Letermovir Prophylaxis and Cytomegalovirus Reactivation in Adult Hematopoietic Cell Transplant Recipients with and without Acute Graft Versus Host Disease
Abstract
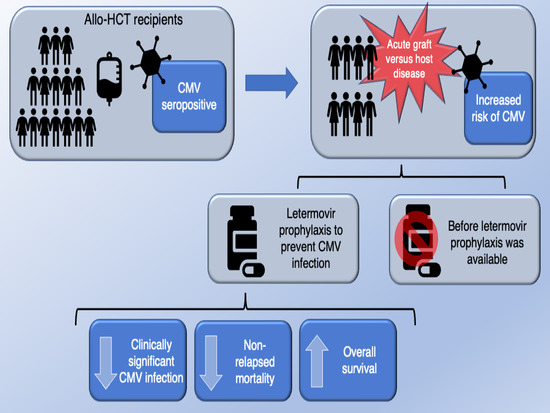
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meyers, J.D.; Flournoy, N.; Thomas, E.D. Risk Factors for Cytomegalovirus Infection after Human Marrow Transplantation. J. Infect. Dis. 1986, 153, 478–488. [Google Scholar] [CrossRef] [PubMed]
- Ljungman, P.; Brand, R.; Hoek, J.; de la Camara, R.; Cordonnier, C.; Einsele, H.; Styczynski, J.; Ward, K.N.; Cesaro, S. Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Donor cytomegalovirus status influences the outcome of allogeneic stem cell trans- plant: A study by the European Group for Blood and Marrow Transplantation. Clin. Infect. Dis. 2014, 59, 473–481. [Google Scholar] [CrossRef]
- Teira, P.; Battiwalla, M.; Ramanathan, M.; Barrett, A.J.; Ahn, K.W.; Chen, M.; Green, J.S.; Saad, A.; Antin, J.H.; Savani, B.N.; et al. Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: A CIBMTR analysis. Blood 2016, 127, 2427–2438. [Google Scholar] [CrossRef]
- Boeckh, M.; Ljungman, P. How we treat cytomegalovirus in hematopoietic cell transplant recipients. Blood 2009, 113, 5711–5719. [Google Scholar] [CrossRef]
- Broers, A.E.; van der Holt, R.; van Esser, J.W.; Gratama, J.W.; Henzen-Logmans, S.; Kuenen-Boumeester, V.; Löwenberg, B.; Cornelissen, J.J. Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation. Blood 2000, 95, 2240–2245. [Google Scholar] [CrossRef] [PubMed]
- Ljungman, P.; Schmitt, M.; Marty, F.; Maertens, J.; Chemaly, R.F.; A Kartsonis, N.; Butterton, J.R.; Wan, H.; Teal, V.L.; Sarratt, K.; et al. A Mortality Analysis of Letermovir Prophylaxis for Cytomegalovirus (CMV) in CMV-seropositive Recipients of Allogeneic Hematopoietic Cell Transplantation. Clin. Infect. Dis. 2019, 70, 1525–1533. [Google Scholar] [CrossRef]
- Dziedzic, M.; Sadowska-krawczenko, I.; Styczynski, J. Risk factors for cytomegalovirus infection after allogeneic hematopoietic cell transplantation in malignancies: Proposal for classification. Anticancer Res. 2017, 37, 6551–6556. [Google Scholar]
- Zaia, J.A.; Gallez-Hawkins, G.M.; Tegtmeier, B.R.; Ter Veer, A.; Li, X.; Niland, J.C.; Forman, S.J. Late cytomegalovirus disease in marrow transplantation is predicted by virus load in plasma. J. Infect. Dis. 1997, 176, 782–785. [Google Scholar] [CrossRef][Green Version]
- El Helou, G.; Razonable, R.R. Letermovir for the prevention of cytomegalovirus infection and disease in transplant recipients: An evidence-based review. Infect. Drug Resist. 2019, 12, 1481–1491. [Google Scholar] [CrossRef] [PubMed]
- Chemaly, R.F.; Ullmann, A.J.; Ehninger, G.; Romee, R.; di Persio, J.F. CMV Prophylaxis in Hematopoietic-Cell Transplantation. N. Engl. J. Med. 2014, 371, 576–577. [Google Scholar] [CrossRef]
- Marty, F.M.; Ljungman, P.; Chemaly, R.F.; Maertens, J.; Dadwal, S.S.; Duarte, R.F.; Haider, S.; Ullmann, A.J.; Katayama, Y.; Brown, J.; et al. Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell trans-plantation. N. Engl. J. Med. 2017, 377, 2433–2444. [Google Scholar] [CrossRef]
- Peric, Z.; Wilson, J.; Durakovic, N.; Ostojic, A.; Desnica, L.; Vranjes, V.R.; Marekovic, I.; Serventi-Seiwerth, R.; Vrhovac, R. Early human cytomegalovirus reactivation is associated with lower incidence of relapse of myeloproliferative disorders after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2018, 53, 1450–1456. [Google Scholar] [CrossRef]
- Karam, E.; LaPorte, J.; Sizemore, C.; Zhang, X.; Holland, K.; Solh, M.; Morris, L.E.; Bashey, A.; Solomon, S.R. Real world outcomes of letermovir prophylaxis in unselected high risk CMV seropositive hematopoietic stem cell transplant recipients. Blood 2019, 134, 3269. [Google Scholar] [CrossRef]
- Anderson, A.; Raja, M.; Vazquez, N.; Morris, M.; Komanduri, K.; Camargo, J. Clinical “real-world” experience with letermovir for prevention of cytomegalovirus infection in allogeneic hematopoietic cell transplant recipients. Clin. Transplant. 2020, 34, e13866. [Google Scholar] [CrossRef]
- Chen, K.; Cheng, M.P.; Hammond, S.P.; Einsele, H.; Marty, F.M. Antiviral prophylaxis for cytomegalovirus infection in allogeneic hematopoietic cell transplantation. Blood Adv. 2018, 2, 2159–2175. [Google Scholar] [CrossRef] [PubMed]
- Studer, U.; Khanna, N.; Leuzinger, K.; Hirsch, H.H.; Heim, D.; Lengerke, C.; Tsakiris, D.A.; Halter, J.; Gerull, S.; Passweg, J.; et al. Incidence of CMV Replication and the Role of Letermovir Primary/Secondary Prophylaxis in the Early Phase After Allogeneic Hematopoietic Stem Cell Transplantation—A Single Centre Study. Anticancer. Res. 2020, 10, 5909–5917. [Google Scholar] [CrossRef] [PubMed]
- Bansal, R.; A Gordillo, C.; Abramova, R.; Assal, A.; Mapara, M.Y.; Pereira, M.R.; Reshef, R. Extended letermovir administration, beyond day 100, is effective for CMV prophylaxis in patients with graft versus host disease. Transpl. Infect. Dis. 2020, 23, e13487. [Google Scholar] [CrossRef]
- Zeiser, R.; Von Bubnoff, N.; Butler, J.; Mohty, M.; Niederwieser, D.; Or, R.; Szer, J.; Wagner, E.M.; Zuckerman, T.; Mahuzier, B.; et al. Ruxolitinib for Glucocorticoid-Refractory Acute Graft-versus-Host Disease. N. Engl. J. Med. 2020, 382, 1800–1810. [Google Scholar] [CrossRef]
- Harris, A.C.; Young, R.; Devine, S.; Hogan, W.J.; Ayuk, F.; Bunworasate, U.; Chanwangphuwana, C.; Efebera, Y.A.; Holler, E.; Litzow, M.; et al. International, multi-center, standardization of acute graft-versus-host disease clinical data collection: A report from the MAGIC consortium. Biol. Blood Marrow Transplant. 2016, 22, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Flowers, M.E.D.; Inamoto, Y.; Carpenter, P.A.; Lee, S.J.; Kiem, H.-P.; Petersdorf, E.W.; Pereira, S.E.; Nash, R.A.; Mielcarek, M.; Fero, M.; et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood 2011, 117, 3214–3219. [Google Scholar] [CrossRef]
- Sharma, N.; Zhao, Q.; Ni, B.; Elder, P.; Puto, M.; Benson, D.; Rosko, A.; Chaudhry, M.; Devarakonda, S.; Bumma, N.; et al. Effect of Early Post-Transplantation Tacrolimus Concentration on the Risk of Acute Graft-Versus-Host Disease in Allogenic Stem Cell Transplantation. Cancers 2021, 13, 613. [Google Scholar] [CrossRef] [PubMed]
- Cutler, C.; Giri, S.; Jeyapalan, S.; Paniagua, D.; Viswaanathan, A.; Antin, J.H. Acute and Chronic Graft-Versus-Host Disease After Allogeneic Peripheral-Blood Stem-Cell and Bone Marrow Transplantation: A Meta-Analysis. J. Clin. Oncol. 2001, 19, 3685–3691. [Google Scholar] [CrossRef]
- Garcia-Cadena, I.; Esquirol, A.; Bosch-Vilaseca, A.; Awol, R.; Novelli, S.; Saavedra, S.; Garrido, A.; Lopez, J.; Caballero, A.C.; Granell, M.; et al. Patterns of infection and infectious-related mortality in patients receiving post-transplant high dose cyclophosphamide as graft-versus-host-drease prophylaxis: Impact of HLA donor matching. Bone Marrow Transplant. 2021, 56, 818–827. [Google Scholar]
- Goldsmith, S.R.; Abid, M.B.; Auletta, J.J.; Bashey, A.; Beitinjaneh, A.; Castillo, P.; Chemaly, R.F.; Chen, M.; Ciurea, S.O.; Dandoy, C.E.; et al. Posttransplant cyclophosphamide is associated with increased cytomegalovirus infection: A CIBMTR analysis. Blood 2021, 137, 3291–3305. [Google Scholar] [CrossRef]
- Crocchiolo, R.; Castagna, L.; Furst, S.; de Villier, R.; Sarina, B.; Bramanti, S.; El-Cheikh, J.; Granata, A.; Harbi, S.; Morabito, L.; et al. The patient’s CMV serological status affects clinical outcome after T-cell replete haplo-HSCT and post-transplant cyclophosphamide. Bone Marrow Transplant. 2016, 51, 1134–1136. [Google Scholar] [CrossRef] [PubMed]
- Pidala, J.; Tomblyn, M.; Nishihori, T.; Ayala, E.; Field, T.; Fernandez, H.; Perez, L.; Locke, F.; Alsina, M.; Ochoa, J.L.; et al. ATG Prevents Severe Acute Graft-versus-Host Disease in Mismatched Unrelated Donor Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2011, 17, 1237–1244. [Google Scholar] [CrossRef]
- Arai, Y.; Tomoyasu, J.; Matsui, H.; Kondo, T.; Takaori-Kondo, A. Efficacy of antithymocyte globulin for allogeneic hematopoietic cell transplantation: A systemic review and meta-analysis. Leuk. Lymphoma 2017, 58, 1840–1848. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Hieber, M.; Schwarck, S.; Stroux, A.; Ganepola, S.; Reinke, P.; Thiel, E.; Uharek, L.; Blau, I.W. Immune reconstitution and cytomegalovirus infection after allogeneic stem cell transplantation: The important impact of in vivo T cell depletion. Int. J. Hematol. 2010, 5, 877–885. [Google Scholar] [CrossRef]


| No Letermovir (n = 143) | Letermovir (n = 119) | p-Value | |
|---|---|---|---|
| Age, median (range) | 60 (18–76) | 56 (21–74) | 0.010 |
| Male | 86 (60.1) | 57 (47.9) | 0.048 |
| Diagnosis | 0.380 | ||
| Acute Myeloid Leukemia | 58 (40.6) | 44 (37.0) | |
| Acute Lymphoblastic Leukemia | 15 (10.5) | 20 (16.8) | |
| Lymphoma (NHL and HL) | 19 (13.3) | 12 (10.1) | |
| Multiple Myeloma | 2 (1.4) | 5 (4.2) | |
| Myelodysplastic Syndrome/Myeloproliferative Neoplasms | 37 (25.9) | 23 (19.3) | |
| Chronic Myeloid Leukemia | 2 (1.4) | 2 (1.7) | |
| Chronic Lymphocytic Leukemia | 6 (4.2) | 6 (5.0) | |
| Other 1 | 4 (2.8) | 7 (5.9) | |
| Donor class | 0.656 | ||
| HLA-mismatched unrelated HLA-matched unrelated | 7 (4.9) 78 (54.5) | 9 (7.6) 62 (52.1) | |
| HLA-matched related | 34 (23.8) | 24 (20.2) | |
| Haploidentical | 24 (16.8) | 24 (20.2) | |
| Stem Cell Source | 0.239 | ||
| Peripheral blood | 115 (80.4) | 86 (72.3) | |
| Bone marrow | 26 (18.2) | 32 (26.9) | |
| Cord blood | 2 (1.4) | 1 (0.8) | |
| Donor positive CMV serostatus 2 | 76 (53.1) | 52 (43.7) | 0.128 |
| Conditioning Regimen | 0.760 | ||
| Myeloablative | 70 (49.0) | 56 (47.1) | |
| Reduced intensity | 73 (51.0) | 63 (52.9) | |
| GVHD Prophylaxis | 0.003 | ||
| Tacrolimus + methotrexate | 94 (65.7) | 67 (56.3) | |
| Tacrolimus + sirolimus | 9 (6.3) | 1 (0.8) | |
| Tacrolimus + mycophenolate | 1 (0.7) | 3 (2.5) | |
| Post-cyclophosphamide | 36 (25.2) | 48 (40.3) | |
| Other | 3 (2.1) | 0 (0.0) | |
| Use of ATG or T-cell depleted graft | 54 (37.7) | 25 (21.0) | 0.004 |
| Acute GVHD Grade | 0.86 | ||
| Grades 0–1 | 65 (45.5) | 50 (42.0) | |
| Grade 2 | 54 (37.8) | 48 (40.3) | |
| Grades 3–4 | 24 (16.8) | 21 (17.7) | |
| Steroid dose ≥ 0.5 mg/kg 3 | 59 (75.6) (n = 78) | 55 (79.7) (n = 69) | 0.65 |
| No Letermovir (n = 143) | Letermovir (n = 119) | p-Value | |
|---|---|---|---|
| CS-CMVi | 81 (56.6) | 29 (24.4) | <0.001 |
| CMV viremia | 108 (75.5) | 47 (39.5) | <0.01 |
| Peak CMV viremia in IU/mL, median (range) | 1003 (51–81300) | 770 (51–18178) | 0.03 |
| Mortality | 62 (43.4) | 38 (31.9) | 0.06 |
| Cause of Death | |||
| Treatment-related | 21 (14.6) | 15 (12.6) | 0.65 |
| Non-relapsed | 14 (9.7) | 10 (8.4) | |
| Disease-related | 27 (18.8) | 13 (10.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolfe, D.; Zhao, Q.; Siegel, E.; Puto, M.; Murphy, D.; Roddy, J.; Efebera, Y.; Tossey, J. Letermovir Prophylaxis and Cytomegalovirus Reactivation in Adult Hematopoietic Cell Transplant Recipients with and without Acute Graft Versus Host Disease. Cancers 2021, 13, 5572. https://doi.org/10.3390/cancers13215572
Wolfe D, Zhao Q, Siegel E, Puto M, Murphy D, Roddy J, Efebera Y, Tossey J. Letermovir Prophylaxis and Cytomegalovirus Reactivation in Adult Hematopoietic Cell Transplant Recipients with and without Acute Graft Versus Host Disease. Cancers. 2021; 13(21):5572. https://doi.org/10.3390/cancers13215572
Chicago/Turabian StyleWolfe, Delaney, Qiuhong Zhao, Emma Siegel, Marcin Puto, Danielle Murphy, Julianna Roddy, Yvonne Efebera, and Justin Tossey. 2021. "Letermovir Prophylaxis and Cytomegalovirus Reactivation in Adult Hematopoietic Cell Transplant Recipients with and without Acute Graft Versus Host Disease" Cancers 13, no. 21: 5572. https://doi.org/10.3390/cancers13215572
APA StyleWolfe, D., Zhao, Q., Siegel, E., Puto, M., Murphy, D., Roddy, J., Efebera, Y., & Tossey, J. (2021). Letermovir Prophylaxis and Cytomegalovirus Reactivation in Adult Hematopoietic Cell Transplant Recipients with and without Acute Graft Versus Host Disease. Cancers, 13(21), 5572. https://doi.org/10.3390/cancers13215572