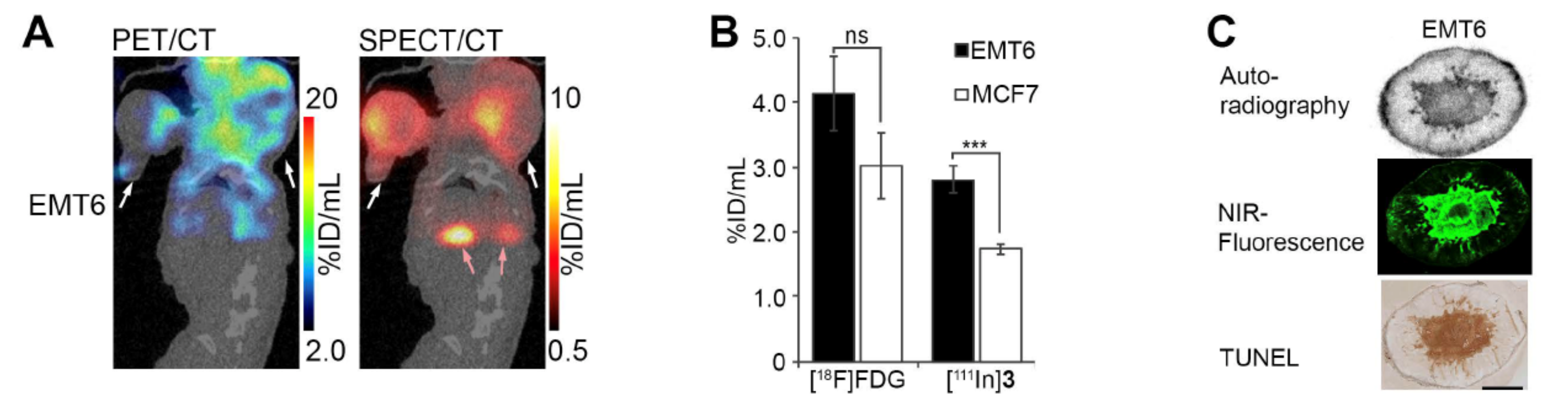
3.6. In Vivo Necrosis Imaging
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, D.; Jin, Q.; Jiang, C.; Gao, M.; Ni, Y.; Zhang, J. Imaging Cell Death: Focus on Early Evaluation of Tumor Response to Therapy. Bioconjug. Chem. 2020, 31, 1025–1051. [Google Scholar] [CrossRef] [PubMed]
- Galluzzi, L.; Vitale, I.; Aaronson, S.A.; Abrams, J.M.; Adam, D.; Agostinis, P.; Alnemri, E.S.; Altucci, L.; Amelio, I.; Andrews, D.W.; et al. Molecular mechanisms of cell death: Recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018, 25, 486–541. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Yu, C.; Luo, M.; Cen, C.; Qiu, J.; Zhang, S.; Hu, K. Ferroptosis in Cancer Treatment: Another Way to Rome. Front. Oncol. 2020, 10, 571127. [Google Scholar] [CrossRef] [PubMed]
- Stammes, M.A.; Knol-Blankevoort, V.T.; Cruz, L.J.; Feitsma, H.R.I.J.; Mezzanotte, L.; Cordfunke, R.A.; Sinisi, R.; Dubikovskaya, E.A.; Maeda, A.; DaCosta, R.S.; et al. Pre-clinical Evaluation of a Cyanine-Based SPECT Probe for Multimodal Tumor Necrosis Imaging. Mol. Imaging Biol. 2016, 18, 905–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bredholt, G.; Mannelqvist, M.; Stefansson, I.M.; Birkeland, E.; Bø, T.H.; Øyan, A.M.; Trovik, J.; Kalland, K.H.; Jonassen, I.; Salvesen, H.B.; et al. Tumor necrosis is an important hallmark of aggressive endometrial cancer and associates with hypoxia, angiogenesis and inflammation responses. Oncotarget 2015, 6, 39676–39691. [Google Scholar] [CrossRef] [Green Version]
- Sprooten, J.; De Wijngaert, P.; Vanmeerbeek, I.; Martin, S.; Vangheluwe, P.; Schlenner, S.; Krysko, D.V.; Parys, J.B.; Bultynck, G.; Vandenabeele, P.; et al. Necroptosis in Immuno-Oncology and Cancer Immunotherapy. Cells 2020, 9, 1823. [Google Scholar] [CrossRef]
- Papaevangelou, E.; Almeida, G.S.; Jamin, Y.; Robinson, S.P.; Desouza, N.M. Diffusion-weighted MRI for imaging cell death after cytotoxic or apoptosis-inducing therapy. Br. J. Cancer 2015, 112, 1471–1479. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Odawara, S.; Kitajima, K.; Katsuura, T.; Kurahashi, Y.; Shinohara, H.; Yamakado, K. Tumor response to neoadjuvant chemotherapy in patients with esophageal cancer assessed with CT and FDG-PET/CT–RECIST 1.1 vs. PERCIST 1.0. Eur. J. Radiol. 2018, 101, 65–71. [Google Scholar] [CrossRef]
- Abramson, R.G.; McGhee, C.R.; Lakomkin, N.; Arteaga, C.L. Pitfalls in RECIST Data Extraction for Clinical Trials: Beyond the Basics. Acad. Radiol. 2015, 22, 779–786. [Google Scholar] [CrossRef] [Green Version]
- Mankoff, D.A.; Eary, J.F.; Link, J.M.; Muzi, M.; Rajendran, J.G.; Spence, A.M.; Krohn, K.A. Tumor-Specific Positron Emission Tomography Imaging in Patients: [18F] Fluorodeoxyglucose and Beyond. Clin. Cancer Res. 2007, 13, 3460–3469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, M.S.; Packard, A.T.; Johnson, D.R.; Johnson, G.B. Pitfalls of a Mixed Metabolic Response at PET/CT. RadioGraphics 2019, 39, 1461–1475. [Google Scholar] [CrossRef] [PubMed]
- Xie, B.; Stammes, M.A.; van Driel, P.B.A.A.; Cruz, L.J.; Knol-Blankevoort, V.T.; Löwik, M.A.M.; Mezzanotte, L.; Que, I.; Chan, A.; van den Wijngaard, J.P.H.M.; et al. Necrosis avid near infrared fluorescent cyanines for imaging cell death and their use to monitor therapeutic efficacy in mouse tumor models. Oncotarget 2015, 6, 39036–39049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stammes, M.A.; Maeda, A.; Bu, J.; Scollard, D.A.; Kulbatski, I.; Medeiros, P.J.; Sinisi, R.; Dubikovskaya, E.A.; Snoeks, T.J.A.; van Beek, E.R.; et al. The Necrosis-Avid Small Molecule HQ4-DTPA as a Multimodal Imaging Agent for Monitoring Radiation Therapy-Induced Tumor Cell Death. Front. Oncol. 2016, 6, 221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stroet, M.C.M.; de Blois, E.; Stuurman, D.C.; de Ridder, C.M.A.; Haeck, J.; Seimbille, Y.; Mezzanotte, L.; de Jong, M.; Löwik, C.W.G.M.; Panth, K.M. In Vivo Evaluation of Indium-111–Labeled 800CW as a Necrosis-Avid Contrast Agent. Mol. Imaging Biol. 2020, 22, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Stroet, M.C.M.; Dijkstra, B.M.; Dulfer, S.E.; Kruijff, S.; den Dunnen, W.F.A.; Kruyt, F.A.E.; Groen, R.J.M.; Seimbille, Y.; Panth, K.M.; Mezzanotte, L.; et al. Necrosis binding of Ac-Lys0(IRDye800CW)-Tyr3-octreotate: A consequence from cyanine-labeling of small molecules. EJNMMI Res. 2021, 11, 47. [Google Scholar] [CrossRef]
- Knudsen Sand, K.M.; Bern, M.; Nilsen, J.; Noordzij, H.T.; Sandlie, I.; Andersen, J.T. Unraveling the interaction between FcRn and albumin: Opportunities for design of albumin-based therapeutics. Front. Immunol. 2015, 6, 682. [Google Scholar] [CrossRef] [Green Version]
- Zorzi, A.; Middendorp, S.J.; Wilbs, J.; Deyle, K.; Heinis, C. Acylated heptapeptide binds albumin with high affinity and application as tag furnishes long-acting peptides. Nat. Commun. 2017, 8, 16092. [Google Scholar] [CrossRef]
- Zorzi, A.; Linciano, S.; Angelini, A. Non-covalent albumin-binding ligands for extending the circulating half-life of small biotherapeutics. MedChemComm 2019, 10, 1068–1081. [Google Scholar] [CrossRef]
- Lau, J.; Jacobson, O.; Niu, G.; Lin, K.-S.; Bénard, F.; Chen, X. Bench to Bedside: Albumin Binders for Improved Cancer Radioligand Therapies. Bioconjug. Chem. 2019, 30, 487–502. [Google Scholar] [CrossRef]
- Dumelin, C.E.; Trüssel, S.; Buller, F.; Trachsel, E.; Bootz, F.; Zhang, Y.; Mannocci, L.; Beck, S.C.; Drumea-Mirancea, M.; Seeliger, M.W.; et al. A Portable Albumin Binder from a DNA-Encoded Chemical Library. Angew. Chem. 2008, 120, 3240–3245. [Google Scholar] [CrossRef]
- Zambito, G.; Gaspar, N.; Ridwan, Y.; Hall, M.P.; Shi, C.; Kirkland, T.A.; Encell, L.P.; Löwik, C.; Mezzanotte, L. Evaluating Brightness and Spectral Properties of Click Beetle and Firefly Luciferases Using Luciferin Analogues: Identification of Preferred Pairings of Luciferase and Substrate for In Vivo Bioluminescence Imaging. Mol. Imaging Biol. 2020, 22, 1523–1531. [Google Scholar] [CrossRef] [PubMed]
- Benešová, M.; Umbricht, C.A.; Schibli, R.; Müller, C. Albumin-Binding PSMA Ligands: Optimization of the Tissue Distribution Profile. Mol. Pharm. 2018, 15, 934–946. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Su, H.; Sun, W.; Cai, J.; Liu, S.; Chai, Y.; Zhang, C. Dual chemodrug-loaded single-walled carbon nanohorns for multimodal imaging-guided chemo-photothermal therapy of tumors and lung metastases. Theranostics 2018, 8, 1966–1984. [Google Scholar] [CrossRef] [PubMed]
- Breeman, W.A.P.; Chan, H.S.; de Blois, E. Determination of peptide content and purity of DOTA-peptides by metal ion titration and UPLC: An alternative method to monitor quality of DOTA-peptides. J. Radioanal. Nucl. Chem. 2014, 302, 825–830. [Google Scholar] [CrossRef]
- Twentyman, P.; Wright, K.; Fox, N. Characterisation of a mouse tumour cell line with in vitro derived resistance to verapamil. Br. J. Cancer 1990, 61, 279–284. [Google Scholar] [CrossRef] [Green Version]
- Sweeney, K.J.; Swarbrick, A.; Sutherland, R.L.; Musgrove, E.A. Lack of relationship between CDK activity and G1 cyclin expression in breast cancer cells. Oncogene 1998, 16, 2865–2878. [Google Scholar] [CrossRef] [Green Version]
- Gao, H.; Luo, C.; Yang, G.; Du, S.; Li, X.; Zhao, H.; Shi, J.; Wang, F. Improved in Vivo Targeting Capability and Pharmacokinetics of 99m Tc-Labeled isoDGR by Dimerization and Albumin-Binding for Glioma Imaging. Bioconjug. Chem. 2019, 30, 2038–2048. [Google Scholar] [CrossRef]
- Siwowska, K.; Haller, S.; Bortoli, F.; Benešová, M.; Groehn, V.; Bernhardt, P.; Schibli, R.; Müller, C. Preclinical comparison of albumin-binding radiofolates: Impact of linker entities on the in vitro and in vivo properties. Mol. Pharm. 2017, 14, 523–532. [Google Scholar] [CrossRef]
- Kuo, H.-T.; Merkens, H.; Zhang, Z.; Uribe, C.F.; Lau, J.; Zhang, C.; Colpo, N.; Lin, K.-S.; Bénard, F. Enhancing Treatment Efficacy of 177 Lu-PSMA-617 with the Conjugation of an Albumin-Binding Motif: Preclinical Dosimetry and Endoradiotherapy Studies. Mol. Pharm. 2018, 15, 5183–5191. [Google Scholar] [CrossRef]
- Wen, X.; Shi, C.; Yang, L.; Zeng, X.; Lin, X.; Huang, J.; Li, Y.; Zhuang, R.; Zhu, H.; Guo, Z.; et al. A radioiodinated FR-β-targeted tracer with improved pharmacokinetics through modification with an albumin binder for imaging of macrophages in AS and NAFL. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 503–516. [Google Scholar] [CrossRef] [PubMed]
- Fanali, G.; Di Masi, A.; Trezza, V.; Marino, M.; Fasano, M.; Ascenzi, P. Human serum albumin: From bench to bedside. Mol. Asp. Med. 2012, 33, 209–290. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Hartner, W.C.; Gillespie, J.W.; Praveen, K.P.; Yang, S.; Mei, L.A.; Petrenko, V.A.; Torchilin, V.P. Enhanced tumor delivery and antitumor activity in vivo of liposomal doxorubicin modified with MCF-7-specific phage fusion protein. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 421–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O, J.H.; Lodge, M.A.; Wahl, R.L. Practical PERCIST: A Simplified Guide to PET Response Criteria in Solid Tumors 1.0. Radiology 2016, 280, 576–584. [Google Scholar] [CrossRef] [Green Version]
- Goorden, M.C.; van der Have, F.; Kreuger, R.; Ramakers, R.M.; Vastenhouw, B.; Burbach, J.P.H.; Booij, J.; Molthoff, C.F.M.; Beekman, F.J. VECTor: A preclinical imaging system for simultaneous submillimeter SPECT and PET. J. Nucl. Med. 2013, 54, 306–312. [Google Scholar] [CrossRef] [Green Version]
- Beroske, L.; Van den Wyngaert, T.; Stroobants, S.; Van der Veken, P.; Elvas, F. Molecular Imaging of Apoptosis: The Case of Caspase-3 Radiotracers. Int. J. Mol. Sci. 2021, 22, 3948. [Google Scholar] [CrossRef]
- Szucs, Z.; Joseph, J.; Larkin, T.J.; Xie, B.; Bohndiek, S.E.; Brindle, K.M.; Neves, A.A. Correction to: Multi-modal imaging of high-risk ductal carcinoma in situ of the breast using C2Am: A targeted cell death imaging agent. Breast Cancer Res. 2021, 23, 32. [Google Scholar] [CrossRef]
- Neves, A.A.; Xie, B.; Fawcett, S.; Alam, I.S.; Witney, T.H.; de Backer, M.M.; Summers, J.; Hughes, W.; McGuire, S.; Soloviev, D.; et al. Rapid Imaging of Tumor Cell Death In Vivo Using the C2A Domain of Synaptotagmin-I. J. Nucl. Med. 2017, 58, 881–887. [Google Scholar] [CrossRef] [Green Version]
- Bulat, F.; Hesse, F.; Hu, D.E.; Ros, S.; Willminton-Holmes, C.; Xie, B.; Attili, B.; Soloviev, D.; Aigbirhio, F.; Leeper, F.J.; et al. 18F-C2Am: A targeted imaging agent for detecting tumor cell death in vivo using positron emission tomography. EJNMMI Res. 2020, 10, 151. [Google Scholar] [CrossRef]
- Lotfi, R.; Kaltenmeier, C.; Lotze, M.T.; Bergmann, C. Until Death Do Us Part: Necrosis and Oxidation Promote the Tumor Microenvironment. Transfus. Med. Hemotherapy 2016, 43, 120–132. [Google Scholar] [CrossRef] [Green Version]
- Lamberts, L.E.; Koch, M.; de Jong, J.S.; Adams, A.L.L.; Glatz, J.; Kranendonk, M.E.G.; Terwisscha van Scheltinga, A.G.T.; Jansen, L.; de Vries, J.; Lub-de Hooge, M.N.; et al. Tumor-Specific Uptake of Fluorescent Bevacizumab–IRDye800CW Microdosing in Patients with Primary Breast Cancer: A Phase I Feasibility Study. Clin. Cancer Res. 2017, 23, 2730–2741. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenthal, E.L.; Warram, J.M.; De Boer, E.; Chung, T.K.; Korb, M.L.; Brandwein-Gensler, M.; Strong, T.V.; Schmalbach, C.E.; Morlandt, A.B.; Agarwal, G.; et al. Safety and tumor specificity of cetuximab-IRDye800 for surgical navigation in head and neck cancer. Clin. Cancer Res. 2015, 21, 3658–3666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Väyrynen, S.A.; Väyrynen, J.P.; Klintrup, K.; Mäkelä, J.; Karttunen, T.J.; Tuomisto, A.; Mäkinen, M.J. Clinical impact and network of determinants of tumour necrosis in colorectal cancer. Br. J. Cancer 2016, 114, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Yee, P.P.; Li, W. Tumor necrosis: A synergistic consequence of metabolic stress and inflammation. BioEssays 2021, 43, 2100029. [Google Scholar] [CrossRef]
- Holub, K.; Biete, A. New pre-treatment eosinophil-related ratios as prognostic biomarkers for survival outcomes in endometrial cancer. BMC Cancer 2018, 18, 1280. [Google Scholar] [CrossRef] [Green Version]
- Breeman, W.A.P.; van der Wansem, K.; Bernard, B.F.; van Gameren, A.; Erion, J.L.; Visser, T.J.; Krenning, E.P.; de Jong, M. The addition of DTPA to [177Lu-DOTA0,Tyr3]octreotate prior to administration reduces rat skeleton uptake of radioactivity. Eur. J. Nucl. Med. Mol. Imaging 2003, 30, 312–315. [Google Scholar] [CrossRef]
| Compound | Chemical Purity a | Radiochemical Purity b | LogD b | Protein Binding b |
|---|---|---|---|---|
| 1 | >99% | >96% | −3.58 ± 0.07 | 70 ± 0.9% |
| 2 | >98% | >95% | −2.47 ± 0.01 | 95 ± 0.1% |
| 3 | >98% | >95% | −2.73 ± 0.14 | 94 ± 0.2% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stroet, M.C.M.; de Blois, E.; de Jong, M.; Seimbille, Y.; Mezzanotte, L.; Löwik, C.W.G.M.; Panth, K.M. Improved Multimodal Tumor Necrosis Imaging with IRDye800CW-DOTA Conjugated to an Albumin-Binding Domain. Cancers 2022, 14, 861. https://doi.org/10.3390/cancers14040861
Stroet MCM, de Blois E, de Jong M, Seimbille Y, Mezzanotte L, Löwik CWGM, Panth KM. Improved Multimodal Tumor Necrosis Imaging with IRDye800CW-DOTA Conjugated to an Albumin-Binding Domain. Cancers. 2022; 14(4):861. https://doi.org/10.3390/cancers14040861
Chicago/Turabian StyleStroet, Marcus C. M., Erik de Blois, Marion de Jong, Yann Seimbille, Laura Mezzanotte, Clemens W. G. M. Löwik, and Kranthi M. Panth. 2022. "Improved Multimodal Tumor Necrosis Imaging with IRDye800CW-DOTA Conjugated to an Albumin-Binding Domain" Cancers 14, no. 4: 861. https://doi.org/10.3390/cancers14040861
APA StyleStroet, M. C. M., de Blois, E., de Jong, M., Seimbille, Y., Mezzanotte, L., Löwik, C. W. G. M., & Panth, K. M. (2022). Improved Multimodal Tumor Necrosis Imaging with IRDye800CW-DOTA Conjugated to an Albumin-Binding Domain. Cancers, 14(4), 861. https://doi.org/10.3390/cancers14040861






