Simple Summary
Gastric cancer is a major health risk, and surgery is the primary curative option. However, the appropriate extent of lymph node dissection and appropriate surgical margins are two major issues that need to be addressed. Clinical tracers are an excellent solution. Therefore, we compiled a list of common clinical tracers for gastric cancer surgery to help surgeons better select and use them.
Abstract
The treatment of gastric cancer mainly depends on radical gastrectomy. Determination of appropriate surgical margins and adequate lymph node (LN) resection are two major surgical steps that directly correlate with prognosis in gastric cancer. Due to the expanding use of minimally invasive procedures, it is no longer possible to locate tumors and LNs through touch. As an alternative, tracers have begun to enter the field due to their capacities for intraoperative visualization. Herein, we summarize the application of contemporary tracers in gastric cancer surgery, including isosulfan blue, methylene blue, patent blue, indocyanine green, carbon particles, and radioactive tracers. Their mechanisms, administration methods, detection efficiency, and challenges, as well as perspectives on them, are also outlined.
1. Introduction
With an estimated annual incidence of more than 100 million cases, gastric cancer (GC) is the fifth most frequent cause of cancer globally []. It is the fourth leading cause of cancer deaths for both sexes, accounting for 7.7% of all malignancy fatalities [].
Nowadays, radical surgery is still the most effective treatment for GC. The most critical issues in radical GC surgery are thorough lymph node dissection and the determination of surgical margins []. Suitable acquisition of LNs is significantly connected to pathological staging and prognosis [,]. However, for most patients with early GC without LN metastases, biopsy of sentinel lymph nodes (SLNs) for the detection of metastases to determine extended or limited resection appears to be the most appropriate option []. Additionally, despite the widespread application of laparoscopy, it is difficult to distinguish the tumor site and identify resection lines due to the inability to palpate through the stomach wall [].
Tracers are useful for addressing the aforementioned issues during gastrectomies and lymphadenectomies. The application of blue dye, indocyanine green (ICG), carbon particles, and radioactive tracers in GC surgery has been explored. Through specific deposition in LNs or staining of tissue surrounding the tumor, the surgical target can be displayed more clearly. For more precise detection, dual tracers are implemented in surgery, in which the simultaneous application of blue dyes and radioactive tracers when harvesting SLNs is most frequently used [].
We aimed to include tracers that are being employed in clinical GC surgery. Their mechanisms of action, application methods, and clinical effects are summarized. Future perspectives are also offered in this review.
2. The Current Status of GC Surgery
GC is a carcinoma with a high propensity for LN metastasis. A total of 87.5% of patients with local recurrence after radical resection show manifestations as LN metastases []. Traditionally, extended LN resection (D2) has been considered a radical method for LN dissection in advanced gastric carcinoma. The number of detected LNs is closely related to pathologic staging and prognosis []. The eight edition of the classifications of the International Union against Cancer/American Joint Committee on Cancer recommended the dissection of more than 16 LNs for the exact TNM staging of GC, while Japanese Regulations on the Management of Gastric Cancer recommend that at least 15 LNs should be dissected [,]. According to the latest version of the German S3-Leitlinien, the number of LNs required for detection in a D2 lymphonodectomy is up to 25 []. However, for patients with early-stage GC without LN metastases, especially patients suffering from cT1N0 GCs smaller than 5 cm in size, D2 lymphadenectomy is redundant and can potentially adversely affect the prognosis [,,]. The concept of SLN biopsy has been put forward, recommending the biopsy of the first LN that receives lymphatic flow and in principle bears the greatest transfer risk to predict whether other LNs have metastasized and determine the follow-up operation plan []. This approach reduces patient injury and aids recovery. After further development, the notion of the sentinel lymphatic basin, where detected SLNs and the majority of metastatic LNs are located, was developed to overcome the complicated and multidirectional lymphatic drainage system and the high incidence of skip metastases in gastric cancer [,,]. Tracers implemented intraoperatively can effectively assist in LN detection as needed, whether to discover as many LNs of patients with advanced GC as possible or accurately identify SLNs of patients in the early stage []. Additionally, in a gastrectomy, complete resection with an appropriate margin is necessary. Safe proximal resection margins can improve curability and reduce recurrence []. According to the Japanese GC surgical standards, the resection margin ought to be at least 2 and 3–5 cm for patients suffering from early GC and advanced GC, respectively []. Due to the difficulty of touching the stomach wall, it is arduous to diagnose tumor location and define the resection lines during laparoscopic surgery, especially when a tumor is located in the upper third of the stomach [,].
Currently, several methods are employed for tumor margin recognition, such as metal clips and intraoperative endoscopy [,]. The time-consuming nature of the procedures, possible complications, and the need for additional personnel and equipment are bottlenecks for these methods. In this context, tracers have gained attention for their simplicity and low cost []. In the stomach, there is a complicated and multidirectional lymphatic system. The lymph from the stomach wall drains into lymphatic vessels arising in the mucosa, which subsequently drain into the peri-gastric lymphatic system spread along the main arteries of the stomach []. For non-selective tracers, proper particle size is the basis of tracing. Since the pore width between the capillary lymphatic cells is about 100–500 nm, which is much larger than that of the capillary endothelium, a tracer with suitable particle size injected around the tumor can selectively enter capillary lymphatic vessels and perform the role of lymphatic tracing []. Moreover, annexin A 1, sialyl-related antigen, and E-cadherin have been reported to be overexpressed in metastatic LNs []. Regrettably, no clinical tracer has yet exploited these molecules as targets to increase the accuracy of tracer targeting. Currently, blue dyes, ICG, carbon particles, and radioactive tracers are increasingly employed in GC surgery.
3. Tracers in GC Surgery
3.1. Blue Dyes
Blue dyes, including isosulfan blue, patent blue, and methylene blue, are extensively applied in SLN biopsies. They are popular due to their inexpensiveness, wide availability, and tractability []. They possess the capacity for lymphatic targeting owing to the binding of their sulfonic acid group to serum proteins [,]. This characteristic ensures that they have a suitable particle size to pass through lymphatic vessels while trapped in LNs []. However, methylene blue, as a substitute for these dyes, does not bind to plasma proteins because of the lack of sulfonic acid groups []. Its LN specificity has therefore been revealed to be inferior []. Through visual inspection without any special equipment, the tumor borders and the flow of lymphatic vessels deriving from the GC site can be monitored intraoperatively after peritumoral injections (Figure 1). LNs are thus visualized, which can be beneficial to SLN harvesting or extensive LN dissection, as needed. Appropriate waiting time is required between injection and detection, as SLN staining takes approximately 5 to 10 min, and second-echelon LNs will be stained as time progresses []. These dyes still have several drawbacks, such as difficulty in quantification and potential allergic reactions []. The rapid transit of dyes through lymphatic vessels after injection, as well as the interference of thick adipose tissue, can possibly allow SLNs to be omitted or multiplied [].
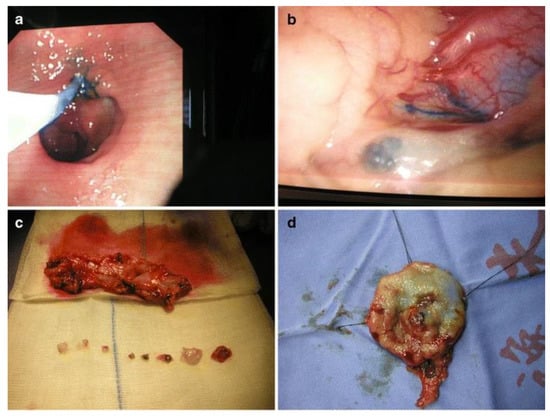
Figure 1.
Procedure for laparoscopic local resection with sentinel node biopsy. (a) Isosulfan blue was injected into the peritumoral submucosal layer after the lesion was localized through an intraoperative endoscopy. (b) Within 5 min of dye injection, lymphatic flow from the lesion was visible. (c) Sentinel nodes were isolated, while perigastric tissue was extracted. (d) Local resection lines were marked at the four edges of the resection margin. Reproduced with permission []. Copyright 2008, Springer Nature.
3.1.1. Isosulfan Blue
As a triphenylmethane-based rosaniline dye, isosulfan blue was the first dye approved by the Food and Drug Administration (FDA) for lymphangiography due to its superior properties and low number of adverse reactions []. Endoscopic submucosal injection or direct serosa injection after laparotomy are the major methods for its clinical application []. One milliliter of one-percent isosulfan blue is implemented as a mainstream dose for imaging, which is usually injected at four spots around the tumor submucosally [,]. Different injection sites are accompanied by distinct imaging times. If the injection is subserosal, 5 min ought to be enough for it to flow into the SLNs, while the waiting time varies from 5 min to 15 min if a submucosal injection is performed [,,,,]. The detection rate for isosulfan blue is as high as 90% or even 100%, with the average SLN number around three and the average number of dissected LNs being over 25 [,,]. Possessing a positive predictive value of over 72%, a negative predictive value of around 87%, and a sensitivity of approximately 97%, isosulfan blue exhibits great potential as a tracer [,,]. Nevertheless, the false-negative rate remains high, most likely as a consequence of the more convoluted lymph drainage or the disconnection of lymphatic vessels resulting from tumors larger than the T2 stage []. The indications of isosulfan blue need to be further explored.
3.1.2. Patent Blue
Patent blue possesses the capacity to label tumors in situ and aid in the identification of LNs. The commonly utilized administration is an injection of 0.2 mL of 2% patent blue solution into four quadrants surrounding the tumor through an intraoperative gastroendoscopy [,,]. Higher doses are required in subserosal or intramuscular approaches [,]. As reported, the dye is visible on the stomach serosa surface immediately after submucosal injection []. It takes 1 to 16 min to observe SLNs after subserous injection []. Stained LNs are still plainly visible until two hours later []. The detection rate is between 76.3% and 97.4% [,]. The particularly low detection rate in the study conducted by Rabin et al. [] was probably due to the inclusion of too many patients with T3 tumors. The dosing method may have been another influencing factor. Although a small sample study illustrated that there existed no significant difference between submucosal and subserosal injections [], studies adopting subserosal injections yielded worse data []. Along with LN detection, patent blue has been applied to ensure proximal surgical margins. With the guidance of clips placed using preoperative gastroendoscopy, patent blue dissolved in sodium hyaluronate has been injected submucosally during surgery, which guaranteed negative proximal resection, although some margins were less than the estimated length [].
3.1.3. Methylene Blue
An alternative to isosulfan blue, methylene blue is more readily available []. The methods and the doses of injections vary across studies. Intraoperative injection of diluted methylene blue solution into the submucosa, subserosa, or left and right gastric arteries has been attempted [,,]. The submucosal injected methylene blue reached SLNs within 5 to 10 min []. SLN detection rates were high for each mode of administration, with a minimum of 87% []. However, the harvesting effect was relatively low in malignancies diagnosed as pT3 or pT4, partially due to the disordered lymphatic drainage [,]. It has been reported that the average number of LNs detected with the assistance of methylene blue was 36 []. It was especially effective for the identification of small LNs smaller than 6 mm in diameter []. Furthermore, methylene blue has been applied in picking out LNs after radical lymphadenectomy for more accurate N staging [].
3.2. ICG
Analogous to blue dyes, ICG tends to attach to plasma proteins or bilirubin and is instantly absorbed by lymphatic vessels [,]. In addition to visual inspection, ICG has the capacity to facilitate infrared and fluorescence observation, making it a novel favorite among tracers. ICG, as a fluorescent dye with an excitation wavelength of around 800 nm, can shift its maximum absorption wavelength to 805 nm if combined with plasma proteins []. When exposed to light approaching the maximum absorption wavelength, the ICG-injected region absorbs the light and darkens, while the background portions reflect light and become brighter []. Tissues stained by ICG, even with a depth up to 5 mm, can hence be observed under infrared light []. To improve the visibility of the dye within human tissue, near-infrared fluorescent imaging (NIFI), infrared ray electronic endoscopy (IREE), and infrared ray laparoscopic system (IRLS) devices have been developed, which are compatible with minimally invasive surgery [,,]. Furthermore, ICG exhibits a maximum fluorescence wavelength of 830 nm after photo-stimulation. Novel fluorescence imaging (FI) systems, including the Hyper Eye Medical System, D-light P System, and PINPOINT Endoscopic FI System, have been exploited to receive light around the wavelength of maximum fluorescence under conventional white light [,]. The observation results for intra- and post-operative fluorescence are illustrated in Figure 2. There is consensus that the observation efficiency of ICG using infrared light is much higher than that of ordinary light []. IREE and IRLS appeared to be more sensitive than FI systems [], and IREE increased the sensitivity and recognition rate compared to NIFI [].
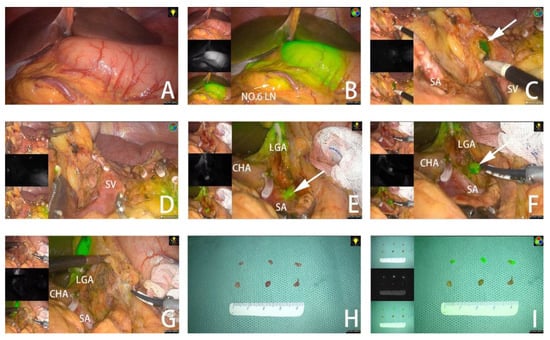
Figure 2.
(A,B) Tumor observed under white light in fluorescent mode. (C) Fluorescent no. 10 LNs detected in fluorescent mode. (D) No remnant no. 10 LNs are found after dissection. (E) Fluorescent no. 11P LNs adjacent to splenic vessels. (F) No. 11P LNs separated from blood vessels. (G) No remnant No. 11P LNs are found after dissection. (H) LNs dissected from the specimen under white light. (I) LNs dissected from the specimen in fluorescent mode. The arrow points to the fluorescent LN. SA, spleen artery; SV, spleen vein; CHA, common hepatic artery; LGA, left gastric artery. Reproduced with permission []. Copyright 2022, Frontiers Media.
ICG is favored because of its hypoallergenic potential, deep detection depth, high sensitivity, and stable signal []. The dose and timing of administration have been the subject of several scientific investigations. In recent research, submucosal injections at concentrations of 0.625 or 1.25 mg/mL were the most popular [,,,]. According to subgroup analysis, surgeries utilizing ICG with a concentration of 0.5 or 0.05 mg/mL had a higher pooled sensitivity than the 5 mg/mL subgroup []. Furthermore, the dosage depended on the equipment due to their different sensitivity to light. With the upgrade from the da Vinci Si to the more advanced da Vinci Xi or the PINPOINT system, the concentration of ICG has been halved as well []. When it comes to ICG at concentrations of 0.625 or 1.25 mg/mL, submucosal administration in four quadrants around the tumor, with 0.5–0.6 mL in each quadrant, is the most common approach [,,,,]. Dosing from the serosal surface [,], along the greater and lesser curvatures of the stomach [], or submucosally with gastrotomy incision [] have been exploited. Chen et al. [] conducted research to investigate the difference between submucosal and subserosal administration. There was little difference except for the lower cost and higher satisfaction scores in the subserosal approach group since no additional endoscopy was required. A gap of at least 20 min between drug administration and lymphadenectomy appeared to be more effective than immediate imaging []. The longest reported waiting time was up to three days, without increasing the dosage [,]. In general, there is still no unified criterion for dosage, which needs to be further standardized.
With the assistance of ICG, the SLN detection rate was able to reach 100% in several studies [,,]. Regardless of the accuracy, sensitivity, specificity, positive predictive value, and negative predictive value, most rates were reported to be greater than 90% [,,]. The accuracy and specificity were determined by clinical neoplasm staging [,]. Tajima et al. [] found that the mean number of detected SLNs after injecting 1–3 days before surgery averaged more than 9, which was distinguished from averages of roughly 3 to 5 reported in other studies [,,,]. The small hydrodynamic diameter of ICG was possibly responsible for this finding, which led to the migration of ICG to second-tier nodes []. A nanocolloid-adsorbed ICG has been developed to increase its hydrodynamic diameter []. It has been pointed out that the application of ICG during gastrectomy and lymphadenectomy increased the total number of detected LNs, shortened the operation time, reduced blood loss, and lowered noncompliance [,,,,]. Even if produced scarring after endoscopic submucosal dissection, the use of ICG still yielded positive effects []. However, it remains controversial whether ICG can benefit LN dissection after neoadjuvant chemotherapy-induced local histological changes [,]. Since fluorescence can be quantitatively analyzed to reduce human subjective error, research has been carried out to determine appropriate fluorescence values for SLN detection []. As expected, the fluorescence intensity of ICG-positive LNs was stronger compared to ICG-negative ones []. The threshold for SLN detection ought to be 10% of maximum signal intensity []. Nevertheless, in a prospective study, the false-negative rate was up to 46% following the preliminary study and remained at 14% even after additional green-stained node sections were examined through paraffin sectioning []. Visual inspection of the LNs may have contributed to this result. Obesity may lead to failed LN identification and prolonged operation times [,,]. It has also been found that the staining appeared to be less associated with metastasis [].
Preoperative submucosal injection of ICG has been employed in resection margin determination. ICG imagining brought about shorter operation times, less operative hemorrhaging, reduced hospital stays, and fewer positive margins [,,]. More interestingly, resin-conjugated fluorescent indocyanine green-equipped endoscopic marking clips have been developed to mark margins []. ICG has also been used in real-time intraoperative vascular monitoring [,].
3.3. Carbon Particles
By blackening the serosa and staining LNs, carbon particles have been widely utilized for tumor localization and LN detection (Figure 3) [,]. The lymphatic targeting mechanism of carbon particles differs from the above-mentioned tracers. With an average diameter of 150 nm, carbon nanoparticle suspension injection (CNSI) tends to be administered through lymphatic capillaries rather than capillaries because the lymphatic capillary intercellular space is between 100 and 500 nm []. Furthermore, because of its diameter, CNSI engulfed by macrophages and aggregated in LNs migrates slowly, remaining in the SLNs for long enough without moving to higher-tier nodes [].
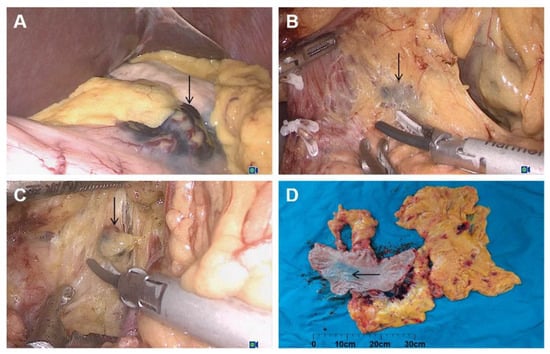
Figure 3.
Carbon nanoparticle-labeling helped to find the lesion site (gastric angle) (A) and in draining lymph nodes (B,C) in laparoscopic radical gastrectomy. (A) Gastric angular lesions labeled with carbon nanoparticles; (B) black staining of lymph node no. 8a; (C) black staining of lymph node no. 11p; (D) gross specimen. Reproduced with permission []. Copyright 2021, Elsevier.
Clinically implemented carbon particles have undergone a multi-stage transition from Indian inks and activated carbon to the latest CNSI. They are frequently utilized due to their ease of application, low cost, and safety []. Indian ink and activated carbon have been adopted in the clinical determination of surgical margins. It has been revealed that injecting activated carbon into the muscle layer or Indian ink into the submucosal layer before surgery ensured the identification of the location of the tumor on the serosal surface during surgery [,,]. Injection times from 1 to 14 days before operations could be selected []. Although all margins were guaranteed to be pathologically negative, proximal resection margins were shorter than expected in 21% of patients, especially in patients with poorly differentiated or signet ring cell lesions []. Intraoperative endoscopy thus remains the most accurate approach to confirm resection margins, and defining tumor boundaries with carbon particles is still a long way off.
CNSI is the most suitable type of carbon particle for LN detection. Appropriate submucosal administration times are reported to range from 6 h to 2 days [,]. A waiting time of less than 6 h might lead to poor imaging effects, while injecting 1 to 2 days before surgery showed similar efficiencies []. For the injection method, CNSI (1 mL: 50 mg) is usually dosed at four points submucosally or at five points subserosally [,]. The no. 12b LN is another target spot for administration to trace para-aortic LNs []. It has been shown that CNSI-assisted lymphadenectomy possessed the advantages of shorter operation time, less bleeding, and more detected LNs [,]. In comparison to the groups adopting methylene blue or ICG, the number of LNs found using CNSI was considerably higher [,]. Additionally, CNSI has been found to be beneficial for identifying positive metastases, synchronous multiple GC, and micro-LNs [,,]. In the study conducted by Yang et al. [], the influence of neoadjuvant chemotherapy on the accuracy of N staging was investigated. Injecting CNSI before neoadjuvant chemotherapy favored the diffusion of CNSI in LNs, which could theoretically improve staining and help in tracing as many LNs as possible. To conclude, carbon particles are excellent clinical tracers with promising development prospects and have been extensively studied.
3.4. Radioactive Tracers
Many species of radioactive tracers have been employed in clinical LN tracing. Technetium-99m (99mTc) antimony sulfur colloid, 99mTc tin colloid, and 99mTc sulfur colloid are preferentially selected []. Applications of Indium-111 penetreotide and positron-emitting gallium-68-DOTA-peptides in surgeries of gastroenteropancreatic neuroendocrine tumors have also been reported []. Similar to carbon nanoparticles, radioactive tracers tend to migrate to the SLNs within 2 h and stay there for more than 20 h thanks to the phagocytosis of macrophages []. As a metastable isomer, 99mTc has a half-life of about 6 h and emits rays of 140 keV in LNs []. Signals are identified by gamma probes for LN detection. Due to the large particle size of the tin colloid, which allows a longer staying time inside SLNs to reduce the false-negative rate, it has been well-received []. However, the 99mTc sulfur colloid seems to be more effective than the 99mTc tin colloid []. The objective measurement of radioactivity, the ability to identify SLNs even in dense intraperitoneal adipose tissue, and the comparatively lengthy LN retention time are benefits of radioactive tracers []. Drawbacks, such as expensiveness, radioactivity, lack of visual examination, challenging lymphatic vessel and pool identification, and strong background scattering, interfere with their application [,].
The 99mTc radioisotope tracers were empirically injected submucosally into the surroundings of a lesion 1 day before surgery []. Injecting 2 mL of radioactive tracers into four quadrants is a common method [,,]. There are also application examples of intraoperative injections [,]. Commonly, if the radioactivity level of an LN is ten times higher than the background, it is defined as a hot LN []. The detection rate, sensitivity, and specificity of LN tracing using radioactive substances alone have been reported to be higher than 90% [,]. There are very few cases of surgical tracing with radioactive tracers alone. Radioisotopes are typically utilized in conjunction with the other dyes, such as ICG or blue dyes, which is considered the gold standard for SLN detection [,].
3.5. Dual Tracers
In order to solve the problem of lymphatic vessels not being revealed by the radiotracer and the false positives caused by the low molecular weight of dyes, two tracers are often applied in one operation. Injections of radioactive tracers are usually performed one day before surgeries. After a 15 min interval following intraoperative submucosal injections of blue dye or ICG, SLNs are detected with the naked eye and gamma-ray detectors [,,]. Despite the use of ICG, its properties cannot be fully exploited in the absence of near-infrared or fluorescence imaging, which might account for the low efficiency of single-tracer detection in certain studies. The combination of the NIFI properties of ICG with radioisotope detection is only mentioned in one trial protocol []. In general, the application of dual tracers improves data describing LN detection since the two complement each another. It was pointed out in one study that the number of hot (high radioactive signal) or dyed nodes was about 2.5 times that of hot and dyed nodes []. The detection rate, sensitivity, and accuracy were 91.2%, 100%, and 100% separately, while these data were 73.5%, 72.2, and 94% in the dye group and 80.9%, 83.3%, and 98.2% in the radioisotope group []. The accuracy became even higher with the usage of sentinel lymphatic basin detection since some patients showed only lymphatic duct staining, and abdominal fat and the primary tumor also had influences on LN identification [,]. With false-negative rates ranging from 0% to over 10%, scientists have attempted to explore the causes of this phenomenon [,,,,]. The stage of the tumor appears to be its main predictor [,]. Furthermore, the radioisotope count was proved to be associated with LN metastasis since the radioisotope counts for metastatic SLNs, lymphatic stations, and basins were substantially higher than those without metastasis [].
In addition to conventional combined usage, patent blue and ICG are combined for dual tracing []. SLNs were harvested 3 to 5 min after subserosal injection of patent blue and ICG at three points, respectively. It was found that the false-negative rate was much lower than that of single-tracer methods. In our institution, the combination of ICG and CNSI is routinely performed for lymph node dual tracing in gastric cancer surgery. To take full advantage of the properties of CNSI for tumor localization and ICG for LN tracking, our institution has attempted to conduct submucosal CNSI plus subserosal ICG-guided laparoscopic gastrectomy, which ensures more accurate tumor identification and enhanced LN detection number.
3.6. Novel Tracers
Regrettably, the primary mechanism of LN localization in traditional tracers depends on their physical properties. Tracers with specific tumor-targeting effects are likely to play a better role. There is one potential tumor-specific tracer, 5-aminolevulinic acid (5-ALA), that is converted to protoporphyrin IX and accumulates in tumors because of changes in enzyme activity in cancer cells []. Cumulated protoporphyrin IX thus emits red fluorescence under blue light excitation []. Unfortunately, 5-ALA can only be applied for postoperative detection because of the poor penetration of blue light []. A carcinoembryonic antigen-targeted fluorescent probe has also been developed for clinical trials [].
With the advance of nanomedicine, multiple nanoparticles have been utilized in gastric carcinoma diagnosis and treatment preclinically, which is another potential development direction []. Through exploitation of the particular combination properties of the Arg-Gly-Asp (RGD) sequence and of integrin overexpressed in gastric cancer cells, ICG has been transported to tumor locations for more specific imaging [,]. Cyclic RGD has been demonstrated to direct the precise uptake of nanomedicines by metastatic gastric cancer cells in SLNs as well []. Tumor-specific markers, such as HER-2, can also be selected as targets []. However, there is still a long way to go for the widespread clinical application of nanomedicines.
4. Conclusions and Future Perspectives
The clinical application of tracers has the potential to alter the way that GC surgery is conducted, whether in resection line identification or LN detection. With the widespread use of intraoperative tracers, the applications and indications of minimally invasive surgical approaches may be greatly broadened and improved []. Allergic reactions appear to be the most common adverse reactions to tracers. Even so, the reported incidence of blue dye anaphylaxis is only 0.07% to 2.7% []. Few fatalities have been reported in allergy sufferers and certain precautions can be taken to prevent allergic responses as well. The allergy rate for new tracers, such as ICG, is lower. In general, the safety of intraoperative tracers is assumed to be guaranteed. Despite the existence of different tracing and imaging principles, diverse traces have shown excellent effects on surgical navigation and huge potential. The advantages and disadvantages of each tracer are shown in Table 1.

Table 1.
The pros and cons of different tracers.
Nevertheless, the exploration of clinical tracers still has a long way to go. There are no guidelines clearly specifying the exact use methods, indications, and contraindications of any tracer. Only the Chinese clinical guidelines mention the possible application prospects of tracers []. Based on data from several clinical studies, we can only roughly conclude that excessive fat, preoperative chemotherapy, and advanced tumor staging seem to be unfavorable to the functions of tracers [,,,]. Numerous limitations remain to be addressed. Firstly, there are still common problems, such as the high false-negative rate and shorter-than-expected surgical margins, during tracer application. Moreover, it is not feasible to detect LNs in individuals with advanced tumor stages and obesity. As surgical tracer usage is still in its infancy, more attempts are required to improve tracer experimental skills and clarify indications. Secondly, most of the articles covered in this review were conducted by different surgical teams. The data obtained probably vary due to the diverse methods of utilizing tracers and the discrepant details of the gastrectomies and lymphadenectomies. Therefore, large-scale, prospective, multicenter clinical studies are required to quantify the exact effects of each tracer. Furthermore, the dual-tracer approach seems to be the preferred choice nowadays due to its higher efficiency compared to single-tracer techniques. Rarely have attempts been put into practice, apart from the simultaneous use of radioisotopes and blue dyes or ICG. Additional drug delivery combinations or novel dosing methods could be explored.
In conclusion, tracers have been proven to be safe and effective. Through the refinement of traditional tracer use and the application of novel tracers, gastric cancer surgery may become more refined, reducing patient pain and improving prognosis.
Author Contributions
X.Z. collected data from published studies. Z.L. wrote the manuscript draft. S.A. aided in manuscript writing and finalized the manuscript. X.L. and S.L. discussed the review content and critically reviewed the manuscript draft. W.G. conceptualized the current review. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China (82172645), Natural Science Foundation of Jiangsu Province for Outstanding Young Scholars (BK20200052), Key Research and Development Program of Jiangsu Province (BE2022667, BE2022753), Key Project of Nanjing Health Commission (ZKX21013), and Clinical Trials from the Affiliated Drum Tower Hospital Medical School of Nanjing University (2021-LCYJ-MS-09).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Xing, J.; Xu, K.; Yuan, P.; Cui, M.; Zhang, C.; Yang, H.; Yao, Z.; Zhang, N.; Tan, F.; et al. Application of Near-Infrared Fluorescence Imaging with Indocyanine Green in Totally Laparoscopic Distal Gastrectomy. J. Gastric Cancer 2020, 20, 290–299. [Google Scholar] [CrossRef]
- Puccetti, F.; Cinelli, L.; Genova, L.; Battaglia, S.; Barbieri, L.A.; Treppiedi, E.; Cossu, A.; Elmore, U.; Rosati, R. Applicative Limitations of Indocyanine Green Fluorescence Assistance to Laparoscopic Lymph Node Dissection in Total Gastrectomy for Cancer. Ann. Surg. Oncol. 2022. [Google Scholar] [CrossRef]
- Lu, X.; Liu, S.; Xia, X.; Sun, F.; Liu, Z.; Wang, J.; Li, X.; Yang, Z.; Kang, X.; Ai, S.; et al. The short-term and long-term outcomes of indocyanine green tracer-guided laparoscopic radical gastrectomy in patients with gastric cancer. World J. Surg. Oncol. 2021, 19, 271. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Pan, M.; Chen, B. A Systematic Review and Meta-Analysis of Sentinel Lymph Node Biopsy in Gastric Cancer, an Optimization of Imaging Protocol for Tracer Mapping. World J. Surg. 2021, 45, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.; Kanda, M.; Funasaka, K.; Miyahara, R.; Murotani, K.; Tanaka, Y.; Takeda, S.; Kobayashi, D.; Hirooka, Y.; Fujiwara, M.; et al. Detection of indocyanine green fluorescence to determine tumor location during laparoscopic gastrectomy for gastric cancer: Results of a prospective study. Asian J. Endosc. Surg. 2020, 13, 160–167. [Google Scholar] [CrossRef]
- Matsuda, S.; Irino, T.; Kawakubo, H.; Takeuchi, H.; Kitagawa, Y. Current status and challenges in sentinel node navigation surgery for early gastric cancer. Chin. J. Cancer Res. 2021, 33, 150–158. [Google Scholar] [CrossRef]
- Giuliani, A.; Miccini, M.; Basso, L. Extent of lymphadenectomy and perioperative therapies: Two open issues in gastric cancer. World J. Gastroenterol. 2014, 20, 3889–3904. [Google Scholar] [CrossRef]
- In, H.; Ravetch, E.; Langdon-Embry, M.; Palis, B.; Ajani, J.A.; Hofstetter, W.L.; Kelsen, D.P.; Sano, T. The newly proposed clinical and post-neoadjuvant treatment staging classifications for gastric adenocarcinoma for the American Joint Committee on Cancer (AJCC) staging. Gastric Cancer 2018, 21, 1–9. [Google Scholar] [CrossRef]
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017, 20, 1–19. [Google Scholar] [CrossRef]
- Moehler, M.; Al-Batran, S.E.; Andus, T.; Arends, J.; Arnold, D.; Baretton, G.; Bornschein, J.; Budach, W.; Daum, S.; Dietrich, C.; et al. S3-Leitlinie Magenkarzinom – Diagnostik und Therapie der Adenokarzinome des Magens und des ösophagogastralen Übergangs – Langversion 2.0 – August 2019. AWMF-Registernummer: 032/009OL. Z. Gastroenterol. 2019, 57, 1517–1632. [Google Scholar] [CrossRef] [PubMed]
- Gotoda, T.; Yanagisawa, A.; Sasako, M.; Ono, H.; Nakanishi, Y.; Shimoda, T.; Kato, Y. Incidence of lymph node metastasis from early gastric cancer: Estimation with a large number of cases at two large centers. Gastric Cancer 2000, 3, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Bu, Z. Sentinel lymph node detection for gastric cancer: Promise or pitfall? Surg. Oncol. 2020, 33, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kinami, S.; Saito, H.; Takamura, H. Significance of Lymph Node Metastasis in the Treatment of Gastric Cancer and Current Challenges in Determining the Extent of Metastasis. Front. Oncol. 2021, 11, 806162. [Google Scholar] [CrossRef]
- Hiramatsu, Y.; Kikuchi, H.; Takeuchi, H. Function-Preserving Gastrectomy for Early Gastric Cancer. Cancers 2021, 13, 6223. [Google Scholar] [CrossRef] [PubMed]
- Miwa, K.; Kinami, S.; Taniguchi, K.; Fushida, S.; Fujimura, T.; Nonomura, A. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br. J. Surg. 2003, 90, 178–182. [Google Scholar] [CrossRef]
- Mitsumori, N.; Nimura, H.; Takahashi, N.; Kawamura, M.; Aoki, H.; Shida, A.; Omura, N.; Yanaga, K. Sentinel lymph node navigation surgery for early stage gastric cancer. World J. Gastroenterol. 2014, 20, 5685–5693. [Google Scholar] [CrossRef]
- Lee, S.E.; Lee, J.H.; Ryu, K.W.; Cho, S.J.; Lee, J.Y.; Kim, C.G.; Choi, I.J.; Kook, M.C.; Nam, B.H.; Park, S.R.; et al. Sentinel node mapping and skip metastases in patients with early gastric cancer. Ann. Surg. Oncol. 2009, 16, 603–608. [Google Scholar] [CrossRef]
- Tian, Y.; Yang, P.; Lin, Y.; Hu, Y.; Deng, H.; Ma, W.; Guo, H.; Liu, Y.; Zhang, Z.; Ding, P.; et al. Assessment of Carbon Nanoparticle Suspension Lymphography-Guided Distal Gastrectomy for Gastric Cancer. JAMA Netw. Open 2022, 5, e227739. [Google Scholar] [CrossRef]
- Ohe, H.; Lee, W.Y.; Hong, S.W.; Chang, Y.G.; Lee, B. Prognostic value of the distance of proximal resection margin in patients who have undergone curative gastric cancer surgery. World J. Surg. Oncol. 2014, 12, 296. [Google Scholar] [CrossRef]
- Nakagawa, M.; Ehara, K.; Ueno, M.; Tanaka, T.; Kaida, S.; Udagawa, H. Accurate, safe, and rapid method of intraoperative tumor identification for totally laparoscopic distal gastrectomy: Injection of mixed fluid of sodium hyaluronate and patent blue. Surg. Endosc. 2014, 28, 1371–1375. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.S.; Yook, J.H.; Kim, B.S.; Jung, H.Y. A simplified technique for tumor localization using preoperative endoscopic clipping and radio-opaque markers during totally laparoscopic gastrectomy. Am. Surg. 2014, 80, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.I.; Hyung, W.J.; Lee, C.R.; Lim, J.S.; An, J.Y.; Cheong, J.H.; Choi, S.H.; Noh, S.H. Intraoperative portable abdominal radiograph for tumor localization: A simple and accurate method for laparoscopic gastrectomy. Surg. Endosc. 2011, 25, 958–963. [Google Scholar] [CrossRef]
- Lirosi, M.C.; Biondi, A.; Ricci, R. Surgical anatomy of gastric lymphatic drainage. Transl. Gastroenterol. Hepatol. 2017, 2, 14. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Tian, Y.; Tan, B.; Ding, P.; Guo, H.; Liu, Y.; Zhang, Z.; Li, Y.; Zhao, Q. Clinical application of nano-carbon to improve the accuracy of lymph node staging in patients with advanced gastric cancer receiving neoadjuvant chemotherapy: A prospective randomized controlled trial. J. Gastrointest. Oncol. 2021, 12, 2052–2060. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.; Hu, X.; Wei, P.; Shan, G. Molecular background of the regional lymph node metastasis of gastric cancer. Oncol. Lett. 2018, 15, 3409–3414. [Google Scholar] [CrossRef] [PubMed]
- Kinami, S.; Kosaka, T. Laparoscopic sentinel node navigation surgery for early gastric cancer. Transl. Gastroenterol. Hepatol. 2017, 2, 42. [Google Scholar] [CrossRef]
- Tsopelas, C.; Sutton, R. Why certain dyes are useful for localizing the sentinel lymph node. J. Nucl. Med. 2002, 43, 1377–1382. [Google Scholar]
- Masannat, Y.; Shenoy, H.; Speirs, V.; Hanby, A.; Horgan, K. Properties and characteristics of the dyes injected to assist axillary sentinel node localization in breast surgery. Eur. J. Surg. Oncol. 2006, 32, 381–384. [Google Scholar] [CrossRef]
- Varghese, P.; Abdel-Rahman, A.T.; Akberali, S.; Mostafa, A.; Gattuso, J.M.; Carpenter, R. Methylene Blue Dye—A Safe and Effective Alternative for Sentinel Lymph Node Localization. Breast J. 2008, 14, 61–67. [Google Scholar] [CrossRef]
- Wong, J.H.; Cagle, L.A.; Morton, D.L. Lymphatic drainage of skin to a sentinel lymph node in a feline model. Ann. Surg. 1991, 214, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Papadia, A.; Gasparri, M.L.; Buda, A.; Mueller, M.D. Sentinel lymph node mapping in endometrial cancer: Comparison of fluorescence dye with traditional radiocolloid and blue. J. Cancer Res. Clin. Oncol. 2017, 143, 2039–2048. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.B.; Shen, J.G.; Dong, L.F.; Xu, C.Y.; Chen, W.J.; Xie, S.D.; Song, X.Y.; Dai, N.; Yuan, X.M. Laparoscopic local resection based on sentinel node evaluation for early gastric cancer: A preliminary report. J. Gastrointest. Surg. 2008, 12, 1359–1363. [Google Scholar] [CrossRef]
- Bézu, C.; Coutant, C.; Salengro, A.; Daraï, E.; Rouzier, R.; Uzan, S. Anaphylactic response to blue dye during sentinel lymph node biopsy. Surg. Oncol. 2011, 20, e55–e59. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Ryu, K.W.; Kim, C.G.; Kim, S.K.; Choi, I.J.; Kim, Y.W.; Chang, H.J.; Bae, J.M.; Hong, E.K. Comparative study of the subserosal versus submucosal dye injection method for sentinel node biopsy in gastric cancer. Eur. J. Surg. Oncol. 2005, 31, 965–968. [Google Scholar] [CrossRef] [PubMed]
- Isozaki, H.; Kimura, T.; Tanaka, N.; Satoh, K.; Matsumoto, S.; Ninomiya, M.; Ohsaki, T.; Mori, M. An assessment of the feasibility of sentinel lymph node-guided surgery for gastric cancer. Gastric Cancer 2004, 7, 149–153. [Google Scholar] [CrossRef]
- Song, X.; Wang, L.; Chen, W.; Pan, T.; Zhu, H.; Xu, J.; Jin, M.; Finley, R.K., 3rd; Wu, J. Lymphatic mapping and sentinel node biopsy in gastric cancer. Am. J. Surg. 2004, 187, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Ryu, K.W.; Lee, J.H.; Kim, H.S.; Kim, Y.W.; Choi, I.J.; Bae, J.M. Prediction of lymph nodes metastasis by sentinel node biopsy in gastric cancer. Eur. J. Surg. Oncol. 2003, 29, 895–899. [Google Scholar] [CrossRef]
- Osaka, H.; Yashiro, M.; Sawada, T.; Katsuragi, K.; Hirakawa, K. Is a lymph node detected by the dye-guided method a true sentinel node in gastric cancer? Clin. Cancer Res. 2004, 10, 6912–6918. [Google Scholar] [CrossRef][Green Version]
- Ishizaki, M.; Kurita, A.; Kubo, Y.; Takashima, S.; Nishina, T.; Nishimura, E. Evaluation of sentinel node identification with isosulfan blue in gastric cancer. Eur. J. Surg. Oncol. 2006, 32, 191–196. [Google Scholar] [CrossRef]
- Saikawa, Y.; Otani, Y.; Kitagawa, Y.; Yoshida, M.; Wada, N.; Kubota, T.; Kumai, K.; Sugino, Y.; Mukai, M.; Kameyama, K.; et al. Interim results of sentinel node biopsy during laparoscopic gastrectomy: Possible role in function-preserving surgery for early cancer. World J. Surg. 2006, 30, 1962–1968. [Google Scholar] [CrossRef] [PubMed]
- Miyake, K.; Seshimo, A.; Kameoka, S. Assessment of lymph node micrometastasis in early gastric cancer in relation to sentinel nodes. Gastric Cancer 2006, 9, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Tonouchi, H.; Mohri, Y.; Tanaka, K.; Konishi, N.; Ohmori, Y.; Kobayashi, M.; Watanabe, Y.; Matsumura, K.; Takeda, K.; Kusunoki, M. Lymphatic mapping and sentinel node biopsy during laparoscopic gastrectomy for early cancer. Dig. Surg. 2003, 20, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Tonouchi, H.; Mohri, Y.; Tanaka, K.; Kobayashi, M.; Ohmori, Y.; Kusunoki, M. Laparoscopic lymphatic mapping and sentinel node biopsies for early-stage gastric cancer: The cause of false negativity. World J. Surg. 2005, 29, 418–421. [Google Scholar] [CrossRef]
- Rabin, I.; Chikman, B.; Lavy, R.; Poluksht, N.; Halpern, Z.; Wassermann, I.; Gold-Deutch, R.; Sandbank, J.; Halevy, A. The accuracy of sentinel node mapping according to T stage in patients with gastric cancer. Gastric Cancer 2010, 13, 30–35. [Google Scholar] [CrossRef]
- Cozzaglio, L.; Bottura, R.; Di Rocco, M.; Gennari, L.; Doci, R. Sentinel lymph node biopsy in gastric cancer: Possible applications and limits. Eur. J. Surg. Oncol. 2011, 37, 55–59. [Google Scholar] [CrossRef]
- Tóth, D.; Kincses, Z.; Plósz, J.; Török, M.; Kovács, I.; Kiss, C.; Damjanovich, L. Value of sentinel lymph node mapping using a blue dye-only method in gastric cancer: A single-center experience from North-East Hungary. Gastric Cancer 2011, 14, 360–364. [Google Scholar] [CrossRef]
- Rino, Y.; Takanashi, Y.; Harada, H.; Ashida, A.; Saeki, H.; Yukawa, N.; Kanari, M.; Satoh, T.; Yamamoto, N.; Yamada, R.; et al. Technique and assessment of sentinel lymph node biopsy usefulness in laparoscopy-assisted distal gastrectomy. Surg. Endosc. 2006, 20, 1887–1891. [Google Scholar] [CrossRef]
- Thevarajah, S.; Huston, T.L.; Simmons, R.M. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am. J. Surg. 2005, 189, 236–239. [Google Scholar] [CrossRef]
- Märkl, B.; Moldovan, A.I.; Jähnig, H.; Cacchi, C.; Spatz, H.; Anthuber, M.; Oruzio, D.V.; Kretsinger, H.; Arnholdt, H.M. Combination of ex vivo sentinel lymph node mapping and methylene blue-assisted lymph node dissection in gastric cancer: A prospective and randomized study. Ann. Surg. Oncol. 2011, 18, 1860–1868. [Google Scholar] [CrossRef]
- Bara, T., Jr.; Gurzu, S.; Jung, I.; Borz, C.; Banias, L.; Bara, T. Sentinel node biospy using intravital blue dye: An useful technique for identification of skip metastases in gastric cancer. Medicine 2019, 98, e14951. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.L.; Lisbona, R.; Sorial, R.; Siblini, A.; Ferri, L.E. Sentinel Lymph Node Sampling for Early Gastric Cancer-Preliminary Results of A North American Prospective Study. J. Gastrointest. Surg. 2019, 23, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, T.; Yoshikawa, T.; Morita, S.; Shirai, J.; Fujikawa, H.; Iwasaki, K.; Hayashi, T.; Ogata, T.; Cho, H.; Yukawa, N.; et al. Methylene blue-assisted technique for harvesting lymph nodes after radical surgery for gastric cancer: A prospective randomized phase III study. BMC Cancer 2014, 14, 155. [Google Scholar] [CrossRef] [PubMed]
- Thongvitokomarn, S.; Polchai, N. Indocyanine Green Fluorescence Versus Blue Dye or Radioisotope Regarding Detection Rate of Sentinel Lymph Node Biopsy and Nodes Removed in Breast Cancer: A Systematic Review and Meta-Analysis. Asian Pac. J. Cancer Prev. 2020, 21, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Knospe, L.; Gockel, I.; Jansen-Winkeln, B.; Thieme, R.; Niebisch, S.; Moulla, Y.; Stelzner, S.; Lyros, O.; Diana, M.; Marescaux, J.; et al. New Intraoperative Imaging Tools and Image-Guided Surgery in Gastric Cancer Surgery. Diagnostics 2022, 12, 507. [Google Scholar] [CrossRef]
- Takahashi, N.; Nimura, H.; Fujita, T.; Yamashita, S.; Mitsumori, N.; Yanaga, K. Quantitative assessment of visual estimation of the infrared indocyanine green imaging of lymph nodes retrieved at sentinel node navigation surgery for gastric cancer. BMC Surg. 2016, 16, 35. [Google Scholar] [CrossRef]
- Nimura, H.; Narimiya, N.; Mitsumori, N.; Yamazaki, Y.; Yanaga, K.; Urashima, M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br. J. Surg. 2004, 91, 575–579. [Google Scholar] [CrossRef]
- Miyashiro, I.; Miyoshi, N.; Hiratsuka, M.; Kishi, K.; Yamada, T.; Ohue, M.; Ohigashi, H.; Yano, M.; Ishikawa, O.; Imaoka, S. Detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging: Comparison with infrared imaging. Ann. Surg. Oncol. 2008, 15, 1640–1643. [Google Scholar] [CrossRef]
- Cahill, R.A.; Ris, F.; Mortensen, N.J. Near-infrared laparoscopy for real-time intra-operative arterial and lymphatic perfusion imaging. Colorectal Dis. 2011, 13 Suppl 7, 12–17. [Google Scholar] [CrossRef]
- Takahashi, N.; Nimura, H.; Fujita, T.; Mitsumori, N.; Shiraishi, N.; Kitano, S.; Satodate, H.; Yanaga, K. Laparoscopic sentinel node navigation surgery for early gastric cancer: A prospective multicenter trial. Langenbecks Arch. Surg. 2017, 402, 27–32. [Google Scholar] [CrossRef]
- He, M.; Jiang, Z.; Wang, C.; Hao, Z.; An, J.; Shen, J. Diagnostic value of near-infrared or fluorescent indocyanine green guided sentinel lymph node mapping in gastric cancer: A systematic review and meta-analysis. J. Surg. Oncol. 2018, 118, 1243–1256. [Google Scholar] [CrossRef] [PubMed]
- Skubleny, D.; Dang, J.T.; Skulsky, S.; Switzer, N.; Tian, C.; Shi, X.; de Gara, C.; Birch, D.W.; Karmali, S. Diagnostic evaluation of sentinel lymph node biopsy using indocyanine green and infrared or fluorescent imaging in gastric cancer: A systematic review and meta-analysis. Surg. Endosc. 2018, 32, 2620–2631. [Google Scholar] [CrossRef] [PubMed]
- Wei, M.; Liang, Y.; Wang, L.; Li, Z.; Chen, Y.; Yan, Z.; Sun, D.; Huang, Y.; Zhong, X.; Liu, P.; et al. Clinical Application of Indocyanine Green Fluorescence Technology in Laparoscopic Radical Gastrectomy. Front. Oncol. 2022, 12, 847341. [Google Scholar] [CrossRef] [PubMed]
- Romanzi, A.; Mancini, R.; Ioni, L.; Picconi, T.; Pernazza, G. ICG-NIR-guided lymph node dissection during robotic subtotal gastrectomy for gastric cancer. A single-centre experience. Int. J. Med. Robot. 2021, 17, e2213. [Google Scholar] [CrossRef] [PubMed]
- Maruri, I.; Pardellas, M.H.; Cano-Valderrama, O.; Jove, P.; López-Otero, M.; Otero, I.; Campo, V.; Fernández, R.; Fernández-Fernández, N.; Sánchez-Santos, R. Retrospective cohort study of laparoscopic ICG-Guided Lymphadenectomy in gastric cancer from a Western country center. Surg. Endosc. 2022. [Google Scholar] [CrossRef]
- Roh, C.K.; Choi, S.; Seo, W.J.; Cho, M.; Son, T.; Kim, H.I.; Hyung, W.J. Indocyanine green fluorescence lymphography during gastrectomy after initial endoscopic submucosal dissection for early gastric cancer. Br. J. Surg. 2020, 107, 712–719. [Google Scholar] [CrossRef]
- Chen, Q.Y.; Xie, J.W.; Zhong, Q.; Wang, J.B.; Lin, J.X.; Lu, J.; Cao, L.L.; Lin, M.; Tu, R.H.; Huang, Z.N.; et al. Safety and Efficacy of Indocyanine Green Tracer-Guided Lymph Node Dissection During Laparoscopic Radical Gastrectomy in Patients With Gastric Cancer: A Randomized Clinical Trial. JAMA Surg. 2020, 155, 300–311. [Google Scholar] [CrossRef]
- Chen, Q.Y.; Zhong, Q.; Li, P.; Xie, J.W.; Liu, Z.Y.; Huang, X.B.; Lin, G.T.; Wang, J.B.; Lin, J.X.; Lu, J.; et al. Comparison of submucosal and subserosal approaches toward optimized indocyanine green tracer-guided laparoscopic lymphadenectomy for patients with gastric cancer (FUGES-019): A randomized controlled trial. BMC Med. 2021, 19, 276. [Google Scholar] [CrossRef]
- Huang, Z.N.; Su, Y.; Qiu, W.W.; Liu, C.H.; Chen, Q.Y.; Zheng, C.H.; Li, P.; Wang, J.B.; Lin, J.X.; Lu, J.; et al. Assessment of indocyanine green tracer-guided lymphadenectomy in laparoscopic gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: Results from a multicenter analysis based on propensity matching. Gastric Cancer 2021, 24, 1355–1364. [Google Scholar] [CrossRef]
- Park, J.H.; Berlth, F.; Wang, C.; Wang, S.; Choi, J.H.; Park, S.H.; Suh, Y.S.; Kong, S.H.; Park, D.J.; Lee, H.J.; et al. Mapping of the perigastric lymphatic network using indocyanine green fluorescence imaging and tissue marking dye in clinically advanced gastric cancer. Eur. J. Surg. Oncol. 2022, 48, 411–417. [Google Scholar] [CrossRef]
- Miyashiro, I.; Hiratsuka, M.; Kishi, K.; Takachi, K.; Yano, M.; Takenaka, A.; Tomita, Y.; Ishiguro, S. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: An institutional trial by experienced surgeons. Ann. Surg. Oncol. 2013, 20, 542–546. [Google Scholar] [CrossRef] [PubMed]
- Tajima, Y.; Yamazaki, K.; Masuda, Y.; Kato, M.; Yasuda, D.; Aoki, T.; Kato, T.; Murakami, M.; Miwa, M.; Kusano, M. Sentinel node mapping guided by indocyanine green fluorescence imaging in gastric cancer. Ann. Surg. 2009, 249, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Tajima, Y.; Murakami, M.; Yamazaki, K.; Masuda, Y.; Kato, M.; Sato, A.; Goto, S.; Otsuka, K.; Kato, T.; Kusano, M. Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann. Surg. Oncol. 2010, 17, 1787–1793. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.; Yasuda, K.; Shiromizu, A.; Etoh, T.; Shiraishi, N.; Kitano, S. Laparoscopic sentinel node navigation achieved by infrared ray electronic endoscopy system in patients with gastric cancer. Surg. Endosc. 2007, 21, 1131–1134. [Google Scholar] [CrossRef]
- Kinami, S.; Oonishi, T.; Fujita, J.; Tomita, Y.; Funaki, H.; Fujita, H.; Nakano, Y.; Ueda, N.; Kosaka, T. Optimal settings and accuracy of indocyanine green fluorescence imaging for sentinel node biopsy in early gastric cancer. Oncol. Lett. 2016, 11, 4055–4062. [Google Scholar] [CrossRef][Green Version]
- Kelder, W.; Nimura, H.; Takahashi, N.; Mitsumori, N.; van Dam, G.M.; Yanaga, K. Sentinel node mapping with indocyanine green (ICG) and infrared ray detection in early gastric cancer: An accurate method that enables a limited lymphadenectomy. Eur. J. Surg. Oncol. 2010, 36, 552–558. [Google Scholar] [CrossRef]
- Zhong, Q.; Chen, Q.Y.; Huang, X.B.; Lin, G.T.; Liu, Z.Y.; Chen, J.Y.; Wang, H.G.; Weng, K.; Li, P.; Xie, J.W.; et al. Clinical implications of Indocyanine Green Fluorescence Imaging-Guided laparoscopic lymphadenectomy for patients with gastric cancer: A cohort study from two randomized, controlled trials using individual patient data. Int. J. Surg. 2021, 94, 106120. [Google Scholar] [CrossRef]
- Kusano, M.; Tajima, Y.; Yamazaki, K.; Kato, M.; Watanabe, M.; Miwa, M. Sentinel node mapping guided by indocyanine green fluorescence imaging: A new method for sentinel node navigation surgery in gastrointestinal cancer. Dig. Surg. 2008, 25, 103–108. [Google Scholar] [CrossRef]
- Ohdaira, H.; Nimura, H.; Takahashi, N.; Mitsumori, N.; Kashiwagi, H.; Narimiya, N.; Yanaga, K. The possibility of performing a limited resection and a lymphadenectomy for proximal gastric carcinoma based on sentinel node navigation. Surg. Today 2009, 39, 1026–1031. [Google Scholar] [CrossRef]
- Tummers, Q.R.; Boogerd, L.S.; de Steur, W.O.; Verbeek, F.P.; Boonstra, M.C.; Handgraaf, H.J.; Frangioni, J.V.; van de Velde, C.J.; Hartgrink, H.H.; Vahrmeijer, A.L. Near-infrared fluorescence sentinel lymph node detection in gastric cancer: A pilot study. World J. Gastroenterol. 2016, 22, 3644–3651. [Google Scholar] [CrossRef]
- van Leeuwen, A.C.; Buckle, T.; Bendle, G.; Vermeeren, L.; Valdés Olmos, R.; van de Poel, H.G.; van Leeuwen, F.W. Tracer-cocktail injections for combined pre- and intraoperative multimodal imaging of lymph nodes in a spontaneous mouse prostate tumor model. J. Biomed. Opt. 2011, 16, 016004. [Google Scholar] [CrossRef] [PubMed]
- Okubo, K.; Uenosono, Y.; Arigami, T.; Matsushita, D.; Yanagita, S.; Kijima, T.; Amatatsu, M.; Ishigami, S.; Maemura, K.; Natsugoe, S. Quantitative assessment of fluorescence intensity of ICG in sentinel nodes in early gastric cancer. Gastric Cancer 2018, 21, 776–781. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.W.; Jeong, B.; Shin, I.H.; Kang, U.; Lee, Y.; Park, Y.S.; Ahn, S.H.; Park, D.J.; Kim, H.H. Sentinel node navigation surgery using near-infrared indocyanine green fluorescence in early gastric cancer. Surg. Endosc. 2019, 33, 1235–1243. [Google Scholar] [CrossRef]
- Miyashiro, I.; Hiratsuka, M.; Sasako, M.; Sano, T.; Mizusawa, J.; Nakamura, K.; Nashimoto, A.; Tsuburaya, A.; Fukushima, N. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: Final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer 2014, 17, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Kong, S.H.; Park, J.H.; Son, Y.G.; Huh, Y.J.; Suh, Y.S.; Lee, H.J.; Yang, H.K. Assessment of the Completeness of Lymph Node Dissection Using Near-infrared Imaging with Indocyanine Green in Laparoscopic Gastrectomy for Gastric Cancer. J. Gastric Cancer 2018, 18, 161–171. [Google Scholar] [CrossRef]
- Cianchi, F.; Indennitate, G.; Paoli, B.; Ortolani, M.; Lami, G.; Manetti, N.; Tarantino, O.; Messeri, S.; Foppa, C.; Badii, B.; et al. The Clinical Value of Fluorescent Lymphography with Indocyanine Green During Robotic Surgery for Gastric Cancer: A Matched Cohort Study. J. Gastrointest. Surg. 2020, 24, 2197–2203. [Google Scholar] [CrossRef] [PubMed]
- Ushimaru, Y.; Omori, T.; Fujiwara, Y.; Yanagimoto, Y.; Sugimura, K.; Yamamoto, K.; Moon, J.H.; Miyata, H.; Ohue, M.; Yano, M. The Feasibility and Safety of Preoperative Fluorescence Marking with Indocyanine Green (ICG) in Laparoscopic Gastrectomy for Gastric Cancer. J. Gastrointest. Surg. 2019, 23, 468–476. [Google Scholar] [CrossRef]
- Yoon, B.W.; Lee, W.Y. The oncologic safety and accuracy of indocyanine green fluorescent dye marking in securing the proximal resection margin during totally laparoscopic distal gastrectomy for gastric cancer: A retrospective comparative study. World J. Surg. Oncol. 2022, 20, 26. [Google Scholar] [CrossRef]
- Namikawa, T.; Iwabu, J.; Hashiba, M.; Munekage, M.; Uemura, S.; Yamada, T.; Kitagawa, H.; Mizuta, H.; Okamoto, K.; Uchida, K.; et al. Novel endoscopic marking clip equipped with resin-conjugated fluorescent indocyanine green during laparoscopic surgery for gastrointestinal cancer. Langenbecks Arch. Surg. 2020, 405, 503–508. [Google Scholar] [CrossRef]
- Kim, M.; Son, S.Y.; Cui, L.H.; Shin, H.J.; Hur, H.; Han, S.U. Real-time Vessel Navigation Using Indocyanine Green Fluorescence during Robotic or Laparoscopic Gastrectomy for Gastric Cancer. J Gastric Cancer 2017, 17, 145–153. [Google Scholar] [CrossRef]
- Ebihara, Y.; Shichinohe, T.; Kurashima, Y.; Murakami, S.; Hirano, S. Laparoscopic real-time vessel navigation using indocyanine green fluorescence during laparoscopy-assisted gastric tube reconstruction: First experience. J. Minim. Access Surg. 2021, 17, 576–579. [Google Scholar] [CrossRef] [PubMed]
- Yamazaki, Y.; Kanaji, S.; Takiguchi, G.; Urakawa, N.; Hasegawa, H.; Yamamoto, M.; Matsuda, Y.; Yamashita, K.; Matsuda, T.; Oshikiri, T.; et al. Preoperative endoscopic tattooing using India ink to determine the resection margins during totally laparoscopic distal gastrectomy for gastric cancer. Surg. Today 2021, 51, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Zheng, X.; Liu, Z.; Yu, J.; Deng, Z.; Xue, F.; Zheng, Y.; Chen, F.; Shi, H.; Chen, G.; et al. A multicenter study of using carbon nanoparticles to show sentinel lymph nodes in early gastric cancer. Surg. Endosc. 2016, 30, 1294–1300. [Google Scholar] [CrossRef]
- Feng, Y.; Yang, K.; Sun, H.H.; Liu, Y.P.; Zhang, D.; Zhao, Y.; Shi, W.; Lu, G.F.; Zhang, Z.Y.; Jia, A.; et al. Value of preoperative gastroscopic carbon nanoparticles labeling in patients undergoing laparoscopic radical gastric cancer surgery. Surg. Oncol. 2021, 38, 101628. [Google Scholar] [CrossRef] [PubMed]
- Hagiwara, A.; Takahashi, T.; Sawai, K.; Iwamoto, A.; Shimotsuma, M.; Yoneyama, C.; Seiki, K.; Itoh, M.; Sasabe, T.; Lee, M. Lymph nodal vital staining with newer carbon particle suspensions compared with India ink: Experimental and clinical observations. Lymphology 1992, 25, 84–89. [Google Scholar] [PubMed]
- Kitamura, K.; Hagiwara, A.; Otsuji, E.; Shimotsuma, M.; Taniguchi, H.; Yamaguchi, T.; Sawai, K.; Takahashi, T. Activated carbon-oriented gastrectomy for early gastric cancer. Br. J. Surg. 1995, 82, 647–650. [Google Scholar] [CrossRef]
- Tokuhara, T.; Nakata, E.; Tenjo, T.; Kawai, I.; Satoi, S.; Inoue, K.; Araki, M.; Ueda, H.; Higashi, C. A novel option for preoperative endoscopic marking with India ink in totally laparoscopic distal gastrectomy for gastric cancer: A useful technique considering the morphological characteristics of the stomach. Mol. Clin. Oncol. 2017, 6, 483–486. [Google Scholar] [CrossRef]
- Zhao, K.; Shan, B.Q.; Gao, Y.P.; Xu, J.Y. Role of carbon nanotracers in lymph node dissection of advanced gastric cancer and the selection of preoperative labeling time. World J Clin Cases 2022, 10, 870–881. [Google Scholar] [CrossRef]
- Li, Z.; Ao, S.; Bu, Z.; Wu, A.; Wu, X.; Shan, F.; Ji, X.; Zhang, Y.; Xing, Z.; Ji, J. Clinical study of harvesting lymph nodes with carbon nanoparticles in advanced gastric cancer: A prospective randomized trial. World J. Surg. Oncol. 2016, 14, 88. [Google Scholar] [CrossRef]
- Mu, G.; Huang, Y.; Wei, C.; Chen, Z.; Wu, X.; Qin, X.; Zeng, Y. Para-aortic lymph node tracing and dissection in advanced gastric cancer: Effectiveness of carbon nanoparticles injection through the no. 12b lymph node. J. Cancer Res. Ther. 2020, 16, 238–242. [Google Scholar] [CrossRef]
- Tian, Y.; Lin, Y.; Guo, H.; Hu, Y.; Li, Y.; Fan, L.; Zhao, X.; Wang, D.; Tan, B.; Zhao, Q. Safety and efficacy of carbon nanoparticle suspension injection and indocyanine green tracer-guided lymph node dissection during robotic distal gastrectomy in patients with gastric cancer. Surg. Endosc. 2022, 36, 3209–3216. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, H.; Kitagawa, Y. Sentinel node navigation surgery in patients with early gastric cancer. Dig. Surg. 2013, 30, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Cockburn, K.C.; Toumi, Z.; Mackie, A.; Julyan, P. Radioguided Surgery for Gastroenteropancreatic Neuroendocrine Tumours: A Systematic Literature Review. J. Gastrointest. Surg. 2021, 25, 3244–3257. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Kitajima, M. Diagnostic validity of radio-guided sentinel node mapping for gastric cancer: A review of current status and future direction. Surg. Technol. Int. 2006, 15, 32–36. [Google Scholar]
- Jimenez, I.R.; Roca, M.; Vega, E.; García, M.L.; Benitez, A.; Bajén, M.; Martín-Comín, J. Particle sizes of colloids to be used in sentinel lymph node radiolocalization. Nucl. Med. Commun. 2008, 29, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Park, D.J.; Kim, H.H.; Park, Y.S.; Lee, H.S.; Lee, W.W.; Lee, H.J.; Yang, H.K. Simultaneous indocyanine green and (99m)Tc-antimony sulfur colloid-guided laparoscopic sentinel basin dissection for gastric cancer. Ann. Surg. Oncol. 2011, 18, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Lianos, G.D.; Bali, C.D.; Hasemaki, N.; Glantzounis, G.K.; Mitsis, M.; Rausei, S. Sentinel Node Navigation in Gastric Cancer: Where Do We Stand? J. Gastrointest. Cancer 2019, 50, 201–206. [Google Scholar] [CrossRef]
- Yasuda, S.; Shimada, H.; Chino, O.; Tanaka, H.; Kenmochi, T.; Takechi, M.; Nabeshima, K.; Okamoto, Y.; Kato, Y.; Kijima, H.; et al. Sentinel lymph node detection with Tc-99m tin colloids in patients with esophagogastric cancer. Jpn J. Clin. Oncol. 2003, 33, 68–72. [Google Scholar] [CrossRef]
- Gretschel, S.; Bembenek, A.; Ulmer, C.; Hünerbein, M.; Markwardt, J.; Schneider, U.; Schlag, P.M. Prediction of gastric cancer lymph node status by sentinel lymph node biopsy and the Maruyama computer model. Eur. J. Surg. Oncol. 2005, 31, 393–400. [Google Scholar] [CrossRef]
- Jalaly, N.Y.; Valizadeh, N.; Azizi, S.; Kamani, F.; Hassanzadeh, M. Sentinel lymph node mapping and biopsy using radioactive tracer in gastric cancer. ANZ J. Surg. 2014, 84, 454–458. [Google Scholar] [CrossRef]
- An, J.Y.; Min, J.S.; Lee, Y.J.; Jeong, S.H.; Hur, H.; Han, S.U.; Hyung, W.J.; Cho, G.S.; Jeong, G.A.; Jeong, O.; et al. Which Factors Are Important for Successful Sentinel Node Navigation Surgery in Gastric Cancer Patients? Analysis from the SENORITA Prospective Multicenter Feasibility Quality Control Trial. Gastroenterol. Res. Pract. 2017, 2017, 1732571. [Google Scholar] [CrossRef]
- Lee, Y.J.; Ha, W.S.; Park, S.T.; Choi, S.K.; Hong, S.C.; Park, J.W. Which biopsy method is more suitable between a basin dissection and pick-up biopsy for sentinel nodes in laparoscopic sentinel-node navigation surgery (LSNNS) for gastric cancer? J. Laparoendosc. Adv. Surg. Tech A 2008, 18, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Shimada, A.; Takeuchi, H.; Ono, T.; Kamiya, S.; Fukuda, K.; Nakamura, R.; Takahashi, T.; Wada, N.; Kawakubo, H.; Saikawa, Y.; et al. Pylorus-Preserving Surgery Based on the Sentinel Node Concept in Early Gastric Cancer. Ann. Surg. Oncol. 2016, 23, 4247–4252. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Kawakubo, H.; Shimada, A.; Hoshino, S.; Matsuda, S.; Mayanagi, S.; Irino, T.; Fukuda, K.; Nakamura, R.; Wada, N.; et al. The Results of Sentinel Node Mapping for Patients with Clinically Early Staged Gastric Cancer Diagnosed with Pt2/deeper Tumors. World J. Surg. 2021, 45, 3350–3358. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Takeuchi, H.; Takagi, Y.; Natsugoe, S.; Terashima, M.; Murakami, N.; Fujimura, T.; Tsujimoto, H.; Hayashi, H.; Yoshimizu, N.; et al. Sentinel node mapping for gastric cancer: A prospective multicenter trial in Japan. J. Clin. Oncol. 2013, 31, 3704–3710. [Google Scholar] [CrossRef] [PubMed]
- Eom, B.W.; Yoon, H.M.; Min, J.S.; Cho, I.; Park, J.H.; Jung, M.R.; Hur, H.; Kim, Y.W.; Park, Y.K.; Nam, B.H.; et al. Prospective Multicenter Feasibility Study of Laparoscopic Sentinel Basin Dissection after Endoscopic Submucosal Dissection for Early Gastric Cancer: SENORITA 2 Trial Protocol. J. Gastric Cancer 2019, 19, 157–164. [Google Scholar] [CrossRef]
- Ichikura, T.; Chochi, K.; Sugasawa, H.; Yaguchi, Y.; Sakamoto, N.; Takahata, R.; Kosuda, S.; Mochizuki, H. Individualized surgery for early gastric cancer guided by sentinel node biopsy. Surgery 2006, 139, 501–507. [Google Scholar] [CrossRef]
- Lee, Y.J.; Jeong, S.H.; Hur, H.; Han, S.U.; Min, J.S.; An, J.Y.; Hyung, W.J.; Cho, G.S.; Jeong, G.A.; Jeong, O.; et al. Prospective Multicenter Feasibility Study of Laparoscopic Sentinel Basin Dissection for Organ Preserving Surgery in Gastric Cancer: Quality Control Study for Surgical Standardization Prior to Phase III Trial. Medicine 2015, 94, e1894. [Google Scholar] [CrossRef]
- Gretschel, S.; Bembenek, A.; Hünerbein, M.; Dresel, S.; Schneider, W.; Schlag, P.M. Efficacy of different technical procedures for sentinel lymph node biopsy in gastric cancer staging. Ann. Surg. Oncol. 2007, 14, 2028–2035. [Google Scholar] [CrossRef]
- Niihara, M.; Takeuchi, H.; Nakahara, T.; Saikawa, Y.; Takahashi, T.; Wada, N.; Mukai, M.; Kitagawa, Y. Sentinel lymph node mapping for 385 gastric cancer patients. J. Surg. Res. 2016, 200, 73–81. [Google Scholar] [CrossRef]
- Lee, J.H.; Ryu, K.W.; Kim, C.G.; Kim, S.K.; Lee, J.S.; Kook, M.C.; Choi, I.J.; Kim, Y.W.; Chang, H.J.; Bae, J.M. Sentinel node biopsy using dye and isotope double tracers in early gastric cancer. Ann. Surg. Oncol. 2006, 13, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, S.; Takeuchi, H.; Nakahara, T.; Niihara, M.; Nakamura, R.; Takahashi, T.; Wada, N.; Kawakubo, H.; Saikawa, Y.; Omori, T.; et al. Auxiliary diagnosis of lymph node metastasis in early gastric cancer using quantitative evaluation of sentinel node radioactivity. Gastric Cancer 2016, 19, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Cheng, X. Clinical application study of sentinel lymph node of double-staining mark in gastric cancer. Chongqing Yi Xue 2010, 39, 1542–1544+1634. [Google Scholar]
- Koizumi, N.; Harada, Y.; Murayama, Y.; Harada, K.; Beika, M.; Yamaoka, Y.; Dai, P.; Komatsu, S.; Kubota, T.; Ichikawa, D.; et al. Detection of metastatic lymph nodes using 5-aminolevulinic acid in patients with gastric cancer. Ann. Surg. Oncol. 2013, 20, 3541–3548. [Google Scholar] [CrossRef]
- Namikawa, T.; Inoue, K.; Uemura, S.; Shiga, M.; Maeda, H.; Kitagawa, H.; Fukuhara, H.; Kobayashi, M.; Shuin, T.; Hanazaki, K. Photodynamic diagnosis using 5-aminolevulinic acid during gastrectomy for gastric cancer. J. Surg. Oncol. 2014, 109, 213–217. [Google Scholar] [CrossRef]
- Namikawa, T.; Yatabe, T.; Inoue, K.; Shuin, T.; Hanazaki, K. Clinical applications of 5-aminolevulinic acid-mediated fluorescence for gastric cancer. World J. Gastroenterol. 2015, 21, 8769–8775. [Google Scholar] [CrossRef]
- Vuijk, F.A.; Hilling, D.E.; Mieog, J.S.D.; Vahrmeijer, A.L. Fluorescent-guided surgery for sentinel lymph node detection in gastric cancer and carcinoembryonic antigen targeted fluorescent-guided surgery in colorectal and pancreatic cancer. J. Surg. Oncol. 2018, 118, 315–323. [Google Scholar] [CrossRef]
- Li, X.H.; Ai, S.C.; Lu, X.F.; Liu, S.; Guan, W.X. Nanotechnology-based strategies for gastric cancer imaging and treatment. RSC Adv. 2021, 11, 35392–35407. [Google Scholar] [CrossRef]
- Ding, J.; Feng, M.; Wang, F.; Wang, H.; Guan, W. Targeting effect of PEGylated liposomes modified with the Arg-Gly-Asp sequence on gastric cancer. Oncol. Rep. 2015, 34, 1825–1834. [Google Scholar] [CrossRef]
- Cheng, H.; Chi, C.; Shang, W.; Rengaowa, S.; Cui, J.; Ye, J.; Jiang, S.; Mao, Y.; Zeng, C.; Huo, H.; et al. Precise integrin-targeting near-infrared imaging-guided surgical method increases surgical qualification of peritoneal carcinomatosis from gastric cancer in mice. Oncotarget 2017, 8, 6258–6272. [Google Scholar] [CrossRef]
- Shi, H.; Yan, R.; Wu, L.; Sun, Y.; Liu, S.; Zhou, Z.; He, J.; Ye, D. Tumor-targeting CuS nanoparticles for multimodal imaging and guided photothermal therapy of lymph node metastasis. Acta Biomater. 2018, 72, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Espelin, C.W.; Leonard, S.C.; Geretti, E.; Wickham, T.J.; Hendriks, B.S. Dual HER2 Targeting with Trastuzumab and Liposomal-Encapsulated Doxorubicin (MM-302) Demonstrates Synergistic Antitumor Activity in Breast and Gastric Cancer. Cancer Res. 2016, 76, 1517–1527. [Google Scholar] [CrossRef]
- Symeonidis, D.; Koukoulis, G.; Tepetes, K. Sentinel node navigation surgery in gastric cancer: Current status. World J. Gastrointest. Surg. 2014, 6, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.H.; Zhang, X.T.; Li, Y.F.; Tang, L.; Qu, X.J.; Ying, J.E.; Zhang, J.; Sun, L.Y.; Lin, R.B.; Qiu, H.; et al. The Chinese Society of Clinical Oncology (CSCO): Clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun. 2021, 41, 747–795. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).