gsp Mutation Is Not a Molecular Biomarker of Long-Term Response to First-Generation Somatostatin Receptor Ligands in Acromegaly
Abstract
Simple Summary
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Patients
2.3. Data Collection
2.4. DNA and RNA Extraction
2.5. DNA Sequencing
2.6. qPCR
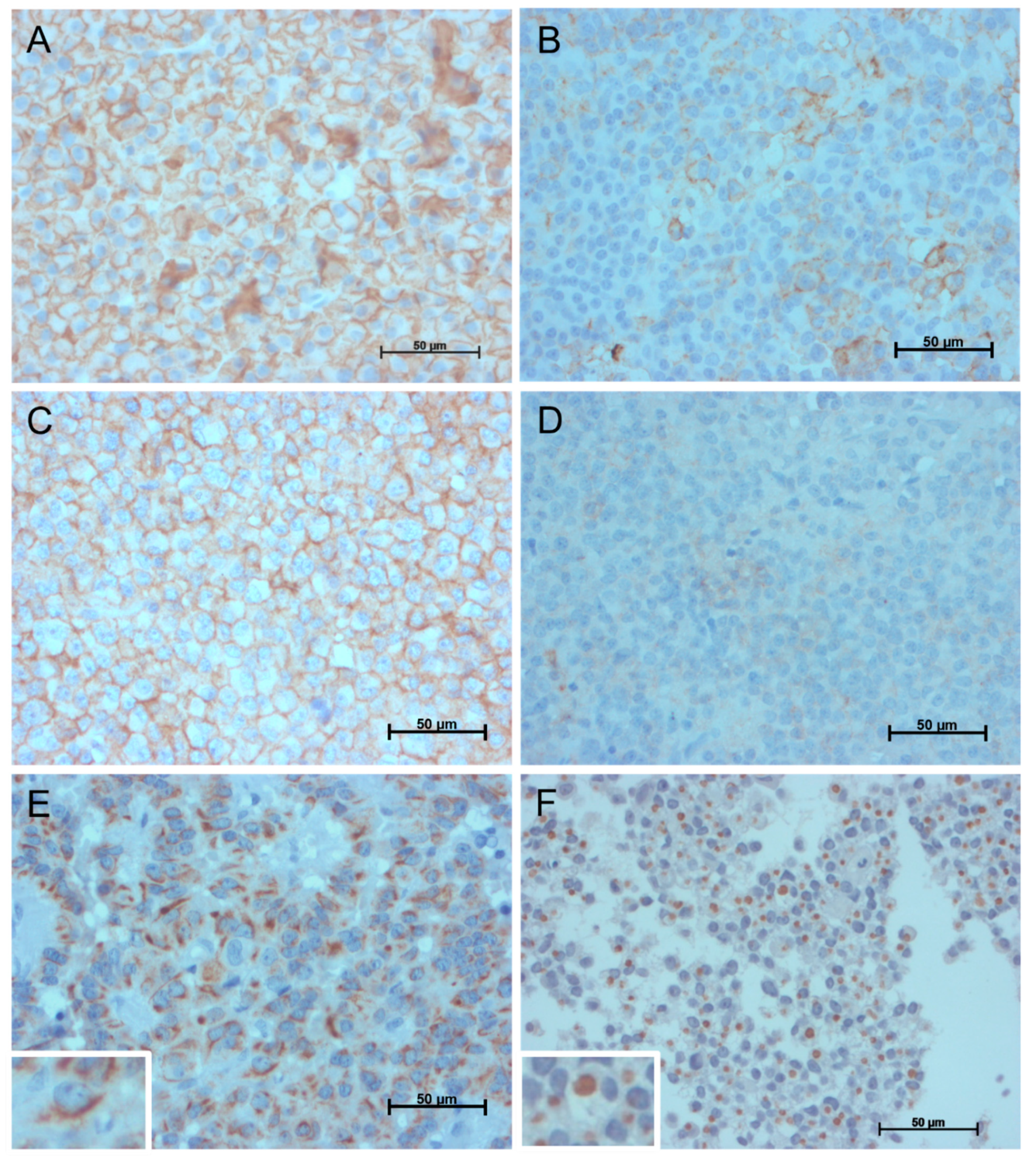
2.7. Immunohistochemistry
2.8. Statistical Analysis
3. Results
3.1. Patient and Sample Characteristics
3.2. gsp Mutation
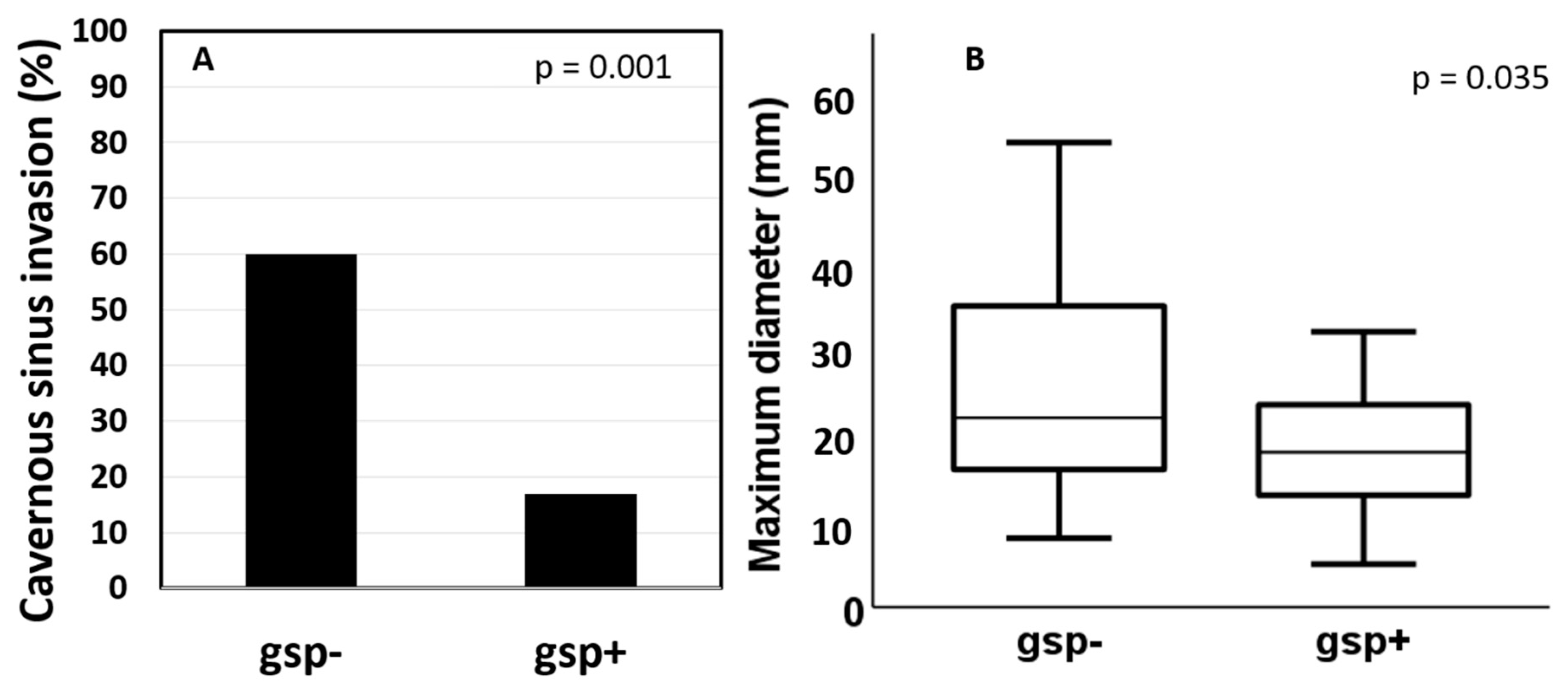
3.3. Predictors of Response to fg-SRL Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katznelson, L.; Laws, E.R.; Melmed, S.; Molitch, M.E.; Murad, M.H.; Utz, A.; Wass, J.A.; Society, E. Acromegaly: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2014, 99, 3933–3951. [Google Scholar] [CrossRef]
- Antunes, X.; Ventura, N.; Camilo, G.B.; Wildemberg, L.E.; Guasti, A.; Pereira, P.J.M.; Camacho, A.H.S.; Chimelli, L.; Niemeyer, P.; Gadelha, M.R.; et al. Predictors of surgical outcome and early criteria of remission in acromegaly. Endocrine 2018, 60, 415–422. [Google Scholar] [CrossRef]
- Shen, M.; Tang, Y.; Shou, X.; Wang, M.; Zhang, Q.; Qiao, N.; Ma, Z.; Ye, Z.; He, W.; Zhang, Y.; et al. Surgical Results and Predictors of Initial and Delayed Remission for Growth Hormone-Secreting Pituitary Adenomas Using the 2010 Consensus Criteria in 162 Patients from a Single Center. World Neurosurg. 2018, 124, e39–e50. [Google Scholar] [CrossRef]
- Colao, A.; Auriemma, R.S.; Pivonello, R.; Kasuki, L.; Gadelha, M.R. Interpreting biochemical control response rates with first-generation somatostatin analogues in acromegaly. Pituitary 2016, 19, 235–247. [Google Scholar] [CrossRef]
- Lania, A.; Mantovani, G.; Spada, A. Genetics of pituitary tumors: Focus on G-protein mutations. Exp. Biol. Med. 2003, 228, 1004–1017. [Google Scholar] [CrossRef]
- Efstathiadou, Z.A.; Bargiota, A.; Chrisoulidou, A.; Kanakis, G.; Papanastasiou, L.; Theodoropoulou, A.; Tigas, S.K.; Vassiliadi, D.A.; Alevizaki, M.; Tsagarakis, S. Impact of gsp mutations in somatotroph pituitary adenomas on growth hormone response to somatostatin analogs: A meta-analysis. Pituitary 2015, 18, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Fougner, S.L.; Borota, O.C.; Berg, J.P.; Hald, J.K.; Ramm-Pettersen, J.; Bollerslev, J. The clinical response to somatostatin analogues in acromegaly correlates to the somatostatin receptor subtype 2a protein expression of the adenoma. Clin. Endocrinol. 2008, 68, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Sohn, S.; Lee, M.; Park, C.; Jung, J.; Park, S. Effect of gsp oncogene on somatostatin receptor subtype 1 and 2 mRNA levels in GHRH-responsive GH3 cells. Pituitary 2005, 8, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Taboada, G.F.; Neto, L.V.; Luque, R.M.; Córdoba-Chacón, J.; de Oliveira Machado, E.; de Carvalho, D.P.; Kineman, R.D.; Gadelha, M.R. Impact of gsp oncogene on the mRNA content for somatostatin and dopamine receptors in human somatotropinomas. Neuroendocrinology 2011, 93, 40–47. [Google Scholar] [CrossRef]
- Larkin, S.; Reddy, R.; Karavitaki, N.; Cudlip, S.; Wass, J.; Ansorge, O. Granulation pattern, but not GSP or GHR mutation, is associated with clinical characteristics in somatostatin-naive patients with somatotroph adenomas. Eur. J. Endocrinol. 2013, 168, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Gadelha, M.R.; Kasuki, L.; Korbonits, M. Novel pathway for somatostatin analogs in patients with acromegaly. Trends Endocrinol. Metab. 2013, 24, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Yang, I.M.; Woo, J.T.; Kim, S.W.; Kim, J.W.; Kim, Y.S.; Choi, Y.K. Characteristics of acromegalic patients with a good response to octreotide, a somatostatin analogue. Clin. Endocrinol. 1995, 42, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Barlier, A.; Gunz, G.; Zamora, A.J.; Morange-Ramos, I.; Figarella-Branger, D.; Dufour, H.; Enjalbert, A.; Jaquet, P. Pronostic and therapeutic consequences of Gs alpha mutations in somatotroph adenomas. J. Clin. Endocrinol. Metab. 1998, 83, 1604–1610. [Google Scholar] [CrossRef][Green Version]
- Micko, A.S.; Wöhrer, A.; Wolfsberger, S.; Knosp, E. Invasion of the cavernous sinus space in pituitary adenomas: Endoscopic verification and its correlation with an MRI-based classification. J. Neurosurg. 2015, 122, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Feelders, R.A.; van der Pas, R.; Kros, J.M.; Waaijers, M.; Sprij-Mooij, D.; Neggers, S.J.; van der Lelij, A.J.; Minuto, F.; Lamberts, S.W.; et al. Immunoreactivity score using an anti-sst2A receptor monoclonal antibody strongly predicts the biochemical response to adjuvant treatment with somatostatin analogs in acromegaly. J. Clin. Endocrinol. Metab. 2013, 98, E66–E71. [Google Scholar] [CrossRef] [PubMed]
- Coelho, M.C.A.; Vasquez, M.L.; Wildemberg, L.E.; Vázquez-Borrego, M.C.; Bitana, L.; Camacho, A.H.d.S.; Silva, D.; Ogino, L.L.; Ventura, N.; Chimelli, L.; et al. Molecular evidence and clinical importance of β-arrestins expression in patients with acromegaly. J. Cell Mol. Med. 2018, 22, 2110–2116. [Google Scholar] [CrossRef]
- Obari, A.; Sano, T.; Ohyama, K.; Kudo, E.; Qian, Z.R.; Yoneda, A.; Rayhan, N.; Mustafizur Rahman, M.; Yamada, S. Clinicopathological features of growth hormone-producing pituitary adenomas: Difference among various types defined by cytokeratin distribution pattern including a transitional form. Endocr. Pathol. 2008, 19, 82–91. [Google Scholar] [CrossRef]
- Gadelha, M.R. A paradigm shift in the medical treatment of acromegaly: From a ‘trial and error’ to a personalized therapeutic decision-making process. Clin. Endocrinol. 2015, 83, 1–2. [Google Scholar] [CrossRef]
- Kasuki, L.; Wildemberg, L.E.; Gadelha, M.R. MANAGEMENT OF ENDOCRINE DISEASE: Personalized medicine in the treatment of acromegaly. Eur. J. Endocrinol. 2018, 178, R89–R100. [Google Scholar] [CrossRef]
- Puig-Domingo, M.; Marazuela, M. Precision medicine in the treatment of acromegaly. Minerva Endocrinol. 2019, 44, 169–175. [Google Scholar] [CrossRef]
- Yuen, K.C.J. Medical therapy for acromegaly: Towards the practice of a personalized medicine approach. Endocr. Pract. 2019, 25, 396–398. [Google Scholar] [CrossRef]
- Ezzat, S.; Caspar-Bell, G.M.; Chik, C.L.; Denis, M.C.; Domingue, M.; Imran, S.A.; Johnson, M.D.; Lochnan, H.A.; Grégoire Nyomba, B.L.; Prebtani, A.; et al. Predictive markers for postsurgical medical management of acromegaly: A systematic review and consensus treatment guideline. Endocr. Pract. 2019, 25, 379–393. [Google Scholar] [CrossRef] [PubMed]
- Corica, G.; Ceraudo, M.; Campana, C.; Nista, F.; Cocchiara, F.; Boschetti, M.; Zona, G.; Criminelli, D.; Ferone, D.; Gatto, F. Octreotide-Resistant Acromegaly: Challenges and Solutions. Ther. Clin. Risk Manag. 2020, 16, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Fougner, S.L.; Casar-Borota, O.; Heck, A.; Berg, J.P.; Bollerslev, J. Adenoma granulation pattern correlates with clinical variables and effect of somatostatin analogue treatment in a large series of patients with acromegaly. Clin. Endocrinol. 2012, 76, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Vieira Neto, L.; Taboada, G.F.; Gadelha, M.R. Somatostatin receptors subtypes 2 and 5, dopamine receptor type 2 expression and gsp status as predictors of octreotide LAR responsiveness in acromegaly. Arq. Bras. Endocrinol. Metabol. 2008, 52, 1288–1295. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Faglia, G.; Arosio, M.; Spada, A. GS protein mutations and pituitary tumors: Functional correlates and possible therapeutic implications. Metabolism 1996, 45, 117–119. [Google Scholar] [CrossRef]
- Spada, A.; Arosio, M.; Bochicchio, D.; Bazzoni, N.; Vallar, L.; Bassetti, M.; Faglia, G. Clinical, biochemical, and morphological correlates in patients bearing growth hormone-secreting pituitary tumors with or without constitutively active adenylyl cyclase. J. Clin. Endocrinol. Metab. 1990, 71, 1421–1426. [Google Scholar] [CrossRef] [PubMed]
- Freda, P.U.; Chung, W.K.; Matsuoka, N.; Walsh, J.E.; Kanibir, M.N.; Kleinman, G.; Wang, Y.; Bruce, J.N.; Post, K.D. Analysis of GNAS mutations in 60 growth hormone secreting pituitary tumors: Correlation with clinical and pathological characteristics and surgical outcome based on highly sensitive GH and IGF-I criteria for remission. Pituitary 2007, 10, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Pokrajac, A.; Claridge, A.G.; Shakoor, S.K.; Trainer, P.J. The octreotide test dose is not a reliable predictor of the subsequent response to somatostatin analogue therapy in patients with acromegaly. Eur. J. Endocrinol. 2006, 154, 267–274. [Google Scholar] [CrossRef]
- Gadelha, M.R.; Kasuki, L.; Korbonits, M. The genetic background of acromegaly. Pituitary 2017, 20, 10–21. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, M.S.; Park, Y.J.; Kim, S.W.; Park, D.J.; Park, K.S.; Kim, S.Y.; Cho, B.Y.; Lee, H.K.; Jung, H.W.; et al. Prevalence of Gs alpha mutations in Korean patients with pituitary adenomas. J. Endocrinol. 2001, 168, 221–226. [Google Scholar] [CrossRef]
- Park, C.; Yang, I.; Woo, J.; Kim, S.; Kim, J.; Kim, Y.; Sohn, S.; Kim, E.; Lee, M.; Park, H.; et al. Somatostatin (SRIF) receptor subtype 2 and 5 gene expression in growth hormone-secreting pituitary adenomas: The relationship with endogenous srif activity and response to octreotide. Endocr. J. 2004, 51, 227–236. [Google Scholar] [CrossRef][Green Version]
- Corbetta, S.; Ballaré, E.; Mantovani, G.; Lania, A.; Losa, M.; Di Blasio, A.M.; Spada, A. Somatostatin receptor subtype 2 and 5 in human GH-secreting pituitary adenomas: Analysis of gene sequence and mRNA expression. Eur. J. Clin. Investig. 2001, 31, 208–214. [Google Scholar] [CrossRef]
- Wildemberg, L.E.; Vieira Neto, L.; Costa, D.F.; Nasciutti, L.E.; Takiya, C.M.; Alves, L.M.; Gadelha, M.R. Validation of immunohistochemistry for somatostatin receptor subtype 2A in human somatotropinomas: Comparison between quantitative real time RT-PCR and immunohistochemistry. J. Endocrinol. Investig. 2012, 35, 580–584. [Google Scholar] [CrossRef]
- Iacovazzo, D.; Carlsen, E.; Lugli, F.; Chiloiro, S.; Piacentini, S.; Bianchi, A.; Giampietro, A.; Mormando, M.; Clear, A.J.; Doglietto, F.; et al. Factors predicting pasireotide responsiveness in somatotroph pituitary adenomas resistant to first-generation somatostatin analogues: An immunohistochemical study. Eur. J. Endocrinol. 2016, 174, 241–250. [Google Scholar] [CrossRef]
- Wildemberg, L.E.; Neto, L.V.; Costa, D.F.; Nasciuti, L.E.; Takiya, C.M.; Alves, L.M.; Rebora, A.; Minuto, F.; Ferone, D.; Gadelha, M.R. Low somatostatin receptor subtype 2, but not dopamine receptor subtype 2 expression predicts the lack of biochemical response of somatotropinomas to treatment with somatostatin analogs. J. Endocrinol. Investig. 2013, 36, 38–43. [Google Scholar] [CrossRef]
- Kiseljak-Vassiliades, K.; Carlson, N.E.; Borges, M.T.; Kleinschmidt-DeMasters, B.K.; Lillehei, K.O.; Kerr, J.M.; Wierman, M.E. Growth hormone tumor histological subtypes predict response to surgical and medical therapy. Endocrine 2015, 49, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Gatto, F.; Biermasz, N.R.; Feelders, R.A.; Kros, J.M.; Dogan, F.; van der Lely, A.J.; Neggers, S.J.; Lamberts, S.W.; Pereira, A.M.; Ferone, D.; et al. Low beta-arrestin expression correlates with the responsiveness to long-term somatostatin analog treatment in acromegaly. Eur. J. Endocrinol. 2016, 174, 651–662. [Google Scholar] [CrossRef][Green Version]
- Selek, A.; Cetinarslan, B.; Gurbuz, Y.; Tarkun, I.; Canturk, Z.; Cabuk, B. Aromatase enzyme expression in acromegaly and its possible relationship with disease prognosis. Endocrine 2015, 49, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Coelho, M.C.A.; Vasquez, M.L.; Wildemberg, L.E.; Vázquez-Borrego, M.C.; Bitana, L.; Camacho, A.H.D.S.; Silva, D.; Ogino, L.L.; Ventura, N.; Sánchez-Sánchez, R.; et al. Clinical significance of filamin A in patients with acromegaly and its association with somatostatin and dopamine receptor profiles. Sci. Rep. 2019, 9, 1122. [Google Scholar] [CrossRef] [PubMed]
- Peverelli, E.; Treppiedi, D.; Giardino, E.; Vitali, E.; Lania, A.G.; Mantovani, G. Dopamine and Somatostatin Analogues Resistance of Pituitary Tumors: Focus on Cytoskeleton Involvement. Front. Endocrinol. 2015, 6, 187. [Google Scholar] [CrossRef] [PubMed]
- Wildemberg, L.E.; da Silva Camacho, A.H.; Miranda, R.L.; Elias, P.C.L.; de Castro Musolino, N.R.; Nazato, D.; Jallad, R.; Huayllas, M.K.P.; Mota, J.I.; Almeida, T.; et al. Machine learning-based prediction model for treatment of acromegaly with first-generation somatostatin receptor ligands. J. Clin. Endocrinol. Metab. 2021. [Google Scholar] [CrossRef] [PubMed]
- Nista, F.; Corica, G.; Castelletti, L.; Khorrami, K.; Campana, C.; Cocchiara, F.; Zoppoli, G.; Prior, A.; Rossi, D.C.; Zona, G.; et al. Clinical and Radiological Predictors of Biochemical Response to First-Line Treatment With Somatostatin Receptor Ligands in Acromegaly: A Real-Life Perspective. Front. Endocrinol. 2021, 12, 677919. [Google Scholar] [CrossRef] [PubMed]

| gsp+ | gsp- | p-Value | |
|---|---|---|---|
| Frequency–n (%) | 54 (40%) | 82 (60%) | NA |
| Sex (Male)–n (%) | 24 (45%) | 38 (46%) | 0.858 |
| Age (years) | 45 (23–68) | 43 (17–69) | 0.413 |
| GH at diagnosis (ng/mL) | 46 (7–611) | 42 (1.1–491) | 0.868 |
| IGF-I at diagnosis (xULN) | 3.8 (1.3–10.2) | 3.9 (1.3–11.4) | 0.736 |
| Diameter (mm) | 18 (5–42) | 22 (8–54) | 0.035 |
| Macroadenoma–n (%) | 44 (96%) | 62 (95%) | 0.660 |
| Cavernous sinus invasion–n (%) | 4 (17%) | 19 (60%) | 0.001 |
| SST2 mRNA (copy number) | 657 (69–1597) | 415 (17–3690) | 0.305 |
| SST5 mRNA (copy number) | 40 (0.3–239) | 102 (4.7–1318) | 0.013 |
| High SST2 IRS–n (%) | 35 (85%) | 44 (70%) | 0.257 |
| High SST5 IRS–n (%) | 18 (43%) | 41 (64%) | 0.047 |
| Sparsely granulated–n (%) | 28 (70%) | 33 (55%) | 0.148 |
| Biochemical control (%)–n = 81 | 11 (37%) | 13 (25%) | 0.219 |
| GH reduction * (%)–n= 81 | 52 (−19–93) | 44 (−41–88) | 0.382 |
| IGF-I reduction * (%)–n=81 | 47 (−4–83) | 35 (−8–90) | 0.682 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wildemberg, L.E.; Henriques, D.; Elias, P.C.L.; Lima, C.H.d.A.; Musolino, N.R.d.C.; Camacho, A.H.S.; Faria, O.; Nazato, D.; Abucham, J.; Vilar, L.; et al. gsp Mutation Is Not a Molecular Biomarker of Long-Term Response to First-Generation Somatostatin Receptor Ligands in Acromegaly. Cancers 2021, 13, 4857. https://doi.org/10.3390/cancers13194857
Wildemberg LE, Henriques D, Elias PCL, Lima CHdA, Musolino NRdC, Camacho AHS, Faria O, Nazato D, Abucham J, Vilar L, et al. gsp Mutation Is Not a Molecular Biomarker of Long-Term Response to First-Generation Somatostatin Receptor Ligands in Acromegaly. Cancers. 2021; 13(19):4857. https://doi.org/10.3390/cancers13194857
Chicago/Turabian StyleWildemberg, Luiz Eduardo, Daniel Henriques, Paula C. L. Elias, Carlos Henrique de A. Lima, Nina R. de Castro Musolino, Aline Helen Silva Camacho, Olivia Faria, Debora Nazato, Julio Abucham, Lucio Vilar, and et al. 2021. "gsp Mutation Is Not a Molecular Biomarker of Long-Term Response to First-Generation Somatostatin Receptor Ligands in Acromegaly" Cancers 13, no. 19: 4857. https://doi.org/10.3390/cancers13194857
APA StyleWildemberg, L. E., Henriques, D., Elias, P. C. L., Lima, C. H. d. A., Musolino, N. R. d. C., Camacho, A. H. S., Faria, O., Nazato, D., Abucham, J., Vilar, L., Mota, J. I., Huayllas, M. K. P., Chimelli, L., Castro, M. d., Kasuki, L., & Gadelha, M. R. (2021). gsp Mutation Is Not a Molecular Biomarker of Long-Term Response to First-Generation Somatostatin Receptor Ligands in Acromegaly. Cancers, 13(19), 4857. https://doi.org/10.3390/cancers13194857






