Added Value of Tomoelastography for Characterization of Pancreatic Neuroendocrine Tumor Aggressiveness Based on Stiffness
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
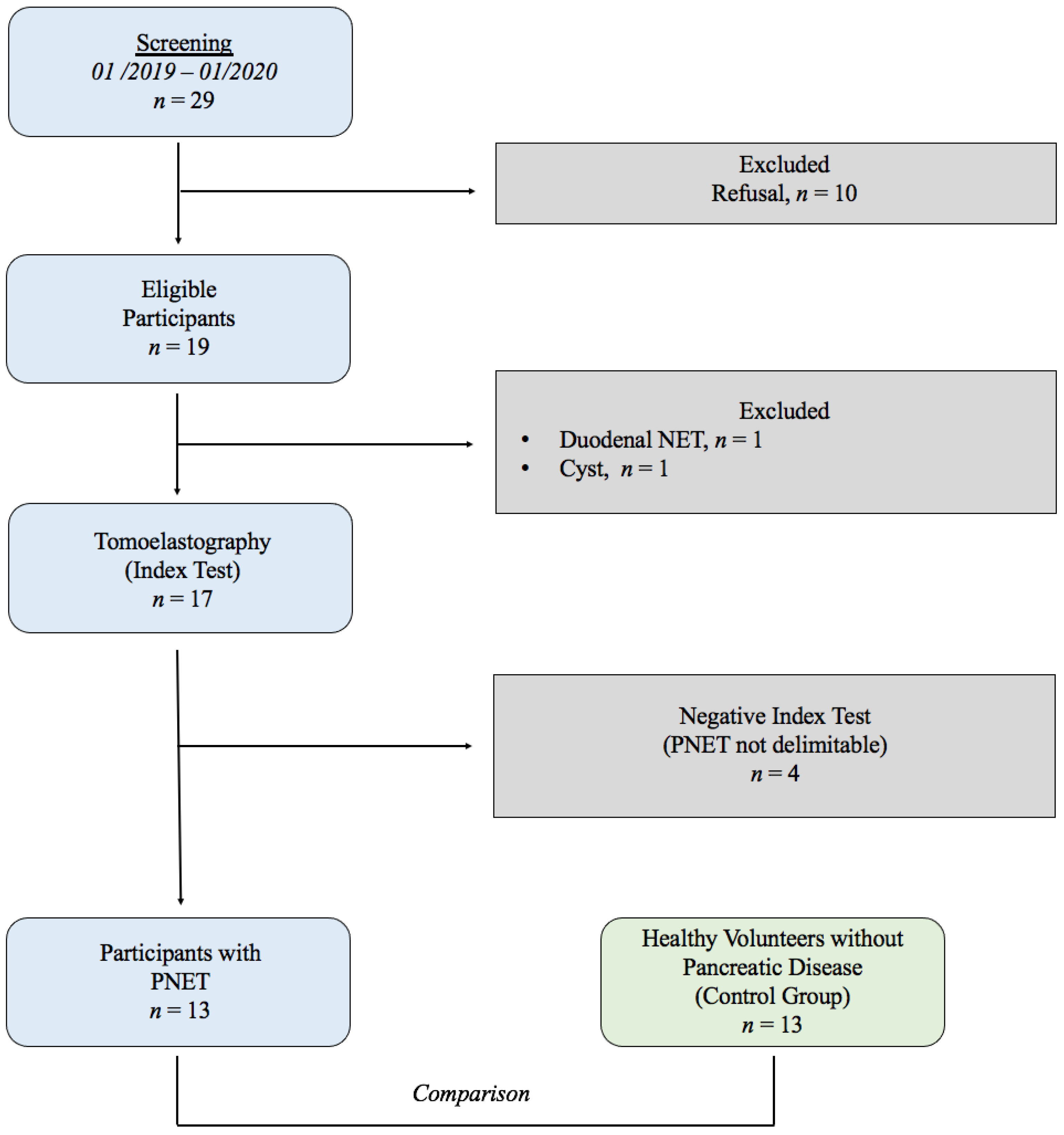
2.1. Study Population
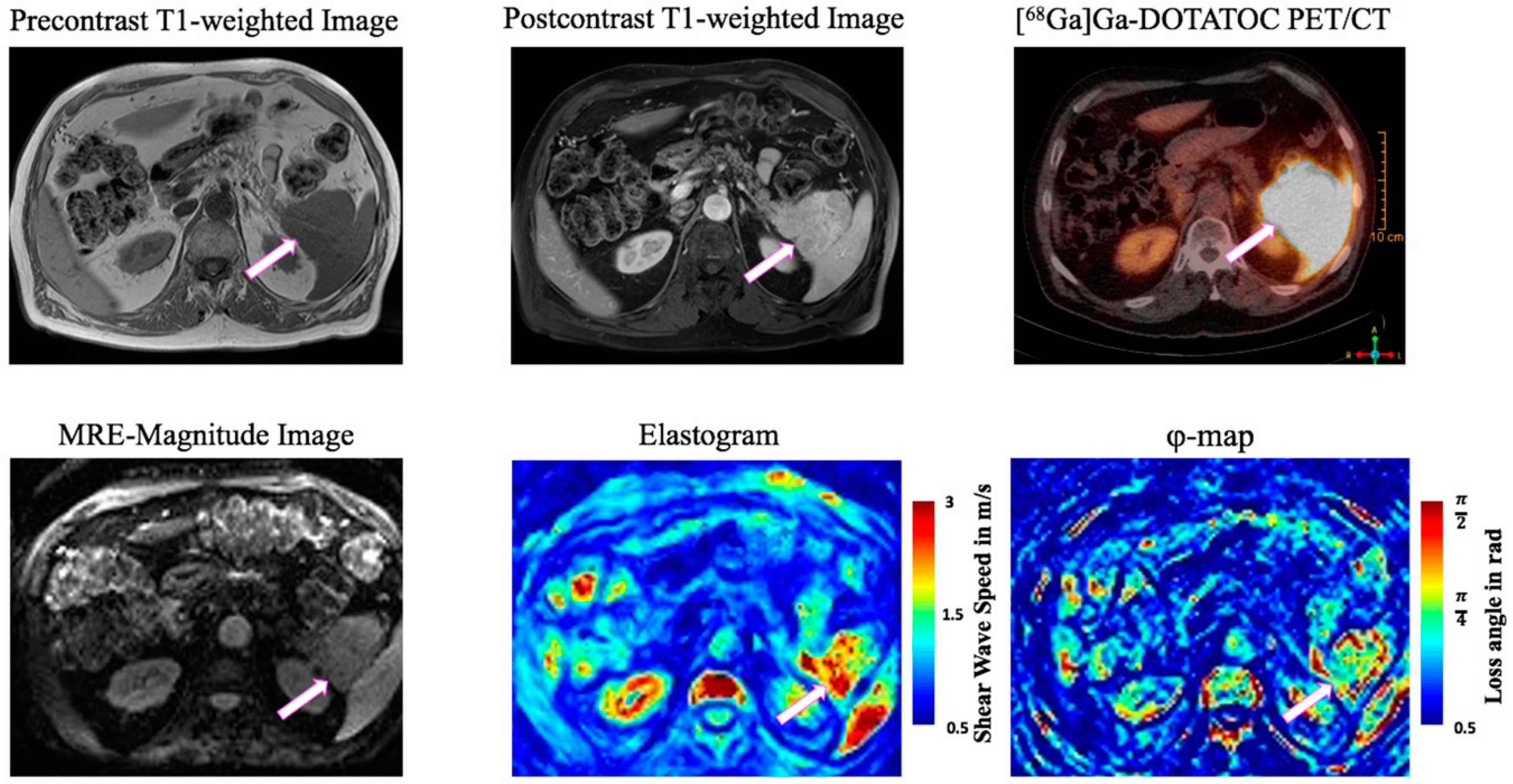
2.2. Multifrequency MRE
2.3. Tomoelastography Postprocessing
2.4. PET Data and Evaluation of Asphericity
2.5. Statistical Methods
3. Results
3.1. Study Population
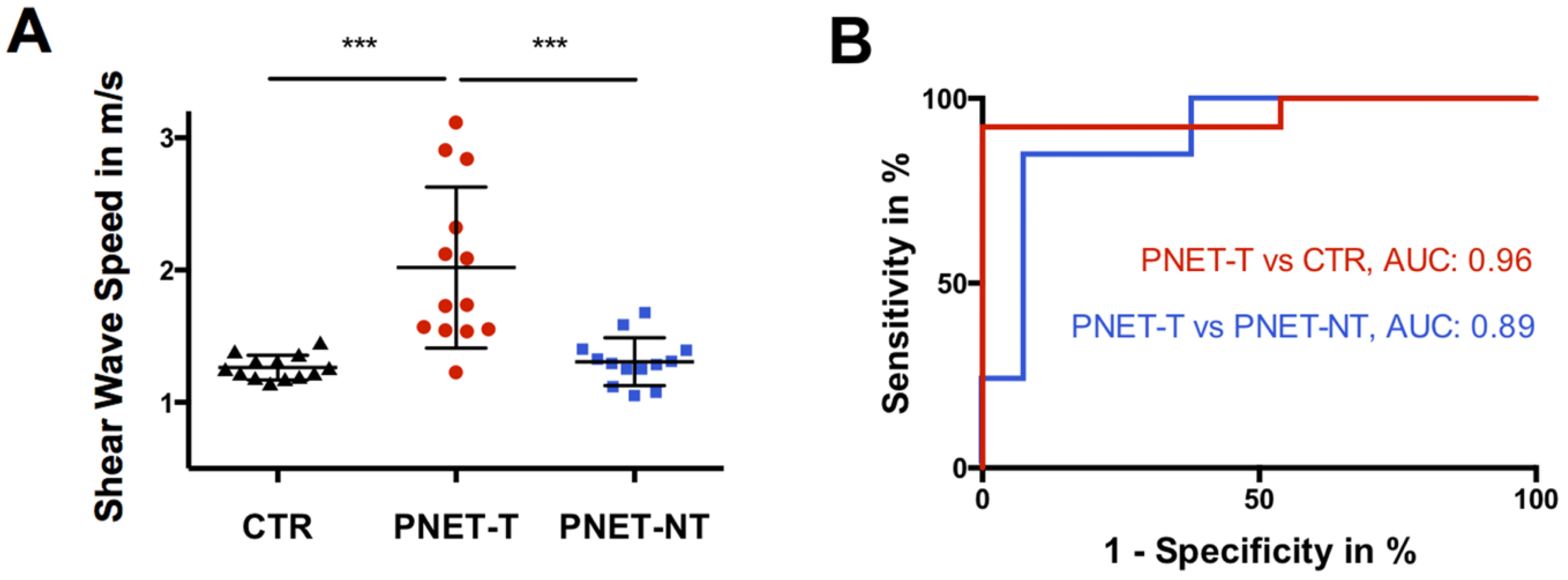
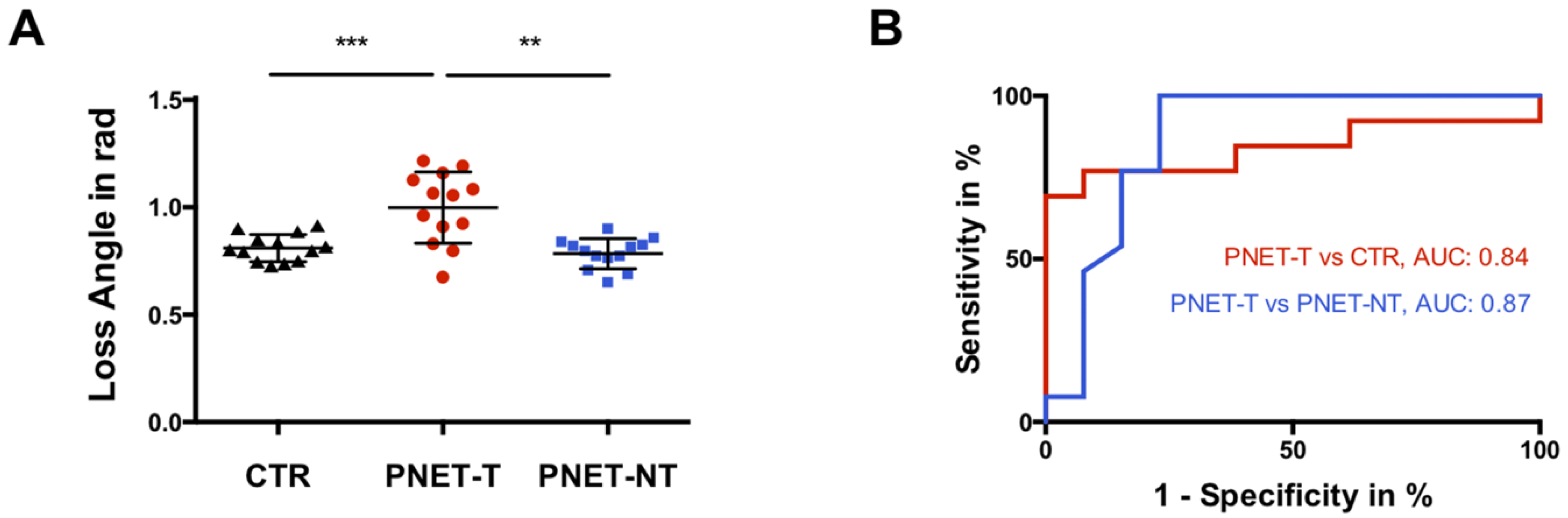
3.2. Viscoelasticity of Pancreatic Neuroendocrine Tumor
3.3. Correlation with Tumor Volume, Functional Imaging and Histopathological Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Patel, N.; Barbieri, A.; Gibson, J. Neuroendocrine Tumors of the Gastrointestinal Tract and Pancreas. Surg. Pathol. Clin. 2019, 12, 1021–1044. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.T.; Howe, J.R. Evaluation and Management of Neuroendocrine Tumors of the Pancreas. Surg. Clin. N. Am. 2019, 99, 793–814. [Google Scholar] [CrossRef] [PubMed]
- Rindi, G.; Wiedenmann, B. Neuroendocrine neoplasms of the gut and pancreas: New insights. Nat. Rev. Endocrinol. 2011, 8, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Tamm, E.P.; Bhosale, P.; Lee, J.H.; Rohren, E.M. State-of-the-art Imaging of Pancreatic Neuroendocrine Tumors. Surg. Oncol. Clin. N. Am. 2016, 25, 375–400. [Google Scholar] [CrossRef] [Green Version]
- Ambrosio, M.R.; Rocca, B.J.; Mastrogiulio, M.G.; Pesci, A.; De Martino, A.; A Mazzei, M.; Volterrani, L.; Arcuri, F.; Cintorino, M.; A Tripodi, S. Cystic gastrointestinal stromal tumors of the pancreas simulating cystoadenocarcinoma. Report of three cases and short review of the literature. Histol. Histopathol. 2014, 29, 1583–1591. [Google Scholar]
- Dromain, C.; Déandréis, D.; Scoazec, J.Y.; Goere, D.; Ducreux, M.; Baudin, E.; Tselikas, L. Imaging of neuroendocrine tumors of the pancreas. Diagn. Interv. Imaging 2016, 97, 1241–1257. [Google Scholar] [CrossRef]
- Lee, N.J.; Hruban, R.H.; Fishman, E.K. Pancreatic neuroendocrine tumor: Review of heterogeneous spectrum of CT appearance. Abdom. Radiol. 2018, 43, 3025–3034. [Google Scholar] [CrossRef]
- Wetz, C.; Apostolova, I.; Steffen, I.G.; Hofheinz, F.; Furth, C.; Kupitz, D.; Ruf, J.; Venerito, M.; Klose, S.; Amthauer, H. Predictive Value of Asphericity in Pretherapeutic [111In]DTPA-Octreotide SPECT/CT for Response to Peptide Receptor Radionuclide Therapy with [177Lu]DOTATATE. Mol. Imaging Biol. 2016, 19, 437–445. [Google Scholar] [CrossRef]
- Wetz, C.; Genseke, P.; Apostolova, I.; Furth, C.; Ghazzawi, S.; Rogasch, J.; Schatka, I.; Kreissl, M.C.; Hofheinz, F.; Grosser, O.S.; et al. The association of intra-therapeutic heterogeneity of somatostatin receptor expression with morphological treatment response in patients undergoing PRRT with [177Lu]-DOTATATE. PLoS ONE 2019, 14, e0216781. [Google Scholar] [CrossRef] [PubMed]
- Wetz, C.; Rogasch, J.; Genseke, P.; Schatka, I.; Furth, C.; Kreissl, M.; Jann, H.; Venerito, M.; Amthauer, H. Asphericity of somatostatin receptor expression in neuroendocrine tumors: An innovative predictor of outcome in everolimus treatment? Diagnostics (Basel) 2020, 10, 732. [Google Scholar] [CrossRef] [PubMed]
- Pavel, M.E.; Hainsworth, J.D.; Baudin, E.; Peeters, M.; Hörsch, D.; Winkler, R.E.; Klimovsky, J.; Lebwohl, D.; Jehl, V.; Wolin, E.M.; et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): A randomised, placebo-controlled, phase 3 study. Lancet 2011, 378, 2005–2012. [Google Scholar] [CrossRef]
- Marticorena Garcia, S.R.; Zhu, L.; Gültekin, E.; Schmuck, R.; Burkhardt, C.; Bahra, M.; Geisel, D.; Shahryari, M.; Braun, J.; Hamm, B.; et al. Tomoelastography for Measurement of Tumor Volume Related to Tissue Stiffness in Pancreatic Ductal Adenocarcinomas. Investig. Radiol. 2020, 55, 769–774. [Google Scholar] [CrossRef]
- Shi, Y.; Gao, F.; Li, Y.; Tao, S.; Yu, B.; Liu, Z.; Liu, Y.; Glaser, K.J.; Ehman, R.L.; Guo, Q. Differentiation of benign and malignant solid pancreatic masses using magnetic resonance elastography with spin-echo echo planar imaging and three-dimensional inversion reconstruction: A prospective study. Eur. Radiol. 2017, 28, 936–945. [Google Scholar] [CrossRef]
- Zhu, L.; Guo, J.; Jin, Z.; Xue, H.; Dai, M.; Zhang, W.; Sun, Z.; Xu, J.; Marticorena Garcia, S.R.; Asbach, P.; et al. Distinguishing pancreatic cancer and autoimmune pancreatitis with in vivo tomoelastography. Eur. Radiol. 2020, 31, 3366–3374. [Google Scholar] [CrossRef] [PubMed]
- Marticorena Garcia, S.R.; Grossmann, M.; Bruns, A.; Dürr, M.; Tzschätzsch, H.; Hamm, B.; Braun, J.; Sack, I.; Guo, J. Tomoelastography Paired with T2* Magnetic Resonance Imaging Detects Lupus Nephritis with Normal Renal Function. Investig. Radiol. 2019, 54, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Shahryari, M.; Tzschätzsch, H.; Guo, J.; Marticorena Garcia, S.R.; Böning, G.; Fehrenbach, U.; Stencel, L.; Asbach, P.; Hamm, B.; Käs, J.A.; et al. Tomoelastography Distinguishes Noninvasively between Benign and Malignant Liver Lesions. Cancer Res. 2019, 79, 5704–5710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dittmann, F.; Hirsch, S.; Tzschätzsch, H.; Guo, J.; Braun, J.; Sack, I. In vivo wideband multifrequency MR elastography of the human brain and liver. Magn. Reson. Med. 2015, 76, 1116–1126. [Google Scholar] [CrossRef] [PubMed]
- Tzschätzsch, H.; Guo, J.; Dittmann, F.; Hirsch, S.; Barnhill, E.; Jöhrens, K.; Braun, J.; Sack, I. Tomoelastography by multifrequency wave number recovery from time-harmonic propagating shear waves. Med. Image Anal. 2016, 30, 1–10. [Google Scholar] [CrossRef]
- Adams, L.C.; Bressem, K.K.; Brangsch, J.; Reimann, C.; Nowak, K.J.; Brenner, W.; Makowski, M.R. Quantitative 3D Assessment of 68Ga-DOTATOC PET/MRI with Diffusion-Weighted Imaging to Assess Imaging Markers for Gastroenteropancreatic Neuroendocrine Tumors: Preliminary Results. J. Nucl. Med. 2019, 61, 1021–1027. [Google Scholar] [CrossRef]
- Hofheinz, F.; Langner, J.; Petr, J.; Beuthien-Baumann, B.; Steinbach, J.; Kotzerke, J.; Hoff, J.V.D. An automatic method for accurate volume delineation of heterogeneous tumors in PET. Med Phys. 2013, 40, 082503. [Google Scholar] [CrossRef]
- Apostolova, I.; Steffen, I.G.; Wedel, F.; Lougovski, A.; Marnitz, S.; Derlin, T.; Amthauer, H.; Buchert, R.; Hofheinz, F.; Brenner, W. Asphericity of pretherapeutic tumour FDG uptake provides independent prognostic value in head-and-neck cancer. Eur. Radiol. 2014, 24, 2077–2087. [Google Scholar] [CrossRef] [PubMed]
- Mullikin, J.C.; Verbeek, P.W. Surface area estimation of digitized planes. Bioimaging 1993, 1, 6–16. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.J.W.L.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-Based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Streitberger, K.J.; Lilaj, L.; Schrank, F.; Braun, J.; Hoffmann, K.T.; Reiss-Zimmermann, M.; Käs, J.A.; Sack, I. How tissue fluidity influences brain tumor progression. Proc. Natl. Acad. Sci. USA 2020, 117, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Barkovskaya, A.; Buffone, A., Jr.; Žídek, M.; Weaver, V.M. Proteoglycans as mediators of cancer tissue mechanics. Fronti. Cell Dev. Biol. 2020, 8, 569377. [Google Scholar] [CrossRef]
- Friedl, P. Reproducibility in Cancer Biology: Rethinking research into metastasis. eLife 2019, 8, e53511. [Google Scholar] [CrossRef]
- Oswald, L.; Grosser, S.; Smith, D.M.; Käs, J.A. Jamming transitions in cancer. J. Phys. D Appl. Phys. 2017, 50, 483001. [Google Scholar] [CrossRef] [Green Version]
- Paszek, M.J.; Zahir, N.; Johnson, K.R.; Lakins, J.N.; Rozenberg, G.I.; Gefen, A.; Reinhart-King, C.; Margulies, S.S.; Dembo, M.; Boettiger, D.; et al. Tensional homeostasis and the malignant phenotype. Cancer Cell 2005, 8, 241–254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reiter, R.; Tzschätzsch, H.; Schwahofer, F.; Haas, M.; Bayerl, C.; Muche, M.; Klatt, D.; Majumdar, S.; Uyanik, M.; Hamm, B.; et al. Diagnostic performance of tomoelastography of the liver and spleen for staging hepatic fibrosis. Eur. Radiol. 2019, 30, 1719–1729. [Google Scholar] [CrossRef] [Green Version]
- Piersma, B.; Hayward, M.; Weaver, V.M. Fibrosis and cancer: A strained relationship. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2020, 1873, 188356. [Google Scholar] [CrossRef]
- Singh, S.; Venkatesh, S.K.; Wang, Z.; Miller, F.H.; Motosugi, U.; Low, R.N.; Hassanein, T.; Asbach, P.; Godfrey, E.M.; Yin, M.; et al. Diagnostic Performance of Magnetic Resonance Elastography in Staging Liver Fibrosis: A Systematic Review and Meta-analysis of Individual Participant Data. Clin. Gastroenterol. Hepatol. 2014, 13, 440–451.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garteiser, P.; Doblas, S.; Van Beers, B. Magnetic resonance elastography of liver and spleen: Methods and applications. NMR Biomed. 2018, 31, e3891. [Google Scholar] [CrossRef]
- Laskaratos, F.M.; Rombouts, K.; Caplin, M.; Toumpanakis, C.; Thirlwell, C.; Mandair, D. Neuroendocrine tumors and fibrosis: An unsolved mystery? Cancer 2017, 123, 4770–4790. [Google Scholar] [CrossRef] [Green Version]
- Buffone, A.; Weaver, V.M. Don’t sugarcoat it: How glycocalyx composition influences cancer progression. J. Cell Biol. 2020, 219, e201910070. [Google Scholar] [CrossRef]
- Lang, S.T.; Guo, J.; Bruns, A.; Dürr, M.; Braun, J.; Hamm, B.; Sack, I.; Marticorena Garcia, S.R. Multiparametric Quantitative MRI for the Detection of IgA Nephropathy Using Tomoelastography, DWI, and BOLD Imaging. Investig. Radiol. 2019, 54, 669–674. [Google Scholar] [CrossRef]
- Marticorena Garcia, S.R.; Fischer, T.; Dürr, M.; Gültekin, E.; Braun, J.; Sack, I.; Guo, J. Multifrequency Magnetic Resonance Elastography for the Assessment of Renal Allograft Function. Investig. Radiol. 2016, 51, 591–595. [Google Scholar] [CrossRef]
- Rishi, A.; Goggins, M.; Wood, L.D.; Hruban, R.H. Pathological and Molecular Evaluation of Pancreatic Neoplasms. Semin. Oncol. 2015, 42, 28–39. [Google Scholar] [CrossRef] [Green Version]
- Dromain, C.; Pavel, M.E.; Ruszniewski, P.; Langley, A.; Massien, C.; Baudin, E.; Caplin, M.E.; on behalf of the CLARINET Study Group. Tumor growth rate as a metric of progression, response, and prognosis in pancreatic and intestinal neuroendocrine tumors. BMC Cancer 2019, 19, 66. [Google Scholar] [CrossRef] [Green Version]
- Eisenhauer, E.; Therasse, P.; Bogaerts, J.; Schwartz, L.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef] [PubMed]
- Northey, J.J.; Przybyla, L.; Weaver, V.M. Tissue Force Programs Cell Fate and Tumor Aggression. Cancer Discov. 2017, 7, 1224–1237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davnall, F.; Yip, C.S.; Ljungqvist, G.; Selmi, M.; Ng, F.; Sanghera, B.; Ganeshan, B.; Miles, K.A.; Cook, G.J.; Goh, V. Assessment of tumor heterogeneity: An emerging imaging tool for clinical practice? Insights Imaging 2012, 3, 573–589. [Google Scholar] [CrossRef] [Green Version]
- Yang, Z.; Tang, L.H.; Klimstra, D.S. Effect of tumor heterogeneity on the assessment of ki67 labeling index in well-differentiated neuroendocrine tumors metastatic to the liver: Implications for prognostic stratification. Am. J. Surg. Pathol. 2011, 35, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.A.; Ilhan, H.; Lehner, S.; Papp, L.; Zsótér, N.; Schatka, I.; Muegge, D.O.; Javadi, M.S.; Higuchi, T.; Buck, A.K.; et al. Pre-therapy somatostatin receptor-based heterogeneity predicts overall survival in pancreatic neuroendocrine tumor patients undergoing peptide receptor radionuclide therapy. Mol. imaging Biol. 2019, 21, 582–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Werner, R.A.; Lapa, C.; Ilhan, H.; Higuchi, T.; Buck, A.K.; Lehner, S.; Bartenstein, P.; Bengel, F.; Schatka, I.; Muegge, D.O.; et al. Survival prediction in patients undergoing radionuclide therapy based on intratumoral somatostatin-receptor heterogeneity. Oncotarget 2016, 8, 7039–7049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, S.; Hallet, J.; Rowsell, C.; Law, C.H. Variability of ki67 labeling index in multiple neuroendocrine tumors specimens over the course of the disease. Eur. J. Surg. Oncol. (EJSO) 2014, 40, 1517–1522. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Kessler, L.; Schaarschmidt, B.M.; Fendler, W.P.; Lahner, H.; Antoch, G.; Umutlu, L.; Herrmann, K.; Rischpler, C. Treatment-related changes in neuroendocrine tumors as assessed by textural features derived from 68Ga-DOTATOC PET/MRI with simultaneous acquisition of apparent diffusion coefficient. BMC Cancer 2020, 20, 326. [Google Scholar] [CrossRef] [Green Version]
- Beier, M.; Sack, I.; Beck-Broichsitter, B.; Hamm, B.; Marticorena Garcia, S.R. Tomoelastography for non-invasive detection of ameloblastoma and metastatic neck lymph nodes. BMJ Case Rep. 2020, 13, e235930. [Google Scholar] [CrossRef]
- Asbach, P.; Ro, S.-R.; Aldoj, N.; Snellings, J.; Reiter, R.; Lenk, J.; Köhlitz, T.; Haas, M.; Guo, J.; Hamm, B.; et al. In Vivo Quantification of Water Diffusion, Stiffness, and Tissue Fluidity in Benign Prostatic Hyperplasia and Prostate Cancer. Investig. Radiol. 2020, 55, 524–530. [Google Scholar] [CrossRef]

| Characteristic | CTR | PNET |
|---|---|---|
| Number of participants | 13 | 13 |
| Number of men | 9 | 9 |
| Number of women | 4 | 4 |
| Age in years | ||
| mean ± SD | 58 ± 13 | 59 ± 17 |
| (range) | (31–76) | (24–79) |
| Body mass index in kg/m2 | ||
| mean ± SD | 24 ± 2 | 27 ± 5 |
| (range) | (20–27) | (20–35) |
| Characteristics | PNET-T | PNET-NT | CTR |
|---|---|---|---|
| SWS in m/s | |||
| mean ± SD | 2.02 ± 0.61 | 1.31 ± 0.18 | 1.26 ± 0.09 |
| (95%-CI) | (1.65–2.39) | (1.20–1.42) | (1.21–1.32) |
| Fluidity expressed as loss angle in rad | |||
| mean ± SD | 1.0 ± 0.17 | 0.78 ± 0.07 | 0.81 ± 0.06 |
| (range) | (0.90–1.10) | (0.74–0.83) | (0.77–0.85) |
| Entity | |||
| Nonfunctional NET | 10/13 (77%) | ||
| Functional NET | 1/13 (8%) * | ||
| Malignant insulinoma | 1/13 (8%) | ||
| NEC | 1/13 (8%) | ||
| Tumor volume in cm3 | |||
| mean ± SD | 55.16 ± 72.05 | ||
| (range) | (0.04–190.53) | ||
| Tumor site (multiple locations possible) | |||
| Head | 5 | ||
| Body | 7 | ||
| Tail | 8 | ||
| Tumor histopathologically proven | 10/13 (77%) | ||
| Grade | |||
| G1 | 1/10 (10%) | ||
| G2 | 8/10 (80%) | ||
| G3 | 1/10 (10%) | ||
| Ki-67 | |||
| mean ± SD | 9 ± 10% | ||
| (range) | 1–30% | ||
| Tumor proven by [68Ga]Ga-DOTATOC PET/CT/PET/MRI | 9/13 (69%) | ||
| SUVmax | |||
| mean ± SD | 45.5 ± 25.6 | ||
| (range) | (13.8–87.9) | ||
| Time between PET/CT/PET/MRI and MRE in months | |||
| mean ± SD | 11 ± 21 | ||
| (range) | (1–68) | ||
| Asphericity (ASP) in % | |||
| mean ± SD | 45.0 ± 20.4 | ||
| (range) | (24.5–84.3) | ||
| Duration of disease in months | |||
| mean ± SD | 24 ± 37 | ||
| (range) | (1–128) | ||
| Presence of metastasis | 7/13 (54%) | ||
| Drug therapy | 6/13 (46%) |
| p | AUC | Cutoff | Sensitivity | Specificity | |
|---|---|---|---|---|---|
| 95%-CI | m/s | 95%-CI | 95%-CI | ||
| Shear Wave Speed | |||||
| PNET-T vs. CTR | <0.001 | 0.96 | 1.49 | 92 | 100 |
| (0.88–1.04) | (64–100) | (75–100) | |||
| PNET-T vs. PNET-NT | <0.001 | 0.89 | 1.46 | 85 | 92 |
| (0.76–1.03) | (55–98) | (64–100) | |||
| Loss Angle | |||||
| PNET-T vs. CTR | 0.003 | 0.84 | 0.92 | 69 | 100 |
| (0.67–1.01) | (38–91) | (75–100) | |||
| PNET-T vs. PNET-NT | 0.001 | 0.87 | 0.83 | 77 | 85 |
| (0.72–1.03) | (46–95) | (55–98) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gültekin, E.; Wetz, C.; Braun, J.; Geisel, D.; Furth, C.; Hamm, B.; Sack, I.; Marticorena Garcia, S.R. Added Value of Tomoelastography for Characterization of Pancreatic Neuroendocrine Tumor Aggressiveness Based on Stiffness. Cancers 2021, 13, 5185. https://doi.org/10.3390/cancers13205185
Gültekin E, Wetz C, Braun J, Geisel D, Furth C, Hamm B, Sack I, Marticorena Garcia SR. Added Value of Tomoelastography for Characterization of Pancreatic Neuroendocrine Tumor Aggressiveness Based on Stiffness. Cancers. 2021; 13(20):5185. https://doi.org/10.3390/cancers13205185
Chicago/Turabian StyleGültekin, Emin, Christoph Wetz, Jürgen Braun, Dominik Geisel, Christian Furth, Bernd Hamm, Ingolf Sack, and Stephan R. Marticorena Garcia. 2021. "Added Value of Tomoelastography for Characterization of Pancreatic Neuroendocrine Tumor Aggressiveness Based on Stiffness" Cancers 13, no. 20: 5185. https://doi.org/10.3390/cancers13205185
APA StyleGültekin, E., Wetz, C., Braun, J., Geisel, D., Furth, C., Hamm, B., Sack, I., & Marticorena Garcia, S. R. (2021). Added Value of Tomoelastography for Characterization of Pancreatic Neuroendocrine Tumor Aggressiveness Based on Stiffness. Cancers, 13(20), 5185. https://doi.org/10.3390/cancers13205185







