Updates in the Use of BCL-2-Family Small Molecule Inhibitors for the Treatment of Relapsed/Refractory Multiple Myeloma
Abstract
:Simple Summary
Abstract
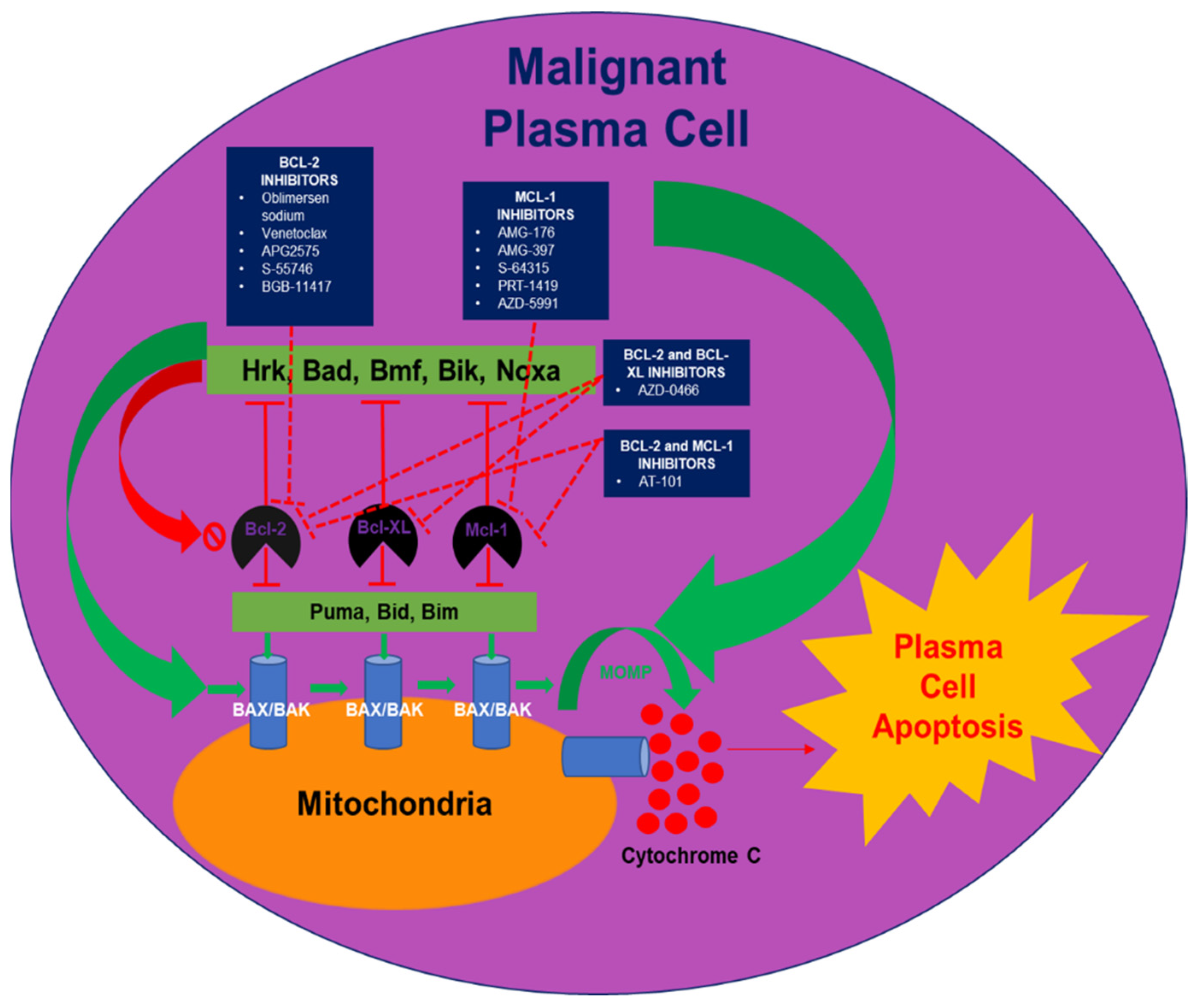
1. Introduction
2. Oblimersen Sodium
3. AT-101
4. Venetoclax
5. APG2575
6. S-55746
7. BGB-11417
8. AZD-0466
9. MCL-1 Inhibition
10. AMG-176 and AMG-397
11. S-64315
12. PRT-1419
13. AZD-5991
14. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kyle, R.A.; Rajkumar, S.V. Multiple myeloma. N. Engl. J. Med. 2004, 351, 1860–1873. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.K.; Rajkumar, S.V.; Dispenzieri, A.; Lacy, M.Q.; Hayman, S.R.; Buadi, F.K.; Zeldenrust, S.R.; Dingli, D.; Russell, S.J.; Lust, J.A.; et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008, 111, 2516–2520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, S.K.; Dispenzieri, A.; Lacy, M.Q.; Gertz, M.A.; Buadi, F.K.; Pandey, S.; Kapoor, P.; Dingli, D.; Hayman, S.R.; Leung, N.; et al. Continued improvement in survival in multiple myeloma: Changes in early mortality and outcomes in older patients. Leukemia 2014, 28, 1122–1128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajkumar, S.V. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am. J. Hematol. 2020, 95, 548–567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, S.K.; Therneau, T.M.; Gertz, M.A.; Lacy, M.Q.; Dispenzieri, A.; Rajkumar, S.V.; Fonseca, R.; Witzig, T.E.; Lust, J.A.; Larson, D.R.; et al. Clinical course of patients with relapsed multiple myeloma. Mayo Clin. Proc. 2004, 79, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, U.H.; Cornell, R.F.; Lakshman, A.; Gahvari, Z.J.; McGehee, E.; Jagosky, M.H.; Gupta, R.; Varnado, W.; Fiala, M.A.; Chhabra, S.; et al. Outcomes of patients with multiple myeloma refractory to CD38-targeted monoclonal antibody therapy. Leukemia 2019, 33, 2266–2275. [Google Scholar] [CrossRef]
- Letai, A.G. Diagnosing and exploiting cancer’s addiction to blocks in apoptosis. Nat. Rev. Cancer 2008, 8, 121–132. [Google Scholar] [CrossRef]
- Touzeau, C.; Ryan, J.; Guerriero, J.; Moreau, P.; Chonghaile, T.N.; Le Gouill, S.; Richardson, P.; Anderson, K.; Amiot, M.; Letai, A. BH3 profiling identifies heterogeneous dependency on Bcl-2 family members in multiple myeloma and predicts sensitivity to BH3 mimetics. Leukemia 2016, 30, 761–764. [Google Scholar] [CrossRef]
- Klasa, R.J.; Gillum, A.M.; Klem, R.E.; Frankel, S.R. Oblimersen Bcl-2 antisense: Facilitating apoptosis in anticancer treatment. Antisense Nucleic Acid Drug Dev. 2002, 12, 193–213. [Google Scholar] [CrossRef]
- Chanan-Khan, A.A. Bcl-2 antisense therapy in multiple myeloma. Oncology 2004, 18, 21–24. [Google Scholar]
- Chanan-Khan, A.A.; Niesvizky, R.; Hohl, R.J.; Zimmerman, T.M.; Christiansen, N.P.; Schiller, G.J.; Callander, N.; Lister, J.; Oken, M.; Jagannath, S. Phase III randomised study of dexamethasone with or without oblimersen sodium for patients with advanced multiple myeloma. Leuk. Lymphoma 2009, 50, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Badros, A.Z.; Goloubeva, O.; Ratterree, B.; Natt, S.; Rapoport, A.; Bolaños-Meade, J.; Zhang, B.; Zeldis, J.; Frankel, S.; Meisenberg, B.; et al. Phase II Trial of Oblimersen Sodium (G3139), Dexamethasone (Dex) and Thalidomide (Thal) in Relapsed Multiple Myeloma Patients (Pts). Blood 2004, 104, 2400. [Google Scholar]
- van de Donk, N.W.; de Weerdt, O.; Veth, G.; Eurelings, M.; van Stralen, E.; Frankel, S.R.; Hagenbeek, A.; Bloem, A.C.; Lokhorst, H.M. G3139, a Bcl-2 antisense oligodeoxynucleotide, induces clinical responses in VAD refractory myeloma. Leukemia 2004, 18, 1078–1084. [Google Scholar] [CrossRef]
- PROFILE, A.R.D. Augmerosen, BCL-2 antisense oligonucleotide-Genta, G 3139, GC 3139. Oblimersen Sodium 2007, 8, 321–334. [Google Scholar]
- Kline, M.P.; Rajkumar, S.V.; Timm, M.M.; Kimlinger, T.K.; Haug, J.L.; Lust, J.A.; Greipp, P.R.; Kumar, S. R-(-)—gossypol (AT-101) activates programmed cell death in multiple myeloma cells. Exp. Hematol. 2008, 36, 568–576. [Google Scholar] [PubMed] [Green Version]
- Paulus, A.; Chitta, K.; Akhtar, S.; Personett, D.; Miller, K.C.; Thompson, K.J.; Carr, J.; Kumar, S.; Roy, V.; Ansell, S.M.; et al. AT-101 downregulates BCL2 and MCL1 and potentiates the cytotoxic effects of lenalidomide and dexamethasone in preclinical models of multiple myeloma and Waldenström macroglobulinaemia. Br. J. Haematol. 2014, 164, 352–365. [Google Scholar]
- Masood, A.; Chitta, K.; Paulus, A.; Khan, A.N.; Sher, T.; Ersing, N.; Miller, K.C.; Manfredi, D.; Ailawadhi, S.; Borrelo, I.; et al. Downregulation of BCL2 by AT-101 enhances the antileukaemic effect of lenalidomide both by an immune dependant and independent manner. Br. J. Haematol. 2012, 157, 59–66. [Google Scholar] [CrossRef]
- Ailawadhi, S.; Alegria, V.R.; Ahmed, S.; Laplant, B.; Manna, A.; Parrondo, R.; Roy, V.; Sher, T.; Edwards, B.; Lanier, S.; et al. Phase I Study of a Novel Bcl-2 Inhibitor, at-101 in Combination with Lenalidomide and Dexamethasone in Patients with Relapsed and/or Refractory Multiple Myeloma (RRMM). Blood 2019, 134 (Suppl. S1), 3137. [Google Scholar] [CrossRef]
- Touzeau, C.; Dousset, C.; Le Gouill, S.; Sampath, D.; Leverson, J.D.; Souers, A.J.; Maïga, S.; Béné, M.C.; Moreau, P.; Pellat-Deceunynck, C.; et al. The Bcl-2 specific BH3 mimetic ABT-199: A promising targeted therapy for t(11;14) multiple myeloma. Leukemia 2014, 28, 210–212. [Google Scholar] [CrossRef]
- Kumar, S.; Kaufman, J.L.; Gasparetto, C.; Mikhael, J.; Vij, R.; Pegourie, B.; Benboubker, L.; Facon, T.; Amiot, M.; Moreau, P.; et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood 2017, 130, 2401–2409. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.L.; Gasparetto, C.J.; Mikhael, J.; Moreau, P.; Touzeau, C.; Vij, R.; Facon, T.; Pegourie, B.; Benboubker, L.; Boise, L.H.; et al. Phase 1 Study of Venetoclax in Combination with Dexamethasone As Targeted Therapy for t (11; 14) Relapsed/Refractory Multiple Myeloma. Blood 2017, 130 (Suppl. S1), 3131. [Google Scholar]
- Qin, J.Z.; Ziffra, J.; Stennett, L.; Bodner, B.; Bonish, B.K.; Chaturvedi, V.; Bennett, F.; Pollock, P.M.; Trent, J.M.; Hendrix, M.J.; et al. Proteasome inhibitors trigger NOXA-mediated apoptosis in melanoma and myeloma cells. Cancer Res. 2005, 65, 6282–6293. [Google Scholar] [PubMed] [Green Version]
- Kumar, S.K.; Harrison, S.J.; Cavo, M.; de la Rubia, J.; Popat, R.; Gasparetto, C.; Hungria, V.; Salwender, H.; Suzuki, K.; Kim, I.; et al. Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): A randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2020, 21, 1630–1642. [Google Scholar] [CrossRef]
- Kumar, S.; Harrison, S.; Cavo, M.; de la Rubia, J.; Popat, R.; Gasparetto, C.; Hungria, V.; Salwender, H.; Suzuki, K.; Kim, I.; et al. A phase 3 study of venentoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed/refractory myeloma. In Proceedings of the European Hematology Association Annual Congress, Amsterdam, The Netherlands, 13–16 June 2019. Abstract #LBA2601. [Google Scholar]
- Available online: https://www.fiercepharma.com/pharma/fda-lifts-partial-hold-venclexta-trial-multiple-myeloma-after-a-spate-deaths (accessed on 9 March 2022).
- Kumar, S.; Harrison, S.; Cavo, M.; de la Rubia, J.; Popat, R.; Gasparetto, C.; Hungria, V.; Salwender, H.; Suzuki, K.; Kim, I.; et al. Final overall survival results from BELLINI, a phase 3 study of venetoclax or placebo in combination with bortezomib and dexamethasone in relapsed/refractory multiple myeloma. Blood 2021, 138 (Suppl. S1), 84. [Google Scholar] [CrossRef]
- Gasparetto, C.; Bowles, K.M.; Abdallah, A.O.; Morris, L.; Mander, G.; Coppola, S.; Wang, J.; Ross, J.A.; Bueno, O.F.; Arriola, E.; et al. A Phase II Study of Venetoclax in Combination With Pomalidomide and Dexamethasone in Relapsed/Refractory Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2021, 21, 775–784. [Google Scholar] [CrossRef]
- Costa, L.J.; Davies, F.E.; Monohan, G.P.; Kovacsovics, T.; Burwick, N.; Jakubowiak, A.; Kaufman, J.L.; Hong, W.-J.; Dail, M.; Salem, A.H.; et al. Phase 2 study of venetoclax plus carfilzomib and dexamethasone in patients with relapsed/refractory multiple myeloma. Blood Adv. 2021, 5, 3748–3759. [Google Scholar] [CrossRef]
- Bahlis, N.J.; Baz, R.; Harrison, S.J.; Quach, H.; Ho, S.-J.; Vangsted, A.J.; Plesner, T.; Moreau, P.; Gibbs, S.D.; Coppola, S.; et al. Phase I Study of Venetoclax Plus Daratumumab and Dexamethasone, With or Without Bortezomib, in Patients With Relapsed or Refractory Multiple Myeloma With and Without t(11;14). J. Clin. Oncol. 2021, 39, 3602–3612. [Google Scholar] [CrossRef]
- Fischer, K.; Al-Sawaf, O.; Bahlo, J.; Fink, A.N.; Tandon, M.; Dixon, M.; Robrecht, S.; Warburton, S.; Humphrey, K.; Samoylova, O.; et al. Venetoclax and Obinutuzumab in Patients with CLL and Coexisting Conditions. N. Engl. J. Med. 2019, 380, 2225–2236. [Google Scholar] [CrossRef]
- Kater, A.; Owen, C.; Moreno, C.; Follows, G.; Munir, T.; Levin, M.-D.; Benjamini, O.; Janssens, A.; Osterborg, A.; Robak, T.; et al. Fixed duration ibrutinib and venetoclax versus chlorambucil plus obinutuzumab for first-line chronic lymphocytic leukemia: Primary analysis of the phase 3 GLOW study. In Proceedings of the European Hematology Association 2021 Virtual Congress, Online, 12 June 2021. Abstract LB1902. [Google Scholar]
- Castillo, J.J.; Allan, J.N.; Siddiqi, T.; Advani, R.H.; Meid, K.; Leventoff, C.; White, T.P.; Flynn, C.A.; Sarosiek, S.; Branagan, A.R.; et al. Venetoclax in Previously Treated Waldenstrom Macroglobulinemia. J. Clin. Oncol. 2021, 40, 63–71. [Google Scholar]
- Zhai, Y. APG2575, Unpublished investigator brochure, Version 3.1. 11 November 2020.
- Ailawadhi, S.; Chanan-Khan, A.A.A.; Chen, Z.; Huang, B.; Konopleva, M.; Brander, D.M.; Rizzieri, D.; Lasica, M.; Tam, C.S.L.; Yannakou, C.K.; et al. First-in-human study of lisaftoclax (APG-2575), a novel BCL-2 inhibitor (BCL-2i), in patients (pts) with relapsed/refractory (R/R) CLL and other hematologic malignancies (HMs). J. Clin. Oncol. 2021, 39 (Suppl. S15), 7502. [Google Scholar] [CrossRef]
- Casara, P.; Davidson, J.; Claperon, A.; Le Toumelin-Braizat, G.; Vogler, M.; Bruno, A.; Chanrion, M.; Lysiak-Auvity, G.; Le Diguarher, T.; Starck, J.B.; et al. S55746 is a novel orally active BCL-2 selective and potent inhibitor that impairs hematological tumor growth. Oncotarget 2018, 9, 20075–20088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, N.; Guo, Y.; Xue, H.; Liu, Y.; Guo, Y.; Wang, F.; Song, X.; Guo, Y.; Chen, S.; Xu, H.; et al. Abstract 3077: Preclinical characterization of BGB-11417, a potent and selective Bcl-2 inhibitor with superior antitumor activities in haematological tumor models. Cancer Res. 2020, 80 (Suppl. S16), 3077. [Google Scholar] [CrossRef]
- Tam, C.S.; Verner, E.; Lasica, M.; Arbelaez, A.; Browett, P.J.; Soumerai, J.D.; Hilger, J.; Fang, Y.; Huang, J.; Simpson, D.; et al. Preliminary Safety and Efficacy Data from Patients (Pts) with Relapsed/Refractory (R/R) B-Cell Malignancies Treated with the Novel B-Cell Lymphoma 2 (BCL2) Inhibitor BGB-11417 in Monotherapy or in Combination with Zanubrutinib. Blood 2021, 138 (Suppl. S1), 1419. [Google Scholar] [CrossRef]
- Oltersdorf, T.; Elmore, S.W.; Shoemaker, A.R.; Armstrong, R.C.; Augeri, D.J.; Belli, B.A.; Bruncko, M.; Deckwerth, T.L.; Dinges, J.; Hajduk, P.J.; et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature 2005, 435, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.W.; Seymour, J.F.; Brown, J.R.; Wierda, W.G.; Kipps, T.J.; Khaw, S.L.; Carney, D.A.; He, S.Z.; Huang, D.C.S.; Xiong, H.; et al. Substantial Susceptibility of Chronic Lymphocytic Leukemia to BCL2 Inhibition: Results of a Phase I Study of Navitoclax in Patients With Relapsed or Refractory Disease. J. Clin. Oncol. 2011, 30, 488–496. [Google Scholar] [PubMed] [Green Version]
- Punnoose, E.A.; Leverson, J.D.; Peale, F.; Boghaert, E.R.; Belmont, L.D.; Tan, N.; Young, A.; Mitten, M.; Ingalla, E.; Darbonne, W.C.; et al. Expression Profile of BCL-2, BCL-XL, and MCL-1 Predicts Pharmacological Response to the BCL-2 Selective Antagonist Venetoclax in Multiple Myeloma Models. Mol. Cancer Ther. 2016, 15, 1132–1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balachander, S.B.; Tabatabai, A.; Wen, S.; Gibbons, F.D.; Fabbri, G.; Zhang, G.S.; Cidado, J.; Graham, L.; Ashford, M.; Davies, B. Abstract 56: AZD0466, a nanomedicine of a potent dual Bcl-2/Bcl-xL inhibitor, exhibits anti-tumor activity in a range of hematological and solid tumor models. Cancer Res. 2020, 80 (Suppl. S16), 56. [Google Scholar] [CrossRef]
- Patterson, C.M.; Balachander, S.B.; Grant, I.; Pop-Damkov, P.; Kelly, B.; McCoull, W.; Parker, J.; Giannis, M.; Hill, K.J.; Gibbons, F.D.; et al. Design and optimisation of dendrimer-conjugated Bcl-2/x(L) inhibitor, AZD0466, with improved therapeutic index for cancer therapy. Commun. Biol. 2021, 4, 112. [Google Scholar] [CrossRef]
- Peperzak, V.; Vikström, I.; Walker, J.; Glaser, S.P.; LePage, M.; Coquery, C.M.; Erickson, L.D.; Fairfax, K.; Mackay, F.; Strasser, A.; et al. Mcl-1 is essential for the survival of plasma cells. Nat. Immunol. 2013, 14, 290–297. [Google Scholar] [CrossRef]
- Wuillème-Toumi, S.; Robillard, N.; Gomez, P.; Moreau, P.; Le Gouill, S.; Avet-Loiseau, H.; Harousseau, J.L.; Amiot, M.; Bataille, R. Mcl-1 is overexpressed in multiple myeloma and associated with relapse and shorter survival. Leukemia 2005, 19, 1248–1252. [Google Scholar] [CrossRef] [Green Version]
- Dousset, C.; Maïga, S.; Gomez-Bougie, P.; Le Coq, J.; Touzeau, C.; Moreau, P.; Le Gouill, S.; Chiron, D.; Pellat-Deceunynck, C.; Moreau-Aubry, A.; et al. BH3 profiling as a tool to identify acquired resistance to venetoclax in multiple myeloma. Br. J. Haematol. 2017, 179, 684–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neri, P.; Maity, R.; Alberge, J.-B.; Sinha, S.; Donovan, J.; Kong, M.; Hasan, F.; Jaffer, A.; Boise, L.H.; Bahlis, N. Mutations and Copy Number Gains of the BCL2 Family Members Mediate Resistance to Venetoclax in Multiple Myeloma (MM) Patients. Blood 2019, 134 (Suppl. S1), 572. [Google Scholar]
- Zhou, L.; Zhang, Y.; Sampath, D.; Leverson, J.; Dai, Y.; Kmieciak, M.; Nguyen, M.; Orlowski, R.Z.; Grant, S. Flavopiridol enhances ABT-199 sensitivity in unfavourable-risk multiple myeloma cells in vitro and in vivo. Br. J. Cancer 2018, 118, 388–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caenepeel, S.R.; Belmontes, B.; Sun, J.; Coxon, A.; Moody, G.; Hughes, P.E. Abstract 2027: Preclinical evaluation of AMG 176, a novel, potent and selective Mcl-1 inhibitor with robust anti-tumor activity in Mcl-1 dependent cancer models. Cancer Res. 2017, 77 (Suppl. S13), 2027. [Google Scholar] [CrossRef]
- Caenepeel, S.; Brown, S.P.; Belmontes, B.; Moody, G.; Keegan, K.S.; Chui, D.; Whittington, D.A.; Huang, X.; Poppe, L.; Cheng, A.C.; et al. AMG 176, a Selective MCL1 Inhibitor, Is Effective in Hematologic Cancer Models Alone and in Combination with Established Therapies. Cancer Discov. 2018, 8, 1582–1597. [Google Scholar] [CrossRef] [Green Version]
- Spencer, A.; Rosenberg, A.S.; Jakubowiak, A.; Raje, N.; Chatterjee, M.; Trudel, S.; Bahlis, N.J.; Siegel, D.S.; Wilop, S.; Harrison, S.J.; et al. A phase 1, first-in-human study of AMG 176, a selective MCL-1 inhibitor, in patients with relapsed or refractory multiple myeloma. Clin. Lymphoma Myeloma Leuk. 2019, 19, e53–e54. [Google Scholar] [CrossRef]
- Canenepeel, S.; Karen, R.; Belmontes, B.; Verlinsky, A.; Tan, H.; Tang, Y.; Chen, X.; Li, K.; Allen, J.; Wahlstrom, J.; et al. Discovery and preclinical evaluation of AMG 397, a potent, selective and orally bioavailable MCL1 inhibitor. Cancer Res. 2020, 80 (Suppl. S16), 6218. [Google Scholar]
- Kotschy, A.; Szlavik, Z.; Murray, J.; Davidson, J.; Maragno, A.L.; Le Toumelin-Braizat, G.; Chanrion, M.; Kelly, G.L.; Gong, J.-N.; Moujalled, D.M.; et al. The MCL1 inhibitor S63845 is tolerable and effective in diverse cancer models. Nature 2016, 538, 477–482. [Google Scholar] [CrossRef]
- Brennan, M.S.; Chang, C.; Tai, L.; Lessene, G.; Strasser, A.; Dewson, G.; Kelly, G.L.; Herold, M.J. Humanized Mcl-1 mice enable accurate preclinical evaluation of MCL-1 inhibitors destined for clinical use. Blood 2018, 132, 1573–1583. [Google Scholar] [CrossRef] [Green Version]
- Algarín, E.M.; Díaz-Tejedor, A.; Mogollón, P.; Hernández-García, S.; Corchete, L.A.; San-Segundo, L.; Martín-Sánchez, M.; González-Méndez, L.; Schoumacher, M.; Banquet, S.; et al. Preclinical evaluation of the simultaneous inhibition of MCL-1 and BCL-2 with the combination of S63845 and venetoclax in multiple myeloma. Haematologica 2020, 105, e116–e120. [Google Scholar] [CrossRef] [Green Version]
- Wong, K.Y.; Chim, C.S. Venetoclax, bortezomib and S63845, an MCL1 inhibitor, in multiple myeloma. J. Pharm. Pharmacol. 2020, 72, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Bhagwat, N.; Grego, A.; Gowen-MacDonald, W.; Wang, M.; Cowart, M.; Wu, X.; Zhuo, J.; Combs, A.; Ruggeri, B.; Scherle, P.; et al. Abstract 983: Preclinical characterization of PRT1419, a potent, selective and orally available inhibitor of MCL1. Cancer Res. 2021, 81 (Suppl. S13), 983. [Google Scholar] [CrossRef]
- Tron, A.E.; Belmonte, M.A.; Adam, A.; Aquila, B.M.; Boise, L.H.; Chiarparin, E.; Cidado, J.; Embrey, K.J.; Gangl, E.; Gibbons, F.D.; et al. Discovery of Mcl-1-specific inhibitor AZD5991 and preclinical activity in multiple myeloma and acute myeloid leukemia. Nat. Commun. 2018, 9, 5341. [Google Scholar] [PubMed]
- Available online: https://www.evaluate.com/vantage/articles/news/snippets/low-key-astra-hold-puts-spotlight-novartis-and-servier (accessed on 22 March 2022).
- Wang, X.; Bathina, M.; Lynch, J.; Koss, B.; Calabrese, C.; Frase, S.; Schuetz, J.D.; Rehg, J.E.; Opferman, J.T. Deletion of MCL-1 causes lethal cardiac failure and mitochondrial dysfunction. Genes Dev. 2013, 27, 1351–1364. [Google Scholar] [CrossRef] [Green Version]
- Thomas, R.L.; Roberts, D.J.; Kubli, D.A.; Lee, Y.; Quinsay, M.N.; Owens, J.B.; Fischer, K.M.; Sussman, M.A.; Miyamoto, S.; Gustafsson, Å.B. Loss of MCL-1 leads to impaired autophagy and rapid development of heart failure. Genes Dev. 2013, 27, 1365–1377. [Google Scholar] [CrossRef] [Green Version]
| ClinicalTrials.Gov Identifier | Phase | Estimated or Actual Enrollment | Arm(s) | Primary Endpoints |
|---|---|---|---|---|
| BCL-2 Inhibitors | ||||
| Venetoclax | ||||
| NCT02899052 | 2 | 120 | Carfilzomib + venetoclax and dexamethasone | Safety, ORR, ≥VGPR rate, ≥CR rate |
| NCT03539744 | 3 | 244 | Venetoclax + pomalidomide and dexamethasone vs. pomalidomide and dexamethasone | PFS |
| APG-2575 | ||||
| NCT04942067 | 1/2 | 108 | APG-2575 + pomalidomide and dexamethasone and APG-2575 + daratumumab, lenalidomide and dexamethasone | DLT rate, MTD/RP2D |
| NCT04674514 | 1/2 | 48 | APG-2575 + lenalidomide and dexamethasone | DLT rate, MTD/RP2D |
| S-55746 | ||||
| NCT02920697 | 1 | 65 | S-557646 | Safety, MTD |
| BGB-11417 | ||||
| NCT04973605 | 1/2 | 146 | BGB-11417 and BGB-11417 + dexamethasone and BGB-11417 + carfilzomib and dexamethasone | Part 1: safety, DLT Part 2: ORR, ≥VGPR rate, ≥CR rate |
| BCL-2 and BCL-XL Inhibitors | ||||
| AZD-0466 | ||||
| NCT04214093 | 1 | 9 | AZD-0466 | Safety, MTD |
| NCT04865419 | 1/2 | 141 | AZD-0466 | Safety |
| MCL-1 Inhibitors | ||||
| AMG-176 | ||||
| NCT02675452 | 1 | 175 | AMG-176 | Safety |
| S-64315 | ||||
| NCT02992483 | 1 | 31 | S-64315 | Safety |
| PRT-1419 | ||||
| NCT04543305 | 1 | 36 | PRT-1419 | Safety, MTD/RP2D |
| AZD-5991 | ||||
| NCT03218683 | 1 | 144 | AZD-5991 | Safety, MTD |
| BCL-2 and MCL-1 Inhibitors | ||||
| NCT04702425 | 1 | 170 | S64315 + S65487 | Safety |
| ClinicalTrials.Gov Identifier | Phase/# of Patients | Regimen | Median Prior Lines (Range) | Maximum Tolerated Dose of Venetoclax | Refractoriness to Lenalidomide and Bortezomib | Cytogenetics | ORR | Median PFS | Most Common Grade 3/4 Adverse Events |
|---|---|---|---|---|---|---|---|---|---|
| NCT01794520 | I/66 | Venetoclax | 5 (1–15) | 1200 mg | Len: 77% Bor: 70% | t (11;14): 45% High Risk:27% | 21% 40% in t (11;14) | NR | thrombocytopenia (32%), neutropenia (27%), anemia (23%), and leukopenia (23%) |
| NCT01794520 | I/20 | Venetoclax and dexamethasone | 3 (1–7) | 800 mg | Len: 85% Bor: 55% | t (11;14): 100% High Risk: NR | 65% | NR | lymphopenia (15), hypophosphatemia (15%), hyperuricemia (10%) and laboratory tumor lysis syndrome (10%) |
| NCT02755597 | III/291 | Venetoclax, bortezomib, and dexamethasone | 53% received 2–3 prior lines | 800 mg | Len: 20% Bor: None | t (11;14): 10% High Risk:16% | 82%; 90% in t(11;14) | 22.4 months | neutropenia (18%), pneumonia (16%), thrombocytopenia (15%), anemia (15%), and diarrhea (15%) |
| NCT03567616 | II/8 | Venetoclax, pomalidomide, and dexamethasone | 1.5 (1–5) | 800 mg | Len: 75% Bor: NR | t (11;14): 37.5% High Risk: 62.5% | 62.5%; 66.7% in t(11;14) | 10.5 months | neutropenia (75%), leukopenia (38%), lymphocyte count decreased (25%), neutrophil count decreased (25%) |
| NCT02899052 | II/49 | Venetoclax, carfilzomib, and dexamethasone | 1 (1–3) | 800 mg | Len: 67% Bor: 47% | t (11;14): 27% High Risk: 27% | 80%; 92% in t(11;14) | 22.8 months | hypertension (16%), pneumonia (12%), lymphopenia (31%), leukopenia (12%), and neutropenia (12%) |
| NCT03314181 | I/48 | Venetoclax +/− bortezomib, daratumumab, and dexamethasone | −Bor:2.5 (1–8) +Bor:1 (1–3) | 800 mg | Len: NR Bor: NR | t (11;14): 62.5% High Risk: 10% | −Bor: 96% +Bor: 92% | −Bor: 90.5% at 18 m +Bor: 66.7% at 18 m | −Bor: hypertension (17%), neutropenia (21%), lymphopenia (8%) +Bor: insomnia (25%), thrombocytopenia (17%), lymphopenia (13%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parrondo, R.D.; Paulus, A.; Ailawadhi, S. Updates in the Use of BCL-2-Family Small Molecule Inhibitors for the Treatment of Relapsed/Refractory Multiple Myeloma. Cancers 2022, 14, 3330. https://doi.org/10.3390/cancers14143330
Parrondo RD, Paulus A, Ailawadhi S. Updates in the Use of BCL-2-Family Small Molecule Inhibitors for the Treatment of Relapsed/Refractory Multiple Myeloma. Cancers. 2022; 14(14):3330. https://doi.org/10.3390/cancers14143330
Chicago/Turabian StyleParrondo, Ricardo D., Aneel Paulus, and Sikander Ailawadhi. 2022. "Updates in the Use of BCL-2-Family Small Molecule Inhibitors for the Treatment of Relapsed/Refractory Multiple Myeloma" Cancers 14, no. 14: 3330. https://doi.org/10.3390/cancers14143330
APA StyleParrondo, R. D., Paulus, A., & Ailawadhi, S. (2022). Updates in the Use of BCL-2-Family Small Molecule Inhibitors for the Treatment of Relapsed/Refractory Multiple Myeloma. Cancers, 14(14), 3330. https://doi.org/10.3390/cancers14143330








