Association of Genetic Polymorphisms and Serum Levels of IL-6 and IL-8 with the Prognosis in Children with Neuroblastoma
Abstract
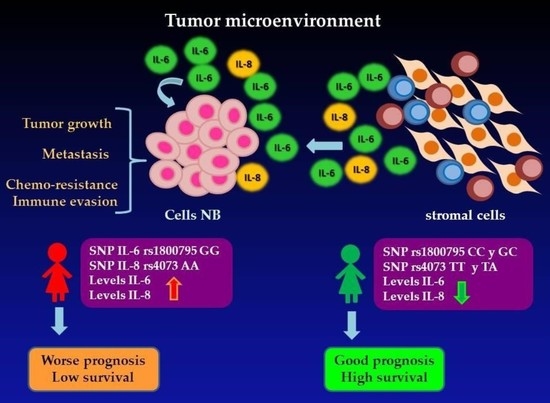
Simple Summary
Abstract
1. Introduction
2. Results
2.1. Characteristics of the Patients
2.2. Relationship of Genetic Polymorphisms of IL-6 and IL-8 between Cases of NB and the Control Group
2.3. Analysis of Genotypes and Prognostic Factors of Patients with NB
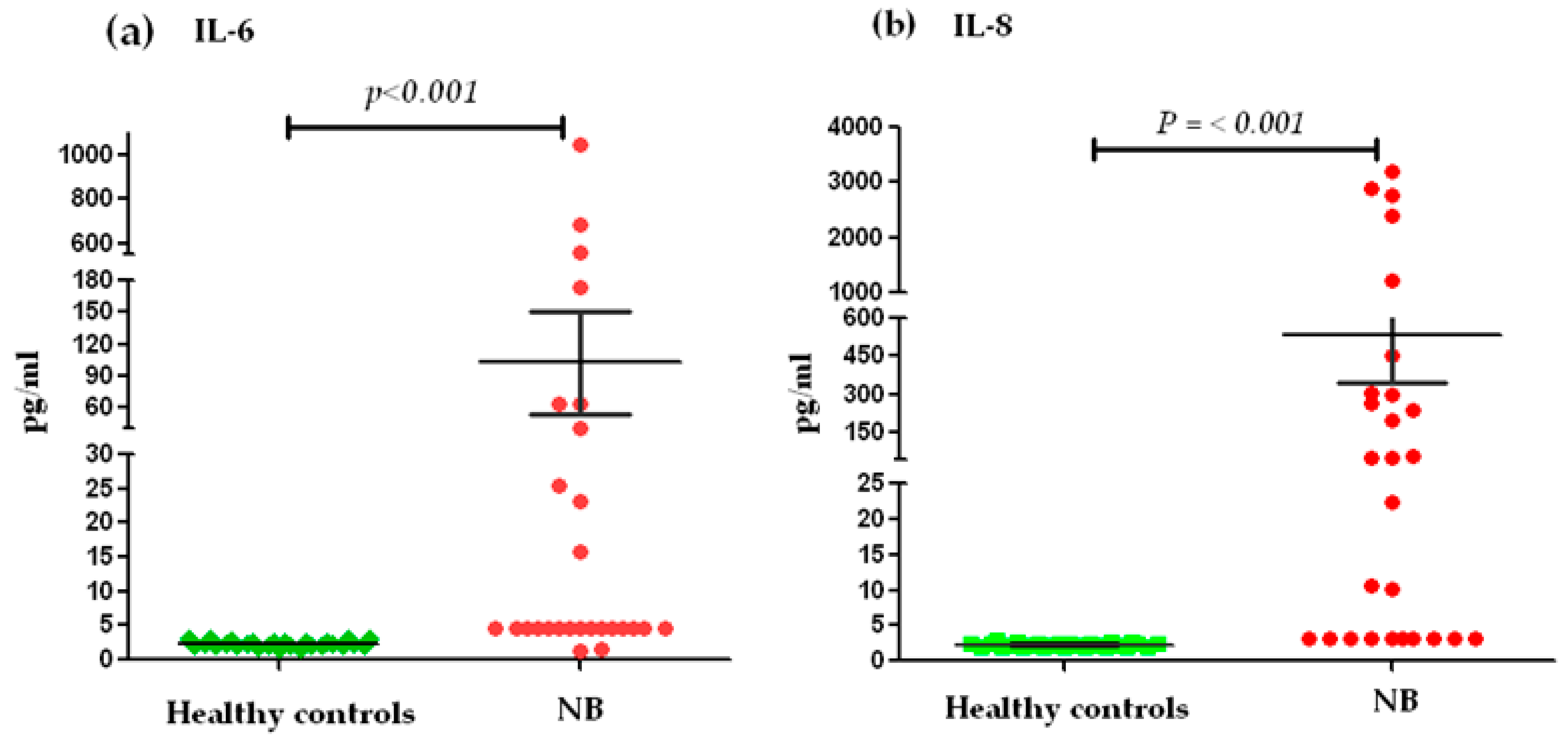
2.4. Relationship of Serum Levels of IL-6 and IL-8 between Cases of NB and the Control Group
2.5. Association of Genotypes and Serum Levels
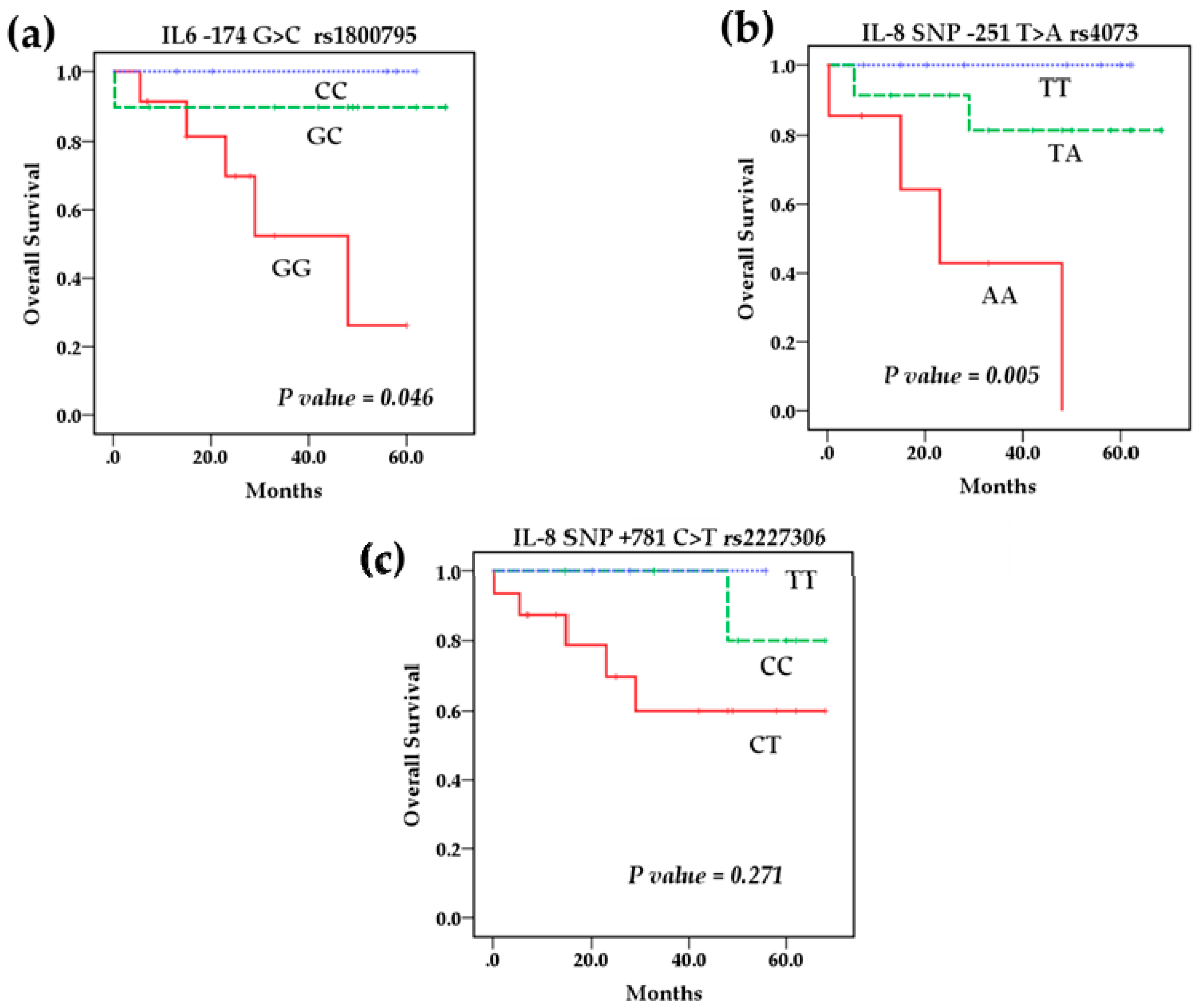
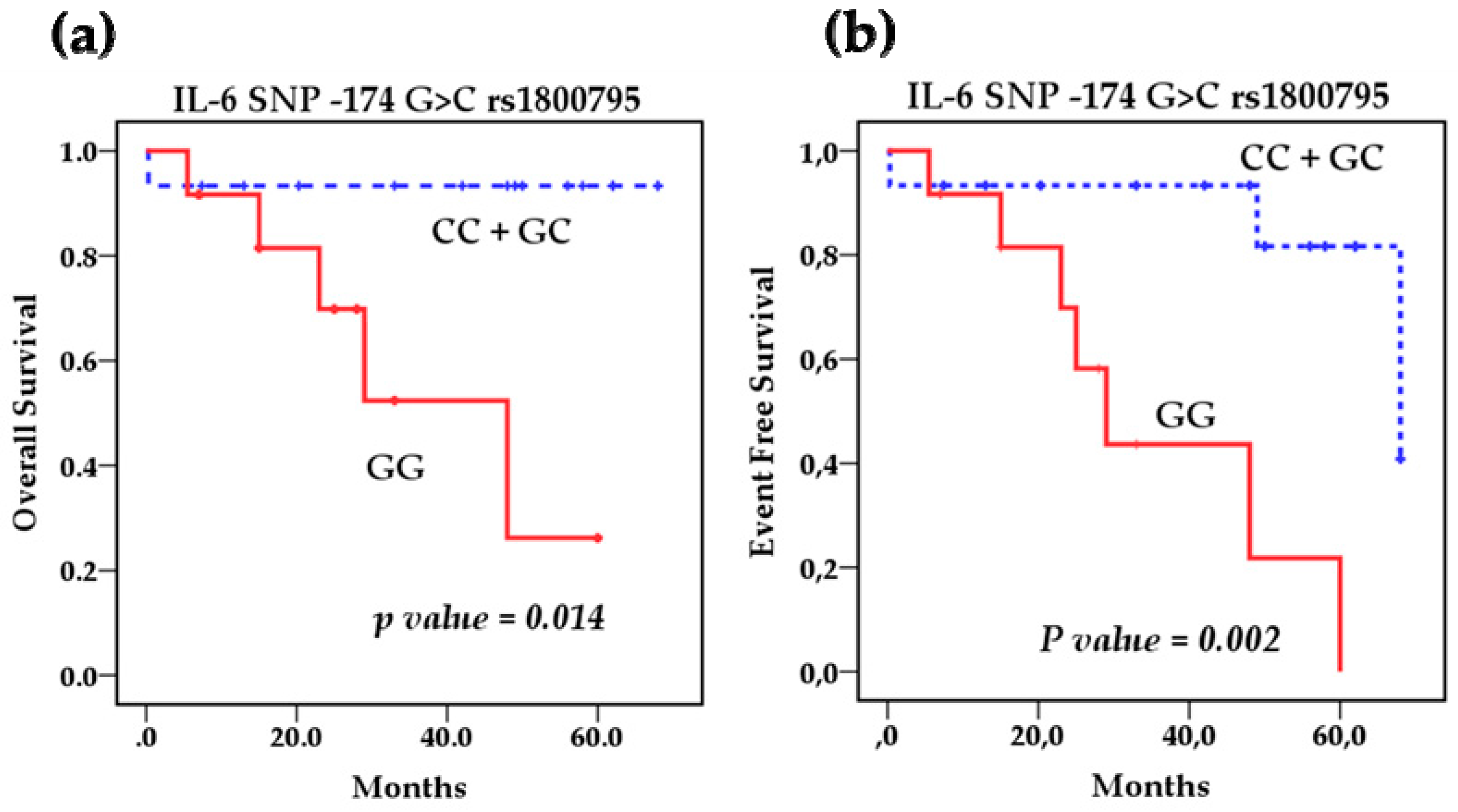
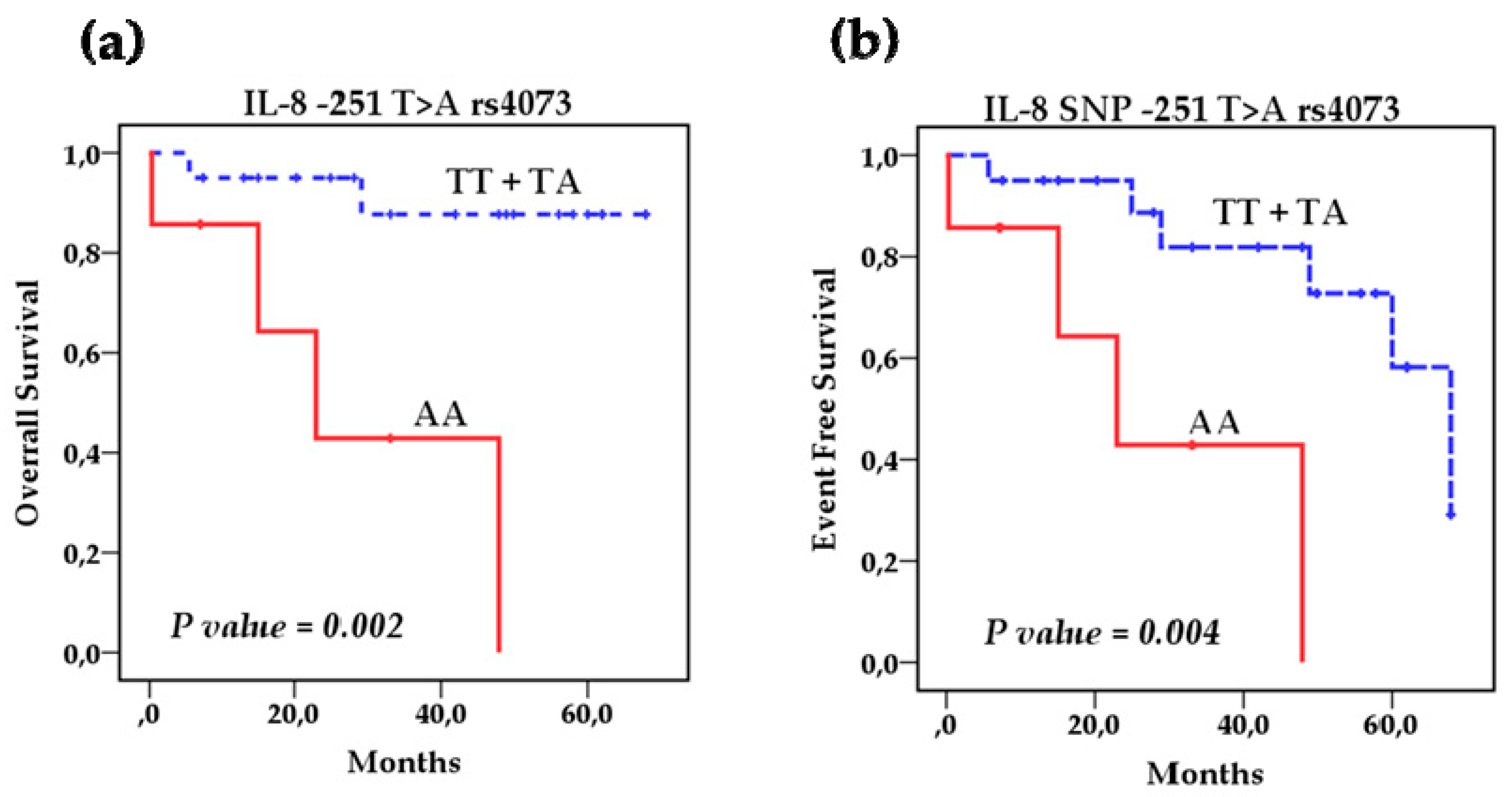
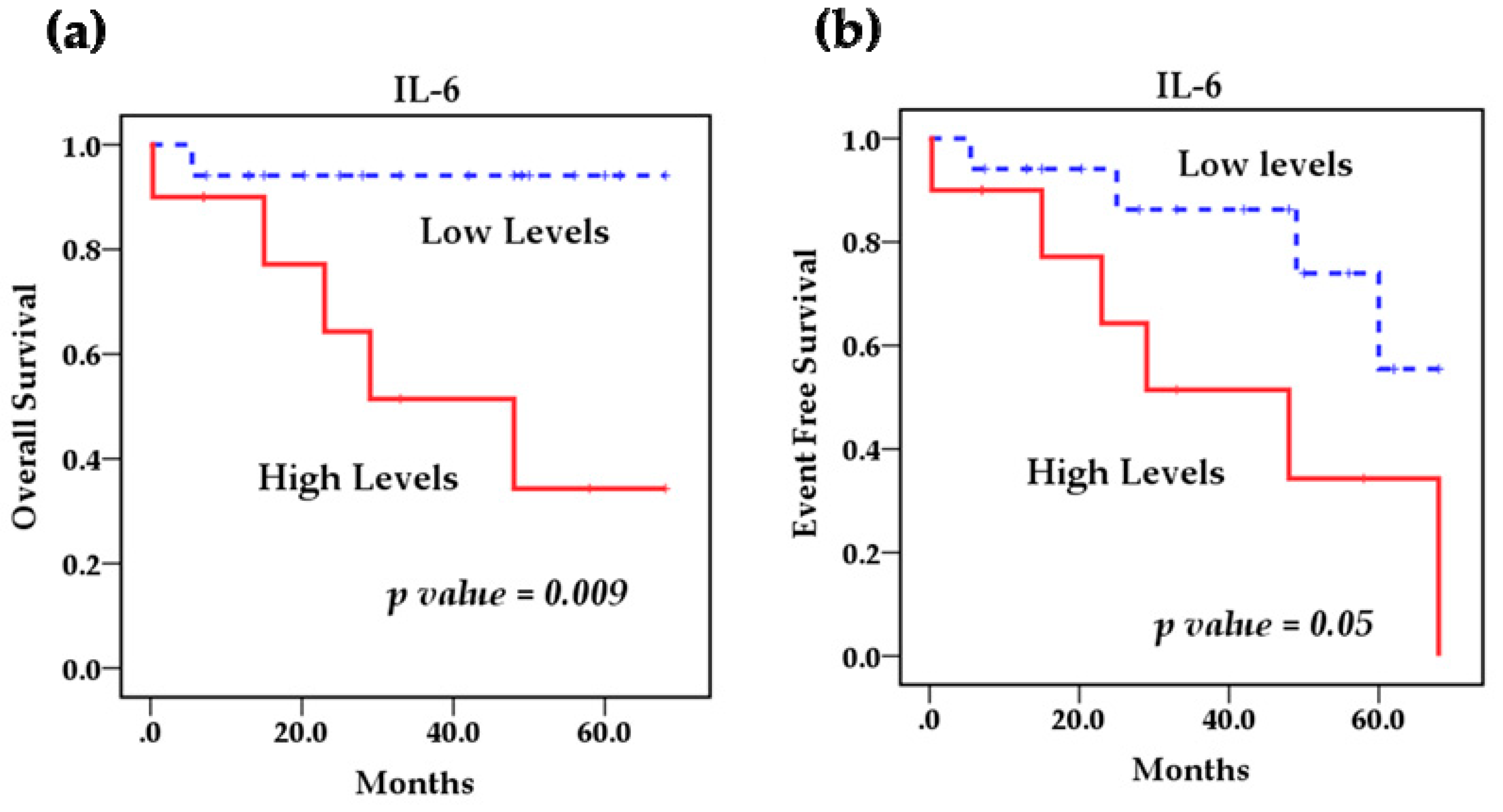
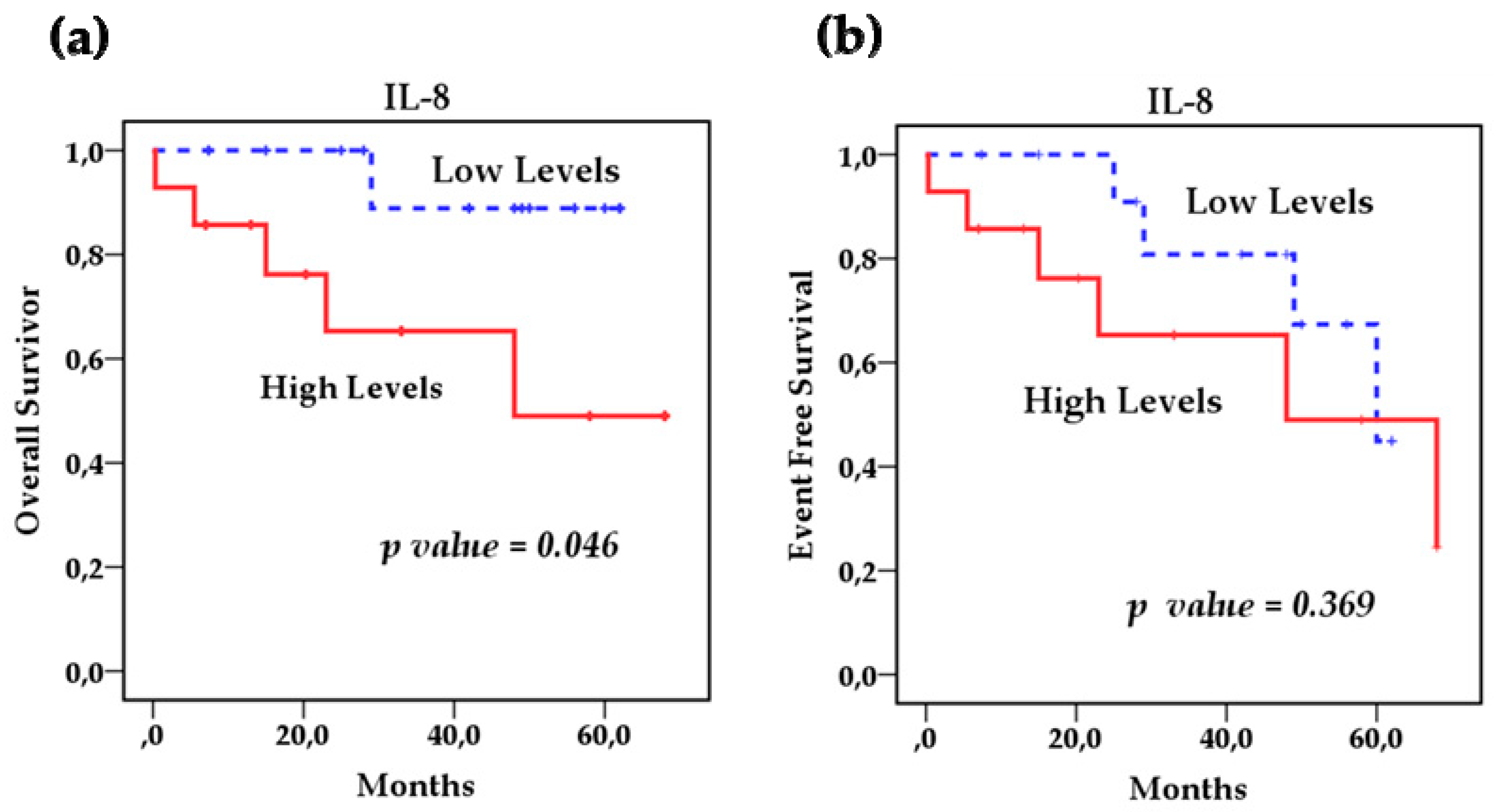
2.6. Survival Analysis
2.7. Cox Regression Analysis
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Collection and Handling of Samples
4.3. Ethical Considerations
4.4. Treatment Protocol
4.5. Detection of MYCN Gene Amplification
4.6. Analysis of Genetic Polymorphisms
4.7. Measurement of IL-6 and IL-8 Levels
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brodeur, G.M.; Hogarty, M.D.; Mosse, Y.P. Principles and Practice of pediatric oncology. In Neuroblastoma, 6th ed.; Poplack, D.G., Pizzo, P.A., Eds.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2011; pp. 886–922. [Google Scholar]
- Irwin, M.S.; Park, J.R. Neuroblastoma: Paradigm for precision medicine. Pediatr. Clin. N. Am. 2015, 62, 225–256. [Google Scholar] [CrossRef] [PubMed]
- Maris, J.M.; Hogarty, M.D.; Bagatell, R.; Cohn, S.L. Neuroblastoma. Lancet 2007, 369, 2106–2120. [Google Scholar] [CrossRef]
- Maris, J.M. The biologic basis for neuroblastoma heterogeneity and risk stratification. Curr. Opin. Pediatr. 2005, 17, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Juárez-Villegas, L.E.; Zapata-Tarrés, M.; Lezama del Valle, P. Resultados del tratamiento de niños con neuroblastoma en el Hospital Infantil de México “Federico Gómez”. Gaceta Mex. Oncol. 2014, 13, 26–30. [Google Scholar]
- Juárez-Ocaña, S.; Palma-Padilla, V.; González-Miranda, G.; Siordia-Reyes, A.G.; López-Aguilar, E.; Aguilar-Martínez, M.; Mejía-Aranguré, J.M.; Carreón-Cruz, R.; Rendón-Macías, M.E.; Fajardo-Gutiérrez, A. Epidemiological and some clinical characteristics of neuroblastoma in Mexican children (1996–2005). BMC Cancer 2009, 3, 266. [Google Scholar] [CrossRef] [PubMed]
- Heck, J.E.; Ritz, B.; Hung, R.J.; Hashibe, M.; Boffetta, P. The epidemiology of neuroblastoma: A review. Paediatr. Perinat. Epidemiol. 2009, 23, 125–143. [Google Scholar] [CrossRef]
- Colon, N.C.; Chung, D.H. Neuroblastoma. Adv. Pediatr. 2011, 58, 297–311. [Google Scholar] [CrossRef]
- Palma-Padilla, V.; Juárez-Ocaña, S.; González- Miranda, G.; Siordia-Reyes, A.G.; Mejia-Aranguré, J.M.; Carreón-Cruz, R.; Fajardo-Gutiérrez, A. Incidencia y tendencia del Neuroblastoma en niños derechohabientes del IMSS. Rev. Med. Inst. Mex. Seguro Soc. 2010, 48, 151–158. [Google Scholar]
- Singh, N.; Baby, D.; Rajguru, J.P.; Patil, P.B.; Thakkannavar, S.S.; Pujari, V.B. Inflammation and cancer. Ann. Afr. Med. 2019, 18, 121–126. [Google Scholar] [CrossRef]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef]
- Vendramini-Costa, B.D.; Carvalho, J. Molecular Link Mechanisms between Inflammation and Cancer. Curr. Pharm. Des. 2012, 18, 3831–3852. [Google Scholar] [CrossRef] [PubMed]
- Rebecca-Deyell, R.J.; Attiyeh, E.F. Advances in the understanding of constitutional and somatic genomic alterations in neuroblastoma. Cancer Genet. 2011, 204, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.H.; Lu, M.Y.; Yang, Y.L.; Chou, S.W.; Lin, D.T.; Lin, K.H.; Hsu, W.M.; Jeng, Y.M.; Jou, S.T. The prognostic roles of and correlation between ALK and MYCN protein expression in neuroblastoma. J. Clin. Pathol. 2020, 73, 154–161. [Google Scholar] [CrossRef]
- Bagatell, R.; Cohn, S.L. Genetic discoveries and treatment advances in neuroblastoma. Curr. Opin. Pediatr. 2016, 28, 19–25. [Google Scholar] [CrossRef]
- Waleh, N.; Seidner, S.; McCurnin, D.; Yoder, B.; Liu, B.M.; Roman, C.; Mauray, F.; Clyman, R.I. The role of monocyte-derived cells and inflammation in baboon ductus arteriosus remodeling. Pediatr. Res. 2005, 57, 254–262. [Google Scholar] [CrossRef]
- Keller, E.T.; Wanagat, J.; Ershler, W.B. Molecular and cellular biology of interleukin-6 and its receptor. Front. Biosci. 1996, 1, d340–d357. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, M.; Hayakawa, N.; Suzuki, M.; Mihara, M. IL-6/sIL-6R trans-signalling, but not TNF-alpha induced angiogenesis in a HUVEC and synovial cell co-culture system. Rheumatol. Int. 2009, 29, 1449–1454. [Google Scholar] [CrossRef] [PubMed]
- Khatibi, S.; Babon, J.; Wagner, J.; Manton, J.H.; Tan, C.W.; Zhu, H.J.; Wormald, S.; Burgess, A.W. Burgess. TGF-β and IL-6 family signalling crosstalk: An integrated model. Growth Factors 2017, 35, 100–124. [Google Scholar] [CrossRef] [PubMed]
- Medzhitov, R. Inflammation 2010: New adventures of an old flame. Cell 2010, 140, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.A.; Jones, S.A. IL-6 as a keystone cytokine in health and disease. Nat. Immunol. 2015, 16, 448–457. [Google Scholar] [CrossRef]
- Liao, C.; Yu, Z.; Guo, W.; Liu, Q.; Wu, Y.; Li, Y.; Bai, L. Prognostic value of circulating inflammatory factors in non-small cell lung cancer: A systematic review and meta-analysis. Cancer Biomark. 2014, 14, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Karin, M. Inflammation and oncogenesis: A vicious connection. Curr. Opin. Genet. Dev. 2010, 20, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Egler, R.A.; Burlingame, S.M.; Nuchtern, J.G.; Russell, H.V. Interleukin-6 and soluble interleukin-6 receptor levels as markers of disease extent and prognosis in neuroblastoma. Clin. Cancer Res. 2008, 14, 7028–7034. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, H.; Fujieda, K.; Senju, S.; Ikeda, T.; Oshiumi, H.; Nishimura, Y. Immune-suppressive effects of interleukin-6 on T-cell-mediated anti-tumor immunity. Cancer Sci. 2018, 109, 523–530. [Google Scholar] [CrossRef]
- Ara, T.; Song, L.; Shimada, H.; Keshelava, N.; Russell, H.V.; Metelitsa, L.S.; Groshen, S.G.; Seeger, R.C.; De Clerck, Y.A. Interleukin-6 in the bone marrow microenvironment promotes the growth and survival of neuroblastoma cells. Cancer Res. 2009, 69, 329–337. [Google Scholar] [CrossRef]
- Tsukamoto, H.; Nishikata, R.; Senju, S.; Nishimura, Y. Myeloid-derived suppressor cells attenuate TH1 development through IL-6 production to promote tumor progression. Cancer Immunol. Res. 2013, 1, 64–76. [Google Scholar] [CrossRef]
- Yu, S.H.; Zheng, Q.; Esopi, D.; Macgregor-Das, A.; Luo, J.; Antonarakis, E.S.; Drake, C.G.; Vessella, R.; Morrissey, C.; De Marzo, A.M.; et al. A Paracrine Role for IL6 in Prostate Cancer Patients: Lack of Production by Primary or Metastatic Tumor Cells. Cancer Immunol. Res. 2015, 3, 1175–1184. [Google Scholar] [CrossRef]
- Rose-John, S. IL-6 trans-signaling via the soluble IL-6 receptor: Importance for the pro-inflammatory activities of IL-6. Int. J. Biol. Sci. 2012, 8, 1237–1247. [Google Scholar] [CrossRef]
- Naugler, W.E.; Karin, M. NF-kappaB and cancer-identifying targets and mechanisms. Curr. Opin. Genet. Dev. 2008, 18, 19–26. [Google Scholar] [CrossRef]
- Xie, K. Interleukin-8 and human cancer biology. Cytokine Growth Factor Rev. 2001, 12, 375–391. [Google Scholar] [CrossRef]
- Brat, D.J.; Bellail, A.C.; Van Meir, E.G. The role of interleukin-8 and its receptors in gliomagenesis and tumoral angiogenesis. Neuro Oncol. 2005, 7, 122–133. [Google Scholar] [CrossRef] [PubMed]
- Yuan, A.; Chen, J.J.; Yao, P.L.; Yang, P.C. The role of interleukin-8 in cancer cells and microenvironment interaction. Front. Biosci. 2005, 10, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, F.A.; Pantschenko, A.G.; Miller, L.J.; Anderson, K.; Grunnet, M.; McKenna, P.H.; Kreutzer, D. Angiogenesis and neuroblastomas: Interleukin-8 and interleukin-8 receptor expression in human neuroblastoma. J. Urol. 2000, 164, 1016–1020. [Google Scholar] [CrossRef]
- Alfaro, C.; Sanmamed, M.F.; Rodríguez-Ruiz, M.E.; Teijeira, Á.; Oñate, C.; González, Á.; Ponz, M.; Schalper, K.A.; Pérez-Gracia, J.L.; Melero, I. Interleukin-8 in cancer pathogenesis, treatment and follow-up. Cancer Treat. Rev. 2017, 60, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Mouawad, R.; Rixe, O.; Meric, J.B.; Khayat, D.; Soubrane, C. Serum interleukin-6 concentrations as predictive factor of time to progression in metastatic malignant melanoma patients treated by biochemotherapy: A retrospective study. Cytokines Cell Mol. Ther. 2002, 7, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Chavez, F.A.; Peters-Hybki, D.L.; Barber, R.C.; O’Keefe, G.E. Interleukin-6 promoter haplotypes and interleukin-6 cytokine responses. Shock 2003, 20, 218–223. [Google Scholar] [CrossRef] [PubMed]
- De Michele, A.; Martin, A.M.; Mick, R.; Gor, P.; Wray, L.; Klein-Cabral, M.; Athanasiadis, G.; Colligan, T.; Stadtmauer, E.; Weber, B. Interleukin-6-174G-->C polymorphism is associated with improved outcome in high-risk breast cancer. Cancer Res. 2003, 63, 8051–8056. [Google Scholar]
- Lagmay, J.P.; London, W.B.; Gross, T.G.; Termuhlen, A.; Sullivan, N.; Axel, A.; Mundy, B.; Ranalli, M.; Canner, J.; McGrady, P.; et al. Prognostic significance of interleukin-6 single nucleotide polymorphism genotypes in neuroblastoma: rs1800795 (promoter) and rs8192284 (receptor). Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2009, 15, 5234–5239. [Google Scholar] [CrossRef]
- Totaro, F.; Cimmino, F.; Pignataro, P.; Acierno, G.; De Mariano, M.; Longo, L.; Tonini, G.P.; Iolascon, A.; Capasso, M. Impact of interleukin-6 -174 G>C gene promoter polymorphism on neuroblastoma. PLoS ONE 2013, 8, e76810. [Google Scholar] [CrossRef]
- Fey, M.F.; Tobler, A. An interleukin-8 (IL-8) cDNA clone identifies a frequent HindIII polymorphism. Hum. Genet. 1993, 91, 298. [Google Scholar] [CrossRef]
- Hacking, D.; Knight, J.C.; Rockett, K.; Brown, H.; Frampton, J.; Kwiatkowski, D.P.; Hull, J.; Udalova, I.A. Increased in vivo transcription of an IL-8 haplotype associated with respiratory syncytial virus disease-susceptibility. Genes Immun. 2004, 5, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Hull, J.; Thomson, A.; Kwiatkowski, D. Association of respiratory syncytial virus bronchiolitis with the interleukin 8 gene region in UK families. Thorax 2000, 55, 1023–1027. [Google Scholar] [CrossRef] [PubMed]
- Xue, H.; Liu, J.; Lin, B.; Wang, Z.; Sun, J.; Huang, G. A meta-analysis of interleukin-8 -251 promoter polymorphism associated with gastric cancer risk. PLoS ONE 2012, 7, e28083. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Sawamura, Y.; Tada, M.; Sakuma, S.; Sudo, M.; Abe, H. p55 and p75 tumor necrosis factor receptor expression on human glioblastoma cells. Neurol. Med. Chir. (Tokyo) 1995, 35, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Mao, P.; Xie, C.; Xie, W.; Wang, M.; Jiang, H. Association between interleukin 8-251 T/A and +781 C/T polymorphisms and glioma risk. Diagn Pathol. 2015, 10, 138. [Google Scholar] [CrossRef]
- Zhao, Q.; Jin, M.; Zhang, D.W.; Zhao, W.; Wang, X.S.; Yue, Z.X.; Duan, C.; Huang, C.; Ma, X.L. Serum Interleukin-6 Level and the rs1800795 Polymorphism in its Gene Associated with Neuroblastoma Risk in Chinese Children. Chin. Med. J. 2018, 131, 1075–1078. [Google Scholar] [CrossRef]
- Moreno, A.; Sandoval, K. Diversidad genómica en México: Pasado indígena y mestizaje. Cuicuilco 2013, 20, 249–275. [Google Scholar]
- Consejo de Salubridad General. Guía de Práctica Clínica (GPC): Diagnóstico y Tratamiento de Neuroblastoma en el Paciente Pediátrico. Available online: http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/303_SSA_10_Neuroblastoma/EyR_SSA_303_10.pdf (accessed on 4 November 2020).
- Fishman, D.; Faulds, G.; Jeffery, R.; Mohamed-Ali, V.; Yudkin, J.S.; Humphries, S.; Woo, P. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J. Clin. Investig. 1998, 102, 1369–1376. [Google Scholar] [CrossRef]
- Burger, R. Impact of interleukin-6 in hematological malignancies. Transfus. Med. Hemother. 2013, 40, 336–343. [Google Scholar] [CrossRef]
- Mihara, M.; Hashizume, M.; Yoshida, H.; Suzuki, M.; Shiina, M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin. Sci. 2012, 122, 143–159. [Google Scholar] [CrossRef]
- Chen, M.F.; Chen, P.T.; Lu, M.S.; Lin, P.Y.; Chen, W.C.; Lee, K.D. IL-6 expression predicts treatment response and outcome in squamous cell carcinoma of the esophagus. Mol. Cancer 2013, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Barartabar, Z.; Nikzamir, A.; Sirati-Sabet, M.; Aghamohammadi, E.; Chaleshi, V.; Rostami Nejad, M.; Asadzadeh-Aghdaei, H.; Zali, M.R. The relationship between 174 G/C and -572 G/C of IL-6 gene polymorphisms and susceptibility of celiac disease in the Iranian population. Prz. Gastroenterol. 2018, 13, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Hormazabal, P.; Romero, S.; Musleh, M.; Bustamante, M.; Stambuk, J.; Pisano, R.; Lanzarini, E.; Chiong, H.; Rojas, J.; Castro, V.G.; et al. IL-8-251T>A (rs4073) Polymorphism Is Associated with Prognosis in Gastric Cancer Patients. Anticancer Res. 2018, 38, 5703–5708. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.F.; Wen, Y.; Loh, M.; Wen, Y.Y.; Yang, S.J.; Zhao, Z.M.; Tian, Z.; Huang, H.; Lan, H.; Chen, F.; et al. Interleukin-4 and -8 gene polymorphisms and risk of gastric cancer in a population in Southwestern China. Asian Pac. J. Cancer Prev. 2014, 15, 2951–2957. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.B.; Li, Y.S.; Li, J.; Han, Y.; Liu, Z.D. Interleukin-8 -251A/T gene polymorphism and lung cancer susceptibility: A meta-analysis. J. Cell Mol. Med. 2015, 19, 1218–1222. [Google Scholar] [CrossRef] [PubMed]
- Michaud, D.S.; Daugherty, S.E.; Berndt, S.I.; Platz, E.A.; Yeager, M.; Crawford, E.D.; Hsing, A.; Huang, W.Y.; Hayes, R.B. Genetic polymorphisms of interleukin-1B (IL-1B), IL-6, IL-8, and IL-10 and risk of prostate cancer. Cancer Res. 2006, 66, 4525–4530. [Google Scholar] [CrossRef]
- Chen, C.H.; Ho, C.H.; Hu, S.W.; Tzou, K.Y.; Wang, Y.H.; Wu, C.C. Association between interleukin-8 rs4073 polymorphism and prostate cancer: A meta-analysis. J. Formos. Med. Assoc. 2020, 119, 1201–1210. [Google Scholar] [CrossRef]
- Puthothu, B.; Krueger, M.; Heinze, J.; Forster, J.; Heinzmann, A. Impact of IL8 and IL8-receptor alpha polymorphisms on the genetics of bronchial asthma and severe RSV infections. Clin. Mol. Allergy 2006, 4, 1–6. [Google Scholar] [CrossRef]
- Wang, N.; Zhou, R.; Wang, C.; Guo, X.; Chen, Z.; Yang, S.; Li, Y. −251 T/A polymorphism of the interleukin-8 gene and cancer risk: A HuGE review and meta-analysis based on 42 case-control studies. Mol. Biol. Rep. 2012, 39, 2831–2841. [Google Scholar] [CrossRef]
- Taguchi, A.; Ohmiya, N.; Shirai, K.; Mabuchi, N.; Itoh, A.; Hirooka, Y.; Niwa, Y.; Goto, H. Interleukin-8 promoter polymorphism increases the risk of atrophic gastritis and gastric cancer in Japan. Cancer Epidemiol. Biomark. Prev. 2005, 14, 2487–2493. [Google Scholar] [CrossRef]
- Huang, C.Y.; Chang, W.S.; Tsai, C.W.; Hsia, T.C.; Shen, T.C.; Bau, D.T.; Shui, H.A. The contribution of interleukin-8 genotypes and expression to nasopharyngeal cancer susceptibility in Taiwan. Medicine (Baltimore) 2018, 97, e12135. [Google Scholar] [CrossRef] [PubMed]
- Georgitsi, M.D.; Vitoros, V.; Panou, C.; Tsangaris, I.; Aimoniotou, E.; Gatselis, N.K.; Chasou, E.; Kouliatsis, G.; Leventogiannis, K.; Velissaris, D.; et al. Hellenic Sepsis Study Group. Individualized significance of the -251 A/T single nucleotide polymorphism of interleukin-8 in severe infections. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.W.; Oh, C.H.; Kim, J.W.; Lee, J.W.; Park, M.J.; Shim, J.J.; Lee, C.K.; Jang, J.Y.; Dong, S.H.; Kim, H.J.; et al. Combination of Helicobacter pylori infection and the interleukin 8 -251 T > A polymorphism, but not the mannose-binding lectin 2 codon 54 G > A polymorphism, might be a risk factor of gastric cancer. BMC Cancer 2017, 17, 388. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Abnet, C.C.; Mark, S.D.; Qiao, Y.L.; Dong, Z.W.; Dawsey, S.M.; Taylor, P.R.; Chanock, S.J. Variants of the IL8 and IL8RB genes and risk for gastric cardia adenocarcinoma and esophageal squamous cell carcinoma. Cancer Epidemiol. Biomark. Prev. 2004, 13, 2251–2257. [Google Scholar]
- Arinir, U.; Klein, W.; Rohde, G.; Stemmler, S.; Epplen, J.T.; Schultze-Werninghaus, G. Polymorphisms in the interleukin-8 gene in patients with chronic obstructive pulmonary disease. Electrophoresis 2005, 26, 2888–2891. [Google Scholar] [CrossRef]
- Qin, X.; Deng, Y.; Liao, X.C.; Mo, C.J.; Li, X.; Wu, H.L.; He, Y.N.; Huang, X.M.; Peng, T.; Chen, Z.P.; et al. The IL-8 gene polymorphisms and the risk of the hepatitis B virus/infected patients. DNA Cell Biol. 2012, 31, 1125–1130. [Google Scholar] [CrossRef]
- Olivo-Diaz, A.; Romero-Valdovinos, M.; Gudiño-Ramirez, A.; Reyes-Gordillo, J.; Jimenez-Gonzalez, D.E.; Ramirez-Miranda, M.E.; Martinez-Flores, W.A.; Martinez-Hernandez, F.; Flisser, A.; Maravilla, P. Findings related to IL-8 and IL-10 gene polymorphisms in a Mexican patient population with irritable bowel syndrome infected with Blastocystis. Parasitol. Res. 2012, 111, 487–491. [Google Scholar] [CrossRef]
| Characteristics | Patients n = 27 (%) | Healthy Controls n = 38 (%) | |
|---|---|---|---|
| Age | <18 months | 16 (59.3) | 22(57.9) |
| 18 months–5 years | 6 (22.2) | 9 (23.7) | |
| >5 years | 5 (18.5) | 7(18.4) | |
| Sex | Male | 10 (37.03) | 14 (36.85) |
| Female | 17 (62.97) | 24 (63.15) | |
| INSS stage | E1 | 5 (18.5) | ----- |
| E2b | 2 (7.5) | ----- | |
| E3 | 7 (25.9) | ----- | |
| E4 | 13 (48.1) | ----- | |
| E4S | 0 (0) | ----- | |
| Staging | E1 | 6 (22.2) | ----- |
| E2a | 1 (3.7) | ----- | |
| E3 | 6 (22.2) | ----- | |
| E4 | 14 (51.9) | ----- | |
| INRG | L1 | 5 (18.5) | ----- |
| L2 | 8 (29.6) | ----- | |
| M | 14 (51.9) | ----- | |
| MS | 0 (0) | ----- | |
| Risk | Low | 5 (18.5) | ----- |
| Intermediate | 7 (25.9) | ----- | |
| High | 15 (55.6) | ----- | |
| Primary Tumor Site | Adrenal | 8 (29.6) | ----- |
| Retroperitoneal | 11 (40.7) | ----- | |
| Paraspinal | 3 (11.1) | ----- | |
| Abdomen/Pelvic | 1 (3.7) | ----- | |
| Mediastinal | 4 (14.9) | ||
| Differentiation | Undifferentiated | 2 (7.4) | ----- |
| Partially differentiated | 16 (59.3) | ----- | |
| Differentiated | 5 (18.5) | ----- | |
| Not specified | 4 (14.8) | ----- | |
| Histology (Shimada) | Favorable | 15 (55.6) | ----- |
| Unfavorable | 12 (44.4) | ----- | |
| MYCN | Amplified | 1 (3.7) | ----- |
| Not amplified | 26 (96.3) | 38 (100) | |
| Metastasis at Diagnosis | Yes | 15 (55.5) | ----- |
| No | 12 (44.5) | ----- | |
| Relapse | Yes | 7 (25.9) | |
| Death | Yes | 6 (22.2) |
| SNP | Controls (%) n = 38 | NB Patients (%) n = 27 | OR * (95% CI) | p Value |
|---|---|---|---|---|
| IL-6 −174 G > C rs1800795 | ||||
| GG | 10 (26.3) | 12 (44.4) | Ref | Ref |
| GC | 13 (34.2) | 10 (37) | 0.64 (0.197–2.078) | 0.459 |
| CC | 15 (39.5) | 5 (18.5) | 0.27 (0.074–1.03) | 0.05 |
| GG + GC | 23 (60.5) | 22 (81.5) | 2.86 (0.891–9.23) a | 0.07 a |
| GC + CC | 28 (73.7) | 15 (55.6) | 0.44 (0.156–1.272) b | 0.131 b |
| Allele G | 33 (43.4) | 34 (62.9) | ---- | ---- |
| Allele C | 43 (56.6) | 20 (37.03) | ---- | ---- |
| IL-8 -251 T > A rs4073 | ||||
| TT | 21 (55.3) | 8 (29.6) | Ref | |
| TA | 12 (31.6) | 12 (44.4) | 2.62 (0.83–8.22) | 0.098 |
| AA | 5 (13.1) | 7 (29.9) | 3.67 (0.89–15.01) | 0.07 |
| TT + TA | 32 (84.2) | 20 (74.1) | 0.53 (0.15–1.82) c | 0.31 c |
| TA + AA | 18 (47.4) | 19 (70.4) | 2.63 (0.92–7.48) d | 0.068 d |
| Allele T | 54 (71.05) | 28 (51.85) | ---- | ---- |
| Allele A | 22 (28.95) | 26 (48.1) | ---- | ---- |
| IL-8 + 781 C/T rs2227306 | ||||
| CC | 7 (18.4) | 8 (29.6) | Ref | |
| CT | 15 (39.5) | 16 (59.3) | 0.93 (0.271–3.20) | 0.913 |
| TT | 16 (42.1) | 3 (11.1) | 0.164 (0.033–0.80) | 0.027 |
| CC + CT | 22 (57.9) | 24 (88.9) | 5.81 (1.49–22.71) e | 0.011 e |
| CT + TT | 31 (81.6) | 19 (80.4) | 0.53 (0.167–1.717) f | 0.294 f |
| Allele C | 29 (38.15) | 32 (59.25) | ---- | ---- |
| Allele T | 47 (61.84) | 22 (40.74) | ---- | ---- |
| Variables | Genotype Frequencies of IL-6 rs1800795 n (%) | |||||
|---|---|---|---|---|---|---|
| GG | GC | CC | GG + GC | GC + CC | ||
| INSS stage | E1 | ---- | 1 (3.7) | 4 (14.8) | 1 (3.7) | 5 (18.5) |
| E2b | ---- | 1 (3.7) | 1 (3.7) | 1 (3.7) | 2(7.4) | |
| E3 | 2 (7.4) | 5 (18.5) | ---- | 7 (25.9) | 5 (18.5) | |
| E4 | 10 (37) | 3 (11.1) | ---- | 13 (48.1) | 3 (11.1) | |
| p value | <0.001 | <0.001 | 0.005 | |||
| INRG | L1 | ---- | 1 (3.7) | 4 (14.8) | 1 (3.7) | 5 (18.5) |
| L2 | 1 (3.7) | 6 (22.2) | 1 (3.7) | 7 (25.9) | 7 (25.9) | |
| M | 11 (40.7) | 3 (11.1) | ---- | 14 (51.9) | 3 (11.1) | |
| p value | <0.001 | 0.001 | 0.001 | |||
| Risk | Low | ---- | ---- | 5 (18.5) | ---- | 5 (18.5) |
| Intermediate | 3 (11.1) | 4 (14.8) | ---- | 7 (25.9) | 4 (14.8) | |
| High | 9 (33.3) | 6 (22.2) | ---- | 15 (55.6) | 6 (22.2) | |
| p value | <0.001 | <0.001 | 0.06 | |||
| Differentiation | Undifferentiated | 1 (3.7) | 1 (3.7) | ---- | 2 (7.4) | 1 (3.7) |
| Partially differentiated | 6 (22.2) | 7 (25.9) | 3 (11.1) | 13 (48.1) | 10 (37) | |
| Differentiated | 3 (11.1) | ---- | 2 (7.4) | 3 (11.1) | 2 (7.4) | |
| Not specified | 2 (7.4) | 2 (7.4) | ---- | 4 (14.8) | 2 (7.4) | |
| p value | 0.5 | 0.6 | 0.8 | |||
| Histology (Shimada) | Favorable | 4 (14.8) | 6 (22.2) | 5 (18.5) | 10 (37) | 11 (40.7) |
| Unfavorable | 8 (29.6) | 4 (14.8) | ----- | 12 (44.4) | 4 (14.8) | |
| p value | 0.04 | 0.04 | 0.05 | |||
| MYCN | Amplified | 1 (3.7) | ---- | ----- | 1 (3.7) | ---- |
| Not amplified | 11 (40.7) | 10 (37) | 5 (18.5) | 21 (77.8) | 15 (55.6) | |
| p value | 0.6 | 1 | 0.3 | |||
| Metastasis | Yes | 11 (40.7) | 4 (14.8) | ---- | 15 (55.6) | 4 (14.8) |
| No | 1 (3.7) | 6 (22.2) | 5 (18.5) | 7 (26.9) | 11 (40.7) | |
| p value | 0.001 | 0.01 | 0.001 | |||
| Variables | Genotype Frequencies n (%) SNP IL-8 rs4073 | |||||
|---|---|---|---|---|---|---|
| TT | TA | AA | TT + TA | TA + AA | ||
| INSS stage | E1 | 2 (7.4) | 2 (7.4) | 1 (3.7) | 4 (14.8) | 3 (11.1) |
| E2b | 1 (3.7) | 1 (3.7) | ---- | 2 (7.4) | 1 (3.7) | |
| E3 | 1 (3.7) | 6 (22.2) | ---- | 7 (25.9) | 6 (22.2) | |
| E4 | 4 (14.8) | 3 (11.1) | 6 (22.2) | 7 (25.9) | 9 (33.3) | |
| p value | 0.1 | 0.12 | 0.69 | |||
| INRG | L1 | 3 (11.1) | 2 (7.4) | ----- | 5 (18.5) | 2 (7.4) |
| L2 | 1 (3.7) | 6 (22.2) | 1 (3.7) | 7 (25.9) | 7 (25.9) | |
| M | 4 (14.8) | 4 (14.8) | 6 (22.2) | 8 (29.6) | 10 (37) | |
| p value | 0.1 | 0.12 | 0.21 | |||
| Risk | Low | 3 (11.1) | 2 (7.4) | 5 (18.5) | 2 (7.4) | |
| Intermediate | 2 (7.4) | 4 (14.8) | 1 (3.7) | 6 (22.2) | 5 (18.5) | |
| High | 3 (11.1) | 6 (22.2) | 6 (22.2) | 9 (33.3) | 12 (44.4) | |
| p value | 0.3 | 0.24 | 0.28 | |||
| Differentiation | Undifferentiated | ----- | 2 (7.4) | ----- | 2 (7.4) | 2 (7.4) |
| Partially differentiated | 5 (18.5) | 8 (29.6) | 3 (11.1) | 13 (48.1) | 11 (40.1) | |
| Differentiated | 3 (11.1) | 1 (3.7) | 1 (3.7) | 4 (14.8) | 2 (7.4) | |
| Not specified | ---- | 1 (3.7) | 3 (11.1) | 1 (3.7) | 4 (14.8) | |
| p value | 0.17 | 0.14 | 0.23 | |||
| Histology (Shimada) | Favorable | 6 (22.2) | 8 (29.6) | 1 (3.7) | 14 (51.9) | 9 (33.3) |
| Unfavorable | 2 (7.4) | 4 (14.8) | 6 (22.2) | 6 (22.2) | 10 (37) | |
| p value | 0.04 | 0.02 | 0.23 | |||
| MYCN | Amplified | ---- | --- | 1 (3.7) | ---- | 1 (3.7) |
| Not amplified | 8 (29.6) | 12 (44.4) | 6 (22.2) | 20 (74.1) | 18 (66.7) | |
| p value | 0.1 | 0.2 | 1 | |||
| Metastasis | Yes | 4 (26.7) | 5 (18.5) | 6 (22.2) | 9 (33.3) | 11 (40.7) |
| No | 4 (26.7) | 7 (25.9) | 1 (3.7) | 11 (40.7) | 8 (29.6) | |
| p value | 0.2 | 0.09 | 1 | |||
| Variables | Genotype Frequencies n (%) SNP IL-8 rs2227306 | |||||
|---|---|---|---|---|---|---|
| CC | CT | TT | CC + CT | CT + TT | ||
| INSS stage | E1 | 2 (7.4) | 2 (7.4) | 1 (3.7) | 4 (14.8) | 3 (11.1) |
| E2b | ---- | 1 (3.7) | 1 (3.7) | 1 (3.7) | 2 (7.4) | |
| E3 | 2 (7.4) | 5 (18.5) | ---- | 7 (25.9) | 5 (18.5) | |
| E4 | 4 (14.8) | 8 (29.6) | 1 (3.7) | 12 (44.4) | 9 (33.3) | |
| p value | 0.5 | 0.21 | 1 | |||
| INRG | L1 | 1 (3.7) | 2 (7.4) | 2 (7.4) | 3 (11.1) | 4 (14.8) |
| L2 | 2 (7.4) | 6 (22.2) | ---- | 8 (29.6) | 6 (22.2) | |
| M | 5 (18.5) | 8 (29.6) | 1 (3.7) | 13 (48.1) | 9 (33.3) | |
| p value | 0.33 | 0.14 | 1 | |||
| Risk | Low | 1 (3.7) | 2 (7.4) | 2 (7.4) | 3 (11.1) | 4 (14.8) |
| Intermediate | 3 (11.1) | 4 (14.8) | ---- | 7 (25.9) | 4 (14.8) | |
| High | 4 (14.8) | 10 (37) | 1 (3.7) | 14 (51.9) | 11 (40.7) | |
| p value | 0.34 | 0.12 | 0.7 | |||
| Differentiation | Undifferentiated | ---- | 2 (7.4) | ---- | 2 (7.4) | 2 (7.4) |
| Partially differentiated | 3 (11.1) | 11 (40.7) | 2 (7.4) | 14 (51.8) | 13 (48.1) | |
| Differentiated | 4 (14.8) | ---- | 1 (3.7) | 4 (14.8) | 1 (3.7) | |
| Not specified | 1 (3.7) | 3 (11.1) | ---- | 4 (14.8) | 3 (11.1) | |
| p value | 0.05 | 1 | 0.04 | |||
| Histology (Shimada) | Favorable | 6 (22.2) | 6 (22.2) | 3 (11.1) | 12 (44.4) | 9 (33.3) |
| Unfavorable | 2 (7.4) | 10 (37) | ----- | 12 (44.4) | 10 (37) | |
| p value | 0.06 | 0.23 | 0.23 | |||
| MYCN | Amplified | 1 (3.7) | ---- | ----- | 1 (3.7) | ---- |
| Not amplified | 7 (26.9) | 16 (59.3) | 3 (11.1) | 23 (85.2) | 19 (70.4) | |
| p value | 0.23 | 1 | 0.23 | |||
| Metastasis | Yes | 5 (18.5) | 9 (33.3) | 1 (3.7) | 14 (51.8) | 10 (37) |
| No | 3 (11.1) | 7 (26.9) | 2 (7.4) | 10 (37) | 9 (33.3) | |
| p value | 0.73 | 0.56 | 0.69 | |||
| Variables | GG | GC + CC | p Value | OR * (95 % CI) |
|---|---|---|---|---|
| Risk | 0.07 | 4.5 (0.85–23.8) | ||
| Low/Intermediate | 3 (11.1) | 9 (33.3) | ||
| High | 9 (33.3) | 6(22.2) | ||
| Histology (Shimada) | 0.04 | 5.49 (1.04–28.8) | ||
| Favorable | 4 (14.8) | 11 (40.7) | ||
| Unfavorable | 8 (29.6) | 4 (14.8) | ||
| MYCN | NC | NC | ||
| Amplified | 1 (3.7) | ---- | ||
| Not amplified | 11 (40.7) | 15 (55.6) | ||
| Metastasis | 0.004 | 0.033 (0.003–0.34) | ||
| Yes | 11 (40.7) | 4 (14.8) | ||
| No | 1 (3.7) | 11 (40.7) | ||
| Relapse | 0.10 | 0.21 (0.032–1.41) | ||
| Yes | 5 (18.5) | 2 (7.4) | ||
| No | 7 (25.9) | 13 (48.1) | ||
| Death | 0.04 | 0.1 (0.009–1.028) | ||
| Yes | 5 (18.5) | 1 (3.7) | ||
| No | 7 (25.9) | 14 (51.9) |
| Variables | TT + TA | AA | p Value | OR * (95 % CI) |
|---|---|---|---|---|
| Risk | 0.08 | 7.33 (0.74–72.6) | ||
| Low/Intermediate | 11 (40.7) | 1 (3.7) | ||
| High | 9 (33.3) | 6 (22.2) | ||
| Histology (Shimada) | 0.026 | 14 (1.37–142.8) | ||
| Favorable | 14 (51.9) | 1 (3.7) | ||
| Unfavorable | 6 (22.2) | 6 (22.2) | ||
| MYCN | NC | NC | ||
| Amplified | ---- | 1 (3.7) | ||
| Not amplified | 20 (74.1) | 6 (22.2) | ||
| Metastasis | 0.08 | 0.13 (0.013–1.35) | ||
| Yes | 9 (33.3) | 6 (22.2) | ||
| No | 11 (40.7) | 1 (3.7) | ||
| Relapse | 0.85 | 0.83 (0.121–5.72) | ||
| Yes | 5 (18.5) | 2 (7.4) | ||
| No | 15 (55.6) | 5 (18.5) | ||
| Death | 0.02 | 0.083 (0.01–0.674) | ||
| Yes | 2 (7.4) | 4 (14.8) | ||
| No | 18 (66.7) | 3 (11.1) |
| IL-6 rs1800795 | Low Serum IL-6 Levels | High Serum IL-6 Levels | Value p | OR * (95% CI) |
|---|---|---|---|---|
| GG | 6 (22.2) | 6 (22.2) | Ref | ---- |
| GC | 7 (25.9) | 3 (11.1) | 0.228 | 0.38 (0.08- 1.82) |
| CC | 4 (14.8) | 1 (3.7) | 0.104 | 0.15 (0.016–1.46) |
| GG + GC | 13 (48.1) | 9 (33.3) | 0.193 a | 4.2 (0.483–36.42) a |
| GC + CC | 11 (40.7) | 4 (14.8) | 0.079 b | 0.27 (0.067–1.15) b |
| IL-8 rs4073 | Low Serum IL-8 Levels | High Serum IL-8 Levels | Value p | OR * (95% CI) |
| TT | 8 (29.6) | ---- | Ref | ---- |
| TA | 9 (33.3) | 3 (11.1) | 0.053 | 9 (0.97–83.06) |
| AA | ----- | 7 (25.9) | 0.004 | 29.4 (2.91–296.53) |
| TT + TA | 13 (48.1) | 7 (25.9) | 0.007 c | 0.142 (0.03–0.58) c |
| TA + AA | 6 (22.2) | 13 (48.1) | 0.014 d | 14.3 (1.71–120.48) d |
| IL-8 rs2227306 | Low Serum IL-8 Levels | High Serum IL-8 Levels | Value p | OR * (95% CI) |
| CC | 4 (14.8) | 4 (14.8) | Ref | ---- |
| CT | 7 (25.9) | 9 (33.3) | 0.941 | 0.94 (0.22–3.99) |
| TT | 2 (7.4) | 1 (3.7) | 0.120 | 0.153 (0.01–1.63) |
| CC + CT | 11 (40.7) | 13 (48.1) | 0.093 e | 6.25 (0.73–53.13) e |
| CT + TT | 9 (33.3) | 10 (37) | 0.50 f | 0.62 (0.15–2.52) f |
| Model | HR (95% CI) | Value p |
|---|---|---|
| A | ||
| IL-6 rs1800795 (GC + CC vs. GG) | 0.11 (0.01–1.08) | 0.05 |
| Age (≥18 months vs. <18 months) | 1.59 (0.26–9.52) | 0.60 |
| INSS stage (4 vs. 1,2,3) | NC | NC |
| MYCN (amplified vs. not amplified) | NC | NC |
| B | ||
| IL-8 rs4073 (TT + TA vs. AA) | 0.09 (0.01–0.62) | 0.015 |
| Age (≥18 months vs. <18 months) | 1.10 (0.16–7.48) | 0.91 |
| INSS stage (4 vs. 1,2,3) | NC | NC |
| MYCN (amplified vs. not amplified) | NC | NC |
| C | ||
| IL -8 rs2227306 (CT + TT vs. CC) | 3.2 (0.37–29.03) | 0.28 |
| Age (≥18 months vs. <18 months) | 2.74 (0.49–15.21) | 0.24 |
| INSS stage (4 vs. 1,2,3) | NC | NC |
| MYCN (amplified vs. not amplified) | NC | NC |
| D | ||
| Serum IL-6 levels (High vs. Low) | 11.7 (1.33–103.7) | 0.027 |
| Age (≥18 months vs. <18 months) | 1.54 (0.27–8.71) | 0.61 |
| INSS stage (4 vs. 1,2,3) | NC | NC |
| MYCN (amplified vs. not amplified) | NC | NC |
| E | ||
| Serum IL-8 levels (High vs. Low) | 10.46 (1.18–92.58) | 0.035 |
| Age (≥18 months vs. <18 months) | 3.23 (0.58–17.98) | 0.18 |
| INSS stage (4 vs. 1,2,3) | NC | NC |
| MYCN (amplified vs. not amplified) | NC | NC |
| SNP | Primer Sequence 5′–3′ | Annealing (°C) | Product Size (bp) | Restriction Enzyme | Digestion Fragments (bp) |
|---|---|---|---|---|---|
| IL-6 −174 G > C rs 1800795 | For: ATGCCAAGTGCTGAGTCACTA Rev: TCGAGGGCAGAATGAGCCTC | 58.5 | 230 | Nla-III (NEB®) | GG: 230 GC: 230, 121/109 CC: 121/109 |
| IL-8 −251 T > A rs4073 | For: TCATCCATGATCTTGTTCTAA Rev: GGAAACGCTGAGGTCGA | 57 | 542 | Mfe-I (NEB®) | TT: 542 TA: 542, 450, 92 AA: 450, 92 |
| IL -8 +781 C/T rs2227306 | For: CTCAACTCTTTATATAGGAATT Rev: GATTGATTTTATCAACAGGCA | 54 | 203 | EcoRI (NEB®) | CC: 184, 19 CT: 203, 184, 19 TT: 203 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno-Guerrero, S.S.; Ramírez-Pacheco, A.; Rocha-Ramírez, L.M.; Hernández-Pliego, G.; Eguía-Aguilar, P.; Escobar-Sánchez, M.A.; Reyes-López, A.; Juárez-Villegas, L.E.; Sienra-Monge, J.J.L. Association of Genetic Polymorphisms and Serum Levels of IL-6 and IL-8 with the Prognosis in Children with Neuroblastoma. Cancers 2021, 13, 529. https://doi.org/10.3390/cancers13030529
Moreno-Guerrero SS, Ramírez-Pacheco A, Rocha-Ramírez LM, Hernández-Pliego G, Eguía-Aguilar P, Escobar-Sánchez MA, Reyes-López A, Juárez-Villegas LE, Sienra-Monge JJL. Association of Genetic Polymorphisms and Serum Levels of IL-6 and IL-8 with the Prognosis in Children with Neuroblastoma. Cancers. 2021; 13(3):529. https://doi.org/10.3390/cancers13030529
Chicago/Turabian StyleMoreno-Guerrero, Silvia Selene, Arturo Ramírez-Pacheco, Luz María Rocha-Ramírez, Gabriela Hernández-Pliego, Pilar Eguía-Aguilar, María Argelia Escobar-Sánchez, Alfonso Reyes-López, Luis Enrique Juárez-Villegas, and Juan José Luis Sienra-Monge. 2021. "Association of Genetic Polymorphisms and Serum Levels of IL-6 and IL-8 with the Prognosis in Children with Neuroblastoma" Cancers 13, no. 3: 529. https://doi.org/10.3390/cancers13030529
APA StyleMoreno-Guerrero, S. S., Ramírez-Pacheco, A., Rocha-Ramírez, L. M., Hernández-Pliego, G., Eguía-Aguilar, P., Escobar-Sánchez, M. A., Reyes-López, A., Juárez-Villegas, L. E., & Sienra-Monge, J. J. L. (2021). Association of Genetic Polymorphisms and Serum Levels of IL-6 and IL-8 with the Prognosis in Children with Neuroblastoma. Cancers, 13(3), 529. https://doi.org/10.3390/cancers13030529