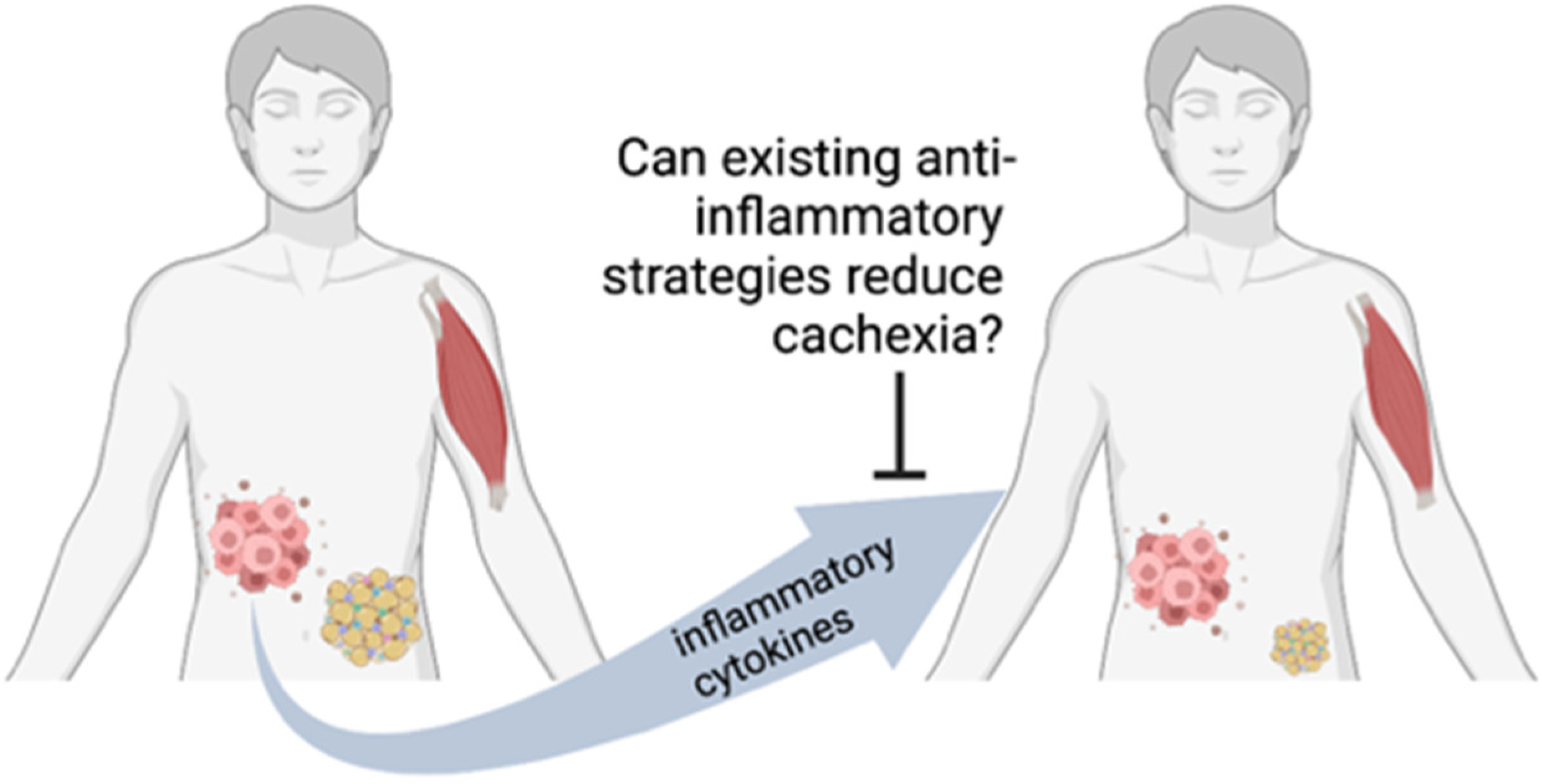
Inflammation as a Therapeutic Target in Cancer Cachexia
Abstract
Simple Summary
Abstract
1. Introduction
2. Mechanisms of Cancer-Associated Cachexia
3. Current Clinical Management
4. Search Strategy
5. Current Status of Anti-Inflammatory Strategies for Cancer Cachexia
5.1. Fish Oils and Omega-3 Fatty Acid Supplements
5.2. Non-Steroid Anti-Inflammatory Drugs
5.2.1. Celecoxib
5.2.2. Ibuprofen
5.2.3. Naproxen
5.2.4. Indomethacin
5.3. Targeted Anti-Inflammatory Strategies
5.3.1. TNF
5.3.2. IL-1β
5.3.3. IL-6
6. Other Anti-Cachexia Strategies of Note
6.1. Immune Checkpoint Inhibitors
6.2. MEK Inhibition
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef]
- Jo, H.; Yoshida, T.; Horinouchi, H.; Yagishita, S.; Matsumoto, Y.; Shinno, Y.; Okuma, Y.; Goto, Y.; Yamamoto, N.; Takahashi, K.; et al. Prognostic significance of cachexia in advanced non-small cell lung cancer patients treated with pembrolizumab. Cancer Immunol. Immunother. 2022, 71, 387–398. [Google Scholar] [CrossRef]
- Dewys, W.D.; Begg, C.; Lavin, P.T.; Band, P.R.; Bennett, J.M.; Bertino, J.R.; Cohen, M.H.; Douglass, H.O.; Engstrom, P.F.; Ezdinli, E.Z. Prognostic Effect of Weight Loss Prior to Chemotherapy in Cancer Patients. Eastern Cooperative Oncology Group. Am. J. Med. 1980, 69, 491–497. [Google Scholar] [CrossRef]
- Lanzotti, V.J.; Thomas, D.R.; Boyle, L.E.; Bs, T.L.S.; Gehan, E.A.; Samuels, M.L. Survival with inoperable lung cancer.An integration of prognostic variables based on simple clinical criteria. Cancer 1977, 39, 303–313. [Google Scholar] [CrossRef]
- Derman, B.A.; Macklis, J.N.; Azeem, M.S.; Sayidine, S.; Basu, S.; Batus, M.; Esmail, F.; Borgia, J.A.; Bonomi, P.; Fidler, M.J. Relationships between Longitudinal Neutrophil to Lymphocyte Ratios, Body Weight Changes, and Overall Survival in Patients with Non-Small Cell Lung Cancer. BMC Cancer 2017, 17, 141. [Google Scholar] [CrossRef]
- Zhang, Q.; Song, M.; Zhang, X.; Ding, J.; Ruan, G.; Zhang, X.; Liu, T.; Yang, M.; Ge, Y.; Tang, M.; et al. Association of systemic inflammation with survival in patients with cancer cachexia: Results from a multicentre cohort study. J. Cachex-Sarcopenia Muscle 2021, 12, 1466–1476. [Google Scholar] [CrossRef]
- Tavares, P.; Gonçalves, D.M.; Santos, L.L.; Ferreira, R. Revisiting the clinical usefulness of C-reactive protein in the set of cancer cachexia. Porto Biomed. J. 2021, 6, e123. [Google Scholar] [CrossRef] [PubMed]
- Nipp, R.D.; Fuchs, G.; El-Jawahri, A.; Mario, J.; Troschel, F.M.; Greer, J.A.; Gallagher, E.R.; Jackson, V.A.; Kambadakone, A.; Hong, T.S.; et al. Sarcopenia Is Associated with Quality of Life and Depression in Patients with Advanced Cancer. Oncologist 2018, 23, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, J.A.; Pothuraju, R.; Jain, M.; Batra, S.K.; Nasser, M.W. Advances in Cancer Cachexia: Intersection between Affected Organs, Mediators, and Pharmacological Interventions. Biochim. Biophys. Acta Ver. Cancer 2020, 1873, 188359. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, T.; Matsui, Y.; Tomida, M.; Suzuki, Y.; Nishita, Y.; Tange, C.; Shimokata, H.; Imagama, S.; Otsuka, R.; Arai, H. Differences in the mass and quality of the quadriceps with age and sex and their relationships with knee extension strength. J. Cachex-Sarcopenia Muscle 2021, 12, 900–912. [Google Scholar] [CrossRef] [PubMed]
- Herremans, K.M.; Riner, A.N.; Cameron, M.E.; Trevino, J.G. The Microbiota and Cancer Cachexia. Int. J. Mol. Sci. 2019, 20, 6267. [Google Scholar] [CrossRef] [PubMed]
- Mannelli, M.; Gamberi, T.; Magherini, F.; Fiaschi, T. The Adipokines in Cancer Cachexia. Int. J. Mol. Sci. 2020, 21, 4860. [Google Scholar] [CrossRef]
- Roeland, E.J.; Bohlke, K.; Baracos, V.E.; Bruera, E.; Del Fabbro, E.; Dixon, S.; Fallon, M.; Herrstedt, J.; Lau, H.; Platek, M.; et al. Management of Cancer Cachexia: ASCO Guideline. J. Clin. Oncol. 2020, 38, 2438–2453. [Google Scholar] [CrossRef] [PubMed]
- Lambert, C.P. Should the Fda’s Criteria for the Clinical Efficacy of Cachexia Drugs Be Changed? Is Ostarine Safe and Effective? J. Cachexia Sarcopenia Muscle 2021, 12, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Temel, J.S.; Abernethy, A.P.; Currow, D.C.; Friend, J.; Duus, E.M.; Yan, Y.; Fearon, K.C. Anamorelin in Patients with Non-Small-Cell Lung Cancer and Cachexia (Romana 1 and Romana 2): Results from Two Randomised, Double-Blind, Phase 3 Trials. Lancet Oncol. 2016, 17, 519–531. [Google Scholar] [CrossRef]
- Katakami, N.; Uchino, J.; Yokoyama, T.; Naito, T.; Kondo, M.; Yamada, K.; Kitajima, H.; Yoshimori, K.; Sato, K.; Saito, H.; et al. Anamorelin (Ono-7643) for the Treatment of Patients with Non-Small Cell Lung Cancer and Cachexia: Results from a Randomized, Double-Blind, Placebo-Controlled, Multicenter Study of Japanese Patients (Ono-7643-04). Cancer 2018, 124, 606–616. [Google Scholar] [CrossRef]
- Currow, D.C.; Glare, P.; Louw, S.; Martin, P.; Clark, K.; Fazekas, B.; Agar, M.R. A randomised, double blind, placebo-controlled trial of megestrol acetate or dexamethasone in treating symptomatic anorexia in people with advanced cancer. Sci. Rep. 2021, 11, 2421. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, C.L.; Kugler, J.W.; Sloan, J.A.; Mailliard, J.A.; Krook, J.E.; Wilwerding, M.B.; Rowland, K.M.; Camoriano, J.K.; Novotny, P.J.; Christensen, B.J. Randomized Comparison of Megestrol Acetate Versus Dexamethasone Versus Fluoxymesterone for the Treatment of Cancer Anorexia/Cachexia. J. Clin. Oncol. 1999, 17, 3299–3306. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.N.; Abdel-Aal, H.H.; Elsherief, W.A.; Farag, D.E.; Riad, N.M.; Alsirafy, S.A. Mirtazapine in Cancer-Associated Anorexia and Cachexia: A Double-Blind Placebo-Controlled Randomized Trial. J. Pain Symptom Manag. 2021, 62, 1207–1215. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Eton, D.; Fairclough, D.L.; Bonomi, P.; Heyes, A.E.; Silberman, C.; Wolf, M.K.; Johnson, D.H. What is a clinically meaningful change on the Functional Assessment of Cancer Therapy–Lung (FACT-L) Questionnaire?: Results from Eastern Cooperative Oncology Group (ECOG) Study 5592. J. Clin. Epidemiol. 2002, 55, 285–295. [Google Scholar] [CrossRef]
- Reid, J.; Hughes, C.; Murray, L.; Parsons, C.; Cantwell, M. Non-steroidal anti-inflammatory drugs for the treatment of cancer cachexia: A systematic review. Palliat. Med. 2013, 27, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Yetiv, J.Z. Clinical Applications of Fish Oils. JAMA 1988, 260, 665–670. [Google Scholar] [CrossRef] [PubMed]
- Gorjao, R.; dos Santos, C.M.M.; Serdan, T.D.A.; Diniz, V.L.S.; Alba-Loureiro, T.C.; Cury-Boaventura, M.F.; Hatanaka, E.; Levada-Pires, A.C.; Sato, F.T.; Pithon-Curi, T.C.; et al. New insights on the regulation of cancer cachexia by N-3 polyunsaturated fatty acids. Pharmacol. Ther. 2018, 196, 117–134. [Google Scholar] [CrossRef]
- Burns, C.P.; Halabi, S.; Clamon, G.; Kaplan, E.; Hohl, R.J.; Atkins, J.N.; Schwartz, M.A.; Wagner, B.A.; Paskett, E. Phase II study of high-dose fish oil capsules for patients with cancer-related cachexia. Cancer 2004, 101, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Bruera, E.; Strasser, F.; Palmer, J.L.; Willey, J.; Calder, K.; Amyotte, G.; Baracos, V. Effect of Fish Oil on Appetite and Other Symptoms in Patients with Advanced Cancer and Anorexia/Cachexia: A Double-Blind, Placebo-Controlled Study. J. Clin. Oncol. 2003, 21, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, G.; Macciò, A.; Madeddu, C.; Serpe, R.; Antoni, G.; Massa, E.; Dessì, M.; Panzone, F. Phase II nonrandomized study of the efficacy and safety of COX-2 inhibitor celecoxib on patients with cancer cachexia. Klin. Wochenschr. 2010, 88, 85–92. [Google Scholar] [CrossRef]
- Lai, V.; George, J.; Richey, L.; Kim, H.J.; Cannon, T.; Shores, C.; Couch, M. Results of a Pilot Study of the Effects of Celecoxib on Cancer Cachexia in Patients with Cancer of the Head, Neck, and Gastrointestinal Tract. Head Neck 2008, 30, 67–74. [Google Scholar] [CrossRef]
- Kouchaki, B.; Janbabai, G.; Alipour, A.; Ala, S.; Borhani, S.; Salehifar, E. Randomized double-blind clinical trial of combined treatment with megestrol acetate plus celecoxib versus megestrol acetate alone in cachexia-anorexia syndrome induced by GI cancers. Support. Care Cancer 2018, 26, 2479–2489. [Google Scholar] [CrossRef] [PubMed]
- Cerchietti, L.C.; Navigante, A.H.; Castro, M.A. Effects of Eicosapentaenoic and Docosahexaenoic n-3 Fatty Acids From Fish Oil and Preferential Cox-2 Inhibition on Systemic Syndromes in Patients With Advanced Lung Cancer. Nutr. Cancer 2007, 59, 14–20. [Google Scholar] [CrossRef]
- Solheim, T.S.; Laird, B.J.; Balstad, T.R.; Stene, G.B.; Bye, A.; Johns, N.; Pettersen, C.H.; Fallon, M.; Fayers, P.; Fearon, K.; et al. A randomized phase II feasibility trial of a multimodal intervention for the management of cachexia in lung and pancreatic cancer. J. Cachex-Sarcopenia Muscle 2017, 8, 778–788. [Google Scholar] [CrossRef]
- McMillan, D.; Wigmore, S.J.; Wigmore, K.C.H.; O’Gorman, P.; Wright, C.E.; McArdle, C.S. A prospective randomized study of megestrol acetate and ibuprofen in gastrointestinal cancer patients with weight loss. Br. J. Cancer 1999, 79, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Lundholm, K.; Gelin, J.; Hyltander, A.; Lönnroth, C.; Sandström, R.; Svaninger, G.; Körner, U.; Gülich, M.; Kärrefors, I.; Norli, B. Anti-inflammatory treatment may prolong survival in undernourished patients with metastatic solid tumors. Cancer Res. 1994, 54, 5602–5606. [Google Scholar] [PubMed]
- Penning, T.D.; Talley, J.J.; Bertenshaw, S.R.; Carter, J.S.; Collins, P.W.; Docter, S.; Graneto, M.J.; Lee, L.F.; Malecha, J.W.; Miyashiro, J.M.; et al. Synthesis and Biological Evaluation of the 1,5-Diarylpyrazole Class of Cyclooxygenase-2 Inhibitors: Identification of 4-[5-(4-Methylphenyl)-3-(Trifluoromethyl)-1h-Pyrazol-1-Yl]Benze Nesulfonamide (Sc-58635, Celecoxib). J. Med. Chem. 1997, 40, 1347–1365. [Google Scholar] [CrossRef] [PubMed]
- Madeddu, C.; Dessi, M.; Panzone, F.; Serpe, R.; Antoni, G.; Cau, M.C.; Montaldo, L.; Mela, Q.; Mura, M.; Astara, G.; et al. Randomized Phase Iii Clinical Trial of a Combined Treatment with Carnitine + Celecoxib +/- Megestrol Acetate for Patients with Cancer-Related Anorexia/Cachexia Syndrome. Clin. Nutr. 2012, 31, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Cerchietti, L.C.; Navigante, A.H.; Peluffo, G.D.; Diament, M.J.; Stillitani, I.; Klein, S.A.; Cabalar, M.E. Effects of celecoxib, medroxyprogesterone, and dietary intervention on systemic syndromes in patients with advanced lung adenocarcinoma: A pilot study. J. Pain Symptom Manag. 2004, 27, 85–95. [Google Scholar] [CrossRef]
- Cushman, D.; Cheung, H. Effect of substrate concentration on inhibition of prostaglandin synthetase of bull seminal vesicles by anti-inflammatory drugs and fenamic acid analogs. Biochim. Biophys. Acta 1976, 424, 449–459. [Google Scholar] [CrossRef]
- McCarthy, D.O.; Whitney, P.; Hitt, A.; Al-Majid, S. Indomethacin and ibuprofen preserve gastrocnemius muscle mass in mice bearing the colon-26 adenocarcinoma. Res. Nurs. Health 2004, 27, 174–184. [Google Scholar] [CrossRef]
- De Souza, C.O.; Kurauti, M.A.; Silva, F.D.; de Morais, H.; Borba-Murad, G.R.; de Andrade, F.G.; de Souza, H.M. Effects of Celecoxib and Ibuprofen on Metabolic Disorders Induced by Walker-256 Tumor in Rats. Mol. Cell Biochem. 2015, 399, 237–246. [Google Scholar] [CrossRef]
- Piffar, P.; Fernandez, R.; Tchaikovski, O.; Hirabara, S.; Folador, A.; Pinto, G.; Jakobi, S.; Gobbo-Bordon, D.; Rohn, T.; Fabrício, V.; et al. Naproxen, clenbuterol and insulin administration ameliorates cancer cachexia and reduce tumor growth in Walker 256 tumor-bearing rats. Cancer Lett. 2003, 201, 139–148.00ED. [Google Scholar] [CrossRef]
- Pinto, J.A.; Folador, A., Jr.; Bonato, S.J.; Aikawa, J.; Yamazaki, R.K.; Pizato, N.; Facin, M.; Grohs, H.; de Oliveira, H.H.; Naliwaiko, K.; et al. Fish Oil Supplementation in F1 Generation Associated with Naproxen, Clenbuterol, and Insulin Administration Reduce Tumor Growth and Cachexia in Walker 256 Tumor-Bearing Rats. J. Nutr. Biochem. 2004, 15, 358–365. [Google Scholar] [CrossRef]
- Ku, E.C.; Wasvary, J.M. Inhibition of Prostaglandin Synthase by Pirprofen. Studies with Sheep Seminal Vesicle Enzyme. Biochim. Biophys. Acta 1975, 384, 360–368. [Google Scholar] [CrossRef]
- Diament, M.J.; Peluffo, G.D.; Stillitani, I.; Cerchietti, L.C.; Navigante, A.; Ranuncolo, S.M.; Klein, S.M. Inhibition of Tumor Progression and Paraneoplastic Syndrome Development in a Murine Lung Adenocarcinoma by Medroxyprogesterone Acetate and Indomethacin. Cancer Investig. 2006, 24, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Lonnroth, C.; Svaninger, G.; Gelin, J.; Cahlin, C.; Iresjö, B.-M.; Cvetkovska, E.; Edstrom, S.; Andersson, M.; Svanberg, E.; Lundholm, K. Effects related to indomethacin prolonged survival and decreased tumor-growth in a mouse-tumor model with cytokine dependent cancer cachexia. Int. J. Oncol. 1995, 7, 1405–1413. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-Z.; Qiu, Z.-G. Combined treatment with GH, insulin, and indomethacin alleviates cancer cachexia in a mouse model. J. Endocrinol. 2011, 208, 131–136. [Google Scholar] [CrossRef][Green Version]
- Xu, J.; Zhou, C.; Zhang, H.; Su, B.; Tang, L.; Cheng, B.; Qin, P.; Li, A. [Relationship of cytokine level with cancer cachexia and therapeutic effects of indomethacin for cancer cachexia]. Zhongguo Fei Ai Za Zhi 2004, 7, 336–338. [Google Scholar]
- Argilés, J.M.; López-Soriano, F.J.; Stemmler, B.; Busquets, S. Novel targeted therapies for cancer cachexia. Biochem. J. 2017, 474, 2663–2678. [Google Scholar] [CrossRef]
- Laird, B.J.; McMillan, D.; Skipworth, R.J.E.; Fallon, M.T.; Paval, D.R.; McNeish, I.; Gallagher, I.J. The Emerging Role of Interleukin 1beta (Il-1beta) in Cancer Cachexia. Inflammation 2021, 44, 1223–1228. [Google Scholar] [CrossRef]
- Bonetto, A.; Aydogdu, T.; Jin, X.; Zhang, Z.; Zhan, R.; Puzis, L.; Koniaris, L.G.; Zimmers, T.A. JAK/STAT3 pathway inhibition blocks skeletal muscle wasting downstream of IL-6 and in experimental cancer cachexia. Am. J. Physiol. Endocrinol. Metab. 2012, 303, E410–E421. [Google Scholar] [CrossRef]
- Guo, D.; Wang, C.; Wang, Q.; Qiao, Z.; Tang, H. Pantoprazole Blocks the Jak2/Stat3 Pathway to Alleviate Skeletal Muscle Wasting in Cancer Cachexia by Inhibiting Inflammatory Response. Oncotarget 2017, 8, 39640–39648. [Google Scholar] [CrossRef]
- Zhang, L.; Tang, H.; Kou, Y.; Li, R.; Zheng, Y.; Wang, Q.; Zhou, X.; Jin, L. MG132-mediated inhibition of the ubiquitin–proteasome pathway ameliorates cancer cachexia. J. Cancer Res. Clin. Oncol. 2013, 139, 1105–1115. [Google Scholar] [CrossRef]
- Penna, F.; Bonetto, A.; Aversa, Z.; Minero, V.G.; Fanelli, F.R.; Costelli, P.; Muscaritoli, M. Effect of the specific proteasome inhibitor bortezomib on cancer-related muscle wasting. J. Cachex-Sarcopenia Muscle 2016, 7, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, M.L.; Talbert, E.; Ahn, D.; Bekaii-Saab, T.; Badi, N.; Bloomston, P.M.; Conwell, D.L.; Cruz-Monserrate, Z.; Dillhoff, M.; Farren, M.R.; et al. Circulating Interleukin-6 Is Associated with Disease Progression, but Not Cachexia in Pancreatic Cancer. Pancreatology 2019, 19, 80–87. [Google Scholar] [CrossRef]
- Ando, K.; Takahashi, F.; Kato, M.; Kaneko, N.; Doi, T.; Ohe, Y.; Koizumi, F.; Nishio, K.; Takahashi, K. Tocilizumab, a Proposed Therapy for the Cachexia of Interleukin6-Expressing Lung Cancer. PLoS ONE 2014, 9, e102436. [Google Scholar] [CrossRef] [PubMed]
- Hirata, H.; Tetsumoto, S.; Kijima, T.; Kida, H.; Kumagai, T.; Takahashi, R.; Otani, Y.; Inoue, K.; Kuhara, H.; Shimada, K.; et al. Favorable Responses to Tocilizumab in Two Patients With Cancer-Related Cachexia. J. Pain Symptom Manag. 2013, 46, e9–e13. [Google Scholar] [CrossRef] [PubMed]
- Ando, K.; Takahashi, F.; Motojima, S.; Nakashima, K.; Kaneko, N.; Hoshi, K.; Takahashi, K. Possible Role for Tocilizumab, an Anti-Interleukin-6 Receptor Antibody, in Treating Cancer Cachexia. J. Clin. Oncol. 2013, 31, e69–e72. [Google Scholar] [CrossRef] [PubMed]
- Yi, C.A.; Tam, C.S.; Verstovsek, S. Efficacy and safety of ruxolitinib in the treatment of patients with myelofibrosis. Futur. Oncol. 2015, 11, 719–733. [Google Scholar]
- Mascarenhas, J. Pacritinib for the treatment of patients with myelofibrosis and thrombocytopenia. Expert Rev. Hematol. 2022, 15, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Talbert, E.E.; Guttridge, D.C. Emerging signaling mediators in the anorexia–cachexia syndrome of cancer. Trends Cancer 2022, 8, 397–403. [Google Scholar] [CrossRef]
- Degens, J.H.; Dingemans, A.C.; Willemsen, A.C.; Gietema, H.A.; Hurkmans, D.P.; Aerts, J.G.; Hendriks, L.E.; Schols, A.M. The prognostic value of weight and body composition changes in patients with non-small-cell lung cancer treated with nivolumab. J. Cachex-Sarcopenia Muscle 2021, 12, 657–664. [Google Scholar] [CrossRef]
- Coss, C.C.; Clinton, S.K.; Phelps, M.A. Cachectic Cancer Patients: Immune to Checkpoint Inhibitor Therapy? Clin. Cancer Res. 2018, 24, 5787–5789. [Google Scholar] [CrossRef]
- Roch, B.; Coffy, A.; Jean-Baptiste, S.; Palaysi, E.; Daures, J.-P.; Pujol, J.-L.; Bommart, S. Cachexia—Sarcopenia as a determinant of disease control rate and survival in non-small lung cancer patients receiving immune-checkpoint inhibitors. Lung Cancer 2020, 143, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Guzman-Prado, Y.; Ben Shimol, J.; Samson, O. Sarcopenia and the risk of adverse events in patients treated with immune checkpoint inhibitors: A systematic review. Cancer Immunol. Immunother. 2021, 70, 2771–2780. [Google Scholar] [CrossRef] [PubMed]
- Bekaii-Saab, T.; Phelps, M.A.; Li, X.; Saji, M.; Goff, L.; Kauh, J.S.W.; O’Neil, B.H.; Balsom, S.; Balint, C.; Liersemann, R.; et al. Multi-Institutional Phase II Study of Selumetinib in Patients With Metastatic Biliary Cancers. J. Clin. Oncol. 2011, 29, 2357–2363. [Google Scholar] [CrossRef] [PubMed]
- Prado, C.M.M.; Bekaii-Saab, T.; Doyle, L.A.; Shrestha, S.; Ghosh, S.; Baracos, V.E.; Sawyer, M.B. Skeletal muscle anabolism is a side effect of therapy with the MEK inhibitor: Selumetinib in patients with cholangiocarcinoma. Br. J. Cancer 2012, 106, 1583–1586. [Google Scholar] [CrossRef]
- Talbert, E.E.; Yang, J.; Mace, T.A.; Farren, M.R.; Farris, A.B.; Young, G.S.; Elnaggar, O.; Che, Z.; Timmers, C.D.; Rajasekera, P.; et al. Dual Inhibition of MEK and PI3K/Akt Rescues Cancer Cachexia through both Tumor-Extrinsic and -Intrinsic Activities. Mol. Cancer Ther. 2017, 16, 344–356. [Google Scholar] [CrossRef]
- Au, E.D.; Desai, A.P.; Koniaris, L.G.; Zimmers, T.A. The MEK-Inhibitor Selumetinib Attenuates Tumor Growth and Reduces IL-6 Expression but Does Not Protect against Muscle Wasting in Lewis Lung Cancer Cachexia. Front. Physiol. 2016, 7, 682. [Google Scholar] [CrossRef]
| Compound | Trial Details | Key Findings in NSAID Group | Reference |
|---|---|---|---|
| Celecoxib | Single arm Phase II; 24 patients; 300 mg/day; 4 months. | ~1% ↑ LBM (p < 0.0001) 19% ↓ TNF (p = 0.007) 15% ↑ HGS (p = 0.004) 14% ↑ QOL (p = 0.024) 20% ↓ ECOG (p = 0.0004) | [26] |
| Randomized pilot; 11 patients; 200 mg bid; 21 days | Likely benefit, but low power 1.4% ↑ weight (p = 0.05) ↑ QOL (p = 0.05) 19% ↓ IL-6 (p = 0.18) 33% ↓ IL-8 (p = 0.19) | [27] | |
| Phase III double-blind randomized; 90 patients; megestrol acetate + placebo v. megestrol + 200 mg/day celecoxib; 30 days | No additional benefits of celecoxib | [28] | |
| Randomized; 22 patients; fish oil (2 gm tid) + placebo v. fish oil (2 gm tid) + celecoxib 200 mg bid; 6 weeks | 55% ↓ CRP (p = 0.05) 15% ↑ HGS (p = 0.02) 2.5% ↑ body weight (p = 0.05) | [29] | |
| Phase II randomized; 46 patients; standard care v. celecoxib 300 mg/ day + 2 gm/day omega-3 fatty acid + exercise; 6 weeks | 4.48% ↑ body weight (p < 0.001) ↑ muscle mass (p = 0.03) | [30] | |
| Ibuprofen | Randomized; 73 patients; megestrol + placebo v. megestrol + ibuprofen 400 mg tid; 12 weeks | 2.3 kg ↑ body weight (p < 0.001) | [31] |
| Indomethacin | Randomized; 135 patients; 50 mg bid; variable length | 14% ↑ KPS (p = 0.03) ↑ survival (p < 0.05) | [32] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clamon, G.; Byrne, M.M.; Talbert, E.E. Inflammation as a Therapeutic Target in Cancer Cachexia. Cancers 2022, 14, 5262. https://doi.org/10.3390/cancers14215262
Clamon G, Byrne MM, Talbert EE. Inflammation as a Therapeutic Target in Cancer Cachexia. Cancers. 2022; 14(21):5262. https://doi.org/10.3390/cancers14215262
Chicago/Turabian StyleClamon, Gerald, Margaret M. Byrne, and Erin E. Talbert. 2022. "Inflammation as a Therapeutic Target in Cancer Cachexia" Cancers 14, no. 21: 5262. https://doi.org/10.3390/cancers14215262
APA StyleClamon, G., Byrne, M. M., & Talbert, E. E. (2022). Inflammation as a Therapeutic Target in Cancer Cachexia. Cancers, 14(21), 5262. https://doi.org/10.3390/cancers14215262





