Plasma hPG80 (Circulating Progastrin) as a Novel Prognostic Biomarker for Hepatocellular Carcinoma
Abstract
:Simple Summary
Abstract
1. Introduction
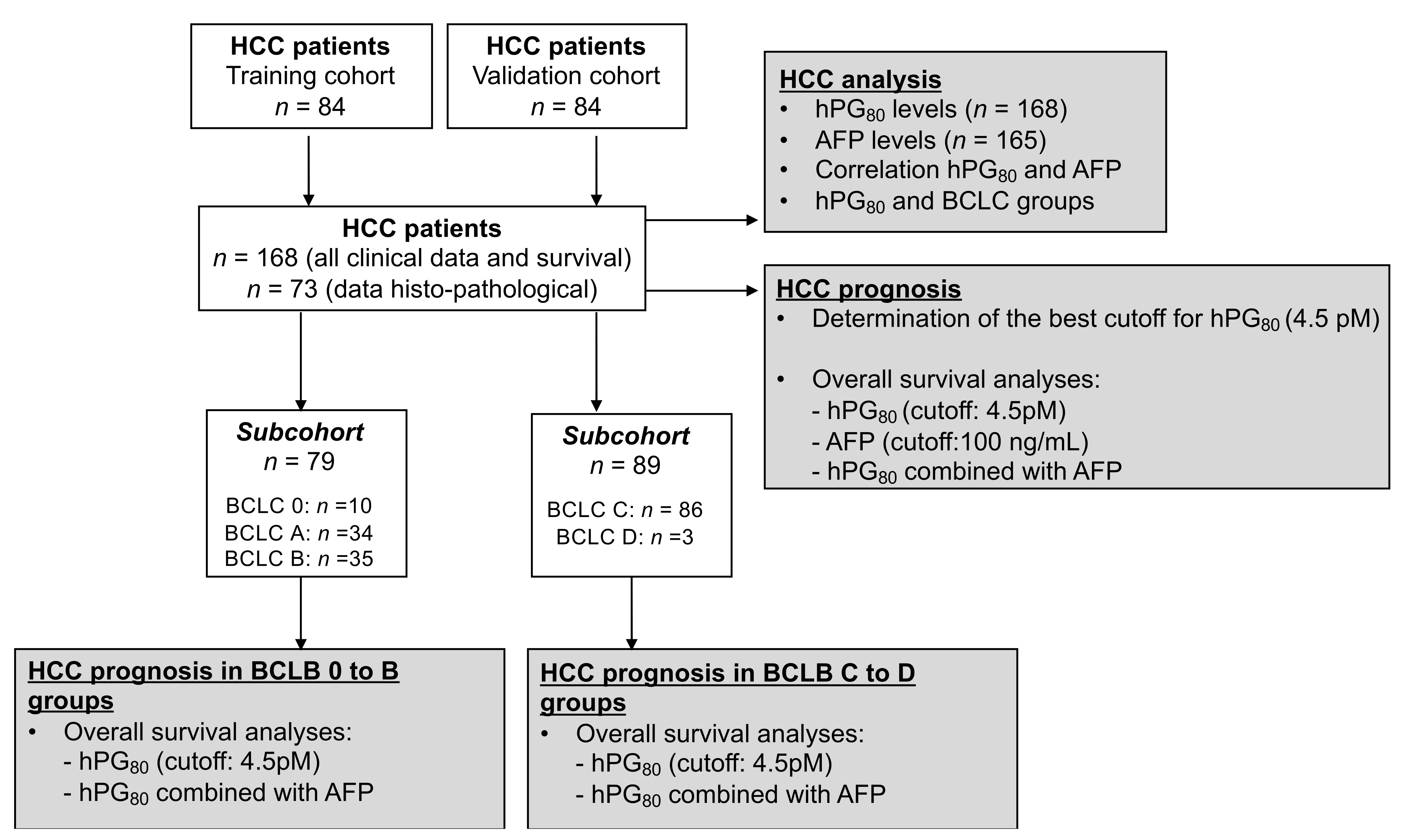
2. Materials and Methods
2.1. HCC Patients
2.2. hPG80 Level Measurements in the Blood Samples
2.3. AFP Level Measurements in the Blood Samples
2.4. Immunohistochemical Analyses
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
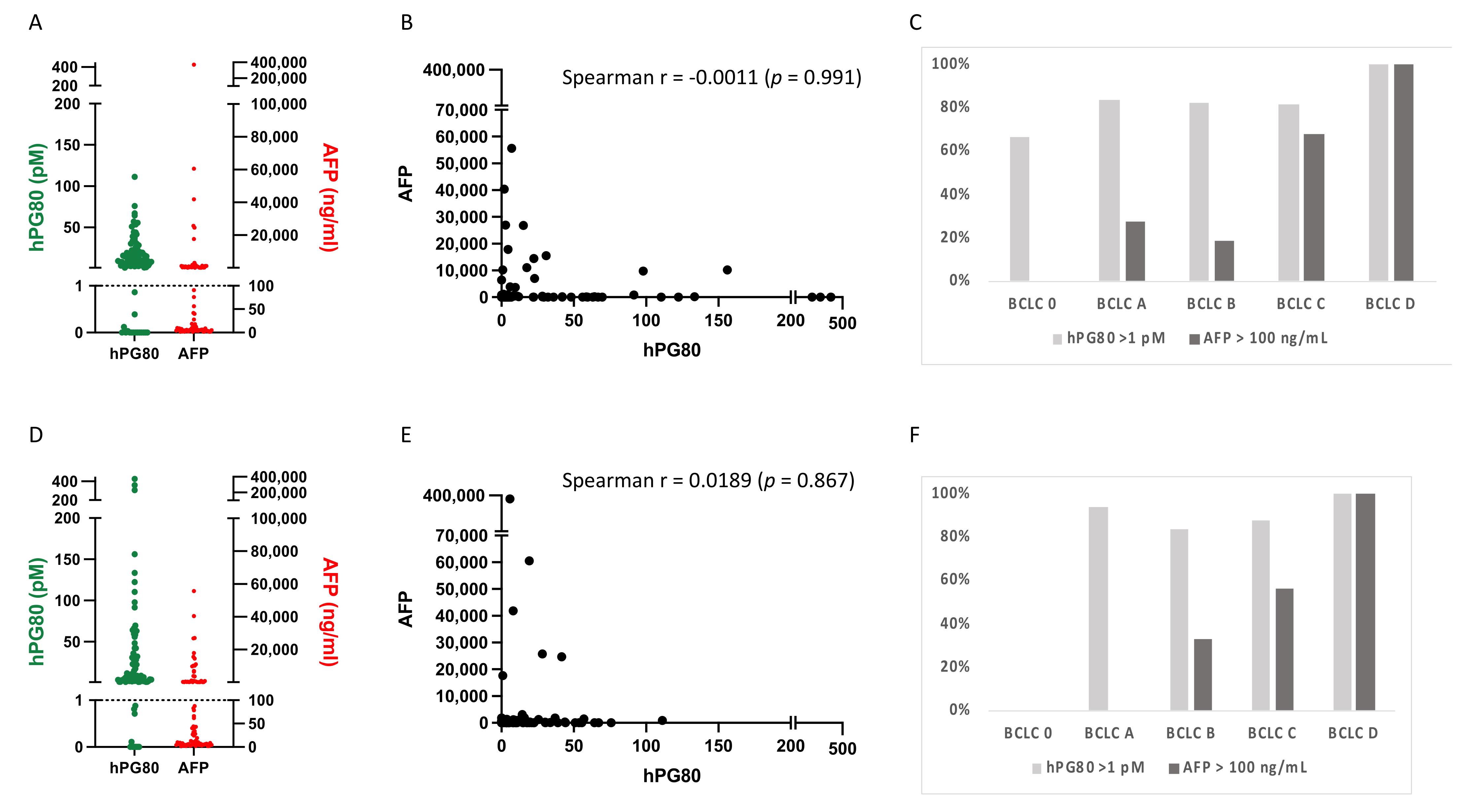
3.2. hPG80 and AFP Levels in the Training and Validation Cohorts
3.3. Correlation between hPG80 and AFP Levels and Various Clinicopathologic Features of HCC Patients According to Their Cutoff Values
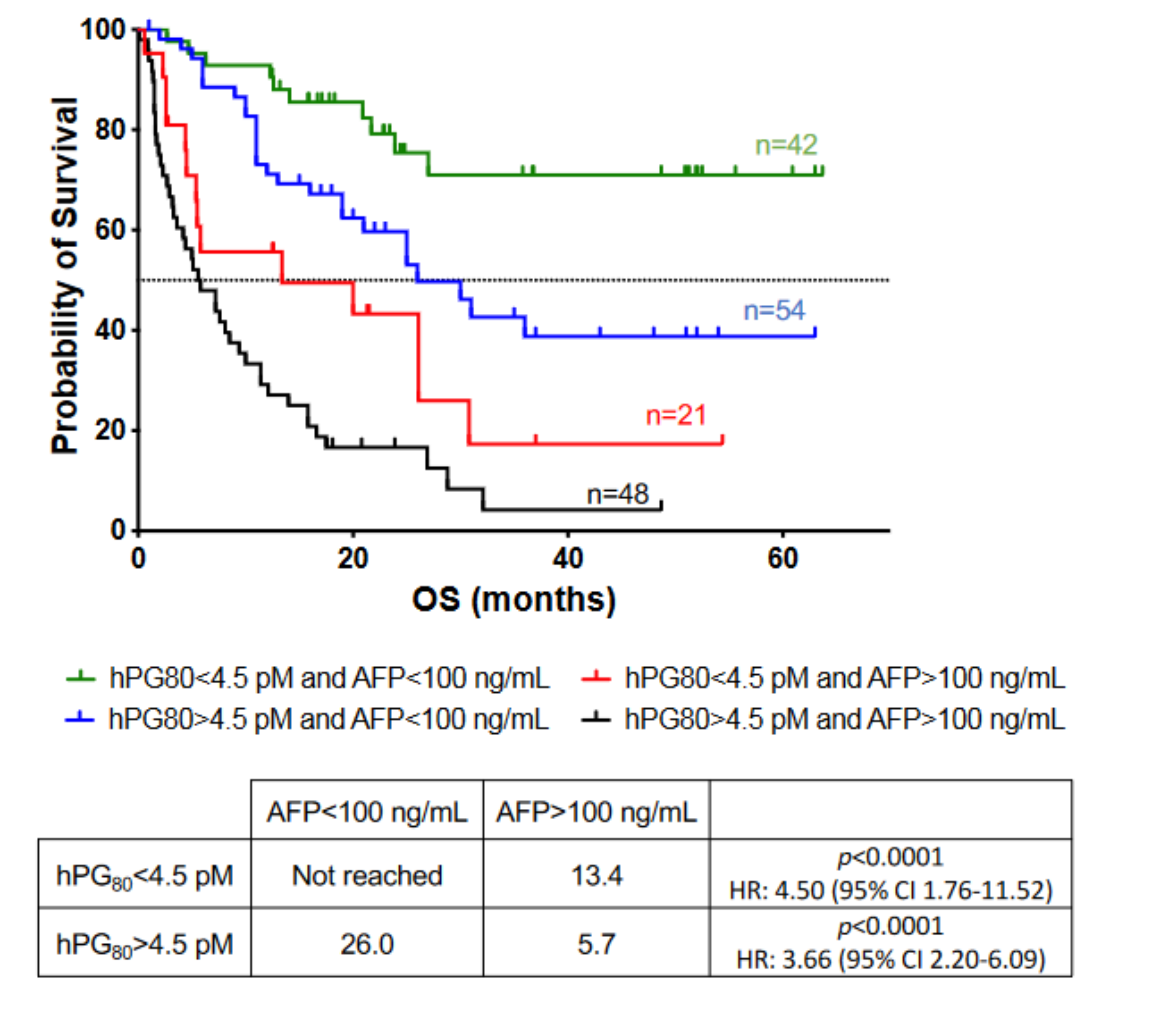
3.4. Prognosis Performance of hPG80 and AFP in HCC Patients
3.5. Prognosis Performance of hPG80 in Combination with AFP in HCC Patients
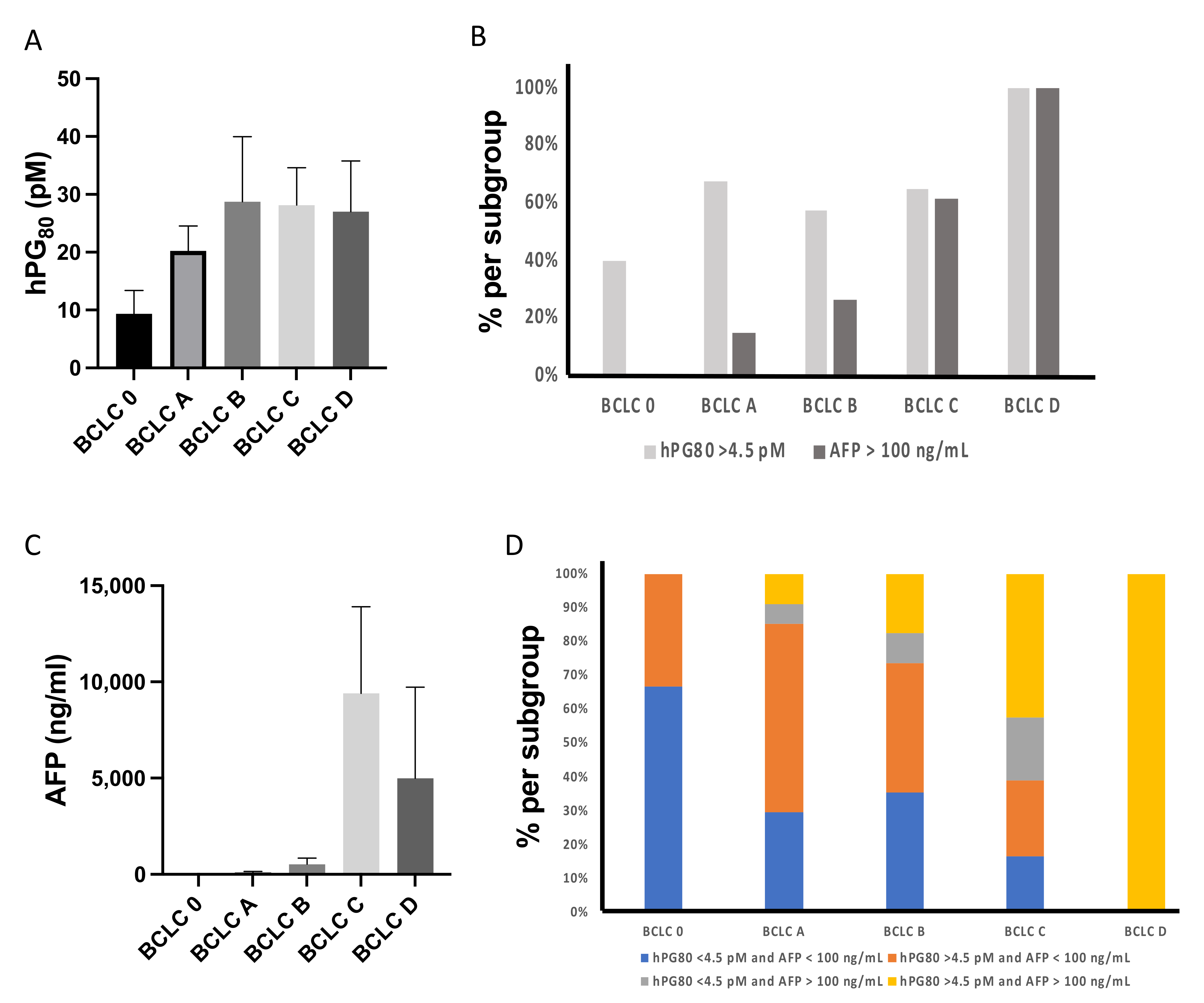
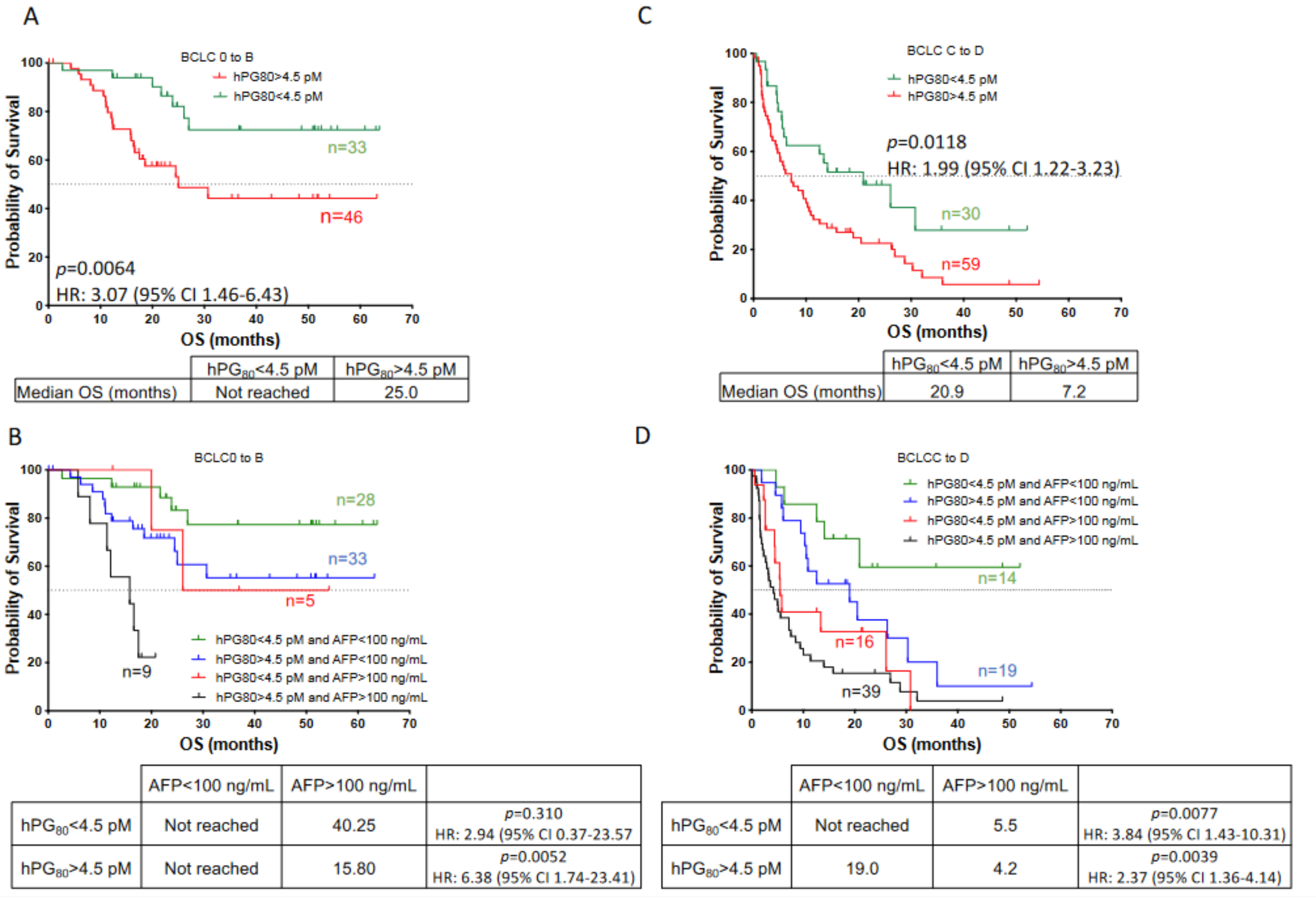
3.6. hPG80 and AFP Levels According to the BCLC Score in HCC Patients
3.7. Prognosis Performance of hPG80 and AFP According to the BCLC Score in HCC Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Villanueva, A. Hepatocellular Carcinoma. Reply. N. Engl. J. Med. 2019, 381, e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Boileve, A.; Hilmi, M.; Delaye, M.; Tijeras-Raballand, A.; Neuzillet, C. Biomarkers in Hepatobiliary Cancers: What is Useful in Clinical Practice? Cancers 2021, 13, 708. [Google Scholar] [CrossRef]
- Craig, A.J.; von Felden, J.; Garcia-Lezana, T.; Sarcognato, S.; Villanueva, A. Tumour evolution in hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 2020, 17, 139–152. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [Green Version]
- D’Amico, G.; Morabito, A.; D’Amico, M.; Pasta, L.; Malizia, G.; Rebora, P.; Valsecchi, M.G. Clinical states of cirrhosis and competing risks. J. Hepatol. 2018, 68, 563–576. [Google Scholar] [CrossRef] [Green Version]
- Llovet, J.M.; Kelley, R.K.; Villanueva, A.; Singal, A.G.; Pikarsky, E.; Roayaie, S.; Lencioni, R.; Koike, K.; Zucman-Rossi, J.; Finn, R.S. Hepatocellular carcinoma. Nat. Rev. Dis. Primers 2021, 7, 6. [Google Scholar] [CrossRef]
- Chan, S.L.; Mo, F.; Johnson, P.J.; Siu, D.Y.; Chan, M.H.; Lau, W.Y.; Lai, P.B.; Lam, C.W.; Yeo, W.; Yu, S.C. Performance of serum alpha-fetoprotein levels in the diagnosis of hepatocellular carcinoma in patients with a hepatic mass. HPB 2014, 16, 366–372. [Google Scholar] [CrossRef] [Green Version]
- You, B.; Mercier, F.; Assenat, E.; Langlois-Jacques, C.; Glehen, O.; Soule, J.; Payen, L.; Kepenekian, V.; Dupuy, M.; Belouin, F.; et al. The oncogenic and druggable hPG80 (Progastrin) is overexpressed in multiple cancers and detected in the blood of patients. EBioMedicine 2019, 51, 102574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehfeld, J.F.; Zhu, X.; Norrbom, C.; Bundgaard, J.R.; Johnsen, A.H.; Nielsen, J.E.; Vikesaa, J.; Stein, J.; Dey, A.; Steiner, D.F.; et al. Prohormone convertases 1/3 and 2 together orchestrate the site-specific cleavages of progastrin to release gastrin-34 and gastrin-17. Biochem. J. 2008, 415, 35–43. [Google Scholar] [CrossRef] [Green Version]
- Varro, A.; Voronina, S.; Dockray, G.J. Pathways of processing of the gastrin precursor in rat antral mucosa. J. Clin. Investig. 1995, 95, 1642–1649. [Google Scholar] [CrossRef] [PubMed]
- Siddheshwar, R.K.; Gray, J.C.; Kelly, S.B. Plasma levels of progastrin but not amidated gastrin or glycine extended gastrin are elevated in patients with colorectal carcinoma. Gut 2001, 48, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Kohli, M.; Tan, W.; Vire, B.; Liaud, P.; Blairvacq, M.; Berthier, F.; Rouison, D.; Garnier, G.; Payen, L.; Cousin, T.; et al. Prognostic Value of Plasma hPG80 (Circulating Progastrin) in Metastatic Renal Cell Carcinoma. Cancers 2021, 13, 375. [Google Scholar] [CrossRef]
- Prieur, A.; Cappellini, M.; Habif, G.; Lefranc, M.P.; Mazard, T.; Morency, E.; Pascussi, J.M.; Flaceliere, M.; Cahuzac, N.; Vire, B.; et al. Targeting the Wnt Pathway and Cancer Stem Cells with Anti-progastrin Humanized Antibodies as a Potential Treatment for K-RAS-Mutated Colorectal Cancer. Clin. Cancer Res. 2017, 23, 5267–5280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalaf, A.M.; Fuentes, D.; Morshid, A.I.; Burke, M.R.; Kaseb, A.O.; Hassan, M.; Hazle, J.D.; Elsayes, K.M. Role of Wnt/beta-catenin signaling in hepatocellular carcinoma, pathogenesis, and clinical significance. J. Hepatocell. Carcinoma 2018, 5, 61–73. [Google Scholar] [CrossRef] [Green Version]
- Hollande, F.; Lee, D.J.; Choquet, A.; Roche, S.; Baldwin, G.S. Adherens junctions and tight junctions are regulated via different pathways by progastrin in epithelial cells. J. Cell Sci. 2003, 116, 1187–1197. [Google Scholar] [CrossRef] [Green Version]
- Singh, P.; Owlia, A.; Varro, A.; Dai, B.; Rajaraman, S.; Wood, T. Gastrin gene expression is required for the proliferation and tumorigenicity of human colon cancer cells. Cancer Res. 1996, 56, 4111–4115. [Google Scholar]
- Wu, H.; Owlia, A.; Singh, P. Precursor peptide progastrin(1-80) reduces apoptosis of intestinal epithelial cells and upregulates cytochrome c oxidase Vb levels and synthesis of ATP. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 285, G1097–G1110. [Google Scholar] [CrossRef] [Green Version]
- Giraud, J.; Failla, L.M.; Pascussi, J.M.; Lagerqvist, E.L.; Ollier, J.; Finetti, P.; Bertucci, F.; Ya, C.; Gasmi, I.; Bourgaux, J.F.; et al. Autocrine Secretion of Progastrin Promotes the Survival and Self-Renewal of Colon Cancer Stem-like Cells. Cancer Res. 2016, 76, 3618–3628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najib, S.; Kowalski-Chauvel, A.; Do, C.; Roche, S.; Cohen-Jonathan-Moyal, E.; Seva, C. Progastrin a new pro-angiogenic factor in colorectal cancer. Oncogene 2015, 34, 3120–3130. [Google Scholar] [CrossRef]
- Cappellini, M.; Flaceliere, M.; Saywell, V.; Soule, J.; Blanc, E.; Belouin, F.; Ortiz, E.; Canterel-Thouennon, L.; Poupeau, S.; Tigrett, S.; et al. A novel method to detect hPG80 (human circulating progastrin) in the blood. Anal. Methods 2021, 13, 4468–4477. [Google Scholar] [CrossRef] [PubMed]
- Calderaro, J.; Ziol, M.; Paradis, V.; Zucman-Rossi, J. Molecular and histological correlations in liver cancer. J. Hepatol. 2019, 71, 616–630. [Google Scholar] [CrossRef] [Green Version]
- Notarpaolo, A.; Layese, R.; Magistri, P.; Gambato, M.; Colledan, M.; Magini, G.; Miglioresi, L.; Vitale, A.; Vennarecci, G.; Ambrosio, C.D.; et al. Validation of the AFP model as a predictor of HCC recurrence in patients with viral hepatitis-related cirrhosis who had received a liver transplant for HCC. J. Hepatol. 2017, 66, 552–559. [Google Scholar] [CrossRef]
- Zhou, L.; Rui, J.A.; Wang, S.B.; Chen, S.G.; Qu, Q. The significance of serum AFP cut-off values, 20 and 400 ng/mL in curatively resected patients with hepatocellular carcinoma and cirrhosis might be of difference. Hepatogastroenterology 2012, 59, 840–843. [Google Scholar] [CrossRef]
- Kinoshita, A.; Onoda, H.; Fushiya, N.; Koike, K.; Nishino, H.; Tajiri, H. Staging systems for hepatocellular carcinoma: Current status and future perspectives. World J. Hepatol. 2015, 7, 406–424. [Google Scholar] [CrossRef]
- Zhang, N.; Gu, J.; Yin, L.; Wu, J.; Du, M.Y.; Ding, K.; Huang, T.; He, X. Incorporation of alpha-fetoprotein(AFP) into subclassification of BCLC C stage hepatocellular carcinoma according to a 5-year survival analysis based on the SEER database. Oncotarget 2016, 7, 81389–81401. [Google Scholar] [CrossRef] [Green Version]
- Duvoux, C.; Roudot-Thoraval, F.; Decaens, T.; Pessione, F.; Badran, H.; Piardi, T.; Francoz, C.; Compagnon, P.; Vanlemmens, C.; Dumortier, J.; et al. Liver transplantation for hepatocellular carcinoma: A model including alpha-fetoprotein improves the performance of Milan criteria. Gastroenterology 2012, 143, 986–994. [Google Scholar] [CrossRef]
- West, J.; Card, T.R.; Aithal, G.P.; Fleming, K.M. Risk of hepatocellular carcinoma among individuals with different aetiologies of cirrhosis: A population-based cohort study. Aliment. Pharmacol. Ther. 2017, 45, 983–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamashita, T.; Koshikawa, N.; Shimakami, T.; Terashima, T.; Nakagawa, M.; Nio, K.; Horii, R.; Iida, N.; Kawaguchi, K.; Arai, K.; et al. Serum Laminin gamma2 Monomer as a Diagnostic and Predictive Biomarker for Hepatocellular Carcinoma. Hepatology 2021, 74, 760–775. [Google Scholar] [CrossRef]
- Hoshida, Y.; Nijman, S.M.; Kobayashi, M.; Chan, J.A.; Brunet, J.P.; Chiang, D.Y.; Villanueva, A.; Newell, P.; Ikeda, K.; Hashimoto, M.; et al. Integrative transcriptome analysis reveals common molecular subclasses of human hepatocellular carcinoma. Cancer Res. 2009, 69, 7385–7392. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyault, S.; Rickman, D.S.; de Reynies, A.; Balabaud, C.; Rebouissou, S.; Jeannot, E.; Herault, A.; Saric, J.; Belghiti, J.; Franco, D.; et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology 2007, 45, 42–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelizzaro, F.; Cardin, R.; Penzo, B.; Pinto, E.; Vitale, A.; Cillo, U.; Russo, F.P.; Farinati, F. Liquid Biopsy in Hepatocellular Carcinoma: Where Are We Now? Cancers 2021, 13, 2274. [Google Scholar] [CrossRef] [PubMed]
- Costentin, C.E.; Mourad, A.; Lahmek, P.; Causse, X.; Pariente, A.; Hagege, H.; Dobrin, A.S.; Becker, C.; Marks, B.; Bader, R.; et al. Hepatocellular carcinoma is diagnosed at a later stage in alcoholic patients: Results of a prospective, nationwide study. Cancer 2018, 124, 1964–1972. [Google Scholar] [CrossRef] [PubMed]

| Cohort | HCC N (%) n = 168 | |
|---|---|---|
| Age, years | Median (range) | 67 (27–85) |
| Gender | Male | 149 (88.7%) |
| Female | 19 (11.3%) | |
| Laboratory values | ||
| hPG80 | Median (IQR), pM | 7.64 (2.53–28.28) |
| Mean (SE), pM | 25.52 (4.16) | |
| AFP | Median (IQR), ng/mL | 40.20 (5.55–712.50) |
| Mean (SE), ng/mL | 5066 (2340) | |
| Etiology | ||
| NASH | Y | 31 (18.5%) |
| N | 137 (81.5%) | |
| Alcohol consumption | Y | 107 (63.7%) |
| N | 61 (36.3%) | |
| Hepatitis B virus | Y | 13 (7.7%) |
| N | 155 (92.3%) | |
| Hepatitis C virus | Y | 45 (26.8%) |
| N | 123 (73.2%) | |
| Tumor size | <3 cm | 54 (49.1%) |
| 3 to 5 cm | 23 (20.9%) | |
| >5 cm | 33 (30.0%) | |
| Vascular invasion | Y | 57 (33.9%) |
| N | 108 (64.3%) | |
| Unspecified | 3 (1.8%) | |
| Cirrhosis | Y | 138 (82.1%) |
| N | 30 (17.9%) | |
| BCLC | 0 | 10 (6.0%) |
| A | 34 (20.2%) | |
| B | 35 (20.8%) | |
| C | 86 (51.2%) | |
| D | 3 (1.8%) | |
| hPG80 (cutoff: 4.5 pM) and AFP (cutoff: 100 ng/mL) levels | neg/neg | 42 (25.5%) |
| neg/pos | 21 (12.7%) | |
| pos/neg | 54 (32.7%) | |
| pos/pos | 48 (29.1%) | |
| Treatments | Radiofrequency | 20 (11.9%) |
| Surgery | 5 (3.0%) | |
| Transplantation | 8 (4.7%) | |
| TACE | 28 (16.7%) | |
| SIRT | 6 (3.6%) | |
| Sorafenib | 50 (29.7%) | |
| Others TKI | 10 (6.0%) | |
| Gemox | 2 (1.2%) | |
| Immunotherapy | 20 (11.9%) | |
| Supportive care | 19 (11.3%) | |
| hPG80 < 4.5 pM | hPG80 > 4.5 pM | p | AFP < 100 ng/mL | AFP > 100 ng/mL | p | ||
|---|---|---|---|---|---|---|---|
| Alcohol | Y | 35 | 72 | 0.0996 | 66 | 40 | 0.1882 |
| N | 28 | 33 | 30 | 29 | |||
| HCV | Y | 15 | 30 | 0.5904 | 28 | 16 | 0.4761 |
| N | 48 | 75 | 68 | 53 | |||
| NASH | Y | 11 | 20 | 0.2568 | 14 | 17 | 0.1029 |
| N | 52 | 85 | 82 | 52 | |||
| Tumor size | <3 cm | 22 | 29 | 0.1193 | 44 | 7 | <0.0001 |
| 3 to 5 cm | 10 | 13 | 19 | 4 | |||
| >5 cm | 8 | 27 | 15 | 19 | |||
| Vascular invasion | Y | 14 | 42 | 0.0182 | 17 | 39 | <0.0001 |
| N | 48 | 61 | 78 | 28 | |||
| AFP score | 0 | 13 | 14 | 0.6905 | 37 | 0 | <0.0001 |
| 1 | 6 | 8 | 14 | 0 | |||
| 2 | 4 | 10 | 10 | 4 | |||
| >3 | 7 | 10 | 8 | 9 | |||
| CRP | mean (sd) | 15.7 (34.8) | 26.2 (38.5) | 0.1359 | 15.6 (31.4) | 32.6 (43) | 0.0138 |
| Median (range) | 4 (0.3–212) | 9.7 (0.5–210.0) | 5.2 (0.3–212) | 14.7 (0.5–210) | |||
| BCLC | 0 | 6 | 4 | 0.3183 | 9 | 0 | <0.0001 |
| A | 12 | 22 | 29 | 5 | |||
| B | 15 | 20 | 25 | 9 | |||
| C | 30 | 56 | 35 | 52 | |||
| D | 0 | 3 | 0 | 3 | |||
| Tumor differentiation | Poor | 6 | 10 | 0.0529 | 11 | 5 | 0.6533 |
| intermediate | 32 | 30 | 39 | 22 | |||
| good | 3 | 13 | 8 | 7 | |||
| GS Score | 0–3 | 15 | 6 | 0.0068 | 4 | 6 | 0.3015 |
| 4–6 | 19 | 33 | 38 | 24 | |||
| CK19 | pos | 2 | 4 | 0.6787 | 4 | 2 | 0.6654 |
| neg | 32 | 35 | 38 | 28 | |||
| p53 | pos | 13 | 9 | 0.1591 | 11 | 11 | 0.3414 |
| neg | 21 | 30 | 31 | 19 | |||
| EPCAM | pos | 5 | 1 | 0.0492 | 3 | 3 | 0.7895 |
| neg | 14 | 21 | 19 | 15 | |||
| p53 or CK19 or EPCAM | pos | 12 | 5 | 0.0088 | 9 | 10 | 0.3561 |
| neg | 7 | 17 | 13 | 8 | |||
| Characteristics | hPG80 > 4.5 pM | AFP > 100 ng/mL | ||
|---|---|---|---|---|
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
| Alcohol | 1.745 | 0.915–3.340 | 0.627 | 0.328–1.194 |
| HCV | 1.280 | 0.631–2.674 | 0.733 | 0.354–1.480 |
| NASH | 1.112 | 0.501–2.578 | 1.915 | 0.872–4.266 |
| Tumor size | ||||
| <3 cm | 0.986 | 0.365–2.706 | 1.105 | 0.268–3.979 |
| 3 to 5 cm | 2.655 | 1.044–7.268 | 5.559 | 2.096–15.915 |
| Vascular invasion | 2.361 | 1.177–4.941 | 6.391 | 3.179–13.344 |
| AFP score | ||||
| 1 | 1.238 | 0.338–4.697 | ||
| 2 | 2.321 | 0.608–10.189 | ||
| >3 | 1.327 | 0.391–4.649 | ||
| BCLC | ||||
| B | 0.923 | 0.374–2.282 | 2.736 | 0.844–9.808 |
| C-D | 1.362 | 0.642–2.865 | 12.667 | 4.898–39.672 |
| Tumor differentiation | ||||
| intermediate | 0.563 | 0.173–1.705 | 1.241 | 0.395–4.360 |
| good | 2.600 | 0.543–14.854 | 1.925 | 0.450–8.768 |
| GS Score 4–6 | 4.342 | 1.499–13.966 | 0.933 | 0.334–2.662 |
| p53 | 0.485 | 0.171–1.326 | 1.632 | 0.591–4.543 |
| OS | |||
|---|---|---|---|
| Hazard Ratio | 95% CI | p | |
| hPG80 | 0.48 | 0.30–0.78 | 0.003 |
| AFP | 1.40 | 0.91–2.15 | 0.121 |
| BCLC | |||
| A | 0.71 | 0.18–2.78 | 0.623 |
| B | 1.73 | 0.50–5.94 | 0.383 |
| C | 4.72 | 1.46–15.25 | 0.009 |
| D | 65.42 | 10.81–396.11 | <0.001 |
| Age | 1.03 | 1.01–1.05 | 0.013 |
| Gender | 4.54 | 1.71–12.03 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dupuy, M.; Iltache, S.; Rivière, B.; Prieur, A.; Pageaux, G.P.; Bedoya, J.U.; Faure, S.; Guillaumée, H.; Assenat, E. Plasma hPG80 (Circulating Progastrin) as a Novel Prognostic Biomarker for Hepatocellular Carcinoma. Cancers 2022, 14, 402. https://doi.org/10.3390/cancers14020402
Dupuy M, Iltache S, Rivière B, Prieur A, Pageaux GP, Bedoya JU, Faure S, Guillaumée H, Assenat E. Plasma hPG80 (Circulating Progastrin) as a Novel Prognostic Biomarker for Hepatocellular Carcinoma. Cancers. 2022; 14(2):402. https://doi.org/10.3390/cancers14020402
Chicago/Turabian StyleDupuy, Marie, Sarah Iltache, Benjamin Rivière, Alexandre Prieur, George Philippe Pageaux, José Ursic Bedoya, Stéphanie Faure, Heloïse Guillaumée, and Eric Assenat. 2022. "Plasma hPG80 (Circulating Progastrin) as a Novel Prognostic Biomarker for Hepatocellular Carcinoma" Cancers 14, no. 2: 402. https://doi.org/10.3390/cancers14020402




