Association of Sentinel Node Biopsy and Pathological Report Completeness with Survival Benefit for Cutaneous Melanoma and Factors Influencing Their Different Uses in European Populations
Abstract
:Simple Summary
Abstract
1. Introduction
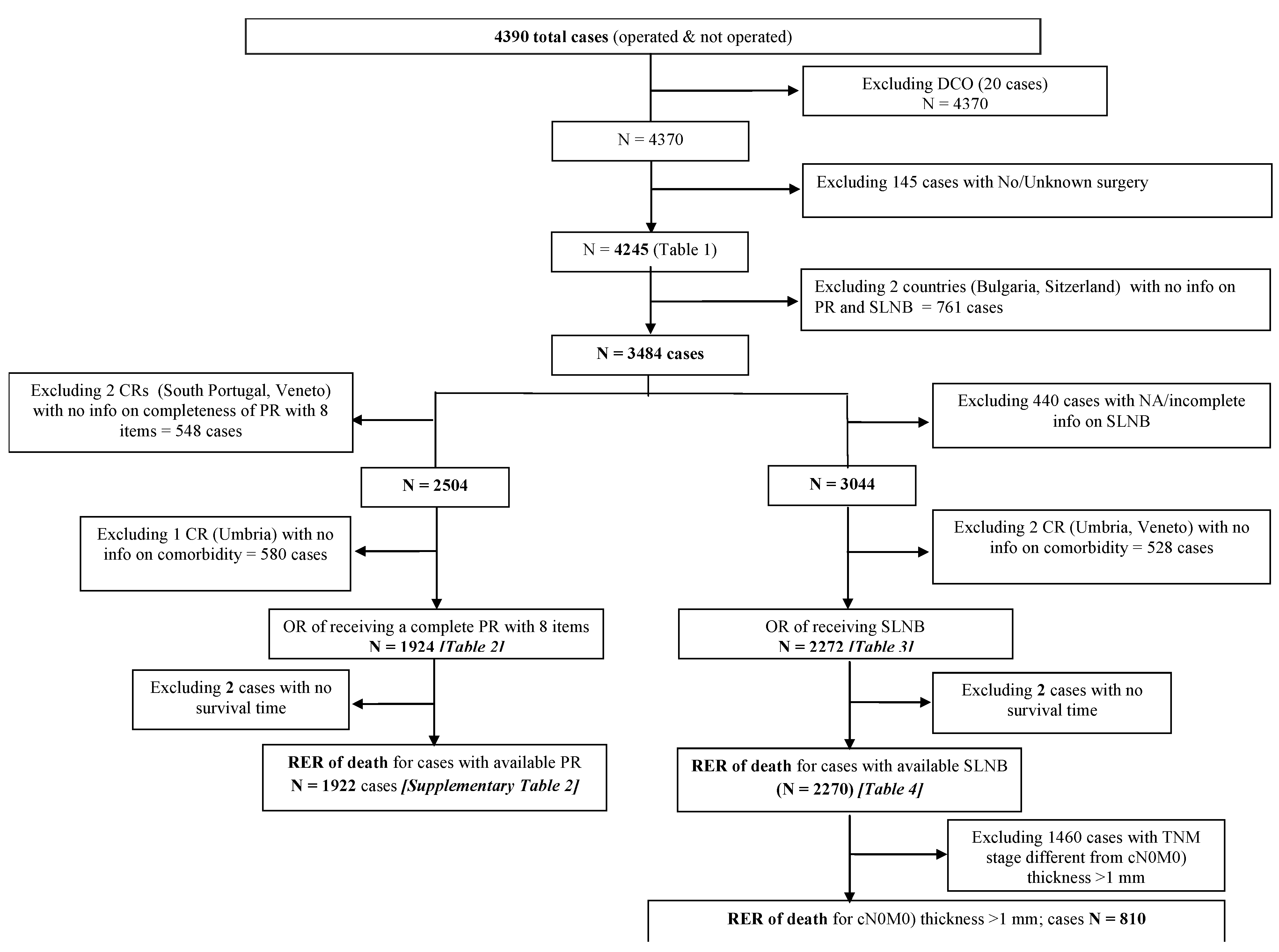
2. Methods
Statistical Analysis
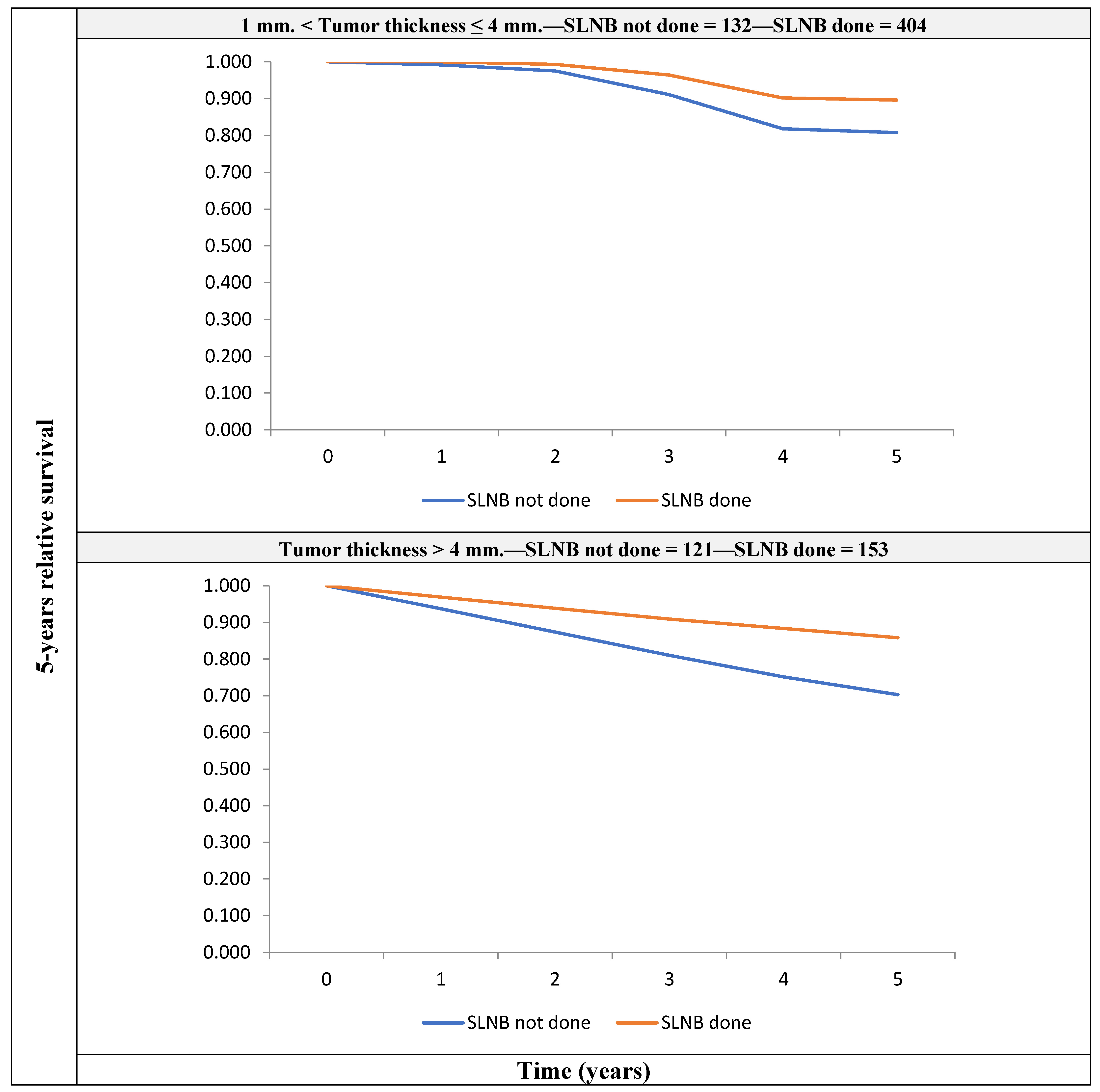
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dummer, R.; Hauschild, A.; Lindenblatt, N.; Pentheroudakis, G.; Keilholz, U. Cutaneous melanoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26, v126–v132. [Google Scholar] [CrossRef] [PubMed]
- Karim, R.Z.; Van Den Berg, K.S.; Colman, M.H.; McCarthy, S.W.; Thompson, J.F.; Scolyer, R.A. The advantage of using a synoptic pathology report format for cutaneous melanoma. Histopathology 2007, 52, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Scolyer, R.A.; Rawson, R.V.; Gershenwald, J.E.; Ferguson, P.M.; Prieto, V.G. Melanoma pathology reporting and staging. Mod. Pathol. 2020, 33, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Tumino, R.; Minicozzi, P.; Frasca, G.; Allemani, C.; Crocetti, E.; Ferretti, S.; Giacomin, A.; Natali, M.; Mangone, L.; Falcini, F.; et al. Population-based method for investigating adherence to international recommendations for pathology reporting of primary cutaneous melanoma: Results of a EUROCARE-5 high resolution study. Cancer Epidemiol. 2015, 39, 424–429. [Google Scholar] [CrossRef]
- Jobson, D.; Roffey, B.; Arnold, C.; Azzi, A.; Button-Sloan, A.; Dawson, T.; Fernandez-Penas, P.; Fishburn, P.; Gyorki, D.E.; Hiscutt, E.L.; et al. Development of melanoma clinical quality indicators for the Australian melanoma clinical outcomes registry (MelCOR): A modified Delphi study. Australas. J. Dermatol. 2022, 63, 344–351. [Google Scholar] [CrossRef]
- McKay, D.R.; Nguyen, P.; Wang, A.; Hanna, T.P. A population-based study of administrative data linkage to measure melanoma surgical and pathology quality. PLoS ONE 2022, 17, e0263713. [Google Scholar] [CrossRef]
- Morton, D.L.; Thompson, J.F.; Cochran, A.J.; Mozzillo, N.; Elashoff, R.; Essner, R.; Nieweg, O.E.; Roses, D.F.; Hoekstra, H.J.; Karakousis, C.P.; et al. Sentinel-Node Biopsy or Nodal Observation in Melanoma. N. Engl. J. Med. 2006, 355, 1307–1317. [Google Scholar] [CrossRef]
- Morton, D.L.; Thompson, J.F.; Cochran, A.J.; Mozzillo, N.; Nieweg, O.E.; Roses, D.F.; Hoekstra, H.J.; Karakousis, C.P.; Puleo, C.A.; Coventry, B.J.; et al. Final Trial Report of Sentinel-Node Biopsy versus Nodal Observation in Melanoma. N. Engl. J. Med. 2014, 370, 599–609. [Google Scholar] [CrossRef]
- Madu, M.F.; Wouters, M.W.J.M.; van Akkooi, A.C.J. Sentinel node biopsy in melanoma: Current controversies addressed. Eur. J. Surg. Oncol. 2017, 43, 517–533. [Google Scholar] [CrossRef]
- Stadler, R.; Leiter, U.; Garbe, C. Lack of survival benefit in sentinel lymph node-positive melanoma with immediate complete lymphadenectomy—A review. J. Ger. Soc. Dermatol. 2019, 17, 7–13. [Google Scholar] [CrossRef]
- Guevara, M.; Rodríguez-Barranco, M.; Puigdemont, M.; Minicozzi, P.; Yanguas-Bayona, I.; Porras-Povedano, M.; Rubió-Casadevall, J.; Sánchez Pérez, M.J.; Marcos-Gragera, R.; Ardanaz, E. Disparities in the management of cutaneous malignant melanoma. A population-based high-resolution study. Eur. J. Cancer Care 2019, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Verstijnen, J.; Damude, S.; Hoekstra, H.J.; Kruijff, S.; ten Tije, A.J.; Louwman, W.J.; Bastiaannet, E.; Stuiver, M.M. Practice variation in Sentinel Lymph Node Biopsy for melanoma patients in different geographical regions in the Netherlands. Surg. Oncol. 2017, 26, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, E.; Windemuth-Kieselbach, C.; Eigentler, T.K.; Rompel, R.; Trefzer, U.; Nashan, D.; Rotterdam, S.; Ugurel, S.; Schadendorf, D. A first prospective population-based analysis investigating the actual practice of melanoma diagnosis, treatment and follow-up. Eur. J. Cancer 2011, 47, 1977–1989. [Google Scholar] [CrossRef] [PubMed]
- W.H.O. (WHO) International Classification of Diseases for Oncology (ICD-O), 3rd ed.; 1st revision; WHO Libr. Cat., III; World Health Organization: La Valletta, Malta, 2013. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Sobin, L.H.; Gospodarowicz, M.K.; Wittekind, C.H. (Eds.) TNM Classification of Malignant Tumours, 7th ed.; Wiley: Chichester, UK, 2010; p. 310. [Google Scholar]
- Menard, S. Applied Logistic Regression Analysis; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2002. [Google Scholar] [CrossRef]
- Ederer, F.; Axtell, L.M.; Cutler, S.J. The relative survival: A statistical methodology. J. Natl. Cancer Inst. Monogr. 1961, 6, 101–121. [Google Scholar]
- Dickman, P.W.; Coviello, E. Estimating and modeling relative survival. Stata J. 2015, 15, 186–215. [Google Scholar] [CrossRef]
- Akaike, H. Information theory and an extension of maximum likelihood principle. In Second International Symposium on Information Theory; Petrov, B.N., Csáki, F., Eds.; Akademiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Thompson, J.F.; Scolyer, R.A. Cooperation between surgical oncologists and pathologists: A key element of multidisciplinary care for patients with cancer. Pathology 2004, 36, 496–503. [Google Scholar] [CrossRef]
- Scolyer, R.A.; Judge, M.J.; Evans, A.; Frishberg, D.P.; Prieto, V.G.; Thompson, J.F.; Trotter, M.J.; Walsh, M.Y.; Walsh, N.M.; Ellis, D.W. International Collaboration on Cancer Reporting. Data set for pathology reporting of cutaneous invasive melanoma: Recommendations from the international collaboration on cancer reporting (ICCR). Am. J. Surg. Pathol. 2013, 37, 1797–1814. [Google Scholar] [CrossRef]
- Blakely, A.M.; Comissiong, D.S.; Vezeridis, M.P.; Miner, T.J. Suboptimal Compliance With National Comprehensive Cancer Network Melanoma Guidelines. Am. J. Clin. Oncol. 2018, 41, 754–759. [Google Scholar] [CrossRef]
- Thompson, B.; Austin, R.; Coory, M.; Aitken, J.F.; Walpole, E.; Francis, G.; Fritschi, L. Completeness of Histopathology Reporting of Melanoma in a High-Incidence Geographical Region. Dermatology 2009, 218, 7–14. [Google Scholar] [CrossRef]
- Haydu, L.E.; Holt, P.E.; Karim, R.Z.; Madronio, C.M.; Thompson, J.F.; Armstrong, B.K.; Scolyer, R.A. Quality of histopathological reporting on melanoma and influence of use of a synoptic template. Histopathology 2010, 56, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Maley, A.; Patrawala, S.; Stoff, B. Compliance with the College of American Pathologists Protocol for Melanoma in Synoptic and Non-Synoptic reports: A cross-sectional study. J. Am. Acad. Dermatol. 2016, 74, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Narang, J.; Hue, J.J.; Bingmer, K.; Hardacre, J.M.; Winter, J.M.; Ocuin, L.M.; Ammori, J.B.; Mangla, A.; Bordeaux, J.; Rothermel, L.D. Sentinel lymph node biopsy guideline concordance in melanoma: Analysis of the National Cancer Database. J. Surg. Oncol. 2021, 124, 669–678. [Google Scholar] [CrossRef]
- Murtha, T.D.; Han, G.; Han, D. Predictors for Use of Sentinel Node Biopsy and the Association with Improved Survival in Melanoma Patients Who Have Nodal Staging. Ann. Surg. Oncol. 2018, 25, 903–911. [Google Scholar] [CrossRef] [PubMed]
- Sant, M.; Minicozzi, P.; Allemani, C.; Cirilli, C.; Federico, M.; Capocaccia, R.; Budroni, M.; Candela, P.; Crocetti, E.; Falcini, F.; et al. Regional inequalities in cancer care persist in Italy and can influence survival. Cancer Epidemiol. 2012, 36, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Gershenwald, J.E.; Ross, M.I. Sentinel-Lymph-Node Biopsy for Cutaneous Melanoma. N. Engl. J. Med. 2011, 364, 1738–1745. [Google Scholar] [CrossRef]
- Hayek, S.A.; Munoz, A.; Dove, J.T.; Hunsinger, M.; Arora, T.; Wild, J.; Shabahang, M.; Blansfield, J. Hospital-Based study of compliance with nCCN guidelines and predictive factors of sentinel lymph node biopsy in the setting of thin melanoma using the national cancer database. Am. Surg. 2018, 84, 672–679. [Google Scholar] [CrossRef]
- Sekula-Gibbs, S.A.; Shearer, M.A. Sentinel node biopsy should be offered in thin melanoma with mitotic rate greater than one. Dermatol. Surg. 2011, 37, 1080–1088. [Google Scholar] [CrossRef]
- Maurichi, A.; Miceli, R.; Patuzzo, R.; Barretta, F.; Gallino, G.; Mattavelli, I.; Barbieri, C.; Leva, A.; Cortinovis, U.; Tolomio, E.; et al. Analysis of sentinel node biopsy and clinicopathologic features as prognostic factors in patients with atypical melanocytic tumors. J. Natl. Compr. Cancer Netw. 2020, 18, 1327–1336. [Google Scholar] [CrossRef]
- Innos, K.; Padrik, P.; Valvere, V.; Aareleid, T. Sex differences in cancer survival in Estonia: A population-based study. BMC Cancer 2015, 15, 72. [Google Scholar] [CrossRef]
- Lasithiotakis, K.; Leiter, U.; Meier, F.; Eigentler, T.; Metzler, G.; Moehrle, M.; Breuninger, H.; Garbe, C. Age and gender are significant independent predictors of survival in primary cutaneous melanoma. Cancer 2008, 112, 1795–1804. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.J.; Lambert, P.C.; Rutherford, M.J. Understanding the impact of sex and stage differences on melanoma cancer patient survival: A SEER-based study. Br. J. Cancer 2021, 124, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Crocetti, E.; Mallone, S.; Robsahm, T.E.; Gavin, A.; Agius, D.; Ardanaz, E.; Lopez, M.C.; Innos, K.; Minicozzi, P.; Borgognoni, L.; et al. EUROCARE-5 Working Group. Survival of patients with skin melanoma in Europe increases further: Results of the EUROCARE-5 study. Eur. J. Cancer 2015, 51, 2179–2190. [Google Scholar] [CrossRef]
- Grann, A.F.; Frøslev, T.; Olesen, A.B.; Schmidt, H.; Lash, T.L. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: A registry-based cohort study. Br. J. Cancer 2013, 109, 265–271. [Google Scholar] [CrossRef]
- Chang, C.K.; Hsieh, Y.S.; Chen, P.N.; Chu, S.C.; Huang, J.Y.; Wang, Y.H.; Wei, J.C. A Cohort Study: Comorbidity and Stage Affected the Prognosis of Melanoma Patients in Taiwan. Front. Oncol. 2022, 12, 846760. [Google Scholar] [CrossRef]
- Garbe, C.; Eigentler, T.K.; Keilholz, U.; Hauschild, A.; Kirkwood, J.M. Systematic review of medical treatment in melanoma: Current status and future prospects. Oncologist 2011, 16, 5–24. [Google Scholar] [CrossRef]
| All patients | Bulgaria | Estonia | Italy | Portugal | Spain | Switzerland | |
|---|---|---|---|---|---|---|---|
| N (%) | 4245 (100.0) | 295 (6.9) | 345 (8.1) | 1483 (34.9) | 732 (17.2) | 924 (21.8) | 466 (10.9) |
| Sex | |||||||
| Men | 2066 (48.7) | 142 (48.1) | 137 (39.7) | 765 (51.6) | 334 (45.6) | 451 (48.8) | 237 (50.9) |
| Women | 2179 (51.3) | 153 (51.9) | 208 (60.3) | 718 (48.4) | 398 (54.4) | 473 (51.2) | 229 (49.1) |
| Age at diagnosis (years) | |||||||
| 15–54 | 1621 (38.2) | 89 (30.2) | 132 (38.3) | 607 (40.9) | 275 (37.6) | 355 (38.4) | 163 (35.0) |
| 55–64 | 801 (18.9) | 80 (27.1) | 59 (17.1) | 263 (17.7) | 149 (20.4) | 165 (17.9) | 85 (18.2) |
| 65–74 | 856 (20.2) | 62 (21) | 81 (23.5) | 293 (19.8) | 148 (20.2) | 175 (18.9) | 97 (20.8) |
| ≥75 | 967 (22.8) | 64 (21.7) | 73 (21.2) | 320 (21.6) | 160 (21.9) | 229 (24.8) | 121 (26) |
| Anatomical Site | |||||||
| Head & neck | 624 (14.7) | 61 (20.7) | 34 (9.8) | 161 (10.9) | 105 (14.3) | 191 (20.7) | 72 (15.5) |
| Trunk | 1696 (40) | 124 (42) | 182 (52.8) | 590 (39.8) | 248 (33.9) | 366 (39.6) | 186 (39.9) |
| Upper limb & shoulder | 631 (14.9) | 28 (9.5) | 49 (14.2) | 220 (14.8) | 119 (16.3) | 125 (13.5) | 90 (19.3) |
| Lower limb & hip | 1061 (25) | 67 (22.7) | 77 (22.3) | 337 (22.7) | 254 (34.7) | 211 (22.8) | 115 (24.7) |
| Skin NOS | 233 (5.5) | 15 (5.1) | 3 (0.9) | 175 (11.8) | 6 (0.82) | 31 (3.35) | 3 (0.64) |
| Histological subtype 1 | |||||||
| Nodular melanoma | 444 (10.5) | 65 (22) | 18 (5.2) | 131 (8.8) | 90 (12.3) | 114 (12.3) | 26 (5.6) |
| Lentigo maligna | 233 (5.5) | 4 (1.4) | 6 (1.7) | 38 (2.6) | 26 (3.5) | 115 (12.4) | 44 (9.44) |
| Superficial spreading | 1698 (40) | 21 (7.1) | 12 (3.5) | 542 (36.6) | 307 (41.9) | 493 (53.4) | 323 (69.3) |
| Acral lentiginous melanoma | 101 (2.4) | 1 (0.3) | 13 (3.8) | 20 (1.3) | 32 (4.37) | 21 (2.27) | 14 (3) |
| Other | 715 (16.8) | 15 (5.1) | 174 (50.4) | 431 (29.1) | 23 (3.1) | 63 (6.8) | 9 (1.9) |
| NOS | 1053 (24.8) | 189 (64.1) | 122 (35.4) | 320 (21.6) | 254 (34.7) | 118 (12.8) | 50 (10.7) |
| Place of Primary Surgery | |||||||
| Specialized hospital | 2189 (51.6) | 253 (85.8) | 298 (86.4) | 781 (52.7) | 214 (29.2) | 557 (60.3) | 86 (18.5) |
| General hospital | 1026 (24.2) | 32 (10.8) | 25 (7.2) | 119 (8) | 490 (66.9) | 360 (39.0) | 0 (0.0) |
| Outpatient | 400 (9.4) | 0 (0.0) | 15 (4.4) | 0 (0.0) | 1 (0.14) | 6 (0.6) | 378 (81.1) |
| Unknown | 630 (14.8) | 10 (3.4) | 7 (2) | 583 (39.3) | 27 (3.7) | 1 (0.1) | 2 (0.4) |
| Completeness of pathological report 2 | |||||||
| Complete (8 histopathological items) | 528 (15.2) | NA | 8 (2.3) | 298 (20.1) | 58 (7.9) | 164 (17.8) | NA |
| Incomplete (<8 items), unknown, not available | 2956 (84.8) | NA | 337 (97.7) | 1185 (79.9) | 674 (92.1) | 760 (82.2) | NA |
| Sentinel Lymph Node Biopsy 3 | |||||||
| Done | 1485 (42.6) | NA | 156 (45.2) | 564 (38.0) | 424 (57.9) | 341 (36.9) | NA |
| Not done | 1559 (44.7) | NA | 159 (46.1) | 555 (37.4) | 302 (41.3) | 543 (58.8) | NA |
| Unknown | 440 (12.6) | NA | 30 (8.7) | 364 (24.5) | 6 (0.8) | 40 (4.3) | NA |
| Sentinel Lymph Node Biopsy in cN0cM0 and Thickness > 1 mm | |||||||
| Done | 557 (68.8) | NA | 94 (65.7) | 112 (69.1) | 228 (81.7) | 123 (54.4) | NA |
| Not done | 253 (31.2) | NA | 49 (34.3) | 50 (30.9) | 51 (18.3) | 103 (45.6) | NA |
| TNM Stage | |||||||
| I | 2313 (54.5) | 78 (26.4) | 180 (52.2) | 884 (59.6) | 380 (51.9) | 596 (64.5) | 195 (41.8) |
| II | 801 (18.9) | 135 (45.8) | 101 (29.3) | 186 (12.5) | 167 (22.8) | 180 (19.5) | 32 (6.9) |
| III | 483 (11.4) | 28 (9.5) | 46 (13.3) | 150 (10.1) | 142 (19.4) | 88 (9.5) | 29 (6.2) |
| IV | 128 (3.0) | 19 (6.4) | 7 (2.0) | 46 (3.1) | 30 (4.1) | 26 (2.8) | 0 (0.0) |
| Incomplete or unknown | 520 (12.2) | 35 (11.9) | 11 (3.2) | 217 (14.6) | 13 (1.8) | 34 (3.7) | 210 (45.1) |
| Charlson comorbidity index (CCI) | |||||||
| CCI 0 | 1490 (68.4) | NA | 225 (65.2) | 1376 (92.8) | 521 (71.2) | 593 (64.2) | NA |
| CCI 1 or higher | 687 (31.9) | NA | 120 (34.8) | 104 (7.0) | 211 (28.8) | 252 (27.3) | NA |
| Unknown | 82 (8.9) | NA | 0 (0.0) | 3 (0.2) | 0 (0.0) | 79 (8.6) | NA |
| N | Adj. OR | 95% CI | p-Value | |
|---|---|---|---|---|
| Total | 441 | |||
| Country 2 | ||||
| Estonia | 8 | 0.11 | [0.06–0.18] | 0.000 |
| Italy | 211 | 6.39 | [4.90–8.34] | 0.000 |
| Portugal | 58 | 1.39 | [1.02–1.89] | 0.038 |
| Spain | 164 | 1.06 | [0.83–1.35] | 0.642 |
| Age at diagnosis (years) | ||||
| 15–54 | 185 | 1.21 | [0.85–1.71] | 0.286 |
| 55–64 | 85 | 1.39 | [0.94–2.06] | 0.096 |
| 65–74 | 78 | 1.06 | [0.73–1.56] | 0.752 |
| 75+ | 93 | 1 | ||
| Sex | ||||
| Men | 209 | 1 | ||
| Women | 232 | 0.97 | [0.76–1.24] | 0.808 |
| Stage at diagnosis | ||||
| I | 223 | 1 | ||
| II | 83 | 1.01 | [0.73–1.40] | 0.937 |
| III | 52 | 0.83 | [0.56–1.22] | 0.336 |
| IV | 5 | 0.22 | [0.08–0.61] | 0.003 |
| Incomplete | 66 | 1.74 | [1.06–2.87] | 0.029 |
| Unknown | 12 | 0.94 | [0.43–2.05] | 0.885 |
| Place of Primary surgery | ||||
| General hospital 3 | 143 | 1 | ||
| Specialized hospital | 298 | 1.42 | [1.08–1.86] | 0.012 |
| Charlson comorbidity index (CCI) | ||||
| CCI 0 | 300 | 1 | ||
| CCI ≥ 1 | 124 | 1.06 | [0.79–1.42] | 0.700 |
| Unknown | 17 | 1.09 | [0.58–1.48] | 0.749 |
| N | Adj. OR | 95% CI | p-Value | |
|---|---|---|---|---|
| Total | 1054 | |||
| Country 1 | ||||
| Estonia | 156 | 0.83 | [0.67–1.02] | 0.078 |
| Italy | 133 | 0.8 | [0.65–0.99] | 0.041 |
| Portugal | 424 | 1.85 | [1.56–2.20] | 0.000 |
| Spain | 341 | 0.82 | [0.70–0.95] | 0.008 |
| Age at diagnosis (years) | ||||
| 15–54 | 444 | 3.3 | [249–4.36] | 0.000 |
| 55–64 | 220 | 3.03 | [2.23–4.13] | 0.000 |
| 65–74 | 224 | 2.25 | [1.68–3.02] | 0.000 |
| 75+ | 166 | 1 | ||
| Sex | ||||
| Men | 488 | 1 | ||
| Women | 566 | 1.10 | [0.92–1.33] | 0.302 |
| Stage at diagnosis | ||||
| I | 449 | 1 | ||
| II | 307 | 3.99 | [3.13–5.10] | 0.000 |
| III | 251 | 7.18 | [5.26–9.79] | 0.000 |
| IV | 23 | 1.10 | [0.64–1.88] | 0.727 |
| Incomplete | 17 | 0.38 | [0.21–0.69] | 0.001 |
| Unknown | 7 | 1.01 | [0.41–2.51] | 0.977 |
| Place of Primary surgery | ||||
| General hospital 3 | 424 | 1 | ||
| Specialized hospital | 630 | 1.86 | [1.50–2.30] | 0.000 |
| Charlson comorbidity index (CCI) | ||||
| CCI 0 | 756 | 1 | ||
| CCI ≥ 1 | 289 | 0.83 | [0.67–1.04] | 0.109 |
| Unknown | 9 | 0.25 | [0.11–0.56] | 0.001 |
| N | RER | 95% CI | p-Value | |
|---|---|---|---|---|
| Country 1 | ||||
| Estonia | 315 | 1.04 | [0.75–1.45] | 0.836 |
| Italy | 347 | 0.94 | [0.63–1.40] | 0.773 |
| Portugal | 726 | 1.09 | [0.86–1.38] | 0.488 |
| Spain | 882 | 0.94 | [0.73–1.21] | 0.631 |
| Age at diagnosis (years) | ||||
| 15–54 | 886 | 0.76 | [0.51–1.12] | 0.162 |
| 55–64 | 415 | 1.03 | [0.68–1.56] | 0.902 |
| 65–74 | 452 | 1.10 | [0.76–1.60] | 0.619 |
| 75+ | 517 | 1 | ||
| Sex | ||||
| Men | 1058 | 1 | ||
| Women | 1212 | 0.82 | [0.62–1.08] | 0.160 |
| Sentinel lymph node biopsy | ||||
| Executed | 1054 | 1 | ||
| Not Executed | 1216 | 1.61 | [1.20–2.15] | 0.002 |
| Mitotic index | ||||
| 0 mitoses per mm2 | 665 | 1 | ||
| ≥1 mitoses per mm2 | 987 | 4.22 | [1.43–12.44] | 0.009 |
| Not mentioned/not available in PR | 618 | 3.32 | [1.10–10.03] | 0.033 |
| Thickness | ||||
| <= 1 mm | 1128 | 0.10 | [0.05-.0.22] | 0.000 |
| 1.01 mm–2 mm | 369 | 0.20 | [0.11–0.38] | 0.000 |
| 2.01 mm–4 mm | 314 | 0.72 | [0.52–0.99] | 0.041 |
| > 4 mm | 414 | 1 | ||
| Unknown | 45 | 0.55 | [0.18–1.65] | 0.287 |
| Ulceration | ||||
| Absent | 579 | 1 | ||
| Present | 1606 | 1.94 | [1.38–2.74] | 0.000 |
| Not mentioned in PR | 85 | 1.78 | [0.63–5.06] | 0.279 |
| Nodal stage | ||||
| N0 | 1584 | 0.57 | [0.40–0.81] | 0.002 |
| N1 | 50 | 1.30 | [0.78–2.15] | 0.309 |
| N2 | 30 | 1.09 | [0.60–1.98] | 0.783 |
| N3 | 15 | 1.02 | [0.43–2.40] | 0.968 |
| N+ | 3 | 2.48 | [0.54–11.41] | 0.242 |
| Nx | 588 | 1 | ||
| M stage | ||||
| M0 | 1954 | 1.02 | [0.54–1.92] | 0.957 |
| M1 | 61 | 5.24 | [2.54–10.83] | 0.000 |
| Mx | 255 | 1 | ||
| Charlson comorbidity index (CCI) | ||||
| CCI 0 | 1551 | 1 | ||
| CCI > = 1 | 668 | 1.26 | [0.94–1.69] | 0.116 |
| Unknown | 51 | 1.41 | [0.51–3.94] | 0.512 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sant, M.; Magri, M.C.; Maurichi, A.; Lillini, R.; Bento, M.J.; Ardanaz, E.; Guevara, M.; Innos, K.; Marcos-Gragera, R.; Rubio-Casadevall, J.; et al. Association of Sentinel Node Biopsy and Pathological Report Completeness with Survival Benefit for Cutaneous Melanoma and Factors Influencing Their Different Uses in European Populations. Cancers 2022, 14, 4379. https://doi.org/10.3390/cancers14184379
Sant M, Magri MC, Maurichi A, Lillini R, Bento MJ, Ardanaz E, Guevara M, Innos K, Marcos-Gragera R, Rubio-Casadevall J, et al. Association of Sentinel Node Biopsy and Pathological Report Completeness with Survival Benefit for Cutaneous Melanoma and Factors Influencing Their Different Uses in European Populations. Cancers. 2022; 14(18):4379. https://doi.org/10.3390/cancers14184379
Chicago/Turabian StyleSant, Milena, Maria Chiara Magri, Andrea Maurichi, Roberto Lillini, Maria José Bento, Eva Ardanaz, Marcela Guevara, Kaire Innos, Rafael Marcos-Gragera, Jordi Rubio-Casadevall, and et al. 2022. "Association of Sentinel Node Biopsy and Pathological Report Completeness with Survival Benefit for Cutaneous Melanoma and Factors Influencing Their Different Uses in European Populations" Cancers 14, no. 18: 4379. https://doi.org/10.3390/cancers14184379
APA StyleSant, M., Magri, M. C., Maurichi, A., Lillini, R., Bento, M. J., Ardanaz, E., Guevara, M., Innos, K., Marcos-Gragera, R., Rubio-Casadevall, J., Sánchez Pérez, M.-J., Tumino, R., Rugge, M., Minicozzi, P., & the Melanoma HR Study Working Group. (2022). Association of Sentinel Node Biopsy and Pathological Report Completeness with Survival Benefit for Cutaneous Melanoma and Factors Influencing Their Different Uses in European Populations. Cancers, 14(18), 4379. https://doi.org/10.3390/cancers14184379








