The Impact of Core Tissues on Successful Next-Generation Sequencing Analysis of Specimens Obtained through Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration
Abstract
Simple Summary
Abstract
1. Introduction
2. Methods
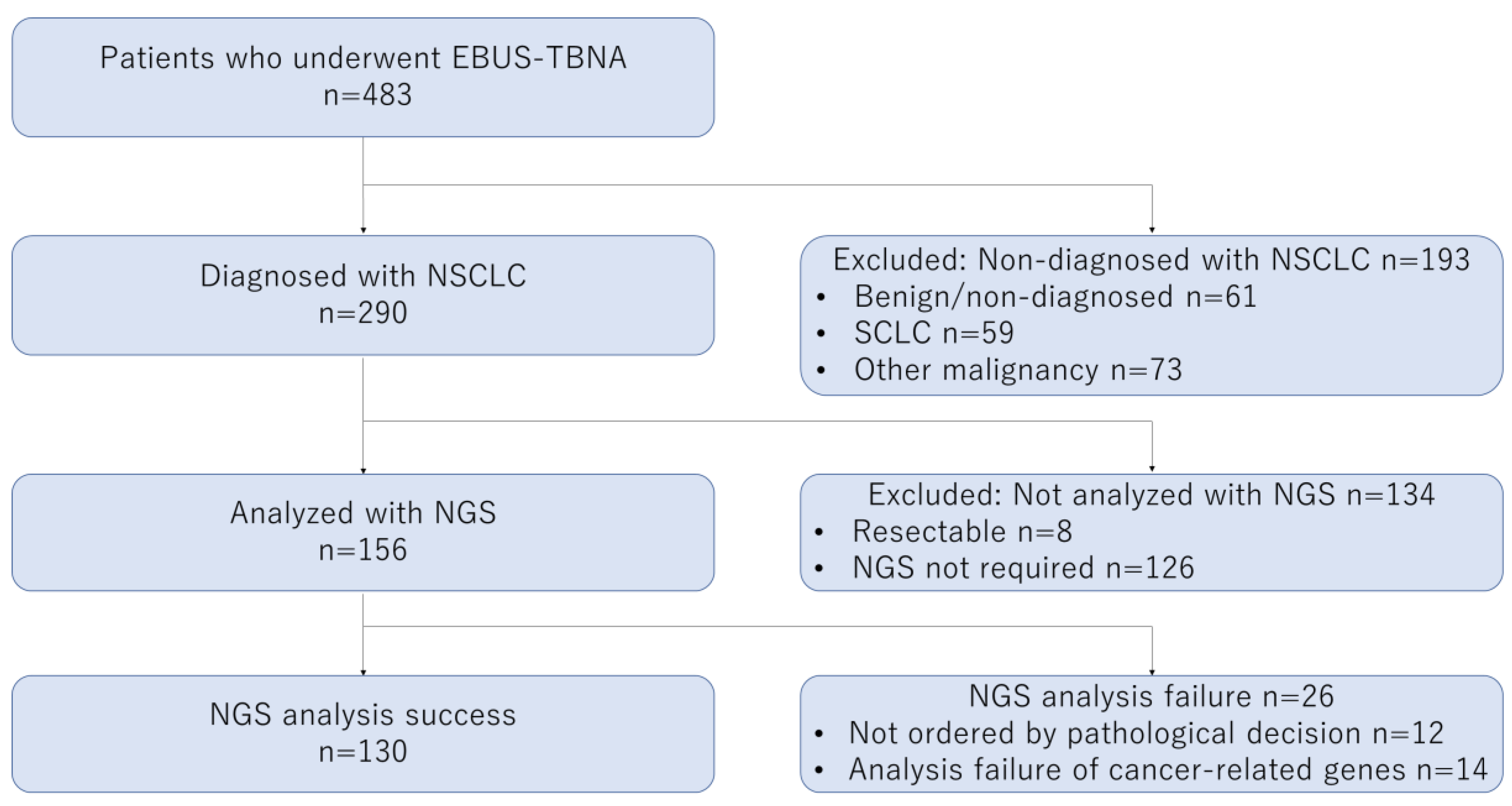
2.1. Patients
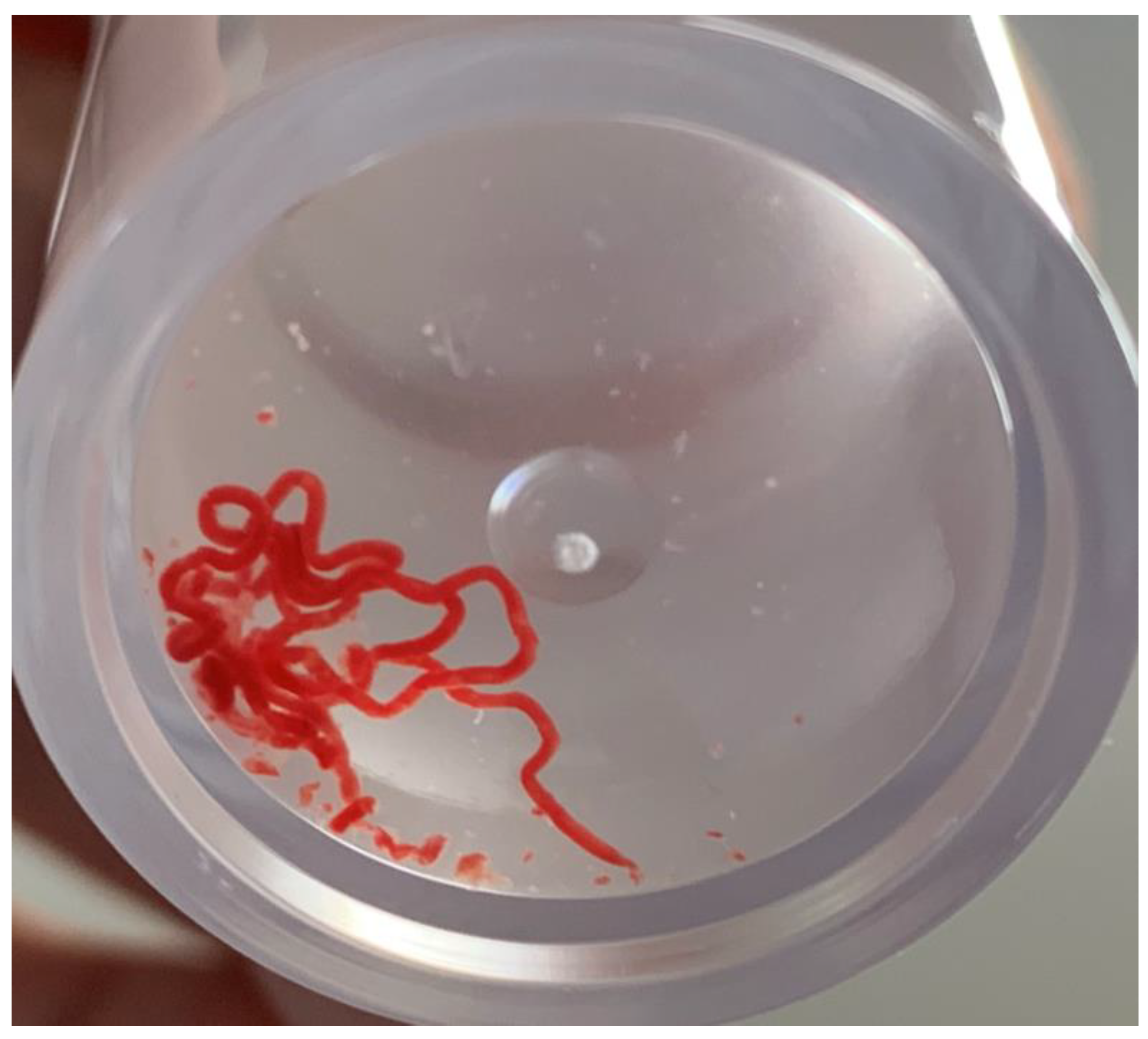
2.2. EBUS-TBNA Procedure
2.3. The OncomineTM Dx Target Test Multi-CDx System
2.4. EBUS Findings and Pathological Diagnosis
2.5. Statistical Analysis
3. Results
3.1. Patients and Target Lesions
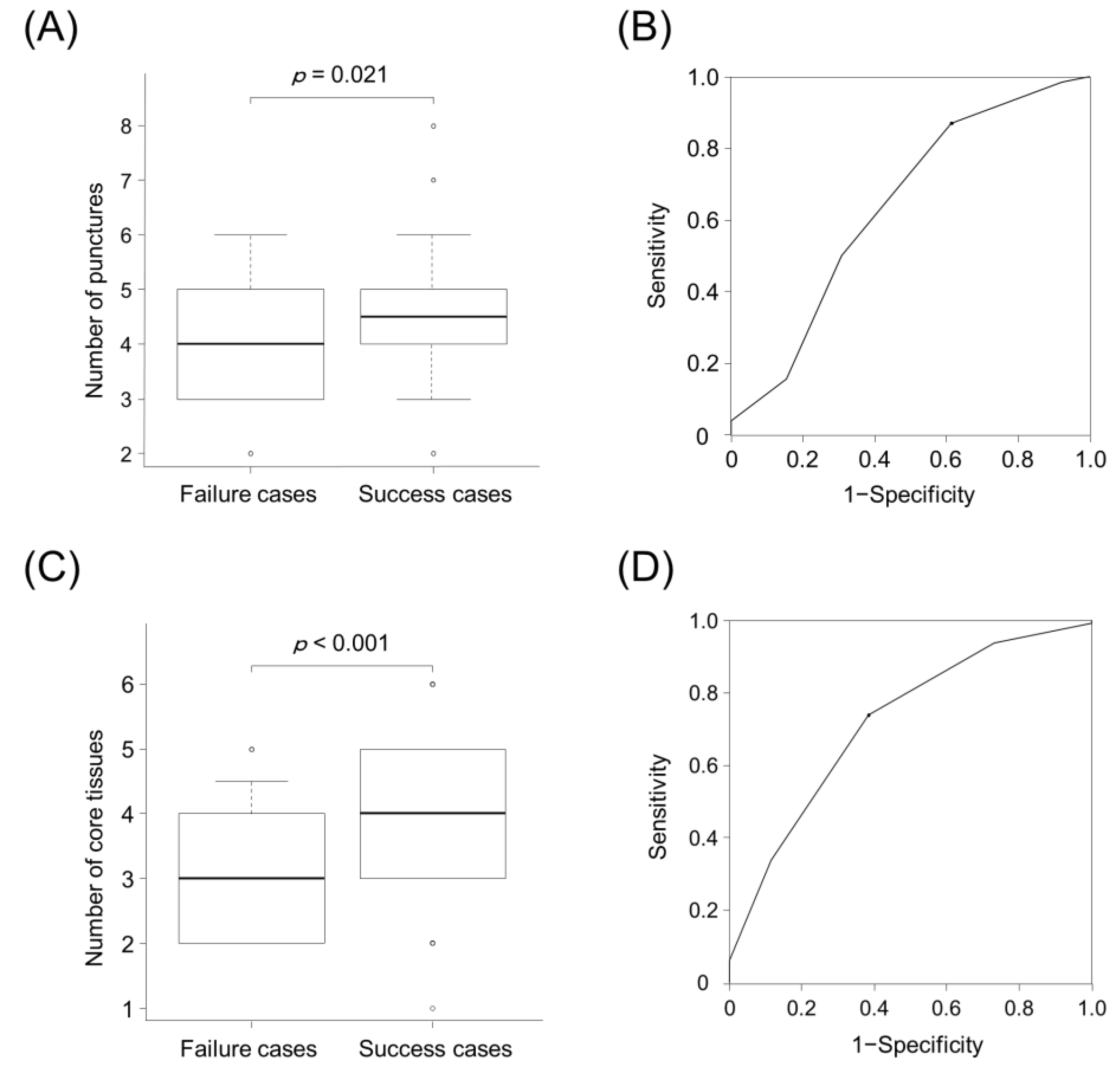
3.2. Numbers of Punctures and Core Tissues for Successful NGS
3.3. Clinical Factors Affecting Successful NGS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herbst, R.S.; Morgensztern, D.; Boshoff, C. The biology and management of non-small cell lung cancer. Nature 2018, 553, 446–454. [Google Scholar] [CrossRef]
- Maemondo, M.; Inoue, A.; Kobayashi, K.; Sugawara, S.; Oizumi, S.; Isobe, H.; Gemma, A.; Harada, M.; Yoshizawa, H.; Kinoshita, I.; et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N. Engl. J. Med. 2010, 362, 2380–2388. [Google Scholar] [CrossRef]
- Solomon, B.J.; Mok, T.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 2014, 371, 2167–2177. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Ou, S.-H.I.; Bang, Y.-J.; Camidge, D.R.; Solomon, B.J.; Salgia, R.; Riely, G.J.; Varella-Garcia, M.; Shapiro, G.I.; Costa, D.B.; et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N. Engl. J. Med. 2014, 371, 1963–1971. [Google Scholar] [CrossRef]
- Planchard, D.; Besse, B.; Groen, H.J.M.; Souquet, P.-J.; Quoix, E.; Baik, C.S.; Barlesi, F.; Kim, T.M.; Mazieres, J.; Novello, S.; et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: An open-label, multicentre phase 2 trial. Lancet Oncol. 2016, 17, 984–993. [Google Scholar] [CrossRef]
- Reck, M.; Rabe, K.F. Precision diagnosis and treatment for advanced non-small-cell lung cancer. N. Engl. J. Med. 2017, 377, 849–861. [Google Scholar] [CrossRef]
- Campbell, J.D.; Alexandrov, A.; Kim, J.; Wala, J.; Berger, A.H.; Pedamallu, C.S.; Shukla, S.A.; Guo, G.; Brooks, A.N.; Murray, B.A.; et al. Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. Nat. Genet. 2016, 48, 607–616. [Google Scholar] [CrossRef]
- Kage, H.; Kohsaka, S.; Shinozaki-Ushiku, A.; Hiraishi, Y.; Sato, J.; Nagayama, K.; Ushiku, T.; Takai, D.; Nakajima, J.; Miyagawa, K.; et al. Small lung tumor biopsy samples are feasible for high quality targeted next generation sequencing. Cancer Sci. 2019, 110, 2652–2657. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, M.; Duose, D.Y.; Singh, R.R.; Barkoh, B.A.; Manekia, J.; Harmon, M.A.; Patel, K.P.; Routbort, M.J.; Medeiros, L.J.; Wistuba, I.I.; et al. Versatile ion S5XL sequencer for targeted next generation sequencing of solid tumors in a clinical laboratory. PLoS ONE 2017, 12, e0181968. [Google Scholar]
- Murakami, S.; Yokose, T.; Nemoto, D.; Suzuki, M.; Usui, R.; Nakahara, Y.; Kondo, T.; Kato, T.; Saito, H. Suitability of bronchosocpic biopsy tissue samples for next-generation sequencing. Diagnostics 2021, 11, 391. [Google Scholar] [CrossRef] [PubMed]
- Tone, M.; Inomata, M.; Awano, N.; Kuse, N.; Takada, K.; Minami, J.; Muto, Y.; Fujimoto, K.; Kumasaka, T.; Izumo, T. Comparison of adequacy between transbronchial lung cryobiopsy samples and endobronchial ultrasound-guided transbronchial needle aspiration samples for next-generation sequencing analysis. Thorac. Cancer 2021, 12, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Takeyasu, Y.; Yoshida, T.; Motoi, N.; Teishikata, T.; Tanaka, M.; Matsumoto, Y.; Shinno, Y.; Okuma, Y.; Goto, Y.; Horinouchi, H.; et al. Feasibility of next-generation sequencing (OncomineTM Dx Target Test) for the screening of oncogenic mutations in advanced non-small-cell lung cancer patients. Jpn. J. Clin. Oncol. 2021, 51, 1114–1122. [Google Scholar] [CrossRef]
- Udagawa, H.; Kirita, K.; Naito, T.; Nomura, S.; Ishibashi, M.; Matsuzawa, R.; Hisakane, K.; Usui, Y.; Matsumoto, S.; Yoh, K.; et al. Feasibility and utility of transbronchial cryobiopsy in precision medicine for lung cancer: Prospective single-arm study. Cancer Sci. 2020, 111, 2488–2498. [Google Scholar] [CrossRef] [PubMed]
- Martin-Deleon, R.; Teixido, C.; Lucena, C.M.; Martinez, D.; Fontana, A.; Reyes, R.; García, M.; Viñolas, N.; Vollmer, I.; Sanchez, M.; et al. EBUS-TBNA cytological samples for comprehensive molecular testing in non–small cell lung cancer. Cancers 2021, 13, 2084. [Google Scholar] [CrossRef]
- Xie, F.; Zheng, X.; Mao, X.; Zhao, R.; Ye, J.; Zhang, Y.; Sun, J. Next-generation sequencing for genotyping of endobronchial ultrasound-guided transbronchial needle aspiration samples in lung cancer. Ann. Thorac. Surg. 2019, 108, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Stoy, S.P.; Segal, J.P.; Mueller, J.; Furtado, L.V.; Vokes, E.E.; Patel, J.D.; Murgu, S. Feasibility of endobronchial ultrasound-guided transbronchial needle aspiration cytology specimens for next generation sequencing in non–small-cell lung cancer. Clin. Lung Cancer 2018, 19, 230–238.e2. [Google Scholar] [CrossRef]
- Oezkan, F.; Herold, T.; Darwiche, K.; Eberhardt, W.E.E.; Worm, K.; Christoph, D.C.; Wiesweg, M.; Freitag, L.; Schmid, K.-W.; Theegarten, D.; et al. Rapid and highly sensitive detection of therapeutically relevant oncogenic driver mutations in EBUS-TBNA specimens from patients with lung adenocarcinoma. Clin. Lung Cancer 2018, 19, e879–e884. [Google Scholar] [CrossRef]
- Turner, S.R.; Buonocore, D.; Desmeules, P.; Rekhtman, N.; Dogan, S.; Lin, O.; Arcila, M.E.; Jones, D.R.; Huang, J. Feasibility of endobronchial ultrasound transbronchial needle aspiration for massively parallel next-generation sequencing in thoracic cancer patients. Lung Cancer 2018, 119, 85–90. [Google Scholar] [CrossRef]
- Chaddha, U.; Hogarth, D.K.; Murgu, S. The role of endobronchial ultrasound transbronchial needle aspiration for programmed death ligand 1 testing and next generation sequencing in advanced non-small cell lung cancer. Ann. Transl. Med. 2019, 7, 351. [Google Scholar] [CrossRef]
- Gu, P.; Zhao, Y.-Z.; Jiang, L.-Y.; Zhang, W.; Xin, Y.; Han, B.-H. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: A systematic review and meta-analysis. Eur. J. Cancer 2009, 45, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.; Shah, P.L.; Edmonds, L.; Lim, E. Test performance of endobronchial ultrasound and transbronchial needle aspiration biopsy for mediastinal staging in patients with lung cancer: Systematic review and meta-analysis. Thorax 2009, 64, 757–762. [Google Scholar] [CrossRef]
- Nakajima, T.; Yasufuku, K.; Takahashi, R.; Shingyoji, M.; Hirata, T.; Itami, M.; Matsui, Y.; Itakura, M.; Iizasa, T.; Kimura, H. Comparison of 21-gauge and 22-gauge aspiration needle during endobronchial ultrasound-guided transbronchial needle aspiration. Respirology 2011, 16, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Wahidi, M.M.; Herth, F.; Yasufuku, K.; Shepherd, R.W.; Yarmus, L.; Chawla, M.; Lamb, C.; Casey, K.R.; Patel, S.; Silvestri, G.A.; et al. Technical aspects of endobronchial ultrasound-guided transbronchial needle aspiration: CHEST guideline and expert panel report. Chest 2016, 149, 816–835. [Google Scholar] [CrossRef]
- Uchimura, K.; Yamasaki, K.; Sasada, S.; Hara, S.; Tachiwada, T.; Kawanami, T.; Kisohara, A.; Yatera, K. Evaluation of histological specimens obtained by two types of EBUS-TBNA needles: A comparative study. Jpn. J. Clin Oncol. 2020, 50, 1298–1305. [Google Scholar] [CrossRef]
- Fujiwara, T.; Yasufuku, K.; Nakajima, T.; Chiyo, M.; Yoshida, S.; Suzuki, M.; Shibuya, K.; Hiroshima, K.; Nakatani, Y.; Yoshino, I. The utility of sonographic features during endobronchial ultrasound-guided transbronchial needle aspiration for lymph node staging in patients with lung cancer: A standard endobronchial ultrasound image classification system. Chest 2010, 138, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, T.; Anayama, T.; Shingyoji, M.; Kimura, H.; Yoshino, I.; Yasufuku, K. Vascular image patterns of lymph nodes for the prediction of metastatic disease during EBUS-TBNA for mediastinal staging of lung cancer. J. Thorac. Oncol. 2012, 7, 1009–1014. [Google Scholar] [CrossRef]
- Uchimura, K.; Yamasaki, K.; Sasada, S.; Hara, S.; Ikushima, I.; Chiba, Y.; Tachiwada, T.; Kawanami, T.; Yatera, K. Quantitative analysis of endobronchial ultrasound elastography in computed tomography-negative mediastinal and hilar lymph nodes. Thorac. Cancer 2020, 11, 2590–2599. [Google Scholar] [CrossRef] [PubMed]
- Glazer, H.S.; Siegel, M.J.; Sagel, S.S. Low-attenuation mediastinal masses on CT. Am. J. Roentgenol. 1989, 152, 1173–1177. [Google Scholar] [CrossRef]
- FDA. Summary of Safety and Effectiveness Data for Oncomine Dx Target Test. 2017. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160045B.pdf (accessed on 29 August 2021).
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Yarmus, L.; Akulian, J.; Gilbert, C.; Feller-Kopman, D.; Lee, H.J.; Zarogoulidis, P.; Lechtzin, N.; Ali, S.Z.; Sathiyamoorthy, V. Optimizing endobronchial ultrasound for molecular analysis. How many passes are needed? Ann. Am. Thorac. Soc. 2013, 10, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Izumo, T.; Sasada, S.; Watanabe, J.; Chavez, C.; Matsumoto, Y.; Tsuchida, T. Comparison of two 22G aspiration needles for histologic sampling during endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). Jpn. J. Clin. Oncol. 2014, 44, 841–845. [Google Scholar] [CrossRef][Green Version]
- Oki, M.; Saka, H.; Kitagawa, C.; Kogure, Y.; Murata, N.; Ichihara, S.; Moritani, S.; Ando, M. Randomized study of 21-gauge versus 22-gauge endobronchial ultrasound-guided transbronchial needle aspiration needles for sampling histology specimens. J. Bronchol. Interv. Pulmonol. 2011, 18, 306–310. [Google Scholar] [CrossRef]
- Felice, C.D.; Young, B.; Matta, M. Comparison of specimen adequacy and diagnostic accuracy of a 25-gauge and 22-gauge needle in endobronchial ultrasound-guided transbronchial needle aspiration. J. Thorac. Dis. 2019, 11, 3643–3649. [Google Scholar] [CrossRef]
- Sakaguchi, T.; Inoue, T.; Miyazawa, T.; Mineshita, M. Comparison of the 22-gauge and 25-gauge needles for endobronchial ultrasound-guided transbronchial needle aspiration. Respir. Investig. 2021, 59, 235–239. [Google Scholar] [CrossRef]
- Okubo, Y.; Matsumoto, Y.; Tanaka, M.; Imabayashi, T.; Uezono, Y.; Watanabe, S.-I.; Tsuchida, T. Clinical validity of 25-gauge endobronchial ultrasound-guided transbronchial needle in lymph node staging of lung cancer. J. Thorac. Dis. 2021, 13, 3033–3041. [Google Scholar] [CrossRef]
- Varela-Lema, L.; Fernández-Villar, A.; Ruano-Ravina, A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: A systematic review. Eur. Respir. J. 2009, 33, 1156–1164. [Google Scholar] [CrossRef] [PubMed]
- Eapen, G.A.; Shah, A.M.; Lei, X.; Jimenez, C.A.; Morice, R.C.; Yarmus, L.; Filner, J.; Ray, C.; Michaud, G.; Greenhill, S.R.; et al. Complications, consequences, and practice patterns of endobronchial ultrasound-guided transbronchial needle aspiration: Results of the AQuIRE registry. Chest 2013, 143, 1044–1053. [Google Scholar] [CrossRef] [PubMed]
- Asano, F.; Aoe, M.; Ohsaki, Y.; Okada, Y.; Sasada, S.; Sato, S.; Suzuki, E.; Semba, H.; Fukuoka, K.; Fujino, S.; et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: A nationwide survey by the Japan Society for Respiratory Endoscopy. Respir. Res. 2013, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Kang, N.; Shin, S.H.; Yoo, H.; Jhun, B.W.; Lee, K.; Um, S.-W.; Kim, H.; Jeong, B.-H. Infectious complications of EBUS-TBNA: A nested case-control study using 10-year registry data. Lung Cancer 2021, 161, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Drilon, A.; Wang, L.; Arcila, M.E.; Balasubramanian, S.; Greenbowe, J.R.; Ross, J.S.; Stephens, P.; Lipson, D.; Miller, V.A.; Kris, M.G.; et al. Broad, hybrid capture-based next-generation sequencing identifies actionable genomic alterations in lung adenocarcinomas otherwise negative for such alterations by other genomic testing approaches. Clin. Cancer Res. 2015, 21, 3631–3639. [Google Scholar] [CrossRef] [PubMed]

| Sample Type | Gene Name | ||||||
|---|---|---|---|---|---|---|---|
| DNA | AKT1 | ALK | AR | BRAF | CDK4 | CTNNB1 | DDR2 |
| EGFR | ERBB2 | ERBB3 | ERBB4 | ESR1 | FGFR2 | FGFR3 | |
| GNA11 | GNAQ | HRAS | IDH1 | IDH2 | JAK1 | JAK2 | |
| JAK3 | KIT | KRAS | MAP2K1 | MAP2K2 | MET | MTOR | |
| NRAS | PDGFRA | PIK3CA | RAF1 | RET | ROS1 | SMO | |
| RNA | ABL1 | ALK | AXL | BRAF | ERBB2 | ERG | ETV1 |
| ETV4 | ETV5 | FGFR1 | FGFR2 | FGFR3 | MET | NTRK1 | |
| NTRK2 | NTRK3 | PDGFRA | PPARG | RAF1 | RET | ROS1 | |
| Characteristics | All Cases | Success Cases | Failure Cases | p Value † |
|---|---|---|---|---|
| (n = 156) | (n = 130) | (n = 26) | ||
| Age, years | 70 (31–91) | 70 (31–87) | 70 (51–91) | 0.54 |
| Sex, male | 103 (66.0) | 84 (64.6) | 19 (73.1) | 0.50 |
| Smoking history | 0.47 | |||
| Current or past | 116 (74.4) | 95 (73.1) | 21 (80.8) | |
| Never | 40 (25.6) | 35 (26.9) | 5 (19.2) | |
| Tumor clinical stage | 0.81 | |||
| II | 3 (1.9) | 3 (2.3) | 0 (0) | |
| III | 64 (41.0) | 53 (40.8) | 11 (42.3) | |
| IV | 77 (49.4) | 65 (50.0) | 12 (46.2) | |
| Recurrence | 12 (7.7) | 9 (6.9) | 3 (11.5) | - |
| Size of lymph nodes | 0.45 | |||
| Short axis on CT, mm | 14.5 (5.2–66.8) | 14.6 (5.2–66.8) | 14.1 (7.5–43.7) | |
| Necrotic finding on CT | 0.52 | |||
| Positive | 70 (44.9) | 60 (46.2) | 10 (38.5) | |
| Negative | 86 (55.1) | 70 (53.8) | 16 (61.5) | |
| Location of lymph nodes | 0.62 | |||
| Upper paratracheal (2R, 2L, 3p) | 11 (7.1) | 9 (6.9) | 2 (7.7) | |
| Lower paratracheal (4R, 4L) | 60 (38.5) | 51 (39.2) | 9 (34.6) | |
| Subcarinal (7) | 43 (27.6) | 34 (26.2) | 9 (34.6) | |
| Hilar (10R, 10L) | 2 (1.3) | 1 (0.8) | 1 (3.8) | |
| Interlobar and lobar (11, 12) | 19 (12.3) | 16 (12.3) | 3 (11.5) | |
| Others (lung, pleura) | 21 (13.5) | 19 (14.6) | 2 (7.7) | |
| Pathological diagnosis | 0.48 | |||
| Adenocarcinoma | 101 (64.7) | 86 (66.2) | 15 (57.7) | |
| Squamous cell carcinoma | 21 (13.5) | 18 (13.8) | 3 (11.5) | |
| Other subtypes or not otherwise specified | 34 (21.8) | 26 (20.0) | 8 (30.8) | |
| SUVmax on PET-CT | 0.15 | |||
| ≥2.5 | 127 (81.4) | 109 (83.8) | 18 (69.2) | |
| <2.5 | 17 (10.9) | 13 (10.0) | 4 (15.4) | |
| Not evaluated | 12 (7.7) | 8 (6.2) | 4 (15.4) | |
| Variables | Univariable Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| Success Cases/All Cases (%) | p Value † | Odds Ratio (95 %CI) | p Value ‡ | |
| Needle size | 0.79 | - | - | |
| 25-gauge | 23/28 (82.1) | |||
| 22-gauge | 107/128 (83.6) | |||
| Systemic staging | 1.0 | - | - | |
| Performed | 41/49 (83.7) | |||
| Not performed | 89/107 (83.2) | |||
| Necrotic finding on CT | 0.52 | - | - | |
| Positive | 55/64 (85.9) | |||
| Negative | 75/92 (81.5) | |||
| B-mode categories | ||||
| Short axis, mm | 0.62 | - | - | |
| ≤10 | 32/37 (86.5) | |||
| >10 | 98/119 (82.4) | |||
| Shape | 0.82 | - | - | |
| Round | 42/51 (82.4) | |||
| Oval | 88/105 (83.8) | |||
| Margin | 0.63 | - | - | |
| Distinct | 97/115 (84.3) | |||
| Indistinct | 33/41 (80.5) | |||
| Echogenicity | 1.0 | - | - | |
| Heterogeneous | 128/154 (83.1) | |||
| Homogeneous | 2/2 (100) | |||
| Central hilar structure | 0.21 | - | - | |
| Presence | 11/11 (100) | |||
| Absence | 119/145 (82.1) | |||
| Coagulation necrosis sign | 1.0 | - | - | |
| Presence | 37/44 (84.1) | |||
| Absence | 93/112 (83.0) | |||
| Color/power Doppler images | 1.0 | - | - | |
| Vascular pattern II–III | 76/91 (83.5) | |||
| Vascular pattern 0–I | 54/65 (83.1) | |||
| Number of punctures | 0.004 | 1.67 (0.49–5.62) | 0.41 | |
| <4 | 17/27 (63.0) | |||
| ≥4 | 113/129 (87.6) | |||
| Number of core tissues | <0.001 | 3.39 (1.09–10.6) | 0.035 | |
| <4 | 34/50 (68.0) | |||
| ≥4 | 96/106 (92.5) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uchimura, K.; Yanase, K.; Imabayashi, T.; Takeyasu, Y.; Furuse, H.; Tanaka, M.; Matsumoto, Y.; Sasada, S.; Tsuchida, T. The Impact of Core Tissues on Successful Next-Generation Sequencing Analysis of Specimens Obtained through Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration. Cancers 2021, 13, 5879. https://doi.org/10.3390/cancers13235879
Uchimura K, Yanase K, Imabayashi T, Takeyasu Y, Furuse H, Tanaka M, Matsumoto Y, Sasada S, Tsuchida T. The Impact of Core Tissues on Successful Next-Generation Sequencing Analysis of Specimens Obtained through Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration. Cancers. 2021; 13(23):5879. https://doi.org/10.3390/cancers13235879
Chicago/Turabian StyleUchimura, Keigo, Komei Yanase, Tatsuya Imabayashi, Yuki Takeyasu, Hideaki Furuse, Midori Tanaka, Yuji Matsumoto, Shinji Sasada, and Takaaki Tsuchida. 2021. "The Impact of Core Tissues on Successful Next-Generation Sequencing Analysis of Specimens Obtained through Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration" Cancers 13, no. 23: 5879. https://doi.org/10.3390/cancers13235879
APA StyleUchimura, K., Yanase, K., Imabayashi, T., Takeyasu, Y., Furuse, H., Tanaka, M., Matsumoto, Y., Sasada, S., & Tsuchida, T. (2021). The Impact of Core Tissues on Successful Next-Generation Sequencing Analysis of Specimens Obtained through Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration. Cancers, 13(23), 5879. https://doi.org/10.3390/cancers13235879






